Abstract
Stress has been identified as a significant factor in health and in racial/ethnic health disparities through biological and psychological mechanisms. A potential mediator in these relationships is body weight. Cross-sectional and longitudinal relationships between perceived stress, race, body weight, and weight change were examined in an ethnically diverse sample of overweight and obese women with type 2 diabetes (n=217) undergoing an intensive behavioral weight loss program. Measures were collected at baseline and 6-months. Stress was not related to baseline body weight. With every 1 unit decrease in perceived stress, −.10 kg ± .04 of weight was lost (p<.05). When stress was divided into tertiles, those in the lowest stress group had significantly greater weight loss (5.2 kg ± 4.9) compared to those in the highest stress group (3.0 kg ± 4.0) (p<.05). There was a statistical trend of African Americans reporting greater levels of mean stress (20.7 ± 8.8) than Whites (18.3 ± 8.3) (p=.08). Stress’ association with lower weight loss has important implications for weight loss programs for women with type 2 diabetes. Future examinations of stress, race, and body weight would benefit the science of weight loss treatment for diverse populations and increase understanding of psychosocial factors in body weight and obesity etiology.
Keywords: Stress, race, body weight, obesity, health disparities
Stress is the process of adaptation in response to a physical or psychological challenge, and affects well-being through disrupting the equilibrium of physical and psychological systems (Lazarus & Cohen, 1977). Linked to the etiology of chronic disease and various disease endpoints (Wenzel, Glanz, & Lerman, 2002), stress has been hypothesized to be an explanatory factor for racial/ethnic disparities in health through differential exposure to acute and chronic stressors (Geronimus, Hicken, Keene, & Bound, 2006; Schulz et al., 2000). African Americans report higher chronic stressors (Turner & Avison, 2003), total stress (Turner & Avison, 2003), discrimination (Turner & Avison, 2003), and stressful life events (Schulz et al., 2000; Turner & Avison, 2003) than Whites. Physiological measures of stress, such as allostatic load, are higher in African Americans, even after controlling for income (Geronimus et al., 2006). Various biological, behavioral, and psychological mechanisms have been proposed to explain the connection between stress and health (Kelly, Hertzman, & Daniels, 1997; McEwen, 2006). A potential mediator is body weight.
Stress may be related to body weight and weight change through several mechanisms. Individuals who eat in response to stress exhibit an increased preference for high fat and/or sweet foods (Epel, Lapidus, McEwen, & Brownell, 2001; Ng & Jeffery, 2003), which may lead to increased body weight. Stress may also deter an individual from engaging in physical activity (Ng & Jeffery, 2003). Excess body weight and physical inactivity have been linked to poor health outcomes (Fontaine, Redden, Wang, Westfall, & Allison, 2003; Mokdad, Marks, Stroup, & Gerberding, 2004; Must et al., 1999). Stress can also encourage dietary disinhibition, or lapses in dietary intake among dieting individuals (Balfour, Romano White, Schiffrin, Dougherty, & Dufresne, 1993). Individuals who are overweight or obese may be particularly vulnerable to dieting disinhibition (Bellisle et al., 2004; Cerrelli et al., 2005; Hainer et al., 2006), which may deter weight loss efforts.
Stress may also contribute to racial/ethnic differences in obesity. African Americans, particularly African American women (Davis, Clark, Carrese, Gary, & Cooper, 2005; Kumanyika, 2002a, 2002b; Kumanyika & Morssink, 1997), bear a disproportionate burden of the obesity epidemic (Ogden et al., 2006) and lose less weight than their White counterparts when in obesity treatment programs (Kumanyika, 2002a; Wing et al., 2004). The unique and/or added stress African Americans may experience in the context of U.S. society may contribute to differential obesity rates and modest success in weight management. The higher obesity rates within African American populations may contribute to the significant and broad range of racial/ethnic health disparities (Kumanyika, 2005).
