Abstract
Colorectal cancer is the third leading cause of cancer deaths in the United States. Although colorectal cancer screenings are effective and recommended by all clinical practice guidelines, only 65.7% of adults ages 50 to 75 years are screened. Colorectal cancer screening is disproportionately underutilized in inner city populations. In 2011, the University of Pennsylvania Health System created a navigation program to specifically address poor colorectal cancer screening rates and increase access to colorectal cancer screening colonoscopies for patients in the underserved areas of West, South, and Southwest Philadelphia. We directed focus on issues surrounding barriers of screening so that we could best leverage our resources and impact the greatest number of patients. The program was designed to target patients who were either due for, never scheduled, or did not keep previously scheduled colorectal cancer screening colonoscopy appointments, or who were referred by providers concerned that the patients would not keep appointments or would misunderstand preprocedural guidelines. The program strives to improve colorectal health by providing free education and screening navigation through a navigator who assists patients from the first phone call to completion of the colonoscopy. This is accomplished by implementing an effective screening program while providing one-on-one service with a cost-effective navigator reaching out to patients who are nonadherent to colorectal cancer screening. Barriers included not having a companion to escort and transport the patient home from the procedure, poor awareness, fear of the procedure or sedation, limited funds to purchase preparation materials, inability to read or comprehend preparation instructions, and hardship in being contacted or scheduling appointments.
Keywords: Colorectal cancer, colorectal cancer screening, patient navigation, outreach program, underserved population
Colorectal cancer is the third leading cause of cancer deaths in the United States. It is estimated that 134,490 men and women will be diagnosed with colorectal cancer and 49,190 will ultimately die from cancer of the colon and rectum in 2016.1 Although colorectal cancer screening is effective and consistently recommended by all clinical practice guidelines,2,3 screening consistently falls short of its potential, with only 65.7% of adults ages 50 to 75 years screened according to 2014 data from the Centers for Disease Control and Prevention.4 Colorectal cancer screenings remain underutilized, as only 39.4% of all colorectal cancer cases are diagnosed at an early stage.1 Because colonoscopy is one of the few screening techniques that can prevent cancer (by removal of the adenomatous precursor lesion so that polyps will not develop into adenocarcinomas), improving colorectal cancer screening rates has become a national priority. Nationally, the American Cancer Society, National Colorectal Cancer Roundtable, and over 900 organizations, including the American Gastroenterological Association, have pledged to work to increase colorectal cancer screening rates to at least 80% by 2018.5
There are significant racial and ethnic disparities in colorectal cancer incidence and mortality. African Americans bear a disproportionately high burden from cancer-related diseases when compared with other racial and ethnic groups. Compared with whites, the incidence and mortality rates of colorectal cancer are approximately 25% and 50% higher, respectively, in African Americans.6 The etiology of this discrepancy is likely multifactorial, including presentation at a later stage of cancer, as well as fundamental differences in treatment and risk factors; many socioeconomic factors are at play in creating these differences.7-11 In addition, there are striking differences in mortality by education. Mortality for black men with fewer than 12 years of education is nearly twice as high as in black men with 12 or more years of education (20.6 vs 11.3 per 100,000, respectively).7,11 Risk of colorectal cancer has been linked to increasing neighborhood deprivation, as measured by factors such as rates of poverty and need for public assistance, in addition to education.7,8 According to the US Census Bureau, the poverty rate in 2012 for African Americans was 3 times as high as for non-Hispanic whites.10 In 2013, nearly one-quarter of families without children and more than 3 in 10 families with children were living in poverty in the Hospital of the University of Pennsylvania service area.10 In 2010, it was estimated that differences in the prevalence of behavioral risk factors and obesity account for approximately 40% of the socioeconomic disparity in colorectal cancer incidence.10 There is a need to offer education about colorectal cancer prevention, including the lifesaving benefit of timely screening, and to provide assistance in overcoming logistical barriers preventing effective screening to struggling communities, such as African American men and women in West Philadelphia. Because early stage at diagnosis is closely associated with survival from colorectal cancer, novel interventions are needed to increase low screening rates as a way to reduce colorectal cancer morbidity and mortality.
