Abstract
Background:
Participation of woman in decision-making processes is one of the key indicators of an appropriate relationship between a woman and the health care professionals. This study aimed to recognize the factors facilitating respect for woman's decision-making in spontaneous birth.
Materials and Methods:
This paper employed a meta-synthesis on articles published in four biomedical databases including MEDLINE, Web of Science, CINAHL, and Cochrane Library. All qualitative studies published after 1990 and directly or indirectly discussing the women's and the health care professional's attitudes toward respect for woman's decision-making in spontaneous birth were searched. Of 5372 citations, 95 full-text papers were considered, of which 14 satisfied the inclusion criteria.
Results:
In this meta-synthesis, initial codes were obtained through meticulous, line-by-line coding of the findings of the primary studies. Then, thematic synthesis was performed on the codes to search for concepts, and 20 descriptive themes were obtained in the second stage. Finally, through an inductive process, five new interpretations were obtained in the last stage of the thematic synthesis. These interpretations included confidence to health care providers, the central role of midwives in maintenance of women's dignity, childbirth as a natural phenomenon, the impact of contextual conditions, and the political and human factors affecting the delivery management and women seek place of safety for childbirth.
Conclusions:
Studies suggested that midwifes have a central role in maintenance of women's dignity and their experience of childbirth.
Key words: Childbirth, dignity, Iran, qualitative study, thematic synthesis
INTRODUCTION
Childbirth is a unique experience for a woman, influencing her dignity for many years.[1] A positive experience of childbirth improves the woman's and her family's mental health, increases the rate of successful breastfeeding, and leads to fewer complications.[2]
The quality of communication is a significant indicator for mutual decision-making between women and midwives.[3] Women have very different prospects toward childbirth that significantly affect their coping with it.[4]
Pain management and constant support are two factors that allow women to cope with labor experience. These factors increase women's dignity and improve shared decision-making between women and health care providers.[5] Enabling women to make informed decisions is a key factor that provides them a positive childbirth experience.[6] Furthermore, suppleness, honor, respect for favorite and dignity, and support and reassurance are not only important in assisting women to cope with childbirth[7,8] but are more precious than physical support.[9]
Nowadays, health care practices tend to reject passive orders, misplace assurance, and make health care decisions on behalf of the patients.[10] Childbirth is also interpreted as a process that occurs between women and health care providers.[10] Such a partnership is highly supported in the modern health care systems[10] and is emphasized in midwifery studies. This attitude has placed woman at the core of midwifery care.[11] Midwifery care is defined as a constant, personal, and sensitive service during the entire childbirth process[3] that should substitute women's fears with control and self-confidence.[12] To this end, a woman's right to participate in decisions regarding her health and care should be the cornerstone of all midwifery care. Then, adequate information should be provided for women by skilled professionals. Such information should provide a range of alternative action modalities that enable women to make the best decisions regarding their health.[13]
Although some of the health care professionals are concerned about the reduction of their professional authority, it should be noted that patients’ participation in health care decisions and women's autonomy does not mean a reduction in professional authority but reflects a shift in the paternalistic view towards women and other clients.[14] As Lothian commented, there is a range of correct health care conducts and health care professionals should enable patients to select the best. In this case, midwives should empower women to select a suitable conduct to give birth, depending on their ideals, attitudes, targets, and psychological facets.[15] This is especially important when we know that childbirth is a natural experience and pregnant women are not patients, but are users of a precise service in the health care system; and they aware of their rights about pregnancy and childbirth.[16,17]
Such shared decision-making needs clearness of vision and duties and a feeling of being conducive to debates and talks on an important health care decision.[18,19] The growth of an open and credulous relationship may facilitate the process of shared decision-making.[18,19]
Studies show that autonomy and shared decision-making are key factors for a positive childbirth experience.[16,17] Hence, it is important to recognize factors that facilitate shared decision-making between women and health care professionals. This study aimed to discover the factors facilitating the process of shared decision-making.
MATERIALS AND METHODS
This study employed a meta-synthesis approach. The study was conducted on articles retrieved from four biomedical databases including MEDLINE, Web of Science, CINAHL, and Cochrane Library.
