Abstract
Background
Following recent approval of pirfenidone and nintedanib for idiopathic pulmonary fibrosis (IPF), questions arise about the use of these antifibrotics in patients awaiting lung transplantation (LTx).
Methods
Safety and efficacy of antifibrotic drugs in IPF patients undergoing LTx were investigated in a single-centre retrospective cohort analysis.
Results
A total of nine patients, receiving antifibrotic therapy for 419 ± 315 days until subsequent LTx, were included. No major side effects were noted. Significant weight loss occurred during antifibrotic treatment (p = 0.0062). FVC tended to stabilize after 12 weeks of treatment in most patients. A moderate decline in FVC, TLC and DLCO was noted during the whole pretransplant time period of antifibrotic therapy. Functional exercise capacity and lung allocation score remained unchanged. No post-operative thoracic wound healing problems, nor severe early anastomotic airway complications were attributable to prior antifibrotic treatment. None of the patients developed chronic lung allograft dysfunction after a median follow-up of 19.8 (11.2–26.5) months; and post-transplant survival was 100% after 1 year and 80% after 2 years.
Conclusions
Antifibrotic drugs can probably be safely administered in IPF patients, possibly attenuating disease progression over time, while awaiting LTx.
Keywords: Antifibrotics, IPF, Lung transplantation, Nintedanib, Pirfenidone, Safety
Background
Idiopathic pulmonary fibrosis (IPF) is a progressive and lethal disease characterized by chronic, fibrosing interstitial pneumonitis of unknown cause, associated with a histopathologic and/or radiologic pattern of usual interstitial pneumonia (UIP) [1]. The course of the disease is unpredictable. Most patients demonstrate a slow, gradual progression; some patients remain stable; while others have an accelerated decline, sometimes due to repeated exacerbations. Consequently, respiratory failure is the most common cause of death in IPF. Once diagnosed, timely referral to an expert centre is therefore essential to assess eligibility for pharmacological therapy and/or lung transplantation (LTx) [2].
In October 2014, the US Food and Drug Administration (FDA) approved two anti-fibrotic drugs for IPF - pirfenidone and nintedanib - based on the results of large randomized clinical trials (CAPACITY-1, CAPACITY-2 and ASCEND with pirfenidone; TOMORROW, INPULSIS-1 and INPULSIS-2 with nintedanib) demonstrating a reduction in the rate of decline in forced vital capacity (FVC) in mild to moderate IPF [3–5]. Post-hoc analysis also demonstrated a risk reduction for IPF-related mortality with pirfenidone compared to placebo (HR 0.32, 95% CI 0.14–0.76, p = 0.006) [6], a same trend which was also observed with nintedanib (HR 0.70; 95% CI 0.46–1.08; p = 0.0954) [7].
Despite these positive findings, it should be emphasized that both antifibrotic drugs do not represent a ‘cure’ for IPF, but only aim to attenuate the decline in FVC, at best resulting in temporary disease stabilization. Moreover, side effects (typically nausea, anorexia, malaise, or rash for pirfenidone; and diarrhea for nintedanib) or adverse events (mainly toxic hepatitis) may force some patients to reduce or even stop treatment, which may again accelerate disease progression. Hence, early evaluation and referral for LTx, which presently remains the only definitive treatment option for well-selected IPF patients, is highly recommendable, particularly since IPF patients have the highest waiting list mortality, due to disease progression. The recent introduction of the lung allocation score (LAS) in some countries may nevertheless decrease future waiting list mortality in IPF. Implementation of the LAS indeed has already led to a substantial increase in the proportion of LTx performed for IPF, making it the most common indication for LTx and reducing waiting list time for IPF in these countries [8].
With increasing use of antifibrotics following recent FDA approval, questions arise about their safety in IPF patients undergoing LTx, yet safety data in this specific setting are currently lacking. The antifibrotic properties of pirfenidone result from inhibition of transforming growth factor (TGF)-β expression, thus attenuating myofibroblast differentiation and fibroblast activity [9]. Nintedanib is a tyrosine kinase inhibitor, which blocks receptors for platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF), thus inhibiting downstream signaling in (myo-)fibroblasts [10]. Both antifibrotics may hence theoretically impair post-operative wound healing and/or cause bronchial anastomotic complications following LTx. Nintedanib, by inhibition of VEGF and PDGF, may in theory also result in an increased peri-operative bleeding risk. Moreover, it is unclear whether antifibrotic treatment, when effectively achieving disease stabilization for several months, would influence LAS or may even interfere with referral for LTx, given an upper age limit for LTx used in most centres.
In the current study we therefore report on safety and efficacy of pretransplant antifibrotics in IPF patients undergoing LTx. Pretransplant pulmonary function, functional exercise capacity; and immediate and long-term post-operative outcomes, including the early post-operative course, presence of bronchial anastomotic complications, chronic lung allograft dysfunction (CLAD) and survival, were retrospectively assessed.
Methods
Study design and population
This is a single-centre, retrospective analysis of IPF patients undergoing LTx in a large volume transplant centre at a tertiary care hospital. The current study was approved by the Leuven University Hospital Ethical Review Board (S51577) and patients gave informed consent. IPF diagnosis was confirmed in by a multidisciplinary board discussion, including an expert chest physician specialized in interstitial lung disease (ILD) (WW), an experienced chest imaging radiologist and a specialized lung-pathologist (EKV). For the current study, we included all IPF patients up to December 2015 who had undergone LTx in our centre whilst being treated with either pirfenidone or nintedanib. There were no IPF patients receiving antifibrotic drugs who died on the waiting list before LTx.
