Abstract
Objective
Brief interventions for adolescent marijuana users offered in schools reach users who otherwise would not present for treatment. The current study builds on previous trials of a school-based, two-session Motivational Enhancement Therapy (MET) intervention by adding periodic, brief motivational check-ins to reinforce gains and bolster motivation.
Methods
Adolescent participants were randomly assigned to a Motivational Check-In (MCI; n = 128) or Assessment-only Check-In (ACI; n = 124) comparison condition. Both conditions received two sessions of MET. Participants in the MCI condition then attended three MET-based check-in sessions at 4-, 7-, and 10-months after baseline, while the ACI condition participants attended assessment-only check-ins at the same time points. Optional cognitive behavior therapy (CBT) sessions were available as needed for twelve months from baseline in both conditions.
Results
Outcomes were assessed at 6, 9, 12, and 15 months after baseline. Participants (59% Caucasian; 68% male; Mean age = 15.84) reported using marijuana on an average of 37 of the last 60 days and 70%% met diagnostic criteria for a marijuana use disorder. Both conditions were associated with reduced use and negative consequences that were sustained throughout the 15 months of follow-up. The MCI condition resulted in greater reductions at the 6-month follow-up but differences between conditions were not found at later follow-ups, and MCI participation did not increase engagement in CBT as predicted.
Conclusions
Results replicated the efficacy of the brief intervention for adolescent marijuana use and provided mixed evidence on the utility of adding repeated check-in sessions.
Keywords: motivational enhancement therapy, marijuana, brief intervention
Introduction
Marijuana remains the most frequently used illicit substance with 8.4%, or 22.2 million, Americans having used in the past month (Center for Behavioral Health Statistics and Quality, 2015). Several national surveys (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2016; Center for Behavioral Health Statistics and Quality, 2015; Washington State Department of Health, 2014) note the high prevalence and frequency of use among adolescents; 7.4% of youth ages 12–17 reported past month use (Center for Behavioral Health Statistics and Quality, 2015). Almost 45% of youth try marijuana by their senior year of high school and 6% are daily users (Johnston et al., 2016). A reported 4.2 million people age 12 and over had a marijuana disorder (abuse or dependence) which was second only to alcohol (17.0 million) and more than twice the rate of the next substance, pain relievers (1.9 million) (Center for Behavioral Health Statistics and Quality HSA, 2015). The risk of dependence increases for those who start in adolescence, going from 9% for adult initiators to 17% for adolescents and almost 50% for daily users (National Institute on Drug Abuse, 2014).
A growing body of research across multiple domains highlights the long term deleterious effects associated with adolescent marijuana use. Academic risks include doubling the chances of receiving poor grades: 48% vs. 20% and 42% vs. 23% for 10th and 12th graders respectively (Washington State Department of Health, 2014). Longitudinal studies show greater likelihood of dropping out of high school among regular marijuana users (46%) relative to those who have never used (20%) (Silins et al., 2014). Heavy, persistent use of marijuana during adolescence may impact brain development and neuropsychological functioning including executive functions, memory, processing speed, perceptual reasoning, and verbal comprehension (Meier et al., 2012). Regular marijuana use in adolescence was related to an average decline of eight IQ points over a twenty-five year follow-up; those losses persisted even after discontinuing use (Meier et al., 2012). Mental health outcomes include increased likelihood of becoming dependent on marijuana or other drugs, attempting suicide (Silins et al., 2014) and experiencing psychosis (e.g., McGrath et al., 2010).
Despite marijuana being the leading reason for adolescent substance abuse treatment admissions (United States Department of Health and Human Services, 2014) an estimated 90% of heavy users never receive treatment (Dennis, Clark, & Huang, 2014). Non-participation in treatment may be partly explained by perceptions of risk. Teenagers perception of risk associated with casual use of marijuana decreased from 2007 to 2013 by 15% (54.6% to 39.5%; Johnston et al., 2014). Other barriers likely include access without parental involvement and stigma associated with needing treatment. Those who engage in treatment most often are coerced by school administrators, parents, or the legal system. As a result, many adolescents with problems related to their marijuana use are unlikely to receive effective interventions.
The Teen Marijuana Checkup (TMCU) was developed to reach marijuana using adolescents in schools who used marijuana frequently. School-based interventions reach a diverse population in terms of both sociodemographic variables and drug use and reduce barriers to accessing help. The TMCU avoids treatment terminology and offers the opportunity to discuss and get feedback on marijuana use, thus appealing to those who may have some concern about their use. In the TMCU, participants receive Motivational Enhancement Therapy (MET) that pairs motivational interviewing strategies with normative and other feedback surrounding marijuana use. The two-session MET intervention has consistently demonstrated the ability to attract heavy using teens (Berghuis, Swift, Roffman, Stephens, & Copeland, 2006; Walker, Roffman, Stephens, Wakana, & Berghuis, 2006;) and has shown efficacy in reducing marijuana use relative to delayed intervention and educational control conditions (Walker et al., 2011). The program was recently determined by the Washington State Institute for Public Policy to be a cost-effective “evidenced based” practice (Lemon, Pennucci, Hanley, & Aos, 2014).
Findings from the TMCU studies are consistent with reviews and meta-analyses of MET interventions for adolescent substance user in supporting the efficacy of this approach (Becker & Curry, 2008; Jensen et al., 2011; Macgowan & Engle, 2010). Yet, improved outcomes (e.g., days of marijuana use, substance disorder symptoms) often diminish over time, suggesting the need to bolster the longevity of the interventions’ effects. Walker and colleagues (2011) attempted to improve on outcomes of the brief MET intervention by offering Cognitive Behavioral Therapy (CBT) sessions. The CBT sessions were intended to attract and engage those participants most needing or desiring more help in making changes after the initial MET sessions. However, CBT participation was low in both the MET (12%) and education control (9%) conditions.
