Abstract
Purpose
Network meta-analysis (NMA) is a comparatively new evidence-based technique in medical disciplines which compares the relative benefits associated with multiple interventions and obtains hierarchies of these interventions for various treatment options. We evaluated the effectiveness and safety of open reduction and internal fixation (ORIF), hemiarthroplasty (HA), reverse shoulder arthroplasty (RSA), intramedullary nailing (IN) and non-operative treatment (NOT) of displaced proximal humeral fractures in adults using Bayesian NMA of data from clinical trials.
Method
PUBMED, EMBASE and CENTRAL in July 2016 were searched and clinical trials that evaluated interventions for treating adults with displaced proximal humeral fractures were identified. Methodological qualities of studies were assessed by the Newcastle—Ottawa Scale and risk of bias using the Cochrane Collaboration tool.
Result
Thirty-four trials involving 2165 participants were included in the study. RSA had significantly the highest Constant score and lower total incidence of complications than ORIF, HA and IN. Moreover, RSA resulted in a lower incidence of additional surgery than ORIF and IN. The rank of treatments in terms high Constant score was: RSA, ORIF, IN, NOT and HA. The rank for reduction in total incidence of complications was: RSA, NOT, HA, IN and ORIF. For lowering the risk of additional surgery, the rank was: RSA, NOT, HA, IN and ORIF.
Conclusion
RSA had the highest probability for improving functional outcome and reduction in the total incidence of complications and requiring additional surgery among the five interventions for treating adults with displaced proximal humeral fracture.
Introduction
Fractures of the proximal humerus are the third most common in elderly patients after those of the hip and distal radius [1], accounting for 5% to 6% of all adult fractures [2]. Their incidence rapidly increases with age, and women are affected between two and three times as often as men [2–4]. Both non-operative and operative methods are used to treat these fractures. Non-operative treatment (NOT) involves a period of immobilization, such as an arm sling, followed by physiotherapy and exercise. It is generally the accepted treatment option for minimally displaced fractures and often used also for people with displaced fractures [3]. Operative treatment is recommended for displaced and unstable fractures and those with more complex fracture patterns to avoid painful and dysfunctional malunion [5]. The common operative treatments include open reduction and internal fixation (ORIF), hemiarthroplasty (HA), reverse shoulder arthroplasty (RSA), intramedullary nailing (IN). The debate among surgeons regarding which treatment should be used is still unresolved today and has been since the 1980s. Previous pairwise meta-analyses [3, 5–8] could not obtain hierarchies of these treatments because some had not been compared one by one.
We compared the effectiveness and safety of these five treatments (NOT, ORIF, HA, RSA, IN) for displaced proximal humeral fracture in adults by network meta-analysis (NMA). Our intention was to provide hierarchies of the comparative Constant score, total incidence of complications and need for additional surgery.
NMA is a powerful technique that has been used for more than a decade to rank treatment options with both direct comparisons of treatments in randomized controlled trials and indirect comparisons across trials with a common comparator. We ensured validity through careful review design and rigorous analysis of criteria for inclusion of the various studies.
Methods
Eligibility criteria and literature search
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [9]. We searched the Cochrane Register of Controlled Trials (CENTRAL, Jul 2016), PubMed (Jan 1980 to Jul 2016), and EMBASE (1980 to Jul 2016) databases to identify all studies that discussed the effectiveness and safety of NOT, ORIF, HA, RSA, IN. Keywords and MeSH terms used in the search strategy included “proximal humeral fracture”, “non-operative treatment”, “open reduction and internal fixation”, “hemiarthroplasty”, “reverse shoulder arthroplasty” and “intramedullary nailing”.
The inclusion criteria were: (1) target population: patient was aged 16 years or older and presented within 3 weeks after sustaining a displaced fracture of the proximal humerus; (2) intervention: NOT, ORIF, HA, RSA, IN; (3) methodological criteria: randomized controlled trials and clinical trials. The exclusion criteria were: (1) target population: patient was aged under 16 years or presented more than 3 weeks after sustaining a displaced proximal humeral fracture; (2) methodological criteria: case reports and cohort studies. The study selection was conducted by two independent reviewers. Any disagreement between review authors was resolved by discussion.
Outcome assessment
The primary outcome measure was Constant score [10] (activity, mobility, strength and pain). The secondary outcome measures included total complications (e.g. surgical site infection, symptomatic malunion, transient paresthesia and avascular necrosis of the humeral head) and incidence of additional surgery.
Data extraction and quality assessments
Study type, country, sample size, length of follow-up and interventions data were gathered from each trial. Data on random sequence generation, allocation concealment, blinding, selective reporting and incomplete outcome data were gathered from randomized controlled trials. Data on representativeness of cases, selection of controls, definition of controls, comparability of cases and controls, ascertainment of exposure, equivalent methods of diagnosis and determination of response rate for cases and controls were gathered from controlled clinical trials. In addition, the following clinical data were extracted if available: Constant score, total number of complications and incidence of additional surgery.
The Cochrane Collaboration tool for assessing risk of bias [11] was used to assess the quality of randomized controlled trials, and the Newcastle—Ottawa Scale [12] was used to assess the quality of case—control trials in terms of selection and comparability of the study groups and determination of outcomes. In evaluating randomized controlled trials by the Cochrane Collaboration tool, quality of the studies was assessed using the following criteria: (1) randomization sequence generation: assessment for selection bias; (2) allocation concealment: assessment of selection bias; (3) level of blinding (blinding of participants and blinding of outcome assessment): assessment for performance bias and detection bias; (4) incomplete outcome data: assessment for attrition bias; and (5) selective reporting: assessment for reporting bias [11]. For case—control studies, the total Newcastle—Ottawa Scale score was calculated with a maximum of nine points using the criteria listed in S1 Table [12].
Data synthesis and analysis
Two researchers extracted data independently according to the prespecified selection criteria. Disagreements were resolved by discussion. In each study, the relative risk (RR) was calculated for dichotomous outcomes (e.g. total complications and incidence of additional surgery), and treatment effects for continuous outcomes (e.g. Constant score) including mean differences (MDs) for studies with comparable outcome measures used a 95% confidence interval (CI).