Pirfenidone was initiated between September 2008 and September 2013; and patients were subsequently transplanted between November 2008 and April 2015. Nintedanib was started between August 2010 and January 2012; and patients were transplanted between March 2011 and October 2014. In Belgium, pirfenidone was approved for mild to moderate IPF (FVC >50%predicted (%pred) and Diffusion Capacity (DLCO) >35%pred) in December 2012 and nintedanib has been approved for mild to severe IPF (FVC ≥50%pred and DLCO ≥30%pred) since December 2015. Patients in whom antifibrotic therapy was initiated before these respective dates thus received the drugs in the context of clinical trials, thereafter patients received open-label treatment according to reimbursement rules. All IPF patients were evaluated on regular intervals (every 3 to 4 months) at a specialized outpatient ILD consultation by a specialized physician (WW) and nurse, who checked compliance and tolerance of their antifibrotic therapy.
Data collection
Data were retrospectively collected from the patients’ electronical medical files, including clinical and demographical variables, duration of antifibrotic treatment, laboratory results, anastomotic problems (scored according to MDS classification as previously reported, [11]), evolution of pulmonary function and functional exercise capacity. The estimated annual decline in pulmonary function parameters (FVC, Total Lung Capacity (TLC) and DLCO) was calculated based on the difference in pulmonary function parameters between the start of antifibrotic therapy (‘baseline’) and at the time of LTx, adjusted for the number of months therapy was taken (monthly decline) and extrapolated to 1 year (monthly decline x12). The same approach was used regarding the decrease in six minute walking test (6MWT) between start of therapy and LTx. LAS was retrospectively assessed at start of antifibrotic therapy, at LTx listing (data summarized in Table 1) and at LTx. However, we used LAS at start of antifibrotic therapy for further statistical analyses regarding pre-LTx evolution of LAS, because most patients were initiated on antifibrotics before LTx listing.
Table 1.
Recipient and donor demographics of the IPF treatment group and historical control group
| ID | Recipient Gender (M/F) | Recipient Age (Years) | Anti-fibrotic Drug | Cardio-Pulmonary Rehabilitation | Time on Therapy (Days) | FVC at start (%pred) | TLC at start (%pred) | DLCO at start (%pred) | 6MWT at start (m) | Time on WL (Days) | LAS at listing | Type of LTx (S/SS) | Donor Gender (M/F) | Donor Age (Years) | Type of Donor | CMV Donor/Recipient |
| 1 | F | 62 | PFD | no | 735 | 91 | 72 | 46 | 529 | 762 | 32 | SS | F | 17 | DBD | D+/R+ |
| 2 | M | 61 | PFD | CPR | 545 | 71 | 61 | 37 | 379 | 179 | 31 | SS | F | 67 | DCD cat III | D-/R- |
| 3 | M | 51 | PFD | CPR | 387 | 88 | 80 | 47 | 552 | 29 | 35 | SS | M | 37 | DBD | D+/R- |
| 4 | M | 63 | PFD | CPR | 539 | 52 | 45 | 32 | 384 | 51 | 30 | SS | M | 55 | DBD | D-/R+ |
| 5 | M | 55 | PFD | CPR | 188 | 56 | 52 | 35 | 631 | 25 | 29 | SS | M | 23 | DBD | D+/R- |
| 6 | M | 64 | PFD | no | 115 | 62 | 48 | 39 | 503 | 163 | 33 | SS | M | 35 | DCD cat V | D+/R+ |
| 7 | M | 64 | PFD | no | 65 | 79 | 56 | 28 | 267 | 419 | 37 | S | F | 42 | DBD | D+/R- |
| 8 | M | 65 | NIN | no | 1003 | 80 | 69 | 58 | 598 | 155 | 31 | SS | M | 62 | DBD | D+/R- |
| 9 | M | 56 | NIN | no | 194 | 58 | 56 | 29 | 275 | 74 | 32 | SS | M | 39 | DCD cat III | D-/R- |
| Mean or Median | 60.1 ± 4.9 | 419 ± 315 | 70.8 ± 14.5 | 59.9 ± 11.7 | 39.0 ± 9.8 | 457.6 ± 135.6 | 155 (40–299) | 32.2 ± 2.5 | 43.6 ± 17.1 | |||||||
| 1 | M | 57 | / | no | / | / | / | / | / | 279 | 33 | SS | F | 48 | DCD cat III | D-/R+ |
| 2 | M | 62 | / | no | / | / | / | / | / | 153 | 35 | SS | F | 66 | DBD | D+/R+ |
| 3 | M | 55 | / | no | / | / | / | / | / | 17 | 34 | SS | M | 74 | DBD | D+/R+ |
| 4 | M | 59 | / | CPR | / | / | / | / | / | 274 | 32 | SS | M | 22 | DCD cat III | D-/R+ |
| 5 | M | 59 | / | CPR | / | / | / | / | / | 253 | 29 | SS | M | 57 | DBD | D-/R- |
| 6 | M | 65 | / | CPR | / | / | / | / | / | 112 | 26 | S | M | 37 | DBD | D+/R+ |
| Mean or Median | 59.5 ± 3.6a | 203 (88–275)a | 31.5 ± 3.4a | 50.7 ± 19.a | ||||||||||||