Few studies have examined the contribution of stress to body weight, and the role of race/ethnicity in the stress-body weight connection. Fewer studies have examined relationships between stress, race, and body weight in women and overweight individuals. In a national sample, men and women reporting a greater number of stressful days in the past 30 days had a higher body mass index (BMI) (Smith & McFall, 2005). Women reporting greater health, legal, and financial stress were more likely to be severely obese than women reporting less perceived stress (Wadden et al., 2006). Perceived stress was also related to higher baseline BMI in adult men and women with impaired glucose tolerance (Delahanty, Meigs, Hayden, Williamson, & Nathan, 2002). In young adult African American women, higher perceived stress was associated with greater overweight and decreased weight control behavior (Walcott-McQuigg, 1995), and higher work stress, conceptualized as job demand, was related to higher BMI among British women (Kivimaki et al., 2006). A cross-sectional study of adults with impaired glucose tolerance reported no interaction of race in the relationship between perceived stress and BMI (Delahanty et al., 2002).
Longitudinal examinations of stress and weight have identified that stress is associated with both greater weight gain and lower weight loss among overweight British men (Kivimaki et al., 2006), but no relationships were apparent between stress and weight in British women. Among leaner men (BMI < 22), higher levels of work stress were related to lower weight gain and higher weight loss (Kivimaki et al., 2006). In a Finnish sample, overweight men who lost at least 5% of their weight but regained more than they initially lost reported higher levels of perceived stress than men who lost and maintained their weight loss (Sarlio-Lahteenkorva, Rissanen, & Kaprio, 2000). However, no association between daily stress and weight trajectory was observed among women who had lost and regained weight.
Overall, few studies have examined the relationship between stress and body weight, particularly the contribution of stress to body weight longitudinally. To the authors’ knowledge, only two studies have addressed stress and weight longitudinally (Kivimaki et al., 2006; Sarlio-Lahteenkorva et al., 2000), and these relationships were examined in European samples. Furthermore, the role of race/ethnicity in relationships between stress and body weight in a multi-ethnic sample has only been examined in one cross-sectional study, which examined overweight US adults with impaired glucose tolerance (Delahanty et al., 2002).
Stress may play an important role in body weight, weight change, and related disparities, but the dearth of research about these relationships merits further examination. Thus, this analysis sought to examine relationships between stress, race, weight, and weight change.
Method
Cross-sectional and longitudinal associations between stress and weight were examined within the context of a randomized, controlled treatment outcome study that examined whether the addition of motivational interviewing (MI) sessions to a group-based behavioral weight control program for overweight women with type 2 diabetes produced greater weight loss than the weight loss program alone. Study methods and primary outcomes have been reported in greater detail (West, DiLillo, Bursac, Gore, & Greene, 2007). In brief, women were randomized to receive individual sessions of either MI or an attention placebo control as an adjunct to a group-based behavioral weight control program; experimental condition was the nature of the individual sessions and not the group-based behavioral weight control program. All women received the same weight loss program, which met weekly for 24 weeks and was delivered by interventionists masked to experimental assignment. The program focused on dietary and physical activity habits, with a strong emphasis on goal setting and problem solving to achieve successful behavior change. Baseline data were obtained across two clinic visits and 6-month follow-up data at a single clinic visit. All research procedures were approved by the University of Alabama at Birmingham Institutional Review Board for Human Use and the University of Arkansas for Medical Sciences Institutional Review Board.
Study Sample
Overweight women with type 2 diabetes were recruited using newspaper and neighborhood advertising, direct mail solicitation, and physician referrals. Potential volunteers were phone screened and then invited to a group orientation where the study was described and informed consent obtained.
