Abstract
Objective
To characterize the vaginal microbiota of women following preterm premature rupture of membranes (PPROM), and determine if microbiome composition predicts latency duration and perinatal outcomes.
Design
A prospective cohort study
Setting
Canada
Population
Women with PPROM between 24+0 and 33+6 weeks gestational age (GA).
Methods
Microbiome profiles, based on pyrosequencing of the cpn60 universal target, were generated from vaginal samples at time of presentation with PPROM, weekly thereafter, and at delivery.
Main Outcome Measures
Vaginal microbiome composition, latency duration, gestational age at delivery, perinatal outcomes.
Results
Microbiome profiles were generated from 70 samples from 36 women. Mean GA at PPROM was 28.8 wk (mean latency 2.7 wk). Microbiome profiles were highly diverse but sequences representing Megasphaera type 1 and Prevotella spp. were detected in all vaginal samples. Only 13/70 samples were dominated by Lactobacillus spp. Microbiome profiles at the time of membrane rupture did not cluster by gestational age at PPROM, latency duration, presence of chorioamnionitis or by infant outcomes. Mycoplasma and/or Ureaplasma were detected by PCR in 81% (29/36) of women, and these women had significantly lower GA at delivery and correspondingly lower birth weight infants than Mycoplasma and/or Ureaplasma negative women.
Conclusion
Women with PPROM had mixed, abnormal vaginal microbiota but the microbiome profile at PPROM did not correlate with latency duration. Prevotella spp. and Megasphaera type I were ubiquitous. The presence of Mollicutes in the vaginal microbiome was associated with lower GA at delivery. The microbiome was remarkably unstable during the latency period.
Introduction
Preterm delivery is the most important contributor to neonatal morbidity and mortality worldwide [1]. Preterm premature rupture of membranes (PPROM) is a precursor to 20–30% of preterm deliveries [2, 3]. If PPROM is remote from term, prolongation of gestation is desirable if no signs of infection and fetal well-being in utero can be assured. The latency period between membrane rupture and delivery is a critical period for determining maternal and neonatal health outcomes, as although longer latencies have been associated with reduced odds of neonatal morbidity [4], there is an associated increased risk of maternal and/or fetal infection [5, 6]. This dilemma in clinical management becomes more profound closer to term and results in much debate about optimal management [7]. It is vital to understand whether the composition of the vaginal microbiome would predict safe latency or if particular dysbiosis would predict adverse outcomes for the infant and/or mother.
Abnormal vaginal microbiota is a recognized risk factor for PPROM [8–10], as endogenous bacteria present in the lower genital tract can ascend into the uterus causing an inflammatory response, which can lead to PPROM and/or preterm labour [2, 11]. Historically, anaerobes, Gram negative organisms and mycoplasmas have been associated with intrauterine infection [2, 12, 13], and some specific microbial species including genital Mycoplasma spp., Ureaplasma spp. [14], and the agents of syphilis, gonorrhea and trichomoniasis have been associated with preterm birth [2]., previous investigations have been greatly limited by dependence on the challenges of culture and isolation of fastidious organisms.
Studies exploiting high throughput DNA sequencing to detect microbes in fetal membranes, placenta and amniotic fluid of women with preterm birth (PTB), PPROM and term labour have resulted in the detection of a wider diversity of microbial species than culture dependent studies and identification of previously unrecognized species [15–18]. These results further support an association between bacterial colonization of fetal membranes and PTB. Recent studies employing sequence-based techniques have shown varied results. Romero et al. [19] detected no difference in the microbial profiles of women who subsequently delivered term or preterm, whereas others showed differences in prevalence and abundance of organisms such as Leptotrichia/Sneathia, BVAB (bacterial vaginosis-associated bacteria), Mobiluncus spp. and Mycoplasma spp. in the vaginal microbiomes of women who deliver preterm [20, 21]. To date there has been no comprehensive study, utilizing high-throughput gene sequencing based methodologies, to characterize the microbiome in the context of preterm premature rupture of the membranes.
The study objectives here were to characterize the vaginal microbiota of women presenting with PPROM and throughout latency, and to determine if vaginal microbial profile at the time of membrane rupture predicts latency duration and/or perinatal outcomes. Results of the study show that women with PPROM had mixed, highly variable vaginal microbiota but the specific type of microbiome profile at PPROM did not correlate with latency duration. Additional associations between the presence of Mollicutes, lower gestational age at delivery, and lower birth weight were detected. The presence of two taxa associated with vaginal dysbiosis, Megasphaera sp. type I and Prevotella spp., in all samples warrants further investigation.
Materials and Methods
Study design
The study received ethics approval from the University of British Columbia Children’s and Women’s Research Ethics Board (certificate no. H08-01904).
This was designed as a prospective exploratory study of women with PPROM between 24+0 and 33+6 weeks gestational age (GA), recruited at BC Women's Hospital, Vancouver, Canada. Women were approached on presentation with suspected PPROM. Verbal consent at the time of speculum examination was approved allowing confirmation of rupture of membranes and permitting immediate sample collection. Subsequently, women were invited to participate through fully informed written consent; if they declined, samples were discarded. Inclusion criteria were: adequate comprehension of English to give written informed consent, singleton gestation, no known fetal anomalies or complications distinct from PPROM, and no maternal or neonatal indication for iatrogenic PPROM. Ruptured membranes were confirmed by evidence of vaginal fluid pooling, a positive nitrazine test (elevated pH), and a positive ferning test [22].
Three swabs were collected from each woman at enrolment: a cervical swab for Chlamydia trachomatis and Neisseria gonorrhea NAT [23, 24], and two vaginal swabs from the posterior fornix and lateral vaginal wall, one for Gram stain assessment using Nugent score [25], and one for microbiome characterization. Swabs for microbiome analysis were stored, dry, at -80°C until processing. At weekly intervals, women were reviewed, clinical status recorded and additional vaginal samples obtained. This continued until delivery. Vaginal swabs for Gram stain and microbiome analysis were obtained prior to delivery where feasible.
Demographic and clinical characteristics were collected from patient charts. Clinical chorioamnionitis was diagnosed based on standard criteria of maternal pyrexia of >38°C and at least two of the following: fetal tachycardia >160 bpm, maternal tachycardia >120 bpm, leukocyte count >14000 cells, uterine tenderness and/or foul amniotic fluid. Histological chorioamnionitis was diagnosed based on placental pathology.
Neonatal outcome data collected included APGAR score [26], birth weight, gender, admission to the Neonatal Intensive Care Unit (NICU) and morbidity assessment index for newborns (MAIN) score [27].
Microbiome profiling
DNA was extracted from vaginal swabs using a magnetic bead-based kit (MagMAX, Life Technologies, Burlington, ON). PCR amplicon libraries were created as described previously using primers targeting the cpn60 universal target [28]. Sequencing was performed on the 454 GS FLX Titanium and GS Junior sequencing platforms.
High quality reads were processed as previously described using the microbial Profiling Using Metagenomic Assembly (mPUMA) pipeline [29]. Taxonomic identification of operational taxonomic units (OTU) was accomplished through comparison of OTU sequences to the cpnDB_nr reference database [30] (downloaded from www.cpndb.ca). For most analyses, OTU sequences with the same nearest reference database sequence were pooled as nearest neighbour "species" and their abundances combined accordingly.
Detection of Mollicutes
Mollicutes (Mycoplasma and Ureaplasma) were detected by genus-specific, conventional semi-nested PCR targeting the 16S rRNA gene [31]. The primary PCR targeted a 700 bp portion of the 16S rRNA gene using primers GPO-1 and MGSO [31]. PCR was performed under the following conditions: 40 cycles of 94°C for 30 s, 64°C for 30 s, and 72°C for 60 s. The secondary PCR used primers My-ins [32] and MGSO, and 2 μl of the primary PCR product as template. Thermocycling parameters included 35 cycles of 94°C for 30 s, 60°C for 30 s, and 72°C for 60 s.
