Abstract
Although entertainment-education narratives are increasingly being used to communicate health information to a diversity of populations, there is limited evidence examining the use of narrative health education videos in low compared with adequate health literacy populations. There are also very few studies directly comparing narrative materials to more traditional, non-narrative materials. Because individuals with low health literacy are less likely than those with adequate health literacy to benefit from health communication interventions, it is especially important to develop an evidence base supporting the use of narrative health education materials in low literacy populations. This study extends knowledge on the use of narrative health education materials in populations with low health literacy by conducting a randomized trial comparing the acceptability and efficacy (knowledge gain) of two fact-equivalent films, one in a narrative and one in a non-narrative format, on individuals with adequate and low health literacy. This study finds that while both films were well-accepted and produced knowledge gains, the narrative film was more effective in this regard. This effect occurred regardless of health literacy level, indicating that narrative health communication materials are appropriate for individuals with low health literacy and do not exacerbate existing health disparities. These findings add to a small but growing body of evidence testing narrative health education materials in individuals with low health literacy, and provide new evidence supporting narrative, entertainment-education style video as a health communication tool to help reduce health literacy-related health disparities.
Keywords: Cervical cancer, Entertainment-education, Health communication, Health disparities, Health literacy, HPV, Knowledge, Narrative
Introduction
Narrative health education materials (e.g. entertainment-education) are increasingly being used to communicate health information and prompt health behavior change. This has important implications for public health and patient care, as a growing body of evidence indicates that narrative health education materials are as effective, if not more effective, at producing knowledge gains and prompting behavior change than traditional non-narrative health education materials, which tend to rely on facts, figures and statistics.1,2,3,4,5,6 However, there is limited work that specifically tests narrative materials in populations with low levels of health literacy. Individuals with low health literacy not only experience worse health outcomes, but also are less likely to benefit from health communication interventions.7,8,9 Thus, as the use of narratives to convey health information increases, it is crucial to carefully evaluate their use among individuals with low health literacy. To address this need, this paper compares the acceptability and efficacy of two fact-equivalent cervical cancer education films – one narrative and one non-narrative – by health literacy level.
Background
Two bodies of literature inform this study. First is research demonstrating the effectiveness health education materials formatted as narratives.1,3,6,10,11,12 For the purposes of this study, we define narrative health education materials as materials that present health information embedded within “a representation of connected events and characters that has an identifiable structure, is bounded in space and time, and contains implicit or explicit messages about the topic being addressed.”1, p. 222 This definition, as used in the current study, aligns more closely with “entertainment-education” style health education materials, rather than with materials that feature personal anecdotes, stories or testimonials in the context of a health issue. “Entertainment education is a theory-based communication strategy for purposefully embedding educational and social issues in the creation, production, processing, and dissemination process of an entertainment program, in order to achieve desired individual, community, institutional, and societal changes among the intended media user populations.”13, p. 272-73 In other words, we are specifically interested in health education materials that present an overarching story into which health information is embedded.
Numerous general population studies have shown that narratives can produce knowledge gains, attitude change and behavior change.4,6,14,15,16 These effects occur primarily through three mechanisms. First, narratives prompt identification with characters in the story who model healthy behaviors and demonstrate the consequences of that behavior.4,6 Second, narratives facilitate transportation, a phenomenon in which individuals become immersed, or involved into a storyline.17, 18 When this happens, barriers to change such as counterarguing are suppressed.4,15,19 and the individual is more likely to attend to the information being presented and respond accordingly. Finally, narratives can prompt emotional responses, such as fear, anger, sadness and happiness2,20,21 which, in turn, can motivate positive health outcomes in response to the message.22,24 To produce such effects, narratives embed health information into a story. Whereas a non-narrative message might explicitly state that the HPV vaccine can prevent the cervical cancer-causing Human Papillomavirus (HPV) in the context of other facts about HPV and cervical cancer, a narrative message might embed this fact within the larger context of a story not necessarily related to cervical cancer. For example, a message about the HPV vaccine preventing cervical cancer might be embedded into a narrative about a mother-daughter relationship.