Inclusion criteria
The aforementioned databases were searched to retrieve qualitative studies focusing on women's and health professional's experiences and attitudes toward respect for woman's decision-making in spontaneous birth. Access to full text articles in English language was an additional inclusion criteria.
Search strategy
The databases were searched with keywords including qualitative study, thematic synthesis decision-making, childbirth, and dignity. Depending on the individual databases, the search operators (AND; OR) were used to extract the articles.
Quality appraisal of studies
The quality of the studies was appraised using a reliable quality evaluation tool (NICE, 2009). The NICE contains 14 criteria and is an appropriate instrument for evaluation of qualitative studies. If a study had all, or approximately all the criteria, it was assigned (++). Studies were assigned a (+) if they had a number of criteria and were assigned (−) if they had an inadequate number of the criteria. The latter studies remained in the review but did not affect the conclusion. Therefore, no papers were excluded from this review.
Data extraction and quality appraisal of the studies were carried out by one researcher (MF) and re-assessment was conducted by three reviewers (TA, MK, and MM). Contradictions and disagreements were resolved through consensus by the research team.
Data synthesis
There are different methods available for synthesis of qualitative studies.[20] We used thematic synthesis.[21] First, the findings of the retrieved studies were discussed by the review team, and then the data were coded and categorized to obtain themes. The themes were then discussed by the review team until an explanatory framework was formed.
RESULTS
The initial search in databases brought up 5372 citations; among them 5265 citations were excluded because they did not match the research question. From all the abstracts of 107 articles, only 8 papers matched the inclusion criteria. Another search up to March 2014 yielded 1208 citations, of which 1202 were excluded, and 6 papers were included in the review at this stage. In general, 14 papers were assessed in the present study. Nine studies had very good quality (++); four studies had good quality (+); and one had poor quality (−) because it did not report the details of the study but was included in this review for its plentiful findings.
Characteristics of included studies
The properties of the included studies are summarized in Table 1. Two studies were carried out by the same authors.[24,31] Nine studies reported the views, attitude, and experiences of women who had labor, however, three studies explored the viewpoints of health care professionals. One study explained the patients’ experience and one study explored the experiences of both midwives and women. Participants were recruited from postpartum wards, maternity units, and women's houses. One study was carried out through email and a number of open-ended questions were added at the end of the questionnaire.[31]
