Abstract
Objective
To evaluate the effectiveness of the Fuel Your Life program, an adaptation of the Diabetes Prevention Program, utilizing implementation strategies commonly used in worksite programs – telephone coaching, small group coaching and self-study.
Methods
The primary outcomes of BMI and weight were examined in a randomized control trial conducted with city/county employees.
Results
Although the majority of participants in all three groups lost some weight, the phone group lost significantly more weight (4.9 lbs.), followed by the small groups (3.4 lbs.) and the self-study (2.7 lbs.). Of the total participants, 28.3% of the phone group, 20.6% of the small group and 15.7 of the self-study group lost 5% or more of their body weight.
Conclusions
Fuel Your Life (DPP) can be effectively disseminated using different implementation strategies that are tailored to the workplace.
Worksites are clearly on the front line of the obesity epidemic. Luckhaupt and colleagues have reported that 27.7% of U.S workers are obese with the prevalence being remarkably consistent across all industry sectors (range of 26.7 to 28.7%).1 Obese workers had the highest prevalence of work limitations and type-2 diabetes2 and obesity-related conditions are estimated to cost employers as much as $73.1 billion dollars annually.3 Studies have shown that obese employees are absent more than non-obese employees, with lost productivity levels estimated at 14% of work time.4
The development and evaluation of the Diabetes Prevention Program (DPP) was a response to the obesity epidemic. The National Institutes of Health funded a multisite clinical research trial that compared a behavioral lifestyle intervention (DPP) to pharmacological treatment (metformin). DPP consisted of 16 lessons conducted over 6 months, with a 6-month maintenance period. Lessons focused on healthy eating, physical activity and overcoming barriers to weight loss and were conducted face-to-face with each participant for about an hour. DPP demonstrated a 58% reduction in the development of Type 2 diabetes in a pre-diabetic population5 which was significantly greater that the pharmacological treatment (31% reduction). DPP was also more cost-effective than the pharmacological intervention.6 It makes sense that workplace health promotion programs could benefit from implementing DPP, although very few have done so to date.7-9
DPP has been one of the most widely translated efficacious programs with most translations occurring in community settings and mirroring DPP's level of intensity (frequency and duration of participant / coach interaction). All of these translations have been effective, although at varying levels. Few translations have varied the intensity of the intervention to achieve a balance between program effects and costs. Finding this intervention “sweet spot” is less important to clinical programs as they are largely concerned with outcomes. However, finding this balance is critical to worksite programs that directly bear the programmatic costs and costs associated with the impact of program participation on employees’ productivity and absenteeism. The purpose of this study was to test optimal levels of Fuel Your Life to maximize outcomes while minimizing costs.
Two important adaptations were introduced to maximize the effects and costs of the program, both revolving around the delivery of the program. First, the program intensity (frequency and duration of interaction with health coach) was reduced to a medium or moderate level (8 sessions instead of 16 for the original DPP). Although there is a strong relationship between program intensity and outcomes,9 it was hypothesized that this should reduce practitioner time and burden and save costs overall without unduly sacrificing program outcomes. Second, the program was conducted in two formats commonly used in worksites: telephone and small groups. Telephone facilitation of a program can provide an opportunity to tailor the program to each participant while increasing the number of employees that can be reached, potentially reaching every employee. It is also more flexible and potentially less disruptive of work activities. Small groups, even though conducted face-to-face, can maximize practitioner effort by reaching multiplepeople at the same time. Small groups also activate the workplace social environment to support the individual in their change efforts, which could offset the inability to tailor the program to each individual.
This study evaluated the effectiveness of the adapted Fuel Your Life (FYL) program with city/county government employees. The primary objective of FYL was similar to DPP - to facilitate weight loss (7% of body weight) while fostering healthy eating and physical activity of participants. It was hypothesized that both small group and phone implementation strategies would be effective compared to the control group. Additionally, it was expected that the program would be less costly than DPP but still effective for reducing diabetes risk.
Methods
Study Design
The study employed an experimental control group design with the three study sites randomly assigned to one of three conditions: telephone coach, small group coach, self-study (control). Data were collected at baseline, 3 months (midpoint), 6 months (posttest) and 12 months (follow-up).
Subjects and Settings
The study was conducted with city-county government employees of three large counties in Georgia. The employee populations ranged from 881 to 2532 employees with employees representing various departments including the court systems, public safety workers (police, fire, sheriff) and public works. As is typical with most worksite health promotion programs, all employees were eligible to participate, however, recruitment was targeted to employees at high risk for developing diabetes (high risk on the Diabetes Risk Screener10 or BMI of 30 or more).