The second body of literature informing this study investigates strategies for effectively communicating health information to individuals with low health literacy. Individuals with low health literacy not only have poorer health outcomes than those with adequate health literacy24 but also tend to benefit less from health education interventions.7-9 As a result, it is critical to ensure that narrative health education messages benefit both those with low and with adequate health literacy equally. There are several sets of guidelines (e.g. CDC's Clear Communication Index, NIH's Plain Language guidelines, AHRQ's Health Literacy Universal Precautions Toolkit) to help health communicators and educators convey information to individuals with low health literacy. These guidelines contain strategies and suggestions to help ensure everyone – and in particular, individuals with low health literacy – is able to comprehend and apply the health information conveyed in a public health message. For example, CDC's Clear Communication Index encourages practitioners to create health education materials that contain an identifiable main message presented at the beginning and to break up information into chunks with headers. Sheridan and colleagues25 identify similar evidence-based strategies that can help health professionals develop materials to reach individuals with low health literacy, such as presenting essential information first and by itself and presenting numerical information in text. Although the use of narrative health education materials is recommended by organizations such as the CDC26 and has been highlighted as a potential health communication strategy to reduce health disparities,27 clear communication and plain language guidelines focus primarily on written, printed and oral communication. There is limited guidance for the communication of health information using narrative form and especially for video-based formats. Given the increasing use of narratives to communicate health information, the rapid changes in contemporary media and technology environment and the increasingly ubiquitous nature of videos – whether through traditional channels such as television or internet sites like YouTube – understanding and developing guidelines on how video-based health education materials affect populations of interest is imperative.
Much of the work testing narrative materials in low health literacy populations has focused on the use of narratives in print materials (e.g. fotonovelas;28-32). This line of research indicates that printed narrative health education materials may in fact be appropriate for populations with low health literacy. Other work has integrated narrative materials with standard-of-care non-narrative materials. For instance, Jibaja-Weiss and colleagues33 found that, when added to standard non-narrative usual care materials, an entertainment-based decision aid for early stage breast cancer patients with low health literacy produced greater knowledge and certainty about one's decision than the non-narrative usual care materials alone. Davis and colleagues34 similarly found that incorporating a short, soap opera-like narrative about breast cancer screening into patient educational materials significantly increased mammography utilization among low-literacy women six months post-intervention. Volk and colleagues35 found that an entertainment-based decision aid for prostate cancer screening produced greater self-advocacy among low health literacy patients than a non-narrative audiobooklet.
Together, these studies support the use of narrative in low health literacy populations. However, several gaps in our knowledge remain. First, there is limited research on the use of narrative materials in non-clinical populations with low health literacy. Second, there are few randomized trials comparing narratively formatted health information against an equivalent non-narrative presentation of identical information. Finally, there is limited work testing whether non-interactive video-formatted narrative health education materials benefit individuals with low and high levels of health literacy equally. Because individuals with low levels of health literacy do not always equitably benefit from health education interventions,7,8 it is crucial to build an evidence base supporting the use of different narrative formats in this population. This need for research examining narrative video in low health literacy populations becomes increasingly important as more individuals obtain health information from television, YouTube and other video-based formats.36-38 Additionally, video-based formats present a unique opportunity for practitioners to reach a large population of individuals in many contexts: for example, videos can be shown in clinic waiting rooms, schools, churches or at community events. Video-based materials can also be used to reach large segments of the population: for example, educational storylines placed on prominent network television shows.6,39,40
The current study responds to this need by presenting an initial study examining how a small sub-group of women with low health literacy responded to a narrative or non-narrative film about cervical cancer, in comparison to a larger group of women with adequate health literacy. Specifically, we compare the acceptability and efficacy (knowledge gain) of the narrative and the non-narrative film (each containing identical health information) between these two groups. To do so, we analyzed data from a randomized study in a sample of African American, Korean American, Mexican American and non-Hispanic white women living in Los Angeles.
Method
This work was part of a larger randomized study comparing the effectiveness of a narrative and non-narrative cervical cancer education film in a general population of African American, Korean American, Mexican American and non-Hispanic white women in Los Angeles.41, 42 Although the primary aim of this larger study did not involve comparing the efficacy of the films in women with varying levels of health literacy, we included a measure of health literacy so that we could conduct post-hoc analyses to examine the relative effects. All study procedures were approved by the researchers’ university Institutional Review Board.
