Abstract
Purpose
the purpose of this study is to describe a new arthroscopic technique for reduction and fixation of coronoid process fractures (CPFs) and report clinical and functional results in 4 patients after a 24-month follow-up.
Methods
four patients underwent arthroscopic reduction and fixation of isolated CPFs (acute or non-unions, type I or type II according to the Regan-Morrey classification) performed using a new technique based on coronoid tunnelling and capsular plication. The patients were evaluated 6, 12 and 24 months after surgery, using the Disability of the Arm, Shoulder and Hand scale (DASH), the Mayo Elbow Performance Index (MEPI), and a visual analog scale (VAS); elbow range of motion (ROM) and joint stability were also evaluated and the rate of complications was reported.
Results
all 4 patients completed the follow-up. At 6, 12 and 24 months, respectively, they recorded mean DASH scores of 22, 14 and 7, mean MEPI scores of 74, 82 and 94, and mean VAS scores of 4, 2 and 1. The mean ROM increased in all directions (at 6, 12 and 24 months, respectively: flexion: 112°, 125°, 144°; extension: 3°, 5°, 6°; pronation: 76°, 84°, 91°; supination: 78°, 82°, 86°). No signs of instability were observed and no complications were reported.
Conclusions
the new all-arthroscopic coronoid tunnelling and capsular plication technique here proposed can restore elbow function, ROM and stability and allows anatomical reconstruction of the joint after type I or type II CPFs. If performed by an experienced arthroscopist, it is a valid alternative to open reduction and external fixation.
Level of evidence
Level IV, retrospective case series.
Keywords: bone tunnelling, coronoid, fracture, capsular plication, elbow arthroscopy
Introduction
The coronoid process of the ulna is fundamental for elbow function and stability (1–3) and coronoid process fractures (CPFs) are, indeed, often associated with elbow instability. Surgical management of these fractures through open reduction and internal fixation (4, 5) has increased in popularity in recent years, while approaches such as excision or expectant management have often proved unsatisfactory (6–8). The coronoid process prevents posterior elbow dislocation by countering the posteriorly directed forces generated on the ulnohumeral joint by all the major muscles that cross the elbow joint (9). The radial head is the other static stabilizer against posterior dislocation, and this explains why CPFs are more serious when they are combined with radial head fractures (10–12). Loss of 50% of the coronoid process height creates a potentially unstable situation, especially in the absence of the radial head (13–17). Coronoid process height loss can be assessed by drawing a line through the tip of the posterior olecranon, parallel to the ulnar shaft; loss of height beyond this level can result in instability (18). CPFs can be classified into three types according to their height, as described by Regan and Morrey (19). Instead, O’Driscoll et al. (20) introduced a more extensive classification that is based on computed tomography (CT) scan evaluation and takes into account the site and size of the fracture and the injury mechanism. According to these Authors, tip fractures are caused by a posterolateral rotatory injury mechanism, anteromedial fractures are caused by a varus pos-teromedial injury mechanism and may be associated with joint subluxation, while body fractures involve the base of the coronoid process and are most commonly observed in association with posterior transolecranon fracture-dislocations (20). Surgical treatment in CPFs is recommended in the presence of varus posteromedial rotatory instability and valgus posterolateral rotatory instability. Moreover, the size and morphology of the coronoid fracture, the degree of elbow instability, and injuries to associated structures must always be taken into account. Early diagnosis and proper treatment may reduce recovery time and improve outcomes (4, 5). The purpose of this study is to describe a new, entirely arthroscopic technique for arthroscopic reduction and fixation of CPFs and to assess clinical and functional results in 4 patients with a 24-month follow-up.
Methods
Four consecutive patients (3 men and 1 woman; mean age 37 years) with isolated acute CPF (2) or CPF non-union (2) were retrospectively enrolled. The inclusion criteria were type I or type II CPF according to the Regan-Morrey classification and CT (Fig. 1) or magnetic resonance imaging evidence of isolated fragment(s) of the coronoid process. All patients gave their informed consent before being included in the study.
Fig. 1.
3D CT scan of a right elbow. The image shows a fracture of the coronoid process of the ulna.