Ureaplasma species (U. parvum and U. urealyticum) were detected using a conventional PCR based on the multiple-banded antigen gene with primers UMS-125 and UMA226, which yield products of two different sizes depending on the target species: 403 bp (Ureaplasma parvum) or 443 bp (Ureaplasma urealyticum) [33, 34]. Specific detection of Mycoplasma genitalium was done using a species-specific conventional PCR targeting the 16S rRNA gene [35]. M. genitalium genomic DNA for use as a positive control was obtained from the American Type Culture Collection (ATCC, Manassas, VA).
Mollicutes-specific 16S rRNA gene PCR amplicons from ten samples obtained from eight women were conveniently chosen and pooled and pyrosequenced as described for cpn60 amplicon libraries in order to gain species level identification of taxa detected by this family-specific PCR.
Statistical analysis
Demographic and clinical variables of the study cohort were investigated using non-parametric, descriptive statistics (IBM SPSS, version 21).
Microbiome data
Shannon’s diversity index, Chao1 estimated number of species and jackknifed Bray-Curtis dissimilarity were calculated using the Quantitative Insights Into Microbial Ecology (QIIME) package [36]. These indexes were bootstrapped 100 times at 1000 reads per sample or their sample maximum when <1000 reads were available. Rarefaction plots of these alpha diversity measures were generated to ensure an adequate sampling depth for each sample had been achieved. Average linkage hierarchical clustering was performed based on the proportion of each nearest neighbour species per sample using the vegan package in R [37].
Results
Maternal clinical data
Women presenting with PPROM between September 2010 and December 2012, who were >18 years of age and able to consent, were approached for participation in the study. Women with multiple gestations, stillbirths, known fetal anomalies or indications for immediate delivery were excluded. At time of study closure 51 women consented and agreed to provide samples. Of these, 17% had assessment vaginal samples that had insufficient cells present to assess by standard microscopy and 15 did not have adequate DNA extracted for evaluation. This resulted in 36 women for whom clinical and microbiologic data was available. Demographic and clinical characteristics of the women are provided in Table 1. Clinical chorioamnionitis was diagnosed in 35.5% (11/36) of women. Histopathological chorioamnionitis was detected in 67.7% (21/36) of women. There was no difference in clinical characteristics between those women for whom there was adequate microbiologic data and those excluded (data not shown).
Table 1. Demographic and clinical data for study participants (n = 36).
BMI; body mass index, BV; bacterial vaginosis, STI; sexually transmitted infection, Continuous variables are reported as means ± standard deviation [range], Counts are reported as median [IQR], Categorical variables are reported as N [%].
| Age | 32.92 ± 4.83 [22–40] |
| Pre-pregnancy BMI | 23.69 ± 4.56 [17.6–37.3] |
| Gestational diabetes | 5 [13.9%] |
| Ethnicity | |
| Asian | 9 [25%] |
| South Asian | 1 [2.8%] |
| White | 20 [55.6%] |
| Aboriginal | 3 [8.3%] |
| Other | 3 [8.3%] |
| Substance use during pregnancy | |
| Smoking | 7 [19.4%] |
| Alcohol use | 4 [11.1%] |
| Sexual history | |
| Marital Status | |
| Partnered | 32 [88.9%] |
| Single | 4 [11.1%] |
| One sexual partner during pregnancy (n = 31) | 31 [100%] |
| Vaginal intercourse during pregnancy (n = 34) | 31 [91.2%] |
| Oral sex received during pregnancy (n = 34) | 11 [32.4%] |
| Pregnancy history | |
| Previous pregnancy | 36 [100%] |
| Number of previous pregnancies (Gravida) | 2 [1.8–3.3] |
| Number of live births | 1 [0–1.3] |
| Any previous preterm birth | 5 [13.9%] |
| BV and STI history during pregnancy | |
| Diagnosed with BV (n = 34) | 2 [5.9%] |
| Diagnosed with yeast | 7 [19.4%] |
| Diagnosed with UTI | 6 [16.7%] |
| Diagnosed with Group B Streptococcus (n = 34) | 2 [5.9%] |
| Diagnosed with Chlamydia (n = 34) | 0 |
| Diagnosed with Gonorrhea (n = 34) | 0 |
| Antimicrobial use for genital tract infection during pregnancy (n = 31) | 5 [13.9%] |
| Other | |
| Feminine wipes or deodorant products (n = 34) | 5 [14.7%] |
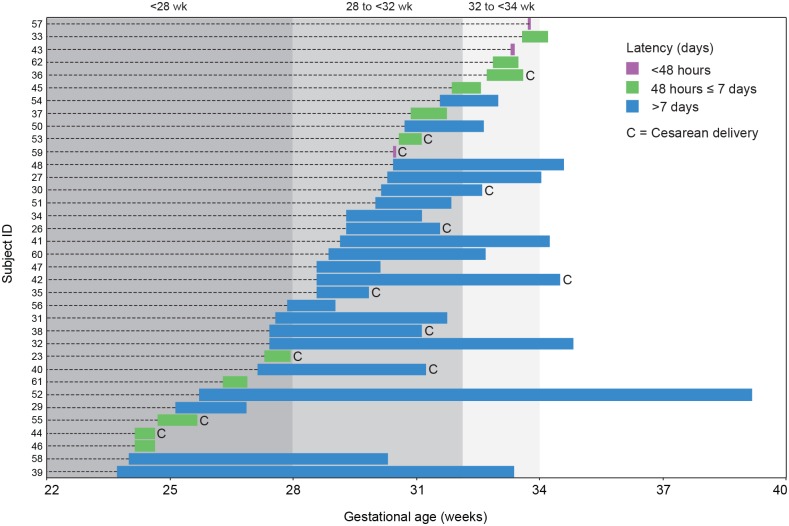
Mean GA at PPROM was 29 weeks; mean GA at delivery was 32 weeks; mean latency period was 18 days (Fig 1, Table 2). As expected, latency (days) was negatively correlated (ρs = -0.390, n = 36, p = 0.019) with GA at PPROM because the number of potential latency days decreases with increasing GA at PPROM. Since latency duration was a variable of particular interest in this study, we considered both absolute latency duration (< 48 hours, between 48 hours and ≤ 7 days, and > 7 days following membrane rupture), and latency duration as a proportion of maximum possible latency. According to the guidelines of the American College of Obstetrics and Gynecologists [38] and Society of Obstetrics and Gynecologists of Canada [5], conservative/expectant management of PPROM is recommended for gestational ages 24 to 33 weeks and induction of labour is warranted after 34 weeks. Thus, the composite variable, "proportional latency", was calculated using the following equation:
Fig 1. GA at PPROM, latency duration and delivery mode for 36 women enrolled in the study.
GA ranges corresponding to extremely (<28 weeks), very (28 to <32 weeks) or moderately (32 to <34 weeks) preterm are indicated by grey shading.
Table 2. Summary of PPROM to delivery timelines.
| No. of women (/36) | |
|---|---|
| Gestational age at PPROM | |
| Extremely preterm (<28 weeks) | 14 |
| Very preterm (28 to <32 weeks) | 17 |
| Moderate preterm (32 to <34 weeks) | 5 |
| Absolute latency | |
| <48 hours | 3 |
| Between 48 hours and < 7days | 11 |
| > 7 days | 22 |
| Proportional latency | |
| 0–0.33 | 15 |
| 0.34–0.66 | 10 |
| 0.67–1.0 | 11 |
| Mode of delivery | |
| Vaginal delivery | 24 |
| Cesarean delivery | 12 |
Clinical variables were analyzed for relationship to latency and we found that proportional and absolute latency were negatively correlated with body mass index (BMI) (ρs = -0.511, n = 31, p = 0.003).
