Abstract
Background
The association between preoperative patient characteristics and the number of major postoperative complications after major surgery is not well defined.
Methods
In a retrospective, single-center cohort of 50,314 adult surgical patients using readily available preoperative clinical data, we modeled the number of major postoperative complications from none to three or more. We included acute kidney injury, prolonged stay (>48h) in an intensive care unit, need for prolonged (>48h) mechanical ventilation, severe sepsis, and cardiovascular, wound, and neurologic complications. Risk probability scores generated from the multinomial logistic models were used to develop an online calculator. We stratified patients based on the risk for having three or more postoperative complications.
Results
Patients older than 65 years (OR 1.5, 95% CI 1.4-1.6), males (OR 1.2, 95% CI 1.2-1.3), patients with a greater Charlson comorbidity index (OR 3.9, 95% CI 3.6-4.2), those requiring emergency surgery (OR 3.5, 95% CI 3.3.-3.7), and those admitted on a weekend (OR 1.4, 95% CI 1.3-1.5) were more likely to have three or more postoperative complications compared to having none. Patients in the medium and high risk categories were 3.7 and 6.3 times more likely to have three or more postoperative complications, and high risk patients were 5.8 and 4.4 times more likely to die within 30 and 90 days of admission respectively.
Conclusions
Readily available, preoperative clinical and sociodemographic factors are associated with a greater number of postoperative complications and adverse surgical outcomes. We developed an online calculator that predicts probability for each number of complications after major surgery.
Index Words: postoperative complications, epidemiology and outcomes, ordinal models, online calculator, risk assessment, outcomes research
Introduction
Over 50 million inpatient surgical procedures are performed in the United States every year.1 It is estimated that between 3% and 17% of all people undergoing surgical procedures develop postoperative complications, while almost 1% of surgical procedures result in death.2-4 Postoperative complications are associated with greater risks of hospital mortality and hospital readmissions after discharge 5-8, and the costs of health care associated with surgical procedures increases proportionally to the number of postoperative complications.9-11
Postoperative acute kidney injury (AKI) is a common and potentially devastating complication. When defined by consensus criteria, AKI affects up to 30% of surgical patients and is associated with increased risk for other major complications including sepsis, respiratory failure, cardiovascular complications and prolonged stay in an intensive care unit (ICU). The combination of these major complications often occurs in the same patient leading to a substantial increase in cost of care, development of chronic critical illness, and increased long-term mortality and disability 6, 11-29. The ability to determine preoperatively the overall risk for multiple major postoperative complications could be important for clinical decision-making. Appropriate risk-stratification of patients prior to surgery may improve patient selection and promote the timely initiation of intraoperative preventive strategies to decrease the number and severity of complications.30
Previously reported predictive models assessing the preoperative risk for complications were often limited to specific types of operations, or used statistical modeling for a single complication or complications grouped into binary categories rather than predicting the overall number of complications.7, 30-33 Ordinal regression models developed to optimize predictive modeling when outcomes of interest have more than two categories have been underutilized in surgical studies, although such approaches may provide better use of the information contained in clinical data with better predictive accuracy.34 In a large, single center cohort of adult patients undergoing any major inpatient surgery by optimizing modeling approaches, using readily available preoperative clinical data, we have developed preoperative risk scores for each number of major postoperative complications.
Methods
Study Cohort
Using the University of Florida (UF) Health Integrated Data Repository, we assembled a single-center cohort of perioperative patients by integrating multiple existing clinical and administrative databases at UF Health. We included all patients with age greater or equal to 18 years admitted to the hospital for greater than 24h after any type of inpatient operative procedure between January, 2000 and November, 2010 as described previously.14 The final cohort included 50,314 patients. The study was approved by the Institutional Review Board and Privacy Office of the University of Florida (eMethods online version only).
Covariates and Outcome
The primary outcome was the exact number of postoperative complications out of the seven major complications we considered: AKI, mechanical ventilation (MV) required for greater than 48h, ICU admission for greater than 48h, severe sepsis, cardiovascular complications and/or the need for vasopressors for greater than 24h, neurologic complications (including delirium), and wound complications (including mechanical wound complications and surgical infections). The number of complications ranged from none to three or more complications. We collapsed the last category to ≥ three, because only a small number of patients had more than three complications. Postoperative AKI was defined using RIFLE (Risk, Injury, Failure, Loss, End-stage renal disease) criteria which corresponds to at least a 50% increase in serum creatinine after operation compared to a reference value which was the minimum of the creatinine values available within six months of admission. For the definition of sepsis, we followed the selection criteria developed by the Agency for Healthcare Research and Quality for the patient safety indicators “Postoperative Sepsis”, while severe sepsis was defined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for acute organ dysfunction due to the diagnosis of sepsis. 35-37 We determined the need for vasopressor therapy for greater than 24h for each patient using administration times and doses of any medication within the category of a vasopressor from the pharmacy database. 38 We defined neurologic complications (including delirium)39, cardiovascular complications40, 41, and wound complications (including mechanical wound complications and surgical site infections)40, 41 using previously described criteria based on ICD-9-CM codes as detailed in eTable 1 (online version only). The exact dates were used to calculate the duration of mechanical ventilation and length of stay in an intensive care unit. Secondary outcomes were 30-day and 90-day mortality. Patient survival status was determined using hospital discharges and the Social Security Death Index.
