Abstract
Introduction:
Male partner HIV testing has been recognized as an important component of prevention of mother-to-child HIV transmission. Scheduled home-based couple HIV testing may be an effective strategy to reach men.
Methods:
Women attending their first antenatal visit at Kisumu County Hospital in Kenya were randomized to home-based education and HIV testing within 2 weeks of enrollment (HOPE) or to written invitations for male partners to attend clinic (INVITE). Male partner HIV testing and maternal child health outcomes were compared at 6 months postpartum.
Results:
Of 1101 women screened, 620 were eligible and 601 were randomized to HOPE (n = 306) or INVITE (n = 295). At 6 months postpartum, male partners were more than twice as likely [relative risk (RR) = 2.10; 95% CI (CI): 1.81 to 2.42] to have been HIV tested in the HOPE arm [233 (87%)] compared with the INVITE arm [108 (39%)]. Couples in the HOPE arm [192 (77%)] were 3 times as likely (RR = 3.17; 95% CI: 2.53 to 3.98) to have been tested as a couple as the INVITE arm [62 (24%)] and women in the HOPE arm [217 (88%)] were also twice as likely (RR = 2.27; 95% CI: 1.93 to 2.67) to know their partner's HIV status as the INVITE arm [98 (39%)]. More serodiscordant couples were identified in the HOPE arm [33 (13%)] than in the INVITE arm [10 (4%)] (RR = 3.38; 95% CI: 1.70 to 6.71). Maternal child health outcomes of facility delivery, postpartum family planning, and exclusive breastfeeding did not vary by arm.
Conclusions:
Home-based HIV testing for pregnant couples resulted in higher uptake of male partner and couple testing, as well as higher rates of HIV status disclosure and identification of serodiscordant couples. However, the intervention did not result in higher uptake of maternal child health outcomes, because facility delivery and postpartum family planning were high in both arms, whereas exclusive breastfeeding was low. The HOPE intervention was successful at its primary aim to increase HIV testing and disclosure among pregnant couples and was able to find more serodiscordant couples compared with the invitation-only strategy.
Trial Registration:
Clinicaltrials.gov registry: NCT01784783.
Key Words: HIV testing and counseling, home-based, PMTCT, pregnancy, male partner, couple, serodiscordant
INTRODUCTION
Male testing during the antenatal period has been identified by the National AIDS Control Council of Kenya as an important strategy for prevention of mother-to-child transmission (PMTCT)1 as susceptibility to HIV acquisition appears higher during pregnancy2–5 and the postpartum period.6–8 Furthermore, male involvement in antenatal care has been associated with better adherence to PMTCT interventions and improved maternal and infant outcomes.9–14 For example, in 1 Kenyan study, HIV acquisition and infant mortality risk were nearly 50% lower with male partner antenatal attendance10 than without. Yet, despite support from key Kenyan agencies and clear benefits of male partner involvement, few male partners are tested. According to Kenya PMTCT programme data, while over 90% of women attending antenatal clinic were tested for HIV in Kenya in 2013, only 4.5% of male partners were tested for HIV in the past 12 months.1 Men cite numerous barriers for partner HIV testing at antenatal clinics, including the belief that antenatal care is a woman's activity and that it is not culturally appropriate as a man to be involved in these visits, as well as not feeling welcome in the clinic.15–22
Nevertheless, partner invitations are the most widely used method among PMTCT programs to try to involve men but have demonstrated limited success, ranging from a 16% partner return rate to a more recent demonstration of 54% return.23–28 Two randomized clinical trials, scheduled home-based testing in Kenya, and partner invitation plus tracing in Malawi, have demonstrated better effectiveness at testing male partners than invitation alone.27,28 Notably in the home-based testing study, 89% of men were reached in the home visit arm compared with 37% reached in the invitation-only arm.27 Home-based testing resulted in higher uptake of male partner testing compared with other strategies during pregnancy, potentially because it overcomes barriers to visiting the antenatal clinic.
Implementation science is well-suited to tackle the barriers of male antenatal involvement as this methodology strives to address issues of service delivery for existing medical interventions, such as couple HIV testing. In this pragmatic trial, we compared the effectiveness of scheduled home visits with pregnant women and their partners to written invitations encouraging men to return to the clinic for the next antenatal visit for couple HIV counseling and testing within a 6-month postpartum follow-up time to increase partner testing and discordant couple identification. This study was conducted in close collaboration with the National AIDS and STD Control Programme, Kenyatta National Hospital, and Kisumu County Hospital.