Some investigators have explored the repeated use of MET sessions following an initial intervention to augment the impact of substance abuse treatment by identifying and engaging those most in need of additional treatment. For instance, Dennis and colleagues (Dennis, Scott, & Funk, 2003; Scott, Dennis, & Foss, 2005) used Recovery Management Checkups (RMC) to encourage early re-engagement of post-discharge relapsers in adult outpatient and inpatient treatments. The RMC involved quarterly assessments of participant functioning. When the assessment revealed need for additional treatment, feedback and motivational interviewing were provided along with efforts to link the participant back into treatment. Results showed that RMC participants were significantly more likely to return to treatment, to return to treatment sooner and to spend more subsequent days in treatment. RMC participants were less likely to be deemed “in need” of treatment at the final 24 month follow-up. More recently, the concept of post-treatment MET check-ups was developed and tested with adults in treatment for marijuana dependence (Walker, Stephens, Towe, Banes, & Roffman, 2015). Although the effectiveness of the post-treatment checkups was mixed, results supported the further exploration of repeated check-ups as a means of extending and augmenting the impact of interventions.
The current study builds on findings from Walker and colleagues (2011) by adding repeated motivational check-ins to a base MET intervention. The additional motivational check-ins were scheduled in three-month intervals and designed to reinforce gains from the initial intervention and increase motivation for change in those still experiencing problems related to marijuana use. Optional CBT sessions were available to all participants who wanted additional help making changes in marijuana use. We expected these sessions to be utilized more often by those receiving motivational check-ins. The check-in sessions employed brief assessments of recent marijuana use and related consequences and MET techniques. A comparison condition received only the brief assessment at each check-in. We hypothesized that:
Repeated Motivational Check-In (MCI) sessions would lead to greater reductions in marijuana use and related consequences relative to Assessment-only Check-Ins (ACI).
The MCI condition would lead to greater utilization of additional CBT, particularly by those participants with more severe marijuana use.
Attendance of additional CBT would partially mediate the effect of the MCI condition on marijuana use and consequences.
Methods
Participants
Sample size was based on a priori power analyses using effect size estimates derived from the Walker et al., 2011 study of a brief MET-based intervention relative to an education control at the 3-month follow-up (partial eta-squared = .04). A target sample size of 250 provided at least 80% power for a growth modeling analysis to detect differences in change in marijuana use across follow-ups allowing for 10% attrition (Raudenbush, Liu, Spybrook, Martinez, & Congdon, 2006).
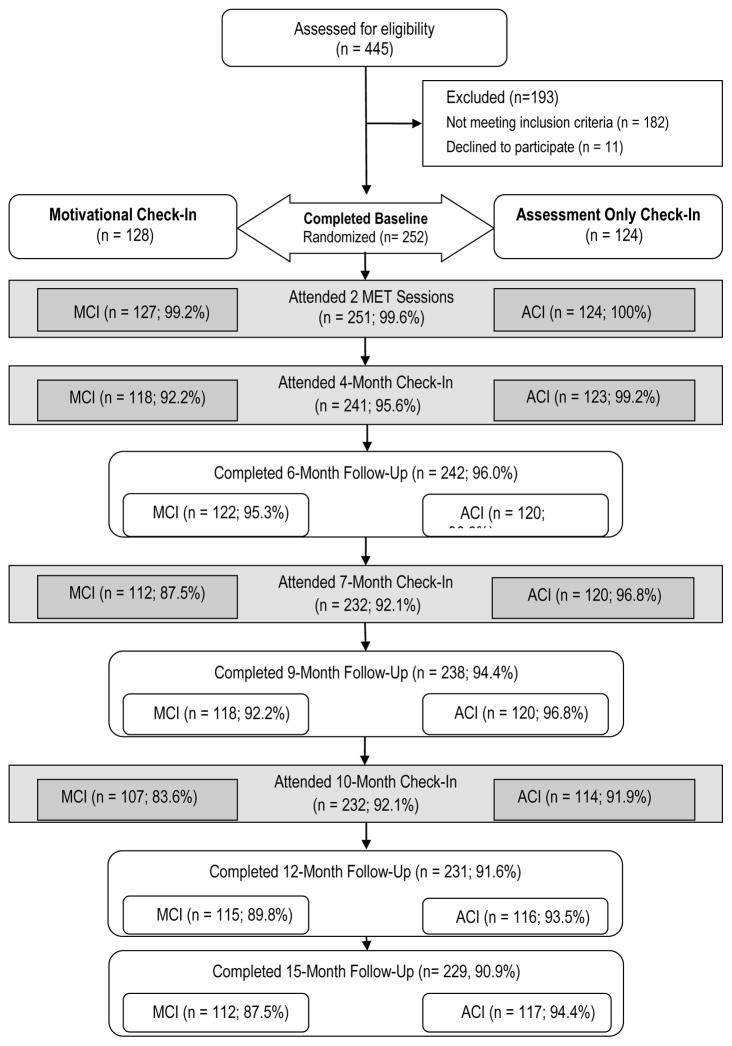
A total of 668 adolescents expressed interest and 445 were screened for eligibility (see Figure 1). Among the 445 participants screened, 193 individuals were ineligible or declined participation. Reasons for ineligibility included: fewer than 9 days of marijuana use in the past 30 days (n = 154; 79.8%), indications of a serious medical or psychiatric condition (n = 3; 1.6%), and lack of availability for participation throughout the course of the study either due to potential move outside of the region (n = 27; 14.0%) or pending graduation (n = 19; 9.8%). A total of 11 participants were eligible for the study but declined to participate (5.7%). The final sample who was eligible and agreed to participate was 252. Participants were primarily male (68%) and fairly racially diverse: Caucasian (59%), multiracial (20%), African-American (6%), Asian (4%), other (11%). Ten percent of the sample identified as Hispanic or Latino. The mean age was 15.84 (SD=0.96), and the mean age of marijuana initiation was 13.38 (SD=1.67). Participants reported a mean of 37.07 days of marijuana use in the previous 60 days (SD=15.05).
Figure 1.
Study Design and Participation Rates. MCI = Motivational Check-In, ACI = Assessment-only Check-In.
Design
Adolescent marijuana users were recruited from six high schools and randomly assigned to either the Motivational Check-In (MCI; n=128) or the Assessment-Only Check-In (ACI; n=124) condition after blocking on school, grade (freshman, sophomore, junior), and gender. Both conditions received the same initial two-session MET intervention conducted over a period of one to two weeks following baseline assessment. Subsequently, participants completed three in-person check-in sessions at 4, 7, and 10 months after baseline. At each check-in, participants in the MCI condition completed a computerized assessment of recent marijuana use and related consequences and then received a brief MET-based intervention. Participants in the ACI condition completed the same computerized assessment at the same time points but did not receive the MET intervention at the check-in sessions. Follow-up evaluations were conducted independently via internet-based assessments at 6, 9, 12, and 15 months after baseline. Participants in both conditions were able to attend optional CBT sessions as desired after the completion of the initial two MET sessions and up until their 12-month follow-up.
