Abstract
Although many studies link teamwork in health care settings to patient safety, evidence linking teamwork to hospital worker safety is lacking. This study addresses this gap by providing evidence linking teamwork perceptions in hospital workers to worker injuries, and further, finds a linkage between manager commitment to safety and teamwork. Organizational records of worker injuries and survey responses regarding management commitment to safety and teamwork from 446 hospital workers within 42 work units in a multi-site hospital system were examined. Results underscored the particular importance of teamwork on worker injuries as well as the importance of management commitment to safety as relating to teamwork. To improve worker safety, organizational leaders and unit managers should work to maintain environments wherein teamwork can thrive.
Keywords: injuries, hospital workers, teamwork, management commitment to safety
1. Introduction
A positive safety climate is critical to keeping workers safe on the job.[1,2] Management commitment to safety, which refers to managers’ demonstrated value of and commitment to workers’ physical safety, is the most important dimension of safety climate, in that it is a known leading indicator of worker safety behaviors, and injuries in a wide variety of jobs,[3,4,5] and in hospital workers specifically.[6] In addition, teamwork is generally considered important in protecting worker safety.[2,7] However, although many studies link teamwork in health care settings to patient safety,[8] evidence linking teamwork to hospital worker safety is lacking. This study addresses this gap by providing evidence linking teamwork perceptions in hospital workers to organizational records of worker injuries, and further, proposes and tests a conceptual model wherein manager commitment to safety facilitates teamwork, which in turn, relates to worker injuries on the job.
From a practical perspective, providing evidence of the importance of teamwork relating to worker safety specifically in a hospital setting will help inform hospital leaders and unit managers of a target for intervention to help keep workers safe (i.e., teamwork), beyond those most commonly related to worker safety (i.e., safety-specific training and climate interventions). Linking management commitment to safety with teamwork also provides an addition to the broader safety literature, wherein worker safety knowledge, safety motivation, and safety behaviors are thought of as the main mediating mechanisms to worker injuries,[1] and teamwork is not conceived as such.
1.1 Management Commitment to Safety
Safety climate represents either individual employee perceptions (psychological climate) or shared employee perceptions (group climate) regarding safety procedures, practices, and behavioral norms around safety. Safety climate at both individual and group levels has been demonstrated to predict worker safety behaviors and, ultimately, worker injuries on the job through influencing workers’ safety knowledge and safety motivation.[1] Management commitment to safety is a specific and critical component of safety climate, which refers to workers’ perceptions of the degree to which their managers value and support safe working and are dedicated to workers’ safety. As mentioned, management commitment to safety predicts worker job-related safety behaviors and incidents/injuries).[7,9– 11]
Managers communicate the relative priority of safety in light of competing demands to their employees, which affects employees’ behaviors and ultimately, the likelihood of employee injuries.[12] For instance, when confronted with a challenging patient-related situation, a hospital worker who perceives a high level of management commitment to safety is more likely to follow strict safety protocol due to management support for following such protocols, and therefore may avoid a needle stick injury. Employees whose managers are committed to safety have expectations that such safe behavior is valued and will be supported by their managers, and further, that unsafe behaviors are discouraged and will be penalized.[13] These expectations translate into behaviors, which in turn, lead to reduced injury risk.
1.2 Teamwork
As mentioned, teamwork is considered to be critical for patient safety in healthcare settings, and has even been identified as a priority by the Agency for Healthcare Research and Quality (AHRQ), the Institute of Medicine, and others.[8] Teamwork is typically conceptualized as part of “patient safety culture”[14] and is included in many measures of leading indicators of patient safety.[15–18]
Despite its apparent importance to determining patient safety, teamwork is typically omitted from studies of worker safety outcomes. In contrast, the literature on worker safety has been dominated to date by a focus on safety-specific climate, or workers’ perceptions of the relative value of worker safety in the working environment, based on enacted policies, practices, and procedures.[13] Indeed, in her meta-analysis, Clarke acknowledged that factors such as work group cohesion and support from coworkers are much less-studied in the safety literature when considering other job-related characteristics, yet they are also likely important to worker safety.[10] Two other prominent meta-analyses of worker safety have only included teamwork indirectly.[1,2] Christian and colleagues refer to “internal group processes” which includes safety-specific communication, as a part of a broader concept of safety climate, and Nahrgang and colleagues refer to teamwork as social support and examined them as part of a broader category of “job resources.” Despite the relative lack of attention, teamwork is a specific critical variable to highlight in relation to worker safety, given its importance in health care settings,[19] along with the fact that it may be influenced by team leaders in order to improve both patient outcomes and worker safety and, thus represents a target for intervention.