We performed conventional pairwise meta- analyses for all outcomes and comparisons, using a random effects model by STATA (version 12.0, Stata Corp, College Station, TX). The pooled estimates of RRs or standardized MDs and 95% CI of three outcomes (Constant score, total incidence of complication and additional surgery) were shown. NMA combines direct and indirect evidence within a Bayesian framework and was implemented using WinBUGS statistical software (version 1.4.3) using Markov Chain Monte Carlo (MCMC) methods. The models, codes and software used in this study are available free online [13]. We performed surface under the cumulative ranking curve (SUCRA) probabilities to rank the five interventions for treating displaced proximal humeral fractures [14]. SUCRA is a proportion, expressed as a percentage of the efficacy of an intervention on the outcome that would be ranked first without uncertainty, and so equals 100% when the treatment is certain to be the best and 0% when certain to be the worst [14].
Inconsistencies of this NMA were assessed by the Higgins model. Significance levels smaller than 0.05 were interpreted as evidence of inconsistency. The sensitivity analysis was performed by comparing the results of different effects models (random effects and fixed effects model).
Results
Study selection
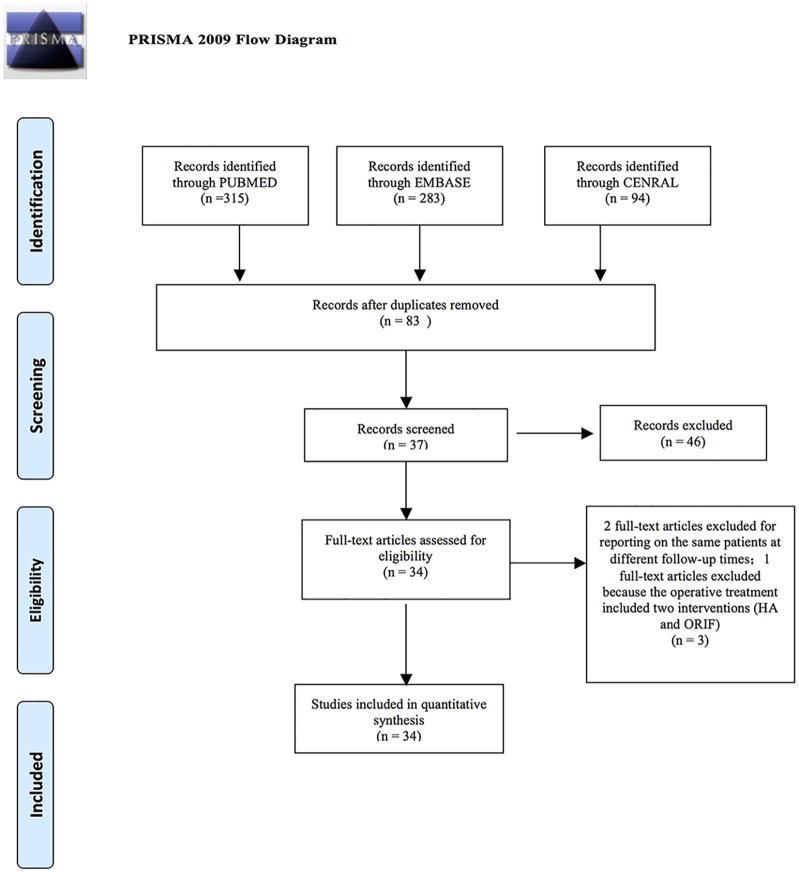
Fig 1 shows the study selection process according to the PRISMA statement. This search strategy retrieved a total of 692 studies: 94 studies were from CENTRAL, 315 studies from PUBMED and 283 studies from EMBASE. Titles and abstracts of these references were examined by two reviewers, and 34 studies [15–48] were identified for further analysis. One study [49] was excluded because the operative treatment included two interventions (HA and ORIF). We also found that Fjalestad (2010) [50], Fjalestad (2012) [51] and Fjalestad (2014) [24] reported on the same patients at different follow-up times, so we included only one article of the multiple studies. Ten randomized controlled trials and twenty four controlled clinical trials remained and were considered for primary relevant studies, which were all included in this NMA.
Fig 1. Flow chart of selection of studies for inclusion in meta- analysis.
From: Moher D, Liberati A, TetZlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi: 10.1371/journal.pmed1000097 For more information, visit www.prisma-statement.org.
Study characteristics and risk of bias in studies included in the review
Table 1 provides a summary of the studies in the review. A total of 2165 participants (mean age: 69 years) were included. For each intervention, 748 patients (mean age: 66.06 years) were assigned to ORIF therapy, 803 (mean age: 71.3 years) to HA therapy, 191 (mean age: 77.3 years) to RSA therapy, 267 (mean age: 61.8 years) to IN therapy and 153 (mean age: 73.9 years) to NOT therapy. Study sample size ranged from 18 to 368. All 34 studies directly compared one treatment with another. These studies were published between 1984 and 2014. Twenty four studies reported Constant score as an outcome. Thirty one studies used total complications as an outcome and twenty studies reported incidence of additional surgery as an outcome.