Procedures
All procedures were approved by the University of Washington and Virginia Tech Internal Review Boards (IRBs).
Recruitment
Participants were recruited from six schools in Seattle, Washington. Potential participants learned about the project via classroom based Marijuana Facts and Myths presentations, lunchtime information tables, staff referrals, brochures, and word of mouth. Study recruitment spanned over two academic years: 2011–2012 and 2012 – 2013. Study staff delivered a total of 106 classroom presentations and 64 lunch time presentations, reaching 4,084 students. The main recruitment sources were self-referral following exposure to lunchtime information tables (39.7%, n=211), classroom presentations (30.0%, n= 164), and friend referral (20.3%, n=111).
Potential participants were screened for eligibility by a Health Educator (HE) in individual sessions using a structured interview. Participants who were eligible and interested signed a form acknowledging informed assent. Parental consent was not sought or required by the IRB. The IRB agreed that requiring parental consent would dissuade many adolescents from participating and that the benefits of participation outweighed the potential for harm. Participants then completed a computerized baseline assessment in a private room at the school. No incentives were provided for completion of the baseline assessment. Following completion of the baseline assessment, participants were randomly assigned to condition and scheduled for a MET session with the same HE. In order to maintain rapport, participants and HEs were paired from baseline through final 10 month check-in for all intervention activities (i.e., initial MET sessions, check-ins, and any optional CBT sessions).
Initial MET sessions
Participants in both conditions received the two-session MET intervention developed and evaluated in previous trials (Walker, et al., 2006; Walker et al., 2011). The first MET session used motivational interviewing strategies including reflective listening, open questions and affirmations to develop rapport and understand how marijuana fit into the student’s life. Motivational Interviewing (MI) techniques were used to explore values and perceptions of the pros and cons of use. The second MET session included a review of a Personalized Feedback Report (PFR) based on the participant’s baseline assessment data. The PFR provided normative feedback about age-matched rates of use and displayed the participant’s self-reported risk factors for problematic use, including use before and during school, and abuse and dependence symptoms. In addition, the amounts of money spent on marijuana, marijuana’s impact on life goals, and marijuana’s relevance to relationships with people important to the participant were presented in order to help develop discrepancies between use and other meaningful aspirations. The second session ended with a summary of the student’s strengths and feedback regarding marijuana use. The HE offered a tailored description of how cutting back might be helpful in meeting life goals. Participants were told about the optional CBT sessions available throughout the next 11 months (until their 12-month follow-up assessment) and those interested in making changes were encouraged to use them or other community resources to support change efforts. Each session was approximately 50 minutes in length. No incentives were provided for completion of the initial MET sessions.
Check-ins
At the 4-, 7-, and 10-month anniversaries of the baseline assessment, HEs contacted participants to complete a check-in. Check-ins were conducted by HEs at the participant’s school in private rooms and participants received a $15 gift card for attending each check-in. In the ACI condition, participants completed a brief computerized assessment consisting of four questions about marijuana use and 17 items assessing the occurrence of cannabis use disorder symptoms during the past 60 days. Contact information was updated and a brief questionnaire about the check-in experience was completed. The HE did not review or discuss the information collected in the assessment with the participants. Participants were reminded of the availability of CBT sessions and of the on-line follow-up assessments that would be forthcoming. The ACI check-in sessions were approximately 15 minutes in duration.
In the MCI condition participants started each check-in by completing the same computerized assessment as completed in the ACI condition. They then participated in a MET session with the HE. The MET session included a review of a PFR that compared data from the brief assessment that was just completed with corresponding baseline information in order to highlight change (or the lack of it). Graphs and charts displayed frequency of marijuana use, dependence symptoms, and negative consequences at baseline and the current check-in. At each subsequent check-in, additional data from that assessment were added to the PFR so that by the final 10-month check-in data were displayed for baseline, 4-, 7-, and 10-month time points. The check-in PFR was designed to allow HEs to affirm reductions in marijuana use and related consequences or highlight discrepancies between stated goals and current behavior. Further, if participants reported any negative marijuana-related consequences, 15 or more days of use per month, any symptoms of cannabis abuse or dependence, or negative impact on life goals as a result of recent use, they were encouraged by the HE to reduce use. HEs were trained to provide this direction after asking the participant for permission to do so, consistent with an MI style. The HE and participant brainstormed the best ways for the participant to meet that goal, including use of the optional CBT sessions. The MCI condition check-ins ended with the participant completing a brief questionnaire about the check-in. The typical length of a check-in session in the MCI condition was 35 minutes.
Optional CBT
Individual CBT sessions were available to participants in both conditions following the second base MET session and until the 12-month follow-up assessment. Participants could schedule the CBT sessions as often as they wished and were reminded of their availability at each check-in session. CBT sessions were conducted by HEs. Participants, with HE guidance, could select from modules that were adapted from the Cannabis Youth Treatment Series (CYT; Center for Substance Abuse Treatment, 2000): All participants started with an orientation to CBT and goal setting module and subsequently could choose from modules on refusal skills, social support, other ways to have fun, dealing with unplanned situations, coping with slips, anger awareness, anger management, effective communication, coping with cravings, depression management, and managing thoughts about marijuana. Adaptations to the original CYT manual included: revising the treatment modules to be applicable for individual rather than group treatment and incorporating homework or real life practice exercises into sessions rather than having them as out-of-session assignments. Each session lasted approximately 45 minutes and started with participants selecting the module. Subsequently, the HE provided education and skill training as described in the manual for that module. Sessions typically ended with discussion of ways to incorporate the new skill into the participant’s life.