Samples for microbiome analysis
Over the study duration, 82 vaginal samples were collected. Vaginal samples collected within 24 hours following PPROM and prior to administration of antibiotics were categorized as T0 samples (time zero, n = 24). Subsequently, weekly samples were collected until delivery, when a delivery sample was collected if possible. Average number of samples per woman was two (range 1–7).
Gram stain results
Nugent’s scoring of 19/24 T0 samples were predominantly inconsistent with bacterial vaginosis (BV) (≥ 7), with 73.9% (17/23) having normal scores (<4), and 8.7% (2/23) having intermediate scores (4–6). One sample had missing data. Altogether, 43 weekly vaginal Gram stains were evaluated. Only one was consistent with BV, 13 (30.2%) were normal and 25 (58.1%) had intermediate scores. Of the seven delivery samples, five had intermediate and two had normal scores.
Microbial profiles
For the 70 vaginal swab samples which yielded sufficient PCR product for cpn60-based microbiome profiling, an average of 12,675 cpn60 sequence reads were obtained per sample (range 36–99,358; median 6,296). One sample (week 2, woman 60) yielded only 36 sequence reads and was excluded from statistical analyses. Rarefaction analysis of alpha diversity measures (Shannon’s diversity index and Chao1 estimated number of species) indicated that all other samples had received adequate coverage for inclusion in further analysis. Raw sequence data files for the samples described in this study were deposited to the NCBI Sequence Read Archive (Accession SRP077099, BioProject PRJNA326844).
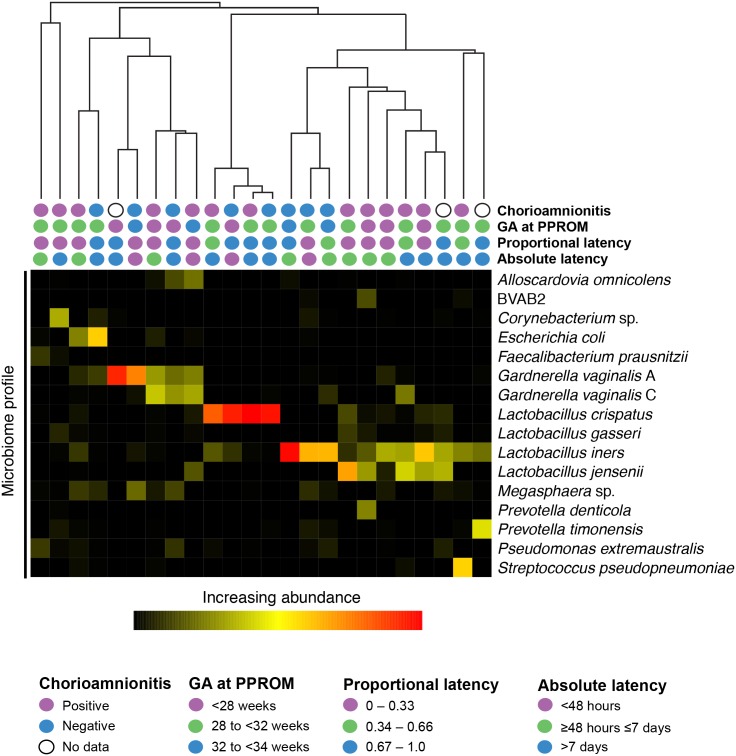
T0 microbiome profiles clustered into profile types, each dominated by one or two species including Lactobacillus crispatus, L. iners, P. timonensis, Gardnerella vaginalis (subgroups A and C), Corynebacterium sp. and Escherichia coli (Fig 2). Half (12/24) of T0 samples were dominated (≥50% of the microbiome) by one or more species of Lactobacillus. In eight cases, a single Lactobacillus sp. comprised at least 50% of the microbiome: L. crispatus (n = 4), L. iners (n = 3) and L. jensenii (n = 1), corresponding to previously described Community State Types (CST) I, III and V, respectively [39, 40]. Profiles dominated by G. vaginalis subgroup A (n = 2) correspond to CST IVC [39]. The remaining profiles included mixtures of G. vaginalis A and C or were dominated by other non-Lactobacillus species and more closely resembled CST IVA, which is defined by its heterogeneity [39].
Fig 2. Average linkage hierarchical clustering of cpn60 based microbiome profiles of T0 vaginal samples from 24 women.
Nearest neighbour species representing at least 10% of the microbiome of at least one woman are included.
Shannon’s diversity index and Chao1 diversity of T0 samples were not significantly different between proportional latency and absolute latency groups (Table 2) (Kruskal-Wallis, p > 0.05). Microbiome profile clusters were not statistically associated with outcomes of GA at PPROM, latency (absolute or proportional), or chorioamnionitis (clinical or histopathological) (Fig 2).
Core microbiome and highly prevalent organisms
A total of 670 OTUs were detected in 70 vaginal samples with 9 OTUs accounting for >50% of sequence reads obtained. Twenty nearest neighbour taxa accounted for 77% of the data (S1 Table). The most abundant OTU (12.4% of the sequence reads) was 97.1% identical to Prevotella timonensis (S1 Table) and was detected in 34/36 women (64/70 samples). An OTU sequence with 99.6% identity to Megasphaera sp. UPII 199–6, a type I Megasphaera, was detected in all 70 vaginal samples (comprising 0.0076% to 22.6% of individual microbiome profiles). OTU sequences with best matches to any Megasphaera spp. were combined with reference sequences to construct the phylogenetic tree (S1 Fig). Four additional OTU sequences clustered with M. micronuciformis, M. elsdenii, and Megasphaera sp. BV3C16-1.
OTU sequences identical to L. iners were detected in all T0 samples (n = 24). In three samples, L. iners was dominant, accounting for ≥50% of total reads.
Prevotella spp. were detected in all vaginal samples, and were dominant (accounting for ≥50% of reads) in 1/24 T0 samples and 10/46 weekly samples. Fourteen different Prevotella spp. were detected in all T0 samples, along with 15 other Prevotella-like OTU sequences with weaker (80–95%) similarity to reference sequences, suggesting possibly novel taxa (S2 Fig). The most prevalent species were P. timonensis and P. bivia, detected in 92% and 42% of T0 samples respectively.