In the healthcare domain, Olsen examined a common model of safety among both health care workers and offshore oil and gas workers and found that management support for safety indirectly affected worker safety behaviors through an influence on teamwork, learning, feedback, and safety improvements.[20] This provides some indirect empirical support for the model; yet the outcome variable in that study was self-reported safety behaviors; therefore the results do not reflect relations between teamwork and actual worker injuries; further relations between self-reported variables are subject to potential biasing effects of common method variance.[21] The current study examines worker perceptions of management commitment to safety and teamwork and organizational records of worker injuries, which represents an important advancement to the literature on teamwork as related to health care worker safety.
1.3 Hypotheses
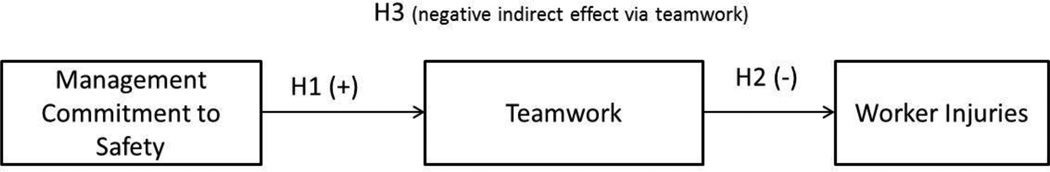
From a theoretical standpoint, management commitment to safety should foster teamwork within work units. According to principles of social exchange, workers who perceive that their manager is concerned about and committed to their physical safety at work are likely to be motivated to reciprocate and enact safety-supportive behaviors in the workplace.[22–26] Supportive attitudes and behaviors engendered by social exchange processes also generally contribute to a positive interpersonal climate where teamwork can thrive. In contrast, in work units where managers do not support workers’ physical safety, workers may lack motivation to engage in behaviors that support both teamwork and workplace safety. Further, by promoting a clear priority of safety and value of workers enacting safety-related behaviors, managers may work to remove some ambiguity from task-relevant situations which would enable better shared understandings of processes and perceptions of effective teamwork. Please see Figure 1.
Hypothesis 1: Management commitment to safety positively relates to teamwork.
Hypothesis 2: Teamwork negatively relates to subsequent worker injuries.
Hypothesis 3: Management commitment to safety is negatively indirectly related to subsequent worker injuries through its association with teamwork.
Figure 1.
Study Hypotheses.
2. Method
2.1 Participants and Procedure
This study was approved by the Institutional Review Board of the university and the participating medical center. Hospital workers (N = 446) within 42 work units within one hospital system in the Midwestern U.S. that includes seven hospitals and approximately 15,000 employees. The seven hospitals encompass one pediatric, one rehabilitation, and five specialty hospitals; five of the seven are urban and two are located in suburban areas. Some of the data used in this study are from a larger study on workplace violence prevention in health care. The 42 units had previously been identified as being at increased risk for workplace violence and aggression using three years of data regarding the probability of occurrence for workplace violence and the severity of previous events within each unit (citation withheld for blind review). Table 1 contains participant characteristics.
Table 1.