HE training and supervision
Four bachelor’s- and master’s-level clinicians served as HEs. All HEs were assigned to approximately equal number of participants in each condition. HE training included: 1) study of literature on current marijuana research, motivational interviewing (MI) theory and practice, human subject protection, and the study design; 2) attendance at a two-day intensive MI workshop led by the project PI and Clinical Director (CD); 3) practice of and feedback on audio-recorded mock sessions; 4) ongoing individual and group supervision of MI skills and intervention delivery. HEs met with actual participants only after role-played sessions scored consistently above minimum proficiency skill levels for at least 2 consecutive sessions according to the Motivational Interviewing Treatment Integrity (MITI) coding indices (Moyers & Martin, 2010).
All intervention sessions were audio recorded. To prevent drift the CD listened to a random selection of sessions and provided behavior counts and feedback during weekly group supervision meetings. Coding of 15% of the MCI check-in sessions (n = 57) and 7.5% of the ACI check-in sessions (n = 28) for MI adherence was conducted by two outside experts using the MITI coding system version 3.1.1 (Moyers & Martin, 2010). Interrater reliability estimates (ICCs) for global measures (e.g., MI Spirit, Empathy, etc.) were in the good to excellent range (.63 – .98) and over 95% of global ratings were coded within a 1 point difference between raters. MCI condition sessions were rated significantly higher than ACI condition sessions on measures of MI Spirit (including Evocation, Collaboration, Autonomy Support), Direction, and Empathy (p <.001 for each) and average scores on these scales in the MCI condition were at competency level. Clinician behavior count summary scores for the MITI behavioral indices on percent open questions and percent complex reflections also met competency, while reflection to question ratio was between beginning (1) and competency levels (2) (M = 1.65). The average MI adherent score of 97.8% indicated competency (beginning = 90%, competency = 100%). A HE was never required to pause from intervention activities due to non-adherence. These data indicate that the MET was delivered with a high degree of adherence and competence and that the treatment conditions differed in the expected directions.
Follow-ups
Internet-based follow-ups were scheduled for 6-, 9-, 12-, and 15-month anniversaries of the baseline assessment. Participants were sent prompts to complete the assessment by email and text messages that included an embedded link to the online assessment. Participants were free to complete these assessments from any location but were encouraged to choose a quiet setting and to be free of drug and alcohol intoxication when completing it. Participants were compensated for the follow-up assessments, which took on average 35 minutes to complete, with $25 gift cards. In addition, participants could earn a $40 bonus gift card if they completed all three check-ins, and the four follow-up assessments.
Measures
Marijuana use
Frequency of marijuana, alcohol, and other drug use were assessed with questions from the Global Appraisal of Individual Needs (GAIN; Dennis, 1998) presented by a computer. Participants reported the number of days out of the past 60 they used marijuana, alcohol, and other recreational drugs. Specifically, the questions asked “During the past 60 days, on how many days did you use marijuana?” with this same question asked about alcohol and other drugs. These measures have been reported to have good reliability and validity, and are comparable to other validated measures of frequency of use (Dennis, Funk, Godley, Godley, & Waldron, 2004). Number of days of marijuana use was the primary outcome measure. Number of days of alcohol use and a composite index of total days of other drug use were used in exploratory analyses.
Marijuana use disorder symptomatology
Symptoms of marijuana use disorder were assessed by 17 questions adapted from the GAIN’s 11 items to diagnose substance disorders (Dennis, 1998). The questions were adapted for ease of computerized administration and tailored to assess symptoms from marijuana use. For example, the GAIN question “you kept using alcohol or drugs even though you knew it was keeping you from meeting your responsibilities at work, school, or home” was separated into three questions (“you kept using marijuana even though you knew it was keeping you from meeting your responsibilities at school”, “you kept using marijuana even though you knew it was keeping you from meeting your responsibilities at home”, etc). The GAIN has been found to be a reliable and valid measure of abuse and dependence symptomatology (Dennis, White, Titus, & Unsicker, 2008). An index of marijuana use disorder symptomatology was created by summing the total number of symptoms endorsed. These symptoms were assessed at baseline, check-ins, and follow-ups. Alpha reliabilities ranged from .77–.92 across assessment points.
Marijuana problems
The Marijuana Problems Index (Johnson & White, 1995) is a 23-item measure adapted from the Rutgers Alcohol Problem Index (White & LaBouvie, 1989) that assesses for a variety of marijuana-related negative consequences. The MPI assesses the frequency of problems on a rating scale of 0 (never) to 4 (more than 10 times) as a result of marijuana use. The total MPI score for each participant was computed by adding the 23 item scores. Alpha reliability coefficients at baseline and follow-ups ranged from .86–.97.
Results
Preliminary analyses
There were no significant differences between conditions at baseline on sociodemographic variables, frequency of marijuana use, marijuana use disorder symptomatology, and marijuana-related problems. Follow-up rates were 96%, 94%, 92%, and 91% at the 6-, 9-, 12-, and 15-month follow-ups, respectively. Chi-square tests showed no evidence of significant differences in follow-up participation by condition (ps = .75, .17, .36, and .08, respectively; see Figure 1). Two-way ANOVAs (condition x attrition status) were conducted on baseline variables for each of the four follow-ups to detect differential attrition. No significant condition by attrition interaction effects were detected for any study variables. A significant main effect of 12-month attrition status was found for baseline marijuana use frequency such that those who did not complete the 12-month reported more frequent marijuana use than those who completed the follow-up. Given the high follow-up rates and the single instance of a difference by attrition status, missing data are not expected to bias results. The mixed model analyses employed are robust in handling missing data (Zaidman-Zait & Zumbo, 2013).
Intervention participation
Figure 1 shows that all but one participant attended both of the initial MET sessions. Eleven participants (4.4%) did not participate in the 4-month check-in, while 20 participants (7.9%) failed to attend the 7-month check-in, and 31 (12.3%) failed to attend the 10-month check-in. Chi-square analyses indicated that those in the ACI condition were significantly more likely to attend check-ins (p =.006, p = .005, and p = .033, respectively) than those in the MCI condition at each time point (4 months: 99% vs 92%; 7 months: 96.8% vs 88%; 10 months: 92 vs. 84%). Potential reasons for differential check-in attendance were explored by examining participants’ ratings of satisfaction with HEs and the helpfulness of various aspects of the check-ins on 5-point scales following each check-in. Overall, satisfaction and helpfulness ratings were very positive and did not change significantly across the three check-in sessions. There were no significant differences by condition on any scale with the exception that the ACI condition rated being reminded of optional CBT sessions as more helpful at the 4-month check-in (p=.01). A clinical chart review revealed that 9 of the 11 participants who did not attend the first check-in were not attending the school at that time, either due to a change of residence, suspension, or expulsion. All of these participants were in the MCI condition. Most of these same individuals were not available for subsequent check-ins. Additional non-attenders at the 7-month and 10-month check-ins also were largely related to students no longer attending school and these occurred disproportionately in the MCI condition as well.