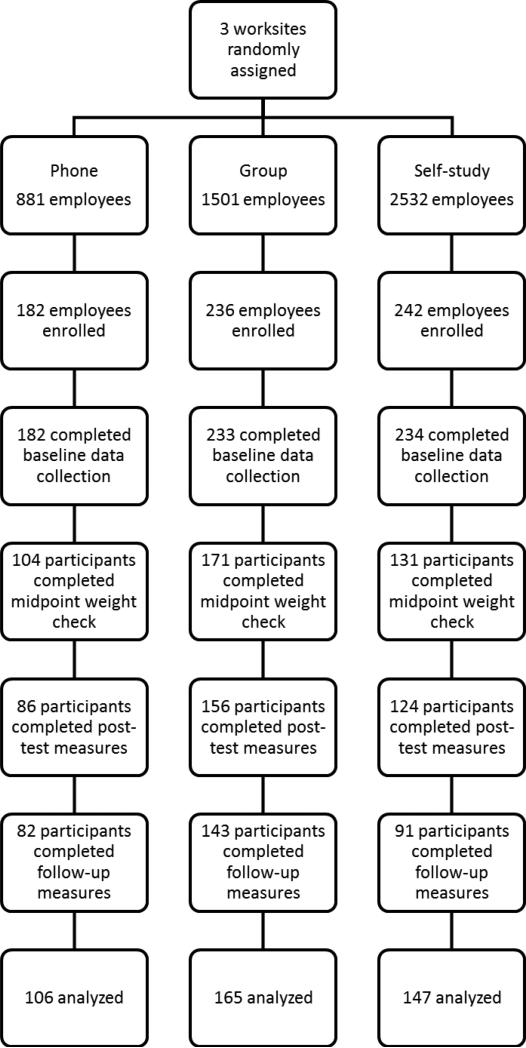
The CONSORT diagram (Figure 1) delineates levels of participation in data collection and inclusion in the analyses. An intent-to-treat analysis was used and participants who had baseline data and at least posttest or follow up data were included in the final analyses. Excluded participants were similar to participants on all demographic variables with the exception of education with the self-study group having slightly higher numbers of individuals with high school degree or less and associate degree. A total of 649 employees across the three sites completed baseline data collection with 418 included in the final analyses for a 64% overall participation rate (58% for phone condition, 71% for small group and 63% for control).
Figure 1.
CONSORT diagram of participant flow through the study.
Intervention
The Fuel Your Life (FYL) program was a translation of the Diabetes Prevention Program (DPP) adapted to the unique characteristics of the workplace. FYL maintained fidelity to the core components of DPP (goal-based behavioral intervention, lifestyle coach delivery, frequent contact, individual tailoring of the intervention, materials for ethnically diverse participations, and network support for the facilitators)11 but modified the participant – coach interaction, ultimately reducing the intensity of the program. The purpose for doing so was to make the program easier to implement, more cost-effective and less disruptive of work. The following describes those adaptations.
Two key aspects of program intensity are the frequency and duration of the interaction. The DPP was considered to be a high intensity program where the coaches met formally one-onone with the participants 16 times over 24 weeks for about one hour each session (8 sessions weekly, 8 sessions every two weeks). FYL adopted a moderate intensity approach which included 8 sessions with a health coach. These sessions were offered in two different formats, both of which are common to workplace health promotion efforts: small group and telephone. Participants in both groups received the FYL program manual, which consisted of the 16 lessons on healthy eating, physical activity and addressing barriers to weight loss originally developed for DPP. The difference was the support that was provided to the participants.
The small groups consisted of 8 to 10 participants that met for approximately 60 minutes each session during the first 6 months of the program (every two weeks for the first four sessions, and monthly for the remaining four sessions) and every two months during the 6 month maintenance period. Each session started with feedback on activities since the last meeting, a review of content and activities for the current lesson and concluded with each person developing an action plan that was to be implemented before the next session. The health coach facilitated the sessions and provided content but sessions were structured to encourage group members to provide support to one another, reinforce concepts by sharing their experiences and hold one another accountable to the program goals and action plans. The same coach facilitated each lesson for a group. The telephone sessions were conducted on-on-one with the health coach and the participant on the same schedule as the group sessions. The format was the same with each lesson lasting around 20 minutes. The participant provided a contact number and the coach called them at a prearranged time. The health coach was better able to tailor the discussion and actions to the specific person, but was solely responsible for reinforcement and accountability as there was no group support. Finally, the study included a comparison group that received the FYL program manual, a brief orientation at baseline which included establishing program goals, and an email reminding them to review each lesson. No other contact by a coach was provided. We referred to this comparison group as the self-study group.
Measures
Data were collected at baseline, midpoint (3 months – for height and weight only), posttest (6 months) and follow-up (12 months) using questionnaires and biometric measures. Participants received a gift card ($10) for completing each questionnaire, but did not receive an incentive for participating in the program. Participation was voluntary and responses were confidential. Responses were matched over time using a participant ID that was generated by and known only to the participant. The study methods were approved by the Institutional Review Board at the University of Georgia.