Table 1.
Characteristics and main themes from included studies
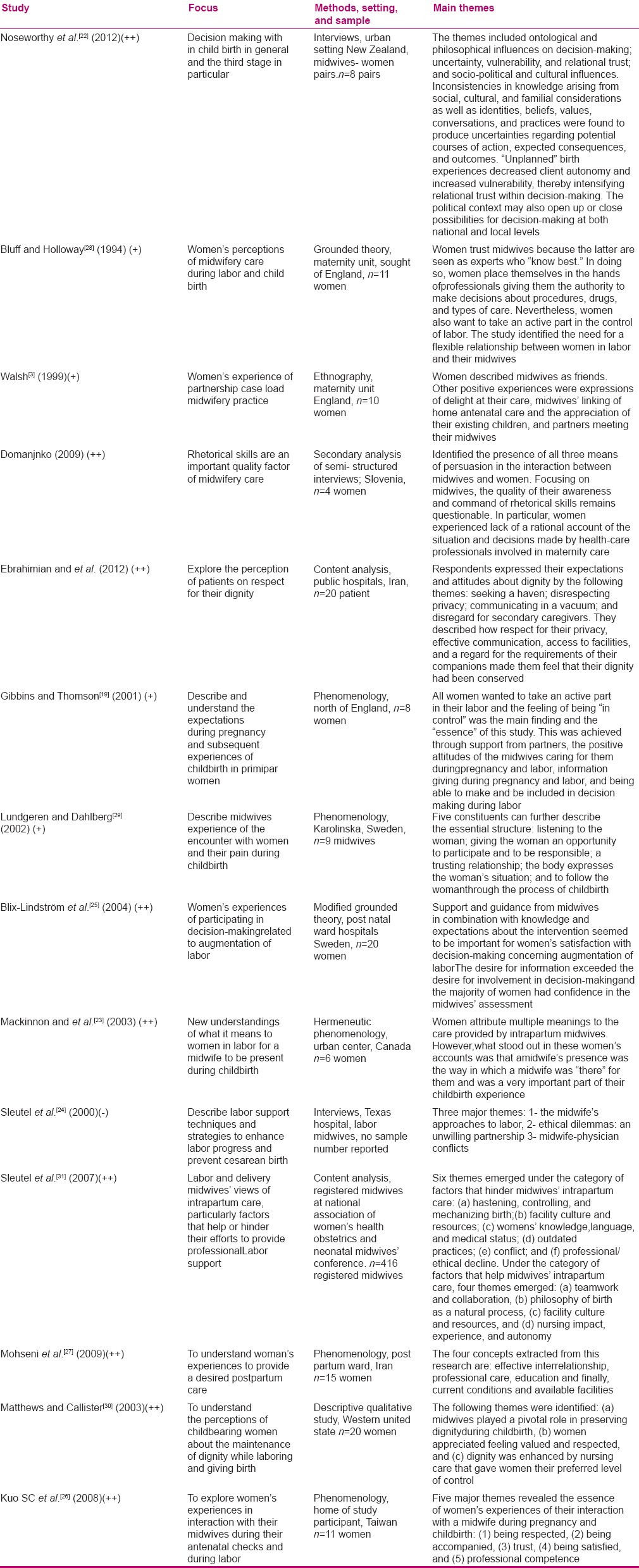
The studies were carried out using a variety of qualitative approaches. Four studies only reported that interviews were used as the main data collection method. Other studies used specific qualitative approaches such as ethnography (one paper),[3] grounded theory (two papers), phenomenology (four papers), and content analysis (two papers). In addition, there was a study which did not report the experiences of women or health providers but described the patients’ dignity as a key element in the process of shared decision-making. Therefore, we did not exclude it from this review. This was done to avoid what Dixon-Wood et al.[20] cited it as “a malfunction that might result in an imperfect review.”
Data extraction
All the texts under the heading “results” were extracted electronically and entered into the computer software MAXqda(version2007). Each of the research team embarked on coding and analysis separately, and then consensus was used to resolve conflicts.
Data synthesis
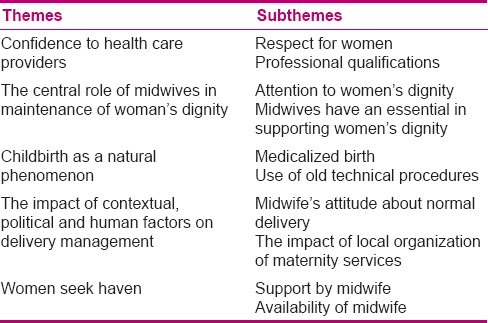
The data synthesis was performed through three inductive phases. In phase 1, the findings of the primary studies were read and coded line-by-line to produce the initial codes. Then, the codes were searched for the pre-existing meanings, and new concepts were created when deemed necessary. In phase 2, the codes were structured into descriptive themes. At this stage, 20 descriptive themes emerged. In phase 3, the descriptive themes were developed into analytic themes, which resulted in 5 new interpretations. The themes and subthemes that emerged from the synthesis are presented in Table 2.
Table 2.
Themes and subthemes
According to the findings, faith in the information and the ability of midwives influence the shared decision-making between women and midwives. Respect for women and professional training were the two key factors that improve woman's trust in health care professionals.
Respect for women
Health care providers’ respect for women is a key factor in obtaining women's assurance. Trust, in turn, facilitates shared decision-making between women and health care providers. Many factors such as people's attitude, social background, educational values and past experiences also affect shared decision-making and should be respected by midwives.[12,19,22,23,24,25,26] Noseworthy et al.[22] reported that the quality communication between midwives and women plays a vital role in selecting a midwife. Tracey, a participant in this study expressed this point when describing why she selected Penny as her midwife: “She's related to my partner … she had also done another friend of mine and my partner's sister, and then I found out through my auntie, you [the midwife] also did my auntie.” Tracey also chose the midwife because she was from a similar cultural group and could talk the equal language.