A total of 65 participants (26%) attended optional CBT sessions. Participation was roughly equivalent across the ACI (n = 33; M = 4.3 sessions) and MCI (n = 32; M = 4.4 sessions) conditions and did not differ significantly. In order to investigate whether check-in sessions stimulated additional CBT participation, CBT initiation rates during the intervals between check-ins were compared. There were no difference between conditions in CBT participation prior to the first check-in at 4-months, nor following the 4-month check-in. Participants in the MCI condition were more likely to initiate CBT between the 7-month and 10-month check-ins compared to the ACI condition (p=.014), but a significant difference in CBT initiation was not found following the 10-month check-in. In general, participants who attended any CBT sessions were more likely to initiate marijuana use at a younger age (F=12.49; p<.01), endorse a higher number of problems at baseline (F=25.29; p<.01), report more symptoms of a marijuana use disorder at baseline (F=10.44; p<.01), and were more likely to endorse a racial/ethnic identity other than Caucasian (p=.006).
Primary Outcome Analyses
Mixed-effects model analyses for repeated measures were used to test for differences between conditions across assessment points for measures of days of marijuana use, marijuana problems, and marijuana use disorder symptoms in the past 60 days. Time was centered at baseline, with baseline time coded as 0 and subsequent follow-ups coded as the number of months from baseline. A series of unconditional growth models (no change, linear change, quadratic change, and cubic change) were used to determine the nature of individual-level change for each outcome. An unconditional growth model that included both linear and quadratic effects of time exhibited the best fit for all outcome measures. Subsequent conditional growth models examining differences in initial status and change by condition included both linear and quadratic representations of time. School was investigated as a moderator of treatment condition, but there were no significant interactions between condition and school; thus, school was not included in the final models.
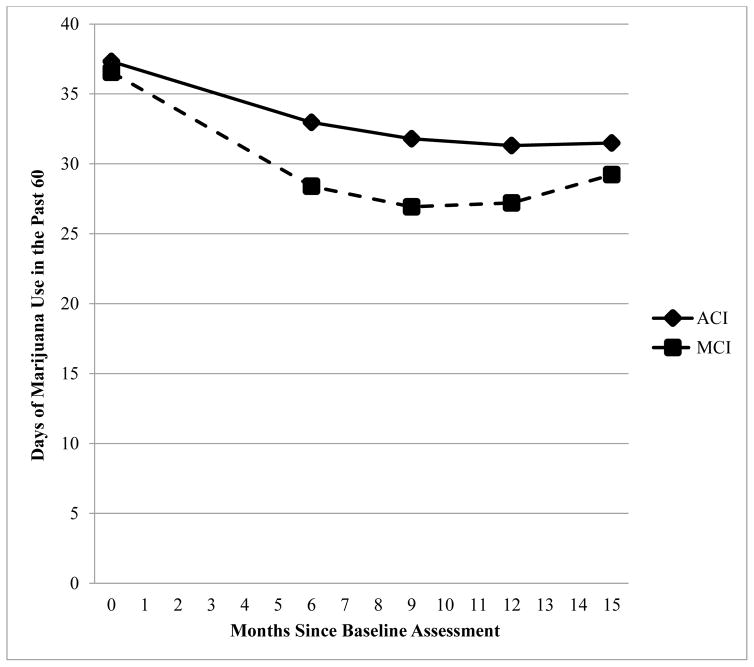
The final mixed effects models included individual change estimated as a random effect and mean change by condition estimated as a fixed effect. All individual-level outcome variables exhibited significant linear and quadratic change over time (days of use ƅlinear = −.95, p = .002, ƅquadratic = .03, p = .047; marijuana problems ƅlinear = −.05, p < .001, ƅquadratic = .002, p = .01; marijuana use disorder symptomatology ƅlinear = −.21, p < .001, ƅquadratic = .01, p = .004), with an initial decrease in the outcome variable, followed by a relatively smaller increase. Fixed effects comparing treatment conditions indicated differential change by condition for days of marijuana use, such that those in the MCI condition exhibited greater linear and quadratic change in days of use (ƅlinear = −.99, p = .02, ƅquadratic = .06, p = .03). MCI participants exhibited greater decreases in use initially, but steeper increases in use following this initial decrease (see Figure 2 and Table 1). Group-level effects did not show differential change by condition for marijuana problems or marijuana use disorder symptomatology (marijuana problems ƅlinear = −.01, p=.37, ƅquadratic = .000, p = .06; marijuana use disorder symptomatology ƅlinear = −.11, p = .08, ƅquadratic = .005, p = .21). Post-hoc analyses indicated significant differences between conditions only at the 6-month assessment: the MCI condition demonstrated fewer days of use (F = 6.12, p = .01) and fewer symptoms of use disorder (F = 6.78, p = .01) at 6-months. There were no significant differences between conditions for other follow-up time points.
Figure 2.
Mixed effects model estimates of days of marijuana use. MCI = Motivational Check-In, ACI = Assessment-only Check-In.
Table 1.
