Abstract
Introduction
The chemical components of olive fruit provide a wide range of cardiovascular benefits. Arterial stiffness is an important cardiovascular risk factor and can be assessed using the Cardio-Ankle Vascular Index (CAVI).
Objective
The objective of this study was to assess the impact of a proprietary standardized olive fruit extract (SOFE) in subjects at risk for arterial stiffness.
Methods
Twelve of 36 subjects were assigned to each of the following groups for this 11-day, double-blind, placebo-controlled study: Group 1: 250 mg SOFE—50 mg active ingredient, hydroxytyrosol (dosage achieved with two capsules per day); Group 2: 500 mg SOFE—100 mg active ingredient, hydroxytyrosol (dosage achieved with two capsules per day); and Group 3: placebo.
Results
All three groups showed a decrease in CAVI scores, although no significant between-group differences were observed. Group 2 had the largest reduction, with mean CAVI scores decreasing from 11.02 to 8.91. Group 2 showed the strongest response in visual analog scale (VAS) energy intensity (11.71% increase). Results for C-reactive protein (CRP) blood levels showed no changes of statistical significance between groups. Mean triglyceride levels from Group 2 decreased by 21.64%, the most significant change among all three groups.
Conclusions
SOFE, an olive fruit extract containing many of the phytochemicals shown to provide cardiovascular benefits, was safe and well-tolerated. SOFE 500 mg had a greater effect on CAVI scores, suggesting improved arterial elasticity, and a clear reduction in triglycerides compared with placebo and SOFE 250 mg. The decreased CAVI scores suggest that increasing high-density lipoprotein cholesterol and lowering triglycerides with SOFE could potentially reduce patients’ risk of developing atherosclerosis. Although more studies are needed, positive cardiovascular health trends, including improved vessel elasticity and positive triglyceride effects, were evident with SOFE.
Key Points
| Phenolic phytochemicals found in olive fruit are potent inhibitors of LDL oxidation, and this type of oxidation is considered to be a key mechanism in the development of atherosclerosis. |
| Arterial stiffness is a non-traditional cardiovascular risk factor, and long-term evidence has shown it to be a marker of all-cause and cardiovascular mortality, including fatal and non-fatal coronary events. |
| The decreased CAVI index suggests that increasing C-HDL and lowering triglycerides with SOFE could potentially reduce patients’ risk of developing atherosclerosis. |
Introduction
Background on Olive Fruit Oil
The chemical components of olive fruit have been studied extensively and shown to provide a wide range of cardiovascular benefits [1–6]. In addition to its high oleic acid content (which is considered to be ‘neutral’ in terms of cardioprotection) [7], substantial evidence indicates that the protective effects of olive oil can be ascribed to the antioxidant properties of its phenolic compounds (PCs), which are absent in seed oil [8–11]. One of those compounds, hydroxytyrosol, is a virgin olive fruit oil phenolic phytochemical with proven health benefits that has been used to generate new lipophilic antioxidants to preserve fats and oils against autoxidation [1].
In Vitro and Preclinical Studies of Olive Fruit Oil Phenolic Compounds (PCs)
In vitro studies have shown phenolics in olive fruit oil to be strong radical scavengers. In order to evaluate the comparative physiological effects of hydroxytyrosol and its lipophilic derivatives, hydroxytyrosol acetate and ethyl hydroxytyrosol ether, in high-cholesterol fed animals, Tabernero et al. [1] fed male Wistar rats (n = 8) a standard diet (C group), a cholesterol-rich diet (Chol group), or a cholesterol-rich diet supplemented with PCs (hydroxytyrosol group, hydroxytyrosol acetate group, and ethyl hydroxytyrosol ether group) for 8 weeks. Plasma levels of total cholesterol, low-density lipoprotein (LDL) cholesterol, glucose, insulin, and leptin, as well as malondialdehyde (MDA) in serum increased in Chol rats compared with C rats (P < 0.05). Rats fed the test diets containing hydroxytyrosol and its derivatives had improved glucose, insulin, leptin, and MDA levels and antioxidant capacity status, with hydroxytyrosol acetate being the most effective compound. The results confirmed the metabolic effects of hydroxytyrosol, which are maintained and even improved by its hydrophobic derivatives, particularly hydroxytyrosol acetate [1]. Studies in other animal models have shown that PCs extracted from extra virgin olive oil (hydroxytyrosol, tyrosol, and oleuropein) significantly inhibited the oxidation of LDL cholesterol [12–14].
In a randomized, crossover controlled trial involving 200 healthy male volunteers, Covas et al. [2] evaluated whether the phenolic content of olive oil, which includes hydroxytyrosol, further benefits plasma lipid levels and lipid oxidative damage compared with monounsaturated acid content. The study was conducted at six research centers in five European countries. A linear increase in high-density lipoprotein (HDL) cholesterol levels was observed for low-, medium-, and high-polyphenol olive oil. The total cholesterol: HDL cholesterol ratio decreased linearly with the phenolic content of the olive oil, and triglyceride levels decreased by an average of 0.05 mmol/L for all olive oils. Oxidative stress markers decreased linearly with increasing phenolic content. Mean changes for oxidized LDL levels were 1.21 U/L (95% confidence interval [CI] −0.8 to 3.6), −1.48 U/L (95% CI −3.6 to 0.6), and −3.21 U/L (95% CI −5.1 to −0.8) for the low-, medium-, and high-polyphenol olive oil, respectively. The investigators concluded that olive oil is more than a monounsaturated fat—its phenolic content can also benefit plasma lipid levels and provide protection from oxidative damage [2].
Clinical Studies of Olive Fruit Oil PCs
Verhoeven et al. [3] conducted a double-blind, placebo-controlled, randomized trial in 50 subjects with metabolic syndrome, as defined by ATP III (Adult Treatment Panel III) criteria. Patients received capsules containing 10.82 mg of monacolins and 9.32 mg of hydroxytyrosol or placebo for 8 weeks. In the intervention group, LDL cholesterol was lowered by 24%, whereas it increased by 1% in the control group (P < 0.001). Other effects observed were reductions in total cholesterol (−17% in the intervention group vs. +2% in the control group; P < 0.001), apolipoprotein B (−15% vs. +6%; P < 0.001), and triglycerides (−9% vs. +16%; P = 0.02). Oxidized LDL decreased by 20% in the intervention group and increased by 5% in the control group (P < 0.001). The investigators concluded that the combination of active products (which included hydroxytyrosol as well as the statin [HMG-CoA reductase inhibitor] monacolin) in this study may be an alternative therapeutic approach in people who do not need, cannot, or do not want to be treated with chemical statins [3].
A direct relation between cardiovascular diseases (CVDs) and oxidation of LDL is now well-established, and oxidation of LDL particles is strongly associated with the risk of coronary heart disease (CHD) and myocardial infarction [15].
Arterial Stiffness
Arterial stiffness is an important risk factor for cardiovascular morbidity and mortality [19], and can be assessed using several methods, including the Cardio-Ankle Vascular Index (CAVI). CAVI is a well-studied marker that is calculated from the pulse wave velocity (PWV) and adjusted to blood pressure (BP) values, and is therefore less dependent on changes in BP than conventional markers [16]. CAVI has been shown to be a biomarker for evaluating the severity of arterial fibrosis with higher sensitivity and specificity than PWV [16].
CAVI reflects the stiffness of arterial segments, including the aorta, femoral artery, and tibial artery. This index was originally derived from Bamwell-Hill’s equation and stiffness parameter β [17]. CAVI has been shown to be a marker for numerous cardiovascular risk factors, such as hypertension [18], diabetes mellitus [19], hyperlipidemia [20], smoking [21], and epicardial adipose tissue [22]. CAVI may also play a role as a surrogate marker of subclinical atherosclerosis, and substantial data have shown associations between CAVI and components of CVD, such as coronary atherosclerosis [19, 23], carotid atherosclerosis [24], and stroke [25, 26].