| ID | Ischemic Time 1th/2nd Lung (min) | Immuno-suppressive Regimen | Time to Extubation (Hours) | PGD at 72 h | Time on ICU (Days) | Time in Hospital (Days) | AR or LB Episodes (Number) | Most Severe AR or LB (Grade) | Respiratory infection before Discharge (Presence = 1) | Respiratory Pathogen before Discharge | Anastomotic Complications (Details in Text) | |||||
| 1 | 187/320 | rATG/FK/MMF/CS | 34 | 0 | 6 | 16 | 0 | 0 | 0 | / | 0 | |||||
| 2 | 432/580 | rATG/FK/MMF/CS | 20 | 3 | 7 | 20 | 1 | 1 | 1 | E. coli, S. viridans | M2aD0aS0 (POD 30) | |||||
| 3 | 498/694 | No ATG, FK/MMF/CS | 37 | 0 | 4 | 16 | 2 | 2 | 1 | A. baumanii, E. coli, S. aureus | M3bD2cS2f (POD 204) | |||||
| 4 | 417/631 | rATG/FK/MMF/CS | 65 | 1 | 13 | 26 | 1 | 1 | 0 | / | M2aD0aS0 (POD 30) | |||||
| 5 | 366/515 | rATG/FK/MMF/CS | 41 | 2 | 6 | 17 | 0 | 0 | 1 | C. freundii | 0 | |||||
| 6 | 385/582 | rATG/FK/MMF/CS | 37 | 1 | 4 | 16 | 3 | 2 | 0 | / | 0 | |||||
| 7 | 341 | rATG/CsA/AZA/CS | 33 | 2 | 3 | 21 | 0 | 0 | 1 | H. influenza, MRSA | 0 | |||||
| 8 | 180/356 | rATG/FK/MMF/CS | 178 | 3 | 10 | 28 | 1 | 3 | 1 | H. influenza, S. pneumoniae | M1aD0aS0 (POD 90) | |||||
| 9 | 239/356 | rATG/FK/MMF/CS | 38 | 2 | 5 | 23 | 1 | 2 | 0 | / | 0 | |||||
| 338 ± 113/504 ± 142 | 37 (33.5–53) | 2 (0.5–2.5) | 6.4 ± 3.2 | 20.3 ± 4.6 | 1 (0–1.5) | 1 (0–2) | ||||||||||
| 1 | 404/626 | rATG/FK/MMF/CS | 72 | 0 | 7 | 19 | 1 | 2 | 0 | / | 0 | |||||
| 2 | 220/412 | rATG/FK/MMF/CS | 16 | 1 | 7 | 25 | 2 | 3 | 1 | S. aureus | M3bD0aS0 (POD 30) | |||||
| 3 | 288/431 | rATG/FK/MMF/CS | 432 | 3 | 60 | 253 | 1 | 1 | 1 | P. aeruginosa, K. pneumoniae, | M3bD2bS0 (POD 40) | |||||
| 4 | 276/423 | rATG/FK/MMF/CS | 48 | 2 | 15 | 32 | 1 | 1 | 1 | E. faecalis | M2aD0aS0 (POD 14) | |||||
| 5 | 209/439 | rATG/CsA/AZA/CS | 48 | 2 | 23 | 32 | 0 | 0 | 1 | K. oxytoca | M3aD0S0 (POD 17) | |||||
| 6 | 186 | rATG/CsA/AZA/CS | 24 | 1 | 8 | 20 | 2 | 1 | 0 | / | 0 | |||||
| 264 ± 79a/466 ± 90a | 48 (22–162)a | 1.5 (0.8–2.3)a | 20.0 ± 20.6b | 63.5 ± 93a | 1 (0.75–2.0)a | 1 (0.75–2.25)a | ||||||||||
| ID | Time of Follow-up(Months) | Status (Dead = 1) | Last FVC Post-LTx (%pred) | Last FEV1 Post-LTx (%pred) | Last FEV1/FVC Post-LTx (%pred) | |||||||||||
| 1 | 7.7 | 0 | 145 | 147 | 86 | |||||||||||
| 2 | 8.6 | 0 | 106 | 90 | 66 | |||||||||||
| 3 | 16.9 | 0 | 70 | 68 | 77 | |||||||||||
| 4 | 21.9 | 0 | 90 | 67 | 58 | |||||||||||
| 5 | 25.8 | 0 | 93 | 93 | 80 | |||||||||||
| 6 | 27.1 | 0 | 123 | 126 | 79 | |||||||||||
| 7 | 19.8 | 1 | 110 | 107 | 76 | |||||||||||
| 8 | 13.8 | 0 | 119 | 115 | 75 | |||||||||||
| 9 | 56.3 | 0 | 132 | 141 | 84 | |||||||||||
| 19.8 (11.2–26.5) | 109 ± 23.1 | 106 ± 29.1 | 75.7 ± 8.8 | |||||||||||||
| 1 | 14.9 | 0 | 117 | 76 | 66 | |||||||||||
| 2 | 23.5 | 0 | 104 | 99 | 76 | |||||||||||
| 3 | 37.0 | 0 | 67 | 61 | 73 | |||||||||||
| 4 | 38.6 | 0 | 107 | 92 | 67 | |||||||||||
| 5 | 52.4 | 0 | 104 | 58 | 43 | |||||||||||
| 6 | 12.2 | 1 | 79 | 82 | 81 | |||||||||||
| 30.3 (14.2–42.1) | 96.3 ± 19.1 | 78.0 ± 16.4 | 67.7 ± 13.3 | |||||||||||||
Data are expressed as mean ± SD, median (interquartile range) or as total values where appropriate
Abbreviations: 6MWT 6 min walking test, AR Acute (cellular) Rejection, AZA azathioprine, cat category, CMV Cytomegalovirus, CPR Cardio-Pulmonary Rehabilitation, CS corticosteroids, CsA cyclosporine A, D donor, DBD donation after brain death, DCD donation after cardiac death, DLCO diffusion capacity, F Female, FK tacrolimus, FVC Forced Vital Capacity, ICU Intensive Care Unit, ID identification, LAS lung allocation score, LB lymphocytic bronchiolitis, LTx lung transplantation, M male, MDS severity of anastomotic complication according to MDS classification, MMF mycophenolate mofetil, NIN nintedanib, PFD pirfenidone, PGD primary graft dysfunction, R recipient, rATG rabbit Anti-Thymocyte Globulin, S single, SS sequential single, TLC Total Lung Capacity, WL waiting list
a:p > 0.05 (not statistically significant compared to treated group), b:p = 0.021 compared to treated group
Historical controls