The primary outcomes for the study were weight and Body Mass Index (BMI). Weight was measured by trained research staff using a portable, calibrated electronic scale (Seca 770). Height was measured using a portable stadiometer (Seca 214). For both measures, two readings were taken in a private setting at the workplace. If the measures varied by more than 5 mm (height) or 0.2 kg (weight) then a third reading was obtained. The mean of the readings was used to calculate BMI following the standard formula (BMI = weight (kg) divided by height2 (m2)).
Secondary measures for the study included food intake and eating behaviors and physical activity. Since reducing fat in the diet was a key component of the intervention, food intake was measured by the 16-item Fat Screener developed by National Cancer Institute.12,13 Scoring followed the rubric developed by the scale developers which results in a calculation of percent calories from fat. Eating behaviors were measured using the Eating Behavior Inventory (EBI).14 The EBI is a 26 item scale that rates both positive and negative weight management behaviors on a five point frequency scale ranging from never to always. The higher the score, the more conducive the individual's behaviors are to weight loss.
Physical activity was measured using two different scales – one for leisure-time activity and one for activity while at work. The Godin Leisure-Time Exercise Questionnaire15 asks participants to estimate the amount of strenuous, moderate, and mild exercise that they perform over a 7-day period. Respondents indicate the number of times per week in their free time they perform certain types of exercise for more than 15 minutes. Scoring followed the formula proposed by the authors which is summarized in Metabolic Equivalent of Task units (METS). The work activity subscale of the Baecke Measure of Habitual Physical Activity was used to measure the amount of activity while at work.16 The seven item scale measures aspects of occupational activity (e.g. ‘at work I sit’, ‘at work I lift heavy loads more than 25 pounds’) and each is rated on a 5-point scale ranging from never to always / very often. Scoring followed the rubric proposed by the developers. Finally, demographics were collected to characterize the sample.
Analyses
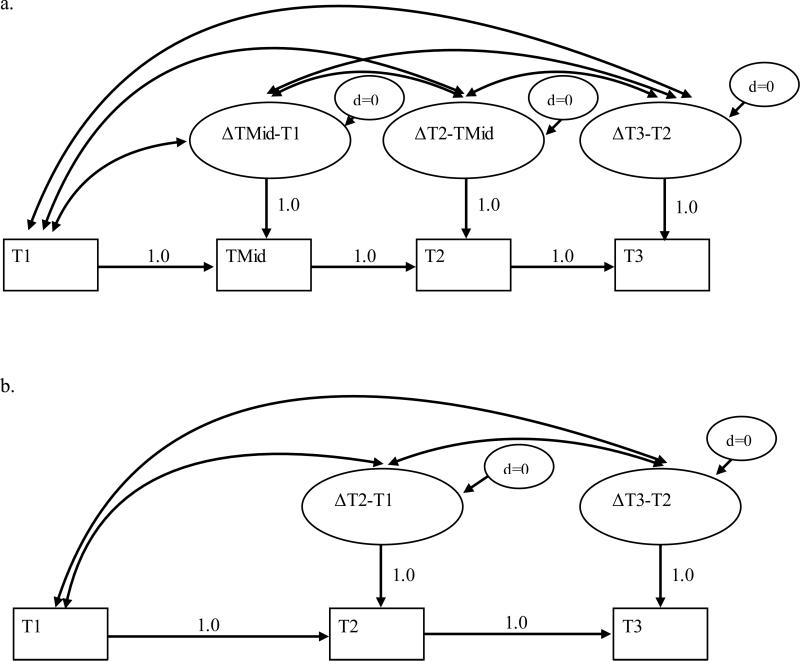
In general, the expectations for the outcomes of the current study focus upon temporal change, and the differences in those temporal changes between the small group, phone and self-study conditions. The analyses for the current study on all of the outcomes were a series of multi-group latent change/difference models (LCM).17,18 Figure 2 summarizes the procedure as applied to the primary (2a) and secondary (2b) outcomes. LCM analysis offers a number of advantages. First, it operationalizes the change from one time point to the next as a latent change score. Therefore, in the case of primary outcomes, there were three latent change scores. For example, ΔTMid-T1 on Figure 2a is the latent difference or change score representing the difference between the midpoint measure and the baseline or T1 measure. Each latent change score has its own mean (slope) and variance with standard errors, and therefore, the statistical significance of the change from one period to the next may be determined. This level of output is not possible with ANOVA. An important advantage of the LCM for the current study was the fact that we could plot the change between times points. Such plots would illustrate the curves associated with change, particularly weight change.
Figure 2.
Basic change models for the primary and secondary outcomes
While the above addresses temporal change in the outcomes, it is the multi-group aspect of the LCM analysis that deals with whether there are differences between the three conditions on the primary and secondary outcomes. Specifically, the differences in the latent change scores between the three conditions can be statistically evaluated. Therefore, and for example, it is possible to test whether the rate of negative change in BMI from T1 to midpoint was significantly greater in the small group condition than in either the phone or self-study conditions. These analyses can be conducted between each of the latent change scores for the primary and secondary outcomes.