METHODS
Female Recruitment and Enrollment
Pregnant women attending their first antenatal visit at Kisumu County Hospital from September 2013 to June 2014 were recruited for participation in a randomized clinical trial. Women gave verbal consent to be screened and were asked about demographics, HIV testing history, and relationship status. Women who were ≥14 years of age, ≥8 weeks gestation (previous criteria ≥14 weeks gestation changed midway through enrollment late January 2014 to boost enrollment as women were presenting earlier than expected; gestational age criteria was meant to reduce early pregnancy losses and miscarriages), married or cohabiting, did not have a male partner present at the clinic visit, had a partner ≥18 years of age, planned to live ≤40 km from the clinic now until 9 months postpartum, and had not experienced physical, verbal, or sexual abuse in the past month, were eligible for participation in the study. Eligible women who gave written informed consent were randomly assigned to receive a scheduled home-based partner education and testing (HOPE) visit within 2 weeks of enrollment or a written invitation encouraging the male partner to attend the clinic for couple HIV counseling and testing and a delayed home-based partner education and testing visit at 6 months postpartum (INVITE). Randomization was performed using computer generated nonsequential IDs sequentially ordered on envelopes with randomization assignment concealed inside. Home location visits were completed for all participants on the day of enrollment to improve tracking and follow-up.
Male Recruitment and Enrollment
Male partners of women who were randomized to the HOPE arm were contacted or approached by study staff at the beginning of the study; those who were willing to participate were consented and enrolled at the HOPE intervention visit within 2 weeks of female enrollment. Male partners of women who were randomized to the INVITE arm were contacted or approached by study staff later in the study; those who were willing to participate were consented and enrolled at the 6-month postpartum follow-up visit at home. Study participation was not contingent on willingness to be tested.
Home-Based Intervention and Follow-up
A team of 2 health advisors trained in HIV counseling and testing, 1 male and 1 female, arranged a time to meet the woman and her partner at the couple's home within 2 weeks of the woman's enrollment. Scheduling the home visit was done over the phone or in-person during the home locator visit. In some instances, the visits were conducted at the clinic because of scheduling convenience for the couple and only rarely due to clinic preference over home testing. Couples in the HOPE intervention arm received education regarding facility delivery, exclusive breastfeeding, and postpartum family planning, in addition to pretest and post-test HIV counseling and testing. A brochure was developed using WHO and UNICEF resources29–31 and translated into Dholuo and Kiswahili. It was provided to couples and also served as a guide for health advisors. Serodiscordant and concordant positive couples received further education on HIV prevention and treatment, PMTCT, and the importance of enrolling at a Comprehensive Care Clinic for HIV care.
Women from both study arms visited the clinics at 6 weeks and 14 weeks postpartum for infant immunizations and completed questionnaires with study staff regarding facility delivery, exclusive breastfeeding, and postpartum family planning. Both women and men were visited at home at 6 months postpartum by study health advisors to ascertain partner HIV testing in the antenatal period and were retested for HIV. Couples in the INVITE arm received relevant maternal child health education at this time as well. Follow-up of couples ended in June 2015.
HIV Testing
Women were initially tested at the clinic after enrollment into the study and were retested with their partners at home (HOPE), or at the 6-month follow-up visit (INVITE), after receiving pretest counseling and giving consent for individual and couple testing. Although couple testing was encouraged, individual testing was offered to those who did not want to test as a couple. Rapid tests and testing algorithms were based on the Kenya National AIDS and STD Control Programme HIV testing protocol at the time.
Data Collection and Statistical Methods
Data were collected with mobile smartphones and tablets using Open Data Kit. Stata version 12.0 (College Station, TX) was used to conduct statistical analyses. All analyses were conducted using the intent-to-treat principle. To determine adequacy of randomization, baseline parameters were compared: independent t tests were calculated for comparisons of continuous variables and χ2 tests were calculated for comparisons of categorical variables. RRs were calculated for each outcome of interest using data from the 6-month postpartum follow-up visit. RRs were also calculated for exclusive breastfeeding and postpartum family planning from data from the 6 week follow-up visits.
RESULTS
Screening and Baseline
Figure 1 illustrates study enrollment and participant follow-up. Between September 26, 2013 and June 6, 2014, 1101 pregnant women attending their first antenatal care visit were screened (Fig. 1). Of the 620 (56.3%) eligible women, 601 (96.9%) consented to study participation and were randomly assigned to receive home-based partner education and testing (HOPE) (n = 306) or a written invitation encouraging the male partner to attend the clinic (INVITE) (n = 295). Reasons for ineligibility among the 481 ineligible women, with some being ineligible for more than 1 reason, included being <14 weeks gestation (n = 105, 21.8%), with a change in criteria midway through enrollment to <8 weeks gestation yielding fewer ineligible clients (n = 29, 6.0%), not in a relationship, not married or cohabiting (n = 177, 36.8%), and residing too far from clinic during pregnancy or immediately postpartum (n = 136, 28.3%). Nineteen (4%) eligible women declined to participate in the study. Of the potential male partners to be enrolled, 276 of 306 (90.2%) consented in the HOPE arm at the intervention visit and 240 of 263 (91.3%) consented in the INVITE arm at the 6-month postpartum visit, which was our first contact with them.