The covariates used to develop predictive models were clinical variables available in routine preoperative assessment, including age (grouped as ≥65 years or <65 years), sex, African-American ethnicity, primary insurance type, Charlson comorbidity index, and type of procedure, including cardiothoracic surgery, non-cardiac general and vascular surgery, neurologic surgery, specialty operations (including orthopedic, gynecologic, head and neck, urologic, and plastic), and other surgeries (including burn, ophthalmology, transplantation, and trauma).
Statistical Analysis
The analytic plan followed the STROBE recommendations for observational cohort studies.42 We compared five ordinal regression modeling approaches (eMethods) to determine the method producing the best estimate of the risk for developing a specific number of complications (from none to ≥three).43 To assess discrimination of the final model, we calculated the area under the receiver operating characteristics curve (AUC) by averaging values obtained from all pairwise comparisons of the classes44 and a confidence interval for the AUC from 100 bootstrap samples. Model fit for different approaches was compared using likelihood-ratio-tests (LRT) and the Akaike Information Criterion (AIC). The multinomial logistic model, a baseline-category logit model with maximal flexibility in the analysis of nominal responses, produced the best fit and was used to calculate the probabilistic risk score for each outcome category for an individual patient. The risk scores for each outcome ranged from 0 to 1 and corresponded to the probability for having that outcome given the preoperative characteristics of a patient.
Because patients with three or more complications had markedly increased mortality, we used a probabilistic risk score calculated with the multinomial logistic model for this outcome to develop two cut-offs that could be used to risk-stratify patients into low, medium, and high risk for having three or more major complications after surgery. The cut-off points for the probabilistic risk score were determined using the maximum Youden index value and plateau of the accuracy curve (eFigure 1 online version only). Relative risks were used to show the association between risk categories and multiple complications, 30-day mortality, and 90-day mortality. The association between the number of complications and 30-day and 90-day mortality were tested using a multivariable logistic regression model. We performed sensitivity analyses by comparing the effect of the inclusion of patients with missing values for serum creatinine. A two sided p < 0.05 was considered significant for all tests performed. Statistical analysis was performed with SAS (v.9.3, Cary, N.C.) and R 3.0.2.
Results
Baseline Characteristics and Resource Utilization
Among 50,314 patients in the final cohort, 41% had no postoperative complications, while 26%, 12%, and 21% had one, two, and three or more complications respectively. Increasing age and number of comorbidities, male sex, and emergent surgery were more likely among patients with complications. Patients undergoing cardiothoracic surgery were more likely to have three or more complications, while patients undergoing specialty operation had the greatest proportion of patients with no complications (Table 1).
Table 1.
Clinical characteristics and resource utilization for all patients stratified by number of complications.
| Variables | Overall cohort (n=50314) | No Postoperative Complications (n=20748) | One Postoperative Complication (n=13200) | Two Postoperative Complications (n=6075) | Three and more Postoperative Complications (n=10291) |
|---|---|---|---|---|---|
| Age >=65, n (%) | 16367 (32.5) | 5791 (27.9) | 4300 (32.6) * | 2237 (36.8) * | 4039 (39.3) * |
| Female sex, n (%) | 24668 (49.0) | 11275 (54.3) | 6396 (48.45) * | 2721 (44.8) * | 4276 (41.6) * |
| African-American ethnicity, n (%) | 6182 (12.3) | 2423 (11.68) | 1706 (13.0)* | 758 (12.5) | 1295 (12.6) |
| Primary Insurance, n (%) | |||||
| Medicare | 19467 (38.7) | 6810 (32.8) | 5360 (40.6) * | 2690 (44.3) * | 4607 (44.8) * |
| Medicaid | 6517 (13.0) | 2680 (12.9) | 1551 (11.8) * | 733 (12.1) | 1553 (15.1) * |
| Private | 20591 (40.9) | 9400 (45.3) | 5367 (40.7) * | 2264 (37.3) * | 3560 (34.6) * |
| No insurance | 3739 (7.4) | 1858 (9.0) | 922 (7.0)* | 388 (6.4) * | 571 (5.6)* |
| Weekend admission, n (%) | 6881 (13.7) | 2105 (10.2) | 1713 (13.0) * | 957 (15.8) * | 2106 (20.5) * |
| Emergency admission, n (%) | 22818 (45.4) | 6995 (33.7) | 5866 (44.4) * | 3128 (51.5) * | 6829 (66.4) * |
| Charlson-Deyo Comorbidity Score, n (%) | |||||
| 0 | 18490 (36.8) | 9996 (48.2) | 4692 (35.6) * | 1630 (26.8) * | 2172 (21.1) * |
| 1-2 | 19398 (38.5) | 7166 (34.5) | 4890 (37.1) * | 2554 (42.0) * | 4788 (46.5) * |
| >=3 | 12426 (24.7) | 3586 (17.3) * | 3618 (27.4) * | 1891 (31.1) * | 3331 (32.4) * |
| Type of Procedure, n (%) | |||||
| Cardiothoracic Surgery | 6755 (13.4) | 912 (4.4) | 1297 (9.8) * | 1282 (21.1) * | 3264 (31.7) * |
| Neurologic Surgery | 8385 (16.7) | 3512 (16.9) | 1985 (15.0) * | 899 (14.8) * | 1989 (19.3) * |
| Non-Cardiac General Surgery | 10741 (21.3) | 4571 (22.0) | 3180 (24.1) * | 1349 (22.2) | 1641 (16.0) * |