Women were eligible if they had type 2 diabetes treated by oral diabetes medications but not insulin, were overweight (BMI of 27- 50), and were generally healthy and could walk for exercise. Those with uncontrolled diabetes (HbA1c > 12%) or hypertension (diastolic blood pressure > 90 or systolic blood pressure > 140) were referred to their physician for treatment and invited to re-screen. Exclusion criteria included pregnancy, recent significant weight loss (≥ 10 lbs), or a severe debilitating disease that might interfere with study participation. Volunteers obtained physician’s consent to participate and completed a 7-day diary monitoring dietary intake before study entry. A total of 561 women were screened with 217 women (39% African American) randomized.
Measures
Measures were collected at baseline and 6 months by data collectors masked to treatment assignment. Body weight was measured without shoes using a calibrated balance beam scale. Height was measured without shoes using a wall-mounted stadiometer. BMI was calculated as weight [kg] / height [m]2. Weight change was calculated as the difference in weight between baseline and 6 months. Demographic information, including self-identified race/ethnicity was obtained by self report at baseline only. Perceived stress was assessed at baseline only with the Cohen 14-item Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983). The PSS assesses perceived stress on a global level over the previous month. Example items include “In the last month, how often have you been upset because of something that happened unexpectedly?” and “In the last month, how often have you felt that you were unable to control the important things in your life?” with responses ranging from ‘Never’ to ‘Often’. The PSS is scored by summing the items (scaled 0 to 4), with 7 items reverse scored. PSS scores range from 0-56, with higher numbers indicating higher perceived stress. The scale has been demonstrated valid and reliable (Cohen et al., 1983) and has been used with African American populations (Culhane et al., 2001; Harville, Savitz, Dole, Thorp, & Herring, 2007).
Statistical Analyses
All analyses were conducted using SAS statistical software (Version 9.1). Descriptive statistics of the sample were generated and Spearman correlations were calculated to explore univariate associations between variables.
Multivariate regression analyses were used to examine cross-sectional and longitudinal relationships between stress and weight, controlling for potential confounding factors as identified, in part, through the correlation analyses. Longitudinal analyses of weight change controlled for baseline weight. Perceived stress did not differ by treatment group; therefore treatment condition was not included in the models. Where there were significant associations between stress and body weight, perceived stress was divided into tertiles and one-way ANOVAs with Tukey adjustments for multiple comparisons was conducted to assess differences in weight loss between stress groups.
Multiple regression and t-tests were conducted to compare differences in body weight at baseline and weight change over 6-months by race/ethnicity. Further, regression analyses and t-tests were conducted to assess whether levels of perceived stress differed by race/ethnicity.
In longitudinal analyses of weight change, baseline weight was carried forward and imputed for body weight data missing at 6-months follow-up (N=7).
Results
Over a third (39%) of the sample was African American and about half (54%) was married or cohabiting (See Table 1). The mean age was 53 years. A little over a third had completed at least a college education or more. The majority were employed and obese (88% with BMI ≥30). Perceived stress scores averaged 19.4± 8.8, which is lower than that reported in an adult community sample (24.0±8.2)(Cohen et al., 1983), female college students (23.6± 7.6)(Cohen et al., 1983), and pregnant women (23.5± 6.4)(Culhane et al., 2001).
Table 1.
Sample Characteristics and Outcomes (Mean ± SD unless otherwise noted)
| Variable | Total Sample (n=217) | White Women | Black Women |
|---|---|---|---|
| African American (%) | 39 | n=133 | n=84 |
| Married (%) | 54 | 56 | 52 |
| Age (years) | 53 ± 10 | 55.6 ± 11 | 49.2 ± 8.9 |
| College Education or higher (%) | 35 | 34 | 37 |
| Employed (%) | 68 | 60 | 81 |
| Weight (kg) | 97 ± 16 | 97 ± 17 | 98 ± 16 |
| BMI | 36.5 ± 5.5 | 36.4 ± 5.7 | 36.7 ± 5.1 |
| Obese (BMI ≥ 30) (%) | 88 | 85 | 92 |
| Perceived Stress | 19.4± 8.8 | 18.6 ± 8.6 | 20.8 ± 8.9 |
Post hoc analyses examining the mean stress levels of completers (n=210) vs. non-completers (n=7) revealed that those who dropped out before 6-month follow up tended to have higher levels of stress [25.3 ± 7.6] than those who completed 6-month follow up [19.2 ± 8.8], but the difference was not statistically significant (p=.08). Thus treatment condition was not considered a confounder and was omitted from analyses.
