Summary
Hip fracture is common in the elderly and it is usually associated with comorbidities and physiological changes which may have an impact on functioning and quality of life. The concept of resilience may explain why this impact varies among patients. The aim of this open, prospective cohort study was to explore the relationships between resilience, frailty and quality of life in orthopedic rehabilitation patients, and also to assess whether these factors might affect rehabilitation outcome. Eighty-one patients, older than 60 years, underwent a multidisciplinary assessment at the beginning and at the end of the rehabilitation period following orthopedic surgery to the lower limb. The assessments were performed using the Resilience Scale, the Multidimensional Prognostic Index (as a measure of frailty), the WHO Quality of Life-BRIEF, the Geriatric Depression Scale, and the Functional Independence Measure (as a measure of the rehabilitation outcome). A negative correlation between disability and resilience emerged and this association interacted with frailty level. We also found that resilience and quality of life are positive predictors of functional status at discharge.
Keywords: frailty, geriatric, hip fracture, quality of life, rehabilitation outcome, resilience
Introduction
The geriatric population is increasing rapidly. In Italy, where the investigation reported in this paper was carried out, the over 65s make up more than 18% of the population, while 4% is aged over 80 years (Iolascon et al., 2011). More and more older people with disabilities are demanding rehabilitation care as acute ward hospital stays become shorter. The prevalence of chronic medical conditions has increased and rehabilitation medicine has begun to play an important role in the diagnosis and treatment of chronic illness (Cully et al., 2005).
Some injuries, such as hip fracture, which are common in the older population and encountered in rehabilitation wards, are associated with a high risk of comorbidities, complications (such as infections and delirium) and frailty (Friedman et al., 2009). Comorbid conditions, in addition to age, gender and pre-fracture functional abilities, may have an impact on the outcome, in terms of both ambulation and quality of life, in hip-fractured patients. Elderly persons may also experience physiological changes which impair their functional reserve and increase their vulnerability to disability (Fried et al., 2004).
The concept of frailty, a status suggested to reflect decreased physiological reserves across multiple organ systems, arising from cumulative comorbid conditions (Fried et al., 2004; Rockwood and Mitnitski, 2011), has been developed to account for this latter phenomenon. Surgical disease and surgery itself are substantial stressors that may interfere with the physiological homeostasis. For these reasons, the presence of frailty is a clinically important consideration in older patients who are considering surgery as a possible treatment. Moreover, the prevalence of frailty in geriatric surgical patients has been found to be much higher than in a community-dwelling population (Partridge et al., 2012). Kim et al. (2014) found that the variables associated with frailty were closely related to postoperative mortality rate and destination at discharge from hospital. Acute or chronic stress, low activity level, poor nutritional status and depression can trigger or accelerate a frailty status (Walston and Fried, 1999).
In addition to this, older people often suffer from depression and other mood disturbances (Addonizio and Alexopoulos, 1993). Some authors found a correlation between mental health and rehabilitation outcomes, and studies have demonstrated that physical outcomes are poorer in older adults with depression (Dubljanin Raspopović et al., 2014). Furthermore, depressed older people have more physical disability than non-depressed ones, and depression increases the risk of reduced independence in activities of daily living (ADL) (Katz et al., 1963), and of disability in mobility in initially non-disabled older persons; the risk of physical disability and reduced independence has been found to be higher than that associated with other baseline chronic conditions (Penninx et al., 1999). Moreover depression in the elderly is correlated with changes in individual global functioning that can lead to a loss of compliance with treatments and malnutrition, as well as a lack of motivation towards rehabilitation protocols (Gantner et al., 2003).
Emotional responses to chronic illness are different from person to person. Some individuals may experience minimal distress in response to dramatic conditions, whereas others may feel shattered in the face of mild medical conditions (White et al., 2008). Resilience is a concept that may help to explain why some individuals seem to deal with injuries more successfully than others (White et al., 2010). Resilience is defined as the capacity of individuals to successfully maintain or regain their mental health in face of significant adversity (Stewart and Yuen, 2011). In the literature this attitude has been interpreted in different ways: it has been defined as ordinary, adaptable and context dependent (Bonanno, 2004); but also as a specific, fixed personality trait (Davey et al., 2003), and thus a non-modifiable dimension of character; for others, on the other hand, the level of resilience may fluctuate (Connor and Davidson, 2003). To explore the concept of resilience, reference must be made to the allied concept of coping strategies. Coping is seen as a potential mechanism of resilience that involves cognition and behavior (Yi-Frazier et al., 2010) and may contribute to resilience in the face of stress.
