Abstract
Lower family cohesion is associated with adolescent internalizing and externalizing problems. However, there are likely individual differences in youth's responses to family processes. For example, adolescents higher in negative emotional reactivity, who often exhibit elevated physiological responsivity to context, may be differentially affected by family cohesion. We explored whether youth's negative emotional reactivity moderated the relation between family cohesion and youth's symptoms and tested whether findings were consistent with the diathesis-stress model or differential susceptibility hypothesis. Participants were 651 adolescents (M = 12.99 ± .95 years old; 72% male) assessed at two time points (Time 1, ages 12–14; Time 2, age 16) in Pittsburgh, PA. At Time 1, mothers reported on family cohesion and youth reported on their negative emotional reactivity. At Time 2, youth reported on their symptoms. Among youth higher in negative emotional reactivity, lower family cohesion predicted higher symptoms than higher family cohesion, consistent with the diathesis-stress model.
Keywords: Negative emotional reactivity, Family cohesion, Internalizing symptoms, Externalizing symptoms, Differential susceptibility
Internalizing and externalizing symptoms often develop in adolescence, may persist into adulthood, and are associated with numerous negative sequelae (e.g., decreased academic achievement, peer rejection) (Keiley, Lofthouse, Bates, Dodge, & Pettit, 2003; Lösel & Slemming, 2012; Masten et al., 2005). Internalizing symptoms may manifest as social withdrawal, anxiety, and depression, whereas externalizing problems often manifest as hyperactivity, aggression, and destructive behavior. Given the negative sequelae associated with internalizing and externalizing problems, it is critical to identify factors associated with risk or resilience for symptom development, which can inform intervention and prevention efforts.
One contextual factor that may influence risk for internalizing and externalizing symptoms among adolescents is family cohesion. Although many studies have examined links between parent–child relationships and youth symptoms (e.g., Bates, Pettit, Dodge, & Ridge, 1998; Pluess & Belsky, 2010; Zarra-Nezhad et al., 2014), family members are affected by each other's emotions and behaviors which, in turn, may influence how members of the family function individually (Cavendish, Montague, Enders, & Dietz, 2014). Family cohesion can be defined as shared affection, support, commitment, and helpfulness that family members exhibit towards each other (Barber & Buehler, 1996; Moos & Moos, 1974). This family process may mitigate risk for symptoms during adolescence, a developmental period characterized by vast changes in neurobiology, emotion, and social interactions (Barber & Buehler, 1996; Drabick & Steinberg, 2011). Cohesive families may have more harmonious interactions and be dedicated to amicably solving problems. In highly cohesive families, family members may feel a greater commitment to helping each other (e.g., adolescents), which could involve assisting youth in responding adaptively to social challenges or modeling how to manage negative emotions (Morris, Silk, Steinberg, Myers, & Robinson, 2007; Richmond & Stocker, 2006). Among less cohesive families, some family members may not feel a sense of belonging, may feel less dedicated to supporting youth within the family, or may experience poorer communication and more contentious disputes. Youth in these settings may thus experience heightened levels of emotional distress, negative affect, and emotion dysregulation (Carthy, Horesh, Apter, & Gross, 2010; Smets & Hartup, 1998).
Not all children are affected in the same manner by family cohesion, suggesting that child-specific attributes, such as negative emotional reactivity, may influence these relations. Similar to the construct of negative affectivity (i.e., the degree to which one experiences emotions such as sadness, fear, or anger) (Nigg, 2006; Watson & Clark, 1984), negative emotional reactivity refers to one's propensity to exhibit higher arousal when exposed to sensory stimuli, negative emotions (e.g., fear), and negative cognitions (e.g., helplessness) (Caprara et al., 1985; Davidson, 1998). Youth higher in negative emotional reactivity may experience higher levels of hypervigilance and interpret benign or ambiguous situations as harmful, which may increase their distress, feelings of vulnerability, autonomic arousal, and anxiety symptoms (Buehler & Welsh, 2009; Schneiders et al., 2006). Youth higher in negative emotional reactivity may also become overwhelmed with their emotional states, which may prompt aggression to mitigate stressors that are perceived as threatening (Sanson, Hemphill, & Smart, 2004; Zeman, Shipman, & Suveg, 2002). In contrast, youth lower in negative emotional reactivity may experience higher sensory thresholds, decreased physiological arousal, and lower negative emotions and cognitions across contexts.
Work examining whether youth varying in negative emotional reactivity are differentially affected by family cohesion during adolescence is limited. Research to date has indicated that relative to youth lower in negative emotional reactivity, youth higher in negative emotional reactivity are at risk for internalizing and externalizing problems when exposed to negative family processes (e.g., interparental or family conflict) during childhood (Buehler & Welsh, 2009; Davies, Cicchetti, & Martin, 2012; Davies, Sturge-Apple, Cicchetti, Manning, & Zale, 2009). However, it is unclear whether positive family processes, such as family cohesion, reduce risk for internalizing and externalizing problems among youth higher in negative emotional reactivity during adolescence, a developmental period that may increase youth's stress responsivity and confer risk for emotional and behavioral problems (Drabick & Steinberg, 2011).
Both the diathesis-stress model and differential susceptibility hypothesis can be considered in determining whether adolescents varying in negative emotional reactivity are differentially responsive to family cohesion. Paralleling Luthar, Cicchetti, and Becker's (2000) vulnerability-reactive model, which suggests that individuals possess attributes that increase risk for maladjustment in the context of environmental risk, the diathesis-stress model posits that individuals who possess certain attributes (e.g., higher negative emotional reactivity) are at an increased risk of experiencing impairment in the context of an environmental stressor (e.g., lower family cohesion) (Monroe & Smith, 1991; Zuckerman, 1999). Studies that have investigated support for the diathesis-stress and differential susceptibility hypothesis indicate that the interaction between temperament and family/parenting variables in late childhood or adolescence and associations with adolescent internalizing and externalizing behaviors supports the diathesis-stress model (Rabinowitz, Drabick, Reynolds, Clark, & Olino, 2016; Rioux et al., 2016). Indeed, when youth with certain temperamental features (e.g., lower temperamental flexibility, impulsivity, effortful control) are exposed to more negative parenting and family behaviors (e.g., lower parental support, acceptance, higher family conflict) during late childhood, they exhibit elevated adolescent internalizing and externalizing symptoms (Rabinowitz et al., 2016; Rioux et al., 2016; Stice & Gonzales, 1998).