All the patients underwent surgical reduction and fixation performed using an all-arthroscopic technique consisting of coronoid tunnelling and capsular plication.
The right side was affected in 2 patients and the left side in 2 patients. On clinical examination, all the patients complained of elbow instability and severe pain at the posterior and medial aspects of the elbow.
Surgical technique
Arthroscopic treatment was performed using an axillary block and mild general anesthesia. A pneumatic tourniquet was positioned high in the axilla and inflated to 250 mmHg after limb exsanguination. The patient was placed in a modified lateral decubitus position with the operative arm positioned in 100° flexion/90° internal rotation at the level of the shoulder and held in place by an arm holder. The elbow was positioned in 90° of flexion, with the forearm hanging free under gravity (Fig. 2). Before establishing the portals, the elbow joint was distended by injecting sterile saline solution (30 cc) through an 18-gauge needle inserted via the proximal posterior portal.
Fig. 2.
Patient positioning: modified lateral decubitus position with the operative arm positioned in 100° flexion/90° internal rotation at the level of the shoulder and held in place by an arm holder. The elbow is positioned in 90° of flexion, with the forearm hanging free under gravity.
The anterior compartment was then addressed. A proximal anteromedial portal was created 2 cm proximal to the medial humeral epicondyle and 1 cm anterior to the intramuscular septum.
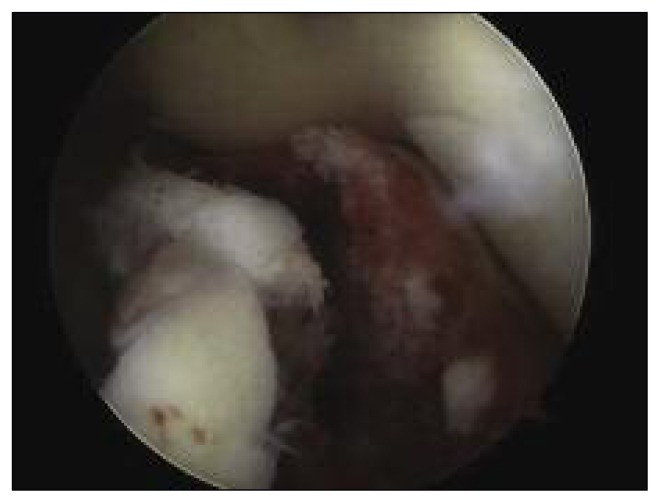
Insertion of a 30° scope into this portal allows intra-articular diagnostic evaluation. An anterolateral portal was then created as well and this side was visualized. After diagnostic evaluation of the CPF (Fig. 3), the procedure was then performed according to the following protocol: a suture passer is introduced through an accessory proximal anteromedial portal and a poly-dioxanone (PDS) suture is delivered through the capsule just anterior to the fragmented coronoid process. This step is usually then repeated a second time.
Fig. 3.
Arthroscopic view through an anterolateral portal obtained using a 30° scope. Right elbow. Diagnostic evaluation of the coronoid fracture is performed.
The sutures are then retrieved through the anteromedial portal and a high-resistance, non-resorbable suture is shuttled into the joint to replace the PDS suture. With the C-arm positioned behind the surgeon, a limited posterior skin incision is performed. Carefully checking the position of the Kirschner wire, posterior-to-anterior drilling is performed.