Overview of Patient Navigation
Originally developed to address racial and socioeconomic disparities in breast cancer outcomes,12 patient navigators have been used recently in the field of colorectal cancer screening and have demonstrated increased completion of screening colonoscopy by urban minorities.13-18 Patient navigators work first to identify patient barriers to screening colonoscopy and then to identify resources that are available at the local, state, and federal levels to overcome these barriers. Patient navigators guide patients through the complex and fragmented health care system to ensure completion of colonoscopy and help patients receive culturally competent care that is confidential, respectful, compassionate, and mindful of the patient’s health literacy level and safety.19 Patients who receive navigation services report greater patient satisfaction.17,20
Development of a Navigation Program
The University of Pennsylvania Health System (UPHS) is the largest provider of health care to the West Philadelphia population. According to the 2010 US Census, African Americans comprise 76.6% of the residents in West Philadelphia, 60% of the residents in Southwest Philadelphia, and 35% of the residents in South Philadelphia.21 Poverty in Philadelphia is widespread, but the highest concentrations of poverty are found primarily in parts of North and West Philadelphia.21 In 25 of the city’s 46 residential zip codes, more than 1 in 5 individuals are living below the poverty line. In Philadelphia, the poverty rate is roughly 19% among whites and 29% among African Americans.22
In an effort to raise awareness and screening rates for colorectal cancer, the Gastroenterology Division at the UPHS designed and implemented a patient navigation program to address a diverse and underserved population that offers education and access to complete colorectal cancer screening. In 2011, the West Philadelphia GI Outreach and Patient Navigation Program was launched. The program was initially seeded by a philanthropic gift from a private donor to improve access to screening colonoscopy to the West Philadelphia community to raise colorectal cancer screening rates; this seed money was leveraged through a variety of public and private grant funding, which allowed us to hire and train the first colorectal cancer screening navigator in the UPHS and to maintain the program’s growth and development for patient education and materials through an expanded patient navigation program. We directed focus on issues surrounding the barriers to screening rather than direct payment for the cost of screening so that we could best leverage our resources and positively impact the greatest number of patients.
Functions of a Navigation Program
The West Philadelphia GI Outreach and Patient Navigation Program helps residents of West Philadelphia who are between the ages of 50 and 75 years and have not completed recommended colorectal cancer screening. Colonoscopy has been identified, within the UPHS, as the preferred colorectal cancer screening modality and is listed in electronic medical records. Our navigation program targets assistance to colonoscopy. If a patient inquires about less-invasive tests or other types of procedures (fecal occult blood test, fecal immunochemical test, virtual colonoscopy, or sigmoidoscopy), we explain the different types of tests, offer to send literature brochures for the patient to read, refer the patient for other options, and assist in speaking with the referring provider about other options. Using electronic medical records, a trained patient navigator identifies patients in the UPHS who are either due for, never scheduled, or did not keep previously scheduled colorectal cancer screening colonoscopy appointments, and contacts each patient to identify the barrier(s) that prevented him or her from undergoing a screening colonoscopy. In addition, the navigator receives real-time referrals from providers who recommend screening colonoscopy to a West Philadelphia resident during a clinical encounter but have recognized barriers to successful completion of colonoscopy. The navigator is able to offer one-on-one assistance by calling and/or directly meeting with the patient, speaking with the patient to identify the barrier, and offering assistance for compliance with the procedure by providing education, motivation, scheduling assistance, low-literacy bowel preparation instructions, and bowel preparation materials. It should be noted that this program specifically targets the UPHS patient community, which requires the patients to have insurance; if a patient does not have insurance, we directly refer him or her to the Pennsylvania Department of Health to inquire about access and eligibility. We do not assist in insurance enrollments.
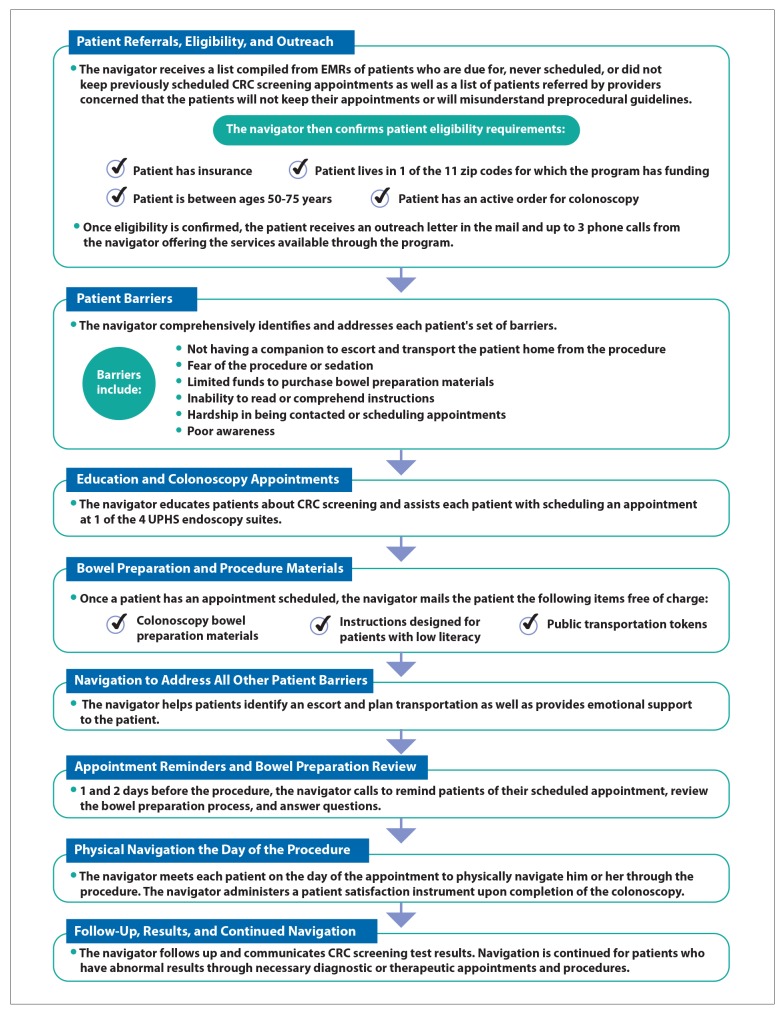