| Specialty Operations† | 15229 (30.3) | 9276 (44.7) | 3789 (28.7) * | 1095 (18.0) * | 1069 (10.4) * |
| Other Operations ‡ | 9204 (18.3) | 2477 (11.9) | 2949 (22.3) * | 1450 (23.9) * | 2328 (22.6) * |
| Postoperative Complications, n (%) | |||||
| Acute kidney Injury | 19644 (39.0) | NA | 6417 (48.6) * | 3767 (62.0) * | 9460 (91.9) * |
| ICU admission for longer than 48 hours | 16,244 (32.3) | NA | 2743 (20.8) * | 3674 (60.5) * | 9827 (95.5) * |
| Cardiovascular complications or need for vasopressors | 11786 (23.4) | NA | 1618 (12.3) * | 2215 (36.5) * | 7953 (77.3) * |
| Mechanical ventilation for greater than 48 hours | 6931 (13.8) | NA | 35 (0.5) * | 319 (4.6) * | 6577 (94.9) * |
| Mechanical wound complications and surgical infections | 5944 (11.8) | NA | 1589 (12.0) * | 1387 (22.8) * | 2968 (28.8) * |
| Neurologic and delirium complications | 4037 (8.0) | NA | 796 (6.0) * | 750 (12.4) * | 2491 (24.2) * |
| Severe sepsis | 2302 (4.6) | NA | 2 (0.02) | 38 (0.63) * | 2262 (22.0) * |
| Resource utilization | |||||
| Days in hospital, Median (25th, 75th) | 7 (4, 12) | 4 (3,6) | 6 (4,10) * | 9 (6,14) * | 20 (12, 35) * |
| Hospital cost (1000$), Median (25th, 75th) | 19 (12, 38) | 13 (9,18) | 17 (12, 28) * | 28 (19, 42) * | 70 (42, 118) * |
| ICU admission, n (%) | 26433 (52.5) | 4454 (21.5) | 6637 (50.3) * | 5130 (84.4) * | 10212 (99.2) * |
| Days in ICU, Median (25th, 75th) § | 4 (2, 8) | 1 (1,2) | 2 (1,4) * | 4 (2,7) * | 10 (5,19) * |
| 12873 (25.6) | 879 (4.2) | 1640 (12.4) * | 1909 (31.4) * | 8445 (82.1) * | |
| Mechanical ventilation, n (%) | |||||
| Days on mechanic ventilation, Median (25th, 75th) § | 3 (2, 11) | 1 (1,2) | 2 (1,2) | 2 (1,2) | 7 (3,18) * |
| Discharge, n (%) | |||||
| Discharge to home | 37220 (76.9) | 17724 (85.4) | 10613 (80.4) * | 4493 (74.0) * | 4390 (42.7) * |
| Discharge to nursing home | 3971 (8.2) | 929 (4.5) | 888 (6.7) * | 522 (8.6) * | 1632 (15.9) * |
| Discharge to other acute care facility/hospital | 3631 (7.5) | 993 (4.8) | 898(6.8) * | 491 (8.1) * | 1249 (12.1) * |
| Discharge to rehab facility | 3594 (7.4) | 1094 (5.3) | 750 (5.7) | 429 (7.1) * | 1321 (12.8) * |
p-value <0.05 for comparison with respect to no postoperative complications group using Bonferroni adjustment
Specialty operations include orthopedic, gynecologic, head and neck, urologic and plastic surgery procedures.
Other operations include trauma, burn and transplant procedures.
Reported only for patients who were admitted to ICU and for patients who required mechanical ventilation, respectively.
Among the seven major complications we evaluated, postoperative AKI (39%, 19,644/50,314) was the most common, followed by ICU admission > 48h, cardiovascular complications and/or the need for vasopressors, and mechanical ventilation > 48h (occurring in 32%, 23%, and 14% of the cohort, respectively). A majority of patients with three or more complications had some combination of prolonged ICU stay, mechanical ventilation, AKI, and cardiovascular complications and/or the need for vasopressors. Hospital duration of stay increased as the number of complications increased ranging from four days among patients with no complications to 20 days among those with three or more complications (P<0.001). Similarly, median duration of stay in the ICU increased from 1 day in the no complication group to 10 days among patients with three or more complications (P<0.001). Patients with three or more complications had an almost five-fold increase in median hospital cost of $70,000 compared to patients with no complications (median cost $13,000, p<0.0001) and were less likely to be discharged to their home compared to patients with no complications (43% vs. 85%, p<0.0001) (Table 1).
Number of postoperative complications and mortality
Overall 30-day mortality and 90-day mortality were 3.5% and 6.6% respectively. For patients with three or more complications, the 30-day mortality increased to 12.2% and 90-day mortality to 20.4%. A majority of deaths within 30 days and 90 days of hospitalization occurred in those patients with three or more complications (72%, 1,256/1,749 and 63%, 2,098/3,330, respectively) (eTable 2). An increasing number of complications were associated with increasing 30-day and 90-day mortality for all types of major operations. Patients who experienced no complications had very low 30-day mortality regardless of type of operation, ranging from 0.3% to 1.2%. Patients with only one complication still had a low 30-day mortality that remained less than 2.2% for all types of operations. Patients with two postoperative complications had up to triple the risk for 30-day mortality regardless of the type of operation. Patients with three or more postoperative complications had up to a 20-fold increase in both 30-day and 90-day mortality. Thirty-day mortality for these patients ranged from 9% to 17%, while 90-day mortality was between 16% and 25% (eTable 2). In multivariable regression analysis, the adjusted odds of 30-day and 90-day mortality for patients with ≥ 3 complications were about 16 and 9 times that for patients with no postoperative complications even after adjusting for demographic and clinical preoperative variables (Table 2)
Table 2.
