Abstract
Purpose
the purpose of the present paper is to present the short-term results of a “detachment-free” (DF) anterolateral approach for primary total hip replacement (THR) performed in a large series of patients.
Methods
two hundred patients submitted to primary THR were retrospectively reviewed for the present study. In all cases, the surgery was performed using a minimally invasive DF anterolateral approach, which entails no disconnection of tendons and no muscle damage. The study population consisted of 96 men (48%) and 104 women (52%), with an average age of 69.4 years (range 38–75). Clinical and radiographic follow-up was performed after 12 months.
Results
the clinical results, evaluated using the Harris Hip Score, were excellent in 95% of the cases and good in 5%; no cases had fair or poor results. X-rays taken at 3, 6 and 12 months after surgery did not show heterotopic ossification, mobilization of the prosthetic components, or hip dislocation. No infections, deep vein thrombosis, or failure of the gluteal muscles were reported.
Conclusions
the DF anterolateral approach for THR proved safe and provided effective results at short-term follow-up.
Level of evidence
Level IV, therapeutic case series.
Keywords: anterolateral, approach, arthroplasty, hip, replacement
Introduction
In recent decades total hip replacement (THR) surgery has improved in terms of prosthetic designs, hardware materials, anesthetic modalities, surgical technique and postoperative care.
The last decade, in particular, has seen the establishment of minimally invasive surgery (MIS), characterized by less invasive surgical approaches and greater respect for soft tissues. The now established practice of incision in the intermuscular septum respects both the muscle bellies and the tendon insertions. The most common approaches (direct lateral, anterolateral, posterolateral and posterior), although necessitating small incisions, cause minimal damage to the muscle and/or to the tendon (1). Nevertheless the greater sparing of the muscles and tendons means that there is less postoperative bleeding and pain. Thanks to preservation of muscle strength and joint proprioception (1, 2), all this translates into a considerable advantage from the perspective of rehabilitation and reduces the complications typical of the standard approaches. This is particularly important for women, who have less muscle mass and are therefore less able to tolerate muscle damage after THR (3). MIS is not indicated in cases of revision surgery, obesity, severe congenital hip dysplasia, osteoporosis or severe joint stiffness, because of the risk of fracture of the greater trochanter.
In recent years, we have developed and optimized a minimally invasive anterolateral approach, defined “detachment free” (DF) since it does not involve any muscle or tendon detachment; it is performed under spinal anesthesia, with the patient in the supine position, and it does not require the use of dedicated surgical instruments (4, 5). The purpose of the present study is to present the short-term results of this technique applied in a large series of patients. The hypothesis of the study was that the DF anterolateral approach provides safe and effective results in THR.
Methods
Participants
Two hundred patients submitted to primary THR were retrospectively reviewed for the present study. All the surgical procedures were performed by a single surgeon who used our minimally invasive DF anterolateral approach. The study population consisted of 96 men (48%) and 104 women (52%), with an average age of 69.4 years (range 38–75). As regards their basic pathology, 168 cases (84%) had primary hip osteoarthritis (OA), 8 (4%) had OA secondary to congenital hip dysplasia (Crowe grade I–II), and 24 (12%) had post-traumatic hip OA secondary to femoral neck fracture.
The prosthetic implants used consisted of Delta PF Cup and C2 Stem (Lima Corporate, San Daniele del Friuli, Italy) in 150 cases (75%), R3 Cup and Nanos Stem for the preservation of the femoral neck (Smith & Nephew, Andover, MA, USA) in 35 cases (17.5%), and R3 Cup and SMF Stem (Smith & Nephew) in 15 cases (7.5%). Ceramic-ceramic coupling was used in all the cases.