Demographic characteristics were examined for associations with perceived stress and weight (See Table 2). There was no relationship between race and weight at baseline. African Americans averaged 98.3 ± 15.6 kg at baseline and Whites 96.8 ± 17.1 kg (p=.35). Age and marriage were significantly correlated with baseline weight. Therefore, in multivariate models where baseline weight was the dependent variable, we controlled for these variables. Given the literature on race and weight (Kumanyika, 2002a, 2002b, 2005; Kumanyika, Wilson, & Guilford-Davenport, 1993) and a main focus on race in our analyses, race was also controlled for in regression analyses where baseline weight was the dependent variable.
Table 2.
Spearman Correlations among Perceived Stress, selected Weight variables, and selected Demographics
| Variables | Weight-Baseline | Weight change1 | Age | Race | Education | Employment | Marriage |
|---|---|---|---|---|---|---|---|
| Perceived Stress | .08 | .17* | −.24*** | −.13 | −.03 | −.04 | −.17* |
| Weight-baseline | --- | −.14* | −.26*** | −.05 | −.03 | −.13 | −.16* |
| Weight change1 | --- | --- | −.08 | −.14* | .09 | −.07 | .05 |
| Age | --- | --- | --- | .33*** | −.14* | .45*** | .26*** |
| Race | --- | --- | --- | --- | −.08 | .22** | .14* |
| Education | --- | --- | --- | --- | --- | −.19** | −.09 |
| Employment | --- | --- | --- | --- | --- | --- | .13 |
Weight at 6-month follow minus weight at baseline
=p<05
=p<01
=p<001
Baseline perceived stress was not associated with weight at study entry. However, the correlation between perceived stress and race bordered on statistical significance (p=0.05). This trend in the relationship between race and perceived stress was confirmed with a two sample t-test in which African Americans reported greater mean levels of stress (20.7 ± 8.8) than Whites (18.3 ± 8.5; p=.08). The association between race and stress did not change substantially when controlling for age and marital status (p=.07). There were no significant interactions between race and perceived stress in relationship to weight at baseline.
Perceived stress scores were significantly correlated with weight change (Table 2) such that higher perceived stress was associated with a positive weight change gain. Weight change was also significantly correlated with both race and baseline weight. Group comparisons indicated that Whites lost 1.6 ± 0.66 kg more weight than African Americans (p=.02) but there was no interaction between race, perceived stress and weight change. Therefore, subsequent longitudinal models examining stress and weight change controlled for baseline weight and race.
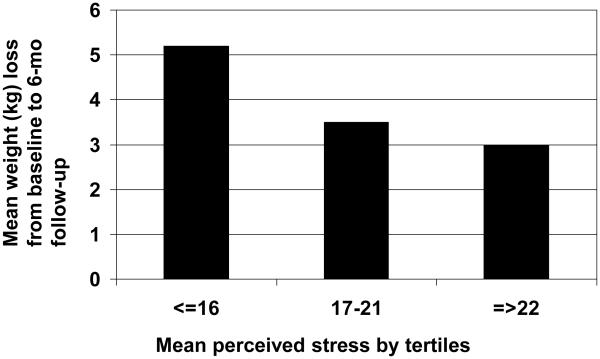
In multivariate models, perceived stress was significantly related to weight change from baseline to 6-months, with women who reported higher levels of perceived stress at baseline losing less weight then women with lower levels of perceived stress. Specifically, with every 1 unit decrease in perceived stress, women lost 0.10 ± .04 kg more weight (p<.05). Controlling for demographic variables (baseline weight, race), the amount of weight lost per unit decrease in stress level was attenuated (0.09 ± .04 kg greater weight loss) but remained significant (p<.05). To further explore the relationship between perceived stress level and weight loss, perceived stress scale scores were divided into tertiles, and mean weight loss was calculated for each stress tertile (Figure 1). Those in the lowest stress quartile (scores ranging from 2 to 16) had a mean weight loss of 5.2 ± 4.9 kg, compared with a mean weight loss of 3.5 ± 4.9 kg for the second stress quartile (scores of 17 to 22) and 3.0 ± 4.0 kg among those in the highest stress quartile (scores of 22 to 47). Women in the lowest stress group had significantly greater weight loss (5.2 ± 4.9 kg) compared to those in the highest stress group (3.0 ± 4.0 kg; p=.01), with women in the middle stress quartile not differing significantly in weight loss from either the lowest or the highest stress groups.