FIGURE 1.
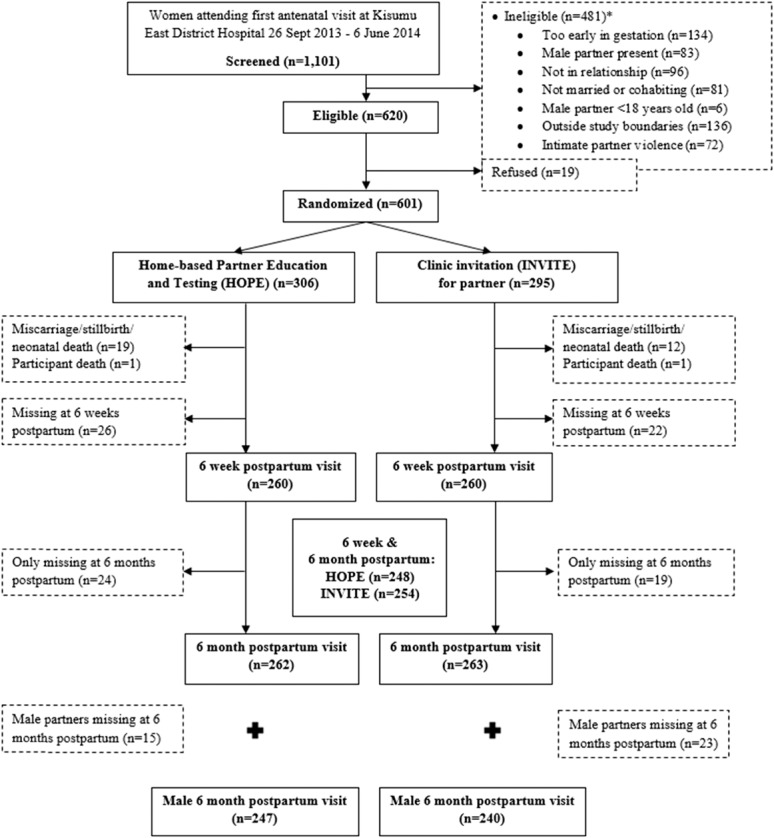
Screening, enrollment, and follow-up of study participants in the home-based partner education and testing (HOPE) study. *Women could be ineligible for more than 1 reason.
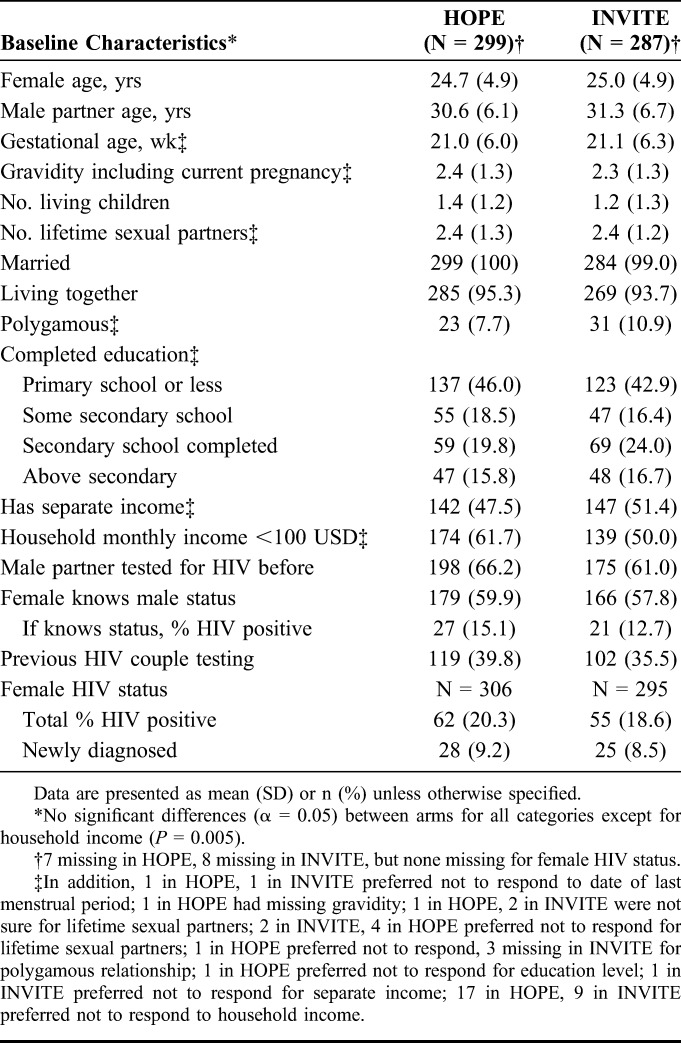
The HOPE and INVITE arms had similar baseline characteristics (Table 1). There were 7 women missing demographic information in HOPE and 8 missing information in INVITE. None were missing information for female HIV status. Mean age was 24.9 years (SD = 4.9) for women and 31.0 years (SD = 6.4) for men. Mean gestation at enrollment was 21 weeks (SD = 6.2), and on average women presenting had 2.4 pregnancies (SD = 1.3), with 28.4% presenting with their first pregnancy. Owing to eligibility criteria requiring being married or living together, all but 3 in the INVITE arm were married, with 554 (94.5%) of 586 couples living together and 54 (9.3%) of 582 women in polygamous marriages. Overall, 260 (44.4%) women completed primary school only or less. Household income differed significantly by arm with 174 (61.7%) of 282 women in HOPE reporting <100 U.S. dollars per month of household income compared with 139 (50.0%) of 278 women in INVITE (P = 0.005). However, having a separate income from their partner was similar in both arms with 289 (49.4%) of all women reporting separate income. Three hundred seventy-three (63.7%) women reported that their partner had been tested for HIV before, and 221 (37.7%) women reported being previously tested as a couple with their current partner. Three hundred forty-five (58.9%) reported knowing their partner's status, and among these 48 (13.9%) women reported that their male partner was HIV positive. In total, 117 (19.5%) of 601 women were HIV positive, with 53 (45.3%) of 117 women diagnosed for the first time at enrollment.
TABLE 1.
Characteristics of Female Participants in the Home-Based Partner Education and Testing (HOPE) and Partner Invitation (INVITE) Arms
