Sleeping sickness, or human African trypanosomiasis (HAT), epitomises the concept of a “neglected tropical disease” [1]. The history of HAT reads like a Hollywood parody of Homeric pestilence. Both the chronic and acute forms of HAT are exclusively confined to sub-Saharan Africa, where they affect the poorest of the rural poor—thriving in weak health systems and conflict zones—and where they have been responsible for massive historic epidemics [2]. Both forms of the disease are invariably fatal if not treated, but available therapies are difficult to administer, highly toxic, and increasingly pose problems of drug resistance [3]. Diagnostics are complex, and the procedures needed to sanction the more toxic treatments are difficult, painful, and dangerous, resulting in massive underreporting [4, 5]. The cunning ability of the causative parasites to evade the immune system has made a mockery of attempts to develop vaccines, and any continued protestations of a vaccine breakthrough on a meaningful timescale are, at best, wishful thinking [6]. Finally, the hope of control through targeting the disease vector, the tsetse fly, has (for the most part) eluded cost-effective, sustainable, large-scale delivery [7].
In the face of such challenges, the talk of effective disease control—elimination even—may at best be thought misplaced optimism and at worst detracting limited resources from a focus on further research to develop better tools for the future. However, disease elimination is a stated aim of the World Health Organization, and the moral imperative must be to deploy control tools to save lives now [8]. Successes arising from a small number of well-run programmes give confidence that even with existing tools, as limited as they may be, effective control—and in some areas elimination—is a realistic target [9]. The main challenge to realising these benefits is securing the necessary financing to enable appropriately designed interventions to be sustainably delivered at scale immediately [10].
HAT is caused by infection with one of two closely related but geographically discrete parasites that results in a progressive systemic disease followed by central nervous system damage and death. In Central and West Africa, disease progression resulting from Trypanosoma brucei gambiense infection is slow, occurring over many years. By contrast, in East Africa, T. b. rhodesiense infections progress rapidly, resulting in death within months of infection. While the total burden of disease is significantly greater for T. b. gambiense than T.b. rhodesiense HAT, where the latter occurs, local disease burden is much higher than might be expected from its relative incidence [11].
A major difference between the epidemiology of the two parasites is the importance of nonhuman animal hosts in the maintenance and spread of infection. As a good working approximation, T. b. rhodesiense is an infection of animals that occasionally spills over to humans [12], while T. b. gambiense is a human infection that occasionally resides in animals [13]. Through understanding this epidemiology, it is now possible to tailor existing tools to maximize benefit and deliver effective control.
This is what has been successfully done for controlling T. b. rhodesiense in Southeast and Central Uganda, where livestock (in particular, cattle) have been shown to be of central importance in the spread of sleeping sickness [14, 15]. Interventions targeted at controlling T. b. rhodesiense infections in livestock—mass administration of veterinary trypanocidal drugs followed up by the routine application of insecticides to protect cattle from tsetse flies—have been modelled [16, 17] and implemented across large areas of the endemic focus in Uganda following a resurgence of the disease in the early 2000s [18, 19].
These interventions deliver a double benefit. Firstly, they protect the human population from sleeping sickness and in so doing shift public health efforts to disease prevention rather than case finding and treatment. Secondly, they improve livestock health and productivity, as nonhuman infectious trypanosomes are a major veterinary health burden in sub-Saharan Africa that significantly affects the productivity of oxen and milking cows and hence rural livelihoods [20]. The societal impacts unlocked by delivering these interventions across the wider endemic areas of East Africa are potentially very large. The economic value that farmers place on their cattle provides a compelling private incentive to participate in disease control activities; indeed, it also opens up the potential to develop models for economic sustainability—overcoming the failures seen with tsetse control using traps—to incentivise and mobilise communities over the long term [21].
Ground-breaking work supported by long-term funding from the United Kingdom Department for International Development (DFID) has been undertaken in Uganda over the last two decades [14, 15, 16, 17, 18, 19]. The continued expansion of the area in Uganda affected by T. b. rhodesiense, threatening the integrity of the HAT focus for T. b. gambiense and risking overlap of the two forms of HAT, is a strong incentive for action [22]. The public–private alliance Stamp Out Sleeping sickness, (http://www.stampoutsleepingsickness.com/) delivered highly cost-effective control through mass cattle treatments and the development of innovative veterinary drug delivery networks. This prevented the spread of zoonotic HAT and has recently been named in the top 20 examples of UK further education institutions benefiting global development, selected from over 7,000 case studies (see: http://www.ukcds.org.uk/the-global-impact-of-uk-research/battling-sleeping-sickness). The WHO aims to eliminate sleeping sickness in Africa by 2030 [23]. The priority now is to scale these validated interventions and attract funding to allow sustained deployment across the entire region affected by HAT in Uganda.
