Abstract
Purpose
The purpose of this study was to establish a normal reference database for fixation stability measured with the bivariate contour ellipse area (BCEA) in the Macular Integrity Assessment (MAIA) microperimeter.
Methods
Subjects were 358 healthy volunteers who had the MAIA examination. Fixation stability was assessed using two BCEA fixation indices (63% and 95% proportional values) and the percentage of fixation points within 1° and 2° from the fovea (P1 and P2). Statistical analysis was performed with linear regression and Pearson's product moment correlation coefficient.
Results
Average areas of 0.80 deg2 (min = 0.03, max = 3.90, SD = 0.68) for the index BCEA@63% and 2.40 deg2 (min = 0.20, max = 11.70, SD = 2.04) for the index BCEA@95% were found. The average values of P1 and P2 were 95% (min = 76, max = 100, SD = 5.31) and 99% (min = 91, max = 100, SD = 1.42), respectively. The Pearson's product moment test showed an almost perfect correlation index, r = 0.999, between BCEA@63% and BCEA@95%. Index P1 showed a very strong correlation with BCEA@63%, r = −0.924, as well as with BCEA@95%, r = −0.925. Index P2 demonstrated a slightly lower correlation with both BCEA@63% and BCEA@95%, r = −0.874 and −0.875, respectively.
Conclusions
The single parameter of the BCEA@95% may be taken as accurately reporting fixation stability and serves as a reference database of normal subjects with a cutoff area of 2.40 ± 2.04 deg2 in MAIA microperimeter.
Translational Relevance
Fixation stability can be measured with different indices. This study originates reference fixation values for the MAIA using a single fixation index.
Keywords: microperimetry, BCEA, fixation, normal
Introduction
Microperimetry (MP) assesses sensitivity of different spatial locations of the retina. It is similar to standard automated perimetry (SAP), with the advantage of correlating retinal sensitivity with retinal morphology through the addition of fundus imaging, allowing precise topographic correlations of macular anatomy to light sensitivity. The main technological advantage is the incorporation of a retinal landmark tracker, which corrects eye movements during examination, and the inclusion of fixation pattern metrics to indicate the preferred retinal locus (PRL) that patients use to perform fixation tasks.
There has been recent interest in MP as a noninvasive tool for evaluating macular diseases.1–12 Furthermore, the analysis of the location and quality of fixation loci has been of particular importance to different authors because of its relevance to reading abilities in patients with central vision loss.
Microperimetry allows an automated analysis of macular function even with unstable fixation, as in the case of central geographic atrophy secondary to dry age-related macular degeneration (AMD).13 Such assessments are independent of the quality of fixation and eye movements. This is possible due to the accurate test-retest of the same retinal point, which is monitored and the projection controlled by eye-tracking technology.6–8 Additionally, fixation locations may be mapped across the retina in order to characterize, evaluate, and compare sequential data in cases where the PRL may vary over time.14
Microperimetry delivers information in the form of retinal threshold sensitivity (TS) and fixation stability (FS). Threshold sensitivity is based on subjective tests similar to SAP. Patients are expected to respond when stimuli of different intensities are projected at known locations within specified retinal areas. Fixation stability is an objective test performed by means of retinal landmark tracking, which samples eye movements at 25 times per second and subsequently plots the scatter of a cloud of fixation points (CFP) over a retinal image reference map. The resulting scatter pattern can then be mathematically analyzed.
With respect to fixation stability, MP systems currently use two different approaches. The first FS measurement method calculates the percentage of fixation points (PFP) falling inside a circle of 1° and 2° radii (defined in the MAIA MP as P1 and P2, respectively) centered in the barycenter of the CFP.15 The main advantage of this method is the clinical classification of FS as suggested by Fuji et al.,16 where eyes with P1 greater than 75% are classified as having stable fixation. If P1 is less than 75% and P2 is more than 75%, fixation is classified as relatively unstable. If both P1 and P2 are less than 75%, the pattern is described as unstable fixation.16 This methodology has been criticized in the literature due to the arbitrarily selected distance of 1° and 2° used to establish such stability index. The second FS measurement method suggested by Crossland et al.,17 is known as the bivariate contour ellipse area (BCEA). It calculates the area and orientation of an ellipse encompassing a given proportion (ρ) of the fixation points' dataset. This is a two-dimensional elliptical representation that describes the limits of the retinal surface area used during a fixation attempt where lower BCEA values define better fixation stability.17–19 The advantage of the BCEA calculation over the PFP is that it is based on a mathematical model used in statistics to describe movement of variables; however, it is not related to any clinical classification in MP.