Participant Characteristics (N = 446)
| N | % | M | SD | |
|---|---|---|---|---|
| Gender (Female) | 364 | 82% | ||
| Intervention or Control Group (Intervention) | 244 | 55% | ||
| Ethnicity | ||||
| White (not Hispanic or Latino) | 263 | 59% | ||
| Black/African American (not Hispanic or Latino) | 133 | 30% | ||
| Asian (not Hispanic or Latino) | 26 | 6% | ||
| Hispanic | 9 | 2% | ||
| Two or More Races (not Hispanic or Latino) | 6 | 1% | ||
| Age | 42.99 | 13.55 | ||
| Organizational Tenure (years) | 9.10 | 10.01 | ||
| Paid Productive Hours (PPH) Post-Survey | 1411.98 | 731.49 | ||
| Job Category | ||||
| Nursing | 270 | 61% | ||
| Security | 38 | 9% | ||
| Administration/Management | 34 | 8% | ||
| Patient Care Associate | 23 | 5% | ||
| Unit Clerk | 20 | 4.5% | ||
| Allied Health Professional | 18 | 4% | ||
| Other Technician | 16 | 4% | ||
| Clerical | 13 | 3% | ||
| Mental Health Technician | 10 | 2% | ||
| Surgical Technician | 4 | 1% |
As explained in detail below, data for this study included organizational records of workplace injuries, along with worker responses to a paper and pencil survey. Workers completed a survey between April 1, 2013 and May 31, 2013. Initially, 2,010 employees were mailed questionnaires and were supplied with postage-paid return envelopes. Due to some envelopes being sent back by the postal service as undeliverable, a total of 1,921 individuals received mailed paper and pencil surveys, and a total of 446, or 23%, mailed back completed surveys. Survey respondents were similar to the total worker population in terms of gender and employment status, but differed in terms of age (respondents were older than non-respondents), job tenure (respondents had greater tenure), and one job category (fewer patient care associates responded). Participants who completed surveys were mailed a $10 gift card. Participants were identified by a code number on their survey, which hospital system database analysts used to match survey responses with organizational records of workplace injuries.
2.2 Measures
2.2.1 Injuries
Records of worker injuries/adverse occupational events related to a) needle sticks, b) slips, trips, and falls, and c) exposure to blood and body fluids (other than needle sticks) were obtained from an organizational database for a period of 13 months following the survey administration (June 1, 2013 – July 31, 2014). For this paper, we refer to all 3 types of adverse events as “injuries.” Reports of injuries could have been entered into the system by any worker; yet they were most commonly entered by the injured worker or his or her manager. Injuries were matched to afflicted workers’ survey responses using a common identifier. A total of 32 injuries were reported in the months following the survey administration by 30 individual workers. Injuries were modeled as a dichotomous variable 0 (no injury) and 1 (injury).
2.2.2 Management commitment to safety and teamwork
A three item scale was adapted to measure management commitment to safety.[27] The coefficient alpha was .631. A sample item is, “Unit management provides a work climate that promotes workplace safety.” A four-item scale was used to measure teamwork.[27] Coefficient alpha was .91. A sample item is, “People support one another in this unit.” For both measures, the response scale ranged from 1 (strongly disagree) to 5 (strongly agree).
2.2.3 Control variables
Participants’ age, gender, organizational tenure, number of paid productive hours worked (PPH) post survey, pre-survey injury count, and whether the participant was part of the intervention group or control group for the violence prevention intervention were collected from organizational records and assessed as possible control variables when estimating results for teamwork and injuries. No significant correlations were found between any of the possible control variables and post-survey injuries or teamwork. Therefore, no control variables were included in the analyses.[28]
2.3 Analyses
Path analysis was used to test study hypotheses. Due to non-independence in the data stemming from nesting of individual workers within work units, possible aggregation of the study variables to the unit level was tested by examining intraclass correlation coefficients, ICC(1) and the Rwgj index of within group agreement. Using a null model, ICC(1) estimates were: .00 for injuries, .05 for teamwork, and .09 for management commitment to safety. With the exception of the management commitment scale, these values indicate low levels of between-unit variance. Mean/median Rwgj values using the uniform distribution for management commitment to safety were only .51/.54 when negative values were set to zero.[29] Overall, the aggregation statistics indicated that it was appropriate to examine relations between variables at the individual level only. However, the nesting of individuals within groups was accounted for in all analyses using the type=two level command and identifying unit as a cluster variable in MPlus version 7.4. Given the dichotomous nature of the injuries variable, Robust Maximum Likelihood was used as an estimator and odds ratios are given. Traditional fit statistics (chi square, CFI, RMSEA, SRMR) are not available with these types of models to assess global fit. Indirect effect estimates and standard errors were calculated using the model constraint function in MPlus.
3. Results
Descriptive statistics and bivariate correlations are presented in Table 2. As expected, management commitment to safety positively correlated with teamwork, and teamwork negatively correlated with post-survey injuries. However, management commitment to safety did not have a significant bivariate correlation with subsequent injuries.
Table 2.