We additionally identified a comparable group of historical controls (n = 6), which consisted of IPF patients who did not receive antifibrotic therapy before LTx, but were transplanted in the same era (7/2010 to 9/2014), had comparable age and lung function at the time of LTx compared to the treatment group: FVC 57.0 (43.0–69.8) %pred (p = 0.69 vs. treatment), TLC 53.0 (42.5–71.0) %pred (p = 1.0 vs. treatment) and DLCO 21.5 (17.0–29.2) %pred (p = 0.11 vs. treatment). Given the small number of available patients, it was impossible to match both groups any further regarding concurrent emphysema (but TLC and DLCO were comparable between both groups, thus excluding major differences due to emphysema), pulmonary hypertension (was not routinely assessed in non-treated IPF patients, no comparison possible with treated group who were all screened at start of antifibrotic therapy) or cardiovascular disease (but major cardiovascular disease is generally an exclusion-criterion to proceed to LTx in any patient). Reasons for not starting antifibrotic therapy in these matched historical controls were: absence of consent (n = 3), DLCO too low for study-inclusion (n = 2) and pending approval by the health care authorities whilst awaiting LTx (n = 1). These historical controls were only used as comparator for the IPF group treated with antifibrotics regarding the annual pre-transplant decline in pulmonary function; and some mportant early post-transplant outcome parameters, including rates of PGD, infection, rejection and anastomotic complications. These historical patients were not the main aim of this study, which focusses on reporting safety and efficacy of antifibrotics in IPF patients undergoing LTx.
Statistical analysis
All analyses were performed using Graphpad Prism 5a software (San Diego, USA). Results are expressed as mean (± standard deviation) or median (interquartile range) where appropriate. Group means were compared using paired or unpaired t-test; Mann-Whitney test or Wilcoxon signed rank test for normally or not-normally distributed variables, respectively. All reported p-values are two-tailed and p < 0.05 was considered significant.
Results
Patients’ characteristics
A total of 9 IPF patients were treated with antifibrotics and subsequently underwent LTx: pirfenidone n = 7 (n = 2 study vs. n = 5 open-label treatment), nintedanib n = 2 (both in study). All patients, but one, underwent bilateral LTx and all, but one, were male. Age at LTx was 60.1 ± 4.9 years. Five patients were on continuous oxygen therapy (4 (3.5–4.0) Liters/min) before LTx, while 4 were not (Table 1). Antifibrotic therapy had been initiated 362 (152–578) days before listing for LTx in 6/9 patients, whereas in 3/9 patients antifibrotics were started 48 (27–354) days after transplant listing. In all 9 cases antifibrotic therapy was continued until the day of transplant procedure. Total duration of antifibrotic therapy until LTx was 419 ± 315 days, or 13.8 ± 10.3 months. All patients received the full, recommended dose (i.e. 801 mg tid for pirfenidone and 150 mg bid for nintedanib).
Nausea was reported as main side-effect of antifibrotic therapy in 9/9 patients; and 7/9 patients lost weight during treatment (n = 6 pirfenidone, n = 1 nintedanib), in one patient (on pirfenidone) weight remained stable and one patient (on nintedanib) gained 1 kg. Overall, body mass index (BMI) decreased from 27.3 ± 3.2 kg/m2 to 25.8 ± 3.3 kg/m2 (p = 0.0063) during antifibrotic treatment, with an absolute weight loss of 329 ± 360 g per month of treatment (p = 0.0062). None of the patients developed toxic hepatitis, nor discontinued their therapy due to other severe side-effects or adverse events. No acute IPF exacerbations occurred in any of the patients during antifibrotic treatment.
Evolution of pretransplant pulmonary function, functional exercise capacity, pulmonary hypertension, renal function and LAS
Spirometry was performed at the start of antifibrotic treatment (‘baseline’) and during subsequent follow-up. Consecutive spirometry after six months of antifibrotic therapy was only available in 6/9 patients, as 3 patients (n = 2 pirfenidone, n = 1 nintedanib) underwent LTx within 6 months after initiating therapy (Fig. 1). In these 6/9 patients (n = 5 pirfenidone, n = 1 nintedanib), the absolute decline in FVC after 12 weeks of treatment compared to baseline was −7.0%pred (−1.8 to −11.5), with 4/6 (66.6%) patients having <10% decline in FVC %pred; and only 2/6 (33.3%) patients demonstrating a ≥10% decline in FVC %pred (p = 0.063 vs. start). Nevertheless, an overall absolute decrease in FVC, TLC and DLCO during the whole pretransplant antifibrotic treatment period (i.e. 419 ± 315 days or 59 ± 44 weeks) was observed in these 6/9 patients (Fig. 2).
Fig. 1.