The common formula used to calculate BCEA is:20
 |
where BCEA is the bivariate contour ellipse area, σH is the standard deviation of point location over the horizontal meridian, σV the standard deviation of point location over the vertical meridian, and ρ the product moment correlation of these two position components. The value k defines the limit for the ellipse and is dependent upon the probability area chosen given by:
 |
where e is the base of the natural logarithm, from where,
 |
This method assumes that fixation points are normally distributed. Different authors have used different probability (P) values,19 such as 0.63,20,21 0.68,17–19 or 0.95.22 The clinical and statistical significance of such P values have never been reported for MAIA MP.
The Macular Integrity Assessment system (MAIA; CenterVue S.p.A., Padova, Italy), is a novel MP device that was introduced into clinical practice several years ago. It reports two BCEAs with proportional values of 63% and 95% converted into degree units. Reference databases of macular sensitivity values have been reported, allowing the correlation of location-specific data from the average threshold sensitivity in normal eyes to those data acquired from eyes with different stages of AMD.5,9,23 The purpose of this study is to establish a reference database for FS measured with the BCEA metric in a group of normal subjects tested with the MAIA microperimeter. It does not directly compare the MAIA BCEA values with other technologies.
Methods
Participants
This was a multisite, cross-sectional, observational, prospective study that included normal healthy subjects without signs of ocular pathology, aged 19 to 86 years old, from June 2012 to June 2016. The clinical study sites involved were located at Nottingham (UK); Crete (Greece); Slidell, Louisiana (USA); and Milan (Italy). A total of 358 participants with normal visual acuity or corrected to normal (20/20 or better), mean spherical equivalent refractive error of −3.06 ± 1.36 (range, −9.50, 5.28), and with no history of any visual abnormalities were tested for FS and macular light stimuli sensitivity using the MAIA MP device. The MAIA automatically corrects for refraction errors in the spherical equivalent of −15 to +10 diopters; therefore such range was part of the inclusion criteria. Only one eye of each patient was tested for inclusion within the reference database. The eye with the better visual acuity was selected, and the right eye was chosen if visual acuity was identical in both eyes. Thirty-one patients were excluded from the analysis due to their low reliability index in the MAIA testing, established by CenterVue as a fixation loss value indicated by the percentage of stimuli reported as seen when a stimulus is projected onto the optic nerve head (blind spot). Microperimetry, through the retinal-landmark tracker, compensates for eye movements in the location of stimuli projection, hence gaze deviation will not interfere while testing the blind spot. In essence, the fixation loss value is a validation measure of the test subject's compliance with reporting only those stimuli that are potentially visible. The test is considered reliable when such index is above 70% (MAIA Operator's Manual). A total of 326 eyes were included in the analysis after the exclusions.
Patient examination data was anonymized prior to inclusion within the database in order to protect patient privacy. Written informed consent was obtained from all participants, and local bioethics board approval was obtained as required for all sites involved in the study. The study was performed in accordance with the tenets of the Declaration of Helsinki.
Equipment and Procedures
A fully automated MAIA examination was performed to assess TS and FS using the MAIA standard macular grid pattern (37 stimuli points) over 10 retinal degrees (±5° around the macula). In the first 10 seconds of the examination, the MAIA microperimeter performs a fixation test in which a central point of reference of the average retinal position is calculated and labeled as PRL_initial (PRLi); subsequently, the projection of the preselected stimuli grid map begins with the grid centered on such PRLi. On completion of the test, the center of the mass (barycenter) of the total fixation points is calculated and defined as PRL_final (PRLf),15 which corresponds to the foveal area in normal subjects. The projection strategy was the standard 4-2, and the examination was performed without dilation in a darkened room (mesopic conditions). Patients were instructed to stare at the center of the fixation target during the examination. The fixation target consists of a 1° diameter red circle with light intensity of 10 ± 3 apostilb (asb).
The MAIA can project stimuli targets with a maximum luminance of 1000 asb and with a stimulus dynamic range of 36 decibels (dB). The MAIA microperimeter utilizes a scanning laser ophthalmoscope (SLO) technology to image the retina to a field of 36°; it has an automatic compensation of refractive error between −15 and +10 diopters (D). The automated retinal eye-tracking system samples and corrects for eye movements at 25 Hz with respect to the positioning of stimulus targets. The fixation location is calculated from the eye-tracking output and plotted 25 times per second as a CFP describing the fixation pattern overlaid onto a reference SLO retinal image acquired at the start of the test. The average examination time is 5 minutes, 50 seconds; therefore, the CFP may contain more than 8700 points (Fig. 1).