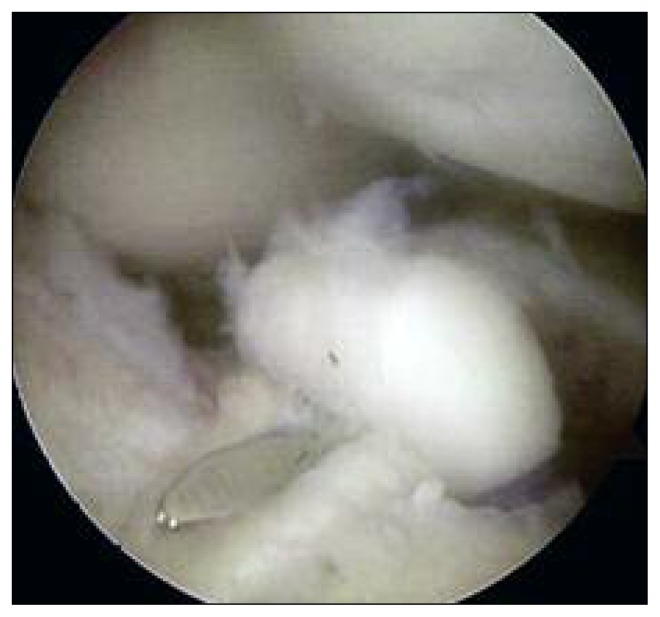
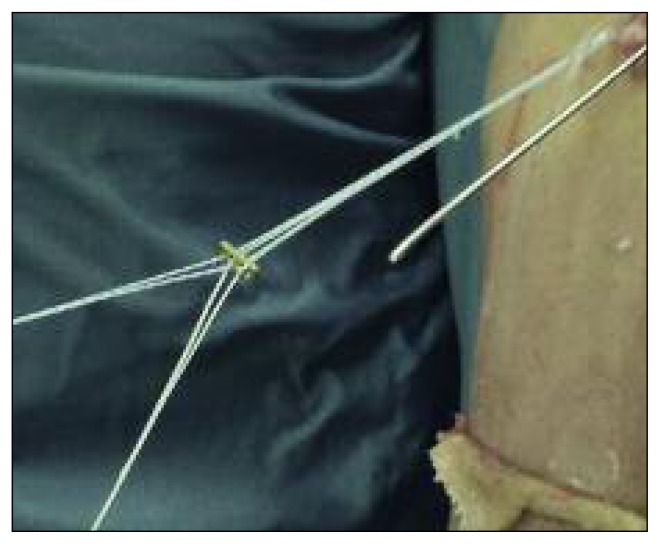
Care is taken to progress very slowly and to check with the C-arm the advancement of the Kirschner wire to prevent it from advancing too far anteriorly. Once the Kirschner wire emerges from the anterior aspect of the unfractured coronoid process, a cannulated drill (4 mm diameter) is advanced over the Kirschner wire (Fig. 4). Once all the sutures have been retrieved posteriorly, an arthroscopic button (Endobutton, Smith&Nephew, London, UK) or is used to complete the knot tying (Fig. 5).
Fig. 4.
Arthroscopic view through an anterolateral portal obtained using a 30° scope. Right elbow. The Kirschner wire emerges from the anterior aspect of the unfractured coronoid process.
Fig. 5.
External view. Once all the sutures have been retrieved posteriorly an Endobutton is used to complete the knot tying.
Postoperative care
After surgery, the elbow is immobilized in a brace with the forearm in neutral rotation and the elbow at 30° of extension. A 30° to 60° range of motion (ROM) is allowed after the first 21 days. In the next few weeks, motion is slowly increased until the functional arc of motion is recovered. At 8 weeks, the brace can be removed for activities of daily living. At approximately 12 weeks after surgery, the patient starts strengthening exercises.
Outcome measurements
The patients were reviewed at 6, 12 and 24 months after surgery. Each follow-up visit included functional outcome assessment, performed using the Disabilities of the Arm, Shoulder and Hand scale (DASH) (21) and the Mayo Elbow Performance Index (MEPI) (22); the follow-up evaluation also included physical examination (elbow ROM, stability), pain rating on a visual analog scale (VAS), and radiographic assessment of bony union with standard anteroposterior and lateral projections. Elbow ROM was assessed using a standard long-arm goniometer to measure flexion, extension, pronation and supination. Measurements were performed as reported by Armstrong et al. (23). Stability was graded according to the MEPI as 1 (stable), 2 (moderate instability), or 3 (gross instability). The patients were also assessed for complications, defined as re-fracture of the coronoid process, dehiscence of the surgical scar, infections or fixation device intolerance.
Results
All 4 patients were available for all follow-up visits. Their demographic data and functional results are summarized in Table 1.
Table 1.
