Abstract
Background:
Globally, smokeless tobacco use is disproportionately concentrated in low-income and middle-income countries like India and Bangladesh.
Objectives:
The current study examined comparative patterns of use and perceptions of harm for different smokeless tobacco products among adults and youth in Navi Mumbai, India, and Dhaka, Bangladesh.
Methods:
Face-to-face interviews were conducted on tablets with adult (19 years and older) smokeless tobacco users and youth (16–18 years) users and non-users in Navi Mumbai (n = 1002), and Dhaka (n = 1081).
Results:
A majority (88.9%) of smokeless tobacco users reported daily use. Approximately one-fifth (20.4%) of the sample were mixed-users (used both smoked and smokeless tobacco), of which about half (54.4%) reported that they primarily used smokeless over smoked forms like cigarettes or bidis. The proportion of users planning to quit was higher in India than in Bangladesh (75.7% vs. 49.8%, p < 0.001). Gutkha was the most commonly used smokeless product in India, and pan masala in Bangladesh. Among users in Bangladesh, the most commonly reported reason for using their usual product was the belief that it was “less harmful” than other types. Perceptions of harm also differed with respect to a respondent's usual product. Bangladeshi respondents reported more negative attitudes toward smokeless tobacco compared to Indian respondents.
Conclusions:
The findings highlight the high daily use of smokeless tobacco, and the high prevalence of false beliefs about its harms. This set of findings reinforces the need to implement effective tobacco control strategies in low and middle-income countries like India and Bangladesh.
Keywords: Smokeless tobacco, India, Bangladesh, health knowledge, attitudes and practice, perceptions of harm
Key messages
False beliefs about the harmfulness of smokeless tobacco products were common in both India and Bangladesh, with more than half of users reporting that they chose their usual product on the basis that it was “less harmful” than other types.
Perceptions of harm differed with respect to a respondent's usual product. For example, while gutkha was rated as the most harmful smokeless tobacco product in India overall, respondents who used gutkha as their “usual product” perceived zarda as more harmful instead.
This set of findings reinforces the need to implement effective tobacco control strategies that include smokeless tobacco products in low and middle-income countries like India and Bangladesh.
Introduction
India and Bangladesh have over 200 million smokeless tobacco users[1,2] —more than the rest of the world combined. Popular packaged forms of smokeless tobacco include pan masala, gutkha, khaini, zarda, dokta, gudhaku, and gul, all of which contain a mixture of ingredients like slaked lime and spices, in addition to tobacco. Another popular form of smokeless tobacco is paan, which is typically handmade using fresh, green betel leaf to wrap tobacco and other ingredients.
Indian and Bangladeshi smokeless tobacco products contain markedly higher levels of carcinogenic agents compared to smokeless products popular in the USA and Sweden.[3] This difference may be due to the addition of other ingredients used in the preparation of smokeless tobacco such as areca nut, which is itself carcinogenic.[4] Indeed, India has one of the highest incidences of oral cancer in the world.[5] Smokeless tobacco use in this context has also been linked with cardiovascular disease and addiction.[6,7,8,9] There is also a growing body of evidence supporting the link between smokeless tobacco use and negative reproductive health outcomes.[10,11,12] Despite evidence linking smokeless tobacco use with adverse health outcomes, knowledge of the health risks remains so low that it continues to be used for medicinal purposes in many communities.[13,14,15,16]
Prevalence estimates vary regionally, but overall, 33% of men and 18% of women use smokeless tobacco in India.[2] Among female users, over 85% use smokeless tobacco exclusively.[2] In Bangladesh, the prevalence of smokeless tobacco use among females actually exceeds that of males, at 28% and 26%, respectively.[1] The high prevalence of use reflects high levels of social acceptability within these countries.[13,16] The production and distribution of packaged forms of smokeless tobacco has recently been banned in all Indian states. However, it is unclear how well these bans are being enforced or whether they will prove effective in curbing consumption.[17,18]
Thus, communicating the health risks of tobacco use remains a priority for tobacco control, particularly in low and middle-income countries that are often characterized by limited access to health information, less exposure to mass media campaigns, and lower literacy levels.[19] In order for a tobacco control strategy to be effective, it must first be informed by the local context. To date, numerous studies have examined patterns and predictors of smokeless tobacco use in India, and relatively few by comparison in Bangladesh.[14,20,21,22,23,24,25,26] The current study is among the first to examine comparative patterns of use and perceptions of harm of different smokeless tobacco products among adults and youth in India and Bangladesh.
