Abstract
Background:
With the growing utilization of ultrasonography in emergency medicine combined with the concern over adequate pain management in the emergency department (ED), ultrasound guidance for peripheral nerve blockade in ED is an area of increasing interest. The medical literature has multiple reports supporting the use of ultrasound guidance in peripheral nerve blocks. However, to perform a peripheral nerve block, one must first be able to reliably identify the specific nerve before the procedure.
Objective:
The primary purpose of this study is to describe the number of supervised peripheral nerve examinations that are necessary for an emergency medicine physician to gain proficiency in accurately locating and identifying the median, radial, and ulnar nerves of the forearm via ultrasound.
Methods:
The proficiency outcome was defined as the number of attempts before a resident is able to correctly locate and identify the nerves on ten consecutive examinations. Didactic education was provided via a 1 h lecture on forearm anatomy, sonographic technique, and identification of the nerves. Participants also received two supervised hands-on examinations for each nerve. Count data are summarized using percentages or medians and range. Random effects negative binomial regression was used for modeling panel count data.
Results:
Complete data for the number of attempts, gender, and postgraduate year (PGY) training year were available for 38 residents. Nineteen males and 19 females performed examinations. The median PGY year in practice was 3 (range 1–3), with 10 (27%) in year 1, 8 (22%) in year 2, and 19 (51%) in year 3 or beyond. The median number (range) of required supervised attempts for radial, median, and ulnar nerves was 1 (0–12), 0 (0–10), and 0 (0–17), respectively.
Conclusion:
We can conclude that the maximum number of supervised attempts to achieve accurate nerve identification was 17 (ulnar), 12 (radial), and 10 (median) in our study. The only significant association was found between years in practice and proficiency (P = 0.025). We plan to expound upon this research with an additional future study that aims to assess the physician's ability to adequately perform peripheral nerve blocks in efforts to decrease the need for more generalized procedural sedation.
Keywords: Forearm, identification, nerves, sonographic, ultrasound
INTRODUCTION
With the growing utilization of ultrasonography in emergency medicine[1] and the combined concern over adequate pain management,[2] the use of ultrasound-guided regional anesthesia is of growing interest within our field.[3,4] Following the momentum built by the anesthesia community,[5,6,7,8,9] ultrasound-guided nerve blocks are being implemented in the emergency department (ED) setting. There exist a sound number of studies, in both the anesthesia and the emergency medicine literature, supporting the safe and efficient use of ultrasound guidance in the employment of peripheral nerve blocks. However, to perform a peripheral nerve block, one must first be able to reliably identify the specific nerve sonographically before the procedure.
The main objective of this study is to describe the number of peripheral nerve examinations that are necessary for an emergency medicine physician to gain proficiency in accurately locating and identifying the neuroanatomy of the forearm. To become proficient and confident, emergency physicians need to perform a recommended number of supervised peripheral nerve examinations. The number of such studies that would confer proficiency in correctly identifying the nerves of the forearm has yet to be established by the guidelines set forth by the American College of Emergency Physicians (ACEP). This study would provide more objective evidence by which to determine the number of peripheral nerve examinations necessary to gain proficiency.
METHODS
This study was constructed as a prospective, interrupted, time-series design without a control group and was formally approved by the University of South Florida Institutional Review Board before its implementation. The participants in the study were current residents and/or ultrasound fellows enrolled in the emergency residency program and/or emergency medicine ultrasound fellowship at the University of South Florida program at Tampa General Hospital in Tampa, Florida, from May 2012 to October 2012. The resident and fellow participation in this study were voluntary, and informed consent was obtained before the start of the study.
Due to the descriptive nature of this study, formal sample size calculations were not performed. The emergency medicine program at USF enrolls 10 residents per year and may enroll up to one ultrasound fellow per year.