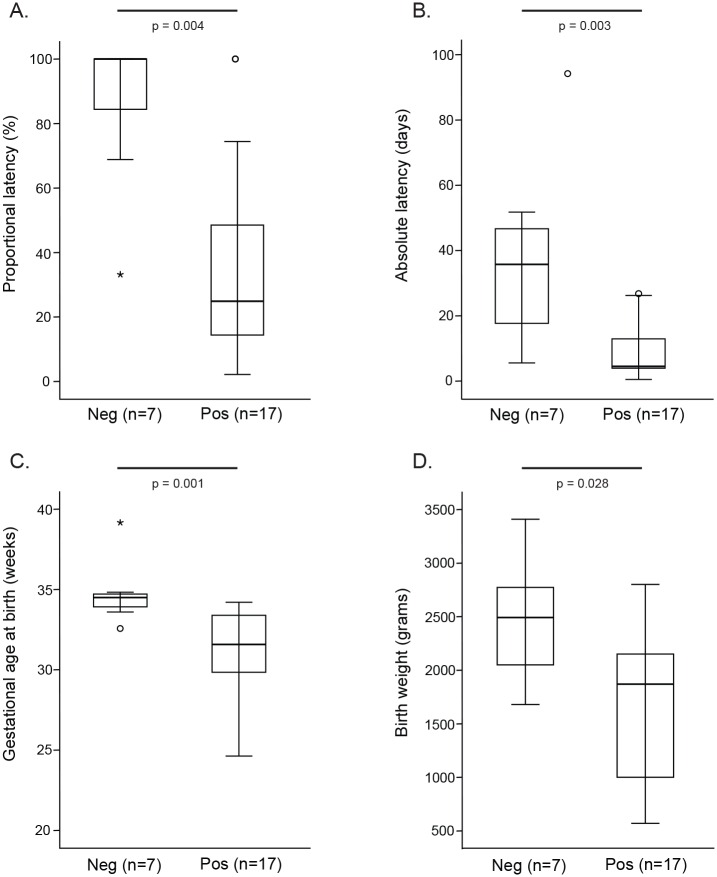
Mollicutes
Mollicutes (Mycoplasma and/or Ureaplasma) were detected by family-specific PCR in 81% (29/36) of women, Ureaplasma spp. in 53% (19/36), U. parvum in 39% (14/36) and U. urealyticum in 17% (5/36) of women. Both Ureaplasma species were detected together in only one sample. When only T0 samples were considered, 70.8% (17/24) were PCR positive for Mollicutes. Both proportional and absolute latency were significantly shorter in women whose T0 samples were PCR positive for Mollicutes compared to women who were Mollicutes negative (Fig 3, panels A, B). Women whose T0 samples were positive for Mollicutes had significantly lower GA at delivery (Fig 3, panel C), delivering correspondingly lower birth weight infants (Fig 3, panel D). In order to gain species-level information about Mycoplasma and to confirm the specificity of the PCR, we performed pyrosequencing of Mollicutes-specific 16S rRNA secondary PCR products pooled from ten samples (representing eight women). All reads (n = 28,278) could be classified as M. hominis, U. parvum or U. urealyticum. No reads were classified as M. genitalium. To rule out the possibility that the Mollicutes specific PCR failed to amplify M. genitalium, we confirmed its performance using purified genomic DNA from M. genitalium (ATCC, Manassas, VA). For additional confirmation of the absence of M. genitalium, we subsequently screened all samples with an M. genitalium species-specific PCR as described in the Methods. All samples were PCR negative for M. genitalium.
Fig 3. Proportional latency (A), absolute latency (B), GA at birth (C) and infant birthweight (D) for women with Mollicutes PCR positive or negative T0 vaginal samples.
Distributions were compared using a Mann-Whitney U test with P <0.05 considered significant.
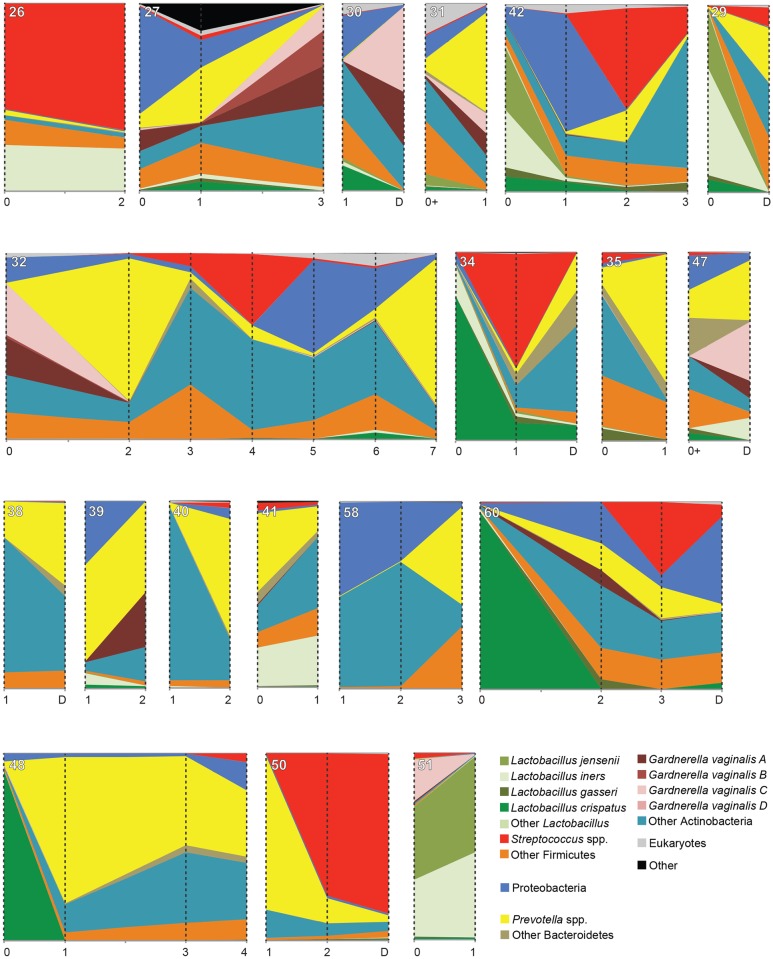
Instability of the vaginal microbiota over the latency period
All women received one or more broad-spectrum antibiotics (range 1–7 types). The variations in the types and duration of antibody therapy in this small cohort size did not allow for any associations to be drawn between antibiotic administration and microbiome changes in the latency period. In all 19 women for whom multiple samples were available, the apparent composition of the vaginal microbiota changed dramatically over the latency period (Fig 4). In 4/5 cases where Lactobacillus dominated the T0 microbiome, its proportional abundance had decreased substantially by the subsequent sample time point. Eight of 19 women for whom multiple samples were available had one or more samples dominated (≥50% of the microbiome) by Prevotella spp. (Fig 4). Of the remaining 11 women, five had Prevotella spp. as the proportionally most abundant taxon in at least one sample.
Fig 4. Vaginal microbiome profiles over the post-PPROM latency period.
Data is presented as proportion of the total sequence reads obtained for each sample, with the height of the ordinate corresponding to 100%. Sampling times are indicated with vertical broken lines, and collection time (weeks) for each sample is indicated on the abscissa. Samples indicated as collected at "0+" were collected within 3 days following PPROM, but were post-antibiotic treatment. Sample identification numbers appear in the upper left corner of each panel. The legend includes nearest neighbour species that account for at least 10% of the sequence reads in at least one sample. All women received one or more broad-spectrum antibiotics including Ampicillin, Erythromycin, Amoxicillin, Metronidazole, Clindamycin, Cefazolin, Nitrofurantoin, and/or Penicillin G.
When the PPROM cohort was compared to a cohort of healthy, non-pregnant women for whom longitudinal data was available [41], the Bray-Curtis dissimilarity between samples within PPROM cohort individuals was significantly greater (ANOVA, F1, 112 = 95.78, p < 0.0001) than the average dissimilarity for samples within individuals in the healthy, non-pregnant cohort, indicating greater instability of PPROM associated microbiomes (S3 Fig).
Neonatal outcomes
Neonatal outcomes are summarized in Table 3. APGAR score at 1 minute was positively correlated to gestational age at delivery (ρs = 0.631, n = 35, p = 0.0001), as was APGAR score at 5 minutes (ρs = 0.592, n = 35, p = 0.0001).
Table 3. Neonatal outcomes.