Demographic data and functional results at 6, 12 and 24 months.
| Patients | Age at surgery | Sex | Side affected | Time (days) between rupture and treatment | DASH score (at 6-12-24 months) | MEPI score (at 6-12-24 months) | Flexion (at 6-12-24 months) | Extension (at 6-12-24 months) | Pronation (at 6-12-24 months) | Supination (at 6-12-24 months) | VAS (at 6-12-24 months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 33 | M | R | 7 | 21 - 9 - 5 | 80 -90 -97 | 108° - 123° - 142° | 2° - 4°-5° | 75° - 83° - 89° | 75° - 80° - 85° | 4- 2 - 1 |
| 2 | 37 | M | R | 14 | 16 - 12 - 7 | 75 – 83 - 92 | 124° - 133° - 159° | 5° - 6° -7° | 77° - 85° - 93° | 81° - 84° - 87° | 2 - 1 - 1 |
| 3 | 44 | F | L | 15 | 23 - 16 - 7 | 73 – 81 - 96 | 116° - 127°- 146° | 4° - 8° - 8° | 81° - 88° -94° | 82° - 87° - 93° | 4 - 2 - 0 |
| 4 | 34 | M | L | 12 | 28 - 19 - 9 | 68 - 74 - 91 | 100° - 117°- 129° | 1° - 2° - 4° | 71° -80° - 88° | 74° - 77° - 79° | 6 - 3- 2 |
| Mean | 37 | 3M | 2 R | 12 | 22 - 14 - 7 | 74 – 82 - 94 | 112° - 125 °- 144° | 3° - 5°- 6° | 76° - 84°- 91° | 78° - 82° - 86° | 4 -2-1 |
| 1F | 2L |
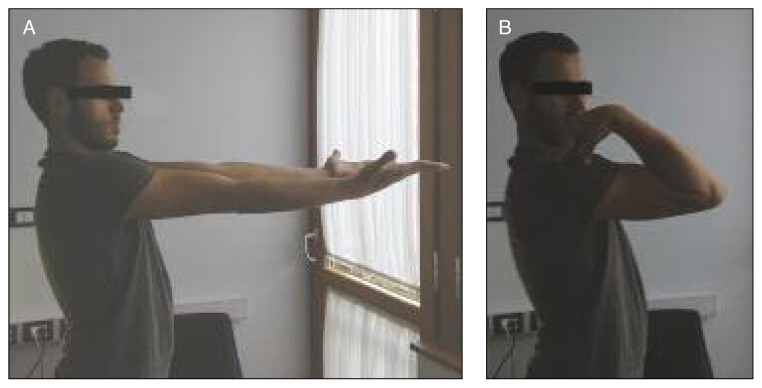
At 6, 12 and 24 months, respectively, they recorded mean DASH scores of 22.0±6, 14±5, and 7±2 and mean MEPI scores of 74±6, 82±8, and 94±3: these results corresponding to an excellent functional outcome. They recorded VAS scores was 4±2, 2±1 and 1±1 at 6, 12 and 24 months respectively. As regards the mean ROM of the affected elbow, they recorded the following values at 6, 12 and 24 months respectively: 112°±12°, 125°±8° and 144°±15° of flexion; 3°±2°, 5°±3° and 6°±2° of extension; 76°±5°, 84°±4° and 91°±3° of pronation; and 78°± 4°, 82°±5° and 86°±7° of supination. There were no elbows with evidence of clinical instability to varus or valgus stress (Fig. 6). No complications were observed. All the patients returned to their daily activities and occupations.
Fig. 6.
Follow-up at 12 months, verifying ROM in flexion and extension. The images show that the patient has recovered full functionality in extension (A) and in flexion (B).
Discussion
In this paper, we have described an all-arthroscopic coronoid tunnelling and capsular plication technique, together with the clinical and functional outcomes of a retrospective case series in which it was used, reporting DASH scores, MEPI scores, elbow ROM, VAS, stability and rate of complications. The technique proposed can restore elbow function, ROM and stability and allows an anatomical reconstruction of the joint after type I or type II CPFs.
The literature reports several surgical techniques for the treatment of CPFs (24–28). The benefits of an arthroscopic procedure include smaller incisions with less soft tissue dissection, better visualization of the joint, direct evaluation of the fracture pattern and easier anatomical reconstruction.
