Abstract
Purpose
Treating pain in primary care is challenging. Primary care providers (PCPs) receive limited training in pain care and express low confidence in their knowledge and ability to manage pain effectively. Models to improve pain outcomes have been developed, but not formally implemented in safety net practices where pain is particularly common. This study evaluated the impact of implementing the Stepped Care Model for Pain Management (SCM-PM) at a large, multisite Federally Qualified Health Center.
Methods
The Promoting Action on Research Implementation in Health Services framework guided the implementation of the SCM-PM. The multicomponent intervention included: education on pain care, new protocols for pain assessment and management, implementation of an opioid management dashboard, telehealth consultations, and enhanced onsite specialty resources. Participants included 25 PCPs and their patients with chronic pain (3,357 preintervention and 4,385 postintervention) cared for at Community Health Center, Inc. Data were collected from the electronic health record and supplemented by chart reviews. Surveys were administered to PCPs to assess knowledge, attitudes, and confidence.
Results
Providers’ pain knowledge scores increased to an average of 11% from baseline; self-rated confidence in ability to manage pain also increased. Use of opioid treatment agreements and urine drug screens increased significantly by 27.3% and 22.6%, respectively. Significant improvements were also noted in documentation of pain, pain treatment, and pain follow-up. Referrals to behavioral health providers for patients with pain increased by 5.96% (P=0.009). There was no significant change in opioid prescribing.
Conclusion
Implementation of the SCM-PM resulted in clinically significant improvements in several quality of pain care outcomes. These findings, if sustained, may translate into improved patient outcomes.
Keywords: quality improvement, primary care, chronic pain, community health, FQHC
Video abstract
Background
There are over 100 million people in the US with chronic pain, costing an estimated $635 billion each year for medical treatment and lost productivity.1 The majority of these patients seek help for their pain from a primary care provider (PCP),2 accounting for up to a third of all visits to primary care.3,4 However, the quality of pain care in primary care remains poor.5–7 PCPs receive little education about pain management during medical training5–8 and lack confidence in their ability to manage chronic pain effectively.3,9–11 Guidelines for the appropriate management of pain have had a limited impact as evidenced by low rates of adherence to recommendations for documentation12 and management of pain.13–15 Studies reveal wide variation in the levels of prescribing of opioid analgesics among PCPs,16,17 but overall, there has been a marked increase in their use and misuse over the past 10 years.18 Evidence now suggests that opioid analgesics are associated with a significant, dose-dependent risk of serious harm, with limited evidence for their long-term benefits.19–21
A comprehensive effort to change the health professionals’ performance in pain care that goes beyond the educational curricula and focuses on changing culture and systems of care is needed.22 The American Academy of Pain Medicine advocates the use of the Stepped Care Model for Pain Management (SCM-PM), with primary care-based screening and routine management of most cases of pain, and the addition of further resources for more complex cases in a stepwise fashion. In 2009, the Veterans Health Administration (VHA) called for implementation of the SCM-PM across the VHA system.23 Since then, the model has been implemented in several VHA centers and shown to improve patient outcomes for pain.24–27 A large VHA practice in Connecticut implemented the SCM-PM (known as Project STEP) and described the implementation. Preliminary results suggest system-wide benefits.25,28
The objective of this study was to evaluate the impact of implementing the SCM-PM on the quality of pain care in a large, state-wide multisite Federally Qualified Health Center (FQHC).
Methods
Setting
Community Health Center, Inc. (CHCI) is a state-wide FQHC providing comprehensive, primary care in 12 primary care health centers across Connecticut. CHCI cares for over 140,000 patients, 68% of whom are racial/ethnic minorities; over 90% are below 200% federal poverty level, 70% have health insurance provided by Medicaid, and 22% are uninsured. Specialist care, including pain-related specialties, is available through outside consultation, but many patients face substantial barriers to securing such care. The study sample for this project included all PCPs at CHCI who cared for adult patients (internists, family practitioners, family nurse practitioners, and physician assistants) and were present for the 3-year duration of the intervention, and all adult patients with at least one medical visit in the previous year who were under the care of the providers in the study. Patients with chronic pain were identified by a validated algorithm using commonly available electronic health record (EHR) data elements (diagnosis codes, pain scores, and medication prescribing information).28
Procedures
Project “STEP-ing Out” was a 3-year project implementing and evaluating the SCM-PM at CHCI. The intervention took place between March 2011 and February 2014. This study was reviewed and approved by the Institutional Review Board (IRB) of CHCI. A waiver of informed consent was granted by the IRB due to the large scale, retrospective data that was being evaluated. Results of a comprehensive baseline assessment of pain management practices and outcomes throughout the organization have been described elsewhere.3 Results of this assessment, covering a 1-year period from April 2010 through March 2011, revealed that chronic pain was highly prevalent among CHCI’s patients. Providers had low confidence in their knowledge of pain, limited adherence to opioid practice guidelines, wide variation in the levels of prescribing of opioid medications, and poor-quality documentation of pain care. Despite the high rate of coexistent behavioral health and addiction disorders, the rate of referral to onsite behavioral health providers was low.