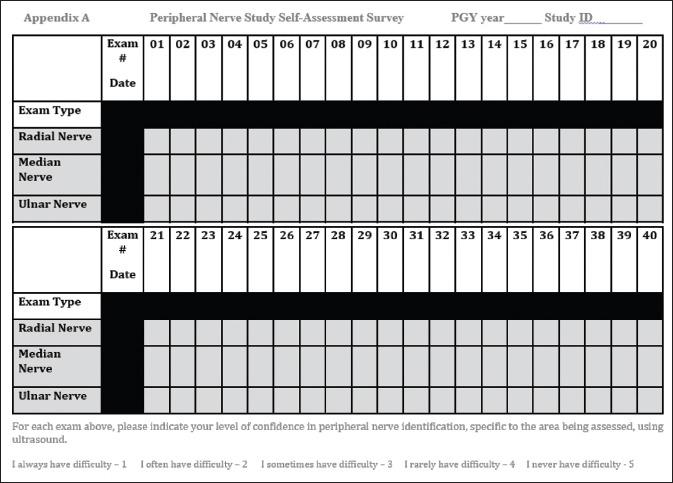
Residents and ultrasound fellows were given an introductory Forearm Peripheral Nerve Block Course (approximately 1 h in length) followed by two supervised hands-on examinations for each nerve. Next, an initial Objective Structured Clinical Examination (OSCE) was performed to evaluate their ultrasound skills and ability to identify the radial, median, and ulnar nerves within the forearm. The number of examinations performed throughout their residency or fellowship was tracked and the residents or fellows were periodically re-evaluated via OSCE. Before performing, each OSCE session participants completed a self-assessment tool [Appendix A] regarding their confidence to correctly locate and identify peripheral nerve anatomy employing the ultrasound machine. Next, their ability to correctly locate and identify the peripheral nerves using ultrasound technology was confirmed by a sonologist experienced in performing soft tissue/musculoskeletal ultrasound which includes visualization of peripheral nerves. The residents’ and fellows’ performance was recorded using a data collection tool. The data collected were then analyzed to determine the median number of examinations required for an emergency medicine physician to become proficient and feel confident in his or her ability to correctly identify peripheral nerves in the upper extremity.
Study participants were excluded if they were determined to have individually completed more than 10 peripheral nerve examinations or simply did not wish to participate in the study. Residents who did not wish to volunteer for the study still received education in regards to the locating of the nerves and proper techniques on how to perform the peripheral blockade of the nerve in question.
The primary study endpoint was the ability to correctly locate and identify, 100% of the time, all of the peripheral nerve anatomies listed in the data tool. The resident or fellow needed to demonstrate this for ten consecutive peripheral nerve examinations to be considered proficient. The secondary study endpoint is the measurement of the resident's or fellow's confidence [Appendix A] in their ability to correctly locate and identify, 100% of the time, all of the peripheral nerve anatomies listed in the data tool.
The results of the data were run by the statisticians of the University of South Florida; a negative binomial regression coefficient was used to describe the data.
The subjects of the OSCE were volunteer members comprised medical students, family members, and nurses. The ultrasound machines used in the study were Sonosite M-Turbo, SonoSite MicroMaxx, and Sonosite Edge (SonoSite Inc., Bothell, Washington 98021, USA). The probes associated with these machines were the Sonosite, L25 × 6–13 MHz, 6 inch, linear array transducer for the M-turbo, and Edge models and the L38e 5–10 MHz, 9 inch, linear array transducer.
RESULTS
The proficiency outcome was defined as the number of attempts before a resident is able to correctly locate and identify 100% of the time all the peripheral nerve anatomies on ten consecutive examinations. Count data are summarized using percentages or medians and range. Random effects negative binomial regression was used for modeling panel count data. P < 0.05 was considered statistically significant.
Complete data for the number of attempts, gender, and postgraduate year (PGY) training were available for 38 residents. Nineteen male and 19 female residents performed examinations. The median PGY year in practice was 3 (range 1–3), with 10 (27%) in year 1, 8 (22%) in year 2, and 20 residents (51%) in year 3 or beyond. The median number (range) of attempts for correctly identifying the radial, median, and ulnar nerves was 1 (0–12), 0 (0–10) and 0 (0–17), respectively. Zero attempts are defined as the resident's ability to achieve proficiency, following only two supervised examinations for ten consecutive examinations with 100% accuracy, from the outset of the proctored OSCE.
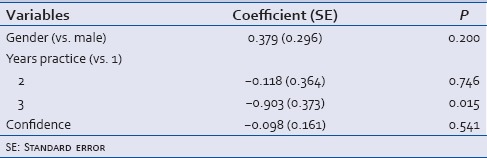
Negative binomial regression for the outcome proficiency was performed to identify significantly associated variables [Table 1]. Negative coefficients indicate increase in proficiency. The only significant association was found between years in practice and proficiency (P = 0.025).
Table 1.
