Abstract
Purpose
Truncating mutations in the maternally imprinted, paternally expressed gene MAGEL2, which is located in the Prader-Willi critical region 15q11-13, have recently been reported to cause Schaaf-Yang syndrome, a Prader-Willi-like disease, manifesting developmental delay/intellectual disability, hypotonia, feeding difficulties, and autism spectrum disorder. The causality of the reported variants in the context of the patients’ phenotypes was questioned, as MAGEL2 whole gene deletions appear to cause little to no clinical phenotype.
Methods
Here we report a total of 18 new individuals with Schaaf-Yang syndrome from 14 families, including one family with three individuals found to be affected with a truncating variant of MAGEL2, 11 individuals clinically affected, but not tested molecularly, and a presymptomatic fetal sibling with carrying the pathogenic MAGEL2 variant.
Results
All cases harbor truncating mutations of MAGEL2, and nucleotides c.1990-1996 arise as a mutational hotspot, with 10 individuals and one fetus harboring a c.1996dupC (p.Q666fs) mutation and two fetuses harboring a c.1996delC (p.Q666fs). The phenotypic spectrum of Schaaf-Yang syndrome ranges from fetal akinesia to individuals with neurobehavioral disease and contractures of the small finger joints.
Conclusion
This study provides strong evidence for the pathogenicity of truncating mutations of the paternal allele of MAGEL2, refines the associated clinical phenotypes, and highlights implications for genetic counseling of affected families.
Keywords: Schaaf-Yang syndrome, Prader-Willi syndrome, MAGEL2, neurodevelopment
Introduction
Truncating pathogenic variants in the maternally imprinted, paternally expressed MAGEL2 gene were initially reported as the cause of developmental delay/intellectual disability (DD/ID), hypotonia, feeding difficulties, and autism spectrum disorder (ASD) in four reported individuals.1 Due to phenotypic overlap with Prader-Willi syndrome (PWS [MIM 176270]), and MAGEL2 being one of the imprinted, protein-coding genes in the Prader-Willi domain on chromosome 15q11-q13, the condition was initially considered a Prader-Willi-like syndrome.
PWS is characterized by neonatal hypotonia, failure to thrive, hyperphagia and excessive weight gain in childhood, DD/ID, hypogonadism, short stature, and a unique behavioral profile.2 While the four previously reported individuals with truncating MAGEL2 mutations exhibited marked phenotypic overlap with PWS, including neonatal hypotonia, poor suck requiring special feeding techniques, DD/ID, hypogonadism, and excessive weight gain, they also manifested phenotypes that appeared to be distinct from PWS. These phenotypes included ASD, present in all four individuals, and contractures of the small finger joints, present in three. Other characteristics of PWS, such as the typical hyperphagia and subsequent obesity, were either absent or only mildly expressed. In order to highlight the phenotypic differences between PWS and the clinical condition caused by truncating MAGEL2 mutations, the latter was renamed to Schaaf-Yang syndrome (SHFYNG [MIM 615547]).
To date, a total of ten individuals with pathogenic variants in MAGEL2 have been reported.1,3,4 Six were diagnosed during childhood or adolescence with clinical features of Schaaf-Yang syndrome, while another four children from two unrelated families manifested severe arthrogryposis.
Importantly, the pathogenicity of truncating mutations of the paternal allele of MAGEL2 has been questioned, due to the small number of cases reported, but also because whole-gene deletions of the paternal copy of MAGEL2 appear to have no phenotype or very mild phenotypes.5,6
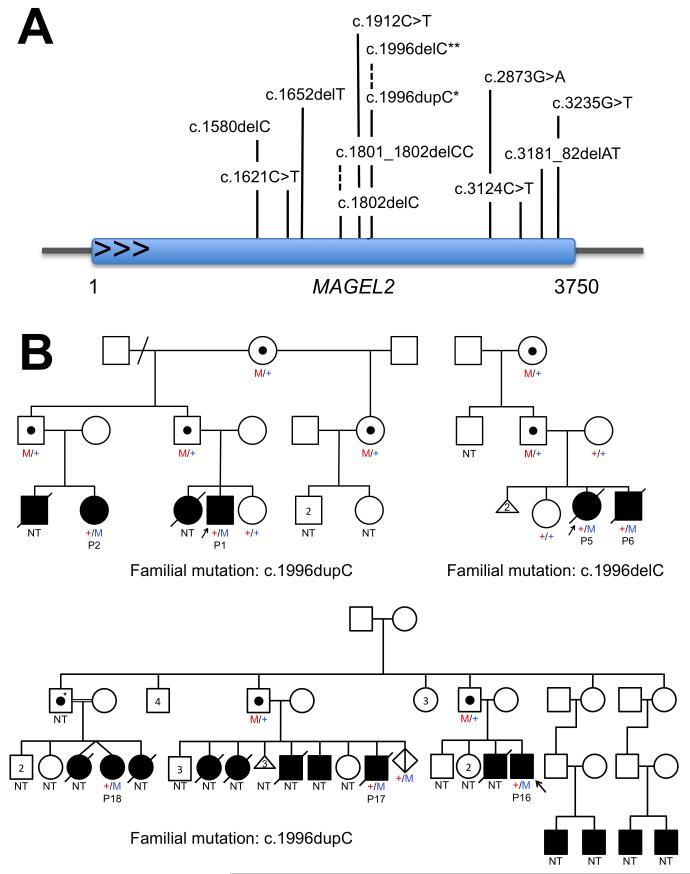
Here we report 18 newly identified individuals with truncating mutations in MAGEL2 (Figure 1A). Among these, there are three families with multiple affected individuals, including one family with three molecularly confirmed individuals, 11 who are clinically affected, but have not been tested molecularly, a fetus with a prenatal molecular diagnosis, and an inheritance pattern consistent with SHFYNG (Fig. 1B). Our study provides strong evidence for the pathogenicity of MAGEL2 mutations. It illustrates the broad phenotypic spectrum of Schaaf-Yang syndrome, which ranges from fetal akinesia and arthrogryposis multiplex congenita to individuals with mild intellectual disability and contractures of the small finger joints. Postnatal complications, including premature lethality, are discussed.
