Abstract
Context:
Type 2 Diabetes Mellitus (T2DM) refers to a group of common metabolic disorders that share the phenotype of Hyperglycemia. More than 60% of the world's population with diabetes comes from Asia.
Aim:
To study the prevalence of Type 2 Diabetes Mellitus among Sikh individuals living in the urban localities of Amritsar.
Settings and Design:
The study was designed in the Faculty of Sports Medicine & Physiotherapy, Guru Nanak Dev University, Amritsar, Punjab, India. The data collection was carried out in various urban localities of Amritsar. Blood samples were analyzed in the Biochemistry laboratory, whereas data analysis and article preparation was carried out in the Faculty of Sports Medicine and Physiotherapy.
Materials and Methods:
Multi-stage random sampling was done with a sample size of 1089 patients.
Statistical Analysis:
The data was analyzed in Stata 11.2 software. Various tests used in the study are Mean ± SD, Pearson Chi Square Test, Students’ t test and multiple logistic regression test.
Results:
Our study showed that the prevalence rate of Type 2 Diabetes Mellitus is 23.2% with the confidence interval of 20.7–25.7. Proportionately more patients with T2DM had hypertension (46.6%). Likewise proportionately more patients, 67.5% had hypertrigylerdemia, 67.6% had low HDL levels, 59.2 % had hypercholesterolemia and 73.1% suffered from metabolic syndrome.
Conclusions:
Our study clearly indicates that the young Sikh adults below 40 years of age have similar high BMI, WC and WHR to that of the older adults above 40 years of age. It is necessary to adopt appropriate preventive strategies and interventions in high-risk individuals to curb the growing epidemic of diabetes. Innovative community outreach programs need to be designed and implemented to create awareness and early screening and treatment of diabetes, especially in the urban population.
Keywords: Diabetes mellitus, India, prevalence, urban population
Introduction
The International Diabetes Federation has predicted that the number of individuals with diabetes will increase from 240 million in 2007 to 380 million in 2025, with 80% of the disease burden in low and middle-income countries.[1] The Diabetes Epidemic is more pronounced than in India than anywhere else as the WHO reports show that 32 million people had Diabetes in the year 2000.[2] The Indian Council of Medical Research (ICMR) study carried out in 1970's reported a prevalence of 2.3% in urban areas[3,4] which rose to 12 15 % in 2000’s. A better understanding about the cause of the modifiable risk factors and habits predisposing this community toward developing Type 2 Diabetes Mellitus (T2DM) is necessary for future planning of healthcare, policy and delivery in order to ensure that the effects of the disease are addressed.[5] So far, no data is available in this particular section of the population regarding the prevalence of the T2DM. The objective of the study was to assess the prevalence of T2DM and its risk factors in the urban Sikh population of Amritsar.
Subjects and Methods
The sample size of 1089 patients was calculated. Anticipated prevalence was 20% and allowable precision was 4%. The multi-stage cluster randomized sampling was done using the probabilities proportional size (PPS) method. This study focused on urban Sikhs living in Amritsar, Punjab, India. The Sikhs constitute 70% of the total population of Amritsar according to 2011 census report. The area was arbitrarily divided into five equal zones namely (Z1, Z2, Z3, Z4, and Z5). Each zone constituted of 13 censes wards. The list provided the name, age and address of those eligible for voting (>18 years). The fieldwork was completed within a period of 20 months, starting in January 2012. A total of 215 patients from each zone were randomly selected. In the selection of the family in a particular ward, WHO method of sampling (Random method of multi-stage sample collection) was followed to prevent any non uniformity. A model consent form was designed to ensure compliance with ICMR guidelines regarding the use of humans in the research. All the protocols and consent documents were reviewed and approved by the Institutional Ethics Committee of Faculty of Sports Medicine and Physiotherapy, Guru Nanak Dev University, Amritsar. The complete detailed performa of all the family members was filled by the investigator, which included number of members in the family, age, educational status and so on. One male and one female member were randomly selected from the list provided by the respondent of the family. These two family members were requested to fill in the self-designed, professionally validated questionnaire. Blood pressure was recorded in sitting position after 5 min rest with a mercury sphygmomanometer according to the standard guidelines. The fasting blood sample (venous blood sample was analyzed for all the biochemical parameters.) was taken for the biochemical readings. The anthropometric readings were taken namely height, weight, waist and hip circumference.
Results
Table 1 shows the prevalence of T2DM in the urban Sikh population of Amritsar with respect to the BMI and waist to hip ratio (WHR).
Table 1.