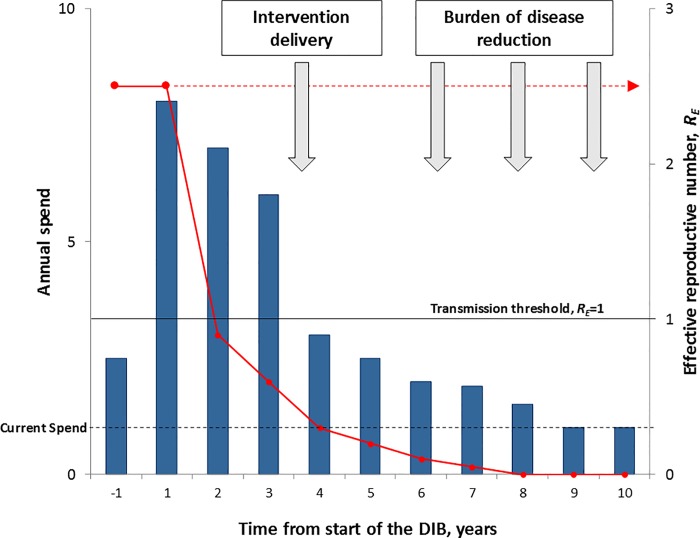
To achieve this vision, DFID has funded research to explore a novel “impact investment” approach that could raise the necessary financing for sustained, scaled HAT control. The approach will build on, and benefit from, the success of GAVI-International Finance Facility for Immunisation (IFFIm) bonds and other social impact bond initiatives, whereby long-term public and/or donor commitments to support proven interventions are used to leverage upfront private sector investment. This financing approach, known as a Development Impact Bond (DIB), uses “private investment to provide upfront risk capital for development programmes, only calling on donor funding to repay capital, plus a potential return, once clearly defined and measured development outcomes are achieved” [24]. The ideal cash flow profile of the DIB (front-loaded investment followed by long-term lower cash needs) mirrors the high upfront effort needed to interrupt transmission followed by the reduced effort needed to maintain disease control. In poor countries, the money is rarely available to cover these upfront costs, and traditional donor grant funding does not advance large amounts of cash; in the DIB, private investors provide the capital needed upfront, at risk (see Fig 1).
Fig 1. DIB cash flow and infectious disease control.
The graph shows a stylised DIB cash flow profile (annual spend) and the impact on disease transmission (effective reproductive number, RE). Before the DIB is implemented, the current spend on control (broken black line) is inadequate to interrupt transmission (RE>1) and shows that in the absence of the additional financing, the disease would persist in an endemic state (broken red line). The DIB financing is shown by the blue bars and can be broken down into four phases. Preimplementation Phase (Y–1): detailed design; establishment of surveillance systems; baseline surveys; piloting reporting systems; strengthening of the policy framework. Suppression Phase (Y1–3): rollout of mass intervention campaigns; flexible, reactive management to achieve critical coverage and to interrupt transmission (RE<1); routine reporting; audit of intervention coverage. Consolidation Phase (Y4–8): shift from mass intervention to surveillance and reactive interventions; protection against reintroduction of the disease. Postcontrol Maintenance Phase (Y9–10): Capacity embedded in local system and ideally fully financed locally. The “front loaded” cash flow profile, which is characteristic of DIB financing, is ideally suited to infectious disease control and stands in contrast to the traditional flat year-on-year funding. Potential payment triggers for partial repayment of capital linked to intervention coverage and full capital repayments plus interest based on disease reduction are also shown (grey arrows).
Alongside the cash flow profile, the transfer of risk of programme failure from the donors to social investors is central to improving the likelihood of DIB financing over direct funding; DIBs could bring a greater focus on implementation and delivery of successful results. If the intervention does not work, the investors lose out. But if it succeeds, international donors repay the social investors with interest (at a rate below the market rate). In this way, DIBs can bring greater rigour to delivery of international development and global health interventions—investors will only back strategies that have evidence of success. The new instrument could promote greater scrutiny and operational flexibility to address the realities on the ground in running the campaign. Under the theoretical scenario outlined in Fig 1, the long-term maintenance of the disease-free state is embedded in local systems and ideally fully financed locally and affordable within the available budget deployed prior to control. The reality of this long-term sustainability is amongst many things that still need to be tested by the deployment of an actual DIB targeted against an NTD.