Unadjusted and adjusted association between number of postoperative complications and mortality.
| No Postoperative Complications | One Postoperative Complication | Two Postoperative Complications | Three or more Postoperative Complications | |
|---|---|---|---|---|
| 30-day mortality | ||||
| Unadjusted OR (95% CI) | 1 (Reference) | 2.36 (1.86, 3)* | 6.73 (5.34, 8.47) * | 25.61 (21.08, 31.12) * |
| Adjusted OR (95% CI)† | 1 (Reference) | 1.83 (1.43, 2.33) * | 4.69 (3.7, 5.94) * | 16.12 (13.13, 19.78) * |
| 90-day mortality | ||||
| Unadjusted OR (95% CI) | 1 (Reference) | 2.01 (1.75, 2.3) * | 3.73 (3.22, 4.31) * | 13.95 (12.46, 15.62) * |
| Adjusted OR (95% CI)† | 1 (Reference) | 1.48 (1.28, 1.7) * | 2.49 (2.14, 2.9) * | 9.03 (7.99, 10.21) * |
Abbreviations. OR, odds ratio; CI, confidence interval.
Denotes statistically significant findings at 0.05 significance level.
Adjusted odds ratios were obtained adjusting for age group, gender, African-American ethnicity, insurance type, comorbidity score, type of operation, emergency surgery status, and weekend admission status.
Predictive models for number of major complications
Using the multinomial logistic model, with a discrimination AUC of 0.710 (95% CI 0.707-0.713), we determined the strength of association between several preoperative factors and the risk for each outcome category. Compared to younger patients, patients older than 65 years had 1.18 odds (95% confidence interval (CI) 1.07-1.29) of having two complications and 1.49 odds (95% CI 1.37-1.62) of having three or more complications (Table 3). Compared to females, males had greater odds of having more than one complication with odds ratios between 1.1 and 1.2. Patients with Medicare insurance had about 30% to 40% greater odds of having more postoperative complications than patients with private insurance. Compared to patients with no comorbidities, patients with comorbidities had greater odds of having a greater number of complications, ranging between 1.4 and 3.9. Patients undergoing cardiothoracic surgery had much greater odds of having three or more postoperative complications versus no complications when compared to patients undergoing specialty operations (OR 23.64, 95% CI 21.36-26.16). Patients who had procedures that were performed under emergency circumstances compared to routine elective procedures and those admitted during the weekend were more likely to develop a greater number of complications (Table 3).
Table 3.
Multivariable analysis of preoperative factors associated with the number of complications after surgery
| Variable | One vs. No Postoperative Complications OR (95% CI) | Two vs. No Postoperative Complications OR (95% CI) | Three or More vs. No Postoperative Complications OR (95% CI) |
|---|---|---|---|
| Age ≥ 65 (vs. <65) | 0.97 (0.91, 1.05) | 1.18 (1.07, 1.29)* | 1.49 (1.37, 1.62)* |
| Male (vs. Female) | 1.11 (1.06, 1.17)* | 1.17 (1.10, 1.24)* | 1.23 (1.17, 1.30)* |
| African-American Ethnicity (vs. others) | 1.12 (1.04, 1.20)* | 1.07 (0.98, 1.18) | 1.02 (0.94, 1.11) |
| Insurance Type (vs. Private) | |||
| Medicare | 1.39 (1.29, 1.49)* | 1.41 (1.28, 1.54)* | 1.29 (1.18, 1.40)* |
| Medicaid | 0.97 (0.90, 1.04) | 1.06 (0.96, 1.17) | 1.32 (1.22, 1.44* |
| Uninsured | 0.76 (0.69, 0.83)* | 0.75 (0.66, 0.84)* | 0.63 (0.56, 0.71)* |
| Charlson-Deyo Comorbidity Score (vs. 0) | |||
| 1-2 | 1.42 (1.35, 1.50)* | 1.97 (1.83, 2.13) * | 2.56 (2.40, 2.74) * |
| >=3 | 2.07 (1.95, 2.20)* | 3.00 (2.76, 3.26)* | 3.89 (3.61, 4.20)* |
| Type of Procedure (vs. Specialty Operations†) | |||
| Cardiothoracic Surgery | 3.10 (2.82, 3.41)* | 9.83 (8.82, 10.95) * | 23.64 (21.36, 26.16) * |
| Neurologic Surgery | 1.39 (1.30, 1.49)* | 2.11 (1.91, 2.33) * | 4.26 (3.89, 4.65) * |
| Non-Cardiac General and Vascular Surgery | 1.64 (1.55, 1.75)* | 2.38 (2.17, 2.60) * | 2.96 (2.71, 3.24) * |
| Other Operations‡ | 2.81 (2.62, 3.02)* | 4.62 (4.19, 5.09) * | 6.40 (5.84, 7.02) * |
| Emergency Surgery (vs. Routine Elective) | 1.44 (1.36, 1.51)* | 1.89 (1.76, 2.02) * | 3.54 (3.33, 3.77) * |
| Weekend admission (vs. Weekday) | 1.05 (0.98, 1.13) | 1.19 (1.09, 1.30) * | 1.36 (1.26, 1.47) * |
Abbreviations. OR, odds ratio; CI, confidence interval.
Denotes statistically significant findings at 0.05 significance level
Specialty operations include orthopedic, gynecologic, head and neck, urologic, and plastic surgery procedures.
Other operations include trauma, burn and transplant procedures.