Participants and Procedure
African American, Korean American, Mexican American and non-Hispanic white women in the greater Los Angeles area participated in both baseline and post-test surveys. Participants were recruited primarily through a random selection procedure that incorporated random digit dial and ethnically-targeted small area geographic lists to create a sampling frame. The response rate for the baseline survey was 2.5%, and the cooperation rate for the baseline survey was 4%. The low response rate may have been due to the large number of disconnected or non-household numbers in the sampling frame; however, our sample was still large enough to be adequately powered. Eighty-five percent of participants who completed the baseline survey also completed the post-test survey. Up to six call attempts were made to sampled phone numbers for the pre-test survey, and up to thirty five call attempts were made to reach participants for the post-test survey. Both surveys were administered over the phone using computer-assisted telephone interviewing (CATI). Inclusion criteria were that participants be between the ages of 25-45, not have a previous diagnosis of cervical cancer, have the ability to view a DVD, and be fluent in English (as both films were in English). After completing the baseline survey, participants were randomly assigned to view either the narrative or non-narrative film, which was mailed to their home as a DVD. Before administering the post-test survey two weeks later, we verified that participants had watched the film by asking them to answer questions about the film content. This resulted in a sample of 775 participants. One participant did not answer all of the questions needed for the current analysis, resulting in a sample size of 774 used for analysis. Chi-square and t-tests to test differences between participants in each condition did not reveal any significant differences in race, income, education, age, prior Pap test status, pre-test knowledge or health literacy level.
Experimental materials
The experimental materials consisted of a non-narrative and a narrative cervical cancer educational film. Cervical cancer was chosen as the topic because it is a disease for which significant ethnic health disparities exist43 and a disease that is also highly preventable and treatable.44 Each film was 11 minutes long and contained identical facts about Pap tests, HPV, the HPV vaccine and cervical cancer. The non-narrative film used a traditional style that featured doctors and women presenting facts and information. The narrative film featured a family in which the oldest daughter found out she had HPV; the women in the family discussed HPV, Pap tests, and the HPV vaccine, as they prepared for their youngest daughter's fifteenth birthday celebration (quinceañera). Figure 1 displays still shots from each film. More details on the films are provided by Authors blinded.42 The full videos can be found at https://www.dropbox.com/sh/ui4creo6pv8nxxv/AADxr_fC8s0iRJmxTgJUF1oxa?dl=0.
Figure 1.
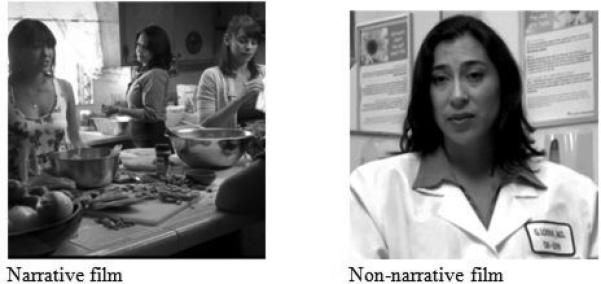
Still shots from the narrative and non-narrative videos.
Measures
Health literacy
Participants were asked the question “How confident are you filling out medical forms by yourself?” and could respond “Not at all confident,” “A little bit confident,” “Somewhat confident,” “Quite a bit confident” and “Extremely confident.” Based on the recommendation of Chew et al.,46 participants who responded “Not at all confident,” “A little bit confident,” or “Somewhat confident,” were coded as having low health literacy (‘0’) while participants who responded “Quite a bit confident” or “Extremely confident” were coded as having adequate health literacy (‘1’). This item has been validated against face-to-face measures of health literacy (REALM, S-TOFHLA) and a cut-off point of ‘somewhat confident’ can distinguish between individuals with low (inadequate or marginal) and adequate health literacy with sufficient sensitivity and specificity.46-49 This single-item measure is recommended for use when more traditional measures that involve considerable time or face-to-face interaction are not feasible.48,50
Acceptability
We assessed the acceptability of the films by asking participants how interesting they thought the film was (1= ‘not interesting at all,’ 10 = ‘very interesting’), how much they liked the film (1=‘not at all,’ 10 =‘very much’) and how much they enjoyed watching the film (1=‘not at all,’ 10=’very much’). Responses to these items were averaged to create a scale representing acceptability of the film (α = .94)
Knowledge
Participants were asked 9 questions about cervical cancer and HPV such as “How is HPV transmitted?” and “If a woman is not sexually active, at what age should she start getting regular Pap tests?” Both films addressed each of these knowledge items. Responses were coded as correct (‘0’) or incorrect (‘1’) and summed to create a cervical cancer knowledge index. The outcome of interest for this analysis was change in knowledge from baseline to post-test.