The differential susceptibility hypothesis suggests that children's individual differences may render them more reactive to negative and positive environmental influences (Pluess & Belsky, 2010). Indeed, the differential susceptibility hypothesis posits that youth with certain attributes, such as negative emotional reactivity, may experience worse outcomes when exposed to adverse conditions; however, in contrast to the diathesis-stress model, the differential susceptibility hypothesis suggests that youth with those attributes also will exhibit enhanced adjustment when exposed to positive environments (Belsky, Bakermans-Kranenburg, & van-IJzendoorn, 2007; Boyce, 2015). Many studies that have substantiated the differential susceptibility hypothesis have examined the interaction of temperament and parenting characteristics assessed in early and middle childhood in the prediction of childhood and adolescent adjustment. In support of the differential susceptibility hypothesis, when exposed to higher positive (e.g., high caregiver sensitivity) and lower negative (e.g., lower coercive parenting) parent–child behaviors in early or middle childhood, children with difficult temperamental features (e.g., lower self-regulation, higher negative emotionality) manifested fewer externalizing and internalizing problems; however, when youth higher in difficult temperamental features were exposed to lower positive and higher negative parenting, these youth experienced higher levels of behavior problems (Bradley & Corwyn, 2008; Rioux et al., 2016; van Zeijl et al., 2007).
Youth higher in negative emotional reactivity may be at risk for symptoms if they experience contextual stress, consistent with the diathesis-stress model. Nevertheless, youth higher in negative emotional reactivity may also possess attributes that make them more likely to benefit from positive contexts. Youth lower in negative emotional reactivity tend to use top-down, assimilative processing, which refers to using one's preconceived ideas based on past experiences (i.e., schemas) to guide one's interpretation of the external world (Bless & Fiedler, 2006; Fiedler, 2002). In contrast, youth higher in negative emotional reactivity often use bottom-up, accommodative processing characterized by the modification of one's cognitive concepts based on external stimuli. Youth who use accommodative processes tend to (a) be more discriminatory; (b) be more detail-oriented; (c) remember specific, rather than global, aspects of an environment; and (d) have greater memory encoding (Forgas, 2013). The increased cognitive processing of stimuli, elevated biological responsiveness, and more intense emotional reactions to stimuli, may make youth higher in negative emotional reactivity disproportionately affected by family cohesion.
In the current study, we sought to address a number of gaps. First, although many studies have examined parent–child dynamics among youth varying in temperamental features (e.g., van Zeijl et al., 2007), we examined whether negative emotional reactivity interacted with a broader positive family process, specifically family cohesion, to prospectively predict adolescent internalizing and externalizing problems. Second, we explored whether child negative emotional reactivity moderated the relation between family cohesion and adolescent adjustment, and whether findings were consistent with the diathesis-stress model or differential susceptibility hypothesis, something no studies to date have explored. Third, we included multiple informants (i.e., mother and youth reports) to minimize mono-rater biases.
Consistent with both the diathesis-stress and differential susceptibility hypothesis, we hypothesized that adolescents higher in negative emotional reactivity would experience greater internalizing and externalizing problems than adolescents lower in negative emotional reactivity when exposed to lower family cohesion. Specific to the differential susceptibility hypothesis, we also expected that adolescents higher in negative emotional reactivity would show lower rates of internalizing and externalizing problems than adolescents lower in negative emotional reactivity in the context of higher family cohesion.
Method
Participants
The sample was recruited from the Center for Education and Drug Abuse Research a longitudinal study conducted to identify youth who may be at risk for substance use disorders (SUD). Fathers who had a child aged 10–12 years were eligible to participate and were further screened for inclusion and exclusion criteria. Youth were grouped into one of three categories according to their biological father's lifetime prevalence of mental disorders: (a) paternal history of SUD (11%), (b) paternal history of other psychiatric disorder not including SUD (44%), or (c) no lifetime paternal history of psychiatric disorder (45%). Biological fathers were recruited through substance dependence and psychiatric treatment programs; courts; and newspaper, television, and radio advertisements. For the purposes of this study, youth with fathers were assigned to one of two groups characterized by either (a) no lifetime history of SUD or psychiatric disorder (44%) or (b) a lifetime diagnosis of SUD or other psychiatric disorder (56%) based on the Structured Clinical Interview for DSM-III-R (Spitzer, Williams, & Gibbon, 1987). Recruitment sources and procedures, as well as inclusionary and exclusionary criteria, are described in detail elsewhere (Tarter and Vanyukov, 2001).
Data from the present study were drawn from assessments when youth were 12–14 years old (Time 1) and 16 years old (Time 2). At Time 1, participants included 651 youth (M = 12.99 ± .95 years old; range = 11–15 years; 72% male; 76% Caucasian, 21% African American, 3% “multiracial”). At Time 2, participants included 631 adolescents (M = 15.50 ± .56 years; range = 15–17 years; 72% male; 76% White, 22% African American, 2% multiracial). Time 2 assessments occurred an average of 2.51 years after Time 1 assessments (range = 1–5 years). The sample contains more males than females because recruitment of females began four years after the Center for Education and Drug Abuse Research project was underway.
Procedure
The study was approved by a University Institutional Review Board. Participants were provided with a detailed description of the study before study participation. Written informed consent was obtained from parents and assent was obtained from children. Participants were informed that their privacy was protected by a Certificate of Confidentiality issued to the Center for Education and Drug Abuse Research from the National Institute on Drug Abuse. Parents and youth were financially compensated after completion of each visit.
Measures
Family cohesion
At Time 1, mothers reported on the extent of family cohesion by completing the Family Environment Scale (FES; Moos & Moos, 1974). The FES is a 90-item self-report measure that is commonly used to assess family social environment. The family cohesion scale includes 10 items (α = .72). Mothers rated whether certain family behaviors were characteristic of their own families (1 = true, 0 = false). A sample item is, “Family members really help and look out for one another.” Higher scores indicate higher levels of family cohesion. The FES has demonstrated good internal and external validity, moderate reliability, and factorial validity (Boyd, Gullone, Needleman, & Burt, 1997; Oliver, Handal, Enos, & May, 1988; Sanford, Bingham, & Zucker, 1999).
Negative emotional reactivity
At Time 1, youth reported on their negative emotional reactivity using the Emotional Susceptibility Scale (Caprara et al., 1985). The Emotional Susceptibility Scale includes 40 items rated on a scale from 1 = completely true to 6 = completely false (α = .90). Higher scores reflect higher negative emotional reactivity. Sample items are “Sometimes I am afraid I will lose control over my feelings;” “When I am moved, I find it difficult to hold back my tears;” and “I have often felt upset.” The Emotional Susceptibility Scale has demonstrated adequate internal consistency and test-retest reliability (Caprara et al., 1985).
Youth-reported symptoms
At Time 2, we used the internalizing and externalizing composites of the Youth Self-Report measure (YSR; Achenbach, 1991). The internalizing composite includes items from the anxious/depressed, withdrawn, and somatic symptoms scales (boys α = .84; girls α = .89). A sample item is, “I feel lonely.” The externalizing composite includes items from the aggression and delinquency scales (boys α = .87; girls α = .85). A sample item is “I argue a lot.” Higher scores indicate higher symptom levels. The YSR has demonstrated extensive reliability and validity (Achenbach & Rescorla, 2001).