Miyoshi and colleagues [27] investigated the association of CAVI with coronary atherosclerosis and left ventricular (LV) systolic and diastolic function in 206 consecutive subjects with ischemic heart disease (IHD) undergoing coronary angiography. The investigators found CAVI to be independently associated with LV systolic and diastolic function as well as coronary artery disease in patients with IHD. The investigators concluded that determination of arterial stiffness using CAVI may be useful for risk stratification and secondary prevention in patients with IHD [27]. There is some indication that CAVI is also useful in evaluating atherogenic risks in metabolic syndrome [28].
The primary aims of assessing arterial stiffness using CAVI have not been merely to aid in early detection of atherosclerosis, arteriosclerosis, and other cardiovascular conditions, in order to allow timely treatment and change in lifestyle, but also to quantitatively evaluate the progression of disease and the effectiveness of treatment [29].
Based on the in vitro and clinical profiles of the phenolic phytochemicals that are found in olive fruit, we were interested in quantifying the impact on cardiovascular assessments of a proprietary standardized olive fruit extract (SOFE) [Proliva® (Euromed, Barcelona, Spain)] that contains many of those same PCs.
Study Objectives
This study was designed to assess and explore the beneficial effects of SOFE, specifically for CAVI score reductions and for exploratory purposes for other key analytes.
Primary Objective for Efficacy Evaluation
The primary objective of this study was to assess the impact of SOFE on the following in subjects with arterial stiffness:
CAVI.
Energy visual analog scale (VAS) questionnaire.
CRP (C-reactive protein).
Blood chemistry.
Endpoints
The primary study endpoints were the reduction and/or improvement of the following cardiovascular parameters:
CAVI reduction ≥7 ≤9.
Increase in energy assessed with a VAS questionnaire (exploratory).
CRP (exploratory).
The secondary exploratory endpoints were potentially positive outcomes on blood chemistry analytes (Table 1) that could be abnormal as a consequence of atherosclerotic risk, as assessed by CAVI prior to treatment.
Table 1.
Blood chemistry analytes
| Total cholesterol |
| Aspartate aminotransferase (AST) |
| Alkaline phosphatase |
| Uric acid |
| Potassium |
| Cholesterol HDL |
| Relation BUN/creatinine |
| Glucose |
| Alanine aminotransferase (ALT) |
| Total proteins (serum) |
| Calcium |
| Chlorine |
| Cholesterol LDL |
| Total bilirubin |
| BUN |
| Lactate dehydrogenase (LDH) |
| Albumin |
| Phosphorus |
| C02 calculated |
| COL T/HDL index |
| A/G relation |
| Creatinine |
| Gamma-glutamyl transpeptidase (GGTP) |
| Globulin |
| Iron |
| Triglycerides |
| LDL/HDL index |
| Sodium |
A/G albumin/globulin, BUN blood urea nitrogen, COL T total cholesterol, HDL high-density lipoprotein, IFCC Internal Federation of Clinical Chemistry and Laboratory Medicine, LDL low-density lipoprotein
Methodology
After protocol approval by the Institutional Review Board (IRB), 36 male and female subjects between 45 and 65 years of age were prescreened to confirm if they met the inclusion and exclusion criteria for this 11-day, double-blind, placebo-controlled study. We replicated the timeline from the pilot study (11 days) to be consistent with the initial design. Thirty-six subjects were selected to participate. For each subject, the study concluded 11 days after enrollment and included three follow-up visits (Days 0, 5, and 10).
Informed consent from each participant was obtained before they were administered the test articles. On Day 0 (baseline), the CAVI test, medical history, and physical examinations were performed on all subjects. Physical examination included measurements of body mass index (BMI), BP, and temperature. On Day 0, participants who did not meet the inclusion criteria were removed from the study. Participants not responding to phone calls within a 3-day period after the previous call were excluded. On Day 0, participants in both groups initiated the 11-day treatment (Table 2).
Table 2.
Study visits schedule
| Description | Prescreening (124 subjects) | Study (36 subjects) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | Day 9 | Day 10 | All days of treatment | ||
| Informed consent | X | ||||||||||||
| Medical history | X | ||||||||||||
| BMI | X | ||||||||||||
| Blood pressure | X | X | X | X | |||||||||
| Physical examination | X | X | X | X | |||||||||
| CAVI | X | X | X | ||||||||||
| Blood chemistry | X | X | X | ||||||||||
| VAS | X | X | X | ||||||||||
| Serum samples 5 mL each (divided in 2 vials) T0 min | X | X | X | ||||||||||
| Subject test article consumption | X | X | X | X | X | X | X | X | X | X | X | X | |
| Project managers: treatment follow-up log sheets | X | X | X | X | X | X | X | X | X | X | X | X | |
| Project managers: concomitant medication log sheets | X | X | X | X | X | X | X | X | X | X | X | X | |
| Randomization | X | ||||||||||||
| Test article delivery | X | ||||||||||||
| Adverse events | X | ||||||||||||
BMI body mass index, CAVI cardio-ankle vascular index, VAS visual analog scale
Project managers followed up with all patients when treatment was competed. If an adverse event occurred after study completion, the subject was evaluated by the physician and the evaluation recorded in the Adverse Event Form.
To enable evaluation of the test article in the context of the patient’s normal diet, the study design precluded lifestyle changes such as restricting or encouraging the consumption of olive oil or any other product that may have affected study results. This applied to both treatment groups.
Test Articles
The test articles in this study were presented as follows:
Capsules marked as HFGBVHFD: white bottles containing 24 capsules each.
Capsules marked as QEDWESDA: white bottles containing 24 capsules each.
Capsules marked as OILKOJPUL: white bottles containing 24 capsules each.
The active ingredient in the SOFE formulation was hydroxytyrosol.
Test articles for this study were supplied/labeled as follows:
HFGBVHFD: 125 mg SOFE/each; dose: two capsules per day (hydroxytyrosol 50 mg).
QEDWESDA: 250 mg SOFE/each; dose: two capsules per day (hydroxytyrosol 100 mg).
OILKOJPUL: placebo; dose: two capsules per day.
Coded capsules were identical in appearance and were packed in identical bottles labeled with the patient number, treatment code, and appropriate period of the study. This ensured that all study personnel as well as all subjects remained blinded to the treatments during the double-blind treatment periods.
Study Subjects
Inclusion Criteria
Inclusion criteria were as follows:
Age range: ≥45 and ≤65 years.
BMI >22 and <28 kg/m2.
CAVI score ≥9.
Free of allergies.
Non-diabetic.
Written informed consent to participate in the 11-day study.
Exclusion Criteria
Exclusion criteria were as follows:
Age <45 and >65 years.
BMI ≤22 and ≥28.
CAVI score <9.
Diabetes.
Female subjects who were pregnant, nursing, or planning to get pregnant.
Subjects participating in another study.
Subjects with CVDs.
Subjects using anti-inflammatory or analgesic medications such as non-steroidal anti-inflammatory drugs (NSAIDs) within 15 days prior to study initiation.
Subjects using statins, antidiabetic drugs, or anti-allergy medicines.
Subjects taking systemic antibiotics or any other treatment that, in the opinion of the investigator, could affect the results of the study.
Subjects receiving treatment for glucose control.
Subjects not providing written informed consent to participate in the 11-day study.
Withdrawal Criteria
Subjects meeting any of the following criteria were to be withdrawn from the study:
Request from the subject to be removed from the study.
Request from the investigator to remove a subject from the study.
Serious adverse events where continuation posed a health risk to the subject.
Subject had not agreed to consume the test article.
Subject consumed excluded medications or supplements.
Drop Out/Lost to Follow-Up Criteria
Subjects were considered to be dropouts if they failed to:
answer daily calls from the project manager for 3 consecutive days; or
appear at one of the three site visits.