Table 1. Characteristics of Included Studies Comparing Different treatments for displaced proximal humeral fracture.
| Study | Country | Interventions | Sample size (mean age: y) | Follow-up (month) | Study design | For analysis |
|---|---|---|---|---|---|---|
| Dietrich 2008 | Germany | ORIF vs HA | 52(82)/59(80) | 12 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Bastian 2009 | Switzerland | ORIF vs HA | 44(60)/33(60) | 60 | PC | Constant score; Total complications; Incidence of additional surgeries |
| Solberg 2009 | USA | ORIF vs HA | 38(66.5)/48(67.4) | 36 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Wang 2009 | China | ORIF vs HA | 12(49)/10(49) | 20 | RC | Constant score; Total complications |
| Zhang 2010 | China | ORIF vs HA | 28(66.5)/30(68.9) | 28 | RC | Constant score; Total complications |
| Kim 2011 | Korea | ORIF vs HA | 38(64.9)/26(64.9) | 24 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Wild 2011 | USA | ORIF vs HA | 42(56.9)/15(66.4) | 35 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Spross 2011 | Switzerland | ORIF vs HA | 22(75)/22(76) | 30 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Cai 2012 | China | ORIF vs HA | 13(72)/19(72) | 24 | RCT | Constant score |
| Lu 2012 | China | ORIF vs HA | 26(67)/22(67) | 6 | RC | Constant score; Total complications |
| Gallinet 2009 | France | HA vs RSA | 17(74)/16(74) | 14.5 | RC | Constant score; Total complications |
| Young 2010 | New Zealand | HA vs RSA | 10(75.5)/10(77.2) | 33 | RC | Total complications |
| Garrigues 2012 | USA | HA vs RSA | 9(69.3)/10(80.5) | 43.2 | RC | Total complications |
| Boyle 2013 | New Zealand | HA vs RSA | 313(71.9)/55(79.6) | 12 | RC | Incidence of additional surgeries |
| Cuff 2013 | USA | HA vs RSA | 23(74.4)/24(74.4) | 24 | PC | Total complications; Incidence of additional surgeries |
| Fu 2013 | China | HA vs RSA | 12(69.5)/11(81.2) | 43.2 | RC | Total complications |
| Baudi 2014 | Italy | HA vs RSA | 28(71.4)/25(77.3) | 27.5 | RC | Constant score; Total complications |
| Chalmers 2014 | USA | HA vs RSA | 9(72)/9(77) | 12 | RC | Total complications |
| Sebastia-Forcada 2014 | Spain | HA vs RSA | 30(73.3)/31(74.7) | 28.5 | RCT | Constant score; Total complications; Incidence of additional surgeries |
| Gradl 2009 | Germany | ORIF vs IN | 76(63)/76(62) | 12 | PC | Constant score; Total complications; Incidence of additional surgeries |
| Matziolis 2010 | Germany | ORIF vs IN | 11(54.8)/11(55.6) | 36 | RC | Constant score; Total complications; Incidence of additional surgeries |
| Smejkal 2011 | Chech | ORIF vs IN | 28(61)/27(61) | 2–18 | RCT | Constant score; Total complications |
| Trepat 2011 | Spain | ORIF vs IN | 14(68.3)/15(64.5) | 6–12 | RC | Total complications; Incidence of additional surgeries |
| Zhu 2011 | China | ORIF vs IN | 26(50.5)/25(54.8) | 12–36 | RCT | Constant score; Total complications; Incidence of additional surgeries |
| Lekic 2012 | USA | ORIF vs IN | 12(59)/11(60) | 3–46 | RC | Total complications; Incidence of additional surgeries |
| Konrad 2012 | Switzerland | ORIF vs IN | 153(65.4)/58(64.8) | 3–12 | PC | Constant score; Total complications; Incidence of additional surgeries |
| Von 2014 | Germany | ORIF vs IN | 28(61)/44(61) | 38–82 | RC | Total complications; Incidence of additional surgeries |
| Zyto 1997 | Sweden | ORIF vs NOT | 20(73)/20(75) | 36–60 | RCT | Constant score; Total complications |
| Olerud 2011a | Sweden | ORIF vs NOT | 30(74)/30(74) | 24 | RCT | Constant score; Total complications; Incidence of additional surgeries |
| Kollig 2003 | Germany | ORIF vs NOT | 13(52.5)/ 9(52.7) | 74–82 | PC | Constant score |
| Fjalestad 2014 | Norway | ORIF vs NOT | 25(72.2)/25(73.1) | 24 | RCT | Constant score; Total complications; Incidence of additional surgeries |
| Stableforth 1984 | England | HA vs NOT | 16(65.6)/16(70.1) | 6–48 | RCT | Total complications |
| Olerud 2011b | Sweden | HA vs NOT | 27(75.8)/28(77.5) | 24 | RCT | Constant score; Total complications; Incidence of additional surgeries |
| Boons 2012 | Netherlands | HA vs NOT | 25(76.4)/25(79.9) | 24 | RCT | Constant score; Total complications; Incidence of additional surgeries |
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment; RC: Retrospective comparative; PC: Prospective comparative; RCT: Randomised controlled trial; y: years.
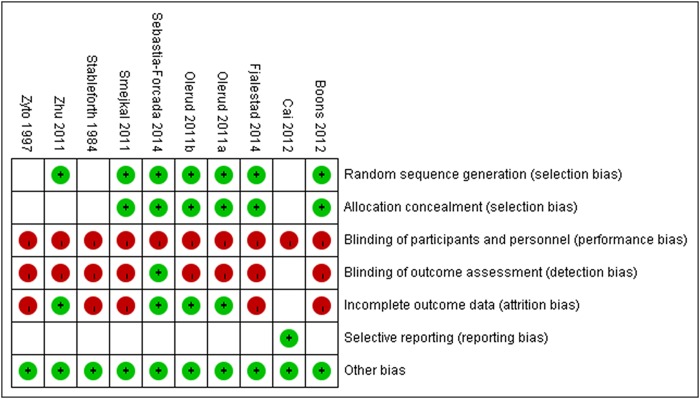
Of the ten randomized controlled trials analyzed [17, 19, 24, 34–37, 40, 47, 48], the Cochrane Collaboration tool indicated that seven trials [17, 24, 34–37, 47] used adequate randomization and six trials [17, 24, 34–37] used adequate allocation concealment. One study [36] reported outcome assessment blinding and also one study [19] was free of selective reporting. Four trials [23, 34–36, 47] mentioned incomplete outcome data reporting (Fig 2). As assessed by the Newcastle—Ottawa Scale, six case—control studies [21, 22, 27, 30, 38, 39] were awarded a score of nine points, eleven studies [15, 16, 20, 25, 28, 29, 31, 41, 42, 45, 46] received a score of eight points, six studies [18, 23, 26, 33, 43, 44] received a score of seven points, and only one study [32] received a score of six points (Table 2).