Figure 1.
Mean weight loss (kg) at 6-month follow-up by stress tertiles
Discussion
In our sample of overweight and obese women with type 2 diabetes, higher levels of perceived stress were related to smaller weight losses over 6-months. These results are consistent with other longitudinal studies of stress and weight, which reported significant relationships between stress and weight regain after weight loss (Sarlio-Lahteenkorva et al., 2000) and lower weight loss (Kivimaki et al., 2006) among men. Contrary to the literature reporting significant cross-sectional associations between stress and body weight (Delahanty et al., 2002; Smith & McFall, 2005; Wadden et al., 2006; Walcott-McQuigg, 1995), there were no relationships between stress and baseline body weight in our sample. Consistent with the body of literature on race/ethnicity and stress, there was a trend in the association between perceived stress and race/ethnicity (Geronimus et al., 2006; Schulz et al., 2000; Turner & Avison, 2003), with African American women reporting higher levels of mean stress compared to White women. Although race was related to weight change, with African American women losing less weight than White women, there were no relationships between race/ethnicity and baseline weight.
Some of our results may have differed from other studies that have been conducted because of the specialized nature of our sample, which consisted of an ethnically diverse group of overweight and obese US women with type 2 diabetes participating in a weight loss program. The restricted range in baseline body weight in the sample may have precluded cross-sectional relationships between baseline body weight and other variables. Higher stress levels have been reported among individuals with diabetes than are evident among non-diabetic individuals (Smith, 2004), which may have also complicated the intricate relationships between race/ethnicity and stress.
Future studies of stress, race/ethnicity, and body weight would benefit from using multidimensional measures of stress. Race/ethnicity may relate differently to various aspects of stress (perceived vs. objective, psychological vs. physiological, chronic/global vs. acute, accumulative, daily hassles), which may influence body weight and weight loss in myriad ways. There may have been more pronounced relationships between race, stress, and body weight in our sample if different aspects of stress were examined. Our study examined global perceived stress, and may not have captured situation-specific stressors related to the racism experienced by African Americans (Clark, Anderson, Clark, & Williams, 1999; Dressler, Oths, & Gravlee, 2005; Williams, 1999; Williams, Neighbors, & Jackson, 2003). In an African American sample of individuals with diabetes, 94% of participants reported experiencing racial discrimination at some time, with African American women reporting higher levels of stress due to discrimination compared to African American men (Wagner & Abbott, 2007). The African American women in our sample may have also had more active coping mechanisms to counter stress, resulting in less pronounced differences in mean stress levels compared to the white women in our sample, although a trend between race/ethnicity and stress existed. Thus, the unique stress African Americans experience, which may contribute to differential weight and weight loss, may not have been adequately assessed with the measures used (Davis et al., 2005; Kumanyika, 2002a, 2002b; Kumanyika & Morssink, 1997).