Minimally invasive techniques allow reconstructions that preserve skin integrity, reducing the risk of scar infection or dehiscence (26, 28).
Adams et al. were the first to describe an arthroscopically assisted technique for CPF fixation (29). They treated 6 patients with type II and type III CPFs classified according to the Regan-Morrey classification. Once the fractures had been reduced arthroscopically, a guide wire was inserted into the fragment and fixation was performed with a cannulated screw. One patient required plate fixation with a limited anterior incision. At a mean follow-up time of 31.8 months, 5 patients had an excellent MEPI score. The Authors of this preliminary report suggested that selected CPFs may be treated arthroscopically with satisfactory outcomes.
Hausman et al. (30) evaluated, at a minimum follow-up of one year, 4 patients with small CPFs with instability of the ulnohumeral joint treated with arthroscopically assisted reduction and fixation. All the patients achieved a functional ROM with an average flexion/extension arc of 2.5° to 140° and full pronation and supination. No patient had recurrent elbow instability. The Authors concluded that arthroscopically assisted management of CPFs can offer excellent joint visualization, enabling anatomical repair without extensive soft tissue dissection.
Recently, Lee et al. (31) reported the clinical characteristics, results and outcomes of 10 cases of Regan-Morrey type I, type II or type III coronoid fractures treated using a novel arthroscopic technique; more than one year after surgery the patients had a mean MEPI score of 98.5. The Authors highlighted that adequate reduction of coronoid fractures using percutaneous Kirschner wires or Ethibond can be achieved arthroscopically. The approach resulted in good clinical and radiological union and excellent functional outcome in the majority of cases.
The retrospective design, the lack of a control group and the small number of patients treated are the limitations of the present study, and its data alone are not sufficient to prove the superiority of this surgical approach to the management of CPFs. However, the results obtained suggest that the technique described, if performed by an experienced arthroscopist, could be a valid alternative to open reduction and internal fixation.
In conclusion, the new all-arthroscopic coronoid tunnelling and capsular plication technique proposed in this study can restore elbow function, ROM and stability and allows anatomical reconstruction of the joint after type I or II CPFs. If performed by an experienced arthroscopist, it is a valid alternative to open reduction and external fixation.
References
- 1.Morrey BF, An KN. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14( 1 Suppl S):174S–178S. doi: 10.1016/j.jse.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 2.Wells J, Ablove RH. Coronoid fractures of the elbow. Clin Med Res. 2008;6:40–44. doi: 10.3121/cmr.2008.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the coronoid and radial head. J Bone Joint Surg Am. 2002;84-A:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Doornberg J, Ring D, Jupiter J. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin Orthop. 2004;429:292–300. doi: 10.1097/01.blo.0000142627.28396.cb. [DOI] [PubMed] [Google Scholar]
- 5.Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86-A:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Xiao K, Zhang J, Li T, et al. Anatomy, definition, and treatment of the “terrible triad of the elbow” and contemplation of the rationality of this designation. Orthop Surg. 2015;7:13–18. doi: 10.1111/os.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeon IH, Sanchez-Sotelo J, Zhao K, et al. The contribution of the coronoid and radial head to the stability of the elbow. J Bone Joint Surg Br. 2012;94:86–92. doi: 10.1302/0301-620X.94B1.26530. [DOI] [PubMed] [Google Scholar]
- 8.Wang YH, Meng QB, Wu JD, et al. Treatment of fractures of the ulnar coronoid process. Orthop Surg. 2009;1:269–274. doi: 10.1111/j.1757-7861.2009.00042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinmann SP. Coronoid process fracture. J Am Acad Orthop Surg. 2008;16:519–529. [PubMed] [Google Scholar]
