Abstract
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive and safe technique for a sampling of mediastinal lesions. Indications for EBUS-TBNA have gradually expanded since its introduction. The usual approach to cytological sampling of the thyroid gland is percutaneous ultrasound-guided fine needle aspiration (US-FNA) performed under local anesthesia. US-FNA may be risky or not feasible in intrathoracic/substernal thyroid location. Feasibility of aspirating thyroid lesions with EBUS-TBNA has been occasionally reported. We report two patients wherein EBUS-TBNA was utilized for thyroid lesion aspiration and definitive diagnosis. We highlight the utility and safety of EBUS-TBNA in the evaluation of intrathoracic thyroid lesions wherein image-guided percutaneous aspiration may be risky/sometimes impossible to perform. A systematic review of literature has also been performed summarizing and discussing the issues pertaining to EBUS-TBNA of the thyroid gland.
KEY WORDS: Endobronchial ultrasound, thyroid, transbronchial needle aspiration
INTRODUCTION
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive and safe technique that enables accurate diagnosis in various mediastinal lesions (masses/lymph nodes).[1] Indications of EBUS-TBNA have gradually expanded with use being reported for other indications such as intravascular/transvascular needle aspiration, transbronchial needle injection into lung tumors, and others.
Thyroid lesions are common in clinical practice, increasingly reported in the era of advanced imaging techniques and most are benign. Exclusion of malignancy however remains a major concern.[2] Percutaneous ultrasound-guided fine needle aspiration (US-FNA) is the most often utilized modality for this purpose and which is safe and has high diagnostic accuracy.[3] However, US-FNA may be risky and often impossible in thyroid lesions which are intrathoracic. For diagnostic evaluation of these lesions, invasive procedures such as mediastinoscopy or surgical biopsy may be required.
Utilization of EBUS-TBNA for evaluation of thyroid lesions has been described in a few reports.[4,5,6] Herein, we described two patients wherein EBUS-TBNA was utilized to establish a definitive diagnosis from thyroid lesion. We also perform a systematic review of the literature on the use of EBUS-TBNA for thyroid aspiration.
CASE REPORTS
Case 1
A 78-year-old never-smoker male presented with a history of dry cough and insidious onset shortness of breath for 3 months. Shortness of breath had gradually progressed. There was no history of chest pain, hemoptysis, wheeze, or weight loss. Past history was not significant. The patient had received oral antibiotics and cough suppressants over last 3 months without any symptomatic relief.
On physical examination, pulse rate was 70/min, respiratory rate 16/min, and an expiratory stridor was audible. There was no use of accessory muscles of respiration and saturation while breathing room air was 95%. Rest of the general physical, respiratory system, and examination of other systems was normal. Routine blood investigations including hemoglobin, total and differential leukocyte count, platelets, and renal and liver function tests were normal. Sputum smear examination for acid-fast bacilli and sputum cultures were negative on two previous occasions.
Posteroanterior chest radiograph demonstrated mediastinal widening, tracheal displacement to the right side and narrowing of midtracheal lumen [Figure 1a]. Contrast-enhanced computed tomography (CT) scan of thorax demonstrated a large intrathoracic mass in contiguity with the left lobe of the thyroid gland, with extension into tracheoesophageal groove causing significant compression of the tracheal lumen. The mass was heterogeneous in appearance with few areas of calcification [Figure 1b]. There was no mediastinal lymphadenopathy, pleural, or pericardial effusion. On18 F-fluorodeoxyglucose (FDG)-positron emission tomography-CT scan, the mass was intensely FDG-avid [Figure 1c].
Figure 1.
(a) Posteroanterior chest radiograph depicting mediastinal widening with tracheal displacement to the right side. (b) Coronal computed tomographic images of thoracic computed tomography showing large heterogeneous mediastinal mass with tracheal compression and displacement. (c) 18F-fluorodeoxyglucose-positron emission tomography-computed tomography scan showing intense fluorodeoxyglucose-avidity in the mass
In view of the possibility of a malignant mediastinal mass with possible origin from the thyroid, EBUS-TBNA was planned. EBUS was performed under mild sedation using the Olympus BF-UC-180 F scope (Olympus Corporation, Japan). On airway examination, extrinsic compression of trachea (starting 3 cm below vocal cords) from the left lateral wall was noted. There was no tracheal mucosal infiltration. EBUS showed a large heterogeneous mass in the upper left paratracheal (2 L) location from which three EBUS-TBNA aspirates were obtained using the 21-G needle [Figure 2]. Cytopathological examination of the aspirates demonstrated relatively monomorphic population of round cells arranged in microfollicular microacinar pattern suggestive of thyroid adenoma. The patient underwent total thyroidectomy via median sternotomy approach. Histopathological examination of the excised specimen showed features of follicular adenoma. There were no postoperative complications and patient recovered uneventfully.