With regard to missing data, a maximum likelihood multiple imputation procedure was used as defined in the Mplus statistical package. Prior to testing the hypotheses, however, we studied the pattern of missingness in the database to determine whether missing data for a given case were considered missing at random or not. This is important because multiple imputation produces unbiased estimates when the missingness is at random.19 All of the cases in the current analysis, therefore, met this criterion. In summary, LCM was used to estimate whether or not the primary and secondary outcomes changed significantly from one period of measurement to the next. Further, we statistically tested between the three conditions the strength and direction of change for each latent change score.
Results
Demographics
Participants were mostly female (61%) and white (50%) or Black/African American (44%) with higher levels of education and income (Table 1). Average weight was 212 lbs. and BMI was 33.6, indicating a very overweight / obese sample (64% with a BMI 30 or greater). 71% of participants were at high risk for diabetes. No significant differences between groups were observed on any of the demographic variables.
Table 1.
Demographics of included study participants at baseline.
| Overall (n=418) | Phone (n=106) | Small group (n=165) | Self-study (n=147) | |
|---|---|---|---|---|
| Mean age (yrs) | 46.62 | 47.75 | 45.91 | 46.61 |
| Gender | ||||
| Female | 256 (61.2%) | 72 (67.9%) | 96 (58.2%) | 88 (59.9%) |
| Male | 157 (37.6%) | 34 (32.1%) | 68 (41.2%) | 55 (37.4%) |
| Race/Ethnicity | ||||
| White | 208 (49.8%) | 43 (40.6%) | 104 (63.0%) | 61 (41.5%) |
| Black/African American | 182 (43.5%) | 56 (52.8%) | 51 (30.9%) | 75 (51.0%) |
| Other | 19 (4.5%) | 6 (5.6%) | 8 (4.8%) | 3 (2.1%) |
| Hispanic | 12 (2.9%) | 2 (1.8%) | 8 (4.8%) | 2 (1.4%) |
| Education | ||||
| High school graduate or GED or less | 52 (12.4%) | 12 (11.3%) | 31 (18.8%) | 9 (6.1%) |
| Some college or technical/vocational training | 151 (36.1%) | 51 (48.1%) | 57 (24.5%) | 43 (29.3%) |
| Associate degree | 52 (12.4%) | 11 (10.4%) | 13 (7.9%) | 28 (19.0%) |
| Bachelor degree | 86 (20.6%) | 19 (17.9%) | 36 (21.5%) | 31 (21.1%) |
| Postgraduate work | 69 (16.5%) | 12 (11.3%) | 25 (15.2%) | 32 (21.8%) |
| Income | ||||
| $0-$20,000 | 11 (2.6%) | 2 (1.9%) | 2 (1.2%) | 7 (4.8%) |
| $20,001-40,000 | 111 (26.6%) | 27 (25.5%) | 52 (31.5%) | 32 (21.8%) |
| $40,001-60,000 | 123 (29.4%) | 45 (42.5%) | 41 (24.8%) | 37 (25.2%) |
| $60,001-100,000 | 108 (25.8%) | 17 (16.0%) | 46 (27.9%) | 45 (30.6%) |
| $100,001+ | 46 (11.0%) | 11 (10.4%) | 16 (9.7%) | 19 (12.9%) |
| Body Weight (kilograms) | 96.29 | 95.42 | 95.58 | 98.85 |
| BMI | 33.56 | 33.64 | 32.68 | 34.52 |
| Overweight (BMI 25 – 29.9) | 106 (25.4%) | 22 (20.8%) | 51 (30.9%) | 33 (22.4%) |
| % Obese (BMI 30 or greater) | 269 (64.4%) | 74 (69.8%) | 97 (58.8%) | 98 (66.7%) |
| High Risk on Diabetes Risk Screener | 213 (51.0%) | 59 (55.7%) | 77 (46.7%) | 77 (52.4%) |
| Total High Risk* | 298 (71.3%) | 82 (77.4%) | 109 (66.1%) | 107 (72.8%) |
High risk on diabetes risk screener or BMI of 30 or greater
Primary Outcomes – Weight and BMI
Overall, the majority of participants in all three groups (phone, small group and self-study) lost some weight (Table 2). At the end of the 6 month intervention, 76% of participants in the phone group, 68% in the small group and 68% in the self-study group had lost some weight. By the end of the 6 month maintenance period, the percentages of successful participants had dwindled to 70%, 63% and 60% respectively. Of those individuals who had lost weight, 41% of the phone, 33% of the small group and 26% of the self-study group had lost greater than 5% of their body weight and had maintained that loss.
Table 2.