Figure 1.
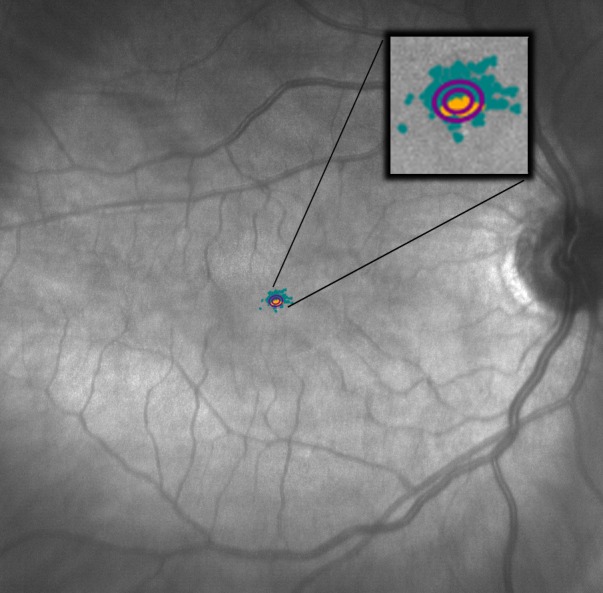
Image of the MAIA microperimeter showing the CFP and both BCEAs (63% and 95%), which lie at approximately the same foveal location on a normal subject.
Primary outcomes of the study were the four MAIA fixation indices: P1, P2, and the two BCEA proportional values of 63% and 95%. Secondary outcomes were the average of sensitivity, distance between the PRLi and PRLf (ΔPRL),15 the MAIA examination time, and the BCEA orientation, which corresponds to the angle between the ellipse major axis (EMA) and the horizontal axis (HA) of the visual meridian, where values between 0° and +90° correspond to an angle measured counterclockwise between the HA and the EMA; values between 0° and −90° are measured clockwise between the HA and the EMA; 0° corresponds to a horizontal orientation and 90° to a vertical one.
Statistical Analysis
All data were exported from the MAIA system as raw data (MAIA software version 1.7.0; CenterVue S.p.A.) and collected into a Microsoft Excel spreadsheet (Microsoft, Bellvue, WA). The statistical analysis was performed with linear regression and Pearson's product moment correlation coefficient. A P value less than 0.05 was considered statistically significant. Linear regression, best-fit values, 95% confidence and prediction intervals, correlation coefficient of determination, and analysis of variance (ANOVA) with 95% CI were calculated and plotted using GraphPad Prism (version 6; GraphPad Software, Inc., La Jolla, CA).