Figure 2.
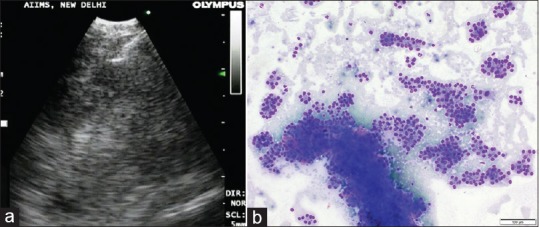
(a) Endobronchial ultrasound image of needle aspiration of the thyroid mass. (b) Cytopathological examination of the endobronchial ultrasound-guided transbronchial needle aspiration aspirate. May-Grünwald-Giemsa stain shows numerous microfollicles and few cohesive fragments of follicular cells. Original magnification × 100
Case 2
A 60-year-old female presented with worsening breathlessness and dry cough of 1-month duration. The patient was diagnosed with interstitial lung disease (ILD) (Idiopathic Interstitial Pneumonia – Nonspecific Interstitial Pneumonia [NSIP] pattern) 2 years previously and was treated with oral immunosuppressive treatment gradually tapered over 1-year duration following which the patient had improved and remained asymptomatic.
General physical examination was unremarkable. On respiratory system examination, bibasilar velcro crepitations were audible. In view of a history of subacute worsening of symptoms, a possibility of disease worsening was considered and a CT scan of the thorax was advised. CT demonstrated worsening of parenchymal lung fibrosis as compared to the older scan and the presence of ground glass opacities consistent with progressive ILD [Figure 3a]. In addition, mediastinal soft tissue opacity with internal hyperdensity was visualized in the upper left paratracheal location in possible relation to the left lobe of the thyroid gland [Figure 3b]. In view of the intrathoracic location of the lesion with possible origin from thyroid, EBUS-TBNA was planned.
Figure 3.
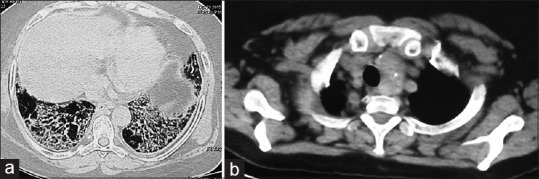
(a) Computed tomography scan of the thorax (lung window section) showing septal thickening and ground glass opacity consistent with nonspecific interstitial pneumonia. (b) Computed tomography (mediastinal window section) demonstrating a left upper paratracheal mass with internal hyperdensity in relation of the left lobe of thyroid
On EBUS examination, prominent soft tissue was visualized in the upper left paratracheal location and two EBUS-TBNA passes were performed using the 21 G needle. Rapid onsite evaluation of the aspirates was consistent with benign thyroid follicular tissue. Final cytopathological examination of the aspirates showed benign follicular cells in the background of colloid. The patient was reassured regarding the benign nature of the mediastinal lesion, and immunosuppressive medications were initiated for the progressive NSIP.
Systematic review
We performed a systematic search of the PubMed and EMBASE databases (2004–2015) to identify the studies reporting the utilization of EBUS-TBNA for thyroid aspiration using the following search terms – ([“EBUS” or “EBUS-TBNA” or “TBNA” or “endobronchial ultrasound” or “endobronchial ultrasonography” or “endobronchial ultrasound guided” or “endoscopic ultrasound” or “TBNA”] and [“thyroid” or “thyroid cancer” or “goiter” or “thyroid carcinoma”]). The reference lists of the extracted studies and the author's personal files were also reviewed. We excluded the following types of studies – (a) studies that did not report the simultaneous utilization of EBUS-TBNA in a thyroid condition (b) studies describing EBUS-TBNA for mediastinal evaluation in the setting of thyroid cancer (c) utilization of endoscopic ultrasound in thyroid condition (d) studies utilizing radial EBUS to assess the depth of airway invasion in thyroid cancer.