Percent Weight Change
| No loss/weight gain | 0.01 – 2.5 % loss | 2.6 – 5% loss | 5.1 – 10% | > 10 % loss | |
|---|---|---|---|---|---|
| Baseline - Midpoint | |||||
| Phone | 29 (27.4%) | 38 (35.8%) | 24 (22.6%) | 14 (13.2%) | 1 (0.9%) |
| Small group | 42 (25.5%) | 74 (44.8%) | 28 (17.0%) | 21 (12.7%) | 0 (0.0%) |
| Self-study | 35 (23.8%) | 55 (37.4%) | 43 (29.3%) | 12 (8.2%) | 2 (1.4%) |
| Baseline – Post-test | |||||
| Phone | 26 (24.5%) | 27 (25.5%) | 22 (20.8%) | 27 (25.5%) | 4 (3.8%) |
| Small group | 53 (32.1%) | 55 (33.3%) | 32 (19.4%) | 20 (12.1%) | 5 (3.0%) |
| Self-study | 47 (32.0%) | 40 (27.2%) | 37 (25.2%) | 20 (13.6%) | 3 (2.0%) |
| Baseline – Follow-up | |||||
| Phone | 32 (30.2%) | 25 (23.6%) | 19 (17.9%) | 23 (21.7%) | 7 (6.6%) |
| Small group | 61 (37.0%) | 42 (25.5%) | 28 (17.0%) | 26 (15.8%) | 8 (4.8%) |
| Self-study | 59 (40.1%) | 40 (27.2%) | 25 (17.0%) | 18 (12.2%) | 5 (3.4%) |
The collection of height and weight data at the midpoint of the intervention provided a unique opportunity to examine change over time. Table 3 shows the mean weight and BMI at each data collection point. The phone condition lost 3.9 lbs. (.6 BMI) during the first half of the intervention and another 1.7 lbs. (.3 BMI) during the second half for a total of 5.6 lbs. over the intervention period. Both of these changes (baseline to midpoint and midpoint to posttest) were statistically significant (Table 4). During the maintenance period, the phone group gained .7 lbs. (.1 BMI) which was not significant, so over the course of the study they lost an average of 4.9 lbs. (.77 BMI). The small group lost 3.4 lbs. (.5 BMI) during the first half of the intervention which was statistically significant and maintained their weight during the second half of the intervention. However they gained about .7 lbs. (.1 BMI) during maintenance for an overall weight loss of 2.7 lbs. (.5 BMI). The self-study group lost 4.5 lbs. (.7 BMI) from baseline to midpoint which was statistically significant but gained .3 lbs. from midpoint to posttest for a net loss of 4.2 lbs. at posttest. From posttest to follow-up they gained another 1.5 lbs. (.2 BMI) which was statistically significant. So, all groups lost weight during the first 3 months, with the self-study gaining more of it back by follow-up and the phone and small groups demonstrating better maintenance. Significant change differences between groups existed for the phone and small group and phone and self-study from midpoint to posttest (Table 5) but other changes between groups were not statistically significant.
Table 3.
Means of primary and secondary outcomes (SD)
| Outcome | Baseline | Midpoint | Posttest | Follow-up |
|---|---|---|---|---|
| Body Mass Index | ||||
| Phone | 33.64 (6.90) | 33.03 (6.98) | 32.78 (7.10) | 32.87 (7.14) |
| Small group | 32.68 (7.44) | 32.16 (7.43) | 32.16 (7.51) | 32.29 (7.59) |
| Self-study | 34.52 (7.95) | 33.81 (7.82) | 33.85 (7.67) | 34.08 (7.77) |
| Body Weight (pounds) | ||||
| Phone | 210.36 (22.36) | 206.49 (22.24) | 204.82 (22.47) | 205.47 (22.68) |
| Small group | 208.51 (56.42) | 205.12 (55.83) | 205.10 (56.00) | 205.83 (56.28) |
| Self-study | 217.92 (54.44) | 213.47 (53.29) | 213.73 (52.51) | 215.18 (53.38) |
| Physical Activity – Leisure Activity | ||||
| Phone | 23.79 (24.35) | - | 37.20 (27.05) | 32.30 (25.94) |
| Small group | 28.74 (28.74) | - | 41.17 (26.25) | 37.10 (22.40) |
| Self-study | 23.72 (23.51) | - | 33.37 (29.79) | 29.20 (27.37) |
| Physical Activity – Work Activity | ||||
| Phone | 2.36 (0.61) | - | 2.41 (0.68) | 2.41 (0.61) |
| Small group | 2.46 (0.70) | - | 2.56 (0.75) | 2.49 (0.70) |
| Self-study | 2.46 (0.66) | - | 2.50 (0.67) | 2.38 (0.68) |
| Diet – Eating Behaviors | ||||
| Phone | 76.68 (10.05) | - | 84.01 (9.11) | 85.16 (10.03) |
| Small group | 79.24 (8.63) | - | 82.53 (7.95) | 83.39 (8.36) |
| Self-study | 76.39 (9.50) | - | 81.05 (8.37) | 80.27 (8.69) |
| Diet – Percent Calories from Fat | ||||
| Phone | 38.13 (6.95) | - | 35.04 (6.67) | 36.24 (6.88) |
| Small group | 36.68 (5.25) | - | 35.20 (4.80) | 34.99 (4.48) |
| Self-study | 37.67 (5.32) | - | 35.69 (5.32) | 35.20 (4.96) |
Table 4.