Intervention
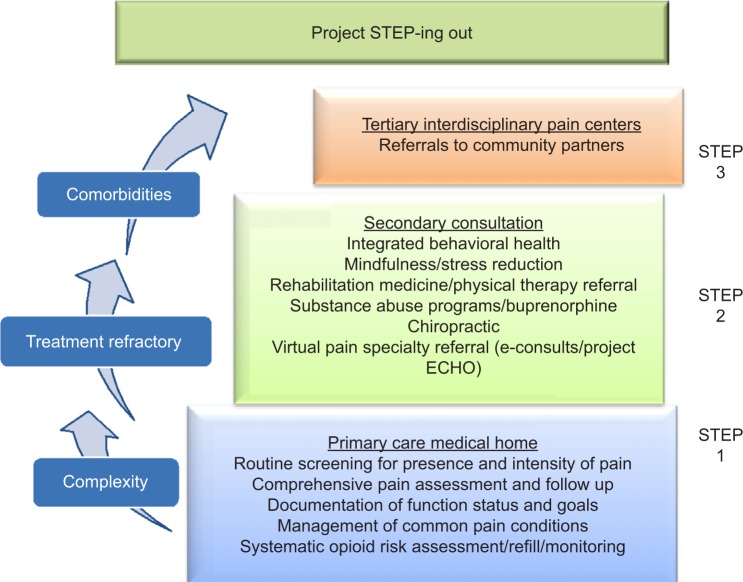
The SCM-PM calls for an individualized approach to managing pain in three steps.29 Step 1 emphasizes the role of the primary care clinician in identifying and discussing the patient’s pain concerns and developing a treatment plan focusing on self-management and primary care-based interventions. Step 2 involves additional resources and collaborative treatment, including behavioral health assessment and intervention, medication, and consultations with specialists from appropriate disciplines. Step 3 focuses on patients with chronic pain requiring significantly more care and involvement from other members of a pain management team. Minor modifications were made to the SCM-PM (Figure 1) to account for the limited access to specialty consultation in the safety net setting by providing more care on site and through videoconferencing. Specifically, greater emphasis was placed on the use of onsite and telehealth resources to account for the limited access to outside specialty care that characterizes the safety net setting. The Promoting Action on Research Implementation in Health Services (PARIHS) framework30,31 was used to guide the process of implementing the SCM-PM. This framework defines the critical elements – context, evidence, and facilitation – for the successful implementation of evidence-based practices.31–36 Details on how the PARIHS framework was employed for this project have been previously published.3 Context was assessed through organizational surveys, staff interviews, and queries of the EHR. Evidence included guidelines and findings from the medical literature, knowledge assessments completed by primary care providers, and patient chart reviews. A detailed facilitation plan that included quality improvement strategies, data dashboards, and engagement of front line staff across the organization was employed to support project implementation.
Figure 1.
Modified Stepped Care Model for Pain Management at CHCI.
Abbreviations: CHCI, Community Health Center, Inc.; ECHO, Extension for Community Health Outcomes.
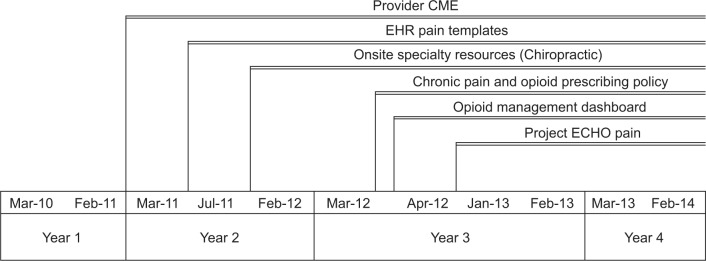
The project’s interventions consisted of six educational and practice support components. The intervention components were introduced between 2011 and 2012 (see Figure 2 for timeline).