Fig 2. Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Table 2. Quality assessment of case—control studies comparing different treatments for displaced proximal humeral fracture using Newcastle—Ottawa Scale.
| Author group | Selection | Comparability | Exposure | |||||
|---|---|---|---|---|---|---|---|---|
| Adequat-e case definitio-n | Representativeness of the cases | Selectio-n of Control-s | Definitio-n of Controls | Comparability of cases and controls | Ascertainm-ent of exposure | Same method of ascertainmen-t | Non Response rate | |
| Bastian 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Baudi 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Boyle 2013 | 1 | 1 | 1 | 1 | - | 1 | 1 | 1 |
| Chalmers 2014 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Cuff 2013 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Dietrich 2008 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| Fu 2013 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Gallinet 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Garrigues 2012 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| Gradl 2009 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Kim 2011 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Kollig 2003 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Konrad 2012 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Lekic 2012 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Lu 2012 | 1 | 1 | 1 | 1 | - | 1 | 1 | - |
| Matziolis 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| Solberg 2009 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Spross 2011 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 |
| Trepat 2011 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Von 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Wang 2009 | 1 | 1 | 1 | 1 | - | 1 | 1 | 1 |
| Wild 2011 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| Young 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Zhang 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
Constant score
For the primary outcome, 24 trials were included in the NMA. The following interventions for treating displaced proximal humeral fracture were tested in the trials: ORIF versus HA (10 trials with 533 patients) [15, 19, 23, 28, 32, 38, 39, 43, 44, 46]; HA versus RSA (3 trials with 147 patients) [16, 25, 36]; HA versus NOT (2 trials with 96 patients) [17, 34]; ORIF versus IN (5 trials with 491 patients) [27, 30, 33, 37, 47]; ORIF versus NOT (4 trials with 152 patients) [24, 29, 35, 48].
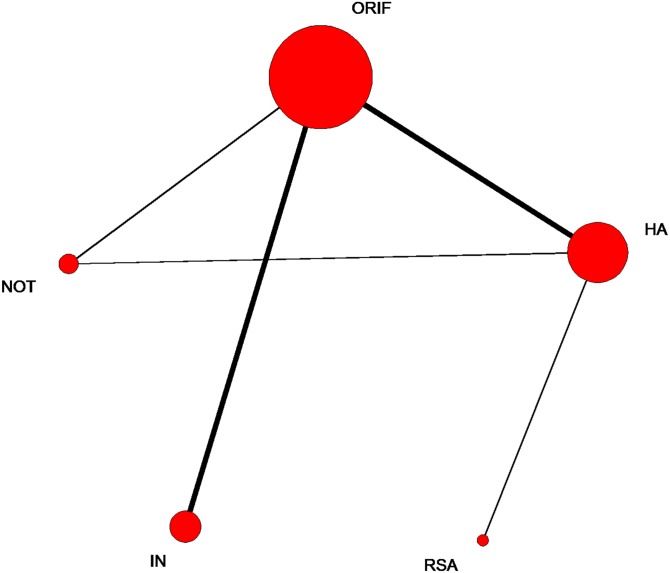
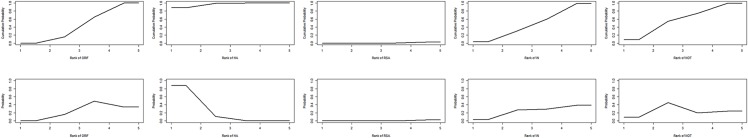
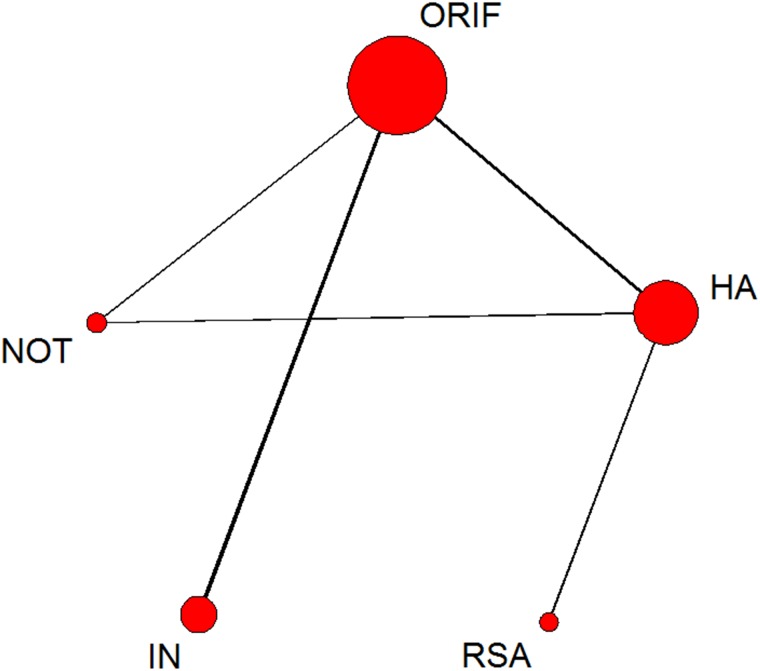
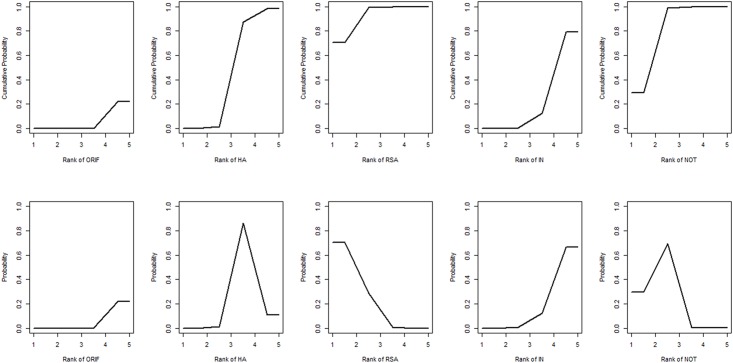
The network of comparisons on Constant score is shown in Fig 3. Table 3 provides hierarchies of effect size on Constant score. Ranking graphs of the distribution of probabilities of Constant score are displayed in Fig 4. The direct and indirect comparisons indicated that HA significantly decreased the Constant score compared with the other groups and RSA was responsible for a significantly higher Constant score compared with the other groups. Based on SUCRA, HA ranked first (0.9675), the second was NOT (0.5905), IN was third (0.4805), the fourth was ORIF (0.4520) with RSA being last (0.0095).