Blinding and Randomization
All project managers and all subjects were blinded. A total of 36 subjects were recruited to participate in this study. After the observation period, the groups were paired by CAVI scores.
Each subject satisfying the inclusion and exclusion criteria was assigned to one of the following study groups:
Group 1: hydroxytyrosol 50 mg (n = 12).
Group 2: hydroxytyrosol 100 mg (n = 12).
Group 3: placebo (n = 12).
Appropriateness of Measurements
Cardio-Ankle Vascular Index (CAVI)
As mentioned in Sect. 1.4, CAVI is a marker of arterial stiffness calculated from the PWV and adjusted to BP values, and is therefore less dependent on changes in BP than conventional markers [16]. CAVI has also been shown to be a biomarker for evaluating the severity of arterial fibrosis with higher sensitivity and specificity than PWV [16]. CAVI was implemented in this study using a VaSera VS-1000 vascular screening system (Fukuda Denshi Co. Ltd., Tokyo, Japan). Cuffs were applied to bilateral upper arms and ankles, with subjects lying in a supine position and holding their heads along the midline. ECG electrodes were placed on both wrists, and the CAVI microphone for detecting heart sounds was placed over the sternum. Subjects rested in this supine position for at least 10 min before the start of monitoring. CAVI was calculated using the following formula (Eq. 1):
| 1 |
where, P s is systolic BP, P d is diastolic BP, ∆P is P s − P d, p is blood density, and a and b are constants.
Visual Analog Scale (VAS) Questionnaire
VAS questionnaires have been used since the 1920s to measure subjective phenomena due to their brevity, universality, and ease of use and scoring [30]. Combined with research showing that the performance of single-item VAS questionnaires rivals that of longer questionnaires with respect to correlation with clinical variables and sensitivity to change [31], the above-described properties have led to widespread use of VAS questionnaires in both clinical medicine and research. For example, VAS questionnaires have shown great utility in measuring numerous symptoms relevant to fibromyalgia, including energy, satiety, functional ability, and pain [30].
VAS questionnaires measuring fatigue have also been shown to be highly reproducible and sensitive for quantifying symptom severity and treatment response in multiple patient populations [31]. They focus on the current phenomena, providing a subjective assessment for each subject; the underlying causes of those phenomena are excluded from the assessment.
The following VAS questions were used to measure energy:
Intensity of energy right now?
Fatigue intensity right now?
Appetite intensity right now?
Feeling warm right now?
Stomach discomfort right now?
How satisfying did you find the study product, in general?
Each VAS questionnaire consisted of 100 mm horizontal lines containing the extreme sensations at either end, as shown in Fig. 1. Subjects completed the VAS questionnaire by placing a vertical slash on the line corresponding to their sensation.
Fig. 1.
Example of the visual analog scale questionnaire used in this study
C-Reactive Protein (CRP)
CRP has been the most widely used biomarker for quantifying inflammation in CVD [32–35] and is the only reproducible indicator for which a standardized assay has been developed [36, 37].
All CRP tests used the immunoturbidimetric method, and were carried out by Laboratorio Clínico Centro Integral de Diagnóstico Médico, an independent analytical laboratory based in Guadalajara, Mexico.
Blood Chemistry
A long-standing association exists between elevated triglyceride levels and CVD [38, 39]. However, the extent to which triglycerides directly promote CVD or represent a biomarker of risk has been debated for 3 decades [40]. To this end, two National Institutes of Health consensus conferences evaluated the evidentiary role of triglycerides in cardiovascular risk assessment and provided therapeutic recommendations for the management of hypertriglyceridemia [41, 42].
In the present study, all blood chemistry analytes, including triglycerides, were evaluated as exploratory endpoints. Blood chemistry tests and measurement methods are displayed in Table 3.
Table 3.
Blood chemistry tests and measurement methods
| Analyte | Test method | Measurement method |
|---|---|---|
| C-reactive protein (CRP) | Immunotherapy | Immunoturbidimetry |
| Triglycerides | Trinder (Wahlefeld) | Enzymatic colorimetry |
| Total cholesterol | Trinder (Roeschlaub & Allain) | Enzymatic colorimetry |
| Cholesterol HDL | Polyethylene glycol | Enzymatic colorimetry |
| Cholesterol LDL | Cholesterol esterase | Enzymatic colorimetry |
| Uric acid | Uricase | Enzymatic colorimetry |
| Albumin | Bromocresol green | Photometry and colorimetry |
| Total bilirubin | Wahlefeld (DPD) | Photometry and colorimetry |
| Calcium | RX-O-cresolphthalein complexone | Enzymatic colorimetry |
| Creatinine | Jaffe (picric acid) | Kinetic colorimetry |
| Iron | Ferrozine (no-deproteinization) | Colorimetry |
| Phosphorus | RX—phosphate with ammonium molybdate | Photometry |
| Total proteins (serum) | Biuret | Colorimetry |
| Alanine aminotransferase (ALT) | IFCC C/S activation by pyridoxal phosphate | UV |
| Aspartate aminotransferase (AST) | IFCC C/S activation by pyridoxal phosphate | UV |
| Gamma-glutamyl transpeptidase (GGTP) | IFCC | Enzymatic colorimetry |
| Lactate dehydrogenase (LDH) | Optimized assay | UV |
DPD 2,5-dichlorophenyldiazonium tetrafluoroborate, HDL high-density lipoprotein, IFCC International Federation of Clinical Chemistry and Laboratory Medicine, LDL low-density lipoprotein, UV ultraviolet
Treatment Compliance
To ensure treatment compliance, adequate instructions regarding treatment administration, study procedures, and informed consent were given to participants prior to study initiation. A project manager was assigned to follow-up with all subjects daily to evaluate treatment progress.
Data Quality Assurance
Project managers and their assistants were provided with detailed instructions on protocol conduct prior to study initiation. The study was monitored regularly, and at each monitoring visit all documentation and CRF entries were verified for accuracy. The quality assurance monitor ensured that the project managers maintained accurate, timely, and complete records.
Statistical Methods
Continuous quantitative variables were presented as the mean with standard deviation. To assess changes between different measurements of the study variables, non-parametric tests were used (Wilcoxon rank test). Continuous quantitative variables were evaluated using the Kruskal–Wallis method. The intragroup difference was calculated using the Wilcoxon rank test.
Sample Size
The sample size was selected based on the assumption that using a sample size four times that of a previous pilot study would be sufficient.
Protocol Deviations
Clinical sites worked under Good Clinical Practice (GCP) guidelines. As standard procedure, all protocol deviations during the study were to be documented. The Sponsor and IRB were to receive copies of the Note to Study and Deviation Form(s), when applicable. After each notification had been made, a CAPA (Corrective and Preventive Action) form was to be included in the Quality Assurance Report, and appropriate follow-up implemented according to standard operating procedures. There were no protocol deviations in this study.
Ethics Statement
This study was conducted in accordance with the ethical principles that have their origin in the 1964 Declaration of Helsinki, and that are consistent with GCP and the applicable regulatory requirement(s). Clinical sites followed ICH Good Clinical Practices (E6), which were developed under the Helsinki Declaration. All personnel involved in this study had been certified with GCP training.
The study was conducted in accordance with all applicable regulatory requirements. Prior to study initiation, the study protocol was submitted to an independent IRB, Investigación Biomédica para el Desarrollo de Fármacos SA de CV, Zapopan, Jalisco, México. The study commenced after an affirmative decision of the IRB concerning the conduct of the study was sent in writing to the investigator. Freely given informed consent was obtained from study participants.