Provider continuing medical education (CME): An agency-wide grand rounds-style presentation was delivered in person and through videoconference and was followed by subsequent biannual pain CME presentations. These presentations included discussions of pain care best practices and review of online CME modules about pain management and opioid prescribing.
EHR pain templates: EHR templates for the initial and follow-up visits related to chronic pain were created to help improve documentation of pain assessment and treatment.
Chronic pain and opioid prescribing policy: CHCI established a new chronic pain and opioid prescribing policy requiring a signed opioid treatment agreement (OTA), a urine drug test (UDT) at least once in every 6 months, and a functional assessment using the Pain Interference Assessment Tool Patient Reported Outcome Measurement Information System (PROMIS) Pain Interference Short Form 8a (SF8a)37 every 3 months for all patients receiving chronic opioid therapy (COT). COT was defined as receipt of 90 days or more of an opioid analgesic in 1 year.
Opioid management dashboard: A new dashboard with key metrics for managing patients receiving COT was introduced that included the number and percentage of adult patients receiving COT in each PCP’s panel, as well as the number of patients with: 1) a signed OTA, 2) an UDT screen within the past 6 months, 3) a completed pain interference assessment questionnaire within the past 3 months, and 4) at least one behavioral health visit in the past year. Providers could also access a list of their individual COT patients and determine which patients were due for any of these items.
Onsite specialty resources: Additional onsite resources, including chiropractic care, pain-focused behavioral health interventions, and buprenorphine treatment, were added to provide options for collaborative, multimodal care for more complex patients who failed to improve with routine primary care management. As part of the educational intervention, medical teams were educated regarding multimodal care, the role of chiropractic care, and the importance of behavioral health evaluation and treatment for chronic pain.
Project Extension for Community Health Outcomes (ECHO) pain: To provide virtual access to pain specialists, Project ECHO for pain care38 was introduced at CHCI, providing weekly videoconferences for selected PCPs during which they could present complex pain cases to an expert multidisciplinary team of pain specialists. One provider from each CHCI practice site joined the weekly sessions to serve as the onsite pain “champion”.
Figure 2.
Timeline for Project STEP-ing Out.
Abbreviations: CME, continuing medical education; ECHO, Extension for Community Health Outcomes; EHR, electronic health record.
Measures
To broaden the scope of the evaluation, Moore et al’s expanded outcomes framework was used to assess learners and evaluate instructional activities.39 Based on this framework, the evaluation included conventional educational outcomes such as knowledge, attitudes, and beliefs, but additionally included outcomes such as clinician’s adherence to guidelines, patient-reported pain scores, and opioid prescribing information.
The KnowPain-50 (KP50) survey40 was used to assess provider’s knowledge regarding pain management. The KP50 contains multiple choice questions as well as questions scored on a six-point Likert scale with an overall maximum possible score of 250. In addition, to assess PCPs’ self-efficacy and attitudes about pain care, a set of eleven questions taken from a VHA-developed survey was used.41 All CHCI PCPs included in the study were invited to complete the KP50 and pain attitudes surveys. The survey administration was conducted anonymously at baseline and following the conclusion of the intervention in March 2013, in order to increase the response rates and to overcome the reluctance of PCPs to have their knowledge formally assessed.
To assess changes in pain care quality, structured data from CHCI’s EHR were pulled for patients with chronic pain seen during the 1-year period prior to the intervention (from March 2010 to February 2011) and compared to data for patients with pain seen during the year after the intervention, between March 2013 and February 2014. These data were supplemented by a random sample of chart reviews. Patients with chronic pain were identified using a validated algorithm28 that used data from the EHR, including pain scores, medication prescribing, and billing codes. For the final analysis, only charts for patients belonging to providers who were employed at CHCI for the duration of the intervention were included. All patients with chronic pain were included in the electronic data analysis. Data points included patient demographics, medications prescribed, pain scores, use of OTA, UDT, functional assessments, and referrals to behavioral health, chiropractic, and other outside specialists.