Continuous variables are reported as means ± 95% CI [range]. Categorical variables are reported as N [%].
| Gender | |
| Male | 25 |
| Female | 11 |
| Birth weight (grams) | 1812.9 [570–3410] |
| Extremely low birth weight (<1000 g) | 6 [16.7%] |
| Very low birth weight (<1500 g) | 4 [11.1%] |
| Low birth weight (<2500 g) | 20 [55.6%] |
| Normal | 6 [16.7%] |
| Small for gestational age (n = 35) | |
| Moderate (<10th percentile) | 2 [5.7%] |
| Severe (<3rd percentile) | 2 [5.7%] |
| Bronchopulmonary dysplasia (n = 32) | |
| None | 23 [71.8%] |
| Mild | 4 [12.5%] |
| Severe | 3 [9.4%] |
| Apgar 1 minute score (n = 35) | |
| <7 (Critical and low) | 19 |
| 7–10 (Normal) | 16 |
| Apgar 5 minute score (n = 35) | |
| <7 (Critical and low) | 5 |
| 7–10 (Normal) | 30 |
| MAIN score | 563.2 [0–1878] |
| NICU admission (n = 34) | 23 [68] |
| Days of stay in NICU | 24.57 [0.81–137.74] |
All but one infant born to women in this study survived. One infant, delivered vaginally at 25 weeks after a three-day latency period (birth weight 570 g), died of late onset sepsis at 46 days of life. Blood culture of the infant tested positive for E. coli at 12 days of life. E. coli was present in the vaginal microbiome of the mother (T0 vaginal sample, detected at 0.02% of the total microbiome). The mother’s microbiome was dominated by L. iners (32% of reads), followed by G. vaginalis. The vaginal T0 sample was positive for Mollicutes and U. urealyticum.
Discussion
Main findings
Highly diverse vaginal microbiomes were found in women at time of rupture of membranes with variability throughout latency. Of note, none of the microbiomes represented classic bacterial vaginosis, nor was a specific microbiome profile type associated with latency or neonatal outcomes. However, it was notable that two taxa associated with vaginal dysbiosis, Megasphaera sp. type I, and Prevotella spp. were found in all samples. Presence of Mycoplasma and/or Ureaplasma was associated with lower gestational age and delivery and lower birth weight.
Strengths and limitations
The strength of this study is that it is an in-depth prospective study which characterizes the microbiome following preterm premature rupture of membranes, providing new insights into the microbial profile of this fastidious, hard to culture bacterial community in these high risk pregnancies. The main limitations of this study are the relatively small number of women followed and the lack of pre-rupture samples as prediction of PPROM is very difficult. The standard use of broad-spectrum antibiotics in the context of PPROM means that the natural changes of the microbiome during latency can no longer be evaluated. Ongoing studies by our group are assessing the microbiomes of women in pregnancy, to establish the pre-rupture microbiome and to try to ascertain causality rather than association of microbial profiles with adverse perinatal outcomes.
Interpretation
Understanding the microbiome associated with PTB and PPROM is critical to creating strategies to prevent this reproductive outcome and to determine when to initiate delivery. To date, characteristics of the vaginal microbiome during the latency period following PPROM have been poorly understood. Here, the diversity and instability of women’s microbiomes following PPROM was striking. Hierarchical clustering of T0 profiles did not reveal specific associations between microbiome profiles and gestational age at PPROM, latency duration, or development of chorioamnionitis. However, although the full profile did not predict outcomes, presence of Mollicutes was a strong predictor of shorter latency. Additionally, analysis of weekly samples collected during the latency period revealed an unstable microbiome different from classic bacterial vaginosis but consistent with a dysbiosis. Of note, despite antibiotic therapy being given to prolong pregnancy, there was not a restoration of a normal Lactobacillus dominant microbiome in these women during the latency period. In fact, in 4/5 cases where Lactobacillus dominated the microbiome at PPROM, its proportional abundance decreased during subsequent latency time points. In the original studies of the use of antibiotics for latency, there were no in depth genomic based analyses available of the microbiome pre and post antibiotic therapy.
Historically, BV has been identified as a risk factor for PTB and PPROM [8, 42–46]. Here, none of the T0 samples had Nugent scores consistent with BV. Amniotic fluid leaking after membrane rupture may have resulted in a more dilute sample, reducing bacteria available for scoring. However, a lack of consistency of T0 microbiota with BV was also apparent in the sequence-based profiles, with few T0 sample microbiome profiles dominated by G. vaginalis (5/24) or Atopobium vaginae (0/24), which are strongly associated with a Nugent score diagnosis of BV [47]. Classic BV profiles were thus not the dominant profile at onset or shortly after PPROM.
Approximately half of the T0 sample profiles were dominated by Lactobacillus. Among these, the most common Lactobacillus was L. iners, either alone or in combination with L. jensenii. L. iners is associated both with normal and BV microbiota, and is reported as a dominant organism when the vaginal microbiota is in a transition state, either from normal to BV or vice versa [48–50], while L. iners-dominated microbiomes have been associated with spontaneous PTB [51]. The hemolytic and mucinolytic potential of L. iners could be involved in its survival during disturbed vaginal conditions, and may be suggestive of its pathogenic potential [52]. In contrast, longitudinal stability of vaginal microbiota in pregnant women with term deliveries has been associated with L. crispatus dominated profiles [19].
Prevotella spp. was detected in all samples from all women and dominated some profiles either at T0 or subsequent time points during latency. In contrast, a cpn60-based study of 91 vaginal samples from clinically healthy, non-pregnant, Canadian women detected Prevotella in only 57% of samples, with the most frequently detected species (P. timonensis) present in 45% of samples [41]. Here, we identified 14 known species based on comparison of OTU sequences to the cpnDB reference database [HILL et al. 2004], which currently contains cpn60 sequences for 46 Prevotella spp. An additional 15 Prevotella-like OTU sequences with no significant similarity to these 46 species, may include novel taxa. Given the suggested role of Prevotella in synergistic relationships with BV associated organisms [53, 54] and their production of lipopolysaccharide in the vaginal environment [55], the prevalence and diversity of Prevotella in PPROM associated vaginal microbiota warrants further investigation.
OTU sequences corresponding to Megasphaera type 1 were detected in all samples. Megasphaera spp. have been associated with BV [56, 57]. Two OTU sequences clustered with M. micronuciformis F0359, an obligate anaerobe isolated from the human oral cavity in the Human Microbiome Project. Identification of bacterial species associated with the oral microbiome in amniotic fluid of women who experience PTB has been observed previously, although the significance of this relationship and whether it is indicative of transfer of organisms is unknown [58, 59].
Genital Mycoplasma and Ureaplasma have been previously associated with adverse maternal/fetal outcomes [60–62]. Cervical colonization of genital mycoplasmas is associated with PTB and PPROM. These organisms have been isolated from amniotic fluid and the chorioamnion of women with PPROM and preterm labour [15, 63]. Since cpn60 genes are known to be absent in some Mollicutes [64], specific PCR was used to detect these organisms. Here, 80% of women were PCR positive for Mycoplasma and/or Ureaplasma, at the higher end of the range reported in pregnant women (10–84%) [65–68]. M. genitalium, an organism associated with cervicitis and infertility issues in women [68–70], was not detected in any woman in this study. This population had low rates of cervicitis, comparable to other studies that either did not detect the species in amniotic fluid or were not able to demonstrate associations with adverse pregnancy outcomes [68, 71]. Here, the presence of vaginal Mollicutes was associated with significantly lower GA at delivery, and correspondingly lower birth weight, supporting previous suggestions of a potential role for these organisms in adverse pregnancy outcomes.
Antibiotic and steroid administration, given as part of standard guidelines for PPROM <32 weeks [5], may have contributed to the diverse and abnormal microbiome profiles observed through latency. Another potential contributor is leakage of amniotic fluid (pH 7 to 7.5) [72] through the normally acidic vaginal environment. These factors likely contributed to the rapid transition to an abnormal microbial profile during latency in the four women who had Lactobacillus dominated profiles at PPROM.