Duplicate citations were eliminated. The citations were then reviewed by their title and abstract and whenever felt appropriate; the full texts were extracted and reviewed. Data were abstracted on a data extraction form and the following information were retrieved from the selected studies – (a) author, (b) year, (c) number of patients, (d) age, (e) sex, (f) indication for EBUS-TBNA, (g) thyroid lesion size, (h) location of thyroid lesion – intrathoracic/extrathoracic, (i) presence of airway narrowing, (j) anesthesia, (k) needle gauge (l) number of passes, (m) rapid on-site evaluation, (n) aspirate adequacy, (o) final diagnosis, and (p) complications.
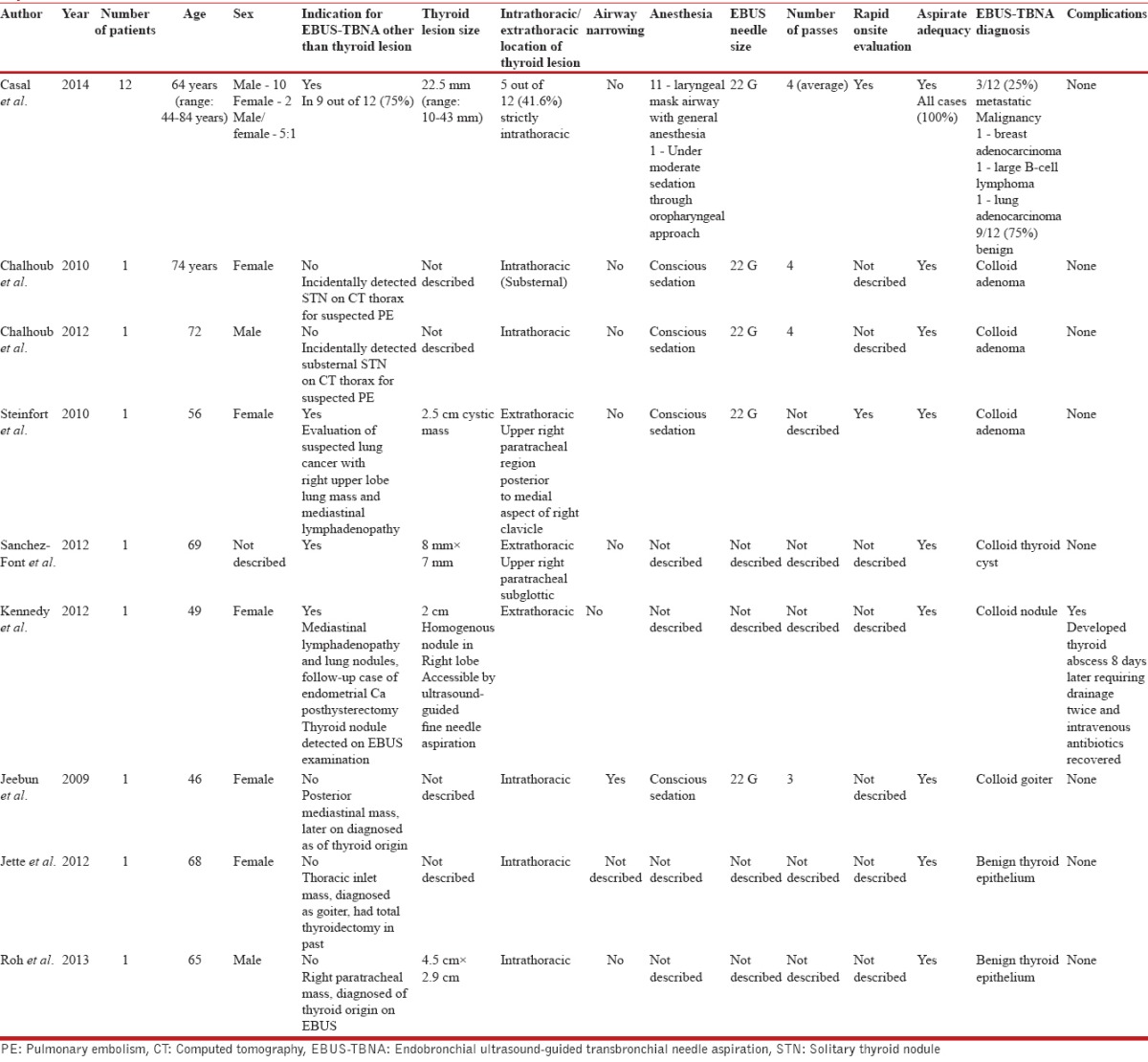
The systematic review methodology is summarized in Figure 4. The details of the finally selected studies for review are summarized in Table 1.