Negative binomial regression coefficients for gender, years in practice, and confidence for 38 residents
The self-reported confidence ratings of each resident or fellow were marked before the completion of each OSCE for each nerve separately. The value range of the confidence scale was set from 1 (not at confident) to 5 (very confident). These data were recorded and analyzed [Figure 1]. All three nerves have statistically significant changes in their respective median confidence scores (at P < 0.001). Radial baseline median confidence = 3 (range 1–4) with an end median confidence = 4 (range 2–5) (P < 0.001). The median baseline median confidence = 3 (range 1–5) with an end median confidence = 4 (range 2–5) (P < 0.001). Ulnar baseline median confidence = 3 (range 1–5) with an end median confidence = 4 (range 2–5) (P < 0.001).
Figure 1.
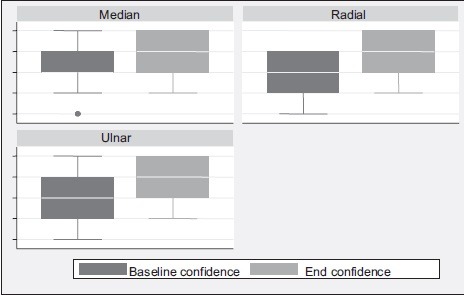
Box plot of confidence by nerve at baseline and endpoint, grouped by nerve type
DISCUSSION
Proficiency in the identification of the peripheral nerves within the forearm compartment was found to be attainable within a reasonably small number of proctored OSCE following 1 h of formalized training and two assisted examinations. No further education was necessary to locate and successfully identify the median and ulnar nerves within the forearm compartment in all of the first ten examinations for the majority of residents involved in this study. The maximum number of attempts at identifying the radial, median, and ulnar nerves 10 consecutive times by any participant was 22, 20, and 27, respectively. The maximum number of assisted OSCE attempts to reach proficiency, as per our definition of 100% accuracy in ten consecutive examinations, for the radial, median, and ulnar nerves was 12, 10, and 17, respectively. In other words it took 17 examinations before the resident then went on to identify the ulnar nerve successfully in the next ten examinations. The difficulty in locating the ulnar nerve was related to the proximity of this nerve to tendons and other soft-tissue structures in its vicinity. The tendons often mimic this nerve when viewed in the transverse axis.
The study also found that the person performing the procedure became more confident as the number of examinations he or she performed increased, signifying that confidence in locating all three nerves improved throughout the study.
The increasing popularity of bedside ultrasound usage in ED has led to the expansion of applications for which it is commonly employed. Previous literature in regards to formalized education and proficiency in using bedside ultrasonography in the realm of regional anesthesia is more commonly available in the anesthesia literature,[5,6,7,8,9] but more recent publications have become available in the emergency medicine literature as well.[3,4,10,11,12] That being said, there has been no formalized study that specifically concentrates on defining proficiency in the identification of the anatomy involved in these procedures. This is what our study set out to accomplish. The ACEP does not set a recommended standard of competency in specific regional anesthetic procedures. We believe that before a reasonable number of completed procedures to demonstrate competency is devised, formal education and evaluation of all aspects of these procedures, including simply locating the structures involved, are of importance.
Limitations
One identified limitation of this study is the small sample size. As a result, only descriptive analysis of the data was possible as there was limited power in the number of participants that we had available to pull from. We completed the study over a 6-month period and, as a result, only had data available for 37 residents and 1 fellow. That being said, the size of each emergency medicine residency at the University of South Florida (10 residents per year) is similar to many other residency programs across the country. A possible second limitation exists in a large number of PGY 3 or higher participants in relation to the number of PGY 1 and 2 participants due to overlap in the academic year.
CONCLUSION
Emergency physicians can develop proficiency in identifying the nerves of the forearm with minimal training. There is an association between years in practice and proficiency suggesting that the speed in which proficiency is reached corresponds to more years of experience in clinical practice. The self-reported confidence of the residents and fellows increased as they performed more examinations. Our study suggests that proficiency is reached more readily in individuals who already have basic ultrasound experience. For this reason, it should be considered a more advanced application that is presented after an initial ultrasound introductory course. Thus, by applying a standardized training curriculum, residents and fellows can become proficient and confident at identifying peripheral nerves in the forearm with the use of ultrasound with only a small amount of formalized instruction, in the way of didactic lecture and supervised hands-on practice.