Materials and Methods
Face-to-face recruitment and interviews took place at 15 sites around Navi Mumbai, India (April 10 to August 6, 2012), and six sites around Dhaka, Bangladesh (May 9 to June 18, 2012). Sites were busy public areas, selected for geographic and demographic diversity. Interviewers recruited respondents using a standard intercept technique,[27] whereby a physical landmark was selected and every other person to pass it was approached in Navi Mumbai; in Dhaka, every third person to pass the landmark was approached in busy locations, which was increased to every person in locations with less pedestrian traffic. Interviews were conducted in the respondents’ preferred language in India (English, Hindi, or Marathi), and in Bengali in Bangladesh. Interviewers read aloud questions to respondents and entered their responses into the tablets. Interviewers from local partner organizations were trained by the same team members to increase consistency between sites, and supervised by local research staff who monitored randomly in the field, to ensure study protocols were followed.
The adult (19 years and older) sample consisted of only smokeless tobacco users, whereas the youth (16–18 years) sample included both smokeless tobacco users and non-users, given the potential for future tobacco initiation among youth. Prior to beginning the interview, all respondents were provided with information about the study and asked to provide verbal consent. No personal information identifiers were collected. The study was reviewed by the Office of Research Ethics (University of Waterloo), the Healis-Sekhsaria Institute for Public Health and the Bangladesh Medical Research Council and received ethical clearance. Respondents were asked a series of socio demographic and psychosocial measures adapted from national International Tobacco Control Policy Evaluation Study surveys.[28,29]
Measures
Demographics
Demographic variables included sex, age, education, and income. For adults, education level was categorized as:‘Low’ (“Illiterate”),‘Moderate’ (“Middle school or less” in India; “Secondary school or less” in Bangladesh), or ‘High’ (“Secondary school” to “Graduate with degree/diploma or more” in India;”SSC/HSC (9–12 years)” to “University degree” in Bangladesh).
For Indian youth, education was categorized as ‘Low’ (“Did not attend school”, and “Primary school” to “Middle School (up to class VII)”), ‘Moderate’ (“Secondary school”), or ‘High’ (“Class XI (Higher Secondary)” or “Graduate (degree, diploma) or more”)). For Bangladeshi youth, education was categorized as ‘Low’ (“Illiterate”, “Literate (no formal education)”, and “Primary (1–5 years)”), ‘Moderate’ (“Secondary school (6–8 years)”), or ‘High’ (“SSC”/”HSC” (9–12 years) or more).
Household income level was categorized as ‘Low’ (<10,000 Indian rupee or INR (India); < 5000 Bangladeshi taka (Bangladesh)), ‘Moderate’ (10,000 to <20,000 INR; 5000 to <10,000 taka), ‘High’ (20,000 INR or more; 10,000 taka or more), or ‘Not stated’. For reference, one US dollar is equivalent to approximately 60 INR, and about 80 taka.
Smokeless tobacco use
Daily smokeless tobacco use was defined as using smokeless tobacco “every day”. Non-daily smokeless tobacco use was defined as using smokeless tobacco “at least once a week”, or “at least once in the last month”. Among youth non-users, susceptibility to smokeless tobacco use was determined based on responses to three questions: 1) “Do you think in the future you might try using smokeless tobacco?”, 2) “If one of your best friends were to offer you smokeless tobacco, would you use it?”, and 3) “At any time during the next year, do you think you will use smokeless tobacco?”. Respondents who reported a firm commitment not to use smokeless tobacco (i.e. “definitely not” for all three measures) were categorized as non-susceptible, and all others were categorized as susceptible, as per previous research on smoking susceptibility.[30]
Quit intentions
Smokeless tobacco users were asked “Are you planning to quit… 1) Within the next month, 2) Within the next 6 months, 3) Sometime in the future, beyond 6 months, or 4) Not planning to quit”. Quit intentions were categorized as ’Planning to quit’ (first three response options) and ‘Not planning to quit’.
Usual smokeless tobacco product
Respondents were asked “Do you currently use any smokeless tobacco products at least once a month?” In India, response options included: mishri, paan, plain chewing tobacco, gutkha, khaini, zarda, tobacco toothpaste, nasal/oral snuff, lal dantmanjan, dokta, gudhaku, gul, or other. Response options in Bangladesh included: zarda, paan, gul, sadapata, pan masala, nasshi, or other. Respondents were asked the follow-up “Which of these products do you use most frequently?”, and their responses comprised a Usual product variable.
Reasons for use
Smokeless tobacco users were asked “In choosing this type of smokeless tobacco [referring to their Usual product], was part of your decision based on any of the following…1) The price, 2) This type is of high quality, or 3) This type is less harmful to my health”, with the following response options for each reason: “Yes”, “No”, “Refused”, and “Don’t know”.