Correlations and Descriptive Statistics
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mgt. comm. to safety | 3.77 | 0.92 | (.63) | |||||||
| 2. Teamwork | 3.24 | 1.15 | .38** | (.92) | ||||||
| 3. Post-Survey Inj. | 0.72 | 0.28 | −.04 | −.11* | -- | |||||
| 4. Age | 42.99 | 13.55 | .13** | .01 | −.05 | -- | ||||
| 5. Gender | 0.82 | 0.39 | −.01 | −.03 | .04 | −.16** | -- | |||
| 6. Org. Tenure | 9.10 | 10.01 | .00 | .00 | .03 | .61*** | .02 | -- | ||
| 7. PPH | 1411.98 | 731.49 | −.03 | −.03 | .05 | .11* | −.15** | .17** | -- | |
| 8. Pre-Survey Inj. | 0.92 | 0.30 | −.04 | −.04 | −.08 | −.01 | .05 | −.05 | −.02 | |
| 9. Intervention Group | 0.55 | 0.50 | .00 | −.02 | .05 | −.10* | .10* | −.10* | −.02 | .01 |
Note. N = 446.
p < .05.
p < .01.
Coefficient alphas for multi-item scales in parentheses along the diagonal. PPH = Paid productive hours post-survey. For Gender, 0 = male and 1 = female. Age, gender, organizational tenure, PPH, pre-survey injuries, and intervention group included to assess as possible control variables.
Results of path analysis revealed a significant path from management commitment to safety to safety to teamwork (b = .38, p < .001). This indicates support for Hypothesis 1. In support of Hypothesis 2, a significant path was also observed from teamwork to subsequent injuries (b = −.45, p = .02). The odds ratio for subsequent injuries predicted by teamwork was 0.64. There was no support for a direct path from management commitment to safety to injuries when teamwork was included in the model (b = .03, p = .88). BIC, an indicator of model misfit, with that direct path removed was 1368.57, which was lower than when it was included (BIC = 1374.65), indicating slightly better fit of a fully mediated model. In support of Hypothesis 3, the indirect effect from management commitment to safety to injuries via teamwork was significant (ab = −.17, p = .01). Due to the dichotomous nature of injuries and concerns about estimating significance of the products of two paths on different scales, we also ran a Sobel test using the online tool from Preacher and Leonardelli[30] and found further supportive evidence of significant mediation (S = −2.30, p = .02).
4. Discussion
As hypothesized, management commitment to safety related positively to teamwork, which, in turn, predicted subsequent worker injuries in a health care worker sample. Management commitment to safety was not directly associated with subsequent injuries; however, teamwork mediated the effect of management commitment to safety on worker injury. A strength of the current study is that it linked hospital employee perceptions of safety climate to actual documented employee injuries. Previous research of teamwork and safety in health care settings has relied upon self-reports of safety behaviors.[20] This study provides empirical evidence directly linking worker perceptions of teamwork with subsequent organizational records of injuries, which fills an important gap in the research literature and presents an important opportunity for intervention to improve worker safety.
4.1 Implications for Practice
One potential way to improve teamwork by focusing on management commitment to safety was highlighted. Team leaders/managers have a responsibility to create conditions in which their teams can function effectively.[19] By providing consistent commitment and support for safety, managers may facilitate a clear understanding of which behaviors are valued and are likely to be rewarded and enhance teamwork. As mentioned, management commitment to safety may also influence teamwork via mechanisms of social exchange – workers may be motivated to reciprocate and also “pay it forward” when they receive messages from their managers that they care about their physical safety and well-being.