Surgical technique
The patient, in L2–L3 spinal anesthesia induced by 17 mg of 1% marcaine and 150 μg of morphine, lies supine on the operating table with the legs parallel and no support or forced posture of the contralateral limb. The most proximal part of the femoral diaphysis and the apex of the greater trochanter are identified and, with respect to the latter landmark, a slightly curved incision of approximately 10 cm is made, extended distally for 1/3 and proximally for 2/3 (Fig. 1). After the incision and opening of the subcutaneous tissues and muscles, the interstice between the fascia lata tensor muscle and the gluteus minimus and medius muscle is identified, cauterizing the vessels. The front of the joint capsule is exposed, inserting a Hohmann retractor on the rear side of the capsule, a second Hohmann rectractor on the front side, and a third on the front wall of the acetabulum (Fig. 2). Reverse-T-shaped capsulotomy and resection and removal of the femoral neck are performed with the limb in external rotation. The capsulectomy is completed and the Hohmann retractors are repositioned on the front and rear edge of the acetabulum and in the acetabular notch. The acetabulum is prepared and the implantation of the acetabular component is carried out (Fig. 3).
Fig. 1.
Skin landmarks skin are drawn and a slightly curved incision of approximately 10 cm is made.
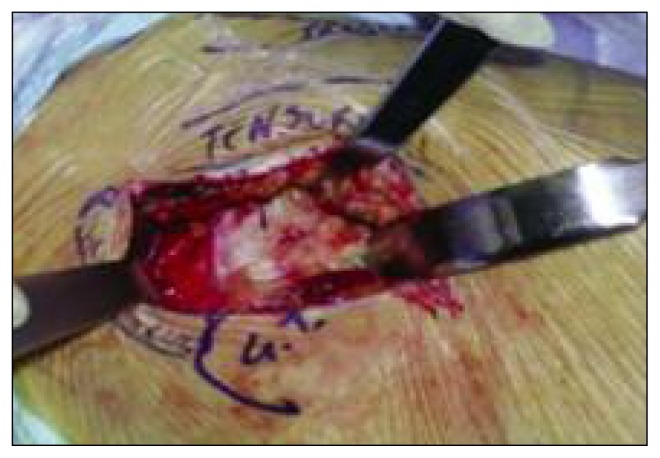
Fig. 2.
Divergence of subcutaneous and muscles and exposure of the joint capsule using three Hohmann retractors.
Fig. 3.
Positioning the metal shell thanks to excellent exposure of the acetabulum.
The rear flap of the fascia is incised transversely at the apex of the greater trochanter; it is then externally rotated and the hip is abducted, moving the limb over the contralateral one. This procedure demands an adequate degree of muscle relaxation, obtained through the administration of an average of 1.2 mg of propofol by syringe pump, and control of spontaneous breathing, by means of end-tidal CO2 (ETCO2) through a face mask, and administration of O2 with fraction of inspired O2 (Fi O2) of 0.4. Control of pain and of sympathetic hypertonia in spontaneous breathing is achieved through this technique and is followed by a rapid recovery of consciousness. Reduction of the muscle tone of the treated limb is essential in order to implement the DF technique. With the hip externally rotated and abducted, a first Hohmann retractor is positioned at the small trochanter, a second retractor at the greater trochanter, in order to retract the gluteal muscles, and a third lever at the proximal end of the greater trochanter to lift and better expose the femur.
The femoral canal is prepared for the trial implant and for testing stability, mobility and length of the limb. The femoral stem and the related head are then implanted, the prosthesis is reduced and finally the range of motion (ROM), stability and length of the limb are evaluated. Two drains (intraarticular and subfascial) are positioned and wound closure is carried out.
Postoperative care
After surgery, antibiotic prophylaxis is carried out for 36 hours together with antithromboembolic, pharmacological and mechanical (plantar pumps and elastic stockings) prophylaxis. Pain is controlled through the intravenous infusion of tramadol 200 ml and ketorolac 60 mg in 500 ml saline. Since the muscle-tendon structures are spared, prophylaxis for heterotopic ossification is not carried out. On removal of the drains, after 24 hours, radiographs are performed and the patient assumes a sitting position on the bed. Rehabilitation begins on the day of the surgery, with isometric and isotonic contractions of the gluteal muscles and the quadriceps muscle, while assisted weight bearing on two legs is allowed on the second day and lasts for 21 days. From the fourth week, free total weight bearing is allowed.
Outcome measurements
The patients were clinically evaluated using the Harris Hip Score (6). Radiographic evaluation consisted of a weight-bearing X-ray of the pelvis to assess possible heterometric compensation.