Analysis
We used independent samples t-tests to examine the bivariate relationships between health literacy and pre-test knowledge. We used ANCOVA to test for the main effects of film condition and health literacy on the outcomes of interest and to probe the interaction between health literacy and film condition on the outcomes of interest. Both analyses controlled for ethnicity and the analysis for post-test knowledge change controlled for pre-test knowledge levels. We specified sum of squares Type 2 due to the unequal number of participants with adequate and low health literacy. All analyses were run using SPSS 17.0.51
Results
Descriptive statistics and bivariate analyses
Table 1 presents descriptive statistics for the entire sample and split by health literacy level. Seventy-four participants (9.6%) had low health literacy, while the remaining 700 (90.4%) had adequate health literacy. Health literacy was significantly associated with baseline knowledge before exposure to the intervention such that those with low health literacy answered significantly fewer questions correctly. Health literacy was also associated with ethnicity, such that non-Hispanic whites were less likely than the other ethnic groups to have low health literacy, and with income, such that those earning less than $30,000 were more likely to have low health literacy.
Table 1.
Sample Descriptive Statistics(a)
| Low health literacy (N = 74) | Adequate health literacy (N = 700) | Total sample (N = 774) | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Race** | |||
| African American | 23 (31.3%) | 199 (28.4%) | 222 (28.7%) |
| Korean American | 14 (18.9%) | 57 (8.1%) | 71 (9.2%) |
| Mexican American | 23 (31.1%) | 210 (30.0%) | 233 (30.1%) |
| Non-Hispanic white | 14 (18.9%) | 234 (33.4%) | 248 (32.0%) |
| Income** | |||
| Income ≤ $30,000/year | 27 (37.5%) | 140 (20.9%) | 167 (21.6%) |
| Income > $30,000/year | 45 (62.5%) | 531 (79.1%) | 576 (74.4%) |
| Education | |||
| ≤ High school education | 13 (17.6%) | 105 (15.0%) | 118 (15.2%) |
| > High school education | 61 (82.4%) | 594 (85.0%) | 655 (84.6%) |
| Pap test status at pre-test | |||
| Up-to-date with Pap | 12 (16.2%) | 71 (10.2%) | 83 (10.7%) |
| Not up-to-date with Pap | 62 (83.8%) | 623 (89.8%) | 685 (88.5%) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
|---|---|---|---|
| Age | 37.7 (6.1) | 38.2 (5.7) | 38.2 (5.7) |
| Baseline knowledge (range 1-9) ** | 4.1 (1.7) | 4.7 (1.7) | 4.6 (1.7) |
| Post-test knowledge change (range 0-9) | 2.1 (1.8) | 1.8 (1.6) | 1.9 (1.6) |
| Acceptability (range 1-10) | 8.4 (1.6) | 8.1 (1.9) | 8.2 (1.9) |
a. **denotes variables that varied by health literacy at p < .01 in bivariate analyses
Multivariate analysis
Results of the ANCOVA indicate that film condition had a significant main effect on change in knowledge from baseline to post-test (η2partial = .008, F(1,766) = 5.916, p = .015), such that the narrative film produced a greater change in knowledge. Health literacy did not have a main effect on post-test knowledge gain (η2partial = .000, F(1,766) = .170, p = .680). Regardless of health literacy level, viewers of the narrative knew two additional knowledge items at post-test. Health literacy did not interact with film condition to affect post-test knowledge gain (η2partial = .001, F(1,766) = .519, p = .472).
The narrative film was also deemed more acceptable than the non-narrative film (η2partial = .005, F(1,767) = 4.055 , p = .044). Health literacy did not have a direct effect on acceptability (η2partial = .002, F(1,767) = 1.377, p = .241), nor did it interact with film condition to affect acceptability (η2partial = .001, F(1,767) = .624, p = .430). Adjusted means for post-test knowledge change and acceptability are presented in Table 2.
Table 2.