Perhaps most important to note was the microbiota instability over the latency period. The microbial profiles and quantitative assessment of ecological distance between samples within and between women are in stark contrast to the generally stable microbial community observed in longitudinal studies of healthy, non-pregnant [40, 41] and pregnant women [73]. Stability in terms of maintenance of a core set of metabolic capabilities of the human microbiome is correlated to health, even when the community structure varies in its taxonomic composition [74]. It is highly likely that the antibiotic and steroid therapy, used in a standard fashion, may be playing a substantive role, but is affecting women in different ways.
Taken together, results here provide an unprecedented characterization of the vaginal microbiota following PPROM, and support previous suggestions of a role for Mollicutes in adverse outcomes associated with PPROM. Results also demonstrate the value of application of culture-independent methods for microbial profiling to better understand this important clinical problem.
Conclusions
Women with PPROM had mixed, highly variable vaginal microbiota but the specific type of microbiome profile at PPROM did not correlate with latency duration. The highly unstable vaginal microbiota of women in this study demonstrates the need for more intense study of the relationship of genital tract microbiota with PPROM, including functional analysis of these microbial communities. Future work should involve larger studies including sampling before/after membrane rupture, to ascertain the predisposing microbiome leading to membrane rupture.
Supporting Information
The tree is based on a 315 bp alignment and was constructed using the F84 distance algorithm followed by neighbour joining using the PHYLIP software package (Felsenstein J. PHYLIP—phylogeny inference package (version 3.2). Cladistics. 1989;5: 164–6). Bootstrap values (>50%) are indicated at nodes.
(TIF)
Study sequences detected in T0 samples are indicated by triangles. Sequences represented by circles were detected only in weekly or delivery vaginal samples. The tree is based on a 300 bp alignment and was constructed using the F84 distance algorithm followed by neighbour joining using the PHYLIP software package (Felsenstein J. PHYLIP—phylogeny inference package (version 3.2). Cladistics. 1989;5: 164–6). Only 28 of the 36 identified Prevotella-like OTU could be included in the tree since the remaining sequences did not provide sufficient overlap to be included in the alignment. Bootstrap values (>50%) are indicated at node.
(TIF)
(TIF)
(DOC)
Acknowledgments
The PPROM Study Group is Deborah M. Money, Janet E. Hill, Sean M. Hemmingsen, Eliana Castillo, Patricia A. Janssen, and Julianne van Schalkwyk. The authors are grateful to Bonnie Chaban for helpful discussion and advice in data analysis. The authors wish to thank the clinicians and laboratory staff at BC Women’s Hospital and Health Centre and their patients for their important contributions to this study.
Data Availability
Raw sequence data files for the samples described in this study were deposited to the NCBI Sequence Read Archive (Accession SRP077099, BioProject PRJNA326844). Due to ethical and legal restrictions related to protecting participant privacy imposed by the University of British Columbia Ethics Board, all other relevant data are available upon request pending ethical approval. Please submit all requests to initiate the data access process to the corresponding author.
Funding Statement
This work was funded by a March of Dimes Prematurity Research Initiative grant awarded to DM (MONEY 21-FY08-537). TPJ was supported by a University of Saskatchewan Graduate Scholarship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10 Suppl 1(S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606): 75–84. 10.1016/S0140-6736(08)60074-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mercer BM. Preterm premature rupture of the membranes. Obstet Gynecol. 2003;101(1): 178–93. [DOI] [PubMed] [Google Scholar]
- 4.Frenette P, Dodds L, Armson BA, Jangaard K. Preterm prelabour rupture of membranes: effect of latency on neonatal and maternal outcomes. J Obstet Gynaecol Can. 2013;35(8): 710–7. [DOI] [PubMed] [Google Scholar]
- 5.Yudin MH, van Schalkwyk J, Van Eyk N, Boucher M, Castillo E, Cormier B, et al. Antibiotic therapy in preterm premature rupture of the membranes. J Obstet Gynaecol Can. 2009;31(9): 863–7, 8–74. [DOI] [PubMed] [Google Scholar]
- 6.Simhan HN, Canavan TP. Preterm premature rupture of membranes: diagnosis, evaluation and management strategies. BJOG. 2005;112 Suppl 1(32–7. [DOI] [PubMed] [Google Scholar]
- 7.Dare MR, Middleton P, Crowther CA, Flenady VJ, Varatharaju B. Planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more). Cochrane Database Syst Rev. 2006;1): CD005302. [DOI] [PubMed] [Google Scholar]
- 8.Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995;333(26): 1737–42. 10.1056/NEJM199512283332604 [DOI] [PubMed] [Google Scholar]
- 9.Leitich H, Bodner-Adler B, Brunbauer M, Kaider A, Egarter C, Husslein P. Bacterial vaginosis as a risk factor for preterm delivery: a meta-analysis. Am J Obstet Gynecol. 2003;189(1): 139–47. [DOI] [PubMed] [Google Scholar]
- 10.Parry S, Strauss JF 3rd. Premature rupture of the fetal membranes. N Engl J Med. 1998;338(10): 663–70. 10.1056/NEJM199803053381006 [DOI] [PubMed] [Google Scholar]
- 11.Locksmith G, Duff P. Infection, antibiotics, and preterm delivery. Semin Perinatol. 2001;25(5): 295–309. [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg RL, Culhane JF. Infection as a cause of preterm birth. Clin Perinatol. 2003;30(4): 677–700. [DOI] [PubMed] [Google Scholar]
- 13.Goldenberg RL, Culhane JF, Johnson DC. Maternal infection and adverse fetal and neonatal outcomes. Clin Perinatol. 2005;32(3): 523–59. 10.1016/j.clp.2005.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Read JS, Klebanoff MA. Sexual intercourse during pregnancy and preterm delivery: effects of vaginal microorganisms. The Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol. 1993;168(2): 514–9. [DOI] [PubMed] [Google Scholar]
- 15.Wang X, Buhimschi CS, Temoin S, Bhandari V, Han YW, Buhimschi IA. Comparative microbial analysis of paired amniotic fluid and cord blood from pregnancies complicated by preterm birth and early-onset neonatal sepsis. PLoS One. 2013;8(2): e56131 10.1371/journal.pone.0056131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fortner KB, Grotegut CA, Ransom CE, Bentley RC, Feng L, Lan L, et al. Bacteria localization and chorion thinning among preterm premature rupture of membranes. PLoS One. 2014;9(1): e83338 10.1371/journal.pone.0083338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DiGiulio DB, Romero R, Kusanovic JP, Gomez R, Kim CJ, Seok KS, et al. Prevalence and diversity of microbes in the amniotic fluid, the fetal inflammatory response, and pregnancy outcome in women with preterm pre-labor rupture of membranes. Am J Reprod Immunol. 2010;64(1): 38–57. 10.1111/j.1600-0897.2010.00830.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones HE, Harris KA, Azizia M, Bank L, Carpenter B, Hartley JC, et al. Differing prevalence and diversity of bacterial species in fetal membranes from very preterm and term labor. PLoS One. 2009;4(12): e8205 10.1371/journal.pone.0008205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romero R, Hassan SS, Gajer P, Tarca AL, Fadrosh DW, Bieda J, et al. The vaginal microbiota of pregnant women who subsequently have spontaneous preterm labor and delivery and those with a normal delivery at term. Microbiome. 2014;2(18 10.1186/2049-2618-2-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson DB, Hanlon A, Nachamkin I, Haggerty C, Mastrogiannis DS, Liu C, et al. Early pregnancy changes in bacterial vaginosis-associated bacteria and preterm delivery. Paediatr Perinat Epidemiol. 2014;28(2): 88–96. 10.1111/ppe.12106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wen A, Srinivasan U, Goldberg D, Owen J, Marrs CF, Misra D, et al. Selected vaginal bacteria and risk of preterm birth: an ecological perspective. J Infect Dis. 2014;209(7): 1087–94. 10.1093/infdis/jit632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunningham FG, Levono KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Williams Obstetrics. 23rd Edition New York: McGraw-Hill Medical; 2010. [Google Scholar]