Additional avenues for fostering teamwork in healthcare settings exist outside of the scope of this article. For instance, Gillespie and colleagues examined factors affecting teamwork in a surgical setting, and found three important factors: “building shared understandings through open communication,” “managing contextual stressors in a hierarchical environment,” and intermittent membership influences team performance.”[14] In addition, Salas et al. outlines eight principles for team effectiveness in health care settings, including emphasizing good leadership of teams, providing team members clear roles and responsibilities, promoting shared understanding of the task, teammates, and objectives, taking time to develop processes for feedback, promoting positive team affect, focusing on developing skills around cooperation, communication, and coordination, articulating a clear vision and values, and being able to adapt and learn from mistakes.[19]
Overall, a broad implication of the findings is that narrow safety-specific interventions that fail to encourage or enhance teamwork may be missing an important element for preventing worker injuries. These findings support Clarke’s calls for broader organizational interventions that also include an emphasis on teamwork, rather than solely safety-specific interventions (e.g., focusing on safety training) to improve worker safety.[10]
4.2 Limitations and Future Research Directions
This study is not without limitations. One relates to possible underreporting of injuries.[31] The relatively low response rate on the surveys (23%) is also a limitation of this study. It is possible respondents differed from those who did not respond in other ways than those described in the Method section that might influence the conclusions. For instance, those who perceive a very low level of management support for safety may be less likely to respond to the survey. Notably, Leiter, Laschinger, Day, and Oore attained a similar survey response rate in their Time 2 assessment (28.6%).[32] Yet, in contrast, Sabbath et al. attained a much higher (79%) survey response rate.[33] One possible reason for this is that participants in Sabbath et al. were emailed an online version of the survey; only non-respondents were sent paper versions, whereas participants in the current study only received mailed paper surveys.
The non-significant correlation between management commitment to safety and worker injuries was unexpected, given prior research. However, it notable that many studies have proposed and found support for indirect effects of management commitment to safety via mediators (e.g., work safety knowledge, safety motivation, and safety behaviors).[1] This study adds teamwork as an additional mediator of the effects on management commitment to safety on worker injuries. Additional research is needed to examine specific effects of management commitment to safety directly predicting injuries.
This study was conducted in a single hospital system, and it remains an empirical question as to whether these findings would generalize to other health care organizations or other occupational contexts. Further, the study included units from one hospital system selected based on higher risk for workplace violence. However, the hospitals treat patients with a broad variety of health conditions across a fairly large geographic area and is thus a very diverse system. Future research should nevertheless seek to understand the generalizability of these findings to other contexts. Future research may also examine additional mediators or mechanisms driving relations between teamwork and injuries. For instance, poor teamwork may drive injuries through workers’ subsequent negative affect and cognitive distraction, or emotional exhaustion.[34]
4.3 Conclusion
The findings suggest that teamwork is important for health care organizations to address for keeping workers safe. Evidence was found that management commitment to safety relates to teamwork, which relates to subsequent worker injuries. Organizational leaders and unit manager should actively work to maintain working environments wherein teamwork is fostered in order to keep workers safe.
Acknowledgments
This publication was supported by the CDC-National Institute for Occupational Safety and Health (R01OH009948). The findings and conclusions in this paper are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention or National Institute for Occupational Safety and Health.
Footnotes