Statistical analyses
Descriptive statistics and bivariate correlations were conducted to investigate associations among independent and outcome variables using SPSS Version 23. For child sex, females were coded as “0” and males were coded as “1.” A child ethnicity variable was coded with Caucasian adolescents as “0” and ethnic-minority adolescents as “1.” A father diagnosis variable was created by coding fathers with no SUD or psychiatric problems as “0” and fathers with a history of SUD or other psychiatric disorder as “1.”
The primary analyses were conducted using Mplus Version 7.11, which uses Full Information Maximum Likelihood (FIML) estimation to address missing data (Muthén & Muthén, 1998–2014). FIML uses all available data to estimate model parameters, but does not impute values. This approach allows for the usage of participants with missing data in model estimation and generates smaller errors in parameter estimates and standard errors relative to other missing data strategies (e.g., complete casewise analysis or listwise deletion, complete case analyses or pairwise deletion), which may introduce bias (Graham, 2009; Little & Rubin, 2002; Newman, 2003).
We conducted four regression analyses to examine (a) the main effects of family cohesion and child negative emotional reactivity, and (b) whether child negative emotional reactivity moderated the relation between family cohesion and adolescent internalizing or externalizing problems. In each regression equation, Step 1 included child age, sex, ethnicity, father diagnostic status, family cohesion, and child negative emotional reactivity assessed at Time 1. Step 2 included Step 1 variables, and the family cohesion × child negative emotional reactivity cross-product interaction term. To reduce multicollinearity, the independent variables were z-scored (M = 0, SD = 1) before inclusion in the regression equations and interaction terms were created from the z-scored variables (Aiken & West, 1991).
Several factors were considered in evaluating support for the diathesis-stress model and differential susceptibility hypothesis, consistent with the most recent recommended guidelines (Belsky & Pluess, 2009; Belsky et al., 2007; Roisman et al., 2012). More specifically, we examined (a) associations between the moderator (negative emotional reactivity) and the outcomes (internalizing and externalizing symptoms); (b) associations between the predictor (family cohesion) and the moderator (negative emotional reactivity); (c) the visual display of the interaction; (d) regions of significance (RoS) values and the proportion of the sample above and below the upper and lower bounds of RoS; and (e) the significance and steepness of each of the slopes (i.e., higher and lower negative emotional reactivity).
Significant associations between the moderator (negative emotional reactivity) and outcome (symptoms) are supportive of the diathesis-stress model (Belsky et al., 2007), whereas no significant associations between the moderator and outcomes are supportive of differential susceptibility (Belsky et al., 2007). In addition, the predictor (family cohesion) and moderator (negative emotional reactivity) should be independent of each other. However, if significant correlations occur between family cohesion and negative emotional reactivity, further analyses can be run regressing the moderator on the predictor as outlined by Roisman et al. (2012). The residuals from these regressions can be used in moderation analyses to control for correlations among negative emotional reactivity and family cohesion. Because there was a small correlation between family cohesion and negative emotional reactivity, ancillary regression analyses were conducted that controlled for these residuals.
In addition, we plotted significant interactions. Visual support for the diathesis-stress model is reflected in an ordinal (fan-shaped) interaction, whereas support for the differential susceptibility hypothesis is reflected in a disordinal (cross-over) interaction. In addition to considering the visual display of the interactions, post-hoc probing of significant interactions were conducted using RoS, a statistical tool that provides a range of values of the predictor variable for which the moderator is significantly associated with the outcome (Preacher, Curran, & Bauer, 2006). This method provides upper and lower bounds of RoS of the predictor variable (family cohesion) below and above which the regression lines for the two groups (higher and lower negative emotional reactivity) significantly differ on the outcome variables (internalizing or externalizing symptoms). In the present study, we investigated interaction effects using ±2 SD below and above the mean of the standardized predictor (family cohesion) to capture 95% of the sample (Roisman et al., 2012).
In addition to determining the RoS, we also examined the number of cases or proportion affected (PA index) in the sample that have values above or below the RoS values. Support for differential susceptibility may occur if over 16% of the cases are both above and below the upper and lower bound of RoS (Roisman et al., 2012). Support for the diathesis-stress model occurs when over 16% of the cases fall below the lower bound of RoS. When fewer than 2% of cases fall above the upper or below the lower bound of RoS, support for differential susceptibility or the diathesis-stress model cannot be concluded. The specific thresholds of 16% and 2% of cases were used as they reflect 1 and 2 SD, respectively, from the mean of a normal distribution.
Lastly, simple slopes were computed to reflect adolescents higher in negative emotional reactivity (+1 SD above the mean of child negative emotional reactivity) and adolescents lower in negative emotional reactivity (−1 SD below the mean of child negative emotional reactivity) to test whether the relation between the moderator (negative emotional reactivity) and the outcome (symptoms) was significantly different from zero and dependent on the predictor variable (family cohesion) (Aiken & West, 1991; Roisman et al., 2012). Support for differential susceptibility and the diathesis-stress model may occur if the slope of one of the groups is significantly different from zero and steeper than the slope for the other group (Belsky et al., 2007).
Results
Participants who were missing any data on Time 1 and 2 assessments (n = 106) differed from those with complete data (n = 547) in terms of age, t(651) = 2.80, p = .005, Cohen's d = .29; child sex, χ2(1) = 4.20, p = .026, ϕ = .07; father diagnostic status, χ2(1) = 5.51, p = .019, ϕ = .08; and child ethnicity, χ2(1) = 4.92, p = .027, ϕ = .08. Thus, individuals with missing data were more likely to be younger, female, identified as ethnic minority, and to have a father without a psychiatric problem or SUD. No additional differences were found for participants with and without missing data (all t's < .97, all p's > .34, all Cohen's ds < .13).
Bivariate correlations, means, standard deviations, and ns for the study variables are presented in Table 1. Internalizing and externalizing symptoms were moderately correlated. There was a small negative correlation between family cohesion and adolescent negative emotional reactivity. There was a small positive correlation between negative emotional reactivity and internalizing and externalizing symptoms, which is supportive of the diathesis-stress model.
Table 1.
Bivariate correlations, means, SDs, ranges, and n's for study variables.
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Child age | – | ||||
| 2. Negative emotional reactivity | .01 | – | |||
| 3. Family cohesion | .01 | −.19** | – | ||
| 4. Internalizing symptoms | .03 | .28** | −.16** | – | |
| 5. Externalizing symptoms | .04 | .21** | −.16** | .53** | – |
| M | 12.99 | 88.79 | 7.15 | 8.02 | 10.51 |
| SD | .95 | 20.29 | 1.96 | 6.99 | 7.43 |
| Range | 11–15 | 30–169 | 0–9 | 0–32 | 0–45 |
| n | 653 | 644 | 615 | 614 | 622 |
p < .01.