Gender-wise distribution of the biochemical parameters in diabetics and non-diabetics (Mean ± SD)
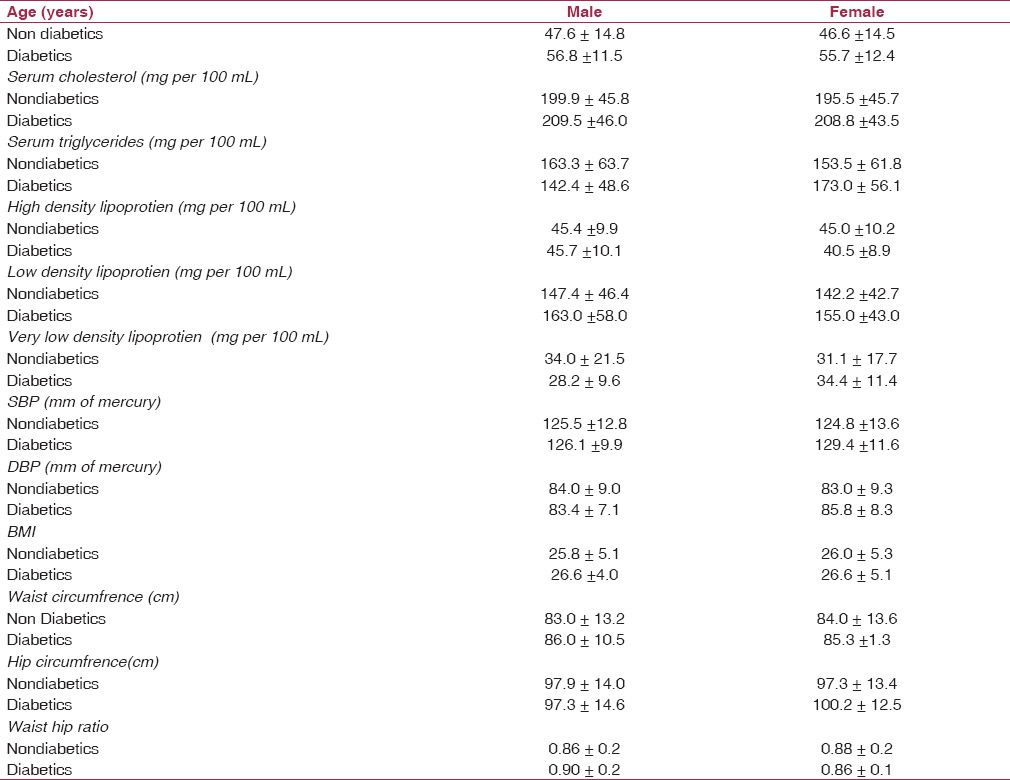
Demographic and clinical profile of patients with and without T2DM
Table 2 shows the gender-wise prevalence of T2DM across different age groups. The study also shows significantly higher rates of T2DM in the older age groups, which has been explained in Table 3. The T2DM rates increase from 4% in the age group of 20–29 years peaking to 32.5% in the age group of 60 + years.
Table 2.
Age specific and age standardized prevalence of Type 2 Diabetes Mellitus gender-wise in percentage with 95% confidence interval
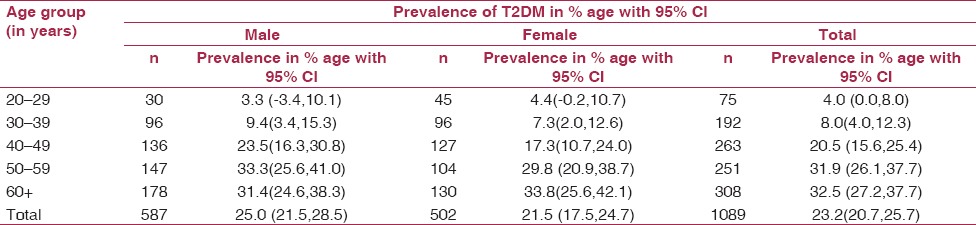
Table 3.