Results
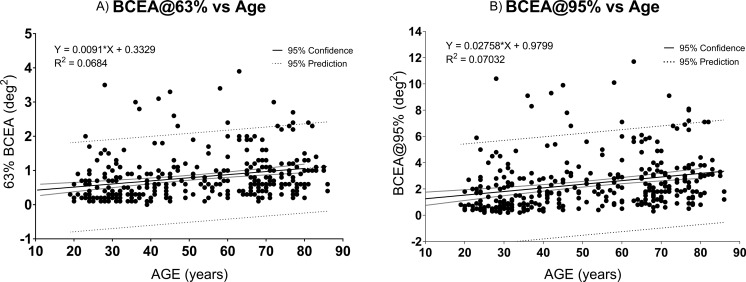
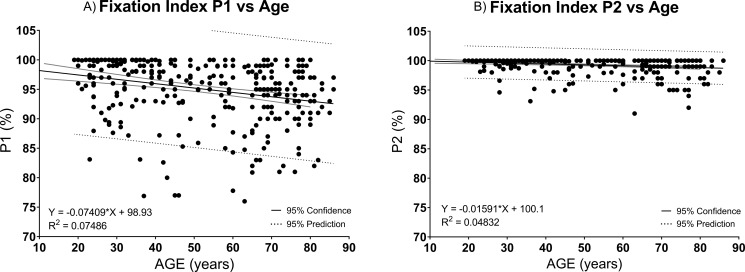
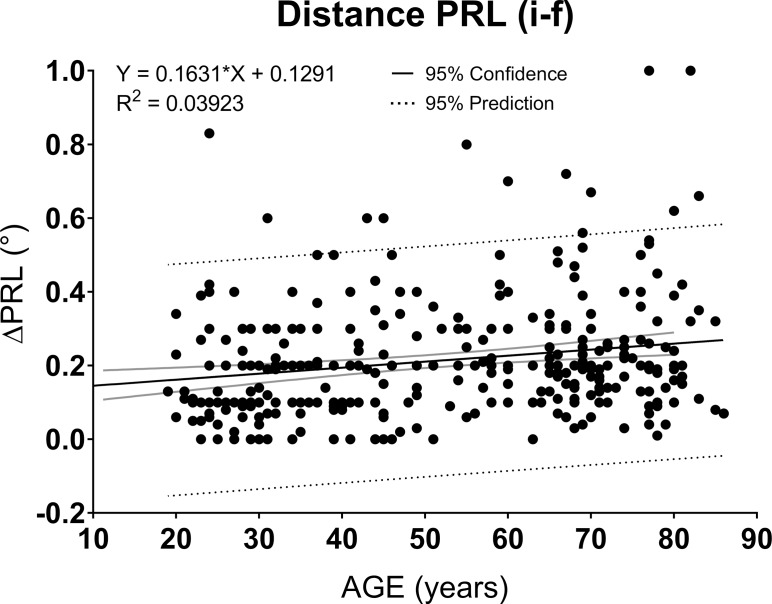
When data from all included eyes (n = 326) were analyzed (Table 1), average areas of 0.80 deg2 (min = 0.03, max = 3.90, SD = 0.68) for the parameter BCEA@63% (Fig. 2A) and 2.40 deg2 (min = 0.20, max = 11.70, SD = 2.04) for BCEA@95% (Fig. 2B) were found. The average values of P1 (Fig. 3A) and P2 (Fig. 3B) were 95% (min = 76, max = 100, SD = 5.31) and 99% (min = 91, max = 100, SD = 1.42), respectively. The maximum fixation value (100%) was recorded in 65 (20%) cases of P1 and 199 (61%) cases of P2. Macular Integrity Assessment P1 and P2 linear regression analysis showed a more sensitive P1 index than P2 (Fig. 3A and 3B). The average sensitivity was 29 dB (min = 18, max = 34, SD = 2.60). The mean ΔPRL was 0.2° (min = 0.0, max = 1.0, SD = 0.16) (Fig. 4). The angular orientation of the BCEA was variable with a mean angle of 3° (min = −90, max = 90, SD = 53.83). The mean examination time for each eye was 5 minutes, 50 seconds (min = 4 minutes, 2 seconds, max = 10 minutes, 40 seconds, SD = 59 seconds).
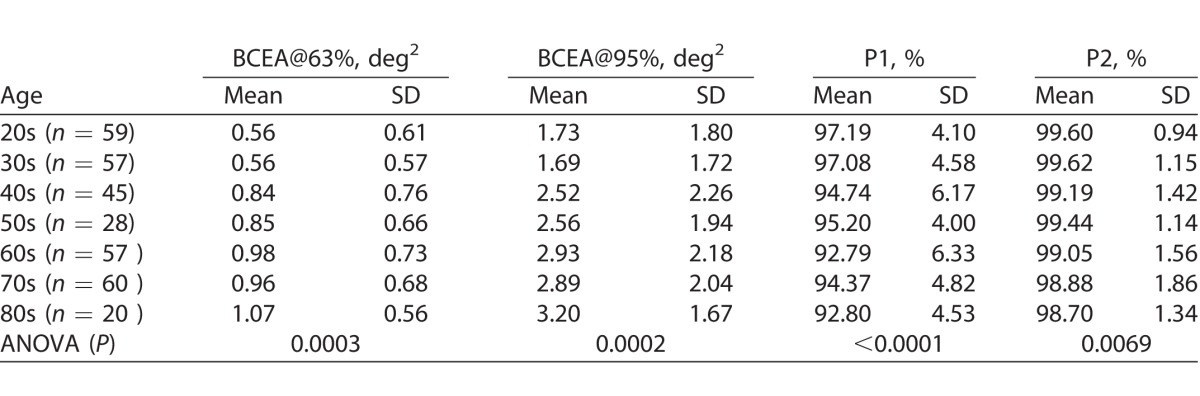
Table 1.
