Abstract
Few studies have examined whether parenting prevention programs might mitigate risk for suicidality in parents, yet parent suicidality is a strong risk factor for offspring suicidality. We report results from a randomized controlled trial of a parenting program for deployed National Guard and Reserve (NG/R) families with a school-aged child. Intent-to-treat analyses showed that random assignment to the parenting program (ADAPT) was associated with improved parenting locus of control (LOC). Improved parenting LOC was concurrently associated with strengthened emotion regulation which predicted reductions in psychological distress and suicidal ideation at 12 months post baseline. Results are discussed in the context of ongoing efforts to reduce suicide rates in military populations.
Introduction
Rates of suicide among military service members have increased significantly since 2005, surpassing rates in the general population (Nock et al., 2013), with military leadership seeking ways of reducing suicide as priority (Department of Defense, 2010). Large-scale suicide prevention efforts in the military are underway, with mixed results (Hoge & Castro, 2012). Most suicide prevention efforts have targeted service members. However, 43% of service members have children (Department of Defense, 2013). No research has yet examined the implications of increases in adult military suicides for offspring. However, two recent studies reported greater suicidal ideation among youth with a military parent compared with civilian youth (Gilreath et al., 2015; Reed, Bell, & Edwards, 2011). Research in civilian populations has demonstrated strong links between parent and child suicide ideation and behavior over time – particularly between mothers and their children (Brent et al., 2015; Geulayov et al., 2015).
In this article, we examine whether a parenting prevention program targeting National Guard and Reserve (NG/R) families is effective in reducing psychological distress, including risk for suicidal ideation, among parents. Few analyses have examined crossover effects on suicidality of general family-based prevention programs not originally designed to address suicidality (e.g., Hawkins, et al., 2005). Kerr and associates (2014) found preventive cross-over effects for parent training of foster parents of delinquent girls. The program reduced rates of girls’ depression and in turn suicidality at nine years post-baseline. In this article, we hypothesize that a parenting program targeting military families may ultimately provide benefit not simply to the ostensible outcome (i.e., parenting and child behavior) but also to indicators of suicidal ideation in parents.
The Need for Parenting Programs for Military Families
While belonging to a military family is not associated with any heightened risk to mental health challenges, deployment of a parent is a family stressor associated with increased risk for adjustment difficulties in the service member, at-home partner and child(ren) (Kelley & Jouriles, 2011). Families with a deployed parent face long separations, uncertainty about the parent’s safety, disruptions in communication, and worries during the deployment period. Reintegration following deployment is marked by joy at a parent’s return, and challenges readjusting to family life – particularly when the service member returns with physical and/or psychological injuries. Disruptions in parental functioning (e.g., PTSD symptoms) following deployment are associated with increases in child adjustment problems, as well as with impairments in parenting practices that predict increased child adjustment problems. Research has demonstrated the mediating role of parenting practices in the relationship between a variety of family stressors (i.e., marital transitions, socioeconomic stressors, parent psychopathology) and child risk for psychopathology.
Parent training programs reduce child maladjustment by improving effective parenting practices (e.g., Forgatch & Gewirtz, in press). However, few evidence-based parenting programs have been developed or tailored specifically for military families with school-aged children. The program examined here, After Deployment, Adaptive Parenting Tools (ADAPT), is the first to be evaluated with a randomized controlled trial.
After Deployment, Adaptive Parenting Tools (ADAPT)
ADAPT is a modification for military families of the empirically supported Parent Management Training-Oregon Model (PMTO; Forgatch, Patterson & Gewirtz, 2013) program. The program’s goals are to improve effective parenting practices and thus reduce child risk for emotional and behavioral problems by providing parents with evidence-based parenting tools. Key modifications of the PMTO model in the ADAPT program included a focus on the deployment family context as well as strengthening emotional regulation skills via mindfulness training and emotion coaching (effectively responding to children’s emotions). The capacity to regulate emotions in family interactions (i.e., modulate affective arousal in responding to partner or child) is key for effective parenting, and particularly salient for military families at risk for post-deployment distress, because of the emotional dysregulation inherent in PTSD (Brockman et al., 2015). Thus we hypothesized that an emotional skills-focused parent-training program may improve parenting LOC, and emotion regulation capacities. Hypotheses regarding the intervention’s effects on suicidality were not part of the original study. However, for this paper, we examine whether putative improvements in parenting LOC, and emotion regulation capacities, would, in turn, contribute to reductions in distress (depression and PTSD symptoms) and suicidal ideation in both mothers and fathers. Although not examined in this study, a key rationale for examining suicidality in parents is the potential for outcomes to lead to reductions in risk for suicidal ideation in their offspring.