- 23.Van Dyck E, Ieven M, Pattyn S, Van Damme L, Laga M. Detection of Chlamydia trachomatis and Neisseria gonorrhoeae by enzyme immunoassay, culture, and three nucleic acid amplification tests. J Clin Microbiol. 2001;39(5): 1751–6. 10.1128/JCM.39.5.1751-1756.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook RL, Hutchison SL, Ostergaard L, Braithwaite RS, Ness RB. Systematic review: noninvasive testing for Chlamydia trachomatis and Neisseria gonorrhoeae. Ann Intern Med. 2005;142(11): 914–25. [DOI] [PubMed] [Google Scholar]
- 25.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29(2): 297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Queiros da Mota V, Prodhom G, Yan P, Hohlfheld P, Greub G, Rouleau C. Correlation between placental bacterial culture results and histological chorioamnionitis: a prospective study on 376 placentas. J Clin Pathol. 2013;66(3): 243–8. 10.1136/jclinpath-2012-201124 [DOI] [PubMed] [Google Scholar]
- 27.American Academy of P, Committee on F, Newborn, American College of O, Gynecologists, Committee on Obstetric P. The Apgar score. Adv Neonatal Care. 2006;6(4): 220–3. 10.1016/j.adnc.2006.04.008 [DOI] [PubMed] [Google Scholar]
- 28.Schellenberg J, Links MG, Hill JE, Hemmingsen SM, Peters GA, Dumonceaux TJ. Pyrosequencing of chaperonin-60 (cpn60) amplicons as a means of determining microbial community composition. Methods Mol Biol. 2011;733(143–58. 10.1007/978-1-61779-089-8_10 [DOI] [PubMed] [Google Scholar]
- 29.Links MG, Chaban B, Hemmingsen SM, Muirhead K, Hill JE. mPUMA: a computational approach to microbiota analysis by de novo assembly of operational taxonomic units based on protein-coding barcode sequences. Microbiome. 2013;1(1): 23 10.1186/2049-2618-1-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hill JE, Penny SL, Crowell KG, Goh SH, Hemmingsen SM. cpnDB: a chaperonin sequence database. Genome Res. 2004;14(8): 1669–75. 10.1101/gr.2649204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Kuppeveld FJ, van der Logt JT, Angulo AF, van Zoest MJ, Quint WG, Niesters HG, et al. Genus- and species-specific identification of mycoplasmas by 16S rRNA amplification. Appl Environ Microbiol. 1992;58(8): 2606–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoshida T, Maeda S, Deguchi T, Ishiko H. Phylogeny-based rapid identification of mycoplasmas and ureaplasmas from urethritis patients. J Clin Microbiol. 2002;40(1): 105–10. 10.1128/JCM.40.1.105-110.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teng LJ, Zheng X, Glass JI, Watson HL, Tsai J, Cassell GH. Ureaplasma urealyticum biovar specificity and diversity are encoded in multiple-banded antigen gene. J Clin Microbiol. 1994;32(6): 1464–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teng LJ, Ho SW, Ho HN, Liaw SJ, Lai HC, Luh KT. Rapid detection and biovar differentiation of Ureaplasma urealyticum in clinical specimens by PCR. J Formos Med Assoc. 1995;94(7): 396–400. [PubMed] [Google Scholar]
- 35.Jensen JS, Borre MB, Dohn B. Detection of Mycoplasma genitalium by PCR amplification of the 16S rRNA gene. J Clin Microbiol. 2003;41(1): 261–6. 10.1128/JCM.41.1.261-266.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5): 335–6. 10.1038/nmeth.f.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oksanen J, Blanchet FG, Kindt R, Legendre P, Minchin PR, O'Hara RB, et al. vegan: Community Ecology Package. R package version 2.0–10. 2012. Available: https://cran.r-project.org/web/packages/vegan.
- 38.Bulletins-Obstetrics ACoP. ACOG Practice Bulletin No. 80: premature rupture of membranes. Clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol. 2007;109(4): 1007–19. 10.1097/01.AOG.0000263888.69178.1f [DOI] [PubMed] [Google Scholar]
- 39.Albert AY, Chaban B, Wagner EC, Schellenberg JJ, Links MG, van Schalkwyk J, et al. A study of the vaginal microbiome in healthy Canadian women utilizing cpn60-based molecular profiling reveals distinct Gardnerella subgroup community state types. PLoS One. 2015;10(8): e0135620 10.1371/journal.pone.0135620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gajer P, Brotman RM, Bai G, Sakamoto J, Schutte UM, Zhong X, et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med. 2012;4(132): 132ra52 10.1126/scitranslmed.3003605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chaban B, Links MG, Jayaprakash TP, Wagner EC, Bourque DK, Lohn Z, et al. Characterization of the vaginal microbiota of healthy Canadian women through the menstrual cycle. Microbiome. 2014;2(23 10.1186/2049-2618-2-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martius J, Krohn MA, Hillier SL, Stamm WE, Holmes KK, Eschenbach DA. Relationships of vaginal Lactobacillus species, cervical Chlamydia trachomatis, and bacterial vaginosis to preterm birth. Obstet Gynecol. 1988;71(1): 89–95. [PubMed] [Google Scholar]
- 43.Foxman B, Wen A, Srinivasan U, Goldberg D, Marrs CF, Owen J, et al. Mycoplasma, bacterial vaginosis-associated bacteria BVAB3, race, and risk of preterm birth in a high-risk cohort. Am J Obstet Gynecol. 2014;210(3): 226 e1-7. 10.1016/j.ajog.2013.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Holst E, Goffeng AR, Andersch B. Bacterial vaginosis and vaginal microorganisms in idiopathic premature labor and association with pregnancy outcome. J Clin Microbiol. 1994;32(1): 176–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gravett MG, Nelson HP, DeRouen T, Critchlow C, Eschenbach DA, Holmes KK. Independent associations of bacterial vaginosis and Chlamydia trachomatis infection with adverse pregnancy outcome. JAMA. 1986;256(14): 1899–903. [PubMed] [Google Scholar]
- 46.Joesoef MR, Hillier SL, Wiknjosastro G, Sumampouw H, Linnan M, Norojono W, et al. Intravaginal clindamycin treatment for bacterial vaginosis: effects on preterm delivery and low birth weight. Am J Obstet Gynecol. 1995;173(5): 1527–31. [DOI] [PubMed] [Google Scholar]
- 47.Menard JP, Fenollar F, Henry M, Bretelle F, Raoult D. Molecular quantification of Gardnerella vaginalis and Atopobium vaginae loads to predict bacterial vaginosis. Clin Infect Dis. 2008;47(1): 33–43. 10.1086/588661 [DOI] [PubMed] [Google Scholar]