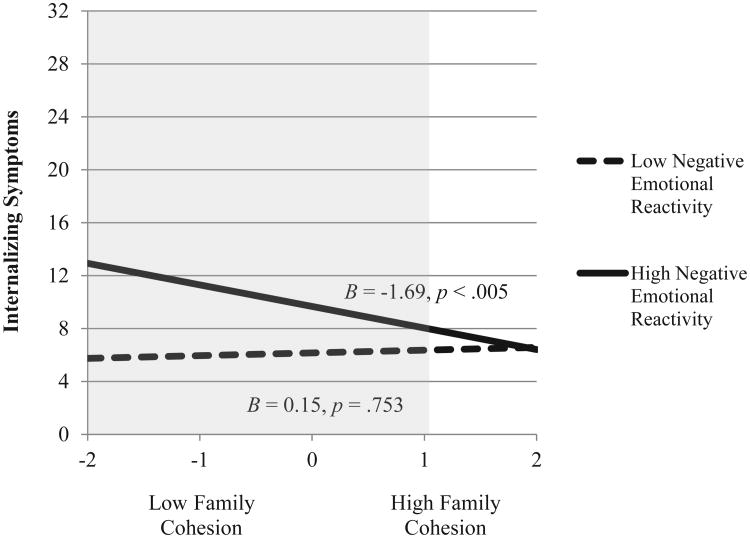
Internalizing symptoms
There was a negative main effect for family cohesion and a positive main effect for child negative emotional reactivity on internalizing symptoms (top of Table 2). The family cohesion × child negative emotional reactivity interaction predicted internalizing problems.1 Plotting this interaction term revealed an ordinal interaction, supportive of the diathesis-stress model (Fig. 1).
Table 2.
Summary of hierarchical regression analyses predicting internalizing and externalizing symptoms from family cohesion and child negative emotional reactivity.
| Variable | B | SE B | β | R2 | f2 |
|---|---|---|---|---|---|
| Internalizing symptoms | |||||
| Step 1 | .14 | .16 | |||
| Sex | 3.35 | .60 | .22** | ||
| Age | .10 | .29 | .01 | ||
| Ethnicity | −.26 | .63 | −.02 | ||
| Father diagnostic status | −.95 | .54 | −.07 | ||
| Family cohesion | −.97 | .31 | −.13** | ||
| Negative emotional reactivity | 1.60 | .28 | .23** | ||
| Step 2 | .16 | .19 | |||
| Sex | 3.44 | .59 | .22** | ||
| Age | .07 | .29 | .01 | ||
| Ethnicity | −.22 | .63 | −.01 | ||
| Father diagnostic status | −.88 | .54 | −.06 | ||
| Family cohesion | −.86 | .31 | −.11** | ||
| Negative emotional reactivity | 1.55 | .28 | .22** | ||
| Family cohesion × Negative emotional reactivity | −.95 | .30 | −.13** | ||
| Externalizing symptoms | |||||
| Step 1 | .07 | .08 | |||
| Sex | −.16 | .65 | −.01 | ||
| Age | .32 | .32 | .04 | ||
| Ethnicity | −.35 | .69 | −.02 | ||
| Father diagnostic status | −1.46 | .60 | −.10* | ||
| Family cohesion | −.95 | .34 | −.12** | ||
| Negative emotional reactivity | 1.40 | .31 | .19** | ||
| Step 2 | |||||
| Sex | −.10 | .65 | −.01 | .08 | .09 |
| Age | .29 | .31 | .04 | ||
| Ethnicity | −.32 | .69 | −.02 | ||
| Father diagnostic status | −1.40 | .60 | −.09* | ||
| Family cohesion | −.88 | .34 | −.11* | ||
| Negative emotional reactivity | 1.37 | .31 | .18** | ||
| Family cohesion × Negative emotional reactivity | −.65 | .33 | −.08* | ||
p < .05,
p < .01.
Fig. 1.
Relation between family cohesion among children with high (+1 SD) and low (−1 SD) negative emotional reactivity in predicting internalizing symptoms. The shaded area represents the regions of significance (lower bound = 1.00).
There was only a lower bound of RoS observed at 1.00, which corresponds to a raw score of 9.11. The shaded area in Fig. 1 illustrates the RoS. The number of children with family cohesion scores below 1.00 was 549 (85% of sample). These findings indicate that the two regression lines (high and low negative emotional reactivity) were significantly different for all possible scores when family cohesion was below 1.00 SDs from the raw family cohesion mean of 9.11. Given that over 16% of the cases fell below the lower bound of RoS, this finding is supportive of the diathesis-stress model.
Simple slope analyses indicated among children higher in negative emotional reactivity, lower family cohesion was associated with heightened internalizing problems compared to higher family cohesion. Children lower in negative emotional reactivity exhibited relatively equivalent and low internalizing symptoms regardless of family cohesion levels. These findings are consistent with the diathesis-stress model.
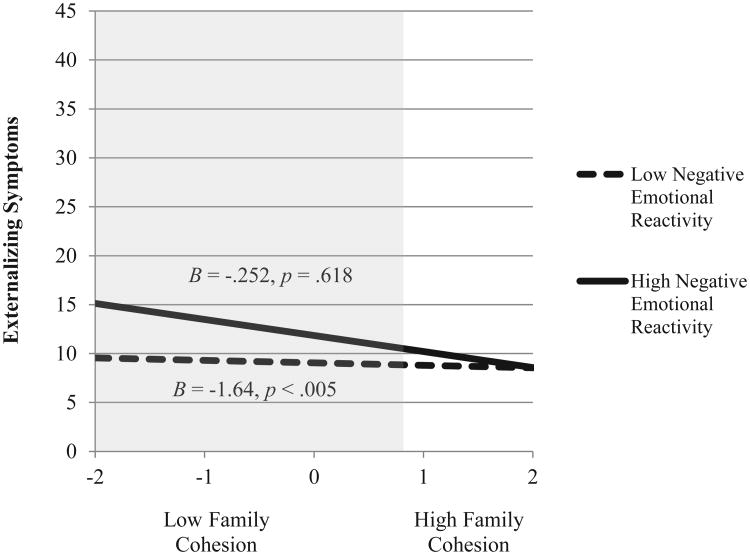
Externalizing symptoms
There was a negative main effect for family cohesion and a positive main effect for child negative emotional reactivity on externalizing behaviors (bottom of Table 2). The family cohesion × child negative emotional reactivity interaction predicted externalizing symptoms. Similar to internalizing symptoms, plotting of the interaction term indicated an ordinal shape, supportive of the diathesis-stress model (Fig. 2).
Fig. 2.
Relation between family cohesion among children with high (+1 SD) and low (−1 SD) negative emotional reactivity in predicting externalizing symptoms. The shaded area represents the regions of significance (lower bound = .83).
There was only a lower bound of RoS observed at .83, which corresponds to a raw score of 8.78 (Fig. 2). The number of children with family cohesion scores below .83 was 518 (80% of sample). These findings indicate that the two regression lines (high and low negative emotional reactivity) were significantly different for all possible scores when family cohesion was below .83 SDs from the raw family cohesion mean of 8.78. The large percentage of cases that fell below the lower bound of RoS is supportive of the diathesis-stress model.