If a DIB for sleeping sickness can be developed and used to underpin successful disease control in Uganda, the financing approach could be extended to the other East African nations as well as the larger problem of T. b. gambiense sleeping sickness in Central and West Africa [13]. Of course, the systems developed through DIB financing to deliver existing interventions can be adapted to deliver improved control technologies (e.g., new therapeutics [25]) as the evidence base justifies their adoption. However, the broader applicability of DIBs could extend to the majority of the neglected tropical diseases, where imperfect but adequate disease control tools already exist.
Rabies is a prime example. The proposed interventions for zoonotic sleeping sickness control in Uganda share many properties of vaccination campaigns: the need for sensitisation of communities; the use of existing public health infrastructure capacity to allow routine delivery of proven interventions at scale; direct benefit(s) seen for the recipients of treatment; nonlinear benefits unlocked through increased coverage; a focus on prevention rather than reactive treatment; and highly cost-effective interventions and societal level benefits unlocked from deployment at scale, achieved without having to wait for the vaccine to be developed. However, we do have vaccines for rabies control—and have had for over 130 years! At the end of 2015, the WHO and the World Organization for Animal Health, in collaboration with the UN Food and Agriculture Organization and the Global Alliance for the Control of Rabies (GARC), launched a global framework to eliminate rabies by 2030 [26]. This is supported by the End Rabies Campaign launched by GARC in 2016 at the House of Lords in London, UK.
As with sleeping sickness, the constraints to rabies control are not technical but are rather the need for public engagement and the mobilization of the necessary financial resources to support effective operational delivery. The use of DIBs to achieve this, focused on mass vaccination of the domestic dog reservoir combined with the provision of postexposure therapy, is currently being explored.
Let us not retreat behind the promise of future success from continued research [10]; for many of the world’s neglected tropical diseases we already have the evidence and the infrastructure and, with DIBs, a potential financing model [27] for their elimination. With the new Global Goals for Sustainable Development in place, now is surely the time for action.
Funding Statement
We thank the UK Department for International Development (DFID) for supporting this work through the Research and Evidence Division (SW, KB, PC). We thank UBS Optimus (PC) and Research into Results/The University of Edinburgh for funding work on DIBs for the control of rabies (SW, PC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hotez PJ, Fenwick A, Savioli L, Molyneux DH. Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009;373: 1570–1575. 10.1016/S0140-6736(09)60233-6 [DOI] [PubMed] [Google Scholar]
- 2.Maudlin I. African trypanosomiasis. Ann Trop Med Parasitol. 2006;100: 679–701. 10.1179/136485906X112211 [DOI] [PubMed] [Google Scholar]
- 3.Brun R, Blum J, Chappuis F, Burri C. Human African trypanosomiasis. Lancet. 2010;375: 148–159. 10.1016/S0140-6736(09)60829-1 [DOI] [PubMed] [Google Scholar]
- 4.Odiit M, Coleman P, Liu WC, McDermott JJ, Fèvre EM, Welburn SC, Woolhouse M. Quantifying the level of under-detection of Trypanosoma brucei rhodesiense sleeping sickness cases. Trop Med Int Health. 2005;10: 840–849. 10.1111/j.1365-3156.2005.01470.x [DOI] [PubMed] [Google Scholar]
- 5.Acup C, Picozzi K, Waiswa C, Welburn SC. Factors Influencing Passive Surveillance for zoonotic T. b. rhodesiense Human African Trypanosomiasis in Uganda. Acta Tropica. 2016; [DOI] [PubMed] [Google Scholar]
- 6.La Greca F, Magez S. Vaccination against trypanosomiasis: Can it be done or is the trypanosome truly the ultimate immune destroyer and escape artist? Hum Vaccines. 2011;11: 1225–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw AP, Wint GR, Cecchi G, Torr SJ, Mattioli RC, Robinson TP. Mapping the benefit-cost ratios of interventions against bovine trypanosomosis in Eastern Africa. Preventive Veterinary Medicine. 2015;122(4): 406–416. 10.1016/j.prevetmed.2015.06.013 [DOI] [PubMed] [Google Scholar]