Fig 3. Network of treatment comparisons for constant score.
The size of the node corresponds to the total sample size of treatments. Directly comparable treatments are linked with a line, the thickness of which represents the number of trials that were compared. ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Table 3. Results for constant score, from network meta-analysis (lower diagonal part) and pairwise meta-analysis (upper diagonal part).
| ORIF | 6.90(1.77–12.04) | NA | -0.175(-3.11–2.76) | -1.45(-7.12–4.22) |
| 5.48(2.15–8.66) | HA | -14.68(-19.14–10.22) | NA | 1.56(-5.48–8.60) |
| -9.15(-16.61–1.6) | -14.63(-21.26–8.11) | RSA | NA | NA |
| 0.04(-5.17–5.17) | -5.44(-11.68–0.52) | 9.19(0.44–18.13) | IN | NA |
| 1.29(-4.45–7.08) | -4.19(-10.15–1.88) | 10.44(1.82–19.49) | 1.25(-6.16–9.68) | NOT |
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment
Fig 4. Ranking of treatment strategies based on the probability of their effects on the outcome of constant score.
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Total incidence of complications
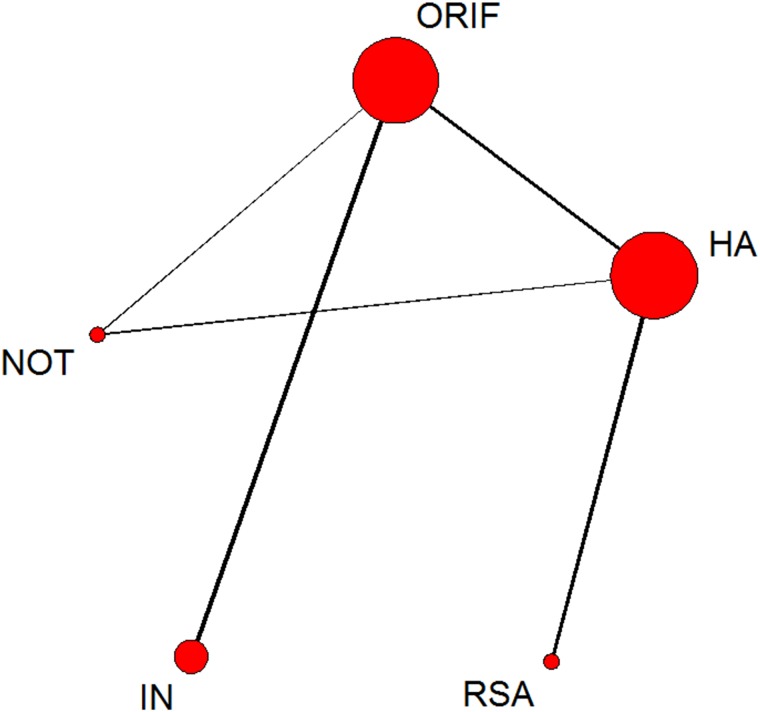
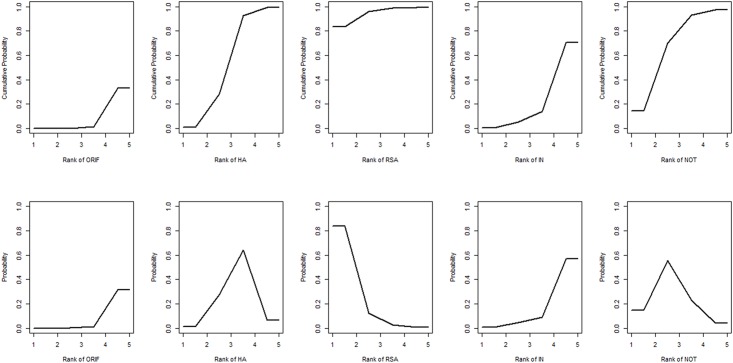
For this outcome, 31 trials were included in the NMA. The network of comparisons on total incidence of complications is shown in Fig 5. Table 4 provides hierarchies of effect size on their incidence. The ranking graphs of distribution of probabilities of incidence can be seen in Fig 6. Direct and indirect comparisons indicate that RSA results in a lower incidence of complications than ORIF, HA and IN. Based on SUCRA, RSA ranked first (0.9248), second was NOT (0.8198), HA was third (0.4678), the fourth was IN (0.2318) with ORIF last (0.0560).
Fig 5. Network of treatment comparisons for incidence of total complications.
The size of the node corresponds to the total sample size of treatments. Directly comparable treatments are linked with a line, the thickness of which represents the number of trials that were compared. ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Table 4. Results for total complications, from network meta-analysis (lower diagonal part) and pairwise meta-analysis (upper diagonal part).
| ORIF | 1.35(0.95–1.92) | NA | 1.08(0.76–1.53) | 1.97(0.43–9.08) |
| 1.95(1.08–3.16) | HA | 2.35(1.18–4.67) | NA | 1.52(0.86–2.70) |
| 7.61(2.46–18.9) | 3.93(1.44–8.8) | RSA | NA | NA |
| 1.27(0.69–2.1) | 0.7(0.31–1.38) | 0.22(0.05–0.6) | IN | NA |
| 5.18(2.1–10.22) | 2.73(1.2–5.45) | 0.86(0.23–2.5) | 4.36(1.5–9.66) | NOT |
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment
Fig 6. Ranking of treatment strategies based on the probability of their effects on the outcome of incidence of total complications.