Professional qualifications
It is clear that some women without thinking accept decisions made by health care providers because they trust in their professional competence. Six studies have directly or indirectly expressed the crucial role of professional competence in the process of shared decision-making.[3,19,23,27,28,29] Some studies reported that women may not always know why those decisions have been made but they obey because of the trust they have in the decision maker, regardless of what the decision entails.[28] For example, in one case, the subject of eating and drinking was not at all discussed between the midwife and woman, but the woman followed the decision which was made on her behalf. This woman said: “I wasn't allowed anything else (other than water). I don't know why. I just accepted it because they obviously know better than I do what's going to happen, what's best for me and the baby, so I just assumed that was what it was, you know. I didn't argue about it at all. I just assumed they knew best.” (laughs).[28]
The central role of midwives in maintenance of woman's dignity
Respect for woman's dignity is a key factor in empowering women to participate in decisions related to childbirth. This gives women a feeling of personal control which consequently influences their approval with childbirth. Woman's dignity in childbirth may differ and depends on personal prospects in relation to the care they will receive. Almost all of the studies in this review have reported that midwives have an essential role in supporting the woman's dignity.
In a study by Matthew,[30] women expressed the significance of the midwife's role in supporting them. The midwife's presence, giving necessary information, support, and their permanence give the woman a sense of respect and dignity. Many women described surprise at the expanded roles of midwives. For instance a woman said: “The birth experience doesn't really matter with your doctor. He's there the last 5 or 10 minutes. It's the midwife that's with you through the whole 12 hours. She plays even a bigger role than the doctor does, because she's the one that's in there all the time with you.”
Some women expressed that sincere concern and positive attitude of midwife helped them in delivery. For example, Lindsey said of triage midwife: “She seemed so excited to see us. She said this is so exciting! How long have you been having contractions?” For me it was like, “Oh, I'm so excited. I'm going to have this baby.” She made me feel that I was doing a great and noble thing, having a baby.”
Midwives, compared with physicians, the more time exhausted with women; therefore, they have a main role in preservation of woman's dignity. Several women expressed surprised that the physicians were not more involved; Mary said she would have appreciated “a little bit more of the doctor's interaction. I just thought he'd be a little bit more involved. He would just poke his head in and sometimes not even talk to me and just talk to the midwife.”
Constant care giving during labor induces women a feeling of being supported and valued in women. Kara, a woman with a 12-hour labor, said: “I had the same midwife stay with me the whole time I was in labor. It was really nice to have help from somebody I knew the whole time, and not have they kept switching on me.”[30]
Childbirth as a natural phenomenon
Data from the included studies proposed that childbirth is a natural procedure. However, medicalized birth, use of old techniques and cold body language avoid mutual decision-making between women and health care providers.
Medicalized birth
A study by Sleutel[31] showed that childbirth is a normal and attractive process. Midwives in this study reported that women are empowered and they must be permitted to have a natural birth. For example, a midwife said “I believe in the birth process and pass that on to my patients/family. I introduce myself as their delivery midwife. I love what I do … Don’t spread the word ‘CS’ so others don’t start planning for it and expecting it. Time, let nature take its course. Our docs are pretty good about supporting (or not interfering with) natural birth … They don’t rush to do CS and tend to give patients every chance to have a vaginal birth. Our chief of service is a DO and is very willing to allow any and everything to facilitate a vaginal birth.”
Another midwife wrote that medical interventions in the process of a normal childbirth are not only the obstacles to good nursing care but also to professional labor support techniques. Commenting on the barriers to labor support a midwife said “… overuse of technology ties the woman to the bed.” Repeatedly, midwives wrote comments such as “MDs use too much Pitocin, especially for induction of labor. [They] do not allow women to come into active labor on their own.” Many midwives cited “MDs,” or “MD practices” as a barrier to natural birth. Such an attitude is visible in the following quotations “Several new MDs at our facility are ‘high techies’;” “Many OBs are oblivious to labor support and women's wishes for labor. They all think, ‘Just get it out and over with’;” “I sometimes see that when patients are up and mobile, physicians will apply internal monitors, which certainly makes them stuck within the length of cables. Obstetricians seem to be … monitored and ‘tinker’ oriented.”