Method
Participants
The current sample included 336 military families comprising 314 mothers and 294 fathers consenting to participate in a prevention study evaluating the effectiveness of a parenting program (ADAPT; After Deployment Adaptive Parenting Tools). Families with at least one child aged 5 to 12 were eligible to participate in the study if at least one parent had deployed to recent conflicts in Iraq or Afghanistan. Parents were mostly married (84%) with 2–3 children (M=2.34), Caucasian (90%), and in their thirties (mothers’ M = 35.67, SD = 5.89; fathers’ M = 37.75, SD = 6.54). About half (48% of fathers and 52% of mothers) reported completing at least a Bachelor’s degree. Most families reported income between $40,000 to $79,999 (43.5%), or $80,000 to $119,999 (28%), with 84% of fathers and 48% of mothers employed full-time.
Fathers deployed in 96% of families; mothers in 18%; and both parents deployed in 13% of families. Most parents were deployed with the Army National Guard (59%), Army Reserves (30%), and Air National Guard (11%). Fifty one percent of deployed parents were deployed more than once, (M= 1.73; SD=1.16); 58% of deployments were longer than 12 months. Both parents participated in the study/intervention.
The 12-month post baseline (T3) assessment was completed by 255 (81%) mothers, and 226 (76.8%) fathers. There were no significant differences in race, income, age, marital status, and number of children between those who completed the T3 assessment and those who dropped out. However, mothers retained at T3 had more children on average (M = 2.27, SD = 0.59) than mothers who dropped out (M = 2.54, SD = 1.21) as measured at baseline (t(307) = − 2.05, p < .05).
Procedures
Participants were recruited through presentations at pre-deployment and reintegration events for NG/R personnel, mailings, media, and word of mouth. All procedures were IRB approved. Initial participant screening and informed consent occurred online through a confidential study website. Additional self-report data were collected from parents and children during an in-home assessment. Parents received $25 for each online assessment; the family received $50 for each in-home assessment.
Following the baseline assessment (T1), 60% of parents were randomized to the intervention/ADAPT condition and 40% to a services-as-usual condition (consisting of “tip sheets” and online parenting resources). ADAPT is a 14-week multi-family group program targeting improvement of parenting skills via active teaching methods such as role play, practice, and discussion (Gewirtz, Pinna, Hanson, & Brockberg, 2014). Groups of 4–15 parents and 2–3 facilitators met weekly for 2 hours in a local college, church, or community center. Dinner was served and childcare was provided. Videos of parenting skills, handouts, and mindfulness practices were also available online.
Online self-report measures – included all measures below - were collected again from parents six months after the baseline assessment (T2) and both online and in-home measures were collected 12 months post- baseline (T3). All measures in the current study, except for the Posttraumatic Stress Disorder Checklist/PCL, were gathered at T1, T2, and T3. The PCL, due to concerns about potential distress of respondents, was only gathered during in-person interviews (i.e. at T1 and T3).
Measures
Psychological Distress
Psychological distress was measured with the Posttraumatic Stress Disorder Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) and the Hopkins Symptoms Checklist Depression subscale (HSCL-25; Hesbacher et al., 1980). The Posttraumatic Stress Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item standardized, clinically validated self-report questionnaire assessing posttraumatic stress disorder (PTSD) as defined by the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (American Psychiatric Association, 1994). Deployed military parents completed the PCL-M (military version), in which the items refer to a traumatic military experience, while non-deployed parents completed the PCL-C (civilian version), rating PTSD symptoms in the past month using a 5-point scale from 1 (not at all) to 5 (extremely). The PCL demonstrated good internal consistency in the present sample (T1 and T3 mother α =.91, .93; father α =.94, .96).