Mixed-use (Smokeless and smoked tobacco)
Respondents were asked “In the past month, have you used any of the following smoked tobacco products?” In India, response options included: cigarettes (factory made and roll-your-own), bidis, hookah/shisha/narghile/water pipe, cigars/small cigars/cigarillos, pipe, chutta, hooklis, or other. Response options in Bangladesh included: cigarettes (factory made and roll-your-own), bidis, hookah/shisha/narghile, or other. Respondents who reported using both smoked and smokeless tobacco products were then asked which they used most often: “Smoked tobacco”, “Smokeless tobacco”, or “Smoked and smokeless tobacco about the same”? Smokeless tobacco users who also selected any smoked tobacco product were classified as mixed users.
Perceptions of harm about smokeless tobacco products
Respondents were asked to rank six popular smokeless tobacco products available in their country, from most harmful to least harmful (where 1 was ‘most harmful’ and 6 was ‘least harmful’). The six products were selected based on previous research and local consultation (Table 3).The order was reverse-coded, and mean ranks for each product were computed, whereby higher numbers corresponded with greater perceptions of harm.
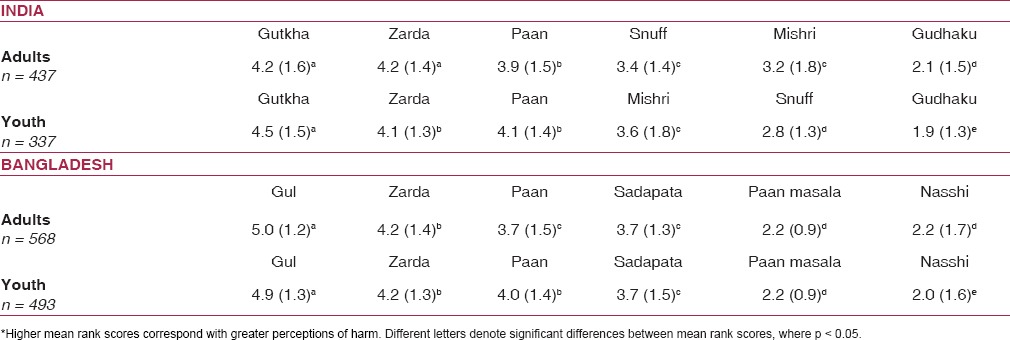
Table 3.
Mean rank score* (SD) for perceived harm rankings of six local smokeless tobacco products, by country and age group (n = 1,835)
Attitudes and beliefs about smokeless tobacco
Respondents were asked whether they “agree”, “disagree”, or “neither agree nor disagree” with each of the following statements. 1) “Indian [Bangladeshi] society disapproves of using smokeless tobacco”, 2) “Smokeless tobacco is highly addictive”, 3) “It is acceptable for women to use smokeless tobacco”, 4) “Using smokeless tobacco sets a bad example for children”, and 5) “Smokeless tobacco use is harmful to health”. Item 3 was reverse-coded so that positive and negative responses were consistent with the direction of the other attitudes and beliefs. An Attitudes and Beliefs Scale was created by summing the number of ‘agree’ responses across the five items, to yield a score of 0–5, where lower scores indicated more positive attitudes and beliefs towards smokeless tobacco.
Analysis
All analyses were conducted using SPSS version 22.0. Descriptive statistics including frequencies, chi-square tests (for categorical variables), one-way ANOVA and t tests (for continuous variables), were conducted to examine differences between the Indian and Bangladeshi samples. Multiple linear regression models were used to examine the associations between country and individual-level predictors on attitudes and beliefs about smokeless tobacco (using the Attitudes and Beliefs Scale as the outcome measure).
In the model examining only adult users, country, age, (p<0.001) sex, education, income, smokeless tobacco use (daily user, non-daily user), mixed-use, and quit intentions were entered as covariates. In the model examining youth (users and non-users), country, age, sex, education, and smokeless tobacco use (daily user, non-daily user, susceptible non-user, non-susceptible non-user) were entered as covariates.
Results
Sample characteristics
In India, interviews were conducted in English (n=33), Hindi (n=456), and Marathi (n=513). In Bangladesh, all interviews were conducted in Bengali (n=1081). Fifty respondents had missing information, and were not included in the analysis. Table 1 represents the characteristics of the adult and youth samples, by country.
Table 1.