Risk score for three or more postoperative complications
Because patients with three or more complications had markedly increased mortality, we used the probabilistic risk score calculated with the multinomial logistic model for this outcome to develop two cut-offs that could be used to risk-stratify patients into low, medium, and high risk for having three or more major postoperative complications. The probabilistic score of 0.2 was used to discriminate between low and medium risk groups, while a probabilistic score of 0.5 was used to discriminate between medium and high risk groups (eFigure 1 and Figure 1A). About 60%, 33%, and 7% of all patients were distributed in low, medium, and high risk categories for developing three or more complications respectively. We observed absolute risks of having at least 3 complications as 9.1%, 33.9%, and 57.5% in low, medium, and high risk categories, respectively. Compared to patients with a low risk score, patients with medium and high risk scores had relative risks of 3.7 (95% CI 3.6-3.9) and 6.3 (95% CI 6.0-6.6) for having three or more complications (Figure 1 B). Relative risks of 30-day and 90-day mortality were 4.5 (95% CI 4.0-5.0) and 3.5 (95% CI 3.3-3.8) for patients with medium risk scores and 5.8 (95% CI 5.0-6.7) and 4.4 (95% CI 4.0-4.9) for patients with high risk scores respectively, compared to patients with low risk scores (Figure 1, panels C and D). Thirty-day and 90-day mortality increased sharply among patients with at least three complications (Figure 2 A). The overall percentage for 30-day mortality was 1.4%, 6.3%, and 8.2% for low, medium, and high risk categories respectively, and for 90-day mortality was 3.2%, 11.3, and 14.3% respectively. Percentages of 30-day and 90-day mortality for each risk category after stratification into groups based on number of complications are reported in Figure 2, panels B and C. Among patients with less than three complications, medium and high risk groups had significantly greater mortality rates than patients in the low risk group.
Figure 1.
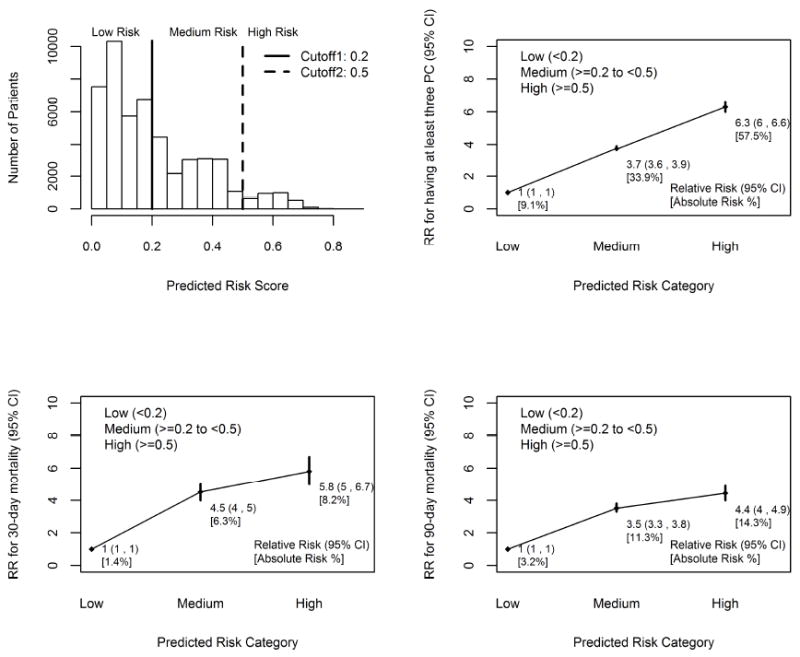
Panel (A) Histogram of predicted risk scores with cut-offs to stratify patients into low, medium, and high risk groups for having at least three postoperative complications. (B) Relative risk and 95% confidence interval (CI) for having at least three postoperative complications. (C) Relative risk and 95% CI for 30-day mortality. (D) Relative risk and 95% CI for 90-day mortality.
Relative risks were obtained for medium and high risk categories with respect to low risk group. p<0.05 for comparison with respect to low risk group.
Figure 2.
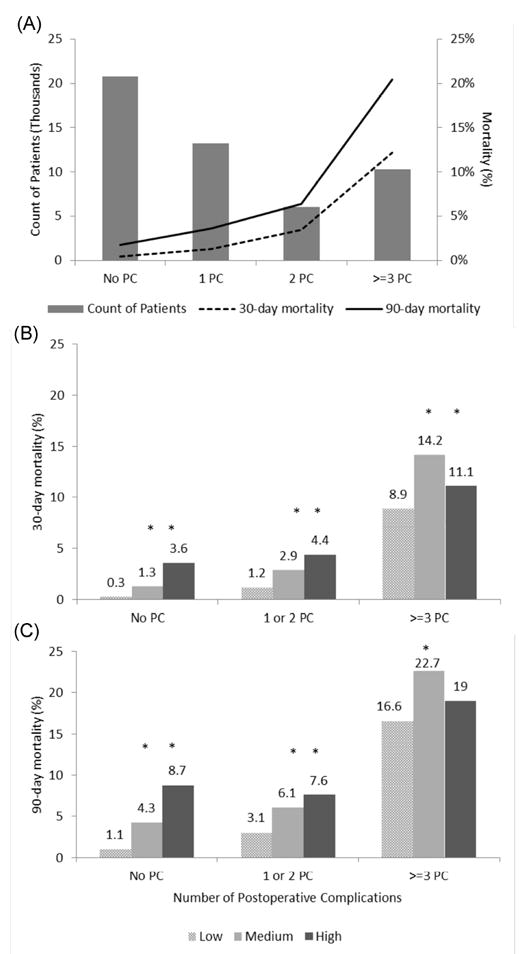
Panel (A) The relationship between 30-day and 90-day mortality and the number of postoperative complications. (B) Percentage of 30-day mortality for patients stratified by number of postoperative complications and risk categories obtained for having at least three complications. (C) Percentage of 90-day mortality for patients stratified by number of postoperative complications and risk categories obtained for having at least three complications. *p<0.05 for comparison with respect to low risk group.