Limitations in our study include the sample of individuals with diabetes and the exclusive focus on women, both of which must temper broad generalizations. Despite these limitations, however, this study examines cross-sectional and longitudinal relationships between perceived stress and body weight in an ethnically diverse sample. To our knowledge, this is the first study to assess the relationship between stress and weight change in a US sample, in an ethnically diverse sample, and in a sample of women with type 2 diabetes. Although the magnitude of the weight loss is modest, the relationship between weight loss and perceived stress is significant and lends credence for future examinations of stress and successful weight loss outcomes.
Our study provides preliminary information that may serve to guide the design of future weight loss treatment programs. We found that individuals who are likely to drop out of a behavioral weight loss program tend to be more stressed than those who remain engaged. Furthermore, among women with type 2 diabetes, lower levels of perceived stress were associated with greater weight loss. With every 1 point decrease in perceived stress, women lost an additional 0.10 kg ± 0.04. Therefore, inclusion of a strong stress management component in behavioral weight loss programs might facilitate weight loss, at least among those individuals with elevated stress levels, and also may serve to retain women with diabetes who are likely to drop out. This role of stress and weight change may be specific to overweight and obese US women with type 2 diabetes. Future work in stress and weight change is needed to better understand the role of stress and stress management in weight loss interventions for the broader range of overweight individuals.
The relationships between stress, race, and weight change are intricate and in need of future delineation. Our results add to the scant existing literature by lending some understanding to these complex relationships, and contribute to the call for future research in this area. Future research contributing to the science of weight loss in diverse populations, and to the understanding of psychosocial factors in body weight and body weight management, would benefit from further examinations of stress, race, and body weight. Our hope is that through providing an initial step towards these efforts, the current study will provoke an increased interest in these important and interesting factors.
References
- Balfour L, Romano White D, Schiffrin A, Dougherty G, Dufresne J. Dietary disinhibition, perceived stress, and glucose control in young, type 1 diabetic women. Health Psychology. 1993;12(1):33–38. doi: 10.1037//0278-6133.12.1.33. [DOI] [PubMed] [Google Scholar]
- Bellisle F, Clement K, Le Barzic M, Le Gall A, Guy-Grand B, Basdevant A. The Eating Inventory and body adiposity from leanness to massive obesity: a study of 2509 adults. Obesity Research. 2004;12(12):2023–2030. doi: 10.1038/oby.2004.253. [DOI] [PubMed] [Google Scholar]
- Cerrelli F, Manini R, Forlani G, Baraldi L, Melchionda N, Marchesini G. Eating behavior affects quality of life in type 2 diabetes mellitus. Eating and Weight Disorders. 2005;10(4):251–257. doi: 10.1007/BF03327492. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. The American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Culhane JF, Rauh V, McCollum KF, Hogan VK, Agnew K, Wadhwa PD. Maternal stress is associated with bacterial vaginosis in human pregnancy. Maternal and child health journal. 2001;5(2):127–134. doi: 10.1023/a:1011305300690. [DOI] [PubMed] [Google Scholar]
- Davis EM, Clark JM, Carrese JA, Gary TL, Cooper LA. Racial and socioeconomic differences in the weight-loss experiences of obese women. American Journal of Public Health. 2005;95(9):1539–1543. doi: 10.2105/AJPH.2004.047050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioral correlates of baseline BMI in the diabetes prevention program (DPP) Diabetes Care. 2002;25(11):1992–1998. doi: 10.2337/diacare.25.11.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annual Review of Anthropology. 2005;34:231–252. [Google Scholar]
- Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. Journal of the American Medical Association. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. "Weathering" and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hainer V, Kunesova M, Bellisle F, Parizkova J, Braunerova R, Wagenknecht M, et al. The Eating Inventory, body adiposity and prevalence of diseases in a quota sample of Czech adults. International Journal of Obesity. 2006;30(5):830–836. doi: 10.1038/sj.ijo.0803202. [DOI] [PubMed] [Google Scholar]