Figure 4.
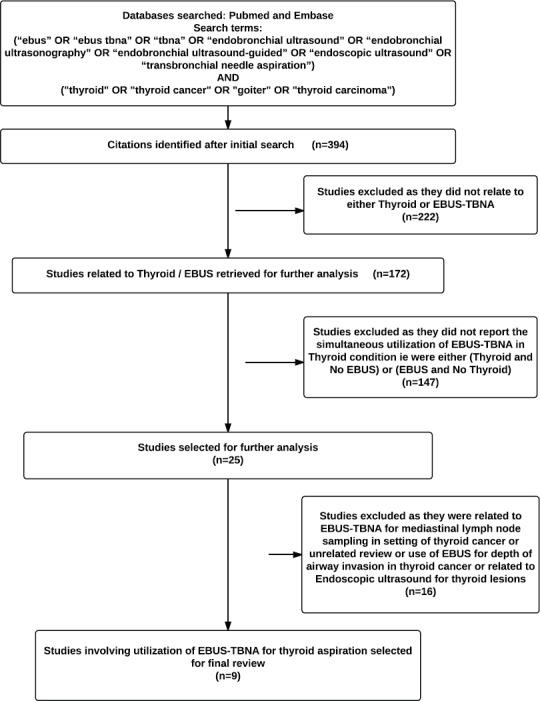
Methodology of systematic review of literature regarding endobronchial ultrasound-guided transbronchial needle aspiration of thyroid
Table 1.
Systematic review of the studies reporting the utilization of endobronchial ultrasound-guided transbronchial needle aspiration for thyroid aspiration
DISCUSSION
EBUS-TBNA is established as a standard of care investigative modality for the diagnostic evaluation of mediastinal lymphadenopathy and mediastinal masses located in proximity to the major airways. It is a safe procedure that is usually performed on an outpatient basis under conscious sedation. Most of the literature on EBUS-TBNA is focused on staging and diagnosis of lung cancer and diagnosis of undiagnosed mediastinal lymphadenopathy. With greater utilization and expertise, the role is being expanded for other indications such as diagnosis of metastatic extrathoracic malignancies, assessment of preoperative tracheobronchial invasion, assessment of airway remodeling in asthma, and diagnosis of nonlymph node intrapulmonary and mediastinal lesions.
Thyroid nodules are seen in 4–7% of the adult population and are four-fold more common in women as compared to males. Utilization of EBUS-TBNA in the evaluation of thyroid lesions has been described infrequently. On performing the systematic review, the initial search yielded 394 citations out of which, nine studies were identified that had reported the utilization of EBUS-TBNA for thyroid aspiration and finally met our inclusion criteria.[4,5,6,7,8,9,10,11,12] The findings of these nine studies are summarized in [Table 2]. EBUS-TBNA for thyroid aspiration was described in a total of twenty patients in these nine studies. Apart from one case series of 12 patients (Casal et al.), all the remaining eight studies were single patient case reports. Casal et al. described a case series of 12 patients wherein EBUS-TBNA was utilized for aspiration of thyroid lesions (five were strictly intrathoracic).[4] In nine out of 12 patients, the primary indication for EBUS was other than for primary aspiration of the thyroid. In remaining three patients, biopsy of intrathoracic thyroid lesion was the primary indication. Eleven out of the 12 lesions (92%) were located in the left thyroid lobe. The procedural difficulty was encountered in one patient wherein difficulty in puncturing the tracheal wall occurred due to the acute angle required to reach the lesion. There were no procedural complications and adequate aspirates (three – malignant and nine – benign lesions) could be obtained in all patients. All the three malignant diagnoses were metastatic nonthyroid cancer (breast adenocarcinoma – one patient, B-cell lymphoma – one patient, and lung adenocarcinoma – one patient).