In the geriatric population chronic illness is a common condition that could reduce coping strategies and resilience, especially when the illness is associated with pain and disability. However, in the context of specific conditions like spinal cord injury, heart transplant, amputation and cancer, some authors found that older people seem to be more resilient than younger ones when confronted with chronic illness. It is probable that past life experiences allowed these elderly to be stronger in face of their physical problems. Nevertheless, other authors have found evidence that older adults with disability and chronic illness exhibit less post-traumatic growth compared with younger ones (Bombardier et al., 2010; Rybarczyk et al., 2012).
Depression, satisfaction with life, and functional independence (White et al., 2010) are correlated with resilience and they are important in modulating the rehabilitation outcome. These personal characteristics may be modifiable during rehabilitation. In the literature contrasting conclusions are reached on the relationships between physical health, mental health, depression and resilience.
Wagnild and Young (1993) found that high resilience scores were positively correlated with physical health and negatively correlated with depression. Staudinger and Fleeson (1996) remarked that extreme physical constraint seemed to limit the possibilities of resilience. Finally, our group has found that resilience interacts with disease in orthopedic surgery: low levels of resilience predict a poorer rehabilitation outcome in elderly hip-fractured patients. On the contrary, in elective surgery patients, no relationship was found between the level of resilience and patients’ autonomy at discharge (unpublished data).
The aim of the present study was to explore the relationships between resilience, frailty and quality of life in orthopedic rehabilitation patients. We were also interested in assessing whether these factors might affect rehabilitation outcome.
Materials and methods
Patients
In this open, prospective cohort study, we enrolled 81 orthopedic rehabilitation patients hospitalized between December 1, 2013 and December 31, 2014 in the rehabilitation department of the Istituto Ortopedico Gaetano Pini in Milan, Italy. All the patients underwent hip or knee surgery, which was either elective or post-traumatic (urgency) surgery.
The patients recruited were over 60 years old. Cognitive impairment, defined as a Mini-Mental State Examination (MMSE) score <15/30 (Yevasage et al., 1982–1983; Bellelli et al., 2008), was an exclusion criterion as it could lead to poor reliability of self-reported depressive symptoms or resilience. We also excluded patients who had an acute worsening of their clinical conditions and medical complications that necessitated their hospitalization in the acute department.
We obtained informed consent from all the patients during their rehabilitation stay. The study was approved by the Ethics Committee of Milan Area B, Italy.
Procedure
The resident doctors on the rehabilitation ward compiled the medical records and conducted the interviews and clinical examinations necessary in order to collect the patient baseline data which covered demographic characteristics (age, gender and living arrangement) and health, nutritional and cognitive status. Interviews with the patients were conducted within 24 hours of their admission to hospital.
All the patients underwent physical therapy rehabilitation sessions twice a day, six days a week throughout their hospital stay. The rehabilitation training included strengthening exercises and transfer, postural and gait training.
Within five days of admission the enrolled patients underwent a multidisciplinary assessment; this was repeated in the five days immediately prior to their discharge.
Resilience was measured using the Italian-validated version (Girtler et al., 2010) of the Wagnild and Young Resilience Scale (RS) (Wagnild and Young, 1993). Wagnild and Young considered five essential characteristics of resilience: a meaningful life (purpose), perseverance, self-reliance, equanimity, and coming home to yourself (existential aloneness). The original scale consisted of 25 items (RS-25) distributed among the five subscales listed above. All the items are assigned a score ranging from 1 “strongly disagree” to 7 “strongly agree”. Higher scores represent higher levels of resilience. In the 25-item version scores range from 25 to 175, where scores equal to or higher than 147 are considered indicators of a high degree of resilience, scores from 121 to 146 represent an intermediate degree, and scores below 121 reflect a low level of resilience. In order to facilitate the administration of the scale to older individuals and reduce missing data, an abbreviated 10-item version of the scale (RS-10) was employed. The RS-10 gives total scores ranging from 10 to 70.