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Incidence of additional surgery
For this outcome, 20 trials were included in the NMA. The network of comparisons on incidence of additional surgery is shown in Fig 7. Table 5 provides the hierarchies of effect size on incidence of additional surgery, with ranking graphs of the distribution of probabilities on incidence of additional surgery in Fig 8. Only indirect comparison indicates that RSA results in a lower incidence of additional surgery than ORIF and IN. Both direct and indirect comparisons suggest that HA results in a lower incidence of additional surgery than ORIF. Based on SUCRA, RSA ranks first (0.9450), NOT second (0.6870), the third was HA (0.5538), the fourth was IN (0.2272) with ORIF last (0.0870).
Fig 7. Network of treatment comparisons for incidence of additional surgery.
The size of the node corresponds to the total sample size of treatments. Directly comparable treatments are linked with a line, the thickness of which represents the number of trials that were compared. ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Table 5. Results for incidence of additional surgery, from network meta-analysis (lower diagonal part) and pairwise meta-analysis (upper diagonal part).
| ORIF | 2.15(1.14–6.13) | NA | 0.98(0.56–1.69) | 3.64(0.42–31.33) |
| 6.14(1.18–24.74) | HA | 2.89(0.62–13.44) | NA | 1.98(0.36–10.97) |
| 132.29(2.01–894.98) | 19.22(0.75–119.46) | RSA | NA | NA |
| 1.93(0.37–6.23) | 0.5(0.04–2.08) | 0.2(0–0.84) | IN | NA |
| 13.91(0.81–65.2) | 2.94(0.18–14.2) | 0.98(0.01–5.45) | 16.78(0.32–71.31) | NOT |
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment
Fig 8. Ranking of treatment strategies based on the probability of their effects on the outcome of incidence of additional surgery.
ORIF: open reduction and internal fixation; HA: hemiarthroplasty; RSA: reverse shoulder arthroplasty; IN: intramedullary nailing; NOT: Non-operative treatment.
Inconsistency and sensitivity analysis
In general, the results obtained from the pairwise meta-analysis closely matched those of the NMA and no inconsistencies were identified in the NMA when using the Higgins model (Chi squared = 1.74, P = 0.1871 > 0.05). The sensitivity analysis was performed by comparing the results of different effects models (random effects and fixed effects models). The results of the random effects model (effective number of parameters [pD] = 38.7 and deviance information criterion [DIC] = 278.9) were similar to the fixed-effect model (pD = 28.1 and DIC = 322.9).
Discussion
The NMA provided hierarchies for the Constant score, incidence of total complications and additional surgery in adult with displaced proximal humeral fracture treated with different methods, which had advantages over comparison with traditional pairwise meta-analyses [3, 5–8]. The meta-analysis indicated that: (1) HA significantly decreased Constant score compared with the other groups and RSA resulted in significantly higher Constant score compared with the other groups; (2) RSA resulted in a lower incidence of complications than ORIF, HA and IN; (3) RSA caused a lower incidence of additional surgery than ORIF and IN. (4) The rank of treatments in terms of Constant score was: RSA, ORIF, IN, NOT and HA; (5) For reduction in total incidence of complications, the rank of treatments was: RSA, NOT, HA, IN and ORIF; (6) The rank of treatments for lowering risk of additional surgery was: RSA, NOT, HA, IN and ORIF. RSA group included patients with higher mean age (77.3 years) and IN group included patients with lower mean age (61.8 years) than other treatments. A total of 2165 participants with the mean age of 69 years were included in this network meta-analysis. So the findings were suitable for the patients with mean age of more than 60 years.
There are some particular strengths to the analysis in this NMA: (1) It was conducted using common methods and was designed to allow for reproducible research selection and inclusion; (2) a broad and extensive search strategy was used to minimize the possibility of publication bias; (3) the study overcomes a major limitation of conventional pairwise meta-analysis by combining direct and indirect evidence of the efficacy of treatment strategies; (4) the SUCRA and posterior probabilities of outcomes were used to distinguish the subtle differences among five treatments.
However, this analysis has several limitations. Firstly, randomized controlled trials and case—control studies were both included in the analysis, and the case—control studies may have reduced the significance of the conclusions. Secondly, the lack of any treatment-provider blinded studies may have introduced detection bias, in which the assessors are likely to have preferentially attributed the occurrence of injury to the control group. Thirdly, some of the study characteristics such as type of fracture, age and performance bias might be potential obstacles to the outcomes of our study. Finally, these interventions (NOT, ORIF, HA, RSA and IN) may have different indications, so the comparisons between treatments within trials and sample for each trial may have interacted in ways that this analysis would not reveal. However, our network meta-analysis can still provide useful information about effectiveness and safety of interventions for treating adults with displaced proximal humeral fracture to the surgeons.
Xie [52] previously reported that operative treatments (including ORIF and HA) did not significantly improve Constant score and led to a higher incidence of postoperative complications compared with NOT. Li [6] also indicated that ORIF did not improve the Constant score when compared with NOT. Dai [5] showed that ORIF resulted in better Constant score than HA, and HA could reduce the rate of revisions and the method-related complications significantly. Wang [7] stated that treatment with ORIF caused no significant difference in Constant score and total number of complications compared with IN. Compared with HA, Shukla [53] reported that RSA resulted in more favorable Constant scores and Zhang [8] demonstrated that RSA was associated with a lower rate of total complications. Our network analysis showed that RSA resulted in significantly higher Constant score compared with the other four interventions. We also found that RSA resulted in lower total incidence of complications than ORIF, HA and IN. RSA also resulted in a lower incidence of additional surgery than ORIF and IN. However, we also use the SUCRA and posterior probabilities of outcomes to distinguish the subtle differences among five treatments. For achieving higher Constant scores the rank on treatments was: RSA, ORIF, IN, NOT and HA. For reducing incidence of total complications, the rank on treatments was: RSA, NOT, HA, IN and ORIF. For lowering risk of additional surgery, the rank on treatments was: RSA, NOT, HA, IN and ORIF.