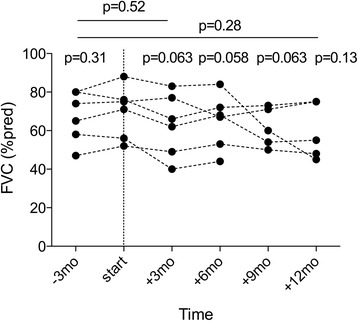
Forced Vital Capacity in IPF patients with at least 6 months antifibrotic therapy before transplantation. Forced Vital Capacity (FVC) (%predicted) is given at the start of antifibrotic therapy (start), 3 months before and respectively 3, 6, 9 and 12 months (mo) after start. Dotted lines connect values in patients (n = 6/9) with consecutive measurements at different time points; p-values (Wilcoxon signed rank test) above each time point are given compared to start; or compared another time point (time-frame indicated by full line)
Fig. 2.
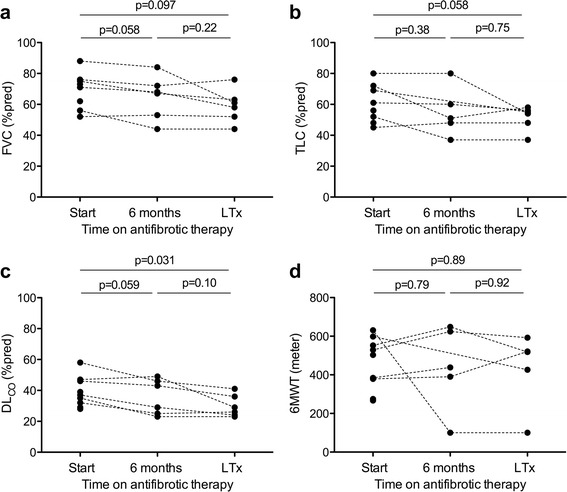
Pretransplant evolution of pulmonary function and functional exercise capacity following treatment with antifibrotic drugs. Forced Vital Capacity (FVC) (a), Total Lung Capacity (TLC) (b), Diffusion capacity (DLCO) (c) (all in (%predicted) and 6 min walk test (6MWT, meter) (d) at start of antifibrotic therapy (start) and at the moment of lung transplantation (LTx) in the included IPF patients. Dotted lines connect values in patients (n = 6/9) with a consecutive measurement at six months and just before transplantation; p-values (Wilcoxon signed rank test) are given for patients that had consecutive measurements
The calculated annual decline during treatment for all included patients was: FVC 322.0 (148.3–1074.0) mL or 6.6 (0–23.8) %pred, TLC 360.0 (157.5–1818.0) mL or 6.0 (2.0–25.7) %pred; and DLCO 0.77 (0.40–1.96) mmol/min/Kpa or 7.5 (4.7–18.6) %pred. Interestingly, the measured annual rate of decline in the matched historical controls (without antifibrotic therapy) during the year preceding LTx appeared to be somewhat more severe compared to the group with antifibrotics, although no significant differences were seen: FVC 460.0 (215.0–732.5) mL or 13.0 (4.8–18.0) %pred (p = 0.69); TLC 945.0 mL (362.5–1490) or 10.0%pred (2.0–20.0) (p = 1.0); and DLCO 1.26 (0.38–2.09) mmol/min/Kpa or 14.0 (4.0–24.8) %pred (p = 0.94).
6MWT was performed before the start of antifibrotic therapy and consecutive 6MWT was available in 5/9 patients (all on pirfenidone), of whom 3/5 were enrolled in a pretransplant cardio-pulmonary rehabilitation (CPR) program upon transplant listing and 2/5 were not. 6MWT overall increased with 54 (−260.0–95.5) m after 12 weeks of treatment compared to baseline (p = 0.62), with an improved in 4/5 patients of 74.5 (21.8–95.8) m, while one patient demonstrated a decline of 531 m (patient n°5 in Table 1, no CPR, concomitant decline in FVC of 12%pred during these 12 weeks of treatment). During the whole pretransplant time period of antifibrotic treatment (59 ± 44 weeks), 6MWT did not significantly change compared to baseline (p = 0.89): 6MWT improved compared to baseline in 2/5 patients (+63 m (no CPR) and +142 m (with CPR), respectively), while 6MWT deteriorated in 3/5 patients (one no CPR, two with CPR), in whom there was an absolute decline of −172 (34–531) meters or a monthly decline of −5.2 (2.7–85.7) meters during treatment (Fig. 2). In the historical controls, unfortunately, 6MWD was only available upon listing for LTx, thus no consecutive 6MWT were available for further comparison.
Transthoracic echocardiography performed before start of antifibrotic therapy (pulmonary arterial pressure (PAP) 31.1 ± 7.4 mmHg) and consecutive echocardiography was available in 4/9 patients, in whom PAP tended to increase during antifibrotic treatment (PAP +9.5 (2.0–15.5) mmHg: p = 0.090). Renal function remained stable during antifibrotic treatment: serum creatinine was 0.96 ± 0.14 mg/dL at start versus 0.95 ± 0.17 mg/dL at LTx (p = 0.97), estimated glomerular filtration rate was 83 ± 13 mL/min/1.73 m2 at start versus 82 ± 14 mL/min/1.73 m2 at LTx (p = 0.83). No hepatic dysfunction was observed in any patient during treatment. LAS did not significantly change during antifibrotic treatment: 32.2 ± 2.5 at start of therapy versus 32.3 ± 1.0 at LTx (p = 0.13).