To evaluate frailty, a comprehensive geriatric assessment was performed using the Multidimensional Prognostic Index (MPI), a tool that predicts short-and long-term mortality in elderly subjects (Pilotto et al., 2007). The MPI is a comprehensive tool that gives a final score calculated from the scores recorded in eight different domains: independent living skills are tested with the ADL (Activities of Daily Living) and IADL (Instrumental Activities of Daily Living) scales (Lawton and Brody, 1969); nutritional status is measured using the Mini Nutritional Assessment (MNA) (Vellas et al., 1999); and comorbidity is assessed using the Cumulative Illness Rating Scale (CIRS) (Linn, 1968). The MPI also includes the Exton-Smith scale (Bliss et al., 1966), which evaluates the risk of cutaneous lesions, and the Short Portable Mental Status Questionnaire (Pfeiffer, 1975); finally, the number of drugs used and cohabitation status are each assessed with a single item. Applying a complex method, the final MPI score, ranging from 0 to 1, was calculated. Three MPI score levels were identified, denoting low (0.0–0.33), medium (0.34–0.66), and high (0.67–1.0) risk of one-year mortality. In our study patients were stratified using these three MPI score levels.
Quality of life (QOL) was measured using the WHO Quality of Life-BRIEF (De Girolamo, 2000), which is a 26-item self-report instrument assessing four domains assumed to represent the QOL construct: physical, psychological, social relationships, and environment, as well as two items assessing overall QOL and general health. Higher scores denote higher levels of well-being.
The presence of depressive symptoms was assessed using the 15-item Geriatric Depression Scale (GDS), a widely used, clinician-administered or self-reported depression assessment scale (Yesavage and Sheikh, 1986; Pedrabissi and Santinello, 1991). The GDS may be used in healthy, medically ill, and mild to moderately cognitively impaired older adults. Scores of 0–4 are considered normal; scores of 5–8 indicate mild depression; scores of 9–11 indicate moderate depression; scores of 12–15 indicate severe depression.
Functional status was assessed using the Functional Independence Measure (FIM), a well-validated measure for assessing rehabilitation functional outcomes (Tesio et al., 2002). The scale comprises 18 items, of which 13 concern physical domains and five cognition. Items are scored according to the level of assistance required for an individual to perform ADL. Possible scores range from 18 to 126, with higher scores indicating a greater level of independence.
Measurement procedures
Statistical analyses were performed using the SPSS software, version 22.
RS-10
In a preliminary analysis, the RS-25 was administered to 45 patients hospitalized for rehabilitation following orthopedic surgery to the lower limbs. The 10 items considered most relevant by the authors were extrapolated and a total score was computed. The results of the two scales (RS-25 and RS-10) were compared by applying an appropriate test of variance, namely the Bonett method for non-normally distributed data. A statistically significant difference between the variances of the two scales in the 45-patient group failed to emerge (p=.061). We also computed Pearson’s correlation coefficient between the scores of the two scales, and a high, statistically significant correlation emerged (r = .91, p<.001). A regression analysis showed the presence of a linear relationship between the two scales: RS-10 scores justify about 83% of the variability of RS-25. These results are suggestive of equivalence between the 10-item version and the original scale. For the purposes of this study, it was decided to continue with the shorter version.
Descriptive analyses
Summary statistics were used to describe the sample. In order to identify differences in frailty conditions we stratified the sample on the basis of their MPI score level into three MPI classes (low, medium and high risk of one-year mortality).
Parametric (analysis of variance – ANOVA and posthoc Tukey HSD test) and non-parametric (Kruskal-Wallis ANOVA and Mann-Whitney test) statistics were employed to verify the existence of any differences in demographic, clinical and functional characteristics between the groups of patients.