Marijuana Use, Use Disorder Symptoms, and Associated Problems at Baseline and Follow-up Assessments
| Baseline | 6 Months | 9 Months | 12 Months | 15 Months | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | ||
| Days of Use in the Past 60 Days | ACI | 37.35 | 15.01 | 32.66 | 19.91 | 31.80 | 20.58 | 31.09 | 21.26 | 31.51 | 21.33 |
| MCI | 36.80 | 15.16 | 26.64 | 20.25 | 28.35 | 22.12 | 26.94 | 22.75 | 29.33 | 23.09 | |
| Total | 37.07 | 15.06 | 29.62 | 20.27 | 30.09 | 21.38 | 29.01 | 22.07 | 30.45 | 22.19 | |
| Symptoms | ACI | 3.65 | 2.61 | 3.05 | 2.90 | 2.26 | 2.62 | 2.28 | 2.82 | 2.44 | 3.13 |
| MCI | 3.66 | 2.62 | 2.26 | 2.57 | 1.82 | 2.37 | 1.67 | 2.43 | 1.84 | 2.68 | |
| Total | 3.65 | 2.61 | 2.65 | 2.76 | 2.04 | 2.50 | 1.97 | 2.65 | 2.15 | 2.92 | |
| Problems | ACI | 1.63 | 0.46 | 1.49 | 0.69 | 1.34 | 0.62 | 1.31 | 0.68 | 1.37 | 0.80 |
| MCI | 1.59 | 0.44 | 1.33 | 0.55 | 1.22 | 0.58 | 1.21 | 0.75 | 1.24 | 0.81 | |
| Total | 1.61 | 0.45 | 1.41 | 0.62 | 1.28 | 0.60 | 1.26 | 0.71 | 1.31 | 0.81 | |
Exploratory Outcome Analyses
Given the significant difference in days of marijuana use and symptoms at the 6-month follow-up assessment, we examined the comparable data collected at the check-in sessions to help determine whether the effect was attributable to the 4-month check-in. Table 2 shows days of marijuana use and use disorders symptoms reported by participants at each check-in. A Condition (2) x Time (3) GLM performed on the days of use revealed no significant effects of condition (F = 0.93, p = .34), time (F = 0.55, p = .58), or their interaction (F = 0.72, p = .49). The GLM on the number of symptoms showed no significant effects of condition (F = 1.06, p = .30) or its interaction with time (F = 1.68, p = .48). A significant main effect of time (F = 11.78, p < .001) reflected reduced reports of symptoms at the 7- and 10- month check-ins relative to the 4-month check-in.
Table 2.
Marijuana Use and Use Disorder Symptoms Reported at Check-Ins
| 4 Month Check-In | 7 Month Check-In | 10 Month Check-In | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | M | SD | ||
| Days of Use in the Past 60 Days | ACI | 31.68 | 18.99 | 31.50 | 19.75 | 31.97 | 20.85 |
| MCI | 30.66 | 19.36 | 28.92 | 19.91 | 28.48 | 21.82 | |
| Symptoms | ACI | 3.11 | 2.30 | 2.60 | 2.32 | 2.59 | 2.60 |
| MCI | 2.91 | 2.39 | 2.41 | 2.42 | 2.10 | 2.47 | |
We also examined whether there was any effect on rates of alcohol use or drugs other than marijuana. At baseline, participants reported using alcohol on 7.41 (SD = 7.41) days and drugs other than marijuana on 1.81 (SD = 5.81) days out of the past 60 days. Analyses revealed no significant effects of condition, time, or their interaction across baseline and the four follow-up assessments (each p > .16).
Mediation by CBT
The lack of differences in CBT attendance by condition precluded formal examination of the hypothesis that CBT utilization would partially mediate the effect of the MCI intervention on outcomes. Instead, the relationships between CBT attendance and outcomes regardless of condition were explored. Partial correlations examined the relationship between total number of CBT sessions attended and outcomes at the 15-month follow-up, controlling for the corresponding baseline measure. Analyses revealed that CBT attendance was associated with a reduction in days of marijuana use, (r = −.16; p = .02) and marijuana related problems (r = −.13; p = .05), but did not significantly predict marijuana use disorder symptoms (r = −.07, p = .33).
Discussion
The current study adds to previous findings regarding a brief, in-school intervention for adolescent marijuana users that was both attractive and effective in reducing use and associated consequences. Participants in the study reduced their use of marijuana and reported fewer problems and symptoms related to marijuana use throughout the 15 month follow-up period. The addition of MET-based check-in sessions appeared to augment the effect of the initial intervention, but the effect dissipated at later assessment points. Contrary to hypothesis, attendance of optional CBT sessions was not systematically increased in the MCI condition but was related to greater severity of marijuana use and problems and predicted greater reductions in these marijuana use indices. The results suggest that a brief intervention may have enduring impact on marijuana use in an adolescent population of heavy users, but they raise questions about the incremental efficacy of adding additional motivational sessions.
Participants in both intervention conditions reduced marijuana use, associated problems, and use disorder symptoms and these reductions were sustained over a 15 month period. In the absence of a no treatment control condition it is impossible to attribute this effect to the intervention with certainty, but the findings from the previous trial with both a delayed intervention and an educational control group provide some confidence that the effect does not simply reflect regression to mean or natural reductions in use in a heavy-using adolescent population (Walker et al., 2011). In that trial, the base MET intervention showed clear and moderately strong differences (effect sizes .3 – .7) compared to a minimal assessment, no intervention control at a 3-month follow-up. Absolute reductions in use and negative consequences were of a magnitude comparable to those in the present trial. Significant differences between the MET condition and the educational condition were found only for days of marijuana use at a 6 month follow-up in that trial, suggesting somewhat greater initial efficacy for the MET approach that had dissipated at later follow-ups. The pattern of findings leaves open the question of whether assessment and education is as effective as the MET approach. The nearly perfect attendance for the initial two MET sessions in the present study is noteworthy in this context. In previous trials, participation in these initial sessions was incentivized in order to yield good attendance and provide a test of the intervention under ideal conditions. No such incentives were offered in the present study and yet attendance remained exceptionally high. These data support the attractiveness of offering an opportunity for assessment and feedback to adolescent marijuana users, most of whom would not otherwise seek treatment. It seems unlikely that simply offering education on marijuana would be as attractive.
The greater reduction of marijuana use and use disorder symptoms at the 6-month follow-up in the MCI condition indicated that the MET-based, 4-month check-in augmented the impact of the initial two MET session intervention. This interpretation is further bolstered by the lack of differences between conditions in the 4-month check-in data. That is, differences between conditions did not emerge until after the 4-month check-in. Notably, this effect occurred despite the ACI participants’ completion of the same brief assessment and similar reminders of the availability of additional treatment, thus ruling out additional assessment or HE contact as the explanation for differences.