Post-transplant outcomes
Patients receiving antifibrotics were listed for 155 (40–299) days before subsequent LTx. Transplant procedures were overall uneventful and only one patient (who had received pirfenidone, had the highest pretransplant PAP of 48 mmHg and underwent single sided LTx) required peri-operative support with veno-arterial extracorporeal membrane oxygenation. There were no bleeding problems (i.e. no need for re-thoracotomy for hemothorax, no additional transfusion of blood products for blood loss) in any patient, including those on nintedanib. Overall, patients were extubated after 37.0 (33.5–53.0) hours of ventilation, discharged from the intensive care unit after 6.4 ± 3.2 days and discharged home after a hospital stay of 20.3 ± 4.6 days. There were no problems with post-operative thoracic wound healing or dehiscence in any patient. All patients, but one, received post-operative induction therapy with anti-thymocyte globulin for 3 days; and post-operative immunosuppressive regimen consisted of tacrolimus, mycophenolate mofetil and steroids in all patients, except one (transplanted in 2008) who received cyclosporine, azathioprine and steroids (our standard regimen before 2010). No major side effects due to possible drug-interactions with prior antifibrotics were seen in the first days post-LTx.
A total of 4/9 patients were included in a clinical trial immediately following LTx: 2 in a therapeutic trial with azithromycin (AZI003, NCT01915082), 1 in an ex-vivo normothermic machine perfusion trial (EXPANDLung, NCT01963780) and 1 in a Diaphragm Pacing trial (NCT02411383), which may obviously influence early and/or late outcomes (including post-transplant evolution of pulmonary function, anastomotic airway complications, primary graft dysfunction (PGD), rejection, infection, CLAD) in these transplant recipients compared to those not included in a trial or historical controls. Overall, incidence of PGD (PGD ≥ 2 in 5/9 patients), early post-operative infection (5/9 patients) and acute cellular rejection (4/9 patients) or lymphocytic bronchiolitis (4/9) during the first 6 months were comparable to findings in the historical controls (all p > 0.5) (Table 1).
Anastomotic airway complications were present in 4/9 patients: in two patients (prior pirfenidone) mild anastomotic necrosis without dehiscence or airway narrowing was noted upon discharge after LTx (post-operative day (POD) 30; MDS classification M2aD0aS0 for right-sided anastomosis and M0aD0aS0 for left-sided anastomosis in both patients), with spontaneous and uncomplicated resolution thereafter. In a third patient (initially no anastomotic complications, prior nintedanib), there was mild protrusion of cartilage on POD 90 (M0aD0aS0 for right-sided anastomosis and M1aD0aS0 for left-sided anastomosis), with spontaneous and uncomplicated resolution thereafter. In the fourth patient (initially no anastomotic complications, prior pirfenidone), following infection with Aspergillus fumigatus at POD 186, late-onset (POD 204) anastomotic necrosis occurred with bronchial narrowing and extensive dehiscence (M0aD0aS0 for right-sided anastomosis and M3bD2cS2f for left-sided anastomosis). Despite antifungal treatment, he developed severe symptomatic anastomotic stenosis, which finally required surgical sleeve-resection and reconstruction of the left main bronchus on POD 410. Thereafter, no other problems occurred and the patient currently has a stable pulmonary function at POD 525. The observed anastomotic airway complications, however, did not appear to be more severe or prevalent compared to previously reported data from our centre [11] or to the historical controls, of whom 4/6 controls had early anastomotic airway complications (ranging from M2aD0aS0 to M3bD2bS0; Table 1).
Overall, long-term outcome in our cohort was good: after a median follow-up of 19.8 (11.2–26.5) months, currently all patients have a stable pulmonary function (Table 1) and none of the patients has developed CLAD. One patient (who underwent single sided LTx), unfortunately, has died because of non-squamous large cell lung carcinoma of his native IPF lung on POD 615, all other patients are alive and ambulatory at present. Overall survival was 100% after 1 year and 80% after 2 years, respectively.
Discussion
Little is known about safety of antifibrotic therapy with pirfenidone or nintedanib in patients undergoing LTx. Actually only 11 IPF patients receiving pirfenidone; and none receiving nintedanib, included in the large randomized trials with these drugs (comprising a total of 2832 study-subjects) were reported as having been transplanted during antifibrotic treatment, yet detailed outcome data for these patients are lacking [3–7]. Only 1 case report has currently been published on pretransplant pharmacological bridging with pirfenidone, allowing stabilization of respiratory function and subsequent single sided LTx in IPF. Anastomic airway complications, however, were not reported in this case [12]. Next to this, there have been two abstracts reporting on this topic, which did not yet result in peer-reviewed papers, but in which, apparently, pirfenidone therapy was not linked to adverse post-transplant events, however follow-up was limited and detailed outcome data missing [13, 14]. In the current case series, we therefore report on pre-operative evolution and post-transplant outcomes of 9 IPF patients, treated with either pirfenidone or nintedanib for a mean of 13.4 months until subsequent LTx and with a median post-transplant follow-up of 19.8 months.