Among youth higher in negative emotional reactivity, lower family cohesion was associated with greater externalizing symptoms than higher family cohesion. Youth lower in negative emotional reactivity exhibited low externalizing symptoms regardless of family cohesion levels. Findings are in line with the diathesis-stress model.
Discussion
Although previous studies have examined the impact of parenting processes on the adjustment of adolescents varying in negative emotional reactivity (e.g., Buehler & Welsh, 2009; Davies et al., 2009), few studies have examined the impact of broader family processes, such as family cohesion, among youth varying in negative emotional reactivity in the prediction of adolescent internalizing and externalizing symptoms. Our results indicate that among adolescents higher in negative emotional reactivity, lower family cohesion predicted greater internalizing and externalizing symptoms than did higher family cohesion. Among adolescents lower in negative emotional reactivity, symptom levels were similar regardless of family cohesion levels. Although youth with higher negative emotional reactivity displayed attenuated symptoms when exposed to higher family cohesion, they did not exhibit lower symptoms compared to youth lower in negative emotional reactivity. Thus, our findings are consistent with the diathesis-stress model.
The present results are consistent with past research indicating that the interaction of child temperament and family features assessed in late childhood and associations with adolescent internalizing and externalizing symptoms is consistent with the diathesis-stress model (Rioux et al., 2016). Findings from our work are also in line with studies showing that poorer parenting and lower family functioning predicted higher internalizing and externalizing problems among youth with difficult temperamental features (Rabinowitz et al., 2016). Families lower in cohesion may have poorer communication and may feel less supported by one another; in these contexts, family members may be less effective in decreasing distress among youth, such as youth higher in negative emotional reactivity. Less cohesive families may also exhibit higher interparental, sibling, or parent–adolescent conflict (Baer, 2002). Higher levels of conflict may be particularly harmful among youth higher in negative emotional reactivity as these youth may manifest heightened autonomic nervous system functioning and helplessness when faced with a stressor (Caprara et al., 1985), increasing risk for symptoms.
Youth lower in negative emotional reactivity displayed lower levels of symptoms regardless of family cohesion levels. Consistent with Luthar's protective-stabilizing model (2000), lower negative emotional reactivity may be protective again symptom development across contexts. These youth may exhibit lower negative affective states (e.g., fear), and be less autonomically aroused and responsive to external stimuli such as family interactions. In contrast to youth lower in negative emotional reactivity, exposure to higher levels of family cohesion among youth higher in negative emotional reactivity was associated with a mitigation of internalizing and externalizing symptoms. Youth higher in negative emotional reactivity may display heightened sensitivity to sensory stimulation and thus, may be more affected by contextual influences consistent with biological sensitivity to context models (Aron, Aron, & Jagiellowicz, 2012; Boyce & Ellis, 2005). More cohesive families may provide greater warmth and support, which may help youth higher in negative emotional reactivity modulate negative emotional/cognitive states and elevated physiological arousal (Morris et al., 2007). Moreover, positive family interactions may help youth higher in negative emotional reactivity to develop positive internal representations of others, which may decrease the risk of these youth feeling fearful or threatened in interpersonal interactions, mitigating risk for symptoms (Cummings & Davies, 1996).
Although youth higher in negative emotional reactivity evidenced attenuated symptoms when exposed to higher family cohesion, they did not exhibit lower symptoms than did youth lower in negative emotional reactivity, which would have been necessary to support the differential susceptibility hypothesis. There are several potential explanations to account for the lack of differential susceptibility support. Although family members in cohesive families may be willing to support one another, adolescents higher in negative emotional reactivity may require more direct emotion regulation strategies from parents. Given that adolescence is often associated with increases in both negative emotions and physiological responses to stressors (Gilbert, 2012), these changes may contribute to dysregulation among youth higher in negative emotional reactivity. More direct parental modeling of effective coping strategies and support for modifying negative cognitions may decrease adolescents' physiological arousal and improve their regulation skills.
Relative to earlier developmental periods, family interactions with adolescent youth generally become more conflictual as adolescents seek more autonomy; these parent–child dynamics may diminish the positive influence of family cohesion on mitigating youth's symptoms above and beyond youth lower in negative emotional reactivity (Granic, Dishion, Hollenstein, & Patterson, 2003). Further, adolescents higher in negative emotional reactivity may exhibit greater social reticence and peer rejection because of their difficulty in modulating affective and cognitive states. These peer difficulties may exacerbate risk for symptoms and reduce the positive effects of a cohesive family on youth's symptoms (Iyer, Kochenderfer-Ladd, Eisenberg, & Thompson, 2010). It is also possible that living in a cohesive family is not enough to attenuate risk for symptoms among youth higher in negative emotional reactivity relative to youth lower in negative emotional reactivity. That is, the cumulative influences of positive contextual factors (e.g., teacher support, neighborhood cohesion) may provide the sufficient resources necessary for youth higher in negative emotional reactivity to exhibit lower symptoms than youth lower in negative emotional reactivity. Last, in the present study, mothers reported on family cohesion. Relative to other family members (e.g., fathers), mothers may be more interested in maintaining family harmony and may view the expression of both positive and negative emotions among youth higher in negative emotional reactivity as a reflection of positive family functioning (Garside & Klimes-Dougan, 2002). Thus, mothers may overestimate the level of cohesion within their families (Garside & Klimes-Dougan, 2002; Klimes-Dougan et al., 2007).
The present study has several strengths. First, the current sample is relatively large and diverse. Second, we explored whether youth negative emotional reactivity moderated the relation between family cohesion and adolescent internalizing and externalizing symptoms. This research may help determine whether youth varying in negative emotional reactivity are at differential risk for symptoms in the context of higher and lower family cohesion, which can inform intervention work. Future work should incorporate additional forms of assessments (e.g., observations) and informants (e.g., fathers, children) of family processes, youth's negative emotional reactivity, and symptoms. Using multiple informants may elucidate whether differences in family members' perspectives have greater predictive validity for youth's symptoms. Third, we examined whether youth negative emotional reactivity moderated the relations between family cohesion and youth symptoms during adolescence, a developmental period characterized by diverse neurobiological, physical, and social changes, whereby the family environment may play a key role in influencing symptom development (Morris et al., 2007). Fourth, we investigated whether moderation findings were consistent with the diathesis-stress and differential susceptibility hypothesis to identify whether adolescents higher in negative emotional reactivity benefited from positive family interactions above and beyond youth lower in negative emotional reactivity. Fifth, we considered several criteria in evaluating support for the diathesis-stress and differential susceptibility hypothesis. Indeed, the consideration of several factors (e.g., correlations between family cohesion and negative emotional reactivity, the shape of the plotted interaction term) allowed us to more accurately assess whether our findings were consistent with the theoretical models referenced above.