The second indicator of psychological distress was the 15-item depression subscale of the HSCL-25. Items were rated on a scale from 1 (not at all) to 4 (extremely) (T1 and T3 mother α =.92, .92; father α =.90, .95, respectively). One item asking how much the respondent had thoughts of ending your life was recoded to 0 for not at all and 1 for a little, quite a bit, or extremely to indicate suicidal ideation. Data were dichotomized because of few occurrences of ratings of 2 or more. The counts including mothers and fathers combined were 24 parents (5.1%) endorsing a 1, 4 parents (0.8%) endorsing a 2, and 1 parent (0.2%) endorsing a 3. The ideation item was removed from the Psychological Distress construct in models below. The item was retained for mean comparisons in Table 1 for comparability to studies using the HSCL. For mothers in the sample, 2% indicated suicidal ideation at T1 and 3% at T3, while, 7% of fathers indicated so at T1 and 9% at T3 (12 months).
Table 1.
Means, Standard Deviations, and Analysis of Covariance Effect and Effect Size of ADAPT Intent to Treat by Parent
| Mothers | ||||||||||
| Intervention | Control | ADAPT Effects | ||||||||
| Pre | Post | Pre | Post | ANCOVA | ||||||
| M | SD | M | SD | M | SD | M | SD | F | η2 | |
| Parenting Locus of Control 6 mos. | 3.65 | .40 | 3.81 | .43 | 3.59 | .45 | 3.59 | .49 | 14.53*** | .06 |
| Difficulty Emotion Regulation 6 mos. | 69.67 | 19.94 | 65.40 | 18.01 | 67.61 | 19.21 | 68.22 | 19.84 | 4.43* | .02 |
| PTSD Symptomology 12 mos. | 27.34 | 9.02 | 24.90 | 9.09 | 27.09 | 10.45 | 27.40 | 10.34 | 5.12* | .03 |
| Depressed Symptomology 12 mos. | 1.53 | .48 | 1.48 | .47 | 1.57 | .49 | 1.50 | .44 | .17 | .00 |
| Suicidal Ideation 12 mos. | .01 | .10 | .05 | .22 | .03 | .18 | .01 | .10 | 2.46 | .01 |
| Fathers | ||||||||||
| Parenting Locus of Control 6 mos. | 3.67 | .41 | 3.73 | .49 | 3.66 | .38 | 3.59 | .49 | 4.13* | .02 |
| Difficulty Emotion Regulation 6 mos. | 69.67 | 19.94 | 69.33 | 20.17 | 69.39 | 18.30 | 68.47 | 20.10 | .02 | .00 |
| PTSD Symptomology 12 mos. | 30.29 | 12.90 | 29.27 | 12.65 | 29.45 | 11.55 | 28.10 | 11.44 | .05 | .00 |
| Depressed Symptomology 12 mos. | 1.52 | .51 | 1.43 | .49 | 1.52 | .50 | 1.48 | .43 | .02 | .00 |
| Suicidal Ideation 12 mos. | .07 | .26 | .10 | .30 | .08 | .27 | .08 | .28 | .07 | .00 |
p< .001;
p <.01;
p <.05
Because the PCL and the HSCL depression subscale formed a one-factor solution in factor analyses, each scale score was rescaled to range from 1 to 5 and averaged to examine pre-post change in psychological distress. Mean findings are reported for raw scale scores for each indicator, suicide item removed from HSCL for analyses.
Emotion regulation
Emotion regulation skills were assessed for each spouse using the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). The DERS is a 36-item self-report questionnaire assessing problems with emotion regulation. Participants rate their responses on a 5-point scale ranging from 1 (almost never) to 5 (almost always). Higher total sum scores indicate more difficulties with emotion regulation. The scale has established convergent, discriminant and construct validity and adequate internal consistency (Gratz & Roemer, 2004) (T1 and T2 mother α =.95, .94; father α =.95, .95).
Parenting Locus of Control
Short Form Revised(PLOC - SFR); (Hassall, Rose, & McDonald, 2005) is a shortened form of the Parental Locus of Control Scale (PLOC; Campis, Lyman, & Prentice-Dunn, 1986). The 24-item self-report questionnaire measures parenting control orientation (i.e., internal vs. external) in four dimensions: parental efficacy, parental responsibility, child control of parents’ life, and parental control of child’s behavior. Participants rated the items on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree). A total mean score was obtained, with high scores indicating high sense of control or internality and low scores indicate an external locus of parenting control(LOC) (T1 and T2 mother α =.75, .79; father α =.73, .83).