Use of old technical procedures
Use of old techniques is one of the factors preventing shared decision-making between women and midwives. Five studies addressed this issue.[19,23,24,29,31] This barrier also hindered midwives’ supportive interventions during labor. In Sleutel's study,[31] midwives took the issue with physicians’ and midwives’ lack of evidence-based practice and unwillingness to strive for alternative processes. For example, some of the midwives described aggravation when physicians did not allow them to use fetal monitoring or have women labor in chairs rather than beds. A midwife who had recently moved from New Mexico to Pennsylvania wrote: “While I have utilized birthing balls, Jacuzzis, squatting bars, rocking chairs, etc., in NM, Pennsylvania, MDs and midwives do not feel comfortable with such techniques, therefore making it difficult to change practice in [my new] facility. At times I make suggestions, but both MDs and patients feel more comfortable with old fashioned supine positions.” Respondents complained of both physician and midwife colleagues who did not continue with their plan of care, did not keep current, and were resistant to new ideas. In fact, a majority of the studies indicated that “midwives didn’t seem to want to try new ideas.”[31]
Lack of a suitable communication between women and midwives is a barrier to shared decision-making. The included studies show that the cold body language of midwives prevents communication between women and midwives. In Sleutel's study,[31] it was described that some of new midwives were not skilled in the art of labor support. Moreover, some of them were lazy, uncaring, or unmotivated. Participants described some unethical aspects of both medical and midwifery care. For instance, some midwives get out of human caring when they avoid being in room with a patient and spend most of their time watching strips at the desk, when a woman is laboring. A respondent also commented: “Midwives [who] sit at the nursing station and the leadership team perpetuate that behavior … There seems to be an attitude that when the volume is reasonable, midwives should put their feet up-as payback for busier days-instead of staying in the room with their laboring women.”
The impact of contextual, political, and human factors on delivery management
A health care decision depends on several factors such as political, setting, social, and civilizing factors. Health reforms have impacted the health care system as budgets are strained and calls for efficiencies are made.[32,33] This can result in limitations on choice. According to results of some studies, the medicalization of childbirth and the enhanced use of medicine have been promoted as the norm. In this new culture, options outside the medical technological discourses are risky.[22] However, midwives’ attitude toward normal delivery is a key factor in organizing the delivery. For example, Cindy (a midwife) said “When I first meet people I actually tell them I am quite a holistic midwife, I’m in to natural birth. If you think you’re one of these persons that come in and want an epidural within two minutes of actually going into labour, then I’m probably not the midwife for you.”[22]
Birthing choices may also be limited by the local organization of maternity services. For instance, in New Zealand, the Canterbury District Health Board funds four primary birthing units, whereas in the Wellington Region, the Capital and Coast District Health Board funds two departments with no primary birthing units. In this situation, most births happen within the secondary or tertiary maternity units in the area.[22]
Women seek haven
Data from the included studies indicated indirectly that women seek a haven during childbirth. In this sense, support from a midwife and availability of a midwife help women in their search for a haven.
Support by midwife
Five studies in this meta-synthesis indicated that being supported by a midwife is a vital factor in childbirth.[19,22,24,25,28] A decision about childbirth should be based on honoring woman's right and dignity. In a study, delivered women frequently described how the midwives had informed and consulted them before decisions were made about oxytocin infusion or other methods for augmentation of labor, as illustrated in the following quotation: “They (the midwives) asked me about everything; they asked if I want them to rupture the membranes and if I want an enema and all kinds of things” (Interview 19).[25]
Several factors affect a woman in feeling certain and being able to manage the childbirth. Being looked after by a midwife gives women a feeling of assurance and being supported. For instance, a woman (Dawen) said “I think it would be good to be looked after in labor by a midwife I know. I like the midwives I have seen. There is one in particular I feel as if I have got on quite well with her. She is very reassuring and I think it would be ideal if she were going to be there, then that would be great. But she won’t, it will be a different team of people.”[19]
Availability of midwife
Midwife's attendance is necessary during childbirth. Women require the midwife to be available, compassionate, and helpful in a particular minute. They also should be active listeners to reduce women's anxiety. Then, they would be able to share the partnership in keeping them safe and exercise a conciliatory role between women's household and their health condition, which would consequently facilitate the process of shared decision-making.[23]
All the articles included in this study indicated that the accessibility of a midwife is necessary during childbirth. In Mackinnon,[23] when asked about the importance of the midwife's presence during her labor, Janet (a woman who had her first baby) said: “It meant everything to me!”