There are, however, some limitations of the present study. First, participants with missing data differed from participants with complete data as they were more likely to be younger, female, identified as ethnic minority, and the child of a father without a lifetime psychiatric diagnosis; however, FIML was used, which employs all available data to estimate model parameters based on the observed data. Second, the duration of assessments between Time 1 and Time 2 were variable (M = 2.51 years; range = 1–5 years). Thus, potential maturation of participants or different experiences during the duration between assessments may have differentially influenced Time 2 reports. Third, youth-reported symptoms at Time 1 were unavailable; thus, it is unclear whether and to what extent the predictor variables contribute over and above earlier symptom levels to predict the outcomes of interest. Future studies should investigate the impact of family features among youth varying in negative emotional reactivity using an autoregressive design (Stoolmiller & Bank, 1995) that could include bidirectional and prospective relations among family processes, negative emotional reactivity, and youth's symptoms. This approach may elucidate whether (a) family processes, negative emotional reactivity, and/or youth's psychological problems interact or otherwise exacerbate each other; and (b) some adolescents exhibit greater changes in symptoms as a function of family processes and their negative emotional reactivity. Fifth, the sample was recruited to represent children who were at differential risk for developing substance use problems. Thus, the generalizability of the current results may be limited. Future research should attempt to replicate the present findings in non-selected (e.g., community) or clinical samples to evaluate the generalizability of these relations.
Sixth, to evaluate support for the diathesis-stress and differential susceptibility models, we considered the absence of or lower symptom levels as an indicator of positive social and emotional adjustment. Although many studies have similarly evaluated support for the differential susceptibility hypothesis using negative indices of youth adjustment (e.g., Hastings et al., 2015; Musci et al., 2015), it is critical also to consider positive indices of adjustment as the absence of symptoms is not necessarily a reflection of positive adjustment (Keyes, Myers, & Kendler, 2010; Pluess, 2015). Indeed, consistent with the Positive Psychology and Positive Youth Development perspectives, the consideration of youth's strengths and ecological supports may help identify factors that contribute to youth flourishing (Snyder, Lopez, & Pedrotti, 2010). Adolescents with higher levels of positive functioning may be able to more effectively contribute to their own well-being, their families, and their communities (Lerner, Dowling, & Anderson, 2003). Thus, future research should identify whether youth higher in negative emotional reactivity exhibit more positive outcomes (e.g., social and emotional competence) in the context of higher family cohesion, which can inform assessments and interventions aimed at bolstering adolescents' positive adjustment. Future research should also include more positive indices of social and emotional functioning (e.g., prosocial behaviors, life satisfaction) when evaluating support for the diathesis-stress and differential susceptibility hypothesis.
The present study contributes to the literature by exploring the effects of a positive contextual factor, specifically family cohesion, on internalizing and externalizing symptoms among adolescents varying in negative emotional reactivity. Results support the diathesis-stress model as youth higher in negative emotional reactivity displayed higher internalizing and externalizing symptoms than did youth lower in negative emotional reactivity in the context of lower family cohesion. Although adolescents higher in negative emotional reactivity evidenced attenuated internalizing and externalizing problems when exposed to higher family cohesion, they did not exhibit lower symptoms than adolescents lower in negative emotional reactivity. As such, findings do not support the differential susceptibility hypothesis. Given that youth higher in negative emotional reactivity may be more sensitive to context, prevention and intervention programs should target the broader family system, as higher levels of cohesion may attenuate youth's risk for symptoms. Family-based interventions should attempt to ensure that family members feel a sense of connectedness to the larger family system. Such an approach may encourage family members to work together and help youth higher in negative emotional reactivity modulate their arousal and emotional/cognitive states. Future work should also explore whether other child-specific features (e.g., emotion regulation) influence the relations among negative emotional reactivity, family cohesion, and the youth's symptoms. This work can inform intervention and prevention efforts aimed at reducing risk for youth psychological symptoms and improving their adaptive functioning.
Acknowledgments
We thank all study participants, in addition to Dr. Ralph Tarter, the Principal Investigator of the current project, Center for Education and Drug Abuse Research (CEDAR). We also thank the National Institute on Drug Abuse (NIDA) for funding for this work (P50 DA 005605). Lastly, we are grateful to Steve Knopf for his assistance with compiling the data.
Footnotes
Given a correlation between negative emotional reactivity and family cohesion, we ran regressions using the residuals from these regressions to control for these correlations. The significance of the interaction terms were similar with and without the inclusion of the residuals in predicting internalizing (β = −.13, p = .002) and externalizing (β = −.08, p = .052) symptoms.
This research was supported in part by NIDA grant P50 DA 005605 awarded to Ralph E. Tarter.
References
- Achenbach TM. Manual for the child behavior checklist/4-18 and 1991 profile. Burlington, VT, US: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. The manual for the ASEBA school-age forms & profiles. Burlington, VT, US: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, California, US: Sage; 1991. [Google Scholar]
- Aron EN, Aron A, Jagiellowicz J. Sensory processing sensitivity: A review in the light of the evolution of biological responsivity. Personality and Social Psychology Review. 2012;16:262–282. doi: 10.1177/1088868311434213. http://dx.doi.org/10.1177/1088868311434213. [DOI] [PubMed] [Google Scholar]
- Baer J. Is family cohesion a risk or protective factor during adolescent development? Journal of Marriage and Family. 2002;64:668–675. http://dx.doi.org/10.1111/j.1741-3737.2002.00668.x. [Google Scholar]
- Barber BK, Buehler C. Family cohesion and enmeshment: Different constructs, different effects. Journal of Marriage and the Family. 1996;58:433–441. http://dx.doi.org/10.2307/353507. [Google Scholar]