Analytic Strategy
Using pre- and post-intervention scores we specified a time-ordered cascade model of intervention effects to test the hypotheses that ADAPT may improve parent LOC and reduce emotion regulation problems as proximal targets of the intervention at T2. In turn, changes in these proximal intervention effects are hypothesized to galvanize 12-month reductions in psychological distress and suicidal ideation.
Using two related approaches we tested intent to treat (ITT) effects on the primary outcomes using Analysis of Covariance controlling for baseline scores. Related, we then specified a time-ordered auto-regressive path model to test indirect influence of the ITT effects from proximal to distal outcomes. Using methods outlined for cascading effects (Dodge et al., 2009), we estimated an intervention cascade model in the Mplus 7.31 structural equation program because it can estimate path models with continuous and logistic outcomes (Muthén & Muthén, 2015). The model was estimated with weighted least squares with robust standard errors, means and variances (WLSMV).
Model fit was evaluated using recommended fit indices (McDonald & Ho, 2002) including a chi-square minimization p value above .05, a CFI above .95; a chi-square ratio (χ2/df) less than 2.0; and a root mean square error of approximation (RMSEA) below .08.
Results
Means, standard deviations and effect sizes are reported in Table 1 by group condition and by military parent. Pre-post ANCOVA models were conducted for parenting LOC, emotion regulation problems, PTSD and depression. Three of the four outcomes demonstrated ITT effects for mothers. These were parenting LOC, F (1, 230) = 14.53, p <.001, η2 = .06; emotion regulation problems, F (1, 230) = 4.43, p <.05, η2 = .05; and PTSD symptoms, F (1, 190) = 14.53, p <.001, η2 = .06. Using Cohen’s (1988) characterization of effect size, partial η2 indicated the ADAPT intervention had a medium effect on improving maternal LOC, and small effects on mothers’ emotion regulation and PTSD symptoms. Among the father outcomes, there was only one direct ITT effect. The ADAPT intervention significantly improved fathers’ parenting LOC F (1, 192) = 4.13, p <.05, η2 = .02, with a small effect size.
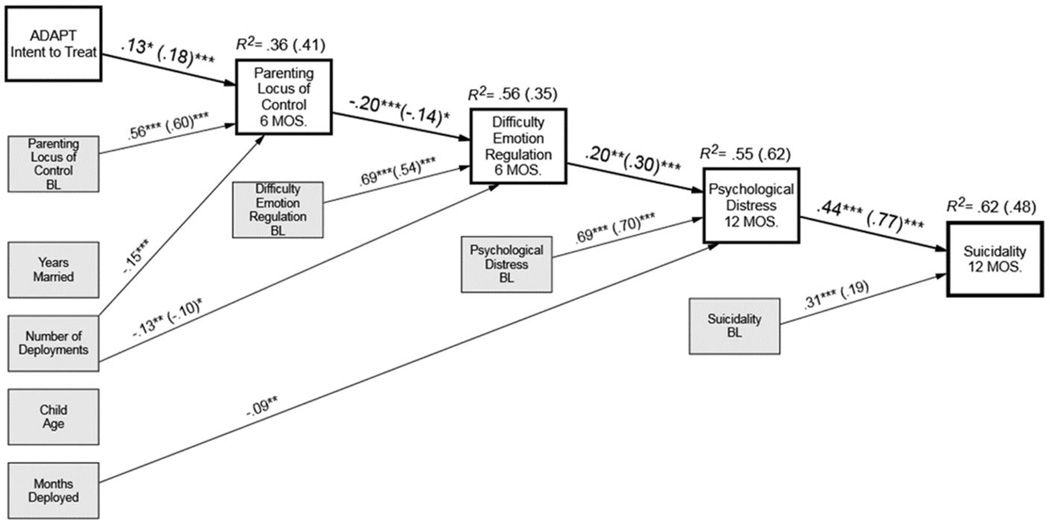
In the next step of the analyses we specified a time-ordered model testing ITT effects on distal outcomes via proximal outcomes. Models were run separately for mothers and fathers. We controlled for baseline status, years married, number of deployments, age of the child, and months deployed. Results are shown in Figure 1 in the form of standardized beta paths. Mother parameters are shown in parentheses, fathers are outside parentheses. Although all dependent variables in the cascade were regressed on control predictors as well as the ITT comparison, only significant paths are displayed for clarity. Although there were few distal main effects for fathers, a preventive cascade model and hypotheses were supported for both mothers and fathers. The significant improvements in LOC were associated with reductions in emotion regulation problems at 6 months. Change in emotion regulation problems was associated with reductions in the psychological distress construct at 12 months. Reductions in distress predicted a lower likelihood of endorsing suicidal ideation at 12 months.