Latent Difference Scores by Site and Time.
| Variable | ΔTMid – T1 | ΔT2 – TMid | ΔT1 – T2 | ΔT3 – T2 |
|---|---|---|---|---|
| Body Mass Index | ||||
| Phone | −0.61** | −0.26** | - | 0.10 |
| Small group | −0.52** | 0.01 | - | 0.12 |
| Self-study | −0.71** | 0.04 | - | 0.22* |
| Body Weight (pounds) | ||||
| Phone | −3.88** | −1.67** | - | 0.65 |
| Small group | −3.39** | −0.02 | - | 0.74 |
| Self-study | −4.45** | 0.27 | - | 1.45* |
| Physical Activity - Leisure Activity | ||||
| Phone | - | - | 13.42** | −4.91 |
| Small group | - | - | 12.44** | −4.08 |
| Self-study | - | - | 9.65** | −4.18 |
| Physical Activity – Work Activity | ||||
| Phone | - | - | 0.05 | 0.01 |
| Small group | - | - | 0.09** | −0.07* |
| Self-study | - | - | 0.04 | −0.12** |
| Diet – Eating Behaviors | ||||
| Phone | - | - | 7.33** | 1.50 |
| Small group | - | - | 3.29** | 0.86 |
| Self-study | - | - | 4.67** | −0.79 |
| Diet – Percent Calories from Fat | ||||
| Phone | - | - | −3.08** | 1.19 |
| Small group | - | - | −1.48** | −0.21 |
| Self-study | - | - | −1.98** | −0.49 |
p<.05
p<.01
Table 5.
Between-Group Differences in Latent Difference Scores.
| Variable | ΔTMid – T1 | ΔT2 – TMid | ΔT1 – T2 | ΔT3 – T2 |
|---|---|---|---|---|
| Body Mass Index | ||||
| Small group vs. Phone | 0.09 | 0.27* | - | 0.03 |
| Small group vs. Self-Study | 0.19 | −0.04 | - | −0.10 |
| Phone vs. Self-study | 0.10 | −0.30* | - | −0.13 |
| Body Weight (pounds) | ||||
| Small group vs. Phone | 0.48 | 1.64* | - | 0.09 |
| Small group vs. Self-Study | 1.06 | −0.29 | - | −0.71 |
| Phone vs. Self-study | −0.57 | −1.93* | - | −0.80 |
| Physical Activity - Leisure Activity | ||||
| Small group vs. Phone | - | - | −0.98 | 0.83 |
| Small group vs. Self-Study | - | - | 2.78 | 0.10 |
| Phone vs. Self-study | - | - | 3.76 | −0.73 |
| Physical Activity – Work Activity | ||||
| Small Group vs. Phone | - | - | 0.04 | −0.07 |
| Small group vs. Self-Study | - | - | 0.05 | 0.05 |
| Phone vs. Self-study | - | - | 0.01 | 0.13* |
| Diet – Eating Behaviors | ||||
| Small Group vs. Phone | - | - | −4.04** | −0.29 |
| Small group vs. Self-Study | - | - | −1.37 | 1.65 |
| Phone vs. Self-study | - | - | 2.67* | 1.94 |
| Diet – Percent Calories from Fat | ||||
| Small group vs. Phone | - | - | 1.60* | −1.40* |
| Self group vs. Self-Study | - | - | 0.49 | 0.29 |
| Phone vs. Self-Study | - | - | −1.11 | 1.68* |
p<.05
p<.01
Secondary Outcomes – Physical Activity and Diet
For the secondary outcomes of physical activity and diet, all groups demonstrated statistically significant increases in leisure activity (Godin) from baseline to posttest with the phone group showing the greatest increase (13.4) followed by small group (12.4) and self-study (9.7)(Tables 3 and 4). Leisure activity for all three groups decreased during the maintenance period at similar levels (4.9, 4.1 and 4.2 respectively). None of the changes were significant between groups (Table 5). Work-related activity (Baecke) showed little change from baseline to follow-up for the phone condition (+.05); small positive changes in the small group from baseline to posttest (+.10) and negative changes posttest to follow-up (−.07) that were statistically significant (Table 4); and statistically significant change from posttest to follow up (−.12) in the self-study group, albeit all of these changes were relatively small.