According to the same definitions used in larger IPF trials [6, 15], we noted relative stabilization (i.e. < 10% change) of FVC during the first 12 weeks of antifibrotic treatment. Importantly, this early stabilization, or perhaps better attenuated rate of decline, in FVC may by no means be a reason to deny subsequent LTx to eligible patients, because further decline in FVC, lung volumina and DLCO is to be expected despite antifibrotic treatment, as was obvious from our results. The estimated annual decline in FVC during treatment in our cohort, however, would be around 6.6%pred, which corroborates recent findings that both pirfenidone and nintedanib reduce the proportion of patients with a ≥10% decline in FVC %pred after 1 year of treatment [5, 6]. As they may attenuate disease progression, these antifibrotics may thus allow for valuable added time on the LTx waiting list. Next to FVC, 6MWT has also been shown to be a valid outcome measure, both in IPF, in whom the clinically important difference in 6MWT distance is reported to be 24–45 m [3–5] and in whom 6MWT is associated with changes in pulmonary function and quality-of-life [16]; and in patients awaiting LTx, in whom it is associated with post-transplant survival [17]. A reduction of the decline in 6MWT was also observed in treated patients compared to placebo in pooled analyses of IPF trials [3–5], which may partly explain why 6MWT overall remained relatively stable during treatment in our cohort, next to the obvious beneficial effects of cardio-pulmonary rehabilitation is some patients. Although the LAS is actually not used in Belgium for prioritizing organ allocation, the calculated LAS (which includes FVC and 6MWT among other parameters) did not significantly change during pretransplant antifibrotic treatment in our cohort. An average LAS of 32 at the time of LTx in our study may seem fairly low for IPF patients, yet LAS was quite comparable between our treated patients and historical controls; and was in the same range (median of ±35) as previously described for IPF patients at LTx listing [18]. We therefore believe that our cohort indeed reflects the general population of IPF patients transplanted during the past 5–10 years. However, in the last few years, as seen in the US, an increase in LAS is also noted in our centre, with more sicker patients (LAS > 40) being listed for LTx [19].
No serious side effects were noted during antifibrotic therapy. However, significant weight loss occurred, which is most likely due to drug-induced anorexia or possibly due to respiratory cachexia in end-stage lung disease. Post-operatively, no problems with bleeding or thoracic wound healing were observed. One patient, treated with nintedanib; and three patients who had received pirfenidone developed, mostly mild and uneventful, anastomic airway complications. Intervention for anastomotic stenosis was needed for one case, which only occurred late-onset after prior fungal infection. Overall, it is unlikely that any of these anastomotic problems were directly related to prior antifibrotic treatment given the time of onset/clinical context of anastomotic complications, comparable anastomotic problems in the historical controls; and rather short half-life of both drugs (for pirfenidone 3 h, for nintedanib 9.5 h) [20, 21]. The short half-life of both antifibrotic drugs is important, as drug-interactions with calcineurin inhibitors, by altered hepatic (CYP3A4) metabolisation leading to changes in tacrolimus/cyclosporine trough levels, are a feared iatrogenic adverse event in LTx. However, hepatic metabolism of pirfenidone primarily occurs through the CYP1A2 enzyme; whereas nintedanib is mainly a substrate of P-glycoprotein (P-gp) and only weakly interferes with CYP3A4. This probably also explains why no major side effects due to drug-interactions with peri-operatively used drugs were noted in our cohort. Finally, long-term outcomes regarding pulmonary function and overall survival were overall good in our current case series, suggesting that antifibrotic agents can probably be safely given without deleterious effects on peri-operative or medium-term outcomes.
Possible limitations of the current study, of course, are its retrospective design, the small number of included patients; and historical controls as comparator for some outcomes, which of course limits interpretations regarding antifibrotic drug efficacy and safety. Also, disease severity ranged from mild to severe IPF, which may bias the observed effects of pretransplant antifibrotic therapy; and post-transplant evolution, including pulmonary function, may be biased by inclusion of some patients in various randomized clinical trials. Larger, preferably prospective, case-series are therefore undeniably needed to confirm our findings, especially for nintedanib additional safety data are needed before firmer conclusions can be made regarding its safety.
Conclusion
In summary, we conclude that antifibrotic drugs are probably safe in IPF patients undergoing LTx. By attenuating disease progression while awaiting LTx, these antifibrotics may perhaps further help to reduce the number of IPF patients dying on the waiting list.
Acknowledgments
Not applicable.
Funding
RV is supported by the Starting Grant (STG/15/023) and JY is supported by the Clinical Research Fund (KOF), UZLeuven, Belgium. WW and RV are senior research fellows of the Research Foundation Flanders (FWO), Belgium (12G8715N). GMV is supported by the FWO (G.0723.10, G.0679.12 and G.0679.12).
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to local Biobanking and legislation policy, but are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
The authors confirm that that the work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form in English or in any other language, without the written consent of the copyright holder.
Authors’ contributions
ID: performed data collection, wrote the paper and helped with its critical appraisal. WW: is responsible ILD physician during pretransplant period and helped with critical appraisal of the manuscript. JY: is responsible ILD physician during pretransplant period and helped with critical appraisal of the manuscript. EV: is responsible ILD pathologist during pretransplant period and helped with critical appraisal of the manuscript. GV: is responsible ILD physician during pretransplant period and responsible LTx physician during post-LTx period, helped with critical appraisal of the manuscript. RV: is responsible LTx physician during post-LTx period, performed design of the study, data collection, statistical analyses, and helped with critical appraisal of the manuscript. All authors read and approved the final manuscript.
Consent for publication
All patients gave informed consent for scientific publication of the data presented in this paper.
Ethics approval and consent to participate
The current study was approved by the Leuven University Hospital Ethical Review Board (S51577) and patients gave informed consent.
Abbreviations
- 6MWT
Six minute walking test
- BMI
Body mass index
- CLAD
Chronic lung allograft dysfunction
- CPR
Cardio-pulmonary rehabilitation
- DLCO
Diffusion capacity
- FDA
Food and Drug Administration
- FGF
Fibroblast growth factor
- FVC
Forced vital capacity
- ILD
Interstitial lung disease
- IPF
Idiopathic pulmonary fibrosis
- LAS
Lung allocation score
- LTx
Lung transplantation
- MDS
Macroscopic Diameter Sutures (MDS Classification)
- PDGF
Platelet-derived growth factor
- PGD
Primary graft dysfunction
- POD
Post-operative day
- TGF- β
Transforming growth factor –beta
- TLC
Total lung capacity
- UIP
Usual interstitial pneumonia
- VEGF
Vascular endothelial growth factor
Contributor Information
Isabelle Delanote, Email: isabelle.delanote@uzleuven.be.