Supplemental chart reviews were conducted to assess providers’ documentation of pain care using the Pain Care Quality extraction tool.25 The tool contains 12 indicators grouped into three domains: pain assessment, pain treatment, and pain reassessment. The tool utilizes a dichotomous scoring system to indicate whether each indicator was present or absent in each progress note.42 Three hundred charts were randomly selected for the baseline and postintervention reviews.
Statistical analysis
Descriptive statistics were used to analyze the data with use of multiple-group models in Mplus43 that accounts for the clustering within provider (using the “complex” type option) and “xtmixed” analyses for the clustered data in Stata data analysis and statistical software version 14 (StataCorp Stata Statistical Software, College Station, TX, USA). All tests were two-sided and considered significant at P<0.05.
Results
Table 1 shows a cross-sectional analysis of the demographic characteristics of participating providers’ patients with chronic pain at baseline and postintervention. Characteristics of patients did not change significantly over the duration of the project, although there was an increase in the total number of patients with pain, consistent with overall growth in patient volume across CHCI during this timeframe. Patients with chronic pain were more likely to be female. Nearly half were nonwhite, and over 65% had state-funded Medicaid insurance. Table 2 shows the characteristics of the 25 PCPs who participated in all 3 years of the intervention.
Table 1.
Demographic information of participating providers’ patients with chronic pain
| Baseline (March 2010–February 2011) N (%) | Postintervention (March 2013–February 2014) N (%) | ||
|---|---|---|---|
| Total patients | 3,357 | 4,385 | |
| Female | 2,109 (63) | 2,789 (64) | |
| Age (years) | 18–29 | 339 (10) | 370 (8) |
| 30–39 | 571 (17) | 746 (17) | |
| 40–49 | 1,019 (31) | 1,105 (25) | |
| 50–59 | 878 (26) | 1,351 (31) | |
| 60–69 | 372 (11) | 576 (13) | |
| 70+ | 151 (5) | 237 (5) | |
| Race/ethnicity | White | 1,399 (42) | 1,822 (42) |
| Black | 451 (14) | 577 (13) | |
| Hispanic | 1,398 (42) | 1,819 (42) | |
| Other | 66 (2) | 124 (3) | |
| Insurance | Medicaid | 2,210 (66) | 2,796 (64) |
| Medicare | 635 (19) | 845 (19) | |
| Private insurance | 241 (7) | 446 (10) | |
| Uninsured | 241 (7) | 286 (7) |
Table 2.
Primary care provider (N=25) characteristics
| Characteristic | n (%) | |
|---|---|---|
| Sex | Male | 11 (44) |
| Female | 14 (56) | |
| Race | White | 19 (76) |
| Black | 2 (8) | |
| Other | 4 (16) | |
| Professional degree | MD/DO | 17 (68) |
| APRN | 8 (32) |
Abbreviations: APRN, Advanced Practice Nurse Practitioner; MD/DO, Medical Doctor/Doctor of Osteopathic Medicine.
PCPs’ knowledge and attitudes about pain care
The anonymous surveys of CHCI providers revealed an average score of 152.5 on the KP50 in the baseline assessment period, which increased to 169.5 (P=0.001) in March 2013 following the intervention. Self-efficacy was higher among providers completing the attitudes and beliefs survey following the intervention, compared to those completing it during the baseline period. The average rate of agreement with the statement “I am confident in my ability to manage chronic pain” was 2.71 at baseline and 4.67 in March 2013 (on 1–6 scale, where 1 is strongly disagree and 6 is strongly agree).
Pain care quality
The quality of pain care improved in several areas following the intervention. During the baseline period, only 360 (34%) of the 1,309 patients receiving COT had a documented OTA in the chart and 680 (64%) had a UDT in the preceding year. After implementation, 778 (61%) out of 1,230 patients receiving COT had an OTA and 1,103 (87%) had a UDT in the past year (both differences significant at P<0.05). The quality of documentation also improved following the intervention. Table 3 shows the results of the review of a randomly selected sample of 14 providers’ patients’ charts. While not all providers routinely used the new EHR templates, documentation improved in several areas. Documentation of the presence of pain and the source and/or cause of pain increased significantly from 64% to 82% (P=0.001) and from 62% to 74% (P=0.025), respectively. There were also significant improvements in documentation of functional status from 5% to 19% (P=0.001), in a documented treatment plan from 92% to 98% (P=0.002), and in documentation of pain reassessment from 17% to 39% (P=0.001).