We believe that the correct identification of neuronal structures is just the first step in teaching regional anesthesia. Before becoming proficient at performing regional blocks, additional education and supervision are required in the areas of equipment selection, needle insertion techniques, injection of regional anesthetic solutions, and patient safety. A future study will aim to expound upon this study and serve to assess the physician's ability (number of procedures completed to define competency) to adequately perform upper extremity peripheral nerve blockade following this additional education. Only after this point, can we evaluate the use of bedside sonography in efforts to decrease the need for more generalized procedural sedation in ED. If proven beneficial, this would likely increase ED efficiency and decrease adverse events associated with procedural sedation, especially given the rising age of the general population and the comorbidities associated with this aging.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge Jotham Keffeler and Sara Marino for their support.
Appendix A
REFERENCES
- 1.Rao VM, Levin DC, Parker L, Frangos AJ, Sunshine JH. Trends in Utilization Rates of the Various Imaging Modalities in Emergency Departments: Nationwide Medicare Data From 2000 to 2008. Journal of the American College of Radiology. 2011;8:706–9. doi: 10.1016/j.jacr.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, et al. Pain in the Emergency Department: Results of the Pain and Emergency Medicine Initiative (PEMI) Multicenter Study. Journal of Pain. 2007;8:460–6. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Herring AA, Stone MB, Fischer J, Frenkel O, Chiles K, Teismann N, et al. Ultrasound-guided Distal Popliteal Sciatic Nerve Block for ED Anesthesia. The American Journal of Emergency Medicine. 2011;29:697.e3–5. doi: 10.1016/j.ajem.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Liebmann O, Price D, Mills C, Gardner R, Wang R, Wilson S, et al. Feasibility of Forearm Ultrasonography-Guided Nerve Blocks of the Radial, Ulnar, and Median Nerves for Hand Procedures in the Emergency Department. Annals of Emergency Medicine. 2006;48:558–62. doi: 10.1016/j.annemergmed.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Bendtsen TF, Nielsen TD, Rohde CV, Kibak K, Linde F. Ultrasound Guidance Improves a Continuous Popliteal Sciatic Nerve Block When Compared with Nerve Stimulation. Regional Anesthesia and Pain Medicine. 2011;36:181–4. doi: 10.1097/aap.0b013e31820d421f. [DOI] [PubMed] [Google Scholar]
- 6.Danelli G, Fanelli A, Ghisi D, Moschini E, Rossi M, Ortu A, et al. Ultrasound vs Nerve Stimulation Multiple Injection Technique for Posterior Popliteal Sciatic Nerve Block. Anaesthesia. 2009;64:638–42. doi: 10.1111/j.1365-2044.2009.05915.x. [DOI] [PubMed] [Google Scholar]
- 7.Perlas A, Brull R, Chan V, Mccartney C, Nuica A, Abbas S. Ultrasound Guidance Improves the Success of Sciatic Nerve Block at the Popliteal Fossa. Regional Anesthesia and Pain Medicine. 2008;33:259–65. doi: 10.1016/j.rapm.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Van Geffen GJ, Van Den Broek E, Braak GJ, Giele JL, Scheiffer GJ. A Prospective Randomised Controlled Trial of Ultrasound Guided versus Nerve Stimulation Guided Distal Sciatic Nerve Block at the Popliteal Fossa. Anesthesia Intensive Care. 2009;37:32–7. doi: 10.1177/0310057X0903700115. [DOI] [PubMed] [Google Scholar]
- 9.Luyet C, Schüpfer G, Wipfli M, Greif R, Luginbühl M, Eichenberger U. Different Learning Curves for Axillary Brachial Plexus Block: Ultrasound Guidance versus Nerve Stimulation. Anesthesiology Research and Practice. 2010;2010:1–7. doi: 10.1155/2010/309462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone MB. Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26:706–10. doi: 10.1016/j.ajem.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Blaivis M. A prospective comparison of procedural sedation and ultrasound-guided interscalene nerve block for shoulder reduction in the emergency department. AcadEmerg Med. 2011;18:922–7. doi: 10.1111/j.1553-2712.2011.01140.x. [DOI] [PubMed] [Google Scholar]
- 12.Francesca BL. Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med. 2010;28:76–81. doi: 10.1016/j.ajem.2008.09.015. [DOI] [PubMed] [Google Scholar]