Means and confidence intervals for knowledge and acceptability by health literacy status and film condition(a)
| Low health literacy | Adequate health literacy | |||
|---|---|---|---|---|
| Non-narrative M [95% CI] | Narrative M [95% CI] | Non-narrative M [95% CI] | Narrative M [95% CI] | |
| Post-test knowledge change | 1.6 [1.2, 2.0] | 2.0 [1.6, 2.3] | 1.8 [1.6, 1.9] | 2.0 [1.8, 2.1] |
| Acceptability | 8.4 [7.8, 9.0] | 8.3 [7.8, 8.9] | 7.9 [7.8, 8.1] | 8.2 [8.1, 8.4] |
a. All estimates adjusted for ethnicity; estimates for post-test knowledge change also adjusted for baseline knowledge
Discussion
This analysis found that the narrative film had a slightly higher level of acceptability than the non-narrative film. Additionally, the narrative film had a significantly greater impact on post-test knowledge than the non-narrative film. Importantly, even though health literacy was associated with baseline knowledge, neither acceptability of the film nor knowledge change was affected by the participant's health literacy level. This indicates that while participants responded favorably to both films, the narrative film was particularly effective and that a low level of health literacy did not suppress participants’ favorable response to the film. Because individuals with low health literacy tend to benefit less from existing health communication interventions,7, 8 it is critical to ensure that health communication materials equitably serve both groups. This study's findings add to the emerging evidence base supporting the use of narrative video in low health literacy populations.
These findings corroborate others’ work linking health literacy with health and disease knowledge52-54 and underscore the potential of narrative to help overcome knowledge gaps and health disparities between individuals with low and high health literacy. The fact that key pieces of information were embedded into the narrative, rather than explicitly stated in an overt and direct way, did not impede the transmission of information. Additionally, beyond their ability to increase knowledge, health-related narratives are particularly well-suited to impact other determinants of health behavior such as perceived susceptibility to a disease or negative health outcome, perceived health-related social norms and health beliefs.55-57 Another important advantage of narratives is that they do not use a traditional educational format in favor of an entertainment-based style that audiences recognize. Populations with low health literacy may have had prior negative experiences with difficult and complicated health education materials and as a result may avoid or quickly disengage when presented with traditionally formatted materials – even when those materials follow clear communication guidelines. Using stories instead of overtly portrayed facts and statistics, narrative health education materials can engage audiences and convey information in a less threatening and more appealing way.
While this study's findings indicate that narrative health education video is appropriate for populations with low health literacy, there is a need for research to inform the development of guidelines regarding the use of narrative health education video in populations with low health literacy. Several sets of guidelines provide useful, evidence-based advice for the creation of printed, written and oral health communication (e.g. CDC's Clear Communication Index, NIH's Plain Language guidelines, AHRQ's Health Literacy Universal Precautions Toolkit). However, while some of these guidelines can apply to narrative health education videos, narrative video also has several unique features that require specific guidance and would benefit from further study. For example, guidelines informing the development of a script that can both engage the audience and communicate health information clearly would help ensure narrative health education materials are developed so that they can be understood by all.
This study represents an initial effort to assess the appropriateness of narrative health education films for populations with low health literacy. As such, several limitations must be addressed. Foremost is the small sample size of individuals with low health literacy. Although steps were taken analytically to account for these unequal group sizes, it would be beneficial to test these materials with a larger sample of individuals with low health literacy. Additionally, while we used a validated measure of health literacy that was appropriate for a phone survey, it could be useful to replicate the study using other measures of health literacy. The response rate of 2.5% for our survey was lower than typical response rates (see Pew's 2012 report59), which may have been due to the large number of disconnected or non-household numbers in the sampling frame; however, our sample was still large enough to be adequately powered. Finally, while the materials we tested focused on cervical cancer prevention, narratives can be and have been used to convey information about a variety of health topics.
Implications and conclusions
Despite these limitations, this study had several strengths, including the use of random selection in the sampling procedure and its randomized experimental design. This study's findings indicate that the narrative film worked equally well for individuals with low and adequate health literacy and was considered to be more acceptable than the non-narrative film by both groups. These findings have important implications for health communication policy and recommendations. There is a compelling body of research demonstrating that when new information is disseminated, those with more advantaged structural positions acquire that information at a faster rate, such that a knowledge gap develops or widens.9,58 In other words, health education materials can potentially exacerbate health disparities based on differential levels of health literacy among audience members. Without careful consideration from material developers, individuals with higher health literacy levels are likely to get more out of health education materials than those with lower health literacy levels.7,8 Thus, it is critical to develop evidence supporting the use of health communication strategies that can reduce these gaps. This study contributes here by providing evidence indicating that a narrative health education video may be appropriate for use in low health literacy populations and does not exacerbate existing disparities between individuals with low and high health literacy. This study's findings that the ability of the narrative films to be as acceptable and as effective in promoting knowledge gain among women with low health literacy as among those with adequate health literacy is promising. If we are to eliminate health literacy-related health disparities, we must ensure that we develop a range of health education materials that will benefit individuals of all levels of health literacy equally.