- 48.Verstraelen H, Verhelst R, Claeys G, De Backer E, Temmerman M, Vaneechoutte M. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 2009;9(116 10.1186/1471-2180-9-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Santiago GL, Tency I, Verstraelen H, Verhelst R, Trog M, Temmerman M, et al. Longitudinal qPCR study of the dynamics of L. crispatus, L. iners, A. vaginae, (sialidase positive) G. vaginalis, and P. bivia in the vagina. PLoS One. 2012;7(9): e45281 10.1371/journal.pone.0045281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jakobsson T, Forsum U. Lactobacillus iners: a marker of changes in the vaginal flora? J Clin Microbiol. 2007;45(9): 3145 10.1128/JCM.00558-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petricevic L, Domig KJ, Nierscher FJ, Sandhofer MJ, Fidesser M, Krondorfer I, et al. Characterisation of the vaginal Lactobacillus microbiota associated with preterm delivery. Sci Rep. 2014;4(5136 10.1038/srep05136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Macklaim JM, Gloor GB, Anukam KC, Cribby S, Reid G. At the crossroads of vaginal health and disease, the genome sequence of Lactobacillus iners AB-1. Proc Natl Acad Sci U S A. 2011;108 Suppl 1(4688–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pybus V, Onderdonk AB. A commensal symbiosis between Prevotella bivia and Peptostreptococcus anaerobius involves amino acids: potential significance to the pathogenesis of bacterial vaginosis. FEMS Immunol Med Microbiol. 1998;22(4): 317–27. [DOI] [PubMed] [Google Scholar]
- 54.Pybus V, Onderdonk AB. Evidence for a commensal, symbiotic relationship between Gardnerella vaginalis and Prevotella bivia involving ammonia: potential significance for bacterial vaginosis. J Infect Dis. 1997;175(2): 406–13. [DOI] [PubMed] [Google Scholar]
- 55.Aroutcheva A, Ling Z, Faro S. Prevotella bivia as a source of lipopolysaccharide in the vagina. Anaerobe. 2008;14(5): 256–60. 10.1016/j.anaerobe.2008.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zozaya-Hinchliffe M, Martin DH, Ferris MJ. Prevalence and abundance of uncultivated Megasphaera-like bacteria in the human vaginal environment. Appl Environ Microbiol. 2008;74(5): 1656–9. 10.1128/AEM.02127-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Datcu R, Gesink D, Mulvad G, Montgomery-Andersen R, Rink E, Koch A, et al. Vaginal microbiome in women from Greenland assessed by microscopy and quantitative PCR. BMC Infect Dis. 2013;13(480 10.1186/1471-2334-13-480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gauthier S, Tetu A, Himaya E, Morand M, Chandad F, Rallu F, et al. The origin of Fusobacterium nucleatum involved in intra-amniotic infection and preterm birth. J Matern Fetal Neonatal Med. 2011;24(11): 1329–32. 10.3109/14767058.2010.550977 [DOI] [PubMed] [Google Scholar]
- 59.Hill GB. Preterm birth: associations with genital and possibly oral microflora. Ann Periodontol. 1998;3(1): 222–32. 10.1902/annals.1998.3.1.222 [DOI] [PubMed] [Google Scholar]
- 60.Goldenberg RL, Iams JD, Mercer BM, Meis PJ, Moawad AH, Copper RL, et al. The preterm prediction study: the value of new vs standard risk factors in predicting early and all spontaneous preterm births. NICHD MFMU Network. Am J Public Health. 1998;88(2): 233–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Waites KB, Katz B, Schelonka RL. Mycoplasmas and ureaplasmas as neonatal pathogens. Clin Microbiol Rev. 2005;18(4): 757–89. 10.1128/CMR.18.4.757-789.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taylor-Robinson D, Lamont RF. Mycoplasmas in pregnancy. BJOG. 2011;118(2): 164–74. 10.1111/j.1471-0528.2010.02766.x [DOI] [PubMed] [Google Scholar]
- 63.Kim MJ, Romero R, Gervasi MT, Kim JS, Yoo W, Lee DC, et al. Widespread microbial invasion of the chorioamniotic membranes is a consequence and not a cause of intra-amniotic infection. Lab Invest. 2009;89(8): 924–36. 10.1038/labinvest.2009.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Clark GW, Tillier ER. Loss and gain of GroEL in the Mollicutes. Biochem Cell Biol. 2010;88(2): 185–94. 10.1139/o09-157 [DOI] [PubMed] [Google Scholar]
- 65.Grattard F, Soleihac B, De Barbeyrac B, Bebear C, Seffert P, Pozzetto B. Epidemiologic and molecular investigations of genital mycoplasmas from women and neonates at delivery. Pediatr Infect Dis J. 1995;14(10): 853–8. [DOI] [PubMed] [Google Scholar]
- 66.Paul VK, Gupta U, Singh M, Nag VL, Takkar D, Bhan MK. Association of genital mycoplasma colonization with low birth weight. Int J Gynaecol Obstet. 1998;63(2): 109–14. [DOI] [PubMed] [Google Scholar]
- 67.Bayraktar MR, Ozerol IH, Gucluer N, Celik O. Prevalence and antibiotic susceptibility of Mycoplasma hominis and Ureaplasma urealyticum in pregnant women. Int J Infect Dis. 2010;14(2): e90–5. 10.1016/j.ijid.2009.03.020 [DOI] [PubMed] [Google Scholar]
- 68.Larsen B, Hwang J. Mycoplasma, Ureaplasma, and adverse pregnancy outcomes: a fresh look. Infect Dis Obstet Gynecol. 2010;2010( [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pepin J, Labbe AC, Khonde N, Deslandes S, Alary M, Dzokoto A, et al. Mycoplasma genitalium: an organism commonly associated with cervicitis among west African sex workers. Sex Transm Infect. 2005;81(1): 67–72. 10.1136/sti.2003.009100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gaydos C, Maldeis NE, Hardick A, Hardick J, Quinn TC. Mycoplasma genitalium as a contributor to the multiple etiologies of cervicitis in women attending sexually transmitted disease clinics. Sex Transm Dis. 2009;36(10): 598–606. 10.1097/OLQ.0b013e3181b01948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cazanave C, Manhart LE, Bebear C. Mycoplasma genitalium, an emerging sexually transmitted pathogen. Med Mal Infect. 2012;42(9): 381–92. 10.1016/j.medmal.2012.05.006 [DOI] [PubMed] [Google Scholar]
- 72.Davidson KM. Detection of premature rupture of the membranes. Clin Obstet Gynecol. 1991;34(4): 715–22. [DOI] [PubMed] [Google Scholar]
- 73.Walther-Antonio MR, Jeraldo P, Berg Miller ME, Yeoman CJ, Nelson KE, Wilson BA, et al. Pregnancy's stronghold on the vaginal microbiome. PLoS One. 2014;9(6): e98514 10.1371/journal.pone.0098514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Human Microbiome Project C. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402): 207–14. 10.1038/nature11234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The tree is based on a 315 bp alignment and was constructed using the F84 distance algorithm followed by neighbour joining using the PHYLIP software package (Felsenstein J. PHYLIP—phylogeny inference package (version 3.2). Cladistics. 1989;5: 164–6). Bootstrap values (>50%) are indicated at nodes.
(TIF)
Study sequences detected in T0 samples are indicated by triangles. Sequences represented by circles were detected only in weekly or delivery vaginal samples. The tree is based on a 300 bp alignment and was constructed using the F84 distance algorithm followed by neighbour joining using the PHYLIP software package (Felsenstein J. PHYLIP—phylogeny inference package (version 3.2). Cladistics. 1989;5: 164–6). Only 28 of the 36 identified Prevotella-like OTU could be included in the tree since the remaining sequences did not provide sufficient overlap to be included in the alignment. Bootstrap values (>50%) are indicated at node.
(TIF)
(TIF)
(DOC)
Data Availability Statement
Raw sequence data files for the samples described in this study were deposited to the NCBI Sequence Read Archive (Accession SRP077099, BioProject PRJNA326844). Due to ethical and legal restrictions related to protecting participant privacy imposed by the University of British Columbia Ethics Board, all other relevant data are available upon request pending ethical approval. Please submit all requests to initiate the data access process to the corresponding author.