The check-in sessions in the MCI condition were designed to help teens revisit their marijuana use and problem indicators starting three months after the initial feedback session. A unique feature of the check-in was the systematic comparison of current use and disorder indicators collected only moments before with data collected at baseline. These data, along with the participant’s reflection on interference with life goals, provided a context for HEs to use MI-techniques to elicit interest in further change when needed. They were also intended to provide HEs with the information needed to affirm those teens who had already made significant changes. Similar to the procedures used in RMCs (Dennis, Scott & Funk, 2003; Scott, Dennis, & Foss, 2005), HEs were trained to provide direct advice to participants to make changes when there were ongoing indicators of problematic marijuana use and they encouraged further treatment as one means to accomplish the change. The advice was presented in a manner consistent with MI and there was no evidence that it was off-putting given highly positive ratings of the check-in sessions that did not change over time.
Differences between conditions were expected to increase across the follow-up period as the MCI condition benefited from additional opportunities to review progress with the HE. We expected a cumulative effect of MET-based check-ins as additional participants were motivated to make changes and already successful changers were rewarded by reviewing the positive consequences of having reduced use. Instead, the initial benefit of the 4-month check-in appeared to dissipate gradually such that there were no statistically significant differences at later follow-ups. Data from the study provided no clues as to the reason for the diminished effects. Participants did not report differences in the helpfulness of the check-ins across time. It is possible that the novelty of the check-ins and sessions with HE’s wore off or were experienced as redundant. Individuals who had not changed by the 7-month check-in may have tired of reviewing the same data showing little change and started tuning out. It is also possible that those who were initially successful in reducing use did not see additional benefits and gradually increased use, thus erasing differences. It is also possible that the repeated assessments, both at check-ins and follow-ups, helped maintain reductions in both conditions. The potential for assessment reactivity during the follow-up period was relatively high due to the nature of the repeated check-ins and the number of follow-up assessments designed to identify change after each check-in (Clifford, Maisto, & Davis, 2007).
The MCI condition also did not lead to greater utilization of additional CBT sessions as hypothesized. CBT attendance overall was greater than in the previous trial (Walker et al., 2011) and was related to greater severity of marijuana use problems, but did not differ overall by condition. Exploratory analyses revealed a significant difference in new CBT initiators following the 7-month check-in, consistent with a cumulative effect of the check-ins, but this did not translate to greater CBT utilization overall or to significant differences in marijuana use and negative consequences at later follow-ups. CBT attendance was associated with greater change in marijuana use but the effect was relatively small. It is encouraging to note that 26% of a sample of “non-treatment seekers” chose to take part in CBT directed at assisting teens in quitting or reducing marijuana use and that those reporting more negative consequences of use were more inclined to participate. New research suggests that offering MET/CBT for substance abuse within school-based health centers is feasible, cost-effective and may be one method for encouraging treatment participation from ethnic minorities (Belur, Dennis, Ives, Vincent, & Muck, 2014). Notably, minority status was a significant predictor of CBT utilization in the current study, further suggesting that making treatment available in the schools may be particularly appealing to minority adolescents.
As noted earlier, one limitation of the present study was the absence of a “no treatment” or delayed feedback control condition. It remains possible that the change in marijuana use in the present study in both conditions at all follow-up assessments relative to baseline was not attributable to the interventions. However, given the findings from the previous trial (Walker et al., 2011), which showed that participation in two sessions of MET or education on marijuana produced greater change than a condition that received only minimal assessment, it may be unethical to withhold some type of immediate intervention. Future studies should create control conditions that determine the role that intensive assessment of marijuana use and related consequences plays in producing and maintaining change (see Walker et al., 2011 for a discussion). For instance, in the present study we carefully controlled the amount of assessment that occurred during the check-ins in order to be sure that the additional MI in the MCI condition accounted for the differences at the 6-month follow-up. However, the sheer amount of assessment in the present study could be partially responsible for the lack of differences seen at later follow-ups. Follow-up assessments taking 30–45 minutes conducted online were administered at 6, 9, 12 and 15-months. Additionally, brief (10 minute) computerized assessments were conducted at the time of the check-ins at 4, 7 and 10 months post-treatment. There is some evidence from the alcohol treatment outcome literature that lengthy (1.5 – 2 hour) and frequent in-person assessments can contribute to patient reactivity and add to the intervention effects (Clifford & Maisto, 2000; Clifford, Maisto, & Davis, 2007). Less is known about the effect of moderate levels of assessment (30–45 minutes) conducted on a computer as opposed to interviewer delivered. However, the frequency and length of these assessments may have contributed to clinical outcomes and studies that vary and control for the amount and timing of assessments are needed.
Another limitation was the reliance on self-reported marijuana use. Several factors led to the decision not to collect biological specimens to corroborate use. In order to minimize the amount of time students were taken out of classes, online follow-up assessments were employed so that participants could respond at other times of the day. Collecting biological specimens would have necessitated repeated in-person meetings and been a burden on students and teachers. In addition, the quantification of marijuana metabolites as a measure of quantity of recent marijuana use has modest validity due to the storage of THC in fat and variable excretion rates. In the absence of complete abstinence from marijuana for a significant period, biological assays are of limited utility. Self-reported drug use has been shown to be reliable and valid when anonymity or confidentiality are ensured as they were in the present study (Del Boca & Darkes, 2003). A third limitation was that incentives were offered for check-in attendance in order to foster good attendance for an initial test of the check-in approach. Thus, it is not clear whether the high participation rates for the check-ins would have occurred under more naturalistic conditions. Despite these limitations, there was evidence that MET-based check-ins may augment the impact of the initial intervention above and beyond any effects of repeated assessment. The limited duration of the effect was disappointing and suggests the need for further study of the approach to determine its cost-effectiveness relative to the two-session base intervention. In particular, research could investigate alternate timing of check-ins and different assessment and feedback formats to engage adolescents in further consideration of change. Given the prevalence of adolescent marijuana use and the hazards associated with heavy use in this age group, innovative methods for reaching the most at-risk users are needed.
Marijuana is the most widely used illicit substance with approximately 25 million people in the U.S. having used marijuana at least once in the past year. An estimated 10% of persons who have ever used marijuana will become daily users, with lifetime marijuana dependence rates estimated at 4% of the general population, the highest of any illicit drug. Given that the great majority of adults with one or more marijuana use disorder symptoms report they began smoking before age 18, early intervention efforts with adolescents, particularly those who are using heavily, becomes an important public health objective in order to prevent later problems.