Women, in this study resolute points where they thought the midwife's presence was not only important but essential in the way things happened. Helen (a woman who had her first baby) commented in this regard “I'm not really aware that changing midwives to a more sympathetic character makes you deliver faster, so that's all total hearsay, but I think that is the impression people are left with in the end.”
DISCUSSION
This meta-synthesis recognized factors that help the process of shared decision-making between women and health care providers during childbirth. We explored five issues that help women and health care providers carry out a safe childbirth. These themes helped us recognize a set of factors that not only support women in decision-making for childbirth but also help health care providers to promote their attitude toward woman's power and dignity.
First, the synthesis established that woman's confidence in health care provider is the main factor in shared decision-making. Assurance causes a woman to trust the information and care provided by the health care personnel. Confidence induces women to converse with health care providers more easily; therefore, health care providers should discuss woman's treatment with her and connect with her for health care decisions. The women usually trust the health care providers’ knowledge and ability; which in turn facilitates the communication between women and health care providers.
Second, our review suggested that midwives have a vital role in preserving the woman's dignity. Dignity has diverse meanings in different cultures and societies. Respect for dignity is respect for beliefs, attitudes, and principles. Another meaning of woman's dignity is respect for their desire to control labor pain. It also means respecting their feeling of self-efficacy and involving them in their own health care decisions.[34] Giving information to woman about childbirth by a midwife enhances woman's self-confidence, which improves the process of mutual decision-making between woman and midwife.
Third, in this study, it was concluded that childbirth is a natural event; consequently, this phenomenon is a foundation for relationship between women and midwives. In this process, medical intervention is rarely necessary. However, verbal ability of midwives is the key issue in the relationship between the woman and midwife in the process of childbirth. Alternative medicine, such as aromatherapy, acupuncture, and reflexology, can also be used by midwives to reduce labor pain in a natural childbirth. These methods are based on communication and collaboration between the woman and midwife.
Fourth, the present study showed that many factors such as contextual, political, cultural, and human factors affect childbirth management. Nonetheless, our findings might not be generalizable to the childbirth management in the entire world. The management of childbirth might vary in different countries because of differences in values, cultures, and the structure of health care systems. The proportion of a country's gross national product dedicated to the health care system and to women’ and children's health affects the number of workers serving the women during childbirth. Then, a lack of skilled midwives in childbirth centers might disrupt shared decision-making between women and midwives.
Finally, our synthesis suggested that women seek a refuge in childbirth. Childbirth is full of stress and fear for the woman especially due to the labor pain. Educational culture of hospitals and lack of sufficient information regarding delivery are other factors influencing women. In this condition, women need to be protected against fear and stress. Trust in midwife is a suitable haven for woman during childbirth. Therefore, a midwife has a main role in reducing women's fears and stresses upon admission into hospital.
Synthesis of qualitative studies is a new method of reviewing and appraisal, with many challenges, and there is little harmony on how to tackle them.[13] In our synthesis, we applied validated methods to search for articles in electronic databases. Synthesis of qualitative studies is also questionable due to interpretation and lack of transparency.[35] We tried to maximize transparency by giving a detailed explanation about the structure of the synthesis.
CONCLUSION
In the recent decades, childbirth procedure has become excessively medicalized. By this definition, shared decision-making is not possible between women and health care providers. Respect for woman's dignity during childbirth is the key factor for an agreeable experience with delivery. This experience affects a woman's decision about the type of delivery performed in the future. Consequently, it is crucial to identify factors facilitating respect for the woman's dignity and shared decision-making during childbirth.