We developed a patient navigation process (Figure) that identifies patients, reviews needs identified during the initial call, facilitates appointment scheduling, sends bowel preparation materials with instructions, contacts patients with reminders and review of the bowel preparation and day-of-procedure instructions, and concludes with a final follow-up call that includes review of the results and aid in scheduling referrals if needed. We initially had 1 full-time navigator. However, due to the labor-intensive nature of the navigation process, we leveraged her expertise with students and volunteers. Significant time was needed to locate patients and contact them via telephone. We estimated that 4.5 hours were expended per patient enrolled in the program through the final result call after colonoscopy. Barriers to reach patients included the phone number being disconnected, the patient refusing or no longer accepting the call, multiple voice messages being left without a response, and patients being apprehensive in speaking with us due to concern that the navigators were not who they stated they were. This program was able to show that once the patient understands that the goal is to help him or her with completion of screening, it is possible to build trust, explain the importance of colorectal cancer screening, and address any questions that the patient posed.
Figure.
Step-by-step patient navigation process displaying the daily actions the navigator takes from the initial outreach phone call to the completion of the colonoscopy.
CRC, colorectal cancer; EMR, electronic medical record; UPHS, University of Pennsylvania Health System.
In order to implement an effective program while providing successful one-on-one service of a navigator reaching out to patients who are nonadherent to colorectal cancer screening, we have had to identify and address additional barriers. These barriers were identified in multiple domains: not having a companion to escort and transport the patient home from the procedure, poor awareness of the risk of colonic neoplasia, fear of the procedure or sedation, limited funds to purchase bowel preparation materials, inability to read or comprehend bowel preparation instructions, and hardship while being contacted and in scheduling appointments. The program was able to overcome these barriers by:
Offering transportation assistance in the form of public transportation tokens or private transportation service of the patient and an accompanying companion
Educating the patient about the procedure, what sedation is and expectations of it, the importance of colorectal cancer prevention, and the value of early detection
Providing free bowel preparation materials and appropriate instructions to the patient
Developing instructions at a 7th grade reading level that included embedded graphics
Following up one-on-one with the patient before the appointment and reviewing the entire bowel preparation process
Scheduling appointments to accommodate both the patient and the companion accompanying him or her
A retrospective cost-effectiveness analysis was performed using data gathered during the first full year (2012) of the navigation program. For this analysis, the results of which were presented at Digestive Disease Week 2014, we analyzed the costs of the program and the cost per patient with completed screening colonoscopy. The outcome of interest was screening colonoscopy completion within 3 months of program enrollment. The navigation program significantly benefited enrolled patients by providing opportunities for care. Navigated patients had a significantly higher rate of colorectal cancer screening completion (79%) and a significantly lower rate of cancelled and/or skipped appointments. In addition, those who were screened as a result of the program had a much higher adenoma detection rate (40%).23 An adenoma detection rate of 40% is an increase of at least 15 percentage points, or a 60% increase, over the national benchmark of 15% to 25%.24 Our research and analysis subsequently demonstrated that such programs are cost-effective and socially effective in this patient population.23
As a result of this research, on July 1, 2015, the program was enlarged and institutionalized by Penn Medicine with expansion to include Southwest and South Philadelphia (11 zip codes). (In comparison, the initial program was designed to serve the residents of the 5 West Philadelphia zip codes.) To date, nearly 2000 patients who received an order for, but were not able to complete, screening colonoscopy were contacted by our navigators and offered navigation services. Of the 1990 patients contacted by our program, 756 (38%) enrolled in the program. Of those who enrolled, 526 (70%) completed colonoscopy. Of those who completed colonoscopy, 195 (37%) were found to have an adenomatous polyp, and 4 were diagnosed with adenocarcinoma.