Risk factors for Type 2 Diabetes Mellitus
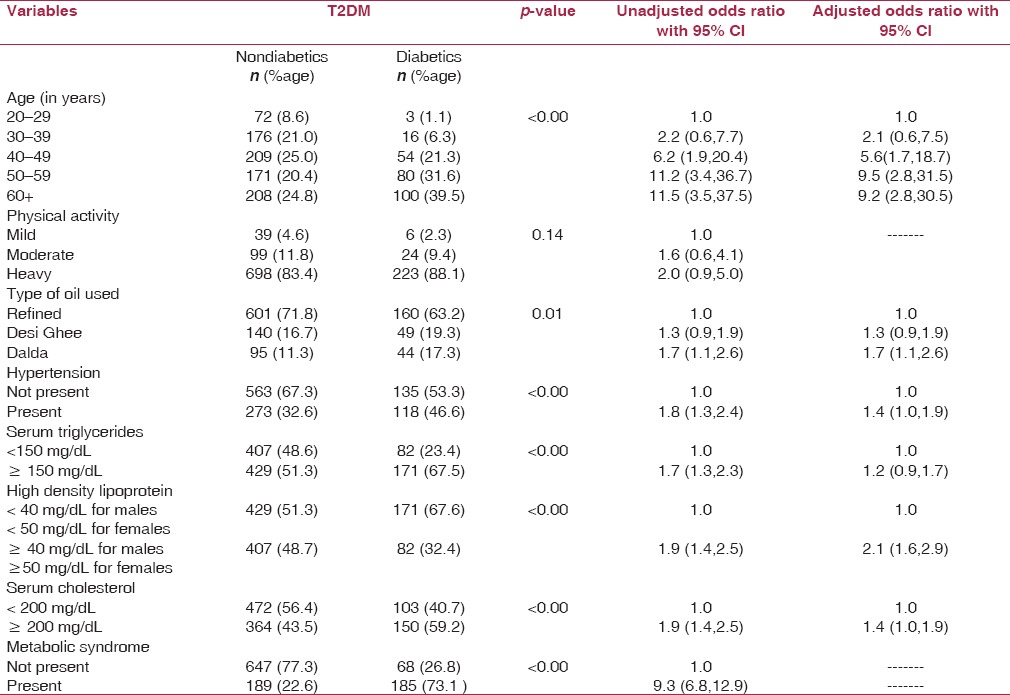
The Chi square outputs of significant proportions with several clinical, demographic and biochemical parameters available to the present study comparing the patients with and without T2DM are shown in Table 4. Proportionately more patients with T2DM had hypertension (46.6%). Likewise proportionately more patients, 67.5% had hypertrigylerdemia, 67.6% had low HDL levels, 59.2 % had hypercholesterolemia and 73.1% suffered from metabolic syndrome.
Table 4.
Body mass index: waist hip ratio distribution in the sample population
Detailed correlates of T2DM in univariate analysis and multivariate logistic regression method showing significant predictors of T2DM are summarized in Table 4. Advancing age, medium of cooking (oil used), hypertension, hypercholesterolemia, hypertrigylerdemia, and low serum HDL levels significantly contributed to the increased T2DM risk.
Those with low HDL levels have double the risk of developing T2DM as compared to the individuals who had healthy HDL levels. Similarly, increased serum cholesterol and serum triglycerides increased the risk of developing T2DM one and half times more.
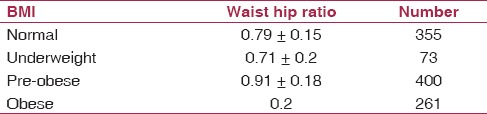
Very few individuals in this study were in the category of healthy BMI. Only 32.6 % (n = 355) of the individuals presented with a healthy BMI as per the WHO guidelines. 6.7% (n = 73) were reported underweight, whereas 36.7% (n = 400) were reported as pre-obese and 24% (n = 261) presented as obese. The patient population presented a picture of general obesity as central obesity was not significantly present in this population. General obesity is related to the abnormal lipid profile values that is increased serum cholesterol, serum triglyride, LDL and decreased HDL values.
Discussion
The overall prevalence of T2DM in urban Sikh population of Amritsar was 23.2% with a slightly higher prevalence along men (25%) compared with women (21.5%).The previous studies reported the prevalence rates ranged from 8.9% to 12.6 % in the various communities and setups.[6,7,8] The present study also revealed that the prevalence of T2DM increases with age. In the target population of 20 years and above, the prevalence of T2DM increased with age from 4% in 20–29 years old age group through 8% in those aged 30–39 years, 20.5% in age group 40–49 years, 31.9% in 50–59 year-old age group and 32.5% in those aged more than or 60 years. Various studies observed a similar trend in rural populations.[6,9] This is also quite consistent with the studies carried out outside the Indian subcontinent like in the United States,[10] Denmark[11] and Hong Kong.[12] Hence, age is considered to be the most consistent risk factor around the world for rise in T2DM prevalence.