Authors’ contributions
MF contributed to the literature review, data extraction and manuscript drafting. MK contributed to the data analysis, reviewing and editing of the manuscript. MM and TA contributed to the data analysis, reviewing and editing of the manuscript. MF contributed to the development and implementation of the search methods. All authors significantly contributed to the work and approved the manuscript for submission.
Financial support and sponsorship
This article has been supported by Mashhad University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Thomson A. The relationship of the legalisation of midwifery and safe motherhood. Midwifery. 2003;19:77–8. doi: 10.1016/s0266-6138(03)00017-2. [DOI] [PubMed] [Google Scholar]
- 2.Rahmani A, Ghahramanian A, Alahbakhshian A. Respecting to patients’ autonomy in viewpoint of nurses and patients in medical-surgical wards. Iran J Nurs Midwifery Res. 2010;15:14–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Walsh D. An ethnographic study of women's experience of partnership caseload midwifery: The professional as a friend. Midwifery. 1999;15:165–76. doi: 10.1016/s0266-6138(99)90061-x. [DOI] [PubMed] [Google Scholar]
- 4.Chibuik OC, Onyeka TC. Denial of pain relief during labor to parturients in southeast Nigeria. Int J Gynaecol Obstet. 2011;114:226–8. doi: 10.1016/j.ijgo.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Wahn EH, Nissen E, Ahlberg BM. Becoming and being a teenage mother: How teenage girls in south western Sweden view their situation. Health Care Women Int. 2005;26:591–603. doi: 10.1080/07399330591004917. [DOI] [PubMed] [Google Scholar]
- 6.Smeenk AD, ten Have HAM. Medicalization and obstetric care: An analysis of developments in Dutch midwifery. Med Health Care Philos. 2003;6:153–65. doi: 10.1023/a:1024132531908. [DOI] [PubMed] [Google Scholar]
- 7.Madi BC, Crow R. Qualitative study of information about available options for childbirth venue and pregnant women's preferences for a place of delivery. Midwifery. 2003;19:328–36. doi: 10.1016/s0266-6138(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 8.Bowers BB. Mother's experiences of labor support: Exploration of qualitative research. J Obstet Gynecol Neonatal Nurs. 2002;31:742–52. doi: 10.1177/0884217502239218. [DOI] [PubMed] [Google Scholar]
- 9.Price S, Noseworthy J, Thornton J. Women's experience with social presence during childbirth. Am J Matern Child Nurs. 2007;32:184–91. doi: 10.1097/01.NMC.0000269569.94561.7c. [DOI] [PubMed] [Google Scholar]
- 10.Domajnko B, Drglin Z, Pahor M. Rhetorical skills as a component of midwifery care. Midwifery. 2011;27:125–30. doi: 10.1016/j.midw.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Bauer S, Kotter C. Midwife-led birth centers: An alternative to hospital child birth? Z Geburtshilfe Neonatal. 2013;217:14–23. doi: 10.1055/s-0032-1333214. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy HP, Shannon MT. Keeping birth normal: Research findings on midwifery care during childbirth. J Obstet Gynecol Neonatal Nurs. 2004;33:554–60. doi: 10.1177/0884217504268971. [DOI] [PubMed] [Google Scholar]
- 13.Abou Zeina HA, El Nouman AA, Zayed MA, Hifnawy T, El Shabrawy EM, El Tahlawy E. Patients’ Rights: A hospital survey in south Egypt. J Empir Res Hum Res Ethics. 2013;8:46–52. doi: 10.1525/jer.2013.8.3.46. [DOI] [PubMed] [Google Scholar]
- 14.Kukla R, Kuppermann M, Little M, Lyerly AD, Mitchell LM, Armstrong EM, et al. Finding Autonomy in Birth. Bioethics. 2009;23:1–8. doi: 10.1111/j.1467-8519.2008.00677.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lothian J. Critical dimensions in perinatal education. AWHONNS Clin Issues Perinat Womens Health Nurs. 1993;4:20–7. [PubMed] [Google Scholar]