Results
Participants
The final sample of 81 subjects was stratified into groups on the basis of MPI score: low risk (MPI-1, value ≤ 0.33), medium risk (MPI-2, value 0.34–0.66), and high risk of one-year mortality (MPI-3, value ≥ 0.67) (Pilotto et al., 2007).
The low-risk patients were found to number 56. They had a mean age of 74 years (range 60–94), and their mean length of hospital stay was 20.53 days. The medium-risk group comprised 25 patients with a mean age of 75.15 years (range 60–94). Their mean length of hospitalization was 21 days. In our sample there were no patients who could be classed as high risk, and therefore the MPI-3 class was not represented.
We thus analyzed two MPI classes: MPI-1 (low risk) and MPI-2 (medium risk). The two groups of patients were compared using appropriate tests to examine differences in demographic, clinical and functional characteristics: the independent samples t-test was used for interval variables with approximately-normal distribution and Fisher’s exact test for dichotomous variables. Comparisons between variables at baseline and discharge were assessed using the paired samples t-test or, for ordinal data, the Mann-Whitney test. The two groups were similar for demographic characteristics.
The participants were also divided into two groups on the basis of the frequency distribution of the RS score on admission (in reference to the median score of 58): those who gave a high score (RS >58: high-RS) and those who gave a low score (RS ≤58: low-RS). Descriptive statistics (means and standard deviations) for the two MPI classes are reported in table I.
Table I.
Mean values (and standard deviations) of all measures in the MPI-1 and MPI-2 classes.
| MPI-1 | MPI-2 | Total | |
|---|---|---|---|
| WQoL (admission) | 62.79 (13.24) | 62.55 (13.61) | 62.65 (13.1) |
| WQoL (discharge) | 64.14 (12.43) | 64.36 (13.01) | 64.41 (12.54) |
| RS (admission) | 57.37 (7.96) | 57.21 (8.16) | 57.23 (8.01) |
| RS (discharge) | 57.67 (8.43) | 57.83 (8.60) | 57.74 (8.40) |
| FIM (admission) | 101.92 (15.48) | 102.11 (15.70) | 101.85 (15.29) |
| FIM (discharge) | 110.72 (14.13) | 110.96 (14.54) | 110.82 (13.94) |
Abbreviations: MPI-1=low risk of one-year mortality; MPI-2=medium risk of one-year mortality; WQoL=WHO Quality of Life-BRIEF; RS=Resilience Scale; FIM=Functional Independence Measure.
MPI and resilience on admission and at discharge and relationships with FIM
The RS scores recorded at the beginning were similar to those recorded at the end of the treatment both in the MPI-1 and the MPI-2 patients. The patients showing high resilience (high-RS) had higher FIM scores, both on admission and at discharge, than those showing low resilience (Mann-Whitney test: respectively, p=.006, p=.001). Since the patients were divided not only into two MPI classes but also into two resilience groups (low-RS and high-RS, using the median resilience scale score of the whole sample as the cutoff value, as mentioned), it was possible to further classify them into four groups: low risk and low resilience (MPI-1+low-RS, group 1), low risk and high resilience (MPI-1+high-RS, group 2), medium risk and low resilience (MPI-2+low-RS, group 3) and medium risk and high resilience (MPI-2+high-RS, group 4).