Results
Efficacy
CAVI Evaluations
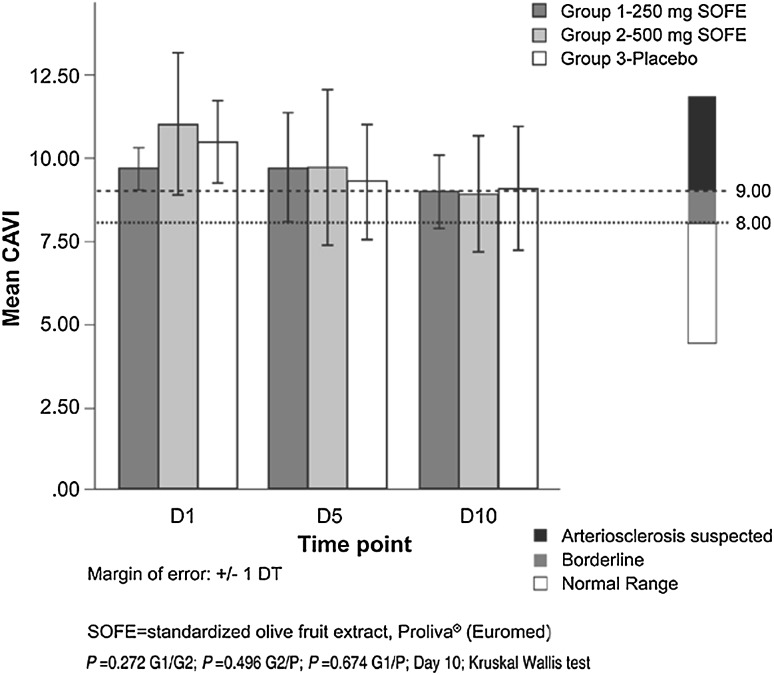
No significant differences were observed in CAVI scores between the control and SOFE groups at the end of treatment. All three groups showed a decrease in CAVI scores. Mean CAVI scores in Group 2 decreased by 2.11 CAVI points from baseline (19.14%) after the 11-day treatment period. Group 2 had the largest reduction among all three groups. Mean CAVI scores for Group 2 decreased from 11.02 (suspected arteriosclerosis) at baseline to 8.91 (borderline) at the end of the 11-day treatment period (Figs. 2 and 3).
Fig. 2.
Cardio-ankle vascular index (CAVI) scores. D1 Day 1, D5 Day 5, D10 Day 10
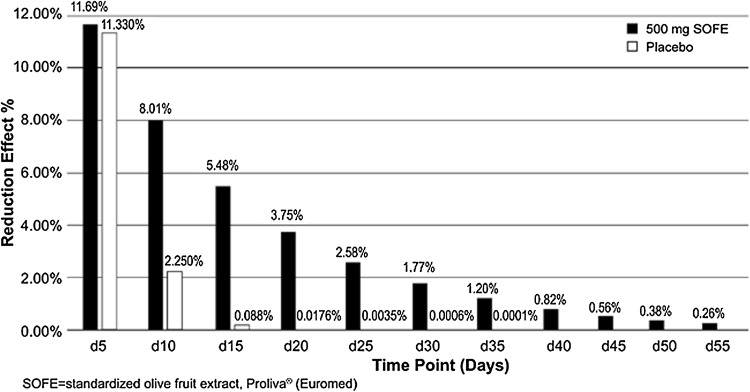
Fig. 3.
Cardio-ankle vascular index: progressive percentage of reduction effect. Projections from Day 15 to Day 55 are only estimations based on the percentage variation taken from study Day 10 with respect to Day 5. Results may vary from subject to subject and from group to group in a study with a larger sample size and a longer treatment period. Many other objective and subjective factors may affect the outcome of the results of a larger study
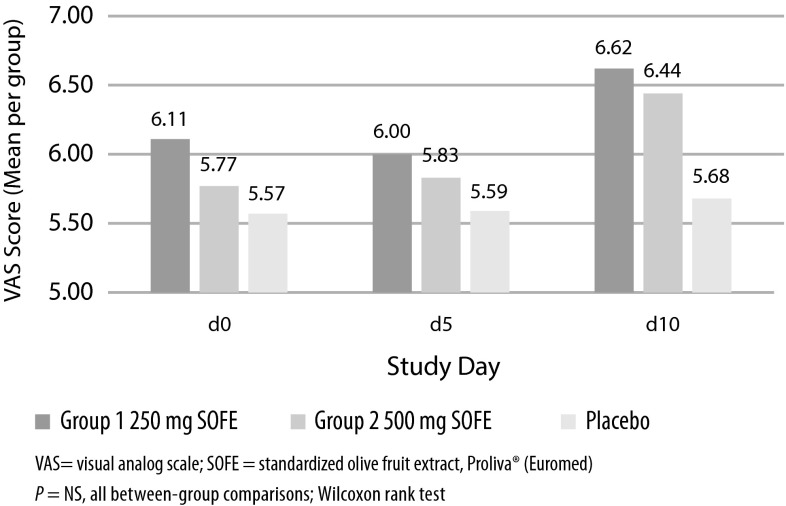
VAS Evaluations
There were no statistically significant changes between the three study groups. Group 2 showed the strongest response in energy intensity (Fig. 4), with an 11.71% increase from baseline, followed by Group 1 (8.32% increase) and placebo (2.10% increase): Group 1 (SOFE 250 mg) showed a reduction of 1.77% in energy intensity levels on Day 5 compared with Day 0, and an increase of 10.28% on Day 10 compared with Day 5. Overall, Group 1 showed an increase of 8.32% in energy intensity levels on Day 10 versus Day 0.
Fig. 4.
Visual analog scale energy intensity
Group 2 (SOFE 500 mg) showed an increase of 1.01% in energy intensity levels on Day 5 compared with Day 0, and an increase of 10.59% on Day 10 compared with Day 5. Overall, Group 2 showed an increase of 11.71% in energy intensity levels on Day 10 versus Day 0.
Group 3 (Placebo) showed an increase of 0.45% in energy intensity levels on Day 5 compared with Day 0, and an increase of 1.64% on Day 10 compared with Day 5. Overall, Group 3 showed an increase of 2.10% in energy intensity levels on Day 10 compared with Day 0.
CRP Evaluations
Group 1 (SOFE 250 mg) showed a reduction of 37.5% in CRP blood levels on Day 5 compared with Day 0 and an increase of 47.42% on Day 10 compared with Day 5. Overall, Group 1 showed a reduction of 7.85% in CRP blood levels on Day 10 compared with Day 0.
Group 2 (SOFE 500 mg) showed a reduction of 8.141% in CRP blood levels on Day 5 compared with Day 0, and an increase of 22.16% on Day 10 compared with Day 5. Overall, Group 2 showed an increase of 12.21% in CRP blood intensity levels on Day 10 compared with Day 0. Group 3 (placebo) showed a reduction of 1.43% in CRP blood levels on Day 5 compared with Day 0, and an increase of 1.94% on Day 10 compared with Day 5. Overall, Group 3 showed an increase of 0.47% in CRP blood levels on Day 10 compared with Day 0.
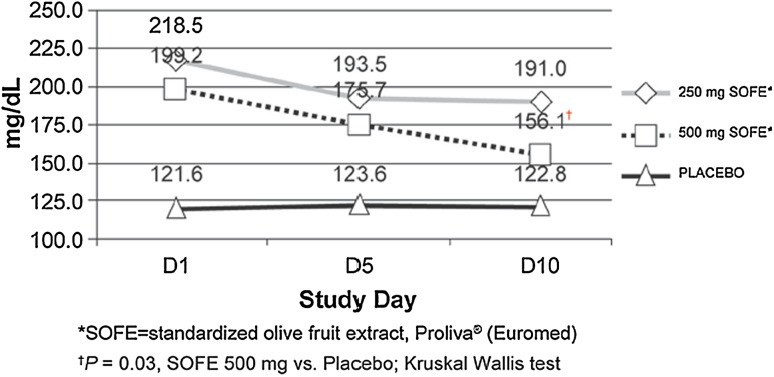
Blood Chemistry Evaluations
Mean serum triglyceride levels from Group 2 (SOFE 500 mg) decreased by 21.64% after the 11-day treatment period, showing the most significant change among all three groups (Fig. 5). Other blood chemistry results were unchanged or remained within the normal range and are displayed in Table 4.