Acknowledgments
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health [R01CA144052 awarded to Murphy/Baezconde-Garbanati]. Dr. Moran was supported by the National Institute on Drug Abuse at the National Institutes of Health [K01DA037903].
Biography
Dr. Moran is an assistant professor in the Department of Health, Behavior and Society at the Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University. Dr. Frank is an assistant professor in the School of Communication at Portland State University. Dr. Chatterjee is an instructor at the Annenberg School for Communication & Journalism at the University of Southern California. Dr. Murphy is a professor Annenberg School for Communication & Journalism at the University of Southern California. Dr. Baezconde-Garbanati is an associate professor in Preventive Medicine and Sociology at the Keck School of Medicine, University of Southern California.
Footnotes
Conflict of Interest Statement: None of the authors have anything to disclose.
References
- 1.Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, et al. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007;33:221–35. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 2.Bollinger S, Kreuter MW. Real-time moment-to-moment emotional responses to narrative and informational breast cancer videos in African-American women. Health Educ Res. 2012;27:537–43. doi: 10.1093/her/cys047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green MC. Narratives and cancer communication. J Commun. 2006;56:S163–183. [Google Scholar]
- 4.McQueen A, Kreuter MW, Kalesan, Alcaraz KI. Understanding narrative effects: the impact of breast cancer survivor stories on message processing, attitudes, and beliefs among African American women. Health Psychol. 2011;30:674–82. doi: 10.1037/a0025395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy ST, Frank LB, Chatterjee JS, et al. Narrative versus nonnarrative: the role of identification, transportation, and emotion in reducing health disparities. J Commun. 2013;63:116–37. doi: 10.1111/jcom.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murphy ST, Frank LB, Moran MB, Patnoe-Woodley P. Involved, transported, or emotional? Exploring the determinants of change in knowledge, attitudes, and behavior in entertainment-education. J Commun. 2011;61:407–31. [Google Scholar]
- 7.Boxell EM, Smith SG, Morris M, Kummer S, Rowlands G, Waller J, et al. Increasing awareness of gynecological cancer symptoms and reducing barriers to medical help seeking: does health literacy play a role? J Health Commun. 2012;17:265–79. doi: 10.1080/10810730.2012.712617. [DOI] [PubMed] [Google Scholar]
- 8.Gazmarian JA, Yang B, Elon L, Graham M, Parker R. Successful enrollment in Text4Baby more likely with higher health literacy. J Health Commun. 2012;17:303–11. doi: 10.1080/10810730.2012.712618. [DOI] [PubMed] [Google Scholar]
- 9.Viswanath K, Emmons KM. Health communication and communication inequalities in addressing cancer disparities. In: Koh HK, editor. Toward the elimination of cancer disparities. Springer; New York: 2009. pp. 277–98. [Google Scholar]
- 10.Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav. 2006;34(5):777–92. doi: 10.1177/1090198106291963. [DOI] [PubMed] [Google Scholar]
- 11.Niederdeppe J, Shapiro MA, Kim HK, Bartolo D, Porticella N. Narrative persuasion, causality, complexity and support for obesity policy. Health Commun. 2014;29:431–44. doi: 10.1080/10410236.2012.761805. [DOI] [PubMed] [Google Scholar]
- 12.Singhal A, Cody MJ, Rogers ME, Sabido M, editors. Entertainment-education and social change: history, research and practice. Lawrence Erlbaum Associates; Mahwah, NJ: 2004. [Google Scholar]
- 13.Wang H, Singhal A. Entertainment-education through digital games. In: Ritterfield U, Cody MJ, Vorderer P, editors. Serious games: mechanisms and effects. Routledge; New York: 2009. pp. 271–92. [Google Scholar]
- 14.Banerjee SC, Greene K. Role of transportation in the persuasion process: cognitive and affective responses to antidrug narratives. J Health Commun. 2012;17(5):564–81. doi: 10.1080/10810730.2011.635779. [DOI] [PubMed] [Google Scholar]
- 15.Moyer-Gusé E. Toward a theory of entertainment persuasion: explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008;2008;18:407–25. [Google Scholar]