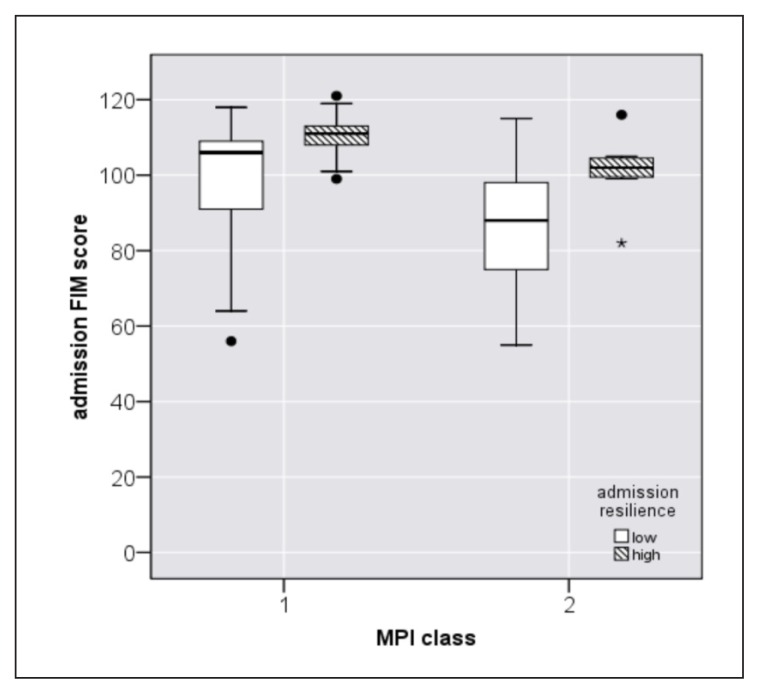
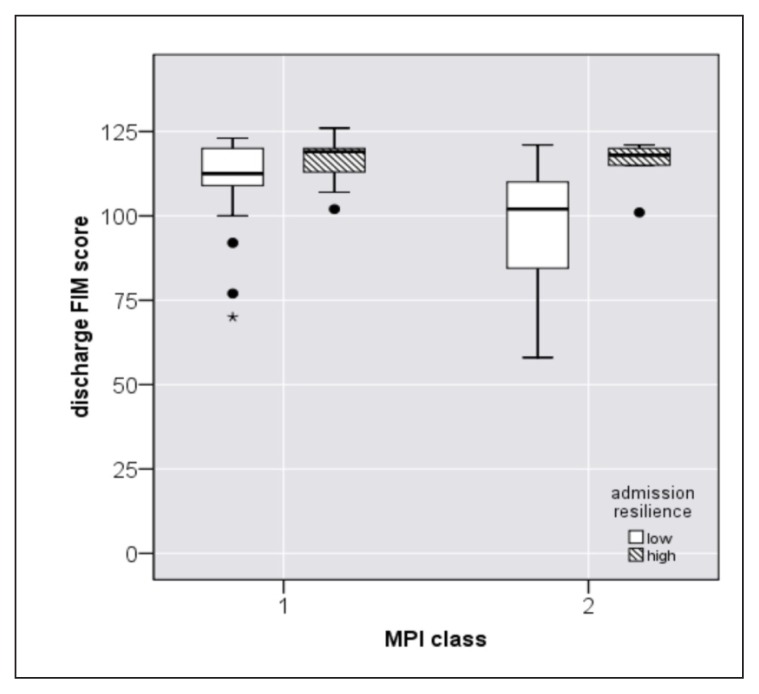
Figure 1 shows that the frail (MPI-2) patients with high resilience on admission recorded higher FIM scores on admission, compared with those with low resilience on admission (Mann-Whitney test: p=.02). Figure 2 shows that frail (MPI-2) patients with a high RS score on admission also had a higher FIM score at discharge compared with MPI-2 patients with a low RS score on admission (Mann-Whitney test: p=.02).
Figure 1.
Relationships between admission resilience, MPI class and FIM score on admission.
Figure 2.
Relationships between admission resilience, MPI class and FIM score at discharge.
Interaction variables
Age
In the MPI-2 class, no difference in age was found between the patients classed as high-RS and low-RS at discharge.
Surgery
Urgency and elective surgery were similarly represented in groups 1, 2, 3 and 4 (Table II, Fisher’s exact test: p=.20).
Table II.
Elective surgery and urgency surgery in the four groups.
| MPI-1, RS-low | MPI-1, RS-high | MPI-2, RS-low | MPI-2, RS-high | |
|---|---|---|---|---|
| Elective surgery | 16 | 19 | 4 | 5 |
| Urgency surgery | 10 | 10 | 9 | 3 |
| Ratio | .4 | .3 | .7 | .4 |
Abbreviations: MPI-1=low risk of one-year mortality; MPI-2=medium risk of one-year mortality; RS-low=low resilience; RS-high=high resilience.
Depression
In the MPI-2 class, patients with depression on admission were similarly distributed between the low-RS and high-RS groups (Table III, Fisher’s exact test: p=.60); the same was found when analyzing those with depression at discharge (Table IV, Fisher’s exact test: p=.60, respectively).