Conclusions
In summary, this Bayesian NMA of data from clinical trials demonstrated that RSA has the highest probability of improving the functional outcome and reducing the total incidence of complications and additional surgery among the five interventions for treating adults with displaced proximal humeral fracture.
Supporting Information
(DOCX)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Barrett JA, Baron JA, Karagas MR, Beach ML. Fracture risk in the U.S. Medicare population. Journal of clinical epidemiology. 1999;52(3):243–9. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37(8):691–7. 10.1016/j.injury.2006.04.130 [DOI] [PubMed] [Google Scholar]
- 3.Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. The Cochrane database of systematic reviews. 2015(11):Cd000434 10.1002/14651858.CD000434.pub4 [DOI] [PubMed] [Google Scholar]
- 4.Lind T, Kroner K, Jensen J. The epidemiology of fractures of the proximal humerus. Archives of orthopaedic and trauma surgery. 1989;108(5):285–7. [DOI] [PubMed] [Google Scholar]
- 5.Dai J, Chai Y, Wang C, Wen G. Meta-analysis comparing locking plate fixation with hemiarthroplasty for complex proximal humeral fractures. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2014;24(3):305–13. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Zhao L, Zhu L, Li J, Chen A. Internal fixation versus nonoperative treatment for displaced 3-part or 4-part proximal humeral fractures in elderly patients: a meta-analysis of randomized controlled trials. PloS one. 2013;8(9):e75464 10.1371/journal.pone.0075464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang G, Mao Z, Zhang L, Zhang L, Zhao Y, Yin P, et al. Meta-analysis of locking plate versus intramedullary nail for treatment of proximal humeral fractures. Journal of orthopaedic surgery and research. 2015;10:122 10.1186/s13018-015-0242-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Zhu Y, Zhang F, Chen W, Tian Y, Zhang Y. Meta-analysis suggests that reverse shoulder arthroplasty in proximal humerus fractures is a better option than hemiarthroplasty in the elderly. International orthopaedics. 2016;40(3):531–9. 10.1007/s00264-015-2811-x [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England). 2010;8(5):336–41. [DOI] [PubMed] [Google Scholar]
- 10.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical orthopaedics and related research. 1987(214):160–4. [PubMed] [Google Scholar]
- 11.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011; http://www.cochrane-handbook.org/.
- 12.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available: http://wwwohrica/programs/clinical_epidemiology/oxfordhtm.
- 13.Salanti G, Mavridis D, Nikolakopoulou A, Gianiatsi M. Multiple-treatments meta-analysis of a network of interventions. Available: http://wwwmtmuoigr/indexphp/how-to-do-an-mtm. 2015.
- 14.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. Journal of clinical epidemiology. 2011;64(2):163–71. 10.1016/j.jclinepi.2010.03.016 [DOI] [PubMed] [Google Scholar]
- 15.Bastian JD, Hertel R. Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: outcomes in a consecutive case series. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2009;18(2):216–9. [DOI] [PubMed] [Google Scholar]
- 16.Baudi P, Campochiaro G, Serafini F, Gazzotti G, Matino G, Rovesta C, et al. Hemiarthroplasty versus reverse shoulder arthroplasty: comparative study of functional and radiological outcomes in the treatment of acute proximal humerus fracture. Musculoskeletal surgery. 2014;98 Suppl 1:19–25. [DOI] [PubMed] [Google Scholar]
- 17.Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clinical orthopaedics and related research. 2012;470(12):3483–91. 10.1007/s11999-012-2531-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyle MJ, Youn SM, Frampton CM, Ball CM. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2013;22(1):32–7. [DOI] [PubMed] [Google Scholar]
- 19.Cai M, Tao K, Yang C, Li S. Internal fixation versus shoulder hemiarthroplasty for displaced 4-part proximal humeral fractures in elderly patients. Orthopedics. 2012;35(9):e1340–6. 10.3928/01477447-20120822-19 [DOI] [PubMed] [Google Scholar]
- 20.Cd F. Hemiarthroplasty versus total shoulder arthroplasty for acute proximal humerus fractures in elderly patients: a mid-term follow up study. HaiNan Med J 2013(24):1910–3. [Google Scholar]
- 21.Chalmers PN, Slikker W III, Mall NA, Gupta AK, Rahman Z, Enriquez D, et al. Reverse total shoulder arthroplasty for acute proximal humeral fracture: comparison to open reduction-internal fixation and hemiarthroplasty. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2014;23(2):197–204. [DOI] [PubMed] [Google Scholar]
- 22.Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. The Journal of bone and joint surgery American volume. 2013;95(22):2050–5. 10.2106/JBJS.L.01637 [DOI] [PubMed] [Google Scholar]
- 23.Dietrich M, Meier C, Lattmann T, Zingg U, Gruninger P, Platz A. Complex fracture of the proximal humerus in the elderly. Locking plate osteosynthesis vs hemiarthroplasty. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 2008;79(3):231–40. [DOI] [PubMed] [Google Scholar]
- 24.Fjalestad T, Hole MO. Displaced proximal humeral fractures: operative versus non-operative treatment—a 2-year extension of a randomized controlled trial. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2014;24(7):1067–73. [DOI] [PubMed] [Google Scholar]
- 25.Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthopaedics & traumatology, surgery & research: OTSR. 2009;95(1):48–55. [DOI] [PubMed] [Google Scholar]
- 26.Garrigues GE, Johnston PS, Pepe MD, Tucker BS, Ramsey ML, Austin LS. Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics. 2012;35(5):e703–8. 10.3928/01477447-20120426-25 [DOI] [PubMed] [Google Scholar]