Acknowledgments
This study was funded by the National Institute on Drug Abuse, grant #5 RO1 DA14296 awarded to CoPIs Denise Walker and Robert Stephens.
Contributor Information
Denise D. Walker, Email: ddwalker@u.washington.edu, Research Associate Professor, University of Washington, School of Social Work, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020, Phone: 206-543-7511, Fax: 206-685-8739
Robert S. Stephens, Email: stephens@vt.edu, Chair, Department of Psychology, Core Faculty, Clinical Science, Faculty/Consultant, Child Study Center, Director, Addictions Lab, Psychology Department, 109 Williams Hall, Blacksburg VA 24061, Virginia Polytechnic Institute and State University, Phone: 540-231-6304
Claire E. Blevins, Psychology Department, 109 Williams Hall, Blacksburg VA 24061, Virginia Polytechnic Institute and State University
Kelsey E. Banes, Psychology Department (0436), 109 Williams Hall, Blacksburg VA 24061, Virginia Polytechnic Institute and State University
Lauren Matthews, University of Washington, School of Social Work, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020.
Roger Roffman, University of Washington, School of Social Work, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020
References
- Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: a quality of evidence review. Journal of Consulting and Clinical Psychology. 2008;76(4):531–43. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Belur V, Dennis ML, Ives ML, Vincent R, Muck R. Feasibility and impact of implementing motivational enhancement therapy–cognitive behavioral therapy as a substance use treatment intervention in school-based settings. Advances in School Mental Health Promotion. 2014;7(2):88–104. doi: 10.1080/1754730X.2014.888223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berghuis J, Swift W, Roffman RA, Stephens RS, Copeland J. Cannabis Dependence: It’s Nature, Consequences and Treatment. United Kingdom: Cambridge University Press; 2006. The Teen Cannabis Check-Up: Exploring strategies for reaching young cannabis users; pp. 275–296. [Google Scholar]
- Center for Substance Abuse Treatment. Cannabis Youth Treatment Project 2000 [Google Scholar]
- Clifford PA, Maisto SA. Subject reactivity effects and alcohol treatment research. Journal of Studies on Alcohol. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: Part I. Alcohol use and related consequences. Journal of Studies on Alcohol and Drugs. 2007;68:519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98:1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Dennis M. Global Appraisal of Individual Needs (GAIN) manual: Administration, scoring and interpretation. Bloomington, IL: Lighthouse Publications; 1998. [Google Scholar]
- Dennis ML, Clark HW, Huang LN. Advances in School Mental Health Promotion. Taylor & Francis; 2014. Mar 5, The need and opportunity to expand substance use disorder treatment in school-based settings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction (Abingdon, England) 2004;99(Suppl 2):120–8. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, White M, Titus JC, Unsicker MS. Global Appraisal of Individual Needs: Administration Guide for the GAIN and Related Measures (Version 5) Bloomington, IL: 2008. [Google Scholar]
- Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26(3):339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2011;79(4):433–40. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- Johnson V, White HR. The relationship between work-specific and generalized stress and alcohol and marijuana use among recent entrants to the labor force. Journal of Drug Issues. 1995;25(2):237–251. [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- Lemon M, Pennucci A, Hanley S, Aos S. Preventing and treating youth marijuana use: An updated review of the evidence. Olympia: 2014. [Google Scholar]
- Macgowan MJ, Engle B. Evidence for optimism: Behavior therapies and motivational interviewing in adolescent substance abuse treatment. Child and Adolescent Psychiatric Clinics of North America. 2010;19(3):527–545. doi: 10.1016/j.chc.2010.03.006.Evidence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath J, Welham J, Scott J, Varghese D, Degenhardt L, Hayatbakhsh MR, … Najman JM. Association between cannabis use and psychosis-related outcomes using sibling pair analysis in a cohort of young adults. Archives of General Psychiatry. 2010;67(5):440–7. doi: 10.1001/archgenpsychiatry.2010.6. [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RSE, … Moffitt TE. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences. 2012 doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers T, Martin T. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1.1 (MITI 3.1.1) Vol. 1. University of New Mexico; 2010. pp. 1–29. [Google Scholar]
- National Institute on Drug Abuse. Marijuana: Research Report Series. Bethesda, MD: 2014. [Google Scholar]
- Raudenbush SW, Liu X-F, Spybrook J, Martinez A, Congdon R. Optimal Design software for multi-level and longitudinal research (Version 1.77) [Computer software] 2006 Available at http://sitemaker.umich.edu/group-based.
- Scott CK, Dennis ML, Foss Ma. Utilizing Recovery Management Checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug and Alcohol Dependence. 2005;78(3):325–38. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson Ca, Hutchinson DM, … Mattick RP. Young adult sequelae of adolescent cannabis use: an integrative analysis. The Lancet Psychiatry. 2014;1(4):286–293. doi: 10.1016/S2215-0366(14)70307-4. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral healthtTrends in the United States: Results from the 2014 National Survey on Drug Use and Health. 2015 (HHS Publication No. SMA 15-4927, NSDUH Series H-50). Retrieved from http://www.samhsa.gov/data/
- United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set -- Admissions (TEDS-A), 2010. Inter-university Consortium for Political and Social Research (ICPSR); 2014. [DOI] [Google Scholar]
- Walker DD, Roffman RA, Stephens RS, Wakana K, Berghuis J. Motivational Enhancement Therapy for adolescent marijuana users: A preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens R, Roffman R, DeMarce J, Lozano B, Towe S, Berg B. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: A further test of the teen marijuana checkup. Psychology of Addictive Behaviors. 2011;25(3):474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens RS, Towe SL, Banes KE, Roffman RA. Maintenance check-ups following treatment for marijuana dependence. Journal of Substance Abuse Treatment. 2015;56:11–15. doi: 10.1016/j.jsat.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington State Department of Health and Office of the Superintendent of Public Instruction. Washington State Healthy Youth Survey 2012 Analytic Report. 2014. [Google Scholar]
- White HR, LaBouvie EW. Towards the assessment of alcohol problem drinking. Journal of Studies on Alcohol. 1989;50(1):30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Zaidman-Zait A, Zumbo B. Can multilevel (HLM) models of change over time adequately handle missing data? The Journal of Educational Research & Policy Studies. 2013;13(1):18–31. [Google Scholar]