Statistically significant positive changes in eating behaviors occurred for each group from baseline to posttest (phone: +7.3; small group: +3.3; self-study: +4.7) (Tables 3 & 4). The phone and small group conditions continued to improve their eating behaviors from posttest to follow-up (phone: +1.2; small group: +.9) (Table 3) but at nonsignificant levels (Table 4). Statistically significant differences occurred between the phone and small groups from baseline to posttest (Table 5) and between the phone and self-study group during the same period. A somewhat similar pattern occurred with percent calories from fat. All groups decreased their percent calories from fat from baseline to posttest (phone: −3.1; small group: −1.5; self-study: −2.0) (Table 3); all at statistically significant levels (Table 4). However, from posttest to follow-up, the phone group increased (+1.2) while the small group and self-study groups decreased slightly (small group: −.2; self-study: −.5). Significant between group differences occurred between phone and small group baseline to posttest and posttest to follow-up and between phone and self-study from posttest to follow-up (Table 5).
Discussion
Overall, all three intervention conditions had a positive impact on employee weight and BMI over the course of the study. The phone condition was the most effective with significant between group differences on a variety of outcomes occurring between the phone and self-study group and phone and small group. Although the small group fared better overall than the self-study group on almost every measure, none of these differences were statistically significant. What was most encouraging was the magnitude of change, with 40% of the phone group and one-third of the small group losing more than 5% of their body weight over a year period. This overall weight loss was comparable to other worksite studies adapting DPP both of which had higher levels of intensity (12 sessions vs 8).7,20
One factor that may have impacted the magnitude of the outcomes was the context of the health promotion program at each site. The self-study group site had a very minimal employee wellness program in place at the beginning of the study. Very few health promotion activities were offered to employees and participation in these activities was low. As a result, employees were eager to participate in a convenient and well-designed program that could help them manage their weight. On the other hand, the small group site was at the opposite end of the spectrum. This site offered its employees a sophisticated wellness program with multiple program options offered that had been offered over a number of years with an advanced incentive plan tied to participation. It was a high level program. The phone group site was basically in between the other sites in terms of wellness programming, with a few activities ongoing over a number of years. This may have impacted the study as there were a number of employees ready to change at one site (self-study), while at another (small group) employees were more resistant to change or had not been successful in previous attempts, a tougher group to change overall.
The Diabetes Prevention Program was a very intensive program that demonstrated considerable success (about 12 lbs. weight loss on average). In a previous study, FYL was tested using a peer health coach model, a very low intensity format, with minimal effects (about 1 lb. weight loss on average).9 This study was intended to provide a moderate level of intensity and in the end achieved a moderate impact (about 5 lbs. phone; 3 lbs. small group). Clearly this provides strong evidence for the linear relationship between intervention intensity and outcome. Furthermore, the phone and small group conditions were designed to provide the same level of intensity. The difference was in the format: one-on-one versus group contact. Motivational interviewing (MI), a key strategy of FYL (and DPP), was originally developed as an individual technique – not conducted in group settings. Even though we worked extensively with the health coaches to appropriately use MI in small groups, the greater outcome in the phone group could have been an indication that MI does not translate well to group activities. It was anticipated that the social support structure of the small group would counterbalance the group application of MI, but the data did not support that conclusion. Worksite practitioners should carefully consider the level of intensity in any program that they adopt.
Adopting an intent-to-change analysis using latent change/difference models provided a unique opportunity to examine the extent of change over the course of the study. All three groups lost a significant amount of weight over the first half of the intervention (at midpoint), with only the phone group continuing to lose during the second half (midpoint to posttest). All three groups gained some weight back during the maintenance period from 6 to 12 months (posttest to follow-up) with the self-study group doing so at significantly greater levels than the phone or small group. This would suggest that the primary impact of the health coach was on maintenance. Considering that maintenance of weight loss is probably the biggest challenge that participants face, these findings reinforce the importance of the change agent (health coach) in helping the participant build the skills and problem solving abilities that allowed them to be more successful in maintaining lost weight. If organizations can provide professional support for maintenance long-term, they are likely to get much better outcomes, although the increased time can impact the cost of the program.
Strengths of the study included randomization of worksites into conditions, intent to treat analyses that maximized the number of participants in the final cohort and latent change/difference analyses that enabled us to examine the nature of change over time. Limitations of the study included self-report measures of secondary outcomes, voluntary participation in the study, drop out of approximately 40% of enrolled participants, analyses that enabled imputation of data, and the inclusion in the study of participants not at risk that may have diluted the effects.
These results suggest that the Fuel Your Life translation of the Diabetes Prevention Program using phone and small group formats was effective for weight loss in employed populations. Although overall outcomes were at a lower level than the original clinical trial of DPP, the results were meaningful enough to have a significant impact on population health. Future research should further explore the use of motivational interviewing techniques in group settings and successful strategies for weight maintenance that could be translated to other behaviors.
Acknowledgements
This project was funded by a National Institute of Diabetes and Digestive and Kidney Diseases grant (5R18DK090672-03) Translational Research to Improve Obesity and Diabetes Outcomes. The contents are solely the responsibility of the authors and do not reflect NIH views or policies.