Follow-up
Women with miscarriage, stillbirth, or neonatal death and women who had died before 6 weeks postpartum were excluded from follow-up (n = 20, 6.6% in HOPE; n = 13, 4.4% in INVITE) (Fig. 1). Thus, the number of women expected for follow-up was 286 for HOPE and 282 for INVITE. Both arms had similar loss to follow-up [38 (13.3%) vs. 28 (9.9%) women lost, respectively] and greater than 85% retention for women having both a 6-week and 6-month postpartum follow-up. Having both follow-ups was important as complete HIV testing information during the study period was ascertained if a woman had both a 6-week and 6-month postpartum follow-up (n = 248, 86.7% in HOPE; n = 254, 90.1% in INVITE). For males, complete HIV testing information for the study period was gathered at 6 months postpartum (n = 247, 86.4% in HOPE; n = 240, 85.1% in INVITE) and also had greater than 85% retention.
HIV Testing Outcomes
At 6 months postpartum, male partners were more than twice as likely [RR = 2.10; 95% CI: 1.81 to 2.42] to have been HIV tested in the HOPE arm [233/247 (87%) tested] compared with the INVITE arm [108/240 (39%) tested] per their own self-report (Table 2). Male self-report for both arms were used rather than using records of home testing for HOPE men and self-report for INVITE men so as to not differentially ascertain HIV testing between arms and to also include testing outside the home or antenatal clinic. Women in the HOPE arm were also twice as likely to know their partner's HIV status as women in the INVITE arm (RR = 2.27; 95% CI: 1.93 to 2.67), with 217 (88%) of 248 women in HOPE knowing their partner's status compared with 98 (39%) of 254 women in INVITE. One reason for the increased likelihood of disclosure is that couples in the HOPE arm were 3 times more likely (RR = 3.17; 95% CI: 2.53 to 3.98) to have been tested as a couple than the INVITE arm [192 (77%) vs. 62 (24%), respectively] as demonstrated in Table 2.
TABLE 2.