Overall, in eight of the twenty patients (40%), aspiration of the thyroid lesion was the primary indication of EBUS-TBNA. In ten of the twenty patients (50%), the thyroid lesion was intrathoracic in location. Both our patients had intrathoracic location of the thyroid lesion. Airway narrowing was present in one (5%) out of the twenty patients.[8] Near exclusive use of general anesthesia (11 of 12 patients) using laryngeal mask airway for EBUS-TBNA procedure was reported by Casal et al. whereas other studies reported the use of conscious sedation. All the studies utilized the 22 G needle. We utilized the 21 G needle in both of our patients and procedure could be successfully performed under conscious sedation. Adequate/diagnostic aspirates were obtained in all the twenty patients. One procedural complication was reported. Kennedy et al. reported a 49-year-old female who underwent EBUS-TBNA for evaluation of mediastinal lymphadenopathy. The patient was a follow-up case of endometrial carcinoma, posthysterectomy and was diagnosed with mediastinal lymphadenopathy and lung nodules on follow-up. During EBUS examination, a thyroid nodule was detected (2 cm size and accessible by US-FNA). EBUS-TBNA was performed and a diagnosis of Colloid nodule was established. However, patient developed thyroid abscess (culture grew Streptococcus mitis) 8 days later which required drainage twice and intravenous antibiotics. The patient recovered with treatment.
We have described the feasibility and safety of EBUS-TBNA from thyroid lesions in two patients and systematically reviewed the literature pertaining to thyroid EBUS-TBNA. There are certain issues which need particular discussion. US-FNA is currently the procedure of choice for evaluation of thyroid lesions, but utility for intrathoracic/substernal lesions is limited. In such circumstances, surgical procedures such as mediastinoscopy/open surgery are usually required for diagnosis. EBUS-TBNA appears a promising modality for especially thyroid lesions in an intrathoracic location wherein performance of US-FNA may be extremely risky. The procedure is minimally invasive and associated with cost benefits as compared with surgical procedures. The occurrence of thyroid abscess in one patient following thyroid EBUS indicates that there is a possible risk of introduction of infection during the passage of EBUS scope through the unsterile oral cavity. This risk is greater for cystic lesions as has been reported in setting of endoscopic ultrasound (EUS) and an antibiotic prophylaxis may be rational in such circumstances.[13] Carefully performed EBUS-TBNA is feasible in patients with airway narrowing. However, it advisable that in these circumstances, facility of rigid bronchoscopy should be standby in case any airway complications ensue.[14] EBUS scope can also be introduced transesophageally for FNA of mediastinal lesions located in close esophageal proximity, a technique described as EUS-B-FNA (transesophageal bronchoscopic US-FNA). This modality has been shown to be safe and efficacious in the diagnosis of mediastinal lymphadenopathy. It is a feasible alternative to EBUS-TBNA in patients who have issues with transtracheal use of EBUS scope due to a number of possible limiting factors such as excessive cough, airway compromise, and nonaccessibility of the lesion.[15,16] Adoption of either EUS-B-FNA/EBUS-TBNA approach for lesions equally accessible by either approach is at the discretion of the operator and the operator experience. In the first patient, EUS-B-FNA was also feasible but as the procedure was performed by an experienced operator, sampling was performed transtracheally at the time of initial airway examination without any complications. In view of the excellent safety and performance characteristics of US-FNA in accessible thyroid lesions and possible risk of infectious complications with EBUS-TBNA, we would recommend reserving EBUS-TBNA only for those patients whose thyroid lesions which are intrathoracic and therefore inaccessible by US-FNA.