Footnotes
No other financial disclosures were reported by the authors.
Contributor Information
Mark G. Wilson, Workplace Health Group, College of Public Health, University of Georgia, 105 Spear Road, Athens, GA 30602, 706-542-1221 (office), 706-542-6730 (fax).
David M. DeJoy, Workplace Health Group, College of Public Health, University of Georgia.
Robert J. Vandenberg, Department of Management, Terry College of Business, University of Georgia
Phaedra Corso, Economic Evaluation Research Group, College of Public Health, University of Georgia.
Heather Padilla, Workplace Health Group, College of Public Health, University of Georgia.
Heather Zuercher, Workplace Health Group, College of Public Health, University of Georgia.
References
- 1.Luckhaupt SE, Cohen MA, Li J, Calvert GM. Prevalence of obesity among U.S. workers and associations with occupational factors. Am J Prev Med. 2014;46:237–248. doi: 10.1016/j.amepre.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Hertz RP, Unger A, McDonald M, Lustik M, Biddulph-Krentar J. The impact of obesity on work limitations and cardiovascular risk factors in the U.S. workforce. J Occup Environ Med. 2004;46:1193–1203. [PubMed] [Google Scholar]
- 3.Finkelstein EA, DiBonaventura M, Burgess SM, Hale BC. The costs of obesity in the workplace. J Occup Environ Med. 52:971–976. doi: 10.1097/JOM.0b013e3181f274d2. 210. [DOI] [PubMed] [Google Scholar]
- 4.Rodbard HW, Fox KM, Grandy S. Impact of obesity on work productivity and role disability in individuals with and at risk for diabetes mellitus. Am J Health Promot. 2009;23:353–360. doi: 10.4278/ajhp.081010-QUAN-243. [DOI] [PubMed] [Google Scholar]
- 5.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabetes Prevention Program Research Group Within-trial cost-effectiveness of lifestyle intervention or metformin for the primary prevention of Type 2 diabetes. Diabetes Care. 2003;26:2518–2523. doi: 10.2337/diacare.26.9.2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barham K, West S, Trief P, Morrow C, Wade M, Weinstock R. Diabetes prevention and control in the workplace: A pilot project for county employees. J Public Health Man. 2011;17:233–241. doi: 10.1097/PHH.0b013e3181fd4cf6. [DOI] [PubMed] [Google Scholar]
- 8.Kramer MK, Molenaar DM, Venditti E, et al. Improving employee health. Evaluation of a worksite lifestyle change program to decrease risk factors for diabetes and cardiovascular disease. J Occup Environ Med. 2015;57:284–291. doi: 10.1097/JOM.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson MG, DeJoy DM, Vandenberg RJ, Padilla H, Davis M. FUEL Your Life: A translation of the Diabetes Prevention Program to worksites. Am J Health Promot. 2016;30:188–197. doi: 10.4278/ajhp.130411-QUAN-169. [DOI] [PubMed] [Google Scholar]
- 10.Bang H, Edwards AM, Bomback AS, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151:775–783. doi: 10.1059/0003-4819-151-11-200912010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Diabetes Prevention Program Research Group The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc. 2007;107:760–767. doi: 10.1016/j.jada.2007.02.006. doi:10.1016/j.jada.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Williams GC, Hurley TG, Thompson FE, et al. Performance of a short percentage energy from fat tool in measuring change in dietary intervention studies. J Nutr. 2008;138:212S–217S. doi: 10.1093/jn/138.1.212S. [DOI] [PubMed] [Google Scholar]
- 14.O'Neil PM, Rieder S. Utility and validity of the Eating Behavior Inventory in clinical obesity research: A review of the literature. Obesity Rev. 2005;6:209–216. doi: 10.1111/j.1467-789X.2005.00192.x. doi:10.1111/j.1467-789X.2005.00192.x. [DOI] [PubMed] [Google Scholar]
- 15.Godin G, Shephard R. Godin leisure-time exercise questionnaire. Med Sci Sports Exerc. 1997;29(6 Supplement):S36–S38. [Google Scholar]
- 16.Baecke J, Burema J, Frijters J. A short questionnaire for measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 17.McArdle JJ, Nesselroade JR. Longitudinal data analysis using structural equation models. American Psychological Association; Washington, D.C.: 2014. [Google Scholar]
- 18.Newsom JT. Longitudinal structural equation modeling: A comprehensive introduction. Routledge; New York: 2015. [Google Scholar]
- 19.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; New York: 1987. [Google Scholar]
- 20.Kramer MK, Molenaar DM, Arena VC, et al. Improving employee health. Evaluation of a worksite lifestyle change program to decrease risk factors for diabetes and cardiovascular disease. J Occup Environ Med. 2015;57:284–291. doi: 10.1097/JOM.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]