When one reverse scored item was removed, alpha = .92. A separate measure was created that excluded this item, and analyses were run using the two-item scale. Results were similar, yet effect sizes for management commitment to safety to teamwork were larger with the two-item scale (results available from first author upon request).
Reference
- 1.Christian MS, Bradley JC, Wallace JC, Burke MJ. Workplace safety: A meta-analysis of the roles of person and situation factors. J Appl Psychol. 2009;94(5):1103–1127. doi: 10.1037/a0016172. http://dx.doi.org/10.1037/a0016172. [DOI] [PubMed] [Google Scholar]
- 2.Nahrgang JD, Morgeson FP, Hofmann DA. Safety at work: A meta-analytic investigation of the link between job demands, job resources, burnout, engagement, and safety outcomes. J Appl Psychol. 2011;96(1):71–94. doi: 10.1037/a0021484. http://dx.doi.org/10.1037/a0021484. [DOI] [PubMed] [Google Scholar]
- 3.Zohar D. A group-level model of safety climate: Testing the effect of group climate on microaccidents in manufacturing jobs. J Appl Psychol. 2000;85(4):587–596. doi: 10.1037/0021-9010.85.4.587. http://dx.doi.org/10.1037/0021-9010.85.4.587. [DOI] [PubMed] [Google Scholar]
- 4.Zohar D, Luria G. The use of supervisory practices as leverage to improve safety behavior: A cross-level intervention model. J Safety Res. 2003;34(5):567–577. doi: 10.1016/j.jsr.2003.05.006. http://dx.doi.org/10.1016/j.jsr.2003.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Zohar D, Luria G. Group leaders as gatekeepers: Testing safety climate variations across levels of analysis. Applied Psychology. 2010;59(4):647–673. http://dx.doi.org/10.1111/j.1464-0597.2010.00421.x. [Google Scholar]
- 6.Gershon RR, Karkashian CD, Grosch JW, Murphy LR, Escamilla-Cejudo A, Flanagan PA, et al. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am J Infect Control. 2000;28(3):211–221. doi: 10.1067/mic.2000.105288. http://dx.doi.org/10.1067/mic.2000.105288. [DOI] [PubMed] [Google Scholar]
- 7.Zohar D, Polachek T. Discourse-based intervention for modifying supervisory communication as leverage for safety climate and performance improvement: A randomized field study. J Appl Psychol. 2014;99(1):113–124. doi: 10.1037/a0034096. http://dx.doi.org/10.1037/a0034096. [DOI] [PubMed] [Google Scholar]
- 8.Havyer RDA, Wingo MT, Comfere NI, Nelson DR, Halvorsen AJ, Mcdonald FS, et al. Teamwork assessment in internal medicine: A systematic review of validity evidence and outcomes. J Gen Intern Med. 2013 Nov;29(6):894–910. doi: 10.1007/s11606-013-2686-8. http://dx.doi.org/10.1007/s11606-013-2686-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beus JM, Payne SC, Bergman ME, Arthur W. Safety climate and injuries: An examination of theoretical and empirical relationships. J Appl Psychol. 2010;95(4):713–727. doi: 10.1037/a0019164. http://dx.doi.org/10.1037/a0019164. [DOI] [PubMed] [Google Scholar]
- 10.Clarke S. An integrative model of safety climate: Linking psychological climate and work attitudes to individual safety outcomes using meta-analysis. J Occup Organ Psychol. 2010;83(3):553–578. http://dx.doi.org/10.1348/096317909X452122. [Google Scholar]
- 11.Mullen JE, Kelloway EK. Safety leadership: A longitudinal study of the effects of transformational leadership on safety outcomes. J Occup Organ Psychol. 2009;82(2):253–272. http://dx.doi.org/10.1348/096317908X325313. [Google Scholar]
- 12.Zohar D. Thirty years of safety climate research: Reflections and future directions. Accid Anal Prev. 2010;42(5):1517–1522. doi: 10.1016/j.aap.2009.12.019. http://dx.doi.org/10.1016/j.aap.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Quick J, Tetrick L. Handbook of occupational health psychology. 2nd. Chapter 8. Washington, D.C.: American Psychological Association; 2011. pp. 141–164. Safety climate: Conceptual and measurement issues. [Google Scholar]
- 14.Gillespie BM, Gwinner K, Chaboyer W, Fairweather N. Team communications in surgery – creating a culture of safety. J Interprof Care. 2013;27(5):387–393. doi: 10.3109/13561820.2013.784243. http://dx.doi.org/10.3109/13561820.2013.784243. [DOI] [PubMed] [Google Scholar]
- 15.Kobuse H, Morishima T, Tanaka M, Murakami G, Hirose M, Imanaka Y. Visualizing variations in organizational safety culture across an inter-hospital multifaceted workforce. J Eval Clin Pract. 2014;20(3):273–280. doi: 10.1111/jep.12123. http://dx.doi.org/10.1111/jep.12123. [DOI] [PubMed] [Google Scholar]
- 16.Modak I, Sexton JB, Lux TR, Helmreich RL, Thomas EJ. Measuring Safety Culture in the Ambulatory Setting: The Safety Attitudes Questionnaire—Ambulatory Version. J Gen Intern Med. 2007;22(1):1–5. doi: 10.1007/s11606-007-0114-7. http://dx.doi.org/10.1007/s11606-007-0114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prati G, Pietrantoni L. Attitudes to teamwork and safety among Italian surgeons and operating room nurses. Work. 2014;49(4):669–677. doi: 10.3233/WOR-131702. http://dx.doi.org/10.3233/WOR-131702. [DOI] [PubMed] [Google Scholar]