Fig. 5.
Effects of treatment on serum triglyceride levels
Table 4.
Blood chemistry: percentage change
| Analyte | Units | Group 1: 250 mg SOFE | Group 2: 500 mg SOFE | Placebo | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| D0: baseline | D10: final | % change | D0: baseline | D10: final | % change | D0: baseline | D10: final | % change | ||
| Glucose | mg/dL | 96.40 | 92.80 | −3.73 | 98.60 | 105.97 | 7.47 | 83.70 | 85.96 | 2.70 |
| Uric acid | mg/dL | 5.50 | 5.90 | 7.27 | 5.70 | 5.90 | 3.51 | 4.90 | 5.14 | 4.90 |
| Cholesterol | mg/dL | 180.70 | 195.40 | 8.14 | 204.90 | 205.88 | 0.48 | 176.40 | 177.34 | 0.53 |
| Triglycerides | mg/dL | 204.10 | 191.00 | −6.42 | 199.20 | 156.09 | −21.64 | 124.00 | 127.01 | 2.43 |
| HDL | mg/dL | 47.90 | 47.90 | 0.00 | 44.00 | 47.42 | 7.77 | 41.90 | 43.26 | 3.25 |
| LDL | mg/dL | 117.90 | 117.90 | 0.00 | 135.10 | 133.02 | −1.54 | 123.90 | 123.00 | −0.73 |
| Urea | mg/dL | 29.80 | 32.00 | 7.38 | 34.40 | 34.31 | −0.26 | 34.93 | 35.87 | 2.69 |
| Creatinine | mg/dL | 0.75 | 0.82 | 9.33 | 0.94 | 0.94 | 0.00 | 0.80 | 0.81 | 0.63 |
| BUN | mg/dL | 13.50 | 14.85 | 10.00 | 16.10 | 16.15 | 0.31 | 16.32 | 16.74 | 2.57 |
| Total bilirubin | mg/dL | 0.42 | 0.49 | 16.67 | 0.41 | 0.51 | 24.39 | 0.43 | 0.41 | −4.65 |
| AST | µ/L | 27.60 | 33.08 | 19.86 | 28.00 | 25.17 | −10.11 | 23.10 | 23.98 | 3.81 |
| ALT | µ/L | 34.60 | 39.05 | 12.86 | 38.40 | 34.02 | −11.41 | 30.04 | 27.00 | −10.12 |
| LDH | µ/L | 316.90 | 316.00 | −0.28 | 329.50 | 321.60 | −2.40 | 323.00 | 315.60 | −2.29 |
| ALP | µ/L | 68.20 | 68.20 | 0.00 | 94.30 | 95.00 | 0.74 | 91.00 | 88.80 | −2.42 |
| GGTP | µ/L | 56.90 | 60.92 | 7.07 | 106.00 | 99.07 | −6.54 | 34.90 | 33.74 | −3.32 |
| Total proteins | g/dL | 6.70 | 7.36 | 9.85 | 7.00 | 7.51 | 7.29 | 7.10 | 7.09 | −0.14 |
| Albumin | g/dL | 4.30 | 4.38 | 1.86 | 4.20 | 4.39 | 4.52 | 4.10 | 4.27 | 4.15 |
| Globulin | g/dL | 3.00 | 2.97 | −1.00 | 2.80 | 3.12 | 11.43 | 2.90 | 2.91 | 0.34 |
| A/G Rxn | 1.40 | 1.49 | 6.43 | 1.50 | 1.45 | −3.33 | 1.40 | 1.40 | 0.00 | |
| Iron | µg/dL | 92.10 | 116.24 | 26.21 | 105.80 | 104.22 | −1.49 | 93.90 | 91.07 | −3.01 |
| Calcium | mg/dL | 9.60 | 9.60 | 0.00 | 9.10 | 9.51 | 4.51 | 9.40 | 9.46 | 0.64 |
| Phosphorous | mg/dL | 3.26 | 3.55 | 8.90 | 3.00 | 3.49 | 16.33 | 3.07 | 3.44 | 12.05 |
| Sodium | mmol/L | 142.00 | 141.25 | −0.53 | 141.60 | 140.33 | −0.90 | 130.30 | 129.17 | −0.87 |
| Potassium | mmol/L | 4.50 | 4.62 | 2.67 | 4.30 | 4.42 | 2.79 | 19.20 | 16.88 | −12.08 |
| Chlorine | mmol/L | 101.50 | 99.30 | −2.17 | 99.10 | 99.05 | −0.05 | 92.80 | 92.66 | −0.15 |
P = 0.102 to 0.789; Kruskal–Wallis test
A/G Rxn albumin/globulin relation, ALP alkaline phosphatase, ALT alanine aminotransferase, AST alanine aminotransferase, BUN blood urea nitrogen, D0 Day 0, D10 Day 10, GGTP gamma-glutamyl transpeptidase, HDL high-density lipoprotein, LDH lactate dehydrogenase, LDL low-density lipoprotein, SOFE standardized olive fruit extract (Proliva® [Euromed])
Adverse Events
Pharmacological intervention with SOFE at both doses (250 and 500 mg) produced results that were similar to those of placebo. Patient profiles of liver and kidney function were not significantly changed during the 11 days of treatment. Both active treatment groups were equally exposed to SOFE, and recorded similar electrolytic profiles, indicating that, for 11 days, treatment with SOFE was as safe as placebo regarding function of the kidney, the organ responsible for homeostasis of the body’s electrolyte system. These results were consistent with those of the protein profile, as the bioavailabilities of albumin and globulin did not change significantly during the study. No adverse events were reported in laboratory tests.
In general terms, oral ingestion of SOFE in a range of 250–500 mg was administered safely for 11 days to patients with significant arterial stiffness and at risk for atherosclerosis (CAVI scores ≥9).
Discussion
Review of Key Results
In this study, all three groups showed a decrease in CAVI scores, although no significant differences were observed between the control and SOFE groups at the end of treatment. Group 2 had the largest reduction among all three groups, with mean CAVI scores decreasing from 11.02 (suspected arteriosclerosis) at baseline to 8.91 (borderline) at the end of the 11-day treatment period.
Although there were no statistically significant changes between the three study groups in the VAS evaluation, the data show trends that can be taken into consideration when designing a longer study by including a larger sample size.
Group 2 showed the strongest response in energy intensity, with an 11.71% increase from baseline.
Results for CRP blood levels showed no changes of statistical significance between groups, and no trends could be determined. A larger study sample would be needed to assess variation between timepoints individually for each study group and variation between groups.
Mean triglyceride levels from Group 2 (SOFE 500 mg) decreased by 21.64% after the 11-day treatment period, showing the most significant change among all three groups (P = 0.03 vs. placebo). Other blood chemistry results were unchanged, remaining within normal limits.
A number of trials provide added insight to the clinical utility of phenolic phytochemicals, and are consistent with the findings of the present study.
Relevant Clinical Trials of Olive Oil
As noted in Sect. 1.2, PCs present in virgin olive oil (e.g., tyrosol, hydroxytyrosol, and oleuropein) have shown anti-inflammatory and antioxidative effects in CVD. The PCs in virgin olive oil may explain some of the protective effects found in epidemiological studies [43].
Moreno-Luna et al. [6] conducted a double-blind, randomized, crossover dietary intervention study to examine the influence of a polyphenol-rich olive oil on BP and endothelial function in 24 young women with high-normal BP or stage 1 essential hypertension, and concluded that the consumption of a diet containing polyphenol-rich olive oil can decrease BP and improve endothelial function in this population.