HIV Testing and Maternal and Child Health Outcomes at 6 Months Postpartum by Study Arm
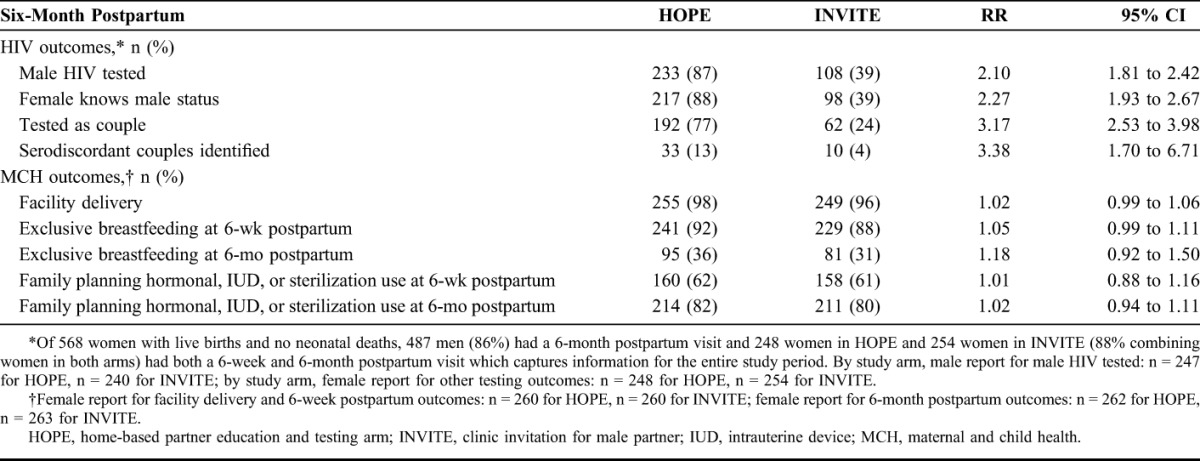
Increase in uptake of partner testing in the HOPE arm also identified greater than 3 times more HIV discordant couples (RR = 3.38; 95% CI: 1.70 to 6.71) in the HOPE arm than the INVITE arm [33 (13%) vs. 10 (4%), respectively] per female report, indicating that women were aware of the discordant status. In addition, more discordant couples in which the male was HIV positive were identified by women in the HOPE arm than in the INVITE arm [13 (5.2%) vs. 1 (0.004%), respectively], although due to low power the RR estimate and CI are unstable (RR = 13.31; 95% CI: 1.75 to 101.01). Furthermore, all of these women did not know they were in discordant partnerships at enrollment. No women in the HOPE arm seroconverted during the study, however, 2 women in the INVITE arm who were HIV negative at enrollment tested HIV positive at 6 months postpartum. One of these women found out her partner was HIV positive sometime after enrollment (was categorized as the 1 male positive discordant in INVITE, although HIV testing at 6 months postpartum revealed she had seroconverted) and 1 who still was unaware of her partner's status at 6 months postpartum.
Maternal Child Health Outcomes
Maternal child health outcomes for both study arms included facility delivery, exclusive breastfeeding, and postpartum family planning. There were high rates of uptake for each of these outcomes in both HOPE and INVITE, with HOPE having slightly higher uptake. The vast majority of women delivered in a health facility [504/520 (97%)], with no significant difference between study arms (RR = 1.02; 95% CI: 0.99 to 1.06).
Most women were exclusively breastfeeding at 6 weeks postpartum [470/520 (90.4%)] with no difference by study arm (RR = 1.05; 95% CI: 0.99 to 1.11). By 6 months postpartum, about a third of women were still exclusively breastfeeding, with a slightly higher uptake in HOPE compared with INVITE [95/262 (36.3%) vs. 81/263 (30.8%), respectively]; this was not statistically different (RR = 1.18; 95% CI: 0.92 to 1.50). However, nearly half of HIV positive women were exclusively breastfeeding at 6 months postpartum [47/100 (47.0%)], but this also did not differ by study arm (RR = 1.05; 95% CI: 0.69 to 1.59). Also, more women in their first pregnancy were more likely to exclusively breastfeed to 6 months postpartum in HOPE compared with INVITE [21/49 (42.9%) vs. 15/60 (25.0%)]; and this yielded a near significant result (RR = 1.71; 95% CI: 0.99 to 2.96).
Family planning uptake was also high in both arms at 6 weeks postpartum, as 318 (61.2%) of 520 women were using a hormonal method, intrauterine device, or sterilization at this time point, which increased to 425 (81.0%) of 525 women by 6 months postpartum, with no significant differences between arms (RR = 1.01; 95% CI: 0.88 to 1.16, and RR = 1.02; 95% CI: 0.94 to 1.11, respectively).
Social Harm/Intimate Partner Violence
One woman in the HOPE arm at 6 months postpartum reported no longer being in the relationship, but she did not attribute it to study participation. In addition, 4 couples in the HOPE arm declined to participate at the 6 months postpartum visit as they informed us they were no longer in a relationship with their partner. They did not attribute this to study participation and no additional information regarding reasons for their separation was obtained. Twelve women in HOPE and 6 women in INVITE reported having experienced physical intimate partner violence (IPV) by their partner at the 6-week postpartum visit, but none attributed this to study participation. Fifty percent of those who experienced IPV in HOPE were in concordant negative partnerships. At the 6-month postpartum visit, 16 women in HOPE (5 of whom also reported IPV at the 6-week postpartum visit) and 12 in INVITE (1 of whom also reported earlier IPV at the 6-week postpartum visit) reported having experienced physical IPV by their partner, and 1 in each arm reported that this might have been due to study participation. All women who experienced IPV were referred to local gender violence services.