Sample Characteristics for Adults and Youth in Navi Mumbai, India and Dhaka, Bangladesh (N = 2,083)
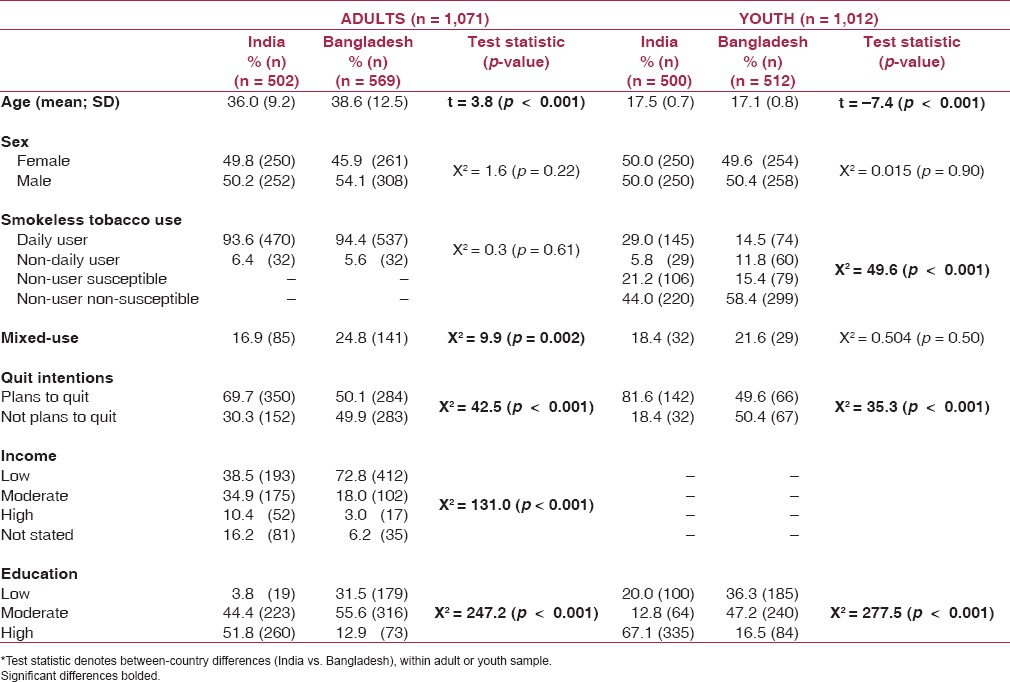
Differences between the Indian and Bangladeshi samples were found for age, quit intentions, and education, for both adults and youth (p < 0.001 for all comparisons). In addition, among adults, between-country differences were found in income level, (p < 0.001) and mixed-use was significantly higher in Bangladesh in the adult sample (p = 0.002). Among youth, between-country differences were found for smokeless tobacco use (p < 0.001.)
Usual product and reasons for use
Table 2 represents the usual products reported by adults and youth in Navi Mumbai and Dhaka. In India, more than half (51.7%) of youth, and one-quarter (26.3%) of adults reported gutkha as their usual product. Mishri, paan, and plain chewing tobacco were also among the most popular ‘usual products’ for adults, whereas youth reported mishri, plain chewing tobacco, and khaini as their second, third, and fourth most popular ‘usual products’. In Bangladesh, more than half of adult and youth users reported using paan masala as their ‘usual product’ (54.6% and 66.1%, respectively). Zarda, gul, and paan were also rated among the most popular ‘usual products’ for both adults and youth.
Table 2.
Percentage of smokeless tobacco users reporting their ‘usual product’, by country and age group (n = 1,339)
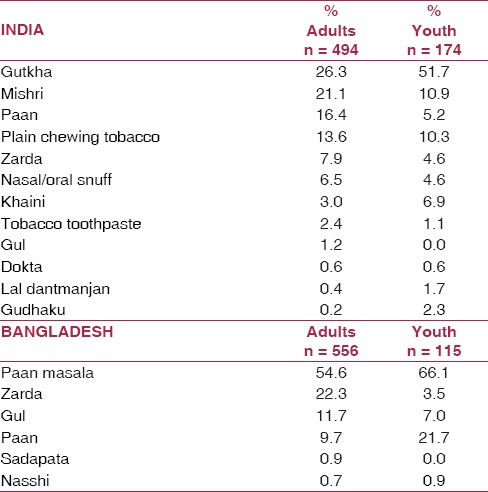
Figure 1 represents the percentages of smokeless tobacco users reporting various reasons for use of their usual product.
Figure 1.