Table 3.
Pain care documentation data elements
| Chronic Pain Care Documentation Element | Baseline (March 2010–February 2011) N=108 (%) | Evaluation (March 2013–February 2014) N=213 (%) | P-values |
|---|---|---|---|
| Documentation of pain | 69 (64) | 174 (81) | <0.001 |
| Source or cause of pain | 67 (62) | 158 (74) | 0.025 |
| Functional assessment | 5 (5) | 42 (19) | <0.001 |
| Review of diagnostic tests | 6 (6) | 37 (17) | <0.003 |
| Treatment plan | 99 (92) | 209 (98) | 0.006 |
| Pain medication ordered | 102 (94) | 182 (85) | 0.017 |
| Pain consult ordered | 7 (7) | 60 (28.2) | <0.001 |
| Patient education | 16 (15) | 47 (22) | 0.121 |
| Diagnostic imaging ordered | 25 (23) | 59 (28) | 0.379 |
| Assessment of treatment effectiveness | 18 (17) | 83 (39) | <0.001 |
Table 4 shows the cross-sectional data for all patients with chronic pain in the years pre- and postintervention, who were cared for by the 25 providers in the intervention. Results demonstrate statistically significant increases in the percentage of patients with pain who had a visit with an onsite behavioral health provider. Referrals to chiropractors also increased significantly for both groups, while there was a significant decline in referrals to neurosurgery or orthopedic surgery and to pain specialists. There was no significant decline in opioid prescribing.
Table 4.
Pain care treatment data from the EHR for patients with chronic pain cared for by the 25 providers present for intervention
| Chronic Pain Care Data Element | Baseline (March 2010–February 2011) |
Postintervention (March 2013–February 2015) |
P-values | |
|---|---|---|---|---|
| Total patients | 3,330 | 4,385 | N/A | |
| Average number of visits (±SD) | 7.30±14.37 | 6.83±14.37 | 0.094 | |
| Pain scores | Pain >8, n (%) | 2,504 (75.2) | 3,245 (74.0) | 0.351* |
| Opioids | Any opioid prescribed, n (%) | 1,615 (48.5) | 1,943 (44.3) | 0.117 |
| Chronic opioid therapy, n (%) | 763 (22.9) | 921 (21.0) | 0.486 | |
| Behavioral health | Patients with a behavioral visit, n (%) | 809 (24.3) | 1,276 (29.1) | 0.009 |
| Pain referrals | Chiropractic, n (%) | 3 (0.1) | 48 (1.1) | 0.008 |
| Physical therapy, n (%) | 480 (14.4) | 750 (17.1) | 0.508 | |
| Neurologic or orthopedic surgery, n (%) | 663 (19.9) | 693 (15.8) | <0.001 | |
| Rheumatology, n (%) | 120 (3.6) | 136 (3.1) | 0.419 | |
Notes:
Stata’s “xtmixed” yielded P=0.052.
Abbreviations: EHR, electronic health record; N/A, not applicable; SD, standard deviation.
Discussion
This study demonstrated improvement in knowledge, self-efficacy, adherence to guidelines, and documentation of care for patients with chronic pain, associated with implementing the SCM-PM across a large, state-wide safety net health system. The intervention was also associated with changes in monitoring and follow-up of patients receiving COT for pain, and with an overall increase in referrals to behavioral health providers and a decrease in referrals to surgical sub-specialties and pain management. These changes were all in the direction predicted by the project model and suggested that the combined elements of the intervention were having the desired effect and leading to changes in how providers treated patients with pain.
While many of the changes observed in the study were modest, they were significant both from a statistical and an organizational perspective, reflecting positive changes across a large organization with 12 practice sites and over 130,000 medically underserved patients. Given the challenge of standardizing care and implementing a complex intervention in a large, under-resourced environment, the achievement of measurable changes in these process measures on such a large scale is important. Based on these findings, CHCI has fully implemented and committed to sustaining the initiative and augmenting the model as needed to achieve more robust improvements in pain care across all of its practice locations.
The goal of this intervention was to change providers’ behaviors and improve the process of care for patients with pain. These results suggest that it did so. Implicit in this goal, however, is the assumption that such process changes will have an impact, further downstream, on patient outcomes. Such patient outcomes are harder to measure and will likely take time to realize. Further studies are needed to evaluate changes in patient outcomes and to fully assess the impact and value of this intervention.