- 27.Gradl G, Dietze A, Kaab M, Hopfenmuller W, Mittlmeier T. Is locking nailing of humeral head fractures superior to locking plate fixation? Clinical orthopaedics and related research. 2009;467(11):2986–93. 10.1007/s11999-009-0916-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim DS, Lee DK, Yi CH, Park JH, Rah JH. Comparison of results between internal plate fixation and hemiarthroplasty in comminuted proximal humerus fracture. J Korean Fract Soc. 2011;24(2):144–50. [Google Scholar]
- 29.Kollig E, Kutscha-Lissberg F, Roetman B, Dielenschneider D, Muhr G. [Complex fractures of the humeral head: which long-term results can be expected?]. Zentralblatt fur Chirurgie. 2003;128(2):111–8. 10.1055/s-2003-37764 [DOI] [PubMed] [Google Scholar]
- 30.Konrad G, Audige L, Lambert S, Hertel R, Sudkamp NP. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clinical orthopaedics and related research. 2012;470(2):602–9. 10.1007/s11999-011-2056-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lekic N, Montero NM, Takemoto RC, Davidovitch RI, Egol KA. Treatment of two-part proximal humerus fractures: intramedullary nail compared to locked plating. HSS journal: the musculoskeletal journal of Hospital for Special Surgery. 2012;8(2):86–91. 10.1007/s11420-012-9274-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu J, Zhou TM. Comparative research of the outcomes after two different methods for treatment of four-part proximal humerus fractures. J Pract Orthop. 2012;18(2):115–7. [Google Scholar]
- 33.Matziolis D, Kaeaeb M, Zandi SS, Perka C, Greiner S. Surgical treatment of two-part fractures of the proximal humerus: comparison of fixed-angle plate osteosynthesis and Zifko nails. Injury. 2010;41(10):1041–46. 10.1016/j.injury.2010.04.017 [DOI] [PubMed] [Google Scholar]
- 34.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2011;20(7):1025–33. [DOI] [PubMed] [Google Scholar]
- 35.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2011;20(5):747–55. [DOI] [PubMed] [Google Scholar]
- 36.Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A, Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2014;23(10):1419–26. [DOI] [PubMed] [Google Scholar]
- 37.Smejkal K, Lochman P, Dedek T, Trlica J, Koci J, Zvak I. Surgical treatment for proximal humerus fracture. Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2011;78(4):321–7. [PubMed] [Google Scholar]
- 38.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. The Journal of bone and joint surgery American volume. 2009;91(7):1689–97. 10.2106/JBJS.H.00133 [DOI] [PubMed] [Google Scholar]
- 39.Spross C, Platz A, Erschbamer M, Lattmann T, Dietrich M. Surgical treatment of Neer Group VI proximal humeral fractures: retrospective comparison of PHILOS(R) and hemiarthroplasty. Clinical orthopaedics and related research. 2012;470(7):2035–42. 10.1007/s11999-011-2207-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stableforth PG. Four-part fractures of the neck of the humerus. The Journal of bone and joint surgery British volume. 1984;66(1):104–8. [DOI] [PubMed] [Google Scholar]
- 41.Trepat AD, Popescu D, Fernández-Valencia JA, Cuñé J, Rios M, Prat S. Comparative study between locking plates versus proximal humeral nail for the treatment of 2-part proximal humeral fractures. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2011;400(22):373–9. [Google Scholar]
- 42.von Ruden C, Trapp O, Hierholzer C, Prohaska S, Wurm S, Buhren V. [Intramedullary nailing vs. locking plate osteosynthesis in proximal humeral fractures: Long-term outcome]. Der Unfallchirurg. 2015;118(8):686–92. [DOI] [PubMed] [Google Scholar]
- 43.Wang DL, Ruan DK, Yin Q, Li HF, Wang PJ. Surgical treatment for complicated proximal humeral fractures and analysis of efficacy. Chin J Bone Joint Injury. 2009;24(11):985–7. [Google Scholar]
- 44.Wild JR, DeMers A, French R, Shipps MR, Bergin PF, Musapatika D, et al. Functional outcomes for surgically treated 3- and 4-part proximal humerus fractures. Orthopedics. 2011;34(10):e629–33. 10.3928/01477447-20110826-14 [DOI] [PubMed] [Google Scholar]
- 45.Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ journal of surgery. 2010;80(11):789–93. 10.1111/j.1445-2197.2010.05342.x [DOI] [PubMed] [Google Scholar]
- 46.Zhang JH, Di ZL, He ZY, Feng JX, Xu RM. Comparison of humeral head replacement and internal fixation for the treatment of 3 parts and 4 parts fractures of proximal humerus in the elderly. Zhongguo gu shang = China journal of orthopaedics and traumatology. 2010;23(6):435–9. [PubMed] [Google Scholar]
- 47.Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. The Journal of bone and joint surgery American volume. 2011;93(2):159–68. 10.2106/JBJS.J.00155 [DOI] [PubMed] [Google Scholar]
- 48.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. The Journal of bone and joint surgery British volume. 1997;79(3):412–7. [DOI] [PubMed] [Google Scholar]
- 49.Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. Jama. 2015;313(10):1037–47. 10.1001/jama.2015.1629 [DOI] [PubMed] [Google Scholar]
- 50.Fjalestad T, Hole MO, Jorgensen JJ, Stromsoe K, Kristiansen IS. Health and cost consequences of surgical versus conservative treatment for a comminuted proximal humeral fracture in elderly patients. Injury. 2010;41(6):599–605. 10.1016/j.injury.2009.10.056 [DOI] [PubMed] [Google Scholar]
- 51.Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. Journal of orthopaedic trauma. 2012;26(2):98–106. 10.1097/BOT.0b013e31821c2e15 [DOI] [PubMed] [Google Scholar]
- 52.Xie L, Ding F, Zhao Z, Chen Y, Xing D. Operative versus non-operative treatment in complex proximal humeral fractures: a meta-analysis of randomized controlled trials. SpringerPlus. 2015;4:728 10.1186/s40064-015-1522-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shukla DR, McAnany S, Kim J, Overley S, Parsons BO. Hemiarthroplasty versus reverse shoulder arthroplasty for treatment of proximal humeral fractures: a meta-analysis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2016;25(2):330–40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.