Discussion
In a large, single-center cohort of patients undergoing major surgery, we have developed a simple preoperative risk model that predicts the number of major postoperative complications using a multinomial logistic regression approach. Our model utilizes readily available clinical and sociodemographic characteristics and can be applied to any type of major surgical procedure. Using probabilistic methods, we developed two cut-offs that can be used to risk-stratify patients into low, medium, and high risk for having three or more major postoperative complications. Compared to patients with a low risk score, patients with medium and high risk scores had significantly increased risks of having multiple complications and mortality within 30 and 90 days of admission. The ability to determine the overall risk for multiple postoperative complications based on readily available demographic and clinical data could be important in choosing optimal treatment options for patients with different preoperative risks and thus improving the quality of their peri- and postoperative care. The ability to predict which patients are at increased risk for complications will allow surgeons to better judge a patient’s fitness for a particular operation and will help the anesthesiologist to better tailor intraoperative care to the patient. Our results corroborate existing evidence in the literature demonstrating association between postoperative complications and greater duration of stay, greater health care costs, and a greater risk of mortality.5-11, 13 Patients with three or more complications had markedly increased 30-day and 90-day mortality, up to 20-fold, compared to patients with no complications. The association between the increase in mortality and number of complications was independent of other factors including patients’ age, sex, comorbidity burden on admission, and type of surgical procedure.
While multiple studies have shown that patient characteristics have an influence on the risk of developing postoperative complications, we are not aware of any previous studies that have modeled the number of complications30,33,35. Consistent with other studies, our study demonstrated that emergent surgery, greater age, and greater number of comorbidities were associated with more postoperative complications.31, 32 One study demonstrated that preoperative functional status may help identify patients at greater risk of postoperative complications.33 A strength of our study is that we were able to use only readily available preoperative demographic and clinical variables to insure that a risk score could be calculated easily and quickly.
The statistical approach in previous studies used mostly dichotomized outcomes by categorizing patients into those who had no postoperative complications and those with one or more complication, rather than taking number of complications as an ordinal variable. Calculations of asymptotic relative efficiency and results of simulations showed that simple logistic regression applied to dichotomized responses have decreased efficiency compared to ordinal regression models.45 In addition, dichotomization can be arbitrary, especially when there are many ordered categories.46 Instead of dichotomizing the outcome, we modeled the number of postoperative complications using several ordinal models, among which multinomial logistic regression performed the best. By using a multinomial logistic regression, the model can be fit using any standard program, and the results can be interpreted easily. The multinomial model is appropriate when the effect of each predictor is different at every level of the outcome variable. Odds ratios in this study differed greatly across outcome levels for variables such as age and type of operation.
This study does have some limitations. Due to the retrospective character of the study design, selection bias may be present. Our large sample size, however, minimizes the effect of any selection bias. Although we attempted to control for selection bias with multivariable statistical methods, we cannot exclude bias due to unmeasured factors, including intraoperative variables that may influence the number of complications. In addition, our data were taken from an administrative database which presents the possibility for errors in reporting or coding for diagnoses, procedures, and cost related measures. Previous analysis of this database has indicated that these errors would be minimal. The discrimination AUC of 0.71 for the strength of association between several preoperative factors and the risk for each outcome category was only fair, but the model was built on a small set of readily available variables for simplicity and accessibility. We have developed an online calculator to calculate the probability for developing zero, one, two, or three or more complications and made it accessible at http://www.prisma-p.org Some of the definitions of the outcomes were arbitrary, particularly ICU stay greater than 48h and duration of mechanical ventilation greater than 48h. While the median ICU stay for patients in this study with no complications was 1 day which provides some justification for this choice, for many complicated procedures, such as open cardiac valve surgery, liver transplantation, and open aortic surgery, an ICU stay for greater than 48h would not be considered a complication. While changing the definitions of the outcomes might change some of the odds ratios, it would not invalidate the use of the model.
Conclusions
This study showed that a selection of readily available demographic and clinical variables are strongly associated with several important postoperative outcomes, and we developed a single scoring system using multinomial logistic regression and a set of these variables which can be used in clinical practice to risk-stratify patients. Given the association between greater number of postoperative complications and increased adverse outcomes and costs, there is a critical need for strategies to better identify preoperatively those patients at risk for postoperative complications. We have developed an online calculator that calculates the risk for each number of complications after major surgery. In describing this technique, we hope to provide a method for clinicians to better stratify patients preoperatively for operative procedures and to help clinicians to institute preventive measures early to decrease the number of complications and to improve outcomes.
Supplementary Material
Acknowledgments
We thank Gigi Lipori, MBA, Christine Bono, PhD, and Yue Du, MS for assistance with data retrieval. A.B. and T.O.B. were supported by Center for Sepsis and Critical Illness Award P50 GM-111152 from the National Institute of General Medical Sciences and by R01 GM110240 from the National Institute of General Medical Sciences. This work was supported in part by the NIH/NCATS Clinical and Translational Sciences Award to the University of Florida UL1 TR000064. A.B. has received a Vision Grant from the Society of Critical Care Medicine and research grants from Astute Medical, Inc. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Society of Critical Care Medicine. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. A.B. and T.O.B. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors report no conflict of interest.