Estruch et al. [44] conducted a multicenter randomized trial to evaluate the Mediterranean diet for the primary prevention of cardiovascular events. The investigators randomly assigned participants who were at high cardiovascular risk, but with no CVD at enrollment, to one of the following three diets: a Mediterranean diet supplemented with extra-virgin olive oil, a Mediterranean diet supplemented with mixed nuts, or a control diet (advice to reduce dietary fat). The rate of major cardiovascular events (myocardial infarction, stroke, or death from cardiovascular causes) was the primary endpoint. Based on the results of an interim analysis, the trial was stopped after a median follow-up of 4.8 years. A total of 7447 subjects were enrolled (age range 55–80 years); 57% were female. A primary endpoint event occurred in 288 participants. The multivariable-adjusted hazard ratios were 0.70 (95% CI 0.54–0.92) and 0.72 (95% CI 0.54–0.96) for subjects receiving the Mediterranean diet with extra-virgin olive oil (96 events) and those assigned to the Mediterranean diet with nuts (83 events), respectively, compared with the control group (109 events). The investigators concluded that among subjects at high cardiovascular risk, a Mediterranean diet supplemented with extra-virgin olive oil or nuts reduced the incidence of major cardiovascular events, and that the primary between-group differences involved the supplemental items. The investigators added that “extra-virgin olive oil and nuts were probably responsible for most of the observed benefits of the Mediterranean diets” [44].
Similarly, although the high ratio of unsaturated to saturated fats found in the Mediterranean diet may contribute to its substantial benefits in CHD, it appears that olive oil may be working in other ways as well. The antioxidant activities of its PCs, shown to inhibit key elements in the pathogenesis of heart disease, are very likely important [43].
Relevant Clinical Trials of Other Fruit Products Containing PCs
Although lacking polyphenols, white wine contains PCs such as tyrosol and hydroxytyrosol, which are characteristic of extra-virgin olive fruit oil, and, as detailed in Sect. 1.2, share similar antioxidant and anti-inflammatory properties [7]. The effects of white wine and extra-virgin olive fruit oil on inflammatory markers was evaluated in ten healthy volunteers and ten patients with chronic kidney disease (CKD), KDOQI (Kidney Disease Outcomes Quality Initiative) stage III–IV, in a prospective, single-blind, randomized, crossover trial. Plasma markers of chronic inflammation were significantly reduced in CKD patients during the combined consumption of white wine and olive fruit oil, suggesting a possible anti-inflammatory effect of this nutritional intervention [45].
In another trial, vascular function testing and microarray analysis were performed by Yonei et al. [46] to evaluate the physical effects of cassis (Ribes nigrum) juice, which contains polyphenols, in healthy women assigned to one of four cassis groups (polysaccharide content: 0, 50, 125, and 250 mg) or a water control group (duration of intake: 2–8 weeks). The following were used to assess vascular function: CAVI, ankle-brachial pressure index (ABPI), accelerated plethysmography, and flow-mediated dilation (FMD). Cassis juice (polysaccharide content: 125–250 mg) (n = 16) increased the body fat percentage (+2.5%; P = 0.011), decreased systolic (121.3 ± 15.8 mmHg at baseline, −4.8%; P = 0.001) and diastolic (76.9 ± 11.2 mmHg at baseline, −5.9%; P = 0.001) BP, and increased FMD blood flow (P = 0.004) and upper (+0.23 ± 0.47 °C; P = 0.011) and lower (+0.55 ± 0.50 °C; P < 0.001) limb temperature. The percentage increase in lower limb temperature was dependent on polysaccharide (P < 0.05) and polyphenol (P < 0.01) contents. The investigators concluded that cassis juice induced limb peripheral vasodilatation, increased in blood flow, and decreased BP. Coupled with the role that vascular endothelium plays in vasodilatation associated with various messenger RNA expressions, the investigators suggested that polyphenol-containing cassis juice may also improve endothelial cell function [46].
Interpretation of Relevant Data by Regulatory Agencies
Following a request from the European Commission, the Panel on Dietetic Products, Nutrition and Allergies was asked to provide a scientific opinion to address the substantiation of health claims for polyphenols contained in olive oil products. The food constituent, which is the subject of the health claims, is polyphenols (e.g., hydroxytyrosol and oleuropein complex) contained in olive (olive fruit, olive mill waste waters or olive oil, Olea europaea L. extract and leaf).
The Panel reported that polyphenols in olive products that are standardized by their content of hydroxytyrosol and its derivatives are sufficiently characterized in relation to the effects claimed by their manufacturers. On the basis of the data presented, the Panel concluded that a cause and effect relationship has been established between the consumption of standardized olive oil polyphenols and protection of LDL particles from oxidative damage. The Panel noted that, in order to realize the benefits of that claim, 5 mg of hydroxytyrosol and its derivatives (e.g., oleuropein complex and tyrosol) derived from olive oil should be consumed daily. These amounts, if provided through moderate amounts of olive oil, can be easily consumed in the context of a balanced diet. The Panel further noted that concentrations in some olive oils may be too low to allow the consumption of this amount of polyphenols in the context of a balanced diet [47].
Atherosclerosis, Arterial Stiffness, and CAVI
Atherosclerosis is a chronic inflammatory disease that develops in lesion-prone regions of medium-sized arteries. Atherosclerotic lesions may be present and clinically silent for decades before becoming active and producing pathological conditions such as acute myocardial infarction, unstable angina, or sudden cardiac death [48].
As indicated in Sect. 1.4, arterial stiffness is a non-traditional cardiovascular risk factor, and long-term evidence has shown it to be a marker of all-cause and cardiovascular mortality, including fatal and non-fatal coronary events [49, 50].
Nakamura et al. [23] found a strong association between CAVI and the presence of coronary atherosclerosis based on their ordinal logistic regression analysis. Kadota et al. [51] suggested the use of CAVI as a screening tool for atherosclerosis based on their findings from a general population study of 1014 adults that showed strong significant associations of CAVI scores with carotid intima-media thickness and with homocysteine, after adjustment for age and sex [51]. Accordingly, it can be concluded that CAVI scores reflect arterial stiffness, atherosclerosis and arteriosclerosis—conditions that are overlapping and inseparable [52].
As noted in Sect. 1.2, phenolic phytochemicals found in olive fruit are potent inhibitors of LDL oxidation, and this type of oxidation is considered to be a key mechanism in the development of atherosclerosis [53]. Other mechanisms by which polyphenols may be protective against CVDs are antioxidant, antiplatelet, and anti-inflammatory effects as well as increasing HDL, and improving endothelial function [54]. Polyphenols may also contribute to stabilization of atheroma plaque [15].
Limitations of the Present Study
Based on the trends seen in this study, a longer treatment period with a larger sample size may more accurately define the placebo effect as well as the full extent of SOFE efficacy. For example, had the period of treatment been extended, it is likely that the trend for the core values would have continued, as was the case in a study by Satoh et al. [28] in which the CAVI score continued to fall for 12 weeks following oral intake of 1.8 g of highly purified eicosapentaenoic acid [28]. Similarly, the effects of pitavastatin (an inhibitor of HMG-CoA reductase) in lowering the rear CAVI consumption index were sustained for 12 months in a clinical trial by Miyashita et al. [55].
These results were consistent with data reported by the same research group regarding the effect of the angiotensin II blocker olmesartan medoxomil (20 mg/day orally) and the calcium channel blocker amlodipine (5 mg/day orally) administered for the same time interval [56].
In addition, a study cohort of 90–120 subjects might be required to demonstrate statistical significance between groups at the P > 0.05 level in a future trial following the same methods.
Conclusions
In the present study, the intake of 250 and 500 mg oral SOFE, an olive fruit extract containing many of the PCs shown to provide a wide range of cardiovascular benefits, was safe and well-tolerated over 11 days, based on the results of analyses of blood chemistry and blood metabolites. Although there were no statistically significant changes versus baseline for the acute and extended measurements at Day 11, oral administration of SOFE 500 mg had a greater effect on CAVI scores, suggesting improved arterial elasticity, and a clear reduction in triglycerides compared with placebo and SOFE 250 mg.