- Harville EW, Savitz DA, Dole N, Thorp JM, Jr., Herring AH. Psychological and biological markers of stress and bacterial vaginosis in pregnant women. BJOG. 2007;114(2):216–223. doi: 10.1111/j.1471-0528.2006.01209.x. [DOI] [PubMed] [Google Scholar]
- Kelly S, Hertzman C, Daniels M. Searching for the biological pathways between stress and health. Annual Review of Public Health. 1997;18:437–462. doi: 10.1146/annurev.publhealth.18.1.437. [DOI] [PubMed] [Google Scholar]
- Kivimaki M, Head J, Ferrie JE, Shipley MJ, Brunner E, Vahtera J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. International Journal of Obesity. 2006;30(6):982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- Kumanyika S. The minority factor in the obesity epidemic. Ethnicity and Disease. 2002a;12(3):316–319. [PubMed] [Google Scholar]
- Kumanyika S. Obesity treatment in minorities. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. The Guilford Press; New York: 2002b. pp. 416–446. [Google Scholar]
- Kumanyika S. Obesity, health disparities, and prevention paradigms: hard questions and hard choices. Preventing Chronic Disease. 2005;2(4):A02. [PMC free article] [PubMed] [Google Scholar]
- Kumanyika S, Morssink CB. Cultural appropriateness of weight management programs. In: Dalton S, editor. Overweight and Weight Management: The Health Professional's Guide to Understanding and Practice. Aspen's Publisher's Inc.; Gaithersburg, MD: 1997. [Google Scholar]
- Kumanyika S, Wilson JF, Guilford-Davenport M. Weight-related attitudes and behaviors of black women. Journal of the American Dietetic Association. 1993;93(4):416–422. doi: 10.1016/0002-8223(93)92287-8. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Cohen JP. Environmental stress. In: Atlman I, Wohlwill JF, editors. Human behavior and environment. Vol. 2. Plenum; New York: 1977. [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators: central role of the brain. Dialogues in Clinical Neuroscience. 2006;8(4):367–381. doi: 10.31887/DCNS.2006.8.4/bmcewen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. Journal of the American Medical Association. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22(6):638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Sarlio-Lahteenkorva S, Rissanen A, Kaprio J. A descriptive study of weight loss maintenance: 6 and 15 year follow-up of initially overweight adults. International Journal of Obesity. 2000;24(1):116–125. doi: 10.1038/sj.ijo.0801094. [DOI] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Social Science and Medicine. 2000;51(11):1639–1653. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- Smith DW. The population perspective on quality of life among Americans with diabetes. Quality of Life Research. 2004;13(8):1391–1400. doi: 10.1023/B:QURE.0000040785.59444.7c. [DOI] [PubMed] [Google Scholar]
- Smith DW, McFall SL. The relationship of diet and exercise for weight control and the quality of life gap associated with diabetes. Journal of Psychosomatic Research. 2005;59(6):385–392. doi: 10.1016/j.jpsychores.2005.06.062. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44(4):488–505. [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Sarwer DB, Fabricatore AN, Crerand CE, Lipschutz PE, et al. Comparison of psychosocial status in treatment-seeking women with class III vs. class I-II obesity. Surgery for Obesity and Related Diseases. 2006;2(2):138–145. doi: 10.1016/j.soard.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Wagner J, Abbott G. Depression and depression care in diabetes: relationship to perceived discrimination in African Americans. Diabetes care. 2007;30(2):364–366. doi: 10.2337/dc06-1756. [DOI] [PubMed] [Google Scholar]
- Walcott-McQuigg JA. The relationship between stress and weight-control behavior in African-American women. Journal of the National Medical Association. 1995;87(6):427–432. [PMC free article] [PubMed] [Google Scholar]
- Wenzel L, Glanz K, Lerman C. Stress, Coping, and Health Behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. Jossey-Bass; San Francisco: 2002. pp. 210–239. [Google Scholar]
- West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30:1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity Research. 2004;12(9):1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]