Thigh circumference was measured at the level of the greater trochanter as a potential predictor of outcome; thigh circumference can be considered a more reliable and accurate measure of local fat distribution than body mass index (BMI), since it is not affected by distribution of the lean and fat mass in the various sites of the body (7, 8). Blood count before and after surgery and duration of hospitalization were also recorded.
Results
The surgery was performed with no difficulty in patients with a thigh circumference up to 70 cm and with some difficulty in those with a thigh circumference measuring up to 80 cm, whereas it was not possible if the measurement was over 80 cm. Before the surgery, the average hemoglobin value was 13.5 g/dl and the average hematocrit value was 39.6%; 24 hours after surgery, the values were 11.2 g/dl and 33.8%, respectively. Seven patients (3.5%) were transfused with one unit of autologous blood and 2 patients (1%) with one unit of packed red blood cells, due to unsuitable predeposits. The average duration of hospitalization was 4.9 days (range 4–6 days). There were no complications in the postoperative phase.
At 12-month follow-up the clinical results, evaluated using the Harris Hip Score, were excellent in 95% of cases and good in 5% of cases; no patient had fair or poor results. In particular, no patient complained of groin and/or trochanteric pain and any preoperative leg length discrepancy had been corrected in all cases. X-rays taken at 3, 6 and 12 months after surgery did not show heterotopic ossification or mobilization of the prosthetic components. There were no cases of infection, deep vein thrombosis, hip dislocation or failure of the gluteal muscles (Trendelemburg sign).
Discussion
There exist different approaches to primary THR. Each surgeon uses the approach he/she is most confident with, in order to obtain a good implant; an approach may be defined minimally invasive if good positioning of the prosthesis is associated with sparing of all the anatomical structures not affected by OA. Sparing of the periarticular muscles, in particular, is very important. This is because the separation and reinsertion of a tendon, even when there is good healing, involves local “biological fatigue” and entails a prolonged motor recovery time, because of impaired proprioception and reduction in muscle strength (1) with a temporary Trendelemburg gait (incidence of 5.7% in the non-minimally invasive anterolateral approach) (9). Lin et al. (10) evaluated muscle strength and walking speed in 53 patients with THR implanted using a mini-invasive anterolateral approach, comparing them with 53 patients treated with a conventional anterolateral approach. In the first 12 months, the patients in the first group had significantly greater muscle strength, a greater walking speed, and a better functional score. One year after the surgery, the performance was statistically equivalent in the two groups. Comparing movements in vivo and contact forces during walking in patients with THR implanted using either a mini-invasive or a standard approach, Glaser et al. (11) found that the average maximal values of the forces applied on the prosthetic components were lower in the patients with prosthesis implanted using a mini-invasive approach. They suggested that sparing of the muscle-tendon structures may reduce the weight-bearing forces at the head-acetabulum interface, thus resulting in greater stability of the implant. The maintenance of muscle strength is particularly important for women, since they have a significantly lower muscle volume; minimally invasive surgery allows them to achieve a more rapid and complete functional recovery.
In the sample examined, thanks to the minimal muscle-tendon trauma and reduced blood loss, there were no cases of heterotopic ossification. In fact, surgical insult to the abductors, especially in men (because of their greater muscle mass), may result in heterotopic ossification, a frequent complication in prosthetic surgery with an incidence ranging from 15 to 90% (12, 13); in addition to the tissue damage, blood transfusion is another of the factors predisposing to the development of heterotopic ossification (14).
The smaller wound, shorter surgical time, reduced blood loss, and absence of periarticular hematomas in MIS are all factors protecting against possible early infections. Moreover, the functional recovery is faster and the rehabilitation and hospitalization times are reduced. Duwelius et al. (15) compared the duration and cost of hospitalization in a group of 214 patients treated using a mini-invasive surgical approach and a group of 265 patients treated using a standard surgical approach; they found that in the first group the hospital stay was on average 2.3 days shorter and the cost approximately $ 3.9 thousand less per patient.
Finally, in order to achieve an esthetically acceptable surgical scar, it is necessary to use the “floating window” principle; this makes it possible to avoid the damage to the skin and soft tissues that can result from the strong retractor pressures needed when a limited skin incision is used (16).