- 16.Moyer-Gusé E, Nabi RL. Explaining the effects of narrative in an entertainment television program: overcoming resistance to persuasion. Hum Commun Res. 2010;36:26–52. [Google Scholar]
- 17.Busselle RW, Bilandzic H. Fictionality and perceived realism in experiencing stories: A model of narrative comprehension and engagement. Commun Theory. 2008;18:255–80. [Google Scholar]
- 18.Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol. 2000;79:701–21. doi: 10.1037//0022-3514.79.5.701. [DOI] [PubMed] [Google Scholar]
- 19.Slater MD, Rouner D. Entertainment Education and elaboration likelihood: understanding the processing of narrative persuasion. Commun Theory. 2002;12:173–91. [Google Scholar]
- 20.Dillard J, Peck E. Affect and persuasion: Emotional responses to public service announcements. Communic Res. 2000;27:461–95. [Google Scholar]
- 21.Nabi RL, Green MC. The role of a narrative's emotional flow in promoting persuasive outcomes. Media Psychol. Advanced publication ahead of print. 2014 10.1080/15213269.2014.912585. [Google Scholar]
- 22.Dillard JP, Nabi RL. The persuasive influence of emotion in cancer prevention and detection messages. J Commun. 2006;56:S123–S139. [Google Scholar]
- 23.Yoo JH, Kreuter MW, Lai C, Fu Q. Understanding narrative effects: the role of discrete negative emotions on message processing and attitudes among low-income African American women. Health Commun. 2014;29:494–504. doi: 10.1080/10410236.2013.776001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 25.Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16:30–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- 26.Health Literacy – Science Says: Findings You Can Use [Internet] Centers for Disease Control; Atlanta (GA): [March 16, 2015]. [updated Feb 13, 2014; cited March 16, 2015]. Available from: http://www.cdc.gov/healthliteracy/sciencesays/. [Google Scholar]
- 27.Freimuth VS, Quinn SC. The contributions of health communication to eliminating health disparities. Am J Public Health. 2004;94(12):2053–55. doi: 10.2105/ajph.94.12.2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cabassa LJ, Molina GB, Baron M. Depression fotonovela development of a depression literacy tool for Latinos with limited English proficiency. Health Promot Pract. 2012;13:747–54. doi: 10.1177/1524839910367578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernandez MY, Organista KC. Entertainment–education? A fotonovela? A new strategy to improve depression literacy and help-seeking behaviors in at-risk immigrant Latinas. Am J of Community Psychol. 2013;52:224–35. doi: 10.1007/s10464-013-9587-1. [DOI] [PubMed] [Google Scholar]
- 30.Unger JB, Cabassa LJ, Molina GB, Contreras S, Baron M. Evaluation of a fotonovela to increase depression knowledge and reduce stigma among Hispanic adults. J Immigr Minor Health. 2013;15:398–406. doi: 10.1007/s10903-012-9623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valle R, Yamada AM, Matiella AC. Fotonovelas: A health literacy tool for educating Latino older adults about dementia. Clin Gerontol. 2006;30:71–88. [Google Scholar]
- 32.Michielutte R, Bahnson J, Dignan MB, Schroeder EM. The use of illustrations and narrative text style to improve readability of a health education brochure. J Cancer Educ. 1992;7:251–60. doi: 10.1080/08858199209528176. [DOI] [PubMed] [Google Scholar]
- 33.Jibaja-Weiss ML, Volk RJ, Granchi TS, Neff NE, Robinson EK, Spann SJ, et al. Entertainment education for breast cancer surgery decisions: a randomized trial among patients with low health literacy. Patient Educ Couns. 2011;84(1):41–8. doi: 10.1016/j.pec.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 34.Davis TC, Berkel HJ, Arnold CL, Nandy I, Jackson RH, Murphy PW. Intervention to increase mammography utilization in a public hospital. J Gen Intern Med. 1998;13:230–33. doi: 10.1046/j.1525-1497.1998.00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Volk RJ, Jibaja-Weiss ML, Hawley ST, Kneuper S, Spann SJ, Miles BJ, et al. Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns. 2008;73(3):482–89. doi: 10.1016/j.pec.2008.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dutta-Bergman MJ. Primary sources of health information: comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004;16:273–88. doi: 10.1207/S15327027HC1603_1. [DOI] [PubMed] [Google Scholar]