Linear Regression and Summary Statistics for All Study Parameters
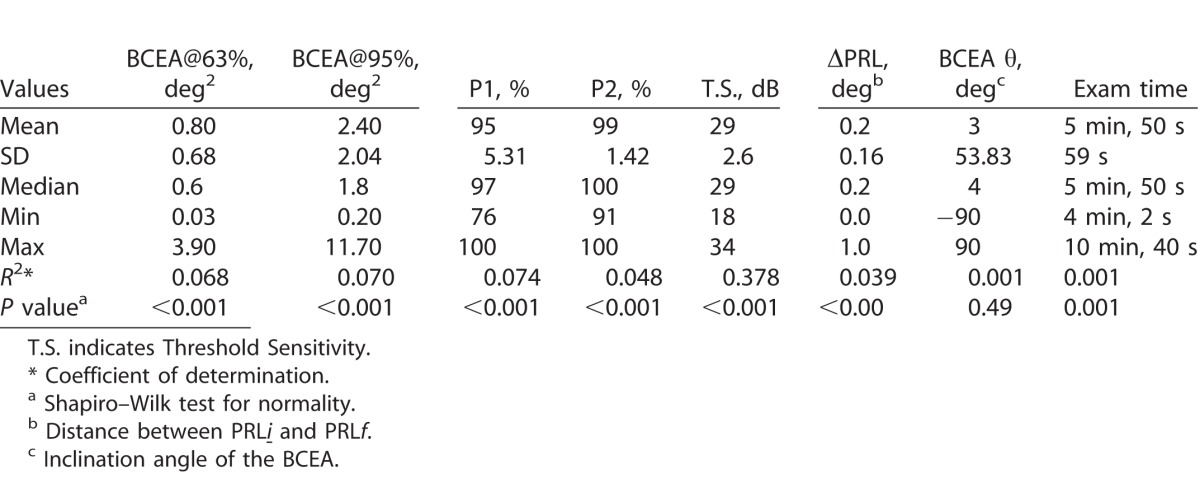
Figure 2.
The BCEA proportional values of 63% shows a mean of 0.80 ± 0.68 deg2 (2A), while the BCEA proportional values of 95% shows a mean of 2.40 ± 2.04 deg2 (2B). Note the distribution similarity between both proportional values' dataset.
Figure 3.
Fixation point P1 (3A) shows mean values of 95% ± 5.31, while P2 (3B) shows mean values of 99% ± 1.42. Note that the R2 value of P1 (0.07), better fits the regression model than does P2 (0.04), which demonstrates higher ceiling effect than P1.
Figure 4.
Distance between both PRLs (i and f) with a mean difference between them of 0.2° ± 0.16°.
The ANOVA comparisons of the FS means within the age groups were highly significant for the indices P1, BCEA@63%, and BCEA@95%, but less significant for P2 (Table 2).
Table 2.
Fixation Stability Values in Different Age Groups
The Pearson's product moment test showed an almost perfect correlation index (r = 0.999) between BCEA@63% and BCEA@95%. The P1 index showed a very strong correlation with BCEA@63% (r = −0.924), as well as with BCEA@95% (r = −0.925). Index P2 demonstrated a slightly lower correlation with both BCEA@63% and BCEA@95%, with r values of −0.874 and −0.875, respectively. The correlation between P1 and P2 (r = 0.792) was lower than that found with the BCEA indices. Finally, low correlations (r < 0.28) between any of the fixation indices and the patient's age were found.
Discussion
Currently available MP instruments can deliver four or more different indices of FS, making the comparison to a reference database overly complicated and somewhat arbitrary in terms of a standard. As such, the CenterVue MAIA MP delivers two PFP indices (P1 and P2) as proposed by Fuji,16 as well as two BCEA indices (63% and 95%) as proposed by Crossland.19 The PFP indices allow the classification of fixation as stable or not stable, but the BCEA indices are not related to any clinical stability standard at the present. This study reports a normative reference database for BCEA FS indices for the MAIA instrument.
In addition, we explored the strongest correlations among all fixation indices, highlighting the near-perfect correlation between BCEA@95% and BCEA@63%, as well as the very strong Pearson's power product between BCEA@95% and P1. Moreover, the P1 and P2 linear regression analysis showed a more sensitive P1 index than P2, with P2 having a higher ceiling effect than P1 (100% maximum percentage).