Figure 1.
Structural equation path model for suicidality preventive intervention cascade for ADAPT post-deployed military families. Paths are standardized estimates. Father parameters (Mother parameters). BL=baseline. Model estimated with weighted least square estimator with robust standard errors, means, and variances (WLSMV). ***p < .001; **p <.01; *p <.05; Father model fit: χ2 (29) = 34.48, p = 22, CFI = .98, RMSEA = .02; χ2/df = 1.18; Mother model fit: χ2 (29) = 46.33, p = .02, CFI = .96, RMSEA = .04; χ2/df = 1.59.
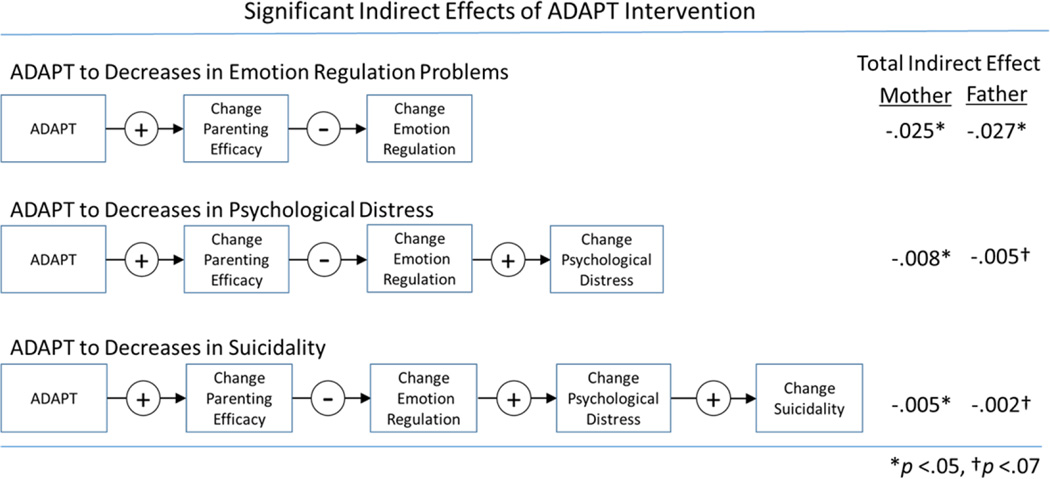
Using directional hypotheses, the indirect effect for ITT to suicidality in Figure 1 was −.005 (p <.044) for mothers, and was −.002 (p < .072) for fathers. The indirect effect to psychological distress was −.008 (p <.033) for mothers and was −.005 (p <.055) for fathers. Overall, the statistical model obtained excellent fit for fathers and adequate fit to the data for mothers (father model fit: χ2 (29) = 34.48, p = .22, CFI = .98, RMSEA = .02; χ2/df = 1.18; mother model fit: χ2 (29) = 46.33, p = .024, CFI = .96, RMSEA = .04; χ2/df = 1.59). Figure 2 provides a summary of the indirect effects of the ADAPT intervention on parent suicidality, through parenting efficacy, emotion regulation and psychological distress.
Figure 2.
Summary of indirect effects for ADAPT intervention. Estimates are sum of standardized indirect effects
Discussion
Our findings indicate that an emotional skills-enhanced parent training program for military families – ADAPT – improved parenting locus of control, leading to reductions in mothers’ and fathers’ suicidal ideation at 12 months post-baseline. One primary main effect was replicated for both mothers and fathers; a significant increase in parenting efficacy over 6 months. For mothers, main effects were observed for decreases in emotion problems and decreases in PTSD symptomatology. Although no further main intervention effects for fathers were observed, for both mothers and fathers, there were statistically reliable indirect effects linking the ADAPT intervention and improvements in parenting efficacy to subsequent reductions in problem outcomes including lower likelihood of suicidal ideation relative to the control group. Improved locus of control was associated with fewer concurrent difficulties in emotion regulation, and six months later, those improvements predicted reductions in psychological distress (PTSD and depression symptoms) and in turn lower suicidal ideation. So although fathers did not exhibit direct benefit on 12-month psychological outcomes, ADAPT demonstrated significant indirect effects in the cascade of outcomes benefiting fathers in the RCT.