Footnotes
Conflicts of Interest
The authors report no conflict of interest
The preliminary report from this research was presented as a poster presentation at the 43rd Annual Meeting of the Society of Critical Care Medicine
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Fast Stats: Inpatient Surgery. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [08/01/2013]. Available from: http://www.cdc.gov/nchs/fastats/insurg.htm. [Google Scholar]
- 2.Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126(1):66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 3.Kable AK, Gibberd RW, Spigelman AD. Adverse events in surgical patients in Australia. International journal for quality in health care : journal of the International Society for Quality in Health Care / ISQua. 2002;14(4):269–76. doi: 10.1093/intqhc/14.4.269. [DOI] [PubMed] [Google Scholar]
- 4.Moonesinghe SR, Mythen MG, Grocott MP. High-risk surgery: epidemiology and outcomes. Anesthesia and analgesia. 2011;112(4):891–901. doi: 10.1213/ANE.0b013e3181e1655b. [DOI] [PubMed] [Google Scholar]
- 5.Kohlnhofer BM, Tevis SE, Weber SM, Kennedy GD. Multiple complications and short length of stay are associated with postoperative readmissions. American journal of surgery. 2014 doi: 10.1016/j.amjsurg.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, et al. Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation. 2009;119(18):2444–53. doi: 10.1161/CIRCULATIONAHA.108.800011. [DOI] [PubMed] [Google Scholar]
- 7.Lin CC, Wu MY, Tsai FC, Chu JJ, Chang YS, Haung YK, et al. Prediction of major complications after isolated coronary artery bypass grafting: the CGMH experience. Chang Gung Med J. 2010;33(4):370–9. [PubMed] [Google Scholar]
- 8.Toumpoulis IK, Anagnostopoulos CE, Swistel DG, DeRose JJ., Jr Does EuroSCORE predict length of stay and specific postoperative complications after cardiac surgery? Eur J Cardiothorac Surg. 2005;27(1):128–33. doi: 10.1016/j.ejcts.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJ, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255(1):1–5. doi: 10.1097/SLA.0b013e3182402c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309(15):1599–606. doi: 10.1001/jama.2013.2773. [DOI] [PubMed] [Google Scholar]
- 11.Hobson CE, Ozrazgat-Baslanti T, Kuxhausen A, Thottakkara P, Efron PA, Moore FA, et al. Cost and Mortality Associated With Postoperative Acute Kidney Injury. Ann Surg. 2015;261(6):1207–14. doi: 10.1097/SLA.0000000000000732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arnaoutakis GJ, Bihorac A, Martin TD, Hess PJ, Jr, Klodell CT, Ejaz AA, et al. RIFLE criteria for acute kidney injury in aortic arch surgery. The Journal of thoracic and cardiovascular surgery. 2007;134(6):1554–60. doi: 10.1016/j.jtcvs.2007.08.039. discussion 60-1. [DOI] [PubMed] [Google Scholar]
- 13.Bihorac A, Yavas S, Subbiah S, Hobson CE, Schold JD, Gabrielli A, et al. Longterm risk of mortality and acute kidney injury during hospitalization after major surgery. Annals of Surgery. 2009;249(5):851–8. doi: 10.1097/SLA.0b013e3181a40a0b. [DOI] [PubMed] [Google Scholar]
- 14.Bihorac A, Brennan M, Ozrazgat-Baslanti T, Bozorgmehri S, Efron PA, Moore FA, et al. National surgical quality improvement program underestimates the risk associated with mild and moderate postoperative acute kidney injury. Crit Care Med. 2013;41(11):2570–83. doi: 10.1097/CCM.0b013e31829860fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gentile LF, Cuenca AG, Efron PA, Ang D, Bihorac A, McKinley B, et al. Persistent inflammation and immunosuppression: A common syndrome and new horizon for surgical intensive care. Journal of Trauma-Injury Infection & Critical Care. 2012;72(6):1491–501. doi: 10.1097/TA.0b013e318256e000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vanzant EL, Lopez CM, Ozrazgat-Baslanti T, Ungaro R, Davis R, Cuenca AG, et al. Persistent inflammation, immunosuppression, and catabolism syndrome after severe blunt trauma. J Trauma Acute Care Surg. 2014;76(1):21–9. doi: 10.1097/TA.0b013e3182ab1ab5. discussion 9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bihorac A, Delano MJ, Schold JD, Lopez MC, Nathens AB, Maier RV, et al. Incidence, clinical predictors, genomics, and outcome of acute kidney injury among trauma patients. Ann Surg. 2010;252(1):158–65. doi: 10.1097/SLA.0b013e3181deb6bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huber M, Ozrazgat-Baslanti T, Thottakkara P, Efron PA, Feezor R, Hobson CE, et al. Mortality and cost of acute and chronic kidney disease after vascular surgery. Annals of Vascular Surgery. 2015;29(4) doi: 10.1016/j.avsg.2015.04.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yende S, Linde-Zwirble W, Mayr F, Weissfeld LA, Reis S, Angus DC. Risk of cardiovascular events in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;189(9):1065–74. doi: 10.1164/rccm.201307-1321OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. Population burden of long-term survivorship after severe sepsis in older americans. J Am Geriatr Soc. 2012;60(6):1070–7. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Annals of Internal Medicine. 2010;153(3):167–75. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iwashyna TJ. Survivorship will be the defining challenge of critical care in the 21st century. Ann Intern Med. 2010;153(3):204. doi: 10.7326/0003-4819-153-3-201008030-00013. [DOI] [PubMed] [Google Scholar]