- 10.Closkey RF, Goode JR, Kirschenbaum D, et al. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82-A:1749–1753. doi: 10.2106/00004623-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Hull JR, Owen JR, Fern SE, et al. Role of the coronoid process in varus osteoarticular stability of the elbow. J Shoulder Elbow Surg. 2005;14:441–446. doi: 10.1016/j.jse.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotator stabilizers of the elbow. J Bone Joint Surg Am. 2004;86-A:975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Deutch SR, Jensen SL, Tyrdal S, et al. Elbow joint stability following experimental osteoligamentous injury and reconstruction. J Shoulder Elbow Surg. 2003;12:466–471. doi: 10.1016/s1058-2746(03)00062-4. [DOI] [PubMed] [Google Scholar]
- 14.Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315–319. doi: 10.1177/036354658301100506. [DOI] [PubMed] [Google Scholar]
- 15.Doornberg JN, van Duijn J, Ring D. Coronoid fracture height in terrible-triad injuries. J Hand Surg Am. 2006;31:794–797. doi: 10.1016/j.jhsa.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez-Sotelo J, O’Driscoll SW, Morrey BF. Anteromedial fracture of the coronoid process of the ulna. J Shoulder Elbow Surg. 2006;15:e5–8. doi: 10.1016/j.jse.2005.05.009. Erratum in: J Shoulder Elbow Surg 2007;16;127. [DOI] [PubMed] [Google Scholar]
- 17.Giannicola G, Sacchetti FM, Greco A, et al. Management of complex elbow instability. Musculoskelet Surg. 2010;94( Suppl 1):S25–36. doi: 10.1007/s12306-010-0065-8. [DOI] [PubMed] [Google Scholar]
- 18.Doornberg JN, Ring DC. Fracture of the anteromedial facet of the coronoid process. J Bone Joint Surg Am. 2006;88:2216–2224. doi: 10.2106/JBJS.E.01127. [DOI] [PubMed] [Google Scholar]
- 19.Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348–1354. [PubMed] [Google Scholar]
- 20.O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 21.Jester A, Harth A, Germann G. Measuring levels of upper-extremity disability in employed adults using the DASH Questionnaire. J Hand Surg Am. 2005;30:1074.e1–1074.e10. doi: 10.1016/j.jhsa.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF, editor. The elbow and its disorders. 2nd ed. WB Saunders; Philadelphia: 1993. pp. 86–89. [Google Scholar]
- 23.Armstrong AD, MacDermid JC, Chinchalkar S, et al. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7:573–580. doi: 10.1016/s1058-2746(98)90003-9. [DOI] [PubMed] [Google Scholar]
- 24.Kiene J, Wäldchen J, Paech A, et al. Midterm results of 58 fractures of the coronoid process of the ulna and their concomitant injuries. Open Orthop J. 2013;19:86–93. doi: 10.2174/1874325001307010086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rouleau DM, Sandman E, van Riet R, et al. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21:149–160. doi: 10.5435/JAAOS-21-03-149. [DOI] [PubMed] [Google Scholar]
- 26.Van Tongel A, MacDonald P, Van Riet R, et al. Elbow arthroscopy in acute injuries. Knee Surg Sports Traumatol Arthrosc. 2012;20:2542–2548. doi: 10.1007/s00167-012-1904-y. [DOI] [PubMed] [Google Scholar]
- 27.Manidakis N, Sperelakis I, Hackney R, et al. Fractures of the ulnar coronoid process. Injury. 2012;43:989–998. doi: 10.1016/j.injury.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 28.Atesok K, Doral MN, Whipple T, et al. Arthroscopy-assisted fracture fixation. Knee Surg Sports Traumatol Arthrosc. 2011;19:320–329. doi: 10.1007/s00167-010-1298-7. [DOI] [PubMed] [Google Scholar]
- 29.Adams JE, Merten SM, Steinmann SP. Arthroscopic-assisted treatment of coronoid fractures. Arthroscopy. 2007;23:1060–1065. doi: 10.1016/j.arthro.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 30.Hausman MR, Klug RA, Qureshi S, et al. Arthroscopically assisted coronoid fracture fixation: a preliminary report. Clin Orthop Relat Res. 2008;466:3147–3152. doi: 10.1007/s11999-008-0502-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee JM, Yi Y, Kim JW. Arthroscopically assisted surgery for coronoid fractures. Orthopedics. 2015;38:742–746. doi: 10.3928/01477447-20151119-04. [DOI] [PubMed] [Google Scholar]