Variation in prevalence rates (3–11.2%) of diabetes mellitus have been reported from the urban areas of India.[13,14] In the urban population of Delhi, the prevalence of diabetes mellitus ranged from 1.6 to 9%, being more common in obese individuals.[15] In rural Indian population, it is reported to be in the range of 1–5%.[14,16,17] Similarly in a rural community in the Punjab, only 4.6% were diabetic.[18] On bivariate analysis, the prevalence of T2DM was found to be significantly associated with age, hypertension, high-serum Cholesterol, low HDL high TG levels, and medium of cooking that is the oil used. Multiple logistic regression analysis identified age, hypertension, serum cholesterol, serum triglycerides as independently associated factors for diabetes. These findings were similar to those reported by Ramachnadran, et al.[8] We also found serum HDL and medium of cooking food (oil used) as independently associated factors for diabetes.
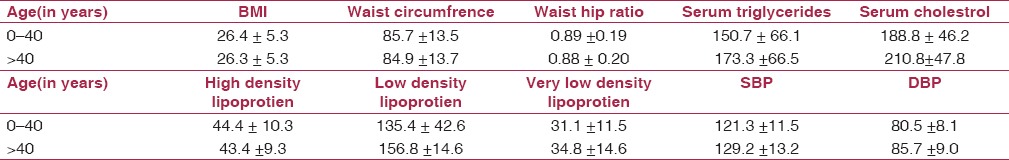
Disturbance of lipid metabolism appears to be an early event in the development of T2DM, potentially preceding the disease by several years.[19] In addition, the different components of diabetic dyslipidemia are believed to be metabolically linked[20,21]. Dyslipidemia associated with insulin resistance is characterized by moderately increased triglyceride levels carried in very-low-density lipoprotein particles, reduced high-density lipoprotein cholesterol levels carried in small HDL particles, and LDL-C levels that do not differ substantially from those of individuals without T2DM.[20,21,22] [Figure 1] Prabhakran, et al.[23] reported the association between T2DM and hypertension, hypercholesterolemia and hypertriglyridemia. Vikram, et al.[24] in their study in North India observed a strikingly high prevalence of abdominal obesity and generalized obesity in T2DM. Although Mohan, et al.[25] reported an association between physical activity and T2DM, we did not find an such association in the subject population in the current study. Our study clearly indicates that the young Sikh adults below40 years of age have similar high BMI, WC and WHR to that of the older adults above 40 years of age [Table 5]. It is necessary to adopt appropriate preventive strategies and interventions in high-risk individuals to curb the growing epidemic of diabetes.
Figure 1.
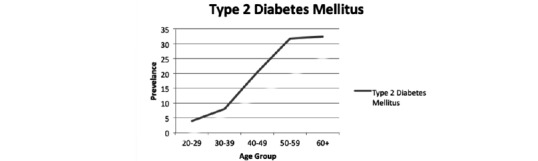
Age-wise trend of Type 2 Diabetes Mellitus
Table 5.
Mean and SD values of the anthropometric physiological and biochemical parameters accordingly to age group
Pertaining to this rising trend of the T2DM in the urban Sikh population of Amritsar, the individuals are getting diabetic in the most productive years of their life. To curb this rise, regular screening of the people should be done to rule out any risk factors associated with T2DM. Educational awareness camps should be organized to make them aware of the disease and its risk factors.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
References
- 1.International Diabetes Federation: Diabetes Atlas 3rd Edition, Brussels, Belgium: International Diabetes Federation: 2006 [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Daibetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Ahuja M. M. S. Prevalence of diabetes in northern India (Delhi area) Hormone and Metabolic Research. 1972;4:321–24. doi: 10.1055/s-0028-1094024. [DOI] [PubMed] [Google Scholar]
- 4.Gupta OP, Joshi MH, Dave DK. Prevalence of diabetes in India. Adv Metab Disorder. 1978;9:147–65. doi: 10.1016/b978-0-12-027309-6.50013-6. [DOI] [PubMed] [Google Scholar]
- 5.Hoskote SS, Joshi SR. Are Indians destined to be diabetic? J Assoc Phys India. 2008;56:225–6. [PubMed] [Google Scholar]
- 6.Deo SS, Zantye A, Mokal R, Mithbawkar S, Rane S, Thakur K. To identify the risk factors for high prevalence of diabetes and impaired glucose tolerance in Indian rural population. Int J Diab Dev Countries. 2006;26:19–23. [Google Scholar]
- 7.Yajnik CS. Early life origins of insulin resistance and type 2 diabetes in India and other Asian countries. J Nutr. 2004;134:205–10. doi: 10.1093/jn/134.1.205. [DOI] [PubMed] [Google Scholar]