- 37.Friedrich B. Trends in health communication. Journal of Media Psychol. 2014;26:1–3. [Google Scholar]
- 38.Madathil KC, Rivera-Rodriguez AJ, Greenstein JS, Gramopadhye AK. Healthcare information on YouTube: A systematic review. Health Informatics. J. 2014 doi: 10.1177/1460458213512220. Advanced publication ahead of print: 10.1177/1460458213512220. [DOI] [PubMed] [Google Scholar]
- 39.Morgan SE, Movius L, Cody MJ. The power of narratives: The effect of entertainment television organ donation storylines on the attitudes, knowledge, and behaviors of donors and nondonors. J Commun. 2009;59(1):135–51. [Google Scholar]
- 40.Movius L, Cody M, Huang G, Berkowitz M, Morgan S. Motivating television viewers to become organ donors. Cases in Public Health Communication & Marketing. 2007;1:1–21. [Google Scholar]
- 41.Murphy ST, Frank LB, Chatterjee J, Moran MB, Zhao N, de Herrera P, et al. Comparing the relative efficacy of narrative versus non-narrative health messages in reducing health disparities using a randomized trial. Am J Public Health. 2015 Apr;23:e1–e7. doi: 10.2105/AJPH.2014.302332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baezconde-Garbanati LA, Chatterjee JS, Frank LB, Murphy ST, Moran MB, Werth LN, et al. Tamale Lesson: a case study of a narrative health communication intervention. J Commun Healthc. 2014;7(2):82–92. [Google Scholar]
- 43.US Cancer Statistics Working Group . United States Cancer Statistics: 1999-2011 Incidence and Mortality Web-based Report. [Internet] U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; Atlanta (GA): 2014. [March 25, 2015]. Available from: http://apps.nccd.cdc.gov/USCS/cancersbyraceandethnicity.aspx. [Google Scholar]
- 44.American Cancer Society . Cancer facts & figures for Hispanics/Latinos 2012-2014 [Internet] American Cancer Society Inc; Atlanta (GA): 2012. [March 16, 2015]. Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-034778.pdf. [Google Scholar]
- 45.Medline Plus: Cervical Cancer [Internet] National Library of Medicine and National Institutes of Health; Bethesda (MD): [March 16, 2015]. pp. c1997–2015. [updated June 15, 2015; cited March 16, 2015]. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000893.htm. [Google Scholar]
- 46.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Internal Med. 2008;23:561–66. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94. [PubMed] [Google Scholar]
- 48.Sarkar U, Schillinger D, López A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26:265–71. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss D. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874–77. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304:76–84. doi: 10.1001/jama.2010.896. [DOI] [PubMed] [Google Scholar]
- 51.SPSS Inc. SPSS Statistics for Windows, Version 17.0. SPSS Inc.; Chicago: 2008. [Google Scholar]
- 52.Gazmarian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 53.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am J of Health Behav. 2011;36:118–28. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease: a study of patients with hypertension and diabetes. Archives Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 55.Frank LB, Murphy ST, Chatterjee J, Moran MB, Baezconde-Garbanati L. Telling stories, saving lives: creating narrative health messages. Health Commun. 2015;30(2):154–63. doi: 10.1080/10410236.2014.974126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Moran MB, Murphy ST, Frank L, Baezconde-Garbanati L. The ability of narrative communication to address health-related social norms. Int Rev of Soc Res. 2013;3:131–49. doi: 10.1515/irsr-2013-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moyer-Gusé E, Nabi RL. Explaining the effects of narrative in an entertainment television program: overcoming resistance to persuasion. Hum Commun Res. 2010;36:26–52. [Google Scholar]
- 58.Guttman N, Salmon CT. Guilt, fear, stigma and knowledge gaps: ethnical issues in public health communication interventions. Bioethics. 2004;18:531–52. doi: 10.1111/j.1467-8519.2004.00415.x. [DOI] [PubMed] [Google Scholar]
- 59.The Pew Research Center for People and the Press Assessing the representativeness of public opinion surveys. 2012 Available from: http://www.people-press.org/2012/05/15/assessing-the-representativeness-of-public-opinion-surveys/