DISCUSSION
Among pregnant women in Kisumu, Kenya, home-based partner education and testing resulted in a more than 2-fold increase in male partner testing and HIV status disclosure and a greater than 3-fold increase in couple HIV testing and identification of HIV discordant couples when compared with partner invitation to attend antenatal care. These results have implications for PMTCT programs as partner HIV testing and male involvement during the antenatal period have been observed to increase uptake of PMTCT and improve infant mortality.9–14 The identification of serodiscordant couples is highly relevant in the context of PMTCT as couples can take steps in pregnancy to prevent horizontal transmission, which in turn would prevent vertical transmission. Female identification of discordant partnerships was higher in HOPE compared with INVITE at 6 months postpartum, including discordant partnerships in which the man was HIV positive. Furthermore, all HIV negative women with HIV positive partners were unaware of discordant status at enrollment. Although the study was not powered to investigate transmission, 2 women in INVITE seroconverted, one of whom later found out her partner was positive and 1 who did not know her partner's status, whereas no women in the HOPE arm seroconverted. Finally, although home-based partner education and testing impacted HIV testing outcomes of partner and couple testing and disclosure, as well as serodiscordant couple identification, the intervention did not result in increases in facility delivery, exclusive breastfeeding, or postpartum family planning.
This randomized clinical trial supports findings from a study conducted in nearby Ahero, Kenya, which also compared HIV testing uptake between partners receiving home-based testing and those receiving clinic invitation at 6 weeks postenrollment.27 The HOPE intervention reached a similar proportion of male partners as in the study by Osoti et al (87% vs. 85%, respectively). The longer follow-up time in our study also suggests that the higher uptake of testing comparing home-based testing and clinic invitation persists through pregnancy and up to 6 months postpartum. Furthermore, the HOPE intervention reached more men than other interventions reported in the literature, including invitation plus phone and in-person tracing of male partners to come to the clinic for testing (52% of men),28 home-based door-to-door testing (only 28% of those met in the home were men, and 75% of household members were tested),32 and written invitations alone without follow-up (up to 54% effectiveness).26 However, a one-size-fits-all approach may not be as efficient as leveraging multiple strategies, which would be reasonable given that invitations and partner tracing to come to clinic have recently demonstrated reaching a relatively high proportion of men in the studies by Osoti et al27 and Rosenberg et al28 published in 2015. Each of these methods could be included as part of an escalating strategy of male partner involvement during the antenatal period, starting with invitations then phone tracing to attend clinic, and scheduled home-based visits for those who are not reached with the first methods. Before a full scale-up, a stepped wedge design in a nontrial environment using existing resources would provide additional answers while beginning to deliver the benefits of this intervention to couples in Kenya. This next step would require careful attention and effective monitoring and evaluation of the program because other factors may have influenced the success of these cited interventions, including transport allowance and study compensation. These incentives may have played a role in convincing male partners to join and potentially inflated outcomes. This next step would also include cost-effective models to make sure the escalating strategy of invitations, phone tracing, and home visits would be as promising as using home-based testing alone.
Home-based partner education and testing did not result in increases in facility delivery, exclusive breastfeeding, or postpartum family planning. Rates of these outcomes were high in both arms, leaving little room for improvement. The education provided in the intervention may have been well-received and beneficial, but in the context of high background uptake and high report of participants having engaged in these behaviors in the past, we were unable to see an increase in the outcomes examined in this study. Reasons for high background uptake include a recent introduction of free maternity care including delivery in Kenya and the direct physical referral to family planning nurses from immunization clinic nurses at Kisumu County Hospital. The exception to high uptake was 6 month exclusive breastfeeding, where only a third of women in both arms achieved this, suggesting that a one-time couple education visit during pregnancy may not be enough to support women. However, women who were first time mothers were more likely to have exclusively breastfed to 6 months postpartum in the HOPE arm compared with INVITE, although we were slightly underpowered to observe a significant result. In addition, although there was no difference between study arm, half of HIV positive women exclusively breastfed to 6 months postpartum, suggesting that overall efforts in the clinic or community to encourage women to exclusively breastfeed may be more successful with HIV positive women.