Conclusion
Intensive one-on-one patient navigation service is a feasible and effective method to increase colorectal cancer screening with a 95% positive patient satisfaction rate for enrolled patients who received navigation service (unpublished data from the authors). Patient navigation is a sustainable intervention that is responsive to socioeconomic challenges while creating a fiscally responsible method for increasing colorectal cancer screening rates in an urban underserved patient population.
We have had a long and interactive journey developing the navigation program and methods for reaching patients; however, we have not yet leveraged all of the resources and tools that are available within the health system. We are currently working on refining appropriate messaging for our patients to increase their understanding of the importance of colorectal cancer screening and the benefits of utilizing navigation. We are also continuing to expand the reach of navigation through community events and marketing efforts.
Footnotes
The authors have no relevant conflicts of interest to disclose.
References
- 1.SEER stat fact sheets: colon and rectum cancer. National Cancer Institute: Surveillance, Epidemiology, and End Results Program. [May 2016]. http://seer.cancer.gov/statfacts/html/colorect.html Published April 2016.
- 2.Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. U.S. Preventive Services Task Force. [DOI] [PubMed] [Google Scholar]
- 3.Levin B, Lieberman DA, McFarland B, et al. American Cancer Society Colorectal Cancer Advisory Group; US Multi-Society Task Force; American College of Radiology Colon Cancer Committee. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58(3):130–160. doi: 10.3322/CA.2007.0018. [DOI] [PubMed] [Google Scholar]
- 4.Basic information about colorectal cancer. Centers for Disease Control and Prevention. [May 2016]. http://www.cdc.gov/cancer/colorectal/basic_info/index.htm Published April 2016.
- 5.Tools & resources: 80% by 2018. National Colorectal Cancer Roundtable. [May 2016]. http://nccrt.org/tools/80-percent-by-2018/ Published April 2016.
- 6.American Cancer Society. Colorectal Cancer Facts & Figures 2014-2016. Atlanta, Ga: American Cancer Society; 2014. [Google Scholar]
- 7.Gupta S, Sussman DA, Doubeni CA, et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014;106(4) doi: 10.1093/jnci/dju032. dju032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doubeni CA, Laiyemo AO, Major JM, et al. Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118(14):3636–3644. doi: 10.1002/cncr.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2012. Washington, DC: US Government Printing Office; 2013. US Census Bureau. Current population reports: P60-245. [Google Scholar]
- 10.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104–117. doi: 10.3322/caac.21220. [DOI] [PubMed] [Google Scholar]
- 11.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 12.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21(1 suppl):S11–S14. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 13.Lebwohl B, Neugut AI, Stavsky E, et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011;45(5):e47–e53. doi: 10.1097/MCG.0b013e3181f595c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen LA, Santos S, Jandorf L, et al. A program to enhance completion of screening colonoscopy among urban minorities. Clin Gastroenterol Hepatol. 2008;6(4):443–450. doi: 10.1016/j.cgh.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Nash D, Azeez S, Vlahov D, Schori M. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006;83(2):231–243. doi: 10.1007/s11524-006-9029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82(2):216–224. doi: 10.1093/jurban/jti046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf L. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008;100(3):278–284. doi: 10.1016/s0027-9684(15)31240-2. [DOI] [PubMed] [Google Scholar]
- 18.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman HP. A model patient navigation program. Oncology Issues. 2004;19:44–46. [Google Scholar]
- 20.Lee T, Ko I, Lee I, et al. Effects of nurse navigators on health outcomes of cancer patients. Cancer Nurs. 2011;34(5):376–384. doi: 10.1097/NCC.0b013e3182025007. [DOI] [PubMed] [Google Scholar]
- 21.Statistical abstract of the United States: 2012. United States Census Bureau. [June 2, 2016]. http://www.census.gov/library/publications/2011/compendia/statab/131ed.html
- 22.The PEW Charitable Trusts. Philadelphia 2015: The State of the City. Philadelphia, Pa: PEW Charitable Trusts; 2015. [Google Scholar]
- 23.Ramos J, Mehta S, Lamanna A, Kochman M, Guerra C. Cost-effectiveness analysis of the first year of a colorectal cancer (CRC) screening patient navigation program at an academic medical center. Gastroenterology. 2014;146(5 suppl 1):S546. [Google Scholar]
- 24.Millan MS, Gross P, Manilich E, Church JM. Adenoma detection rate: the real indicator of quality in colonoscopy. Dis Colon Rectum. 2008;51(8):1217–1220. doi: 10.1007/s10350-008-9315-3. [DOI] [PubMed] [Google Scholar]