Various geometric and statistical models using multivariable datasets have been used to simplify and describe the complexity and dynamic nature of movement sampling. The BCEA model describes the horizontal and vertical displacements of the retinal position over the course of time during fixation attempts. By describing FS in this manner, the BCEA has a graphical advantage in its ability to represent a specific proportion of the total CFP dataset points collected. The dimensions and orientation of the BCEA illustrate the total extent of the retinal area used by subjects while attempting to maintain constant fixation.
Crossland et al.19 suggested the analysis of FS by means of BCEA instead of PFP after demonstrating a strong relationship between FS measured with BCEA and many parameters of reading ability, as well as a very poor correlation between PFP indices with any of the standard parameters of reading ability in low vision patients.
Tarita-Nistor et al.24 have stated that the BCEA description of fixation is scientifically more acceptable than the Fuji classification due to the analysis being based on a well-known mathematical model versus the quantification of fixation points falling into an arbitrarily selected fixed circular area of 1° and 2° in radius. However, the main advantage of the Fuji metrics is that it has established a differentiation between normal and non-normal fixation with cutoff values of 75% within 1° radius from the centroid of the fixation dataset.
According to the above, the discrepancy between our MAIA-based findings and the cutoff values of stable fixation proposed by Fuji16 is worthy of comment. Our studied population demonstrated higher P1 values (fixation points within 1° radius) than those proposed by Fuji16 (95% ± 5% vs. 75%), while the P2 index (fixation points within 2° radius) reached a ceiling effect in a high number (61%) of the studied subjects. In contrast, our BCEA values showed only one participant who reached the floor effect in the BCEA@63%, while none of the subjects reached the lowest limiting value in the BCEA@95%.
A literature search reveals reports of different BCEA ellipse values for normal control groups evaluated with MP systems other than the MAIA.24–27 It is noteworthy that some of these previously reported results are based on a fixation-only test lasting between 10 and 30 seconds, and the amount of data collected is less than 800 points. In contrast, the MAIA-based BCEA ellipse is derived from a CFP with more than 8000 data points, a greater than 10-fold difference in data sampling. Furthermore, because the complete MAIA MP examination has a median duration of 5.5 minutes, fixation fatigue may play a major role in creating a larger BCEA ellipse.
In particular, the majority of the participants in our study were naïve clinical patients with no previous experience in maintaining fixation for long periods of time. Other possible explanations for BCEA outcome discrepancy include differences in the N values of the study groups, the motivation and inclusion criteria for selecting study participants, differences in the fixation target dimensions and appearance, and other protocol differences that are beyond the scope of this report.
Tarita-Nistor et al.24 reported in a study with the Nidek MP-1 (Nidek, Gamagori, Japan), 10 experienced healthy controls (age 41 ± 18.1 years) with very small mean BCEA@68% values (0.053 ± 0.022 deg2).This is different from the results obtained by Dunbar et al.,25 who reported the BCEA@68% values of 16 normally sighted volunteers with the Rodenstock SLO and the Nidek MP-1, showing different values among both of their studied instruments that are even larger than our findings (3.3 deg2 with the Rodenstock and 5.0 deg2 with the Nidek).
Liu et al.26 reported BCEA data in subjects with and without maculopathies with two different systems, the MP-1 and optical coherence tomography (OCT)/SLO. The technologies behind the two instruments are different. The MP-1 uses an infrared camera to image the retina controlled by a 25-Hz eye tracker, which is the same eye-tracker frequency found in the MAIA. The second is an SLO imaging device with a much slower eye tracker (8 Hz). Such a study was based on a fixation-only test of 20 seconds, which is largely different from the examination time (mean 350 seconds) studied in this article. Their results suggest that the patient's pattern of FS may be the same, although calculated with different technologies. Furthermore, Liu et al.26 normalized their data with a log transformation of the BCEA units (minutes of arc2) to undertake statistical comparison of the two technologies. In our study, the whole dataset was analyzed using the MAIA output layout with the purpose of establishing reference values for the MAIA that is useful to clinicians.
Similar to the findings reported by Cutini et al.,27 who evaluated BCEA indices in the MP-1 microperimeter (Nidek), our study demonstrates a weak, but statistically significant, correlation between the fixation indices and the patient's age.
Our study data, which was collected from multiple clinical sites, represents true characteristics of the clinical data that will be encountered by eye care professionals using the MAIA system. Because of the aforementioned protocol and technical differences among various systems, the quality and accuracy of fixation results reported for other MP devices are questionable and therefore not directly relatable to the MAIA system.