- 8.Holmes P. On the Road to Elimination of Rhodesiense Human African Trypanosomiasis: First WHO Meeting of Stakeholders. PloS Negl Trop Dis. 2015;9(4): e0003571 10.1371/journal.pntd.0003571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simarro PP, Jannin J, Cattand P. Eliminating human African trypanosomiasis: where do we stand and what comes next? PLoS Med. 2008;5: e55 10.1371/journal.pmed.0050055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molyneux D, Ndung'u J, Maudlin I. Controlling sleeping sickness—"when will they ever learn?". PLoS Negl Trop Dis. 2010; 4:e609 10.1371/journal.pntd.0000609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fèvre EM, Odiit M, Coleman PG, Woolhouse ME, Welburn SC. Estimating the burden of rhodesiense sleeping sickness during an outbreak in Serere, eastern Uganda. BMC Public Health. 2008;8: 96 10.1186/1471-2458-8-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welburn SC, Coleman PG, Fevre E, Maudlin I. Sleeping sickness–a tale of two diseases. Trends Parasitol. 2001;17: 19–24. [DOI] [PubMed] [Google Scholar]
- 13.Welburn SC, Maudlin I, Molyneux D. Beyond Tsetse—Implications for Research and Control of Human African Trypanosomiasis. Trends Parasitol. 2016;32(3) [DOI] [PubMed] [Google Scholar]
- 14.Fèvre EM, Coleman PG, Odiit M, Magona JW, Welburn SC, Woolhouse ME. The origins of a new Trypanosoma brucei rhodesiense sleeping sickness outbreak in eastern Uganda. Lancet. 2001;358: 625–628. [DOI] [PubMed] [Google Scholar]
- 15.Welburn SC, Picozzi K, Fevre EM, Coleman PG, Odiit M, Carrington M, Maudlin I. Identification of human infective trypanosomes in animal reservoir of sleeping sickness in Uganda by means of serum-resistance-associated (SRA) gene. Lancet. 2001;358: 2017–19. [DOI] [PubMed] [Google Scholar]
- 16.Welburn SC, Fèvre EM, Coleman PG, Odiit M, Maudlin I. Crisis, what crisis? Control of Rhodesian sleeping sickness. Trends Parasitol. 2006;22: 123–128. 10.1016/j.pt.2006.01.011 [DOI] [PubMed] [Google Scholar]
- 17.Kajunguri D, Hargrove JW, Ouifki R, Mugisha JYT, Coleman PG, Welburn SC. Modelling the use of insecticide-treated cattle to control tsetse and Trypanosoma brucei rhodesiense in a multi-host population. Bulletin of Mathematical Biology. 2014;76(3): 673–696. 10.1007/s11538-014-9938-6 [DOI] [PubMed] [Google Scholar]
- 18.Fyfe J, Picozzi K, Bardosh K, Waiswa C, Welburn SC. Impact of mass chemotherapy in domestic livestock to control zoonotic T.b. rhodesiense. Acta Tropica. 2016; [DOI] [PubMed] [Google Scholar]
- 19.Welburn SC, Coleman P. 2015. Human and Animal African Trypanosomiasis In: Zinsstag J, Schelling E, Waltner-Toews D, Whittaker M, Tanner M, editors. One Health: The Theory and Practice of Integrated Health Approaches. CABI International; 2015. pp. 201–221. [Google Scholar]
- 20.Okello WO, Muhanguzi D, MacLeod ET, Welburn SC, Waiswa C, Shaw AP. Contribution of draft cattle to rural livelihoods in a district of southeastern Uganda endemic for bovine parasitic diseases: an economic evaluation. Parasit Vectors. 2015; 8(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bardosh K, Waiswa C, Welburn SC. Conflict of interest: use of pyrethroids and amidines against tsetse and ticks in zoonotic sleeping sickness endemic areas of Uganda. Parasit Vectors. 2013;6: 204 10.1186/1756-3305-6-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Picozzi K, Fevre EM, Odiit M, Carrington M, Eisler MC, Maudlin I, Welburn SC. Sleeping sickness in Uganda: a thin line between two fatal diseases. British Medical Journal, 2005;331(7527): 1238–41 10.1136/bmj.331.7527.1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simarro PP, Cecchi G, Franco JR, Paone M, Diarra A, Priotto G, Mattioli RC, Jannin JG. Monitoring the progress towards the elimination of Gambiense human African trypanosomiasis. PLoS Negl Trop Dis. 2015; 9(6): e0003785 10.1371/journal.pntd.0003785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centre for International Development and Social Finance. Case Study 1: Reduction of Rhodesian sleeping sickness in Uganda. 2013. Available: http://www.socialfinance.org.uk/resources/socoal-finance/dib-workinggroup-report-consultation-dr
- 25.Singh Grewal A, Pandita D, Bhardwaj S, Lather V. Recent Updates on Development of Drug Molecules for Human African Trypanosomiasis. Current Topics in Medicinal Chemistry. 2016;16(20): 2245–65. [DOI] [PubMed] [Google Scholar]
- 26.Editorial Lancet. Time to eliminate rabies. Lancet. 2015;386 (10012): 2446. [DOI] [PubMed] [Google Scholar]
- 27.DfID. UK development bonds will combat global poverty. 2014. Available: https://www.gov.uk/government/news/uk-development-bonds-will-combat-global-poverty.