- Bates JE, Pettit GS, Dodge KA, Ridge B. Interaction of temperamental resistance to control and restrictive parenting in the development of externalizing behavior. Developmental Psychology. 1998;34:982–995. doi: 10.1037//0012-1649.34.5.982. http://dx.doi.org/10.1037/0893-3200.21.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Bakermans-Kranenburg MJ, van-IJzendoorn For better and for worse: Differential susceptibility to environmental influences. Current Directions in Psychological Science. 2007;16:300–304. http://dx.doi.org/10.1111/j.1467-8721.2007.00525.x. [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin. 2009;135:885–908. doi: 10.1037/a0017376. http://dx.doi.org/10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Bless H, Fiedler K. Mood and the regulation of information processing and behavior. In: Forgas JP, editor. Affect in social thinking and behavior. New York, NY, US: Psychology Press; 2006. pp. 65–84. [Google Scholar]
- Boyce TW. Differential susceptibility of the developing brain to contextual adversity and stress. Neuropsychopharmacology. 2015:1–21. doi: 10.1038/npp.2015.294. http://dx.doi.org/10.1038/npp.2015.294. [DOI] [PMC free article] [PubMed]
- Boyce TW, Ellis BJ. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Developmental and Psychopathology. 2005;17:271–301. doi: 10.1017/s0954579405050145. http://dx.doi.org/10.1017/S0954579405050145. [DOI] [PubMed] [Google Scholar]
- Boyd CP, Gullone E, Needleman GL, Burt T. The family environment scale: Reliability and normative data for an adolescent sample. Family Process. 1997;36:369–373. doi: 10.1111/j.1545-5300.1997.00369.x. http://dx.doi.org/10.1111/j.1545-5300.1997.00369.x. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF. Infant temperament, parenting, and externalizing behavior in first grade: A test of the differential susceptibility hypothesis. Journal of Child Psychology and Psychiatry. 2008;49:124–131. doi: 10.1111/j.1469-7610.2007.01829.x. http://dx.doi.org/10.1111/j.1469-7610.2007.01829.x. [DOI] [PubMed] [Google Scholar]
- Buehler C, Welsh DP. A process model of adolescents' triangulation into parents' marital conflict: The role of emotional reactivity. Journal of Family Psychology. 2009;23:167–180. doi: 10.1037/a0014976. http://dx.doi.org/10.1037/a0014976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caprara GV, Cinanni V, D'Imperio G, Passerini S, Renzi P, Travaglia G. Indicators of impulsive aggression: Present status of research on irritability and emotional susceptibility scales. Personality and Individual Differences. 1985;6:665–674. http://dx.doi.org/10.1016/0191-8869(85)90077-7. [Google Scholar]
- Carthy T, Horesh N, Apter A, Gross JJ. Patterns of emotional reactivity and regulation in children with anxiety disorders. Journal of Psychopathology and Behavioral Assessment. 2010;32:23–36. http://dx.doi.org/10.1007/s10862-009-9167-8. [Google Scholar]
- Cavendish W, Montague M, Enders C, Dietz S. Mother's and adolescents' perceptions of family environment and adolescent social-emotional functioning. Journal of Child and Family Studies. 2014;23:52–66. http://dx.doi.org/10.1007/s10826-012-9685-y. [Google Scholar]
- Cummings ME, Davies P. Emotional security as a regulatory process in normal development and the development of psychopathology. Development and Psychopathology. 1996;8:123–139. http://dx.doi.org/10.1017/S0954579400007008. [Google Scholar]
- Davidson RJ. Affective style and affective disorders: Perspectives from affective neuroscience. Cognition and Emotion. 1998;12:307–330. http://dx.doi.org/10.1080/026999398379628. [Google Scholar]
- Davies PT, Cicchetti D, Martin MJ. Toward greater specificity in identifying associations among interparental aggression, child emotional reactivity to conflict, and child problems. Child Development. 2012;83:1789–1804. doi: 10.1111/j.1467-8624.2012.01804.x. http://dx.doi.org/10.1111/j.1467-8624.2012.01804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cicchetti D, Manning LG, Zale E. Children's pattern of emotional reactivity to conflict as explanatory mechanisms in links between interparental aggression and child physiological functioning. Journal of Child Psychology and Psychiatry. 2009;50:1384–1391. doi: 10.1111/j.1469-7610.2009.02154.x. http://dx.doi.org/10.1111/j.1469-7610.2009.02154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drabick DAG, Steinberg L. Developmental psychopathology. In: Brown BB, Prinstein MJ, editors. Encyclopedia of adolescence. Vol. 3. San Diego, CA, US: Academic Press; 2011. pp. 136–142. [Google Scholar]
- Fiedler K. Mood-dependent processing strategies from a meta-theoretical perspective. Psychological Inquiry. 2002;13:49–54. [Google Scholar]
- Forgas JP. Don't worry, be sad! On the cognitive, motivational, and interpersonal benefits of negative mood. Current Directions in Psychological Science. 2013;22:225–232. http://dx.doi.org/10.1177/0963721412474458. [Google Scholar]
- Garside RB, Klimes-Dougan B. Socialization of discrete negative emotions: Gender differences and links with psychological distress. Sex Roles. 2002;47:115–128. http://dx.doi.org/10.1023/A:1021090904785. [Google Scholar]
- Gilbert KE. The neglected role of positive emotion in adolescent psychopathology. Clinical Psychology Review. 2012;32:467–481. doi: 10.1016/j.cpr.2012.05.005. http://dx.doi.org/10.1016/j.cpr.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. http://dx.doi.org/10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Granic I, Dishion TJ, Hollenstein T, Patterson GR. Longitudinal analysis of flexibility and reorganization in adolescence: A dynamic systems study of family interactions. Developmental Psychology. 2003;39:606–617. doi: 10.1037/0012-1649.39.3.606. http://dx.doi.org/10.1037/0012-1649.39.3.606. [DOI] [PubMed] [Google Scholar]
- Hastings PD, Helm J, Mills RSL, Serbin LA, Stack DM, Schwartzman AE. Dispositional and environmental predictors of the development of internalizing problems in childhood: Testing a multilevel model. Journal of Abnormal Child Psychology. 2015;43:831–845. doi: 10.1007/s10802-014-9951-0. http://dx.doi.org/10.1007/s10802-014-9951-0. [DOI] [PubMed] [Google Scholar]
- Iyer RV, Kochenderfer-Ladd B, Eisenberg N, Thompson M. Peer victimization and effortful control: Relations to school engagement and academic achievement. Merrill-Palmer Quarterly. 2010;56:361–387. doi: 10.1353/mpq.0.0058. http://dx.doi.org/10.1353/mpq.0.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiley MK, Lofthouse N, Bates JE, Dodge KA, Pettit GS. Differential risks of covarying and pure components in mother and teacher reports of externalizing and internalizing behavior across ages 5 to 14. Journal of Abnormal Child Psychology. 2003;31:267–283. doi: 10.1023/a:1023277413027. http://dx.doi.org/10.1023/A:1023277413027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CLM, Myers JM, Kendler SK. The structure of the genetic and environmental influences on mental well-being. American Journal of Public Health. 2010;100:2379–2384. doi: 10.2105/AJPH.2010.193615. http://dx.doi.org/10.2105/AJPH.2010.193615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimes-Dougan B, Brand AE, Zahn-Waxler C, Usher B, Hastings PD, Kendziora K, et al. Parental emotion socialization in adolescence: Differences in sex, age and problem status. Social Development. 2007;16:326–342. http://dx.doi.org/10.1111/j.1467-9507.2007.00387.x. [Google Scholar]
- Lerner RM, Dowling EM, Anderson PM. Positive youth development: Thriving as the basis of personhood and civil society. Applied Developmental Science. 2003;7:172–180. doi: 10.1002/yd.14. http://dx.doi.org/10.1207/S1532480XADS0703_8. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analyses with missing data. 2nd. New York, NY, US: Wiley; 2002. [Google Scholar]