- 23.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA: The Journal of the American Medical Association. 2010;304(16):1787–94. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hopkins RO, Jackson JC. Short- and long-term cognitive outcomes in intensive care unit survivors. Clinics in Chest Medicine. 2009;30(1):143–53. ix. doi: 10.1016/j.ccm.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Korenkevych D, Ozrazgat-Baslanti T, Thottakkara P, Hobson CE, Pardalos P, Momcilovic P, et al. The Pattern of Longitudinal Change in Serum Creatinine and 90-Day Mortality After Major Surgery. Annals of Surgery. 2015 doi: 10.1097/SLA.0000000000001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vaught A, Ozrazgat-Baslanti T, Javed A, Morgan L, Hobson C, Bihorac A. Acute kidney injury in major gynaecological surgery: an observational study. BJOG : an international journal of obstetrics and gynaecology. 2014 doi: 10.1111/1471-0528.13026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White LE, Hassoun HT, Bihorac A, Moore LJ, Sailors RM, McKinley BA, et al. Acute kidney injury is surprisingly common and a powerful predictor of mortality in surgical sepsis. J Trauma Acute Care Surg. 2013;75(3):432–8. doi: 10.1097/TA.0b013e31829de6cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bihorac A, Schold JD, Hobson CE. Acute kidney injury and long-term outcomes: more to learn. Kidney International. 2010;77(8):745. doi: 10.1038/ki.2009.554. [DOI] [PubMed] [Google Scholar]
- 29.Bihorac A, Schold JD, Hobson CE. Long-term mortality associated with acute kidney injury requiring dialysis. JAMA. 2010;303(3):229. doi: 10.1001/jama.2009.1878. [DOI] [PubMed] [Google Scholar]
- 30.Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93(17):1577–82. doi: 10.2106/JBJS.J.01048. [DOI] [PubMed] [Google Scholar]
- 31.de Silva S, Ma C, Proulx MC, Crespin M, Kaplan BS, Hubbard J, et al. Postoperative Complications and Mortality Following Colectomy for Ulcerative Colitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2011;9(11):972–80. doi: 10.1016/j.cgh.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 32.Polanczyk CsA, Marcantonio E, Goldman L, Rohde LEP, Orav J, Mangione CM, et al. Impact of Age on Perioperative Complications and Length of Stay in Patients Undergoing Noncardiac Surgery. Annals of Internal Medicine. 2001;134(8):637–43. doi: 10.7326/0003-4819-134-8-200104170-00008. [DOI] [PubMed] [Google Scholar]
- 33.Saxton A, Velanovich V. Preoperative frailty and quality of life as predictors of postoperative complications. Ann Surg. 2011;253(6):1223–9. doi: 10.097/SLA.0b013e318214bce7. [DOI] [PubMed] [Google Scholar]
- 34.High R. Proceedings of the SAS Global Forum 2013 Conference. Cary, NC: SAS Institute Inc; [Accessed May 20, 2016]. Models for ordinal response data. Paper 445-2013. Available at http://support.sas.com/resources/papers/proceedings13/445-2013.pdf. [Google Scholar]
- 35.Vogel TR, Dombrovskiy VY, Carson JL, Graham AM, Lowry SF. Postoperative sepsis in the United States. Ann Surg. 2010;252(6):1065–71. doi: 10.97/SLA.0b013e3181dcf36e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agency for Healthcare Research and Quality. [April 9, 2012];Patient safety indicators:technical specifications. Ver 4.2. 2010 Available from: http://www.qualityindicators.ahrq.gov.19.
- 37.Lagu T, Rothberg MB, Shieh MS, Pekow PS, Steingrub JS, Lindenauer PK. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2012;40(3):754–61. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 38.U.S. Department of Veterans Affairs VHA. [03/03/2015];National Drug File – Reference Terminology (NDF-RT™) Documentation. 2015 Available from: http://evs.nci.nih.gov/ftp1/NDF-RT/NDF-RT%20Documentation.pdf.
- 39.Lin RY, Heacock LC, Fogel JF. Drug-induced, dementia-associated and nondementia, non-drug delirium hospitalizations in the United States, 1998-2005: an analysis of the national inpatient sample. Drugs & aging. 2010;27(1):51–61. doi: 10.2165/11531060-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.LaPar DJ, Bhamidipati CM, Mery CM, Stukenborg GJ, Jones DR, Schirmer BD, et al. Primary payer status affects mortality for major surgical operations. Annals of Surgery. 2010;252(3):544–50. doi: 10.1097/SLA.0b013e3181e8fd75. discussion 50-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004;239(1):43–52. doi: 10.1097/01.sla.0000103071.35986.c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.von Elm E, A D, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Annals of Internal Medicine. 2007;147(8):573–7. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 43.Agresti A. Analysis of ordinal categorical data. second. Hoboken, NJ: John Wiley & Sons, Inc; 2010. [Google Scholar]
- 44.Hand D, Till R. A Simple Generalisation of the Area Under the ROC Curve for Multiple Class Classification Problems. Machine Learning. 2001;45(2):171–86. [Google Scholar]
- 45.Armstrong BG, Sloan M. Ordinal regression models for epidemiologic data. Am J Epidemiol. 1989;129(1):191–204. doi: 10.1093/oxfordjournals.aje.a115109. [DOI] [PubMed] [Google Scholar]
- 46.Cande V, Ananth DGK. Regression Models for Ordinal Responses: A Review of Methods and Applications. International Journal of Epidemiology. 1997;26(6):1323–33. doi: 10.1093/ije/26.6.1323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