The decreased CAVI scores reported in the present study suggest that increasing HDL cholesterol and lowering triglycerides with SOFE could potentially reduce patients’ risk of developing atherosclerosis. The minimal improvements seen in the placebo group indicate that, in patients not exposed to the SOFE contained in Proliva®, the parameters of primary and secondary efficacy did not change.
Although more studies are needed, positive cardiovascular health trends, including improved vessel elasticity and positive triglyceride effects, were evident with SOFE.
Acknowledgements
This study was sponsored by Euromed, Barcelona, Spain. The authors thank NutraClinical, Inc., San Diego, CA, USA for their contributions to the design and conduct of this study, as well as for data analyses and data reporting. The authors also thank Aesculapius Consulting, Inc. for editorial assistance in developing this manuscript. Support for this assistance was provided by Euromed.
Compliance with Ethical Standards
Conflicts of interest
PP, AV, and SR are employed by Euromed, which funded this study. The authors report no other conflicts of interest in this work.
Author participation
Each of the authors participated in the data collection, data organization, and/or writing of this manuscript.
Funding
This study was funded by Euromed, Barcelona, Spain.
References
- 1.Tabernero M, Sarriá B, Largo C, et al. Comparative evaluation of the metabolic effects of hydroxytyrosol and its lipophilic derivatives (hydroxytyrosyl acetate and ethyl hydroxytyrosyl ether) in hypercholesterolemic rats. Food Funct. 2014;5:1556–1563. doi: 10.1039/c3fo60677e. [DOI] [PubMed] [Google Scholar]
- 2.Covas MI, Nyyssönen K, Poulsen HE, et al. The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann Intern Med. 2006;145:333–341. doi: 10.7326/0003-4819-145-5-200609050-00006. [DOI] [PubMed] [Google Scholar]
- 3.Verhoeven V, der Auwera Van A, Gaal Van L, et al. Can red yeast rice and olive extract improve lipid profile and cardiovascular risk in metabolic syndrome? A double blind, placebo controlled randomized trial. BMC Complement Altern Med. 2015;15:52. doi: 10.1186/s12906-015-0576-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubick MA, Omaye ST. Evidence for grape, wine and tea polyphenols as modulators of atherosclerosis and ischemic heart disease in humans. J Nutraceut Funct Med Foods. 2001;3:67–93. doi: 10.1300/J133v03n03_04. [DOI] [Google Scholar]
- 5.Nardini M, Natella F, Scaccini C. Role of dietary polyphenols in platelet aggregation. A review of the supplementation studies. Platelets. 2007;18:224–243. doi: 10.1080/09537100601078083. [DOI] [PubMed] [Google Scholar]
- 6.Moreno-Luna R, Munoz-Hernandez R, Miranda ML, et al. Olive oil polyphenols decrease blood pressure and improve endothelial function in young women with mild hypertension. Am J Hypertens. 2012;25:1299–1304. doi: 10.1038/ajh.2012.128. [DOI] [PubMed] [Google Scholar]
- 7.Visioli F, Bernardini E. Extra virgin olive oil’s polyphenols: biological activities. Curr Pharm Des. 2011;17:786–804. doi: 10.2174/138161211795428885. [DOI] [PubMed] [Google Scholar]
- 8.Visioli F, Bellomo G, Galli C. Free radical-scavenging properties of olive oil polyphenols. Biochem Biophys Res Commun. 1998;247:60–64. doi: 10.1006/bbrc.1998.8735. [DOI] [PubMed] [Google Scholar]
- 9.Visioli F, Galli C. The effect of minor constituents of olive oil on cardiovascular disease; new findings. Nutr Rev. 1998;56:142–147. doi: 10.1111/j.1753-4887.1998.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 10.Visioli F, Galli C. Antiatherogenic components of olive oil. Curr Atheroscler Rep. 2001;3:64–67. doi: 10.1007/s11883-001-0012-0. [DOI] [PubMed] [Google Scholar]
- 11.Visioli F, Galli C, Bornet F, et al. Olive oil phenolics are dose-dependently absorbed in humans. FEBS Lett. 2000;468:159–160. doi: 10.1016/S0014-5793(00)01216-3. [DOI] [PubMed] [Google Scholar]
- 12.Wiseman SA, Mathot JN, de Fouw NJ, et al. Dietary non-tocopherol antioxidants present in extra virgin olive oil increase the resistance of low density lipoproteins to oxidation in rabbits. Atherosclerosis. 1996;120:15–23. doi: 10.1016/0021-9150(95)05656-4. [DOI] [PubMed] [Google Scholar]
- 13.Caruso D, Berra B, Giavarini F, et al. Effect of virgin olive oil phenolic compounds on in vitro oxidation of human low density lipoproteins. Nutr Metab Cardiovasc Dis. 1999;9:102–107. [PubMed] [Google Scholar]
- 14.Coni E, Di Benedetto R, Di Pasquale M, et al. Protective effect of oleuropein, an olive oil biophenol, on low density lipoprotein oxidizability in rabbits. Lipids. 2000;35:45–54. doi: 10.1007/s11745-000-0493-2. [DOI] [PubMed] [Google Scholar]
- 15.Pandey KB, Rizvi SI. Plant polyphenols as dietary antioxidants in human health and disease. Oxid Med Cell Longev. 2009;2:270–278. doi: 10.4161/oxim.2.5.9498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angerer P, Kothny W, Störk S, et al. Effect of dietary supplementation with v-3 fatty acids on progression of atherosclerosis in carotid arteries. Cardiovasc Res. 2002;54:183–190. doi: 10.1016/S0008-6363(02)00229-8. [DOI] [PubMed] [Google Scholar]
- 17.Shirai K, Hiruta N, Song M, et al. Cardio-ankle vascular index (cavi) as a novel indicator of arterial stiffness: theory, evidence and perspectives. J Atheroscler Thromb. 2011;18:924–938. doi: 10.5551/jat.7716. [DOI] [PubMed] [Google Scholar]
- 18.Kinouchi K, Ichihara A, Sakoda M, et al. Effects of telmisartan on arterial stiffness assessed by the cardio-ankle vascular index in hypertensive patients. Kidney Blood Press Res. 2010;33:304–312. doi: 10.1159/000316724. [DOI] [PubMed] [Google Scholar]
- 19.Izuhara M, Shioji K, Kadota S, et al. Relationship of cardioankle vascular index (CAVI) to carotid and coronary arteriosclerosis. Circ J. 2008;72:1762–1767. doi: 10.1253/circj.CJ-08-0152. [DOI] [PubMed] [Google Scholar]
- 20.Takaki A, Ogawa H, Wakeyama T, et al. Cardio-ankle vascular index is superior to brachial-ankle pulse wave velocity as an index of arterial stiffness. Hypertens Res. 2008;31:1347–1355. doi: 10.1291/hypres.31.1347. [DOI] [PubMed] [Google Scholar]
- 21.Kubozono T, Miyata M, Ueyama K, et al. Acute and chronic effects of smoking on arterial stiffness. Circ J. 2011;75:698–702. doi: 10.1253/circj.CJ-10-0552. [DOI] [PubMed] [Google Scholar]
- 22.Park HE, Choi SY, Kim HS, et al. Epicardial fat reflects arterial stiffness: assessment using 256 slice multidetector coronary computed tomography and cardio-ankle vascular index. J Atheroscler Thromb. 2012;19:570–576. doi: 10.5551/jat.12484. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura K, Tomaru T, Yamamura S, et al. Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J. 2008;72:598–604. doi: 10.1253/circj.72.598. [DOI] [PubMed] [Google Scholar]