In summary, our study found that scheduled home-based visits are an effective, acceptable, and feasible strategy to conduct couple HIV testing for pregnant women and their partners. In addition, more serodiscordant couples were identified with this method than with written invitation to attend clinic, which is important as the intervention has the potential to prevent further HIV transmission vertically and horizontally. Although there were no observed differences between arms for maternal and child outcomes, home-based couple education on these topics may be influential in areas of lower uptake. Scaling up interventions to involve partners should be considered in antenatal programs in areas of high HIV prevalence to increase partner and couple HIV testing during this vulnerable transmission period.
ACKNOWLEDGMENTS
The authors would like to thank the clinical, outreach, and administrative staff for their work on this study, as well as the participants who made this study possible.
Footnotes
Supported by the U.S. National Institutes of Health (NIH) Grant R01 HD075108. D.K. received support from Achievement Rewards for College Scientists (ARCS) Fellowship, the University of Washington Top Scholar Award and Global Opportunities Health Fellowship (GO Health). C.F. received support from NIH Grant K24 AI087399. J.M. was supported by NIH Research Training Grant R25 TW009345 by the Fogarty International Center, a Boren Awards Fellowship by the National Security Education Program, and 2 Foreign Language Area Studies Fellowships awarded to the University of Washington and the University of Pittsburgh.
Presented at 2016 Conference on Retroviruses and Opportunistic Infections (CROI), February 23, 2016, Boston, MA.
The authors have no funding or conflicts of interest to disclose.
C.F., J.K., A.O.O., D.K., R.B., M.A.G., and V.A. developed and implemented the HOPE trial protocol. D.K., B.B., S.P., J.M., and M.S. created the study questionnaires and assisted with study logistics. M.A.G. and V.A. coordinated data collection. D.K. analyzed the data and drafted the article. All authors contributed to editing of the article and approved submission of the final draft for publication.
This study was approved by the Kenya Ethics Review Committee and the University of Washington Human Subjects Division.
REFERENCES
- 1.National AIDS Control Council of Kenya. Kenya AIDS Response Progress Report 2014: Progress Towards Zero. Joint United Nations Programme on HIV/AIDS (UNAIDS). NACC, Nairobi, Kenya: 2014. Available at: http://www.unaids.org/sites/default/files/country/documents/KEN_narrative_report_2014.pdf. Accessed December 4, 2015. [Google Scholar]
- 2.Gray RH, Li X, Kigozi G, et al. Increased risk of incident HIV during pregnancy in Rakai, Uganda: a prospective study. Lancet. 2005;366:1182–1188. [DOI] [PubMed] [Google Scholar]
- 3.Kinuthia J, Kiarie JN, Farquhar C, et al. Cofactors for HIV-1 incidence during pregnancy and postpartum period. Curr HIV Res. 2010;8:510–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moodley D, Esterhuizen TM, Pather T, et al. High HIV incidence during pregnancy: compelling reason for repeat HIV testing. AIDS. 2009;23:1255–1259. [DOI] [PubMed] [Google Scholar]
- 5.Mugo NR, Heffron R, Donnell D, et al. Increased risk of HIV-1 transmission in pregnancy: a prospective study among African HIV-1-serodiscordant couples. AIDS. 2011;25:1887–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Humphrey JH, Hargrove JW, Malaba LC, et al. HIV incidence among post-partum women in Zimbabwe: risk factors and the effect of vitamin A supplementation. AIDS. 2006;20:1437–1446. [DOI] [PubMed] [Google Scholar]
- 7.Munjoma MW, Mhlanga FG, Mapingure MP, et al. The incidence of HIV among women recruited during late pregnancy and followed up for six years after childbirth in Zimbabwe. BMC Public Health. 2010;10:668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Schacht C, Mabunda N, Ferreira OC, et al. High HIV incidence in the postpartum period sustains vertical transmission in settings with generalized epidemics: a cohort study in Southern Mozambique. J Int AIDS Soc. 2014;17:18808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farquhar C, Kiarie JN, Richardson BA, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37:1620–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aluisio A, Richardson BA, Bosire R, et al. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV free survival. J Acquir Immune Defic Syndr. 2011;66:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peltzer K, Mlambo M, Phaswana-Mafuya N, et al. Determinants of adherence to a single-dose nevirapine regimen for the prevention of mother-to-child HIV transmission in Gert Sibande district in South Africa. Acta Paediatr. 2010;99:699–704. [DOI] [PubMed] [Google Scholar]