- 16.Harding D. Making choices in childbirth. In: Page L, editor. The New Midwifery Science and Sensitivity in Practice. Edinburgh: Churchill Livingstone; 2000. pp. 71–85. [Google Scholar]
- 17.Edwards A, Elwyn G, Smith C, William S, Thornton H. Consumers’ views of quality in the consultation and their relevance to ‘shared decision- making’ approaches. Health Expect. 2001;4:151–61. doi: 10.1046/j.1369-6513.2001.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurse. 2004;46:212–9. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- 19.Gibbins J, Thomson AM. Women's expectations and experiences of childbirth. Midwifery. 2001;17:302–13. doi: 10.1054/midw.2001.0263. [DOI] [PubMed] [Google Scholar]
- 20.Dixon-Woods M, Agarwal S, Young B, Jones D, Sutton A. NHS Health development Agency. London: UK; 2004. Integrative Approaches to Qualitative and Quantitative Evidence. [Google Scholar]
- 21.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noseworthy D, Phibbs SR, Benn CA. Towards a relational model of decision-making in midwifery care. Midwifery. 2013;29:e42–8. doi: 10.1016/j.midw.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 23.Mackinnon K, McIntyre M, Quance M. The meaning of the nurse's presence during childbirth. J Obstet Gynecol Neonatal Nurse. 2005;34:28–36. doi: 10.1177/0884217504272808. [DOI] [PubMed] [Google Scholar]
- 24.Sleutel MR. Intra partum nursing care: A case study of supportive interventions and ethical conflicts. Birth. 2000;27:38–45. doi: 10.1046/j.1523-536x.2000.00038.x. [DOI] [PubMed] [Google Scholar]
- 25.Blix-Lindström S, Christensson K, Johansson E. Women's satisfaction with decision-making related to augmentation of labour. Midwifery. 2004;20:104–12. doi: 10.1016/j.midw.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Kuo SC, Wu CJ, Mu PF. Taiwanese women's experiences of hospital midwifery care: A phenomenological study. Midwifery. 2010;26:450–6. doi: 10.1016/j.midw.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Mohseni M, Bahadoran P, Abedi H. The quality of postpartum care from women’ viewpoint. Hakim Res J. 2009;12:27–34. [Google Scholar]
- 28.Bluff R, Holloway I. ‘They know best’: Women's perceptions of midwifery care during labour and childbirth. Midwifery. 1994;10:157–64. doi: 10.1016/0266-6138(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 29.Lundgren I, Dahlberg K. Midwives ‘experience of the encounter with women and their pain during childbirth. Midwifery. 2002;18:155–64. doi: 10.1054/midw.2002.0302. [DOI] [PubMed] [Google Scholar]
- 30.Matthews R, Callister LC. Childbearing Women's Perceptions of Nursing Care That Promotes Dignity. J Obstet Gynecol Neonatal Nurse. 2003;33:498–507. doi: 10.1177/0884217504266896. [DOI] [PubMed] [Google Scholar]
- 31.Sleutel M, Schultz S, Wyble K. Nurses’ views of factors that help and hinder their intra partum care. J Obstet Gynecol Neonatal Nurse. 2007;36:203–11. doi: 10.1111/j.1552-6909.2007.00146.x. [DOI] [PubMed] [Google Scholar]
- 32.Segall M. From cooperation to competition in national health systems and back? Impact on professional ethics and quality of care. Int J health Plann Manage. 2000;15:61–79. doi: 10.1002/(SICI)1099-1751(200001/03)15:1<61::AID-HPM573>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 33.Chapman AR. Globalization, human rights, and the social determinants of health. Bioethics. 2009;23:97–111. doi: 10.1111/j.1467-8519.2008.00716.x. [DOI] [PubMed] [Google Scholar]
- 34.Lothian K, Philip I. Care of older people: Maintaining the dignity and autonomy of older people in the healthcare setting. BMJ. 2001;322:668–70. doi: 10.1136/bmj.322.7287.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: Lessons learnt. BMC Med Res Methodol. 2008;16:8–21. doi: 10.1186/1471-2288-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]