One of the most significant challenges to implementing the SCM-PM was providing access to specialty expertise and guidance for more complex patients who failed to improve with primary care-based treatment and management. Limited access to pain care, particularly for racial and ethnic minorities and patients with lower socioeconomic status, has been well documented.44,45 Project ECHO, a novel strategy to provide education and consultation from pain specialists, helped overcome this obstacle.46 Further research is underway to evaluate the specific impact of Project ECHO, but experience suggests that it augmented the ability to effectively manage complex patients with pain in primary care.
The baseline assessment identified that staff had significant concerns about time and resources available to successfully make changes in pain management practices.3 To address this, dedicated time was provided for educational activities and team-based strategies were developed to help share the work of pain management among different members of the clinical team. The addition of onsite chiropractors and the strengthening of behavioral health integration through colocation and open scheduling provided added resources that clinicians could offer to their patients, in addition to, or in place of opioid analgesics. Selected providers were given the opportunity to join Project ECHO and become local, onsite pain experts. Findings suggest that this strategy was successful, with referrals to onsite behavioral health providers and chiropractors increasing.
One strength of this study was the use of a validated identification algorithm to identify patients with chronic pain. This allowed for an analysis of the impact of the intervention on a broad population of patients with chronic pain without relying solely on specific diagnoses such as back pain. The diversity of locations and the large scale of implementation in a state-wide, multisite delivery system also was an asset. In addition, the integrated EHR and data warehouse allowed collection of detailed medical and behavioral health data along with medications, laboratory results, and referrals. Use of the PARIHS framework also provided a strong implementation framework to guide the process.
This project had several limitations. First, the evaluation focused on process measures and did not include measures of patient outcomes other than pain scores. Subsequent work should include more robust patient assessments to help determine if such process changes ultimately impact patients. Studies of the SCM-PM in the VHA have employed cluster randomized designs and applied complex analytics to account for lack of randomization.24,25 However, conducting such a study in a large, multisite FQHC presented challenges that precluded such approaches. The interventions employed in this study, such as templates and dashboards, were implemented agency-wide and could not be limited to selected practices. As such, randomization was not possible, limiting the ability to eliminate unmeasured confounders. Also, the use of multiple components in the intervention prevents drawing any inference on the relative impact of each individual element. Provider turnover, which ranged from 11% to 20% over the project, also limited the number of providers included in the analysis. Lastly, the interventions were introduced in phases over the 3-year project, limiting the ability to evaluate the impact of any one element of the intervention.
There is a compelling need to improve the management of pain in primary care, especially in medically underserved settings. Pain management must become a core competency of primary care, with the providers being well educated and trained in the proper assessment, management, and follow-up of pain. In light of the growing epidemic of prescription opioid abuse and diversion, PCPs need training and support to apply appropriate risk mitigation strategies and take a more judicious approach to the prescribing of opioids for management of COT based on the principles of universal precautions.47
This initiative focused heavily on provider education and protocol-driven care and demonstrated modest but significant improvements in knowledge, self-efficacy, and adherence to guidelines. In addition, positive changes in referral patterns and opioid prescribing suggest that structured improvement initiatives based on data and effective conceptual models can lead not only to increased knowledge acquisition, but also application of that knowledge in ways that have direct impact on patient care. These changes are likely to result in reduced pain, improved patient safety, and more confident, knowledgeable, satisfied health care teams.