- Losel F, Slemming M. Continuity and patterns of externalizing and internalizing behavior in girls: A variable- and person-oriented study from preschool to youth age. Psychological Test and Assessment Modeling. 2012;54:307–319. [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71:543–562. doi: 10.1111/1467-8624.00164. http://dx.doi.org/10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradović J, Riley JR, et al. Developmental cascades: Linking academic achievement and internalizing and externalizing symptoms over 20 years. Developmental Psychology. 2005;41:733–746. doi: 10.1037/0012-1649.41.5.733. http://dx.doi.org/10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. http://dx.doi.org/10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Moos R, Moos B. Family environment scale manual: Development, applications, and research. 3rd. Palo Alto, CA, US: Consulting Psychologist Press; 1974. [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. http://dx.doi.org/10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musci RJ, Masyn KE, Benke K, Maher B, Uhl G, Ialongo NS. The effects of the interplay of genetics and early environmental risk on the course of internalizing symptoms from late childhood through adolescence. Developmental Psychopathology. 2015;28:225–237. doi: 10.1017/S0954579415000401. http://dx.doi.org/10.1017/S0954579415000401. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 7th. Los Angeles, CA, US: Muthén & Muthén; 1998-2014. [Google Scholar]
- Newman DA. Longitudinal modeling with randomly and systematically missing data: A simulation of ad hoc, maximum, likelihood, and multiple imputation techniques. Organizational Research Methods. 2003;6:328–362. http://dx.doi.org/10.1177/1094428103254673. [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. http://dx.doi.org/10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Oliver JM, Handal PJ, Enos DM, May MJ. Factor structure of the family environment scale: Factors based on items and scale. Educational and Psychological Measurement. 1988;48:469–477. http://dx.doi.org/10.1177/0013164488482022. [Google Scholar]
- Pluess M. Genetics of psychological well-being: The role of heritability and genetics in positive psychology. Oxford, United Kingdom: Oxford University Press; 2015. [Google Scholar]
- Pluess M, Belsky J. Differential susceptibility to parenting and quality child care. Developmental Psychology. 2010;46:379–390. doi: 10.1037/a0015203. http://dx.doi.org/10.1037/a0015203. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. http://dx.doi.org/10.3102/10769986031004437. [Google Scholar]
- Rabinowitz JA, Drabick DAG, Reynolds MD, Clark DB, Olino TM. Child temperamental flexibility moderates the relation between positive parenting and adolescent adjustment. Journal of Applied Developmental Psychology. 2016;43:43–53. doi: 10.1016/j.appdev.2015.12.006. http://dx.doi.org/10.1016/j.appdev.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond MK, Stocker CM. Associations between family cohesion and adolescent siblings' externalizing behavior. Journal of Family Psychology. 2006;20:663–669. doi: 10.1037/0893-3200.20.4.663. http://dx.doi.org/10.1037/0893-3200.20.4.663. [DOI] [PubMed] [Google Scholar]
- Rioux C, Castellanos-Ryan N, Parent S, Vitaro F, Tremblay RE, Séguin JR. Differential susceptibility to environmental experiences: Interactions between child temperament and parenting in adolescent alcohol use. Development and Psychopathology. 2016;28:265–275. doi: 10.1017/S0954579415000437. http://dx.doi.org/10.1017/S0954579415000437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roisman GI, Newman DA, Fraley C, Haltigan JD, Groh AM, Haydon KC. Distinguishing differential susceptibility from diathesis-stress: Recommendations for evaluating interaction effects. Development and Psychopathology. 2012;24:389–409. doi: 10.1017/S0954579412000065. http://dx.doi.org/10.1017/S0954579412000065. [DOI] [PubMed] [Google Scholar]
- Sanford K, Bingham CR, Zucker RA. Validity issues with the family environment scale: Psychometric resolution and research application with alcoholic families. Psychological Assessment. 1999;11:315–325. http://dx.doi.org/10.1037/1040-3590.11.3.315. [Google Scholar]
- Sanson A, Hemphill SA, Smart D. Connections between temperament and social development: A review. Social Development. 2004;13:142–170. http://dx.doi.org/10.1046/j.1467-9507.2004.00261.x. [Google Scholar]
- Schneiders J, Nicolson NA, Feron FJ, Berkhof J, van Os J, deVries MW. Mood reactivity to daily negative events in early adolescence: Relationship to risk for psychopathology. Developmental Psychology. 2006;42:543–554. doi: 10.1037/0012-1649.42.3.543. http://dx.doi.org/10.1037/0012-1649.42.3.543. [DOI] [PubMed] [Google Scholar]
- Smets AC, Hartup WW. Systems and symptoms: Family cohesion/adaptability and childhood behavior problems. Journal of Abnormal Child Psychology. 1998;16:233–246. doi: 10.1007/BF00913598. http://dx.doi.org/10.1007/BF00913598. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Lopez SJ, Pedrotti JT. Positive psychology: The scientific and practice explorations of human strengths. Thousand Oaks, CA, US: Sage Publishing, Inc; 2010. [Google Scholar]
- Spitzer R, Williams B, Gibbon M. Instruction manual for the structured interview for DSM-III-R. New York: New York State Psychiatric Institute, Biometrics Research Department; 1987. [Google Scholar]
- Stice E, Gonzales N. Adolescent temperament moderates the relation of parenting to antisocial behavior and substance use. Journal of Adolescent Research. 1998;13:5–31. http://dx.doi.org/10.1177/0743554898131002. [Google Scholar]
- Stoolmiller M, Bank L. Autoregressive effects in structural equation models: We see some problems. In: Gottman JM, editor. The analysis of change. Mahwah, NJ, US: Lawrence Erlbaum Associates, Inc; 1995. pp. 261–276. [Google Scholar]
- Tarter RE, Vanyukov MM. Introduction: Theoretical and operational framework for research into the etiology of substance use disorders. Journal of Child and Adolescent Substance Abuse. 2001;10:1–12. http://dx.doi.org/10.1300/J029v10n04_01. [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin. 1984;96:465–490. http://dx.doi.org/10.1037/0033-2909.96.3.465. [PubMed] [Google Scholar]
- Zarra-Nezhad M, Kiuru N, Aunola K, Zarra-Nezhad M, Ahonen T, Poikkeus AM, et al. Social withdrawal in children moderates the association between parenting styles and the children's own socioemotional development. Journal of Child Psychology and Psychiatry. 2014;55:1260–1269. doi: 10.1111/jcpp.12251. http://dx.doi.org/10.1111/jcpp.12251. [DOI] [PubMed] [Google Scholar]
- van Zeijl J, Mesman J, Stolk MN, Alink LRA, van Ijzendoorn MH, Bakermans-Kranenburg, et al. Differential susceptibility to discipline: The moderating effect of child temperament on the association between maternal discipline and early childhood externalizing problems. Journal of Family Psychology. 2007;21:626–636. doi: 10.1037/0893-3200.21.4.626. http://dx.doi.org/10.1037/0893-3200.21.4.626. [DOI] [PubMed] [Google Scholar]
- Zeman J, Shipman K, Suveg C. Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology. 2002;31:393–398. doi: 10.1207/S15374424JCCP3103_11. http://dx.doi.org/10.1207/S15374424JCCP3103_11. [DOI] [PubMed] [Google Scholar]
- Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC, US: American Psychological Association; 1999. [Google Scholar]