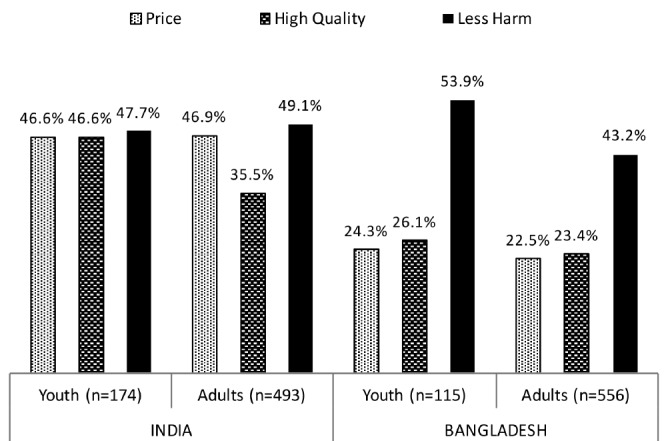
Percentage of smokeless tobacco users reporting reasons for using their ‘usual product’, by country and age group (n = 1,338)
Among Indian youth, no differences were found in the proportions of smokeless tobacco users reporting that they chose their usual product based on the ‘price’, the ‘qualilty’, and the belief that it was ‘less harmful’ than other types (46.6%, 46.6%, and 47.7%, respectively).
Among Indian adults, significantly lower proportions reported that they selected their usual product because it was of higher quality (35.5%) compared to those who reported they selected their usual product because of the price (46.9%, X2(df = 1) = 25.0, p < 0.001), or the belief that it was less harmful (49.1%, X2(df = 1) = 32.5, p < 0.001, respectively).
Bangladeshi youth reported ‘less harm’ (53.9%) as the primary reason for selecting their usual product, compared to beliefs about the products ‘high quality’ (26.1%) and ‘price’ (24.3%) X2(df = 1) = 28.4, p < 0.001;X2(df = 1) = 28.9, p < 0.001). Similarly, ‘less harm’, was the primary reason that Bangladeshi adults reported for selecting their usual product (43.2%), compared to beliefs about ‘high quality’ (23.4%), and ‘price’ (22.5%) X2(df = 1) = 73.8, p < 0.001; X2(df = 1) = 66.5, p < 0.001).
Perceptions of harm of popular local smokeless tobacco products
Table 3 represents the mean rank scores of perceived harm for six local smokeless tobacco products available in each country, from most to least harmful.
Among Indian youth (users and non-users), gutkha was ranked as most harmful compared to other products. Among adults, guktha and zarda were rated the most harmful. Bangladeshi adults and youth both ranked gul as most harmful. Overall, adults and youth ranked perceived harm similarly, with few exceptions.
Differences were found in perceptions of harm based on the type of product used by the respondent. In India, among usual users of gutkha (the most commonly used product), both adults and youth perceived zarda as most harmful harmful [mean rank = 4.4 (SD = 1.2) for adults; mean rank = 4.3 (SD = 1.2) for youth]. In Bangladesh, among usual users of pan masala (the most commonly used product), adults perceived gul to be most harmful [mean rank = 4.9 (SD = 1.3), whereas youth perceived sadapata to be most harmful [mean rank = 4.6 (SD = 1.3)].
Attitudes and beliefs towards smokeless tobacco: adults
Multiple linear regression models were conducted, with the Attitudes and Beliefs Scale as the dependent variable. Among adults, country X2(df = 1) = 42.4, p < 0.001), income X2(df = 3) = 43.8, p < 0.001), and quit intentions X2(df = 1) = 23.0, p < 0.001) were significantly associated with the Attitudes and Beliefs scale. Respondents from Bangladesh (β = 0.69; vs. India), those who were planning to quit (β = 0.43; vs. not planning to quit), and those with low(β = 0.92), moderate (β = 0.96) or [high-income (β = 1.10) levels vs. not stating income] reported more negative attitudes and beliefs about smokeless tobacco (p<0.001 for all contrasts).
Attitudes and beliefs towards smokeless tobacco: youth
In a model conducted among youth smokeless tobacco users and non-users, age X2(df = 1) = 5.8, p = 0.02), sex X2(df = 1) = 4.1, p = 0.04), country X2(df = 1) = 16.2, p < 0.001), education X2(df = 2) = 19.6, p < 0.001), and smokeless tobacco use (X2(df = 3) = 100.7, p < 0.001) were associated with the Attitudes and Beliefs scale. Older youth (β = 0.13, p = 0.02), men (β = 0.17, p = 0.04), and respondents in Bangladesh (β = 0.39; p < 0.001) reported more negative attitudes and beliefs. Respondents with low levels of education reported more positive attitudes and beliefs than those with moderate (β = 0.34, p = 0.002) or high (β = 0.49, p < 0.001) levels of education. Daily smokeless tobacco users also reported more positive attitudes and beliefs than did non-daily users (β = 0.75, p < 0.001), susceptible non-users (β = 1.18, p < 0.001) and non-susceptible non-users (β = 1.02, p < 0.001). Lastly, non-daily smokeless tobacco users reported more positive attitudes and beliefs than susceptible non-users (β = 0.44, p < 0.001).