Table III.
Depression status on admission in the MPI classes.
| MPI-1, RS-low | MPI-1, RS-high | MPI-2, RS-low | MPI-2, RS-high | |
|---|---|---|---|---|
| No admission depression | 19 | 28 | 8 | 6 |
| Admission depression | 6 | 0 | 4 | 1 |
| Ratio | .2 | .0 | .3 | .1 |
Abbreviations: MPI-1=low risk of one-year mortality; MPI-2=medium risk of one-year mortality; RS-low=low resilience; RS-high=high resilience.
Table IV.
Depression at discharge in the MPI classes.
| MPI-1, RS-low | MPI-1, RS-high | MPI-2, RS-low | MPI-2, RS-high | |
|---|---|---|---|---|
| No discharge depression | 22 | 26 | 8 | 6 |
| Discharge depression | 4 | 1 | 4 | 1 |
| Ratio | .2 | .0 | .3 | .1 |
Abbreviations: MPI-1=low risk of one-year mortality; MPI-2=medium risk of one-year mortality; RS-low=low resilience; RS-high=high resilience.
Regression analysis
A linear regression analysis was performed to examine the influence of the levels of resilience, frailty, QOL and kind of surgery on functional status. Resilience, MPI, WHO Quality of life-BRIEF, kind of surgery (elective vs urgency) and admission FIM score were taken as independent variables and FIM score at discharge as the dependent variable. The model was statistically significant (R2 = .40, F(5,41) = 15.57, p<.001). The results are reported in table V.
Table V.
Linear regression analysis: influence of admission RS, WQoL, MPI and FIM scores and kind of surgery on FIM score at discharge.
| Predictors | Beta | T | p |
|---|---|---|---|
| RS (on admission) | .45 | 4.02 | <.001 |
| WQoL (on admission) | .25 | 2.21 | <.05 |
| MPI (on admission) | −.09 | −.79 | .43 |
| FIM (on admission) | .68 | 5.50 | <.001 |
| Surgery (elective/urgency) | −.07 | −.90 | .39 |
Abbreviations: RS=Resilience Scale; WQoL=WHO Quality of Life-BRIEF; MPI= Multidimensional Prognostic Index; FIM=Functional Independence Measure
The levels of the indicators resilience, QOL and functional status (i.e. FIM) measured on admission appeared to be significant positive predictors of the functional status at discharge. On the contrary, the level of frailty and the kind of surgery were not found to be significant predictors of the FIM score at discharge. These results indicate that higher levels of resilience, QOL and functional status successfully predict the functional outcome that patients achieve at discharge.
Discussion
In the literature there are many studies examining factors associated with orthopedic surgery, rehabilitation and comorbidities (Cully et al., 2005). The concept of frailty, a status suggested to reflect decreased physiological reserves across multiple organ systems, arising from cumulative comorbid conditions (Fried et al., 2004; Rockwood and Mitnitski, 2011), has been developed to account for the physiological changes that impair functional reserve and increase vulnerability to disability. The prevalence of frailty in geriatric surgical patients was found to be higher than in a control population (Partridge et al., 2012).
Frailty could also increase the risk of psychological problems (Fried et al., 2004), and the concept of resilience (Wagnild and Young, 1993) was introduced in an attempt to shed light on different psychological reactions to adversity. Although many studies have demonstrated relationships between depression and functional outcome (Penninx et al., 1999) and between outcome and frailty, the role of frailty and resilience in elderly individuals in rehabilitation settings has not yet received adequate attention. For this reason, studies in rehabilitation settings should include measures of frailty and resilience.
Our paper investigated adults older than 60 years who had undergone orthopedic surgery and were hospitalized in a rehabilitation ward. This study produced several findings. First of all, it supported the use of the shortened version of the RS scale (RS-10) as a valid instrument for measuring resilience. Indeed, the RS-10 was found to justify more than 80% of the variability of the RS-25, and the short version of the scale was found to show adequate content validity.