Wim A. Wuyts, Email: wim.wuyts@uzleuven.be
Jonas Yserbyt, Email: jonas.yserbyt@uzleuven.be.
Eric K. Verbeken, Email: eric.verbeken@uzleuven.be
Geert M. Verleden, Email: geert.verleden@uzleuven.be
Robin Vos, Phone: + 32 16 341548, Email: robin.vos@uzleuven.be.
References
- 1.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Clinical Guideline Centre (UK) Diagnosis and management of suspected idiopathic pulmonary fibrosis: idiopathic pulmonary fibrosis. London: Royal College of Physicians (UK); 2013. [PubMed] [Google Scholar]
- 3.Noble PW, Albera C, Bradford WZ, Costabel U, Glassberg MK, Kardatzke D, CAPACITY Study Group et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377(9779):1760–9. doi: 10.1016/S0140-6736(11)60405-4. [DOI] [PubMed] [Google Scholar]
- 4.King TE, Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, ASCEND Study Group et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083–92. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 5.Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, INPULSIS Trial Investigators et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–82. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 6.Noble PW, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47(1):243–53. doi: 10.1183/13993003.00026-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazzei ME, Richeldi L, Collard HR. Nintedanib in the treatment of idiopathic pulmonary fibrosis. Ther Adv Respir Dis. 2015;9(3):121–9. doi: 10.1177/1753465815579365. [DOI] [PubMed] [Google Scholar]
- 8.Kistler KD, Nalysnyk L, Rotella P, Esser D. Lung transplantation in idiopathic pulmonary fibrosis: a systematic review of the literature. BMC Pulm Med. 2014;14:139. doi: 10.1186/1471-2466-14-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conte E, Gili E, Fagone E, Fruciano M, Iemmolo M, Vancheri C. Effect of pirfenidone on proliferation, TGF-β-induced myofibroblast differentiation and fibrogenic activity of primary human lung fibroblasts. Eur J Pharm Sci. 2014;58:13–9. doi: 10.1016/j.ejps.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Wollin L, Wex E, Pautsch A, Schnapp G, Hostettler KE, Stowasser S, et al. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1434–45. doi: 10.1183/09031936.00174914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yserbyt J, Dooms C, Vos R, Dupont LJ, Van Raemdonck DE, Verleden GM. Anastomotic airway complications after lung transplantation: risk factors, treatment modalities and outcome-a single-centre experience. Eur J Cardiothorac Surg. 2016;49(1):e1–8. doi: 10.1093/ejcts/ezv363. [DOI] [PubMed] [Google Scholar]
- 12.Paone G, Sebastiani A, Ialleni E, Diso D, Rose D, Quagliarini F, et al. A combined therapeutic approach in progressive idiopathic pulmonary fibrosis-pirfenidone as bridge therapy for ex vivo lung transplantation: a case report. Transplant Proc. 2015;47(3):855–7. doi: 10.1016/j.transproceed.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Riddell P, Minnis P, Ging P, Egan JJ. Pirfenidone as a bridge to lung transplantation in patients with progressive IPF. Thorax. 2014;69:A183. doi: 10.1136/thoraxjnl-2014-206260.370. [DOI] [Google Scholar]
- 14.Mortensen A, Cherrier L, Walia R. Lung transplantation on pirfenidone: a single center experience. J Heart Lung Transplant. 2016;35(4S):883. [Google Scholar]
- 15.Taniguchi H, Kondoh Y, Ebina M, Azuma A, Ogura T, Taguchi Y, Pirfenidone Clinical Study Group in Japan et al. The clinical significance of 5% change in vital capacity in patients with idiopathic pulmonary fibrosis: extended analysis of the pirfenidone trial. Respir Res. 2011;12:93. doi: 10.1186/1465-9921-12-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nathan SD, du Bois RM, Albera C, Bradford WZ, Costabel U, Kartashov A, et al. Validation of test performance characteristics and minimal clinically important difference of the 6-min walk test in patients with idiopathic pulmonary fibrosis. Respir Med. 2015;109(7):914–22. doi: 10.1016/j.rmed.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Castleberry AW, Englum BR, Snyder LD, Worni M, Osho AA, Gulack BC, et al. The utility of preoperative six-minute-walk distance in lung transplantation. Am J Respir Crit Care Med. 2015;192(7):843–52. doi: 10.1164/rccm.201409-1698OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, et al. Development of the new lung allocation system in the United States. Am J Transplant. 2006;6(5 Pt 2):1212–27. doi: 10.1111/j.1600-6143.2006.01276.x. [DOI] [PubMed] [Google Scholar]
- 19.Egan TM, Edwards LB. Effect of the lung allocation score on lung transplantation in the United States. J Heart Lung Transplant. 2016;35(4):433–9. doi: 10.1016/j.healun.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 20.ESBRIET® (pirfenidone) hard capsules, for oral use. electronic Medicines Compendium. Genentech. Accessed 12 Dec 2015.
- 21.OFEV® (nintedanib) capsules, for oral use. electronic Medicines Compendium. Boehringer Ingelheim. Accessed 12 Dec 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available due to local Biobanking and legislation policy, but are available from the corresponding author on reasonable request.