Acknowledgments
Presented at the North American Primary Care Research Group (NAPCRG) Annual Meeting, October 24–28, 2015, Cancun, Mexico and the Academy Health Seventh Annual Conference on the Science of Dissemination and Implementation, December 8–9, 2014, Bethesda, MD. The Mayday Fund and the Wallace Foundation supported the study.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Committee on advancing pain research, institute of medicine . Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academy Press; 2011. [Google Scholar]
- 2.Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- 3.Anderson D, Wang S, Zlateva I. Comprehensive assessment of chronic pain management in primary care: a first phase of a quality improvement initiative at a multisite community health center. Qual Prim Care. 2013;20(6):421–433. [PubMed] [Google Scholar]
- 4.Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21(6):652–655. doi: 10.1111/j.1525-1497.2006.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turk D, Brody M, Okifuji E. Physicians’ attitudes and practices regarding the long-term prescribing of opioids for non-cancer pain. Pain. 1994;59(2):201–208. doi: 10.1016/0304-3959(94)90072-8. [DOI] [PubMed] [Google Scholar]
- 6.Green C, Wheeler J, Marchant B, LaPorte F, Guerrero E. Analysis of the physician variable in pain management. Pain Med. 2001;2(4):317–327. doi: 10.1046/j.1526-4637.2001.01045.x. [DOI] [PubMed] [Google Scholar]
- 7.Starrels JL, Becker WC, Alford DP, Kapoor A, Williams AR, Turner BJ. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712–720. doi: 10.7326/0003-4819-152-11-201006010-00004. [DOI] [PubMed] [Google Scholar]
- 8.Mezei L, Murinson BB, Johns Hopkins Pain Curriculum Development Team Pain education in North American medical schools. J Pain. 2011;12(12):1199–1208. doi: 10.1016/j.jpain.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Ponte CD, Johnson-Tribino J. Attitudes and knowledge about pain: an assessment of West Virginia family physicians. Fam Med. 2005;37(7):477–480. [PubMed] [Google Scholar]
- 10.Barry DT, Irwin KS, Jones ES, et al. Opioids, chronic pain, and addiction in primary care. J Pain. 2010;11(12):1442–1450. doi: 10.1016/j.jpain.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Starrels JL, Fox AD, Kunins HV, Cunningham CO. They don’t know what they don’t know: Internal medicine residents’ knowledge and confidence in urine drug test interpretation for patients with chronic pain. J Gen Intern Med. 2012;27(11):1521–1527. doi: 10.1007/s11606-012-2165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zubkoff L, Lorenz KA, Lanto AB, et al. Does screening for pain correspond to high quality care for veterans? J Gen Intern Med. 2010;25(9):900–905. doi: 10.1007/s11606-010-1301-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhamb B, Brown D, Hariharan J, Anderson J, Balousek S, Fleming M. Survey of select practice behaviors by primary care physicians on the use of opioids for chronic pain. Curr Med Res Opin. 2006;22(9):1859–1865. doi: 10.1185/030079906X132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chodosh J, Solomon D, Roth C, et al. The quality of medical care provided to vulnerable older patients with chronic pain. J Am Geriatr Soc. 2004;52(5):756–761. doi: 10.1111/j.1532-5415.2004.52214.x. [DOI] [PubMed] [Google Scholar]
- 15.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Potter M, Schafer S, Gonzalez-Mendez E, et al. Opioids for chronic nonmalignant pain: Attitudes and practices of primary care physicians in the UCSF/Stanford collaborative research network. J Fam Pract. 2001;50(2):145–151. [PubMed] [Google Scholar]
- 17.Hutchinson K, Moreland AME, de C Williams AC, Weinman J, Horne R. Exploring beliefs and practice of opioid prescribing for persistent non-cancer pain by general practitioners. Eur J Pain. 2007;11(1):93–98. doi: 10.1016/j.ejpain.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Atluri S, Sudarshan G, Manchikanti L. Assessment of the trends in medical use and misuse of opioid analgesics from 2004 to 2011. Pain Physician. 2014;17(2):E119–E128. [PubMed] [Google Scholar]
- 19.Chou R, Deyo R, Devine B, et al. The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Rockville, MD: Agency for Healthcare Research and Quality (US); 2014. [DOI] [PubMed] [Google Scholar]
- 20.Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155(5):325–328. doi: 10.1059/0003-4819-155-5-201109060-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, Fiellin DA. Systematic review: Opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 22.Fishman SM, Young HM, Lucas Arwood E, et al. Core competencies for pain management: results of an interprofessional consensus summit. Pain Med. 2013;14(7):971–981. doi: 10.1111/pme.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Department of Veterans Affairs Department of Defense VA/DoD Clinical Practice Guideline: Management of opioid therapy for chronic pain. [Accessed May 1, 2010]. Available from: http://www.va.gov/painmanagement/docs/cpg_opioi-dtherapy_fulltext.pdf.