- 24.Okura T, Watanabe S, Kurata M, et al. Relationship between cardio-ankle vascular index (cavi) and carotid atherosclerosis in patients with essential hypertension. Hypertens Res. 2007;30:335–340. doi: 10.1291/hypres.30.335. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki J, Sakakibara R, Tomaru T, et al. Stroke and cardio-ankle vascular stiffness index. J Stroke Cerebrovasc Dis. 2013;22:171–175. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Choi SY, Oh BH, Bae Park J, et al. Age-associated increase in arterial stiffness measured according to the cardio-ankle vascular index without blood pressure changes in healthy adults. J Atheroscler Thromb. 2013;20:911–923. doi: 10.5551/jat.18267. [DOI] [PubMed] [Google Scholar]
- 27.Miyoshi T, Doi M, Hirohata S, et al. Cardio-ankle vascular index is independently associated with the severity of coronary atherosclerosis and left ventricular function in patients with ischemic heart disease. J Atheroscler Thromb. 2010;17:249–258. doi: 10.5551/jat.1636. [DOI] [PubMed] [Google Scholar]
- 28.Satoh N, Shimatsu A, Kotani K, et al. Highly purified eicosapentaenoic acid reduces cardio-ankle vascular index in association with decreased serum amyloid A-LDL in metabolic syndrome. Hypertens Res. 2009;32:1004–1008. doi: 10.1038/hr.2009.145. [DOI] [PubMed] [Google Scholar]
- 29.Sun CK. Cardio-ankle vascular index (CAVI) as an indicator of arterial stiffness. Integr Blood Press Control. 2013;6:27–38. doi: 10.2147/IBPC.S34423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 31.Wolfe F. Fatigue assessments in rheumatoid arthritis: comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. J Rheumatol. 2004;31:1896–1902. [PubMed] [Google Scholar]
- 32.Ridker PM, Rifai N, Pfeffer MA, et al. Long-term effects of pravastatin on plasma concentration of C-reactive protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation. 1999;100:230–235. doi: 10.1161/01.CIR.100.3.230. [DOI] [PubMed] [Google Scholar]
- 33.Ridker PM, Cannon CP, Morrow D, et al. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005;352:20–28. doi: 10.1056/NEJMoa042378. [DOI] [PubMed] [Google Scholar]
- 34.Morrow DA, de Lemos JA, Sabatine MS, et al. Clinical relevance of C-reactive protein during follow-up of patients with acute coronary syndromes in the Aggrastat-to-Zocor Trial. Circulation. 2006;114:281–288. doi: 10.1161/CIRCULATIONAHA.106.628909. [DOI] [PubMed] [Google Scholar]
- 35.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 36.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.CIR.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 37.Passacquale G, Di Giosia P, Ferro A. The role of inflammatory biomarkers in developing targeted cardiovascular therapies: lessons from the cardiovascular inflammation reduction trials. Cardiovascular Res. 2016;109:9–23. doi: 10.1093/cvr/cvv227. [DOI] [PubMed] [Google Scholar]
- 38.Austin MA, Hokanson JE, Edwards KL. Hypertriglyceridemia as a cardiovascular risk factor. Am J Cardiol. 1998;81:7B–12B. doi: 10.1016/S0002-9149(98)00031-9. [DOI] [PubMed] [Google Scholar]
- 39.Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–458. doi: 10.1161/CIRCULATIONAHA.106.637793. [DOI] [PubMed] [Google Scholar]
- 40.Hulley SB, Rosenman RH, Bawol RD, et al. Epidemiology as a guide to clinical decisions: the association between triglyceride and coronary heart disease. N Engl J Med. 1980;302:1383–1389. doi: 10.1056/NEJM198006193022503. [DOI] [PubMed] [Google Scholar]
- 41.Conference Consensus. treatment of hypertriglyceridemia. JAMA. 1984;251:1196–1200. doi: 10.1001/jama.1984.03340330054025. [DOI] [PubMed] [Google Scholar]
- 42.NIH Consensus Development Panel on Triglyceride, High-Density Lipoprotein, and Coronary Heart Disease NIH Consensus Conference: triglyceride, high-density lipoprotein, and coronary heart disease. JAMA. 1993;269:505–510. doi: 10.1001/jama.1993.03500040071040. [DOI] [PubMed] [Google Scholar]
- 43.Patrick L, Uzick M. Cardiovascular disease: C-reactive protein and the inflammatory disease paradigm: HMG-CoA reductase inhibitors, alpha-tocopherol, red yeast rice, and olive oil polyphenols. A review of the literature. Altern Med Rev. 2001;6:248–271. [PubMed] [Google Scholar]
- 44.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 45.Migliori M, Panichi V, de la Torre R, et al. Anti-inflammatory effect of white wine in CKD patients and healthy volunteers. Blood Purif. 2015;39:218–223. doi: 10.1159/000371570. [DOI] [PubMed] [Google Scholar]
- 46.Yonei Y, Iwabayashi M, Fujioka N. Evaluation of effects of cassis (Ribes nigrum L.) juice on human vascular function and gene expression using a microarray system. Anti-Aging Med. 2009;6:22–31.
- 47.EFSA Panel on Dietetic Products. EFSA Panel on dietetic products. Nutrition and Allergies (NDA). Scientific opinion on the substantiation of health claims related to polyphenols in olive and protection of LDL particles from oxidative damage. EFSA J. 2011;9:2033.
- 48.Vita JA. Polyphenols and cardiovascular disease: effects on endothelial and platelet function. Am J Clin Nutr. 2005;81:292–297. doi: 10.1093/ajcn/81.1.292S. [DOI] [PubMed] [Google Scholar]
- 49.Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002;39:10–15. doi: 10.1161/hy0102.099031. [DOI] [PubMed] [Google Scholar]
- 50.Blacher J, Guerin AP, Pannier B, et al. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99:2434–2439. doi: 10.1161/01.CIR.99.18.2434. [DOI] [PubMed] [Google Scholar]
- 51.Kadota K, Takamura N, Aoyagi K, et al. Availability of cardioankle vascular index (CAVI) as a screening tool for atherosclerosis. Circ J. 2008;72:304–308. doi: 10.1253/circj.72.304. [DOI] [PubMed] [Google Scholar]
- 52.Namekata T, Suzuki K, Ishizuka N, et al. Establishing baseline criteria of cardio-ankle vascular index as a new indicator of arteriosclerosis: a cross-sectional study. BMC Cardiovasc Disord. 2011;11:51. doi: 10.1186/1471-2261-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aviram M, Dornfeld L, Rosenblat M, et al. Pomegranate juice consumption reduces oxidative stress, atherogenic modifications to LDL, and platelet aggregation: studies in humans and in atherosclerotic apolipoprotein E-deficient mice. Am J Clin Nutr. 2000;71:1062–1076. doi: 10.1093/ajcn/71.5.1062. [DOI] [PubMed] [Google Scholar]
- 54.García-Lafuente A, Guillamón E, Villares A, et al. Flavonoids as anti-inflammatory agents: implications in cancer and cardiovascular disease. Inflamm Res. 2009;58:537–552. doi: 10.1007/s00011-009-0037-3. [DOI] [PubMed] [Google Scholar]
- 55.Miyashita Y, Endo K, Saiki A, et al. Effects of pitavastatin, a 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor, on cardio-ankle vascular index in type 2 diabetic patients. J Atheroscler Thromb. 2009;16:539–545. doi: 10.5551/jat.281. [DOI] [PubMed] [Google Scholar]
- 56.Miyashita Y, Saiki A, Endo K, et al. Effects of olmesartan, an angiotensin II receptor blocker, and amlodipine, a calcium channel blocker, on Cardio-Ankle Vascular Index (CAVI) in type 2 diabetic patients with hypertension. J Atheroscler Thromb. 2009;16:621–626. doi: 10.5551/jat.497. [DOI] [PubMed] [Google Scholar]