Discussion
Overall, the patterns of use observed in the present study are similar to findings from the Global Adult Tobacco Survey (GATS), a nationally representative household survey of adult smokeless tobacco users (15 years and older) in India and Bangladesh.[1,2] It is important to note that the adult sample in the current study was made up of entirely smokeless tobacco users, so prevalence of smokeless tobacco use cannot be estimated. However, it is possible to compare prevalence of use in the study's youth sample against national estimates, as it is made up of both smokeless tobacco users and non-users between the ages of 16 and 18 years. According to GATS data from India (which defines “adult” as those 15 years of age and above), the overall prevalence of smokeless tobacco use was 8.2% among women aged 15–24 years and 23.1% among men. The sample in the current study followed a similar pattern, with 13.0% of women and 21.8% of men aged 16–18 years reporting smokeless tobacco use. In Bangladesh, GATS data estimates the overall prevalence of smokeless tobacco use at 4.0% among women aged 15–24 years, and 9.3% among men. Smokeless tobacco in the current study sample was 6.2% of women and 19.9% of men aged 16–18 years. Although the general patterns are consistent with nationally representative data, estimates from the current study were higher, which could be due to a variety of factors, the most likely of which was the sampling method.
Among youth, daily smokeless tobacco users reported more positive attitudes and beliefs than non-daily users, and susceptible and non-susceptible non-users. In addition, false beliefs about the harmfulness of smokeless tobacco products were common in both India and Bangladesh, with more than half of users reporting that they chose their usual product on the basis that it was “less harmful” than other types. Perceptions of harm also differed with respect to a respondent's usual product. For example, while gutkha was rated as the most harmful smokeless tobacco product in India overall, respondents who used gutkha as their “usual product” perceived zarda to be most harmful instead.
This set of findings may be explained through Cognitive Dissonance theory.[31] In the context of tobacco use, this theory suggests that those with a greater dependence on tobacco may attempt to rationalize their behaviour to help overcome the dissonance they experience when faced with information that runs counter to their lifestyle choice. Further, these findings might also indicate an optimistic bias among smokeless tobacco users, particularly those with a “usual product”, in which they perceive their own product as “less harmful” than other products.[32,33] Thus, there is a need to communicate the health effects of smokeless tobacco use within these populations to try to address the false beliefs found in this and other studies.[13,14,16,34]
Aside from the burden of smokeless tobacco, Navi Mumbai in India and Dhaka in Bangladesh are substantially different with respect to culture and tobacco control policy environments. Thus, it was not surprising that country differences were observed. For example, with respect to youth, Indian respondents were more likely to be daily smokeless tobacco users, and non-users were more likely to be susceptible to smokeless tobacco use, compared to their Bangladeshi counterparts. These findings may highlight the influential role of the marketing environment in India, the ease of access, and permissive cultural and social norms with regards to the social acceptability of smokeless tobacco.[35]
Despite the tendency for Indian respondents to be either daily users, or susceptible non-users, the findings also demonstrate greater intentions to quit compared to their Bangladeshi counterparts. The longer history of tobacco control in India may help explain this difference. In 2006, India became the first country in the world to implement pictorial health warnings on smokeless tobacco packages. Further, in 2009 the first mass media campaign highlighting the harmful effects of smokeless tobacco from real-life users was aired on radio and television in India.[36] In recent years, Bangladesh has made progress with respect to some tobacco control policies; however, these policy changes may not have had enough time to penetrate the public's understanding of smokeless tobacco issues the same way it has in India. Overall, this set of findings reinforces the urgent need to implement effective tobacco control strategies that include smokeless tobacco products in low and middle-income countries like India and Bangladesh.
Limitations
The current sample was not a probabiltity-based or nationally representative sample, although study sites were selected to capture demographic diversity within the sampling areas. Therefore, caution is advised when generalizing the results from the present study to other regions. In particular, it is important to note the regional diversity of India. According to GATS data, the prevalence of current smokeless tobacco use varies markedly by state, ranging from 5% in Goato 49% in Bihar.[2,15] The current study was conducted in the state of Maharashtra, where the prevalence of smokeless tobacco use was around 28%.[2] The present study also has limitations common to survey research, including social desirability in self-reports. For example, Bangladeshi respondents agreed with more statements about negative attitudes and beliefs, a pattern that persisted across different levels of income, mixed-use, age, and quit intentions, possibly highlighting an increased level of social desirability in responding when compared to their Indian counterparts.