- 24.Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242–1252. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- 25.Dorflinger L, Moore B, Goulet J, Becker W, Heapy AA, Sellinger JJ, Kerns RD. A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management. J Gen Intern Med. 2014;29(Suppl 4):870–876. doi: 10.1007/s11606-014-3019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenberger PH, Philip EJ, Lee A, Kerns RD. The VHA’s national pain management strategy: Implementing the stepped care model. Fed Pract. 2011;28(8):39. [Google Scholar]
- 27.Kroenke K, Bair MJ, Damush TM, Wu J, Hoke S, Sutherland J, Tu W. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. JAMA. 2009;301(20):2099–2110. doi: 10.1001/jama.2009.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tian TY, Zlateva I, Anderson DR. Using electronic health records data to identify patients with chronic pain in a primary care setting. J Am Med Inform Assoc. 2013;20(e2):e275–e280. doi: 10.1136/amiajnl-2013-001856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.von Korff M, Moore JC. Stepped care for back pain: Activating approaches for primary care. Ann Intern Med. 2001;134(9 Pt 2):911–917. doi: 10.7326/0003-4819-134-9_part_2-200105011-00016. [DOI] [PubMed] [Google Scholar]
- 30.Ullrich PM, Sahay A, Stetler CB. Use of implementation theory: a focus on PARIHS. Worldviews Evid-Based Nurs. 2014;11(1):26–34. doi: 10.1111/wvn.12016. [DOI] [PubMed] [Google Scholar]
- 31.Rycroft-Malone J. The PARIHS framework—a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual. 2004;19(4):297–304. doi: 10.1097/00001786-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci. 2008;3:1. doi: 10.1186/1748-5908-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harvey G, Loftus-Hills A, Rycroft-Malone J, et al. Getting evidence into practice: The role and function of facilitation. J Adv Nurs. 2002;37(6):577–588. doi: 10.1046/j.1365-2648.2002.02126.x. [DOI] [PubMed] [Google Scholar]
- 34.McCormack B, Kitson A, Harvey G, Rycroft-Malone J, Titchen A, Seers K. Getting evidence into practice: the meaning of ‘context’. J Adv Nurs. 2002;38(1):94–104. doi: 10.1046/j.1365-2648.2002.02150.x. [DOI] [PubMed] [Google Scholar]
- 35.Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care. 1998;7(3):149–158. doi: 10.1136/qshc.7.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helfrich CD, Damschroder LJ, Hagedorn HJ, et al. A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implement Sci. 2010;5:82. doi: 10.1186/1748-5908-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katzman JG, Comerci G, Boyle JF, et al. Innovative telementoring for pain management: Project ECHO pain. J Contin Educ Health Prof. 2014;34(1):68–75. doi: 10.1002/chp.21210. [DOI] [PubMed] [Google Scholar]
- 39.Moore DE, Green JS, Gallis HA. Achieving desired results and improved outcomes: Integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1–15. doi: 10.1002/chp.20001. [DOI] [PubMed] [Google Scholar]
- 40.Harris Jr JM, Fulginiti JV, Gordon PR, Elliott TE, Davis BE, Chabal C, Kutob RM. KnowPain-50: a tool for assessing physician pain management education. Pain Med. 2008;9(5):542–554. doi: 10.1111/j.1526-4637.2007.00398.x. [DOI] [PubMed] [Google Scholar]
- 41.Dobscha S, Corson K, Flores J, Tansill E, Gerrity M. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9(5):564–571. doi: 10.1111/j.1526-4637.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 42.Moore BA, Anderson DR, Dorflinger L, et al. Stepped care model of pain management and quality of pain care in long-term opioid therapy. J Rehabil Res Dev. 2016;53(1):137–146. doi: 10.1682/JRRD.2014.10.0254. [DOI] [PubMed] [Google Scholar]
- 43.Muthén LK, Muthén BO. Mplus User’s Guide: Statistical Analysis with Latent Variables: User’s Guide. 6th ed. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- 44.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(Suppl 1):108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 45.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6(5):301–314. doi: 10.1016/j.jpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 46.Arora S, Geppert CM, Kalishman S, et al. Academic health center management of chronic diseases through knowledge networks: Project ECHO. Acad Med. 2007;82:154–160. doi: 10.1097/ACM.0b013e31802d8f68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chang YP, Compton P. Management of chronic pain with chronic opioid therapy in patients with substance use disorders. Addict Sci Clin Pract. 2013;8(1):21. doi: 10.1186/1940-0640-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]