- 18.Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006 Mar;6(1) doi: 10.1186/1472-6963-6-44. http://dx.doi.org/10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salas E, Rosen MA, King H. Managing teams managing crises: principles of teamwork to improve patient safety in the emergency room and beyond. Theor Issues Ergon Sci. 2007;8(5):381–394. http://dx.doi.org/10.1080/14639220701317764. [Google Scholar]
- 20.Olsen E. Exploring the possibility of a common structural model measuring associations between safety climate factors and safety behaviour in health care and the petroleum sectors. Accid Anal Prev. 2010;42(5):1507–1516. doi: 10.1016/j.aap.2010.02.002. http://dx.doi.org/doi:10.1016/j.aap.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Podsakoff PM, Mackenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annu Rev Psychol. 2012 Oct;63(1):539–569. doi: 10.1146/annurev-psych-120710-100452. http://dx.doi.org/10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- 22.Credo KR, Armenakis AA, Feild HS, Young RL. Organizational ethics, leader-member exchange, and organizational support: Relationships with workplace safety. Journal of Leadership & Organizational Studies. 2010 Oct;17(4):325–334. http://dx.doi.org/10.1177/1548051810366712. [Google Scholar]
- 23.Cropanzano R, Mitchell MS. Social exchange theory: An Interdisciplinary Review. J Manage. 2005 Jan;31(6):874–900. http://dx.doi.org/10.1177/0149206305279602. [Google Scholar]
- 24.Hofmann DA, Morgeson FP. Safety-related behavior as a social exchange: The role of perceived organizational support and leader–member exchange. J Appl Psychol. 1999;84(2):286–296. http://dx.doi.org/10.1037/0021-9010.84.2.286. [Google Scholar]
- 25.Hofmann DA, Morgeson FP, Gerras SJ. Climate as a moderator of the relationship between leader-member exchange and content specific citizenship: Safety climate as an exemplar. J Appl Psychol. 2003;88(1):170–178. doi: 10.1037/0021-9010.88.1.170. http://dx.doi.org/10.1037/0021-9010.88.1.170. [DOI] [PubMed] [Google Scholar]
- 26.Mearns K, Reader T. Organizational support and safety outcomes: An un-investigated relationship? Saf Sci. 2008;46(3):388–397. http://dx.doi.org/10.1016/j.ssci.2007.05.002. [Google Scholar]
- 27.Sorra J, Nieva V. Hospital survey on patient safety culture. Agency for Healthcare Research and Quality; [cited 2014 Jan 1]. Hospital survey on patient safety culture [Internet] Available from: http://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospcult.pdf. [Google Scholar]
- 28.Carlson KD, Wu J. The illusion of statistical control: Control variable practice in management research. Organ Res Methods. 2011;15(3):413–435. http://dx.doi.org/10.1177/1094428111428817. [Google Scholar]
- 29.James LR, Demaree RG, Wolf G. Estimating within-group interrater reliability with and without response bias. J Appl Psychol. 1984;69(1):85–98. http://dx.doi.org/10.1037/0021-9010.69.1.85. [Google Scholar]
- 30.Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: An interactive calculation tool for mediation tests [Internet] Calculation for the Sobel test: An interactive calculation tool for mediation tests. Available from: http://quantpsy.org/sobel/sobel.htm. [Google Scholar]
- 31.Probst TM, Brubaker TL, Barsotti A. Organizational injury rate underreporting: The moderating effect of organizational safety climate. J Appl Psychol. 2008;93(5):1147–1154. doi: 10.1037/0021-9010.93.5.1147. http://dx.doi.org/10.1037/0021-9010.93.5.1147. [DOI] [PubMed] [Google Scholar]
- 32.Leiter MP, Laschinger HKS, Day A, Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. J Appl Psychol. 2011;96(6):1258–1274. doi: 10.1037/a0024442. http://dx.doi.org/10.1037/a0024442. [DOI] [PubMed] [Google Scholar]
- 33.Sabbath EL, Hurtado DA, Okechukwu CA, Tamers SL, Nelson C, Kim S-S, et al. Occupational injury among hospital patient-care workers: What is the association with workplace verbal abuse? Am J Ind Med. 2013;57(2):222–232. doi: 10.1002/ajim.22271. http://dx.doi.org/10.1002/ajim.22271. [DOI] [PubMed] [Google Scholar]
- 34.Grandey AA, Kern JH, Frone MR. Verbal abuse from outsiders versus insiders: Comparing frequency, impact on emotional exhaustion, and the role of emotional labor. J Occup Health Psychol. 2007;12(1):63–79. doi: 10.1037/1076-8998.12.1.63. http://dx.doi.org/10.1037/1076-8998.12.1.63. [DOI] [PubMed] [Google Scholar]