Financial support and sponsorship
This work has been funded by the International Development Research Centre (IDRC) “The Impact of Health Warning Labels on Smokeless Tobacco Products in India and Bangladesh” (grant number 105136-008), with additional funding provided by the National Institutes of Health (grant number 1 P01 CA138-389-01: “Effectiveness of Tobacco Control Policies in High vs Low Income Countries”). Additional support was provided by the Propel Centre for Population Health Impact, a Canadian Institutes for Health Research New Investigator Award (Hammond) and a Canadian Cancer Society Research Institute Junior Investigator Research Award (Hammond).
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Acknowledgements
We wish to extend our gratitude to the field staff and interviewers at the Healis-Sekhsaria Institute for Public Health and the University of Dhaka, for their assistance in conducting this work.
References
- 1.World Health Organization. Global Adult Tobacco Survey: Bangladesh Report 2009 Dhaka, Bangladesh Country Office for Bangladesh 2009 [Google Scholar]
- 2.International Institute for Population Sciences, Ministry of Health and Family Welfare, Government of India. Global Adult Tobacco Survey India (GATS India), 2009-10 2010 New Delhi Ministry of Health and Family Welfare; Mumbai: International Institute for Population Sciences [Google Scholar]
- 3.Stepanov I, Hecht SS, Ramakrishnan S, Gupta PC. Tobacco? specific nitrosamines in smokeless tobacco products marketed in India. Int J Cancer. 2005;116:16–9. doi: 10.1002/ijc.20966. [DOI] [PubMed] [Google Scholar]
- 4.Nair U, Bartsch H, Nair J. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: A review of agents and causative mechanisms. Mutagenesis. 2004;19:251–62. doi: 10.1093/mutage/geh036. [DOI] [PubMed] [Google Scholar]
- 5.Khan ZU. An overview of oral cancer in Indian subcontinent and recommendations to decrease its incidence. Webmed Central Cancer. 2012;3 WMC003626- doi: 10.9754/journal.wmc.2012.003626. [Google Scholar]
- 6.Gupta P, Pednekar M, Parkin D, Sankaranarayanan R. A cohort study of 99,570 individuals in Mumbai, India for tobacco associated mortality. Int J Epidemiol. 2005;34:1395–402. doi: 10.1093/ije/dyi196. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R, Gupta N, Khedar R. Smokeless tobacco and cardiovascular disease in low and middle income countries. Indian Heart J. 2013;65:369–77. doi: 10.1016/j.ihj.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.IARC monographs on the evaluation of carcinogenic risks to humans: volume 85: betel-quid and areca-nut chewing and some areca-nut-derived nitrosamines. Lyon, France: International Agency for Research on Cancer; 2004. International Agency for Research on Cancer. [PMC free article] [PubMed] [Google Scholar]
- 9.Murti P, Gupta P, Bhonsle R, Daftary D, Mehta F, Pindborg J. Effect on the incidence of oral submucous fibrosis of intervention in the areca nut chewing habit. J Oral Pathol Med. 1990;19:99–100. doi: 10.1111/j.1600-0714.1990.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh JS, Motghare DD, Zodpey SP, Wadhva SK. Low birth weight and associated maternal factors in an urban area. Indian Pediatr. 1998;35:33–6. [PubMed] [Google Scholar]
- 11.Gupta PC, Subramoney S. Smokeless tobacco use, birth weight, and gestational age: Population based, prospective cohort study of 1217 women in Mumbai, India. BMJ. 2004;328:15–38. doi: 10.1136/bmj.38113.687882.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta PC, Subramoney S. Smokeless tobacco use and risk of stillbirth: a cohort study in Mumbai, India. Epidemiology. 2006;17:47–51. doi: 10.1097/01.ede.0000190545.19168.c4. [DOI] [PubMed] [Google Scholar]
- 13.Gupta PC, Ray CS. Smokeless tobacco and health in India and South Asia. Respirology. 2003;8:419–31. doi: 10.1046/j.1440-1843.2003.00507.x. [DOI] [PubMed] [Google Scholar]
- 14.Rahman MA, Mahmood MA, Spurrier N, Rahman M, Choudhury SR, Leeder S. Why do Bangladeshi people use smokeless tobacco products? Asia Pac J Public Health. 2015 doi: 10.1177/1010539512446957. doi: 10.1177/1010539512446957. [DOI] [PubMed] [Google Scholar]
- 15.Sinha D, Gupta P, Ray C. Prevalence of smokeless tobacco use among adults in WHO South-East Asia. Indian J Cancer. 2012;49:342–6. doi: 10.4103/0019-509X.107726. [DOI] [PubMed] [Google Scholar]