Second, we described an association between resilience and disability and found that this association interacted with frailty level. In detail, resilience and frailty were associated in determining functional status at the beginning of the rehabilitation stay. Low resilience and a condition of frailty were associated with a poorer functional status at onset, whereas high resilience was associated with higher functional status on admission and at discharge.
We also found a positive association between level of resilience, QOL, kind of surgery, and functional status. Our model showed that the level of resilience, quality of life and admission functional status successfully predict the functional outcome reached at discharge.
Although we found a relationship between frailty, resilience, kind of surgery and functional status, frailty itself did not emerge as a significant predictor of FIM score. This finding shows that many factors are involved in determining an unfavorable health status, and that further multidimensional research is required. In the present study we decided not to use FIM improvement during rehabilitation (“delta FIM”: discharge FIM vs admission FIM) as the main indicator of outcome, but rather to focus on the relationship between resilience, frailty and functional status first on admission and then at discharge. Indeed, we wanted to highlight the role of resilience and frailty in determining patients’ functional status at these specific times. After all, our aim is to have patients who are independent when they return to their lives, and not only to improve their level of independence during the rehabilitation program. The aim of a geriatric rehabilitation unit is to restore functional status in elderly patients so that their disabilities will not cause physical and social decline; in other words, it aims to preserve their QOL.
In our regression model, the kind of surgery (elective vs urgency) was not itself found to predict the FIM score at discharge. This issue requires further investigation.
Another important finding in our sample was that depression was similarly distributed in the different frailty groups. We did not find an association between frailty and depressive symptoms. However, the small sample did not allow further statistical analyses on depression or on the relationships between depression, frailty and resilience.
Limitations
Some limitations of this study should be acknowledged. First of all the small size of the sample did not allow us to perform more complex analyses to test the independence of the relationships between resilience and functional outcome.
There were also confounding factors such as the FIM score at the start of the treatment. For this reason we cannot conclude that there exists a linear connection between resilience, frailty and disability.
Conclusions
Many factors influence functional recovery after orthopedic surgery in the elderly. Resilience and frailty play an important role, and they interact in determining the functional outcome. We strongly support the use of multidimensional evaluation of the elderly in rehabilitation settings. Screening for low resilience and frailty at initial assessment enables patients with lower rehabilitation potential to be identified, and should therefore be introduced. The possibility of identifying frail and non-resilient patients represents an opportunity for improving early functional outcome.
It is now clear that every patient needs to be prescribed a personal rehabilitation program. Identifying frail patients is one way of ensuring that therapeutic programs are suitable for the individuals concerned and will allow them to achieve their own best level of performance. From this perspective it is very important to evaluate all the variables that could modify performance status: cognitive impairment, depression, family support and the environment. The findings from this study endorse the call for evaluation models that are in line with the International Classification of Functioning, Disability and Health model, in other words models that are not based solely on the organic consequences of diseases, but also focus on the personal factors, environmental factors, and social and economic factors that could help to boost an individual’s performance in ADL and level of participation (WHO, 2001).