Direct effects of the ADAPT program on reductions in emotion regulation problems and PTSD symptoms were limited to mothers. There are two possible reasons for this. In military families, as in civilian families, mothers are typically primary caregivers. Moreover, deployment and military service, which disproportionately affects fathers, is associated with long absences, i.e., fewer opportunities to parent, and to regulate emotions in family interactions. Despite this, fathers found ADAPT to be acceptable and feasible; they participated in the ADAPT group sessions almost as frequently as mothers (47% vs. 53%) and were equally satisfied (Gewirtz et al., 2014).
Another possible reason that ADAPT’s direct effects on parent distress, particularly PTSD symptoms and emotion regulation problems, were limited to mothers, is that the program is insufficiently potent to directly improve outcomes in those who have been exposed to more severe traumatic events or who demonstrate more difficulties at baseline (i.e., fathers). At baseline, for example, 16% of fathers but just 6% of mothers reported clinical levels of PTSD symptom severity; similarly, 7% of fathers but just 2% of mothers reported suicidal ideation. If ADAPT had smaller direct effects in fathers, the power to detect them was insufficient given our sample size. However, in prior research with the PMTO prevention model, effect sizes for both key outcomes and crossover effects (e.g., socioeconomic status changes) were found to magnify over time (e.g., Patterson et al., 2010). It is conceivable then, that fathers may experience improvements in outcomes over time.
The goal of ADAPT was not to treat parents’ psychological distress (PTSD, depression or suicidality), but to provide them with parenting tools to improve their children’s outcomes. Prior data suggests that parent suicidality is strongly related to suicidal ideation and behaviors of their children. This is particularly the case for the transmission of suicidality between mothers and their children (Brent et al., 2015). Given the relatively high-risk military context for suicide, it seems important for future research to investigate whether the reduced risk for suicidality in parents in the ADAPT condition will be associated with lowered child suicidal ideation and behaviors.
Limitations
In this study, parenting LOC and emotion regulation were measured concurrently, as were psychological distress and suicidality. Only a replication of this model over more time points can establish true directionality. Moreover, suicidality was not the focus of the larger study and was measured with one item. Positive endorsement of the item could have reflected a range of ideation severity. The proportion of the sample reporting suicidal ideation was smaller than the 10–15% recommended for a logistic regression and so these results should be interpreted with caution.
In conclusion, our findings indicate that ADAPT appears to reap benefits beyond enhanced parenting skills. Parents felt more positive about their capacity to be effective; these feelings of competence were associated, in turn, with fewer difficulties in emotion regulation and less distress (depression and PTSD). And reductions in distress were associated with less likelihood of suicidal ideation. These findings run parallel to findings from other prevention studies showing cross-over effects on children’s suicidality (e.g., Lynn et al., 2014). Future research on the effects of parenting factors on children’s outcomes should consider better measures of suicide ideation and behavior. However, our findings provide preliminary evidence for the utility of parenting programs to address one of the most tragic public health challenges for our nation’s military community.
Contributor Information
Abigail H. Gewirtz, Department of Family Social Science & Institute of Child Development, & Institute for Translational Research in Children’s Mental Health, University of Minnesota.
David S. DeGarmo, Prevention Science Institute, Department of Educational Methodology, Policy, and Leadership, University of Oregon.