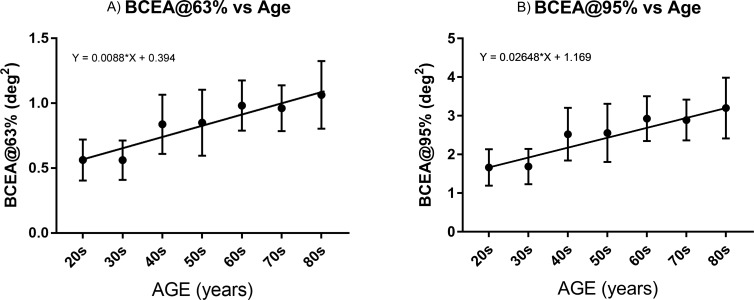
In light of these correlations, we conclude that in clinical practice, the single parameter of the BCEA@95% should be considered as accurately reporting fixation stability and serves as an age-dependent reference database of normal subjects with a cutoff area of 2.4 ± 2.0 deg2 in MAIA MP. This study now establishes an important normative standard for future fixation stability studies of diseased and disease-suspect eyes analyzed with BCEA in the MAIA MP (Fig. 5A and 5B).
Figure 5.
Mean BCEA@63% (5A) and BCEA@95% (5B ) values ± 95% confidence interval (CI) of the mean in the different age groups.
Acknowledgments
We thank CenterVue S.p.A., Padua, Italy, for loaning the MAIA microperimeter to the University of Nottingham for a limited period.
Dr. Smolek is employed by the United States Army. This study was not funded by the United States Army. The subject matter was reviewed, and there is no objection to its publication. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting true views of the Department of the Army or the Department of the Defense.
The initial results of this material have been presented as a Poster Presentation for the Association for Research in Vision and Ophthalmology (ARVO) 2016 Annual Meeting.
Disclosure: M.U. Morales, (C); S. Saker, None; C. Wilde, None; C. Pellizzari, (E); A. Pallikaris, None; N. Notaroberto, None; M. Rubinstein, None; C. Rui, (E); P. Limoli, None; M.K. Smolek, None; W.M. Amoaku, None
Footnotes
This work was done as part of the University of Nottingham PhD research program of Marco U. Morales. The sponsor or funding organization had no role in the design or conduct of this research.
References
- 1. Midena E,, Vujosevic S,, Convento E,, et al. Microperimetry and fundus autofluorescence in patients with early age-related macular degeneration. Br J Ophthalmol. 2007. ; 91: 1499–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nakamura Y,, Mitamura Y,, Ogata K,, et al. Functional and morphological changes of macula after subthreshold micropulse diode laser photocoagulation for diabetic macular oedema. Eye (Lond). 2010. ; 24: 784 –78 . [DOI] [PubMed] [Google Scholar]
- 3. Hatef E,, Colantuoni E,, Wang J,, et al. The relationship between macular sensitivity and retinal thickness in eyes with diabetic macular edema. Am J Ophthalmol. 2011. ; 152: 400 –4 . [DOI] [PubMed] [Google Scholar]
- 4. Pilotto E,, Vujosevic S,, Grgic VA,, et al. Retinal function in patients with serpiginous choroiditis: a microperimetry study. Graefes Arch Clin Exp Ophthalmol. 2010. ; 248: 1331 –133 . [DOI] [PubMed] [Google Scholar]
- 5. Vujosevic S,, Smolek MK,, Lebow KA,, et al. Detection of macular function changes in early (AREDS 2) and intermediate (AREDS 3) age-related macular degeneration. Ophthalmologica. 2011. ; 225: 155 –1 . [DOI] [PubMed] [Google Scholar]
- 6. Alexander P,, Mushtaq F,, Osmond C,, et al. Microperimetric changes in neovascular age-related macular degeneration treated with ranibizumab. Eye. 2012. ; 26: 678 –6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Markowitz SN,, Reyes SV. Microperimetry and clinical practice: an evidence-based review. Can J Ophthalmol. 2012; 48: 350–357. [DOI] [PubMed] [Google Scholar]
- 8. Martínez-Costa L,, VictoriaIbañez M,, Murcia-Bello C,, et al. Use of microperimetry to evaluate hydroxychloroquine and chloroquine retinal toxicity. Can J Ophthalmol. 2013; 48: 400–405. [DOI] [PubMed] [Google Scholar]
- 9. Leal C,, De Bats F,, Decullier E,, et al. Anatomical-functional correlation using microperimetry on age-related macular degeneration: a study of 59 eyes. Invest Ophthalmol Vis Sci. 2014; 55: 5208. [Google Scholar]