Percutaneous sonographic features suggesting malignancy in thyroid lesions include solid, hypoechoic nodules with ill-defined margins and microcalcifications. EBUS may also be helpful in revealing the sonographic characteristics of thyroid nodules thus assessing the possible risk for malignancy and can be investigated in future studies. Our patients had no procedural complications. We propose EBUS-TBNA as a useful modality for evaluation of thyroid lesions particularly those with a strict intrathoracic location wherein US-FNA is risky not feasible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Madan K, Mohan A, Ayub II, Jain D, Hadda V, Khilnani GC, et al. Initial experience with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) from a tuberculosis endemic population. J Bronchology Interv Pulmonol. 2014;21:208–14. doi: 10.1097/LBR.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 2.Singer PA, Cooper DS, Daniels GH, Ladenson PW, Greenspan FS, Levy EG, et al. Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Arch Intern Med. 1996;156:2165–72. [PubMed] [Google Scholar]
- 3.Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med. 2004;351:1764–71. doi: 10.1056/NEJMcp031436. [DOI] [PubMed] [Google Scholar]
- 4.Casal RF, Phan MN, Keshava K, Garcia JM, Grosu H, Lazarus DR, et al. The use of endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of thyroid lesions. BMC Endocr Disord. 2014;14:88. doi: 10.1186/1472-6823-14-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalhoub M, Harris K. The use of endobronchial ultrasonography with transbronchial needle aspiration to sample a solitary substernal thyroid nodule. Chest. 2010;137:1435–6. doi: 10.1378/chest.09-2840. [DOI] [PubMed] [Google Scholar]
- 6.Sánchez-Font A, Peralta S, Curull V. Thyroid cyst diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration in a patient with lung cancer. Arch Bronconeumol. 2013;49:38–9. doi: 10.1016/j.arbres.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Chalhoub M, Harris K. Endobronchial ultrasonography with transbronchial needle aspiration to sample a solitary substernal thyroid nodule: A new approach. Heart Lung Circ. 2012;21:761–2. doi: 10.1016/j.hlc.2012.04.022. [DOI] [PubMed] [Google Scholar]
- 8.Jeebun V, Natu S, Harrison R. Diagnosis of a posterior mediastinal goitre via endobronchial ultrasound-guided transbronchial needle aspiration. Eur Respir J. 2009;34:773–5. doi: 10.1183/09031936.00046309. [DOI] [PubMed] [Google Scholar]
- 9.Jette L, Parrish S, Cordero S. Ectopic intrathoracic thyroid, presenting two years after total thyroidectomy. Chest. 2012 142(4_MeetingAbstracts):977A. doi:10.1378/chest.1387935. [Google Scholar]
- 10.Kennedy MP, Breen M, O’Regan K, McCarthy J, Horgan M, Henry MT. Endobronchial ultrasound-guided transbronchial needle aspiration of thyroid nodules: Pushing the boundary too far? Chest. 2012;142:1690–1. doi: 10.1378/chest.12-1871. [DOI] [PubMed] [Google Scholar]
- 11.Roh E, Hong ES, Ahn HY, Park SY, Yoon HI, Park KS, et al. A case of mediastinal ectopic thyroid presenting with a paratracheal mass. Korean J Intern Med. 2013;28:361–4. doi: 10.3904/kjim.2013.28.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinfort DP, Irving LB. Endobronchial ultrasound staging of thyroid lesion in small cell lung carcinoma. Thorac Cardiovasc Surg. 2010;58:128–9. doi: 10.1055/s-0029-1185821. [DOI] [PubMed] [Google Scholar]
- 13.Dumonceau JM, Polkowski M, Larghi A, Vilmann P, Giovannini M, Frossard JL, et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2011;43:897–912. doi: 10.1055/s-0030-1256754. [DOI] [PubMed] [Google Scholar]
- 14.Madan K, Agarwal R, Bal A, Gupta D. Bronchoscopic management of a rare benign endobronchial tumor. Rev Port Pneumol. 2012;18:251–4. doi: 10.1016/j.rppneu.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Madan K, Garg P, Kabra SK, Mohan A, Guleria R. Transesophageal bronchoscopic ultrasound-guided fine-needle aspiration (EUS-B-FNA) in a 3-year-old child. J Bronchology Interv Pulmonol. 2015;22:347–50. doi: 10.1097/LBR.0000000000000169. [DOI] [PubMed] [Google Scholar]
- 16.Dhooria S, Aggarwal AN, Singh N, Gupta D, Behera D, Gupta N, et al. Endoscopic ultrasound-guided fine-needle aspiration with an echobronchoscope in undiagnosed mediastinal lymphadenopathy:First experience from India. Lung India. 2015;32:6–10. doi: 10.4103/0970-2113.148399. [DOI] [PMC free article] [PubMed] [Google Scholar]