References
- Adonizio G, Alexopoulos GS. Affective disorders in the elderly. Int J Geriatr Psychiatry. 1993;8:41–47. [Google Scholar]
- Bellelli G, Frisoni GB, Turco R, et al. Depressive symptoms combined with dementia affect 12-months survival in elderly patients after rehabilitation post-hip fracture surgery. Int J Geriat Psychiatry. 2008;23:1073–1077. doi: 10.1002/gps.2035. [DOI] [PubMed] [Google Scholar]
- Bliss MR, McLaren R, Exton-Smith AN. Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv. 1966;25:238–268. [PubMed] [Google Scholar]
- Bombardier CH, Ehde DM, Stoelb B, et al. The relationship of age-related factors to psychological functioning among people with disabilities. Phys Med Rehabil Clin N Am. 2010;21:281–297. doi: 10.1016/j.pmr.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Cully JA, Gfeller JD, Heise RA, et al. Geriatric depression, medical diagnosis, and functional recovery during acute rehabilitation. Arch Phys Med Rehabil. 2005;86:2256–2260. doi: 10.1016/j.apmr.2005.07.292. [DOI] [PubMed] [Google Scholar]
- Davey M, Eaker DG, Walters LH. Resilience processes in adolescents: personality profiles, self-worth, and coping. Journal of Adolescent Research. 2003;18:347–362. [Google Scholar]
- De Girolamo G, Rucci P, Scocco P, et al. Quality of life assessment: validation of the Italian version of the WHO-QOL-Brief. Epidemiol Psichiatr Soc. 2000;9:45–55. doi: 10.1017/s1121189x00007740. [DOI] [PubMed] [Google Scholar]
- Dubljanin Raspopović E, Marić N, Nedeljković U, et al. Do depressive symptoms on hospital admission impact early functional outcome in elderly patients with hip fracture? Psychogeriatrics. 2014;14:118–123. doi: 10.1111/psyg.12049. [DOI] [PubMed] [Google Scholar]
- Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- Friedman SM, Mendelson DA, Bingham KW, et al. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169:1712–1717. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- Gantner AB, Schubert DS, Wolf SR, et al. Screening for depression in a rehabilitation sample. Int J Psychiatry Med. 2003;33:333–41. doi: 10.2190/YMVW-7HVE-QHQN-TUTW. [DOI] [PubMed] [Google Scholar]
- Girtler N, Casari EF, Brugnolo A, et al. Italian validation of the Wagnild and Young Resilience Scale: a perspective to rheumatic diseases. Clin Exp Rheumatol. 2010;28:669–678. [PubMed] [Google Scholar]
- Iolascon G, Cervone M, Gimigliano R, et al. Neuropsychiatric disorders in hip fracture. Clin Cases Miner Bone Metab. 2011;8:49–53. [PMC free article] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kim SW, Han HS, Jung HW, et al. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg. 2014;149:633–640. doi: 10.1001/jamasurg.2014.241. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41:142–147. doi: 10.1093/ageing/afr182. [DOI] [PubMed] [Google Scholar]
- Pedrabissi L, Santinello M. Contributo all’adattamento italiano e taratura della Geriatric Depression Scale. Bollettino di Psicologia Applicata. 1991;198:3–7. [Google Scholar]
- Penninx BW, Leveille S, Ferrucci L, et al. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pilotto A, Franceschi M, Ferrucci L. A multidimensional Prognostic Index (MPI) for the evaluation of the hospitalized frail older patient. Giornale di Gerontologia. 2007;55:7–10. [Google Scholar]
- Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27:17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Rybarczyk B, Emery EE, Guequierre L, et al. The role of resilience in chronic illness and disability in older adults. Annual Review of Gerontology and Geriatrics. 2012;32:173–187. [Google Scholar]
- Staudinger UM, Fleeson W. Self and personality in old and very old age: A sample case of resilience? Development and Psychopathology. 1996;8:867–885. [Google Scholar]
- Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. 2011;52:199–209. doi: 10.1016/j.psym.2011.01.036. [DOI] [PubMed] [Google Scholar]
- Tesio L, Granger CV, Perucca L, et al. The FIM instrument in the United States and Italy: a comparative study. Am J Phys Med Rehabil. 2002;81:168–176. doi: 10.1097/00002060-200203000-00003. [DOI] [PubMed] [Google Scholar]
- Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–122. doi: 10.1016/s0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1:165–178. [PubMed] [Google Scholar]
- Walston J, Fried LP. Frailty and the older man. Med Clin North Am. 1999;83:1173–1194. doi: 10.1016/s0025-7125(05)70157-7. [DOI] [PubMed] [Google Scholar]
- White B, Driver S, Warren AM. Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabil Psychol. 2010;55:23–32. doi: 10.1037/a0018451. [DOI] [PubMed] [Google Scholar]
- White B, Driver S, Warren AM. Considering resilience in the rehabilitation of people with traumatic disabilities. Rehabil Psychol. 2008;53:9–17. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva: WHO; 2001. [Google Scholar]
- Yi-Frazier JP, Smith RE, Vitaliano PP, et al. A person-focused analysis of resilience resources and coping in diabetes patients. Stress Health. 2010;26:51–60. doi: 10.1002/smi.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Sheikh JI. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist. 1986;5:165–173. [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 17:1982–1983. 37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]