- 10. MacLaren RE,, Groppe M,, Barnard AR,, et al. Retinal gene therapy in patients with choroideremia: initial findings from a phase 1/2 clinical trial. Lancet. 2014. ; 383: 1129 –11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wu Z,, Ayton LN,, Luu CD,, et al. Microperimetry of nascent geographic atrophy in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2014. ; 56: 115 –1 . [DOI] [PubMed] [Google Scholar]
- 12. Ozdemir H,, Karacorlu M,, Senturk F,, et al. Microperimetric changes after intravitreal bevacizumab injection for exudative age-related macular degeneration. Acta Ophthalmol. 2012. ; 90: 71 –7 . [DOI] [PubMed] [Google Scholar]
- 13. Hanout M,, Horan N,, Do DV. Introduction to microperimetry and its use in analysis of geographic atrophy in age-related macular degeneration. Curr Opin Ophthalmol. 2015. ; 26: 149 –1 . [DOI] [PubMed] [Google Scholar]
- 14. Pilotto E,, Benetti E,, Convento E,, et al. Microperimetry, fundus autofluorescence and retinal layer changes in progressing geographic atrophy. Can J Ophthalmol. 2013; 48: 386–393. [DOI] [PubMed] [Google Scholar]
- 15. Morales MU,, Saker S,, Mehta RL,, et al. Preferred retinal locus profile during prolonged fixation attempts. Can J Ophthalmol. 2013. ; 48: 368 –3 . [DOI] [PubMed] [Google Scholar]
- 16. Fujii GY,, de Juan E,, Sunness J,, et al. Patient selection for macular translocation surgery using the scanning laser ophthalmoscope. Ophthalmology. 2002. ; 109: 1737 –17 . [DOI] [PubMed] [Google Scholar]
- 17. Crossland MD,, Dunbar HM,, Rubin GS. Fixation stability measurement using the MP1 microperimeter. Retina. 2009. ; 29: 651 –65 . [DOI] [PubMed] [Google Scholar]
- 18. Crossland MD,, Sims M,, Galbraith RF,, et al. Evaluation of a new quantitative technique to assess the number and extent of preferred retinal loci in macular disease. Vision Res. 2004; 44: 1537–1546. [DOI] [PubMed] [Google Scholar]
- 19. Crossland MD,, Rubin GS. The use of an infrared eyetracker to measure fixation stability. Optom Vis Sci. 2002. ; 79: 735 –73 . [DOI] [PubMed] [Google Scholar]
- 20. Steinman RM. Effect of target size, luminance, and color on monocular fixation. J Opt Soc Am. 1965; 55: 1158–1164. [Google Scholar]
- 21. Kosnik W,, Fikre J,, Sekuler R. Visual fixation stability in older adults. Invest Ophthalmol Vis Sci. 1986. ; 27: 1720 –17 . [PubMed] [Google Scholar]
- 22. Schuchard RA,, Raasch TW. Retinal locus for fixation: pericentral fixation targets. Clin Vision Sci. 1992; 7: 511–520. [Google Scholar]
- 23. Midena E,, Vujosevic S,, Cavarzeran F. Normal values for fundus perimetry with the microperimeter MP1. Ophthalmology. 2010. ; 117: 1571 –157 . [DOI] [PubMed] [Google Scholar]
- 24. Tarita-Nistor L,, Gonzalez EG,, Markowitz SN,, et al. Fixation characteristics of patients with macular degeneration recorded with the mp-1 microperimeter. Retina. 2008; 28: 125–133. [DOI] [PubMed] [Google Scholar]
- 25. Dunbar H,, Crossland M,, Rubin G. Fixation stability: a comparison between the Nidek MP-1 and the Rodenstock scanning laser ophthalmoscope in persons with and without diabetic maculopathy. Invest Ophthalmol Vis Sci. 2010; 51: 4346–4350. [DOI] [PubMed] [Google Scholar]
- 26. Liu H,, Bittencourt M,, Sophie R,, et al. Fixation stability measurement using two types of microperimetry devices. Trans Vis Sci Tech. 2015; 4 (2): 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cutini A,, Fragiotta S,, Spadea L,, et al. Normal values and repeatability of bivariate contour ellipse area (BCEA) with Microperimeter Mp-1. Invest Ophthalmol Vis Sci. 2014; 55: 169–169. 24334451 [Google Scholar]