- 8.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK. Diabetes Epidemiology Study Group in India (DESI). High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 9.Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK. Prevalence of diabetes and impaired fasting glucose in Korea. Diabetes Care. 2006;29:226–31. doi: 10.2337/diacare.29.02.06.dc05-0481. [DOI] [PubMed] [Google Scholar]
- 10.Harris MI, Hadden WC, Knowler WC, Bennet PH. Prevalence of diabetes and impaired glucose tolerance and plasma glucose levels in the US population. Diabetes. 1987;36:523–34. doi: 10.2337/diab.36.4.523. [DOI] [PubMed] [Google Scholar]
- 11.Anger E, Thorsteinson Erikson M. Impaired glucose tolerance and diabetes mellitus in elderly subjects. Diabetes Care. 1989;5:600–4. doi: 10.2337/diacare.5.6.600. [DOI] [PubMed] [Google Scholar]
- 12.Woo J, Swaminathan R, Cockram C, Pang CP, Mak YT, Au SY. The prevalence of Diabetes mellitus and assessment of methods of detection among the community of elderly Chinese in Hong Kong. Diabetologia. 1987;30:863–68. doi: 10.1007/BF00274795. [DOI] [PubMed] [Google Scholar]
- 13.Ramachandran A, Snehalatha C, Latha E, Vijay V, Viswanathan M. Rising prevalence of NIDDM in an urban population in India. Diabetologia. 1997;40:232–7. doi: 10.1007/s001250050668. [DOI] [PubMed] [Google Scholar]
- 14.Gupta OP, Joshi MH, Dave SK. Prevalence of diabetes in India. Adv Metab Disord. 1978;9:147–65. doi: 10.1016/b978-0-12-027309-6.50013-6. [DOI] [PubMed] [Google Scholar]
- 15.Gopinath N, Chadha SL, Jain P, Shekhawat S, Tandon R. An epidemiological study of obesity in adults in the urban population of Delhi. J Assoc Phys Ind. 1994;42:212–215. [PubMed] [Google Scholar]
- 16.Tripathy BB, Panda NC, Tej SC, Sahoo GN, Kar BN. Survey for the detection of glycocusira, hyperglycemia, and diabetes mellitus in urban and rural areas of Cuttak district. J Assoc Phys Ind. 1971;19:681–92. [PubMed] [Google Scholar]
- 17.Patandin S, Bots ML, Abel R, Valkenburg HA. Impaired glucose intolerance and diabetes mellitus in a rural population in South India. Diabetes Res ClinPract. 1994;24:47–5. doi: 10.1016/0168-8227(94)90085-x. [DOI] [PubMed] [Google Scholar]
- 18.Wander GS, Khurana SB, Gulati R, Sachar RK, Gupta RK, Khurana S, Anand IS. Epidemiology of coronary heart disease in a rural Punjab population-prevalence and correlation with various risk factors. Indian Heart J. 1994;46:319–323. [PubMed] [Google Scholar]
- 19.Adiels M, Olofsson SO, Taskinen MR, Boren J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28:1225–36. doi: 10.1161/ATVBAHA.107.160192. [DOI] [PubMed] [Google Scholar]
- 20.Adiels M, Olofsson SO, Taskinen MR, Boren J. Diabetic dyslipidaemia. Curr Opin Lipidol. 2006;17:238–46. doi: 10.1097/01.mol.0000226115.97436.c0. [DOI] [PubMed] [Google Scholar]
- 21.Taskinen MR. Type 2 diabetes as a lipid disorder. CurrMol Med. 2005;5:297–308. doi: 10.2174/1566524053766086. [DOI] [PubMed] [Google Scholar]
- 22.Krentz AJ. Lipoprotein abnormalities and their consequences for patients with type 2 diabetes. Diabetes Obes Metab. 2003;5(Suppl 1):S19–S27. doi: 10.1046/j.1462-8902.2003.0310.x. [DOI] [PubMed] [Google Scholar]
- 23.Prabhakaran D, Chaturvedi V, Ramakrishnan L, Jeemon P, Shah P, Snehi U. Risk factors related to the development of diabetes in men working in a north Indian industry. Natl Med J India. 2007;20:4–10. [PubMed] [Google Scholar]
- 24.Vikram NK, Misra A, Pandey RM, Dudeja V, Sinha S, Ramadevi J. Anthropometry and body composition in northern Asian Indian patients with type 2 diabetes: receiver operating characteristics (ROC) curve analysis of body mass index with percentage body fat as standard. Diabetes Nutr Metab. 2003;16:32–40. [PubMed] [Google Scholar]
- 25.Mohan V, Shanthirani CS, Deepa R. Glucose intolerance (diabetes and IGT) in a selected South Indian population with special reference to family history, obesity and lifestyle factors–the Chennai Urban Population Study (CUPS 14) J Assoc Physicians India. 2003;51:771–7. [PubMed] [Google Scholar]