- 12.Wettstein C, Mugglin C, Egger M, et al. Missed opportunities to prevent mother-to-child transmission in sub-Saharan Africa: systematic review and data analysis. AIDS. 2012;26:2361–2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delvaux T, Elul B, Ndagije F, et al. Determinants of nonadherence to a single-dose nevirapine regimen for the prevention of mother-to-child HIV transmission in Rwanda. J Acquir Immune Defic Syndr. 2009;50:223–230. [DOI] [PubMed] [Google Scholar]
- 14.Msuya SE, Mbizvo EM, Hussain A, et al. Low male partner participation in antenatal HIV counseling and testing in northern Tanzania: implications for preventive programs. AIDS Care. 2008;20:700–709. [DOI] [PubMed] [Google Scholar]
- 15.Kwambai TK, Dellicour S, Desai M, et al. Perspectives of men on antenatal and delivery care service utilization in rural western Kenya: a qualitative study. BMC Pregnancy and Childbirth. 2013;13:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morfaw F, Mbuagbaw L, Thabane L, et al. Male involvement in prevention of mother to child transmission of HIV: a systematic review to identify barriers and facilitators. Syst Rev. 2013;2:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aarnio P, Olsson P, Chimbiri A, et al. Male involvement in antenatal HIV counseling and testing: exploring men's perceptions in rural Malawi. AIDS Care. 2009;21:1537–1546. [DOI] [PubMed] [Google Scholar]
- 18.Theuring S, Mbezi P, Luvanda H, et al. Male involvement in PMTCT services in Mbeya region, Tanzania. AIDS Behav. 2009;13:S92–S102. [DOI] [PubMed] [Google Scholar]
- 19.Nkuoh GN, Meyer DJ, Tih PM, et al. Barriers to men's participation in antenatal and prevention of mother-to-child transmission care in Cameroon, Africa. J Midwifery Womens Health. 2010;55:363–369. [DOI] [PubMed] [Google Scholar]
- 20.Koo K, Makin JD, Forsyth BWC. Barriers to male-partner participation in programs to prevent mother-to-child HIV transmission in South Africa. AIDS Educ Prev. 2013;25:14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Falnes EF, Moland KM, Tylleskar T, et al. “It is her responsibility”: partner involvement in prevention of mother to child transmission of HIV programmes, northern Tanzania. J Int AIDS Soc. 2011;14:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nyondo AL, Chimwaza AF, Muula AS. Stakeholders' perceptions on factors influencing male involvement in prevention of mother to child transmission of HIV services in Blantyre, Malawi. BMC Public Health. 2014;14:691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katz DA, Kiarie JN, John-Stewart GC, et al. Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS One. 2009;4:e7602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Byamugisha R, Astrom AN, Ndeezi G, et al. Male partner antenatal attendance and HIV testing in eastern Uganda: a randomized facility-based intervention trial. J Int AIDS Soc. 2011;14:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohlala BKF, Boily MC, Gregson S. The forgotten half of the equation: randomized controlled trial of a male invitation to attend couple voluntary counselling and testing. AIDS. 2011;25:1535–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jefferys LF, Nchimbi P, Mbezi P, et al. Official invitation letters to promote male partner attendance and couple voluntary HIV counselling and testing in antenatal care: an implementation study in Mbeya Region, Tanzania. Reprod Health. 2015;12:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osoti AO, John-Stewart G, Kiarie J, et al. Home visits during pregnancy enhance male partner HIV counseling and testing in Kenya: a randomized clinical trial. AIDS. 2014;28:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenberg NE, Mtande TK, Saidi F, et al. Recruiting male partners for couple HIV testing and counselling in Malawi's option B+ programme: an unblinded randomised controlled trial. Lancet HIV. 2015;2(11):e483–e491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control (CDC), World Health Organization (WHO), United Nations Children's Fund (UNICEF), and United States Agency for International Development (USAID). Geneva, Switzerland. Testing and Counseling for Prevention of Mother-to-Child Transmission of HIV (TC for PMTCT) Support Tools. Available at: http://www.who.int/hiv/pub/vct/tc/en/. Accessed November 20, 2015. [Google Scholar]
- 30.World Health Organization (WHO). Reproductive Choices and Family Planning for People Living With HIV. WHO, Department of Reproductive Health and Research, Geneva, Switzerland: 2012. Available at: http://www.who.int/reproductivehealth/publications/family_planning/9241595132/en/. Accessed November 20, 2015. [Google Scholar]
- 31.United Nations Children's Fund (UNICEF). Infant and Young Child Feeding: Counselling Cards for Community Workers. UNICEF, New York, NY; 2012. Available at: http://www.unicef.org/nutrition/files/counseling_cards_Oct._2012small.pdf. Accessed November 20, 2015. [Google Scholar]
- 32.Naik R, Tabana H, Doherty T, et al. Client characteristics and acceptability of a home-based HIV counselling and testing intervention in rural South Africa. BMC Public Health. 2012;12:824. [DOI] [PMC free article] [PubMed] [Google Scholar]