- 16.Kakde S, Bhopal R, Jones C. A systematic review on the social context of smokeless tobacco use in theSouthAsianpopulation: implications for public health. Public Health. 2012;26:635–45. doi: 10.1016/j.puhe.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Arora M, Madhu R. Banning smokeless tobacco in India: Policy analysis. Indian J Cancer. 2012;49:336–41. doi: 10.4103/0019-509X.107724. [DOI] [PubMed] [Google Scholar]
- 18.Khan A, Huque R, Shah SK, Kaur J, Baral S, Gupta PC. Smokeless tobacco control policies in South Asia: A gap analysis and recommendations. Nicotine Tob Res. 2014;16:890–94. doi: 10.1093/ntr/ntu020. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. WHO report on the global tobacco epidemic, 2008: the MPOWER package World Health Organization 2008 [Google Scholar]
- 20.Gupta V, Yadav K, Anand K. Patterns of tobacco use across rural, urban, and urban-slum populations in a north Indian community. Indian J Community Med. 2010;35:245–51. doi: 10.4103/0970-0218.66877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhawna G. Burden of smoked and smokeless tobacco consumption in India – Results from the Global Adult Tobacco Survey India (GATS India)-2009-2010. Asian Pacific J Cancer Prev. 2013;14:3323–29. doi: 10.7314/apjcp.2013.14.5.3323. [DOI] [PubMed] [Google Scholar]
- 22.Rooban T, Elizabeth J, Umadevi KR, Ranganathan K. Sociodemographic correlates of male chewable smokeless tobacco users in India: a preliminary report of analysis of National Family Health Survey, 2005-2006. Indian J Cancer. 2010;47:91–100. doi: 10.4103/0019-509X.63865. [DOI] [PubMed] [Google Scholar]
- 23.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control. 2003;12 doi: 10.1136/tc.12.4.e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abdullah AS, Driezen P, Ruthbah UH, Nargis N, Quah AC, Fong GT. Patterns and predictors of smokeless tobacco use among adults in Bangladesh: Findings from the International Tobacco Control (ITC) Bangladesh survey. PloS one. 2014;9 doi: 10.1371/journal.pone.0101934. doi: 10.1371/journal.pone.0101934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanifi Choudhury K, A. S. M, Mahmood S. S, Bhuiya A. Socio demographic characteristics of tobacco consumers in a rural area of Bangladesh. J Health Popul Nutr. 2007;25:4456. [PMC free article] [PubMed] [Google Scholar]
- 26.Pradhan Sreeramareddy CT, S. P. M, Mir I. A, Sin S. Smoking and smokeless tobacco use in nine South and Southeast Asian countries: prevalence estimates and social determinants from Demographic and Health Surveys. Popul Health Metr. 2014;12:22. doi: 10.1186/s12963-014-0022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sudman S. Improving the quality of shopping center sampling. J Market Res. :1980423–431. [Google Scholar]
- 28.International Tobacco Control Policy Evaluation Project. Tobacco Control Project India Wave 1 Technical Report (2010-2012) Available from: http://www.itcproject.org/technical-report/?country=India .
- 29.International Tobacco Control Policy Evaluation Project. ITC Bangladesh Survey Wave 2 Technical Report (June 2011) Available from: http://www.itcproject.org/technical-report/?country=Bangladesh .
- 30.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15:355. doi: 10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 31.Festinger L. A theory of cognitive dissonance 1962 Stanford university press [Google Scholar]
- 32.Arnett JJ. Optimistic bias in adolescent and adult smokers and nonsmokers. Addict Behav. 2000;25:625–32. doi: 10.1016/s0306-4603(99)00072-6. [DOI] [PubMed] [Google Scholar]
- 33.Weinstein ND, Marcus SE, Moser RP. Smokers’ unrealistic optimism about their risk. Tob Control. 2005;14:55–9. doi: 10.1136/tc.2004.008375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khawaja M, Mazahir S, Majeed A, Malik F, Merchant K, Maqsood M. Chewing of betel, areca and tobacco: perceptions and knowledge regarding their role in head and neck cancers in an urban squatter settlement in Pakistan. Asian Pac J Cancer Prev. 2006;7:95. [PubMed] [Google Scholar]
- 35.Schensul JJ, Nair S, Bilgi S, Cromley E, Kadam V, Mello SD. Availability, accessibility and promotion of smokeless tobacco in a low-income area of Mumbai. Tob Control. 2013;22:324–30. doi: 10.1136/tobaccocontrol-2011-050148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murukutla N, Turk T, Prasad C, Saradhi R, Kaur J, Gupta S. Results of a national mass media campaign in India to warn against the dangers of smokeless tobacco consumption. Tob Control. 2012;21:12–7. doi: 10.1136/tc.2010.039438. [DOI] [PubMed] [Google Scholar]