In conclusion, like all surgical techniques, the DF anterolateral approach in total hip replacement has a learning curve that depends directly on the surgeon’s experience with the standard surgical approaches. Correct patient selection and precise execution of the incision and anesthetic relaxation are indispensable for correct execution of the DF surgical approach.
References
- 1.Wojciechowski P, Kusz D, Kopeć K, et al. Minimally invasive approaches in total hip arthroplasty. Ortop Traumatol Rehabil. 2007;9:1–7. [PubMed] [Google Scholar]
- 2.Tang Z. Minimally invasive total hip replacement. Issues Emerg Health Technol. 2004;(60):1–4. [PubMed] [Google Scholar]
- 3.Preininger B, Schmorl K, Von Roth P, et al. The sex specificity of hip-joint muscles offers an explanation for better results in men after total hip arthroplasty. Int Orthop. 2012;36:1143–1148. doi: 10.1007/s00264-011-1411-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bopp F. Total hip arthroplasty with a less invasive anterolateral approach. Z Orthop Unfall. 2014;152:117–118. doi: 10.1055/s-0034-1368207. [DOI] [PubMed] [Google Scholar]
- 5.Graf R, Mohajer MA. The Stolzalpe technique: a modified Watson-Jones approach. Int Orthop. 2007;31(Suppl 1):S21–S24. doi: 10.1007/s00264-007-0437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dettoni F, Pellegrino P, La Russa MR, et al. Validation and cross cultural adaptation of the Italian version of the Harris Hip Score. Hip Int. 2015;25:91–97. doi: 10.5301/hipint.5000184. [DOI] [PubMed] [Google Scholar]
- 7.Bray GA. Overweight is risking fate. Definition, classification, prevalence and risks. Ann N Y Acad Sci. 1987;499:14–28. doi: 10.1111/j.1749-6632.1987.tb36194.x. [DOI] [PubMed] [Google Scholar]
- 8.Grano GF. Minimally invasive anterolateral approach in primary hip prosthetic surgery: notes of surgical technique. Medit J Surg Med. 2002;10:59–62. [Google Scholar]
- 9.Edmunds CT, Boscainos PJ. Effect of surgical approach for total hip replacement on hip function using Harris Hip scores and Trendelenburg’s test. A retrospective analysis. Surgeon. 2011;9:124–129. doi: 10.1016/j.surge.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Lin DH, Jan MH, Liu TK, et al. Effects of anterolateral minimally invasive surgery in total hip arthroplasty on hip muscle strength, walking speed and functional score. J Arthroplasty. 2007;22:1187–1192. doi: 10.1016/j.arth.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Glaser D, Dennis DA, Komistek RD, et al. In vivo comparison of hip mechanics for minimally invasive versus traditional total hip arthroplasty. Clin Biomech (Bristol, Avon) 2008;23:127–134. doi: 10.1016/j.clinbiomech.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Ahrengart L. Periarticular heterotopic ossification after total hip arthroplasty. Risk factors and consequences. Clin Orthop Relat Res. 1991;(263):49–58. [PubMed] [Google Scholar]
- 13.Pavlou G, Salhab M, Murugesan L, et al. Risk factors for heterotopic ossification in primary total hip arthroplasty. Hip Int. 2012;22:50–55. doi: 10.5301/HIP.2012.9057. [DOI] [PubMed] [Google Scholar]
- 14.Fransen M, Neal B, Cameron ID, et al. Determinants of heterotopic ossification after total hip replacement surgery. Hip Int. 2009;19:41–46. doi: 10.1177/112070000901900108. [DOI] [PubMed] [Google Scholar]
- 15.Duwelius PJ, Moller HS, Burkhart RL, et al. The economic impact of minimally invasive total hip arthroplasty. J Arthroplasty. 2011;26:883–885. doi: 10.1016/j.arth.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Mow CS, Woolson ST, Ngarmukos SG, et al. Comparison of scars from total hip replacements done with a standard or a mini incision. Clin Orthop Relat Res. 2005;441:80–85. doi: 10.1097/01.blo.0000191317.85422.c3. [DOI] [PubMed] [Google Scholar]