Osnat Zamir, Institute for Translational Research in Children’s Mental Health, University of Minnesota.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: Diagnostic criteria from DSM-IV. American Psychiatric Association; 1994. [Google Scholar]
- Brent DA, Melhem NM, Mann JJ. Pathways to offspring suicidal behavior may begin with maternal suicide attempt. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(10):868. doi: 10.1016/j.jaac.2015.07.010. [doi] [DOI] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, DeGarmo D. Relationship of service members' deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology (Division 43) 2015 doi: 10.1037/fam0000152. doi:2015-45467-001 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campis LK, Lyman RD, Prentice-Dunn S. The parental locus of control scale: Development and validation. Journal of Clinical Child Psychology. 1986;15:260–267. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Department of Defense. Final Report of the DOD Task Force on Prevention of Suicide by Members of the Armed Forces. Washington, DC: 2010. The Challenge and the Promise: Strengthening the Force, Preventing Suicide, and Saving Lives. [Google Scholar]
- Department of Defense. Demographics profile of the military community. Washington DC: Author; 2013. Retrieved from http://download.militaryonesource.mil/12038/MOS/Reports/2013-Demographics-Report.pdf. [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monographs of the Society for Research on Child Development. 2009;74(3):vii-119. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forgatch MS, Gewirtz AH. Kazdin A, Weisz J, editors. Evolution of Parent Management Training-Oregon Model: A dynamic model of an empirically supported intervention. Evidence Based Psychotherapies for Children and Adolescents. (in press) [Google Scholar]
- Forgatch MS, Patterson GR, Gewirtz AH. Looking forward the promise of widespread implementation of parent training programs. Perspectives on Psychological Science. 2013;8:682–694. doi: 10.1177/1745691613503478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geulayov G, Metcalfe C, Heron J, Kidger J, Gunnell D. Parental suicide attempt and offspring self-harm and suicidal thoughts: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(5):509.e2–517.e2. doi: 10.1016/j.jaac.2013.12.022. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Pinna KL, Hanson SK, Brockberg D. Promoting parenting to support reintegrating military families: After deployment, adaptive parenting tools. Psychological Services. 2014;11(1):31–40. doi: 10.1037/a0034134. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilreath TD, Wrabel SL, Sullivan KS, Capp GP, Roziner I, Benbenishty R, Astor RA. Suicidality among military-connected adolescents in california schools. European Child & Adolescent Psychiatry. 2016;25(1):61–66. doi: 10.1007/s00787-015-0696-2. [doi] [DOI] [PubMed] [Google Scholar]
- Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Eemotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Hassall R, Rose J, McDonald J. Parenting stress in mothers of children with an intellectual disability: The effects of parental cognitions in relation to child characteristics and family support. Journal of Intellectual Disability Research. 2005;49:405–418. doi: 10.1111/j.1365-2788.2005.00673.x. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: Long-term effects from the seattle social development project. Archives of Pediatrics & Adolescent Medicine. 2005;159(1):25–31. doi: 10.1001/archpedi.159.1.25. doi:159/1/25 [pii] [DOI] [PubMed] [Google Scholar]
- Hesbacher PT, Rickels K, Morris RJ, et al. Psychiatric illness in family practice. Journal of Clinical Psychiatry. 1980;41(6–10) [PubMed] [Google Scholar]
- Hoge CW, Castro CA. Preventing suicides in US service members and veterans: Concerns after a decade of war. Jama. 2012;308(7):671–672. doi: 10.1001/jama.2012.9955. [doi] [DOI] [PubMed] [Google Scholar]
- Kelley ML, Jouriles EN. An introduction to the special section on U.S. military operations: Effects on military members' partners and children. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2011;25(4):459–460. doi: 10.1037/a0024569. [doi] [DOI] [PubMed] [Google Scholar]
- Kerr DCR, DeGarmo DS, Leve LD, Chamberlain P. Juvenile justice girls’ depressive symptoms and suicidal ideation 9 years after multidimensional treatment foster care. Journal of Consulting and Clinical Psychology. 2014;82(4):684–693. doi: 10.1037/a0036521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn CJ, Acri MC, Goldstein L, Bannon W, Beharie N, McKay MM. Improving youth mental health through family-based prevention in family homeless shelters. Children and Youth Services Review. 2014;44:243–248. doi: 10.1016/j.childyouth.2014.05.024. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP, Ho M-HR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7(1):64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables User's Guide. Seventh. Los Angeles, CA: StatModel; 1998–2015. [Google Scholar]
- Nock MK, Deming CA, Fullerton CS, Gilman SE, Goldenberg M, Kessler RC, Ursano RJ. Suicide among soldiers: A review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. doi: 10.1521/psyc.2013.76.2.97. doi: http://doi.org/10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Forgatch MS, DeGarmo DS. Cascading effects following intervention. Development and Psychopathology. 2010;22(4):949–970. doi: 10.1017/S0954579410000568. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed SC, Bell JF, Edwards TC. Adolescent well-being in Washington state military families. American Journal of Public Health. 2011;101(9):1676–1682. doi: 10.2105/AJPH.2011.300165. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. Oct, [Google Scholar]