Figure 1. Newly identified truncating mutations of MAGEL2 in Schaaf-Yang syndrome.
A, Truncating MAGEL2 mutations reported in this manuscript are indicated by their positions in the coding sequence of the gene. *, 11 individuals with a c.1996dupC mutation; **, two individuals with a c.1996delC mutation. B, Pedigrees of familial cases. Pedigree 1, family of patients 1 and 2; pedigree 2, family of patients 5 and 6; pedigree 3, family of patients 16-18. Blackened squares and circles indicate individuals that are/were clinically affected. Black dots indicate carrier individuals, harboring the familial MAGEL2 mutation on their maternal allele. Maternal alleles are indicated in red, paternal alleles in blue. +, reference sequence for MAGEL2; M, familial MAGEL2 mutation; NT, not tested; P, patient; * obligate carrier.
Materials and Methods
Individuals with truncating MAGEL2 variants were enrolled based on genotype. Of the 14 probands reported in this study, 12 were identified by clinical whole exome sequencing, and two by targeted, clinical Sanger sequencing of the MAGEL2 gene. Five probands were enrolled through the Baylor Miraca Genetics Laboratories (BMGL) and four probands were enrolled through the GeneDx laboratory, of which one was enrolled through GeneMatcher. One family was ascertained at the Leiden University Medical Center. Cases identified by whole exome sequencing (WES) were subsequently confirmed by Sanger sequencing. Additional affected family members were identified by targeted Sanger sequencing of the known familial mutations. Upon identification of a probable pathogenic variant in MAGEL2, genetic counselors from the respective laboratories and institutions contacted the referring providers, informing them of a research interest in Dr. Schaaf’s laboratory. Four families contacted Dr. Schaaf directly because of a new diagnosis of Schaaf-Yang syndrome made by molecular genetic testing. An initial phenotypic assessment was obtained of all newly identified and molecularly confirmed individuals harboring pathogenic variants in MAGEL2 (patients 1-18 presented in Tables S1, S2, and S3). Upon consent to share clinical information, all were contacted for a detailed review of medical history, family history, ascertainment of developmental milestones, and physical features. Medical records were reviewed. Written informed consent was obtained for use of medical history, genetic testing report, and use of photograph (if applicable), as approved by the Institutional Review Board of Baylor College of Medicine.
Results
Combining the phenotypic characteristics of the novel 18 individuals with pathogenic variants in MAGEL2 reported herein with those previously identified by Schaaf et al.1, Soden et al.3, and Mejlachowicz et al.4, we are able to delineate the physical, cognitive, and behavioral spectrum of phenotypes associated with Schaaf-Yang syndrome (Table 1). Developmental delay, intellectual disability, and hypotonia represent the most common phenotypes, present among all individuals for whom this information has been available (Table 1).
Table 1.
Summary of published and novel patients with deleterious variants in MAGEL2
| This manuscript |
Schaaf et al.1 |
Soden et al.3 |
Mejlachowicz et al.4 |
Summary | Summary | |
|---|---|---|---|---|---|---|
| (n = 18*) | (n = 4) | (n = 2) | (n = 4) | (n = 28) | (%) | |
| Cognitive/behavioral characteristics | ||||||
|
| ||||||
| DD/ID | 14/14 | 4/4 | 2/2 | N/A | 20/20 | 100% |
| Autism spectrum disorder | 4/7** | 4/4 | 2/2 | N/A | 10/13 | 77% |
| Behavioral abnormalities (impulsivity, compulsivity, stubbornness, manipulative) |
9/11 | 2/4 | Unknown | N/A | 11/15 | 73% |
| Skin picking/automutilation | 7/12 | 2/4 | Unknown | N/A | 9/16 | 56% |
| Hyperphagia | 4/13 | 2/4 | Unknown | N/A | 6/17 | 35% |
|
| ||||||
| Physical characteristics | ||||||
|
| ||||||
| Hypotonia (at time of exam) | 13/13 | Unknown | Unknown | N/A | 13/13 | 100% |
| Feeding problems, need for special feeding technique |
15/16 | 3/4 | 2/2 | N/A | 20/22 | 91% |
| Neonatal hypotonia, poor suck | 14/15 | 3/4 | 2/2 | 1/1 | 20/22 | 91% |
| Contractures | 15/18 | 2/4 | 2/2 | 4/4 | 23/28 | 82% |
| Dysmorphic facial features | 16/18 | 1/4 | Unknown | 4/4 | 21/26 | 81% |
| Eye abnormalities (esotropia, myopia, strabismus) |
11/14 | 3/4 | Unknown | N/A | 14/18 | 78% |
| Hypogonadism | 8/11 M; 1/1 F |
3/4 | Unknown | Unknown | 11/15 M; 1/1 F |
73% |
| Small hands | 12/14 | 1/4 | Unknown | Unknown | 13/18 | 72% |
| Sleep apnea | 9/13 | 2/4 | Unknown | N/A | 11/17 | 65% |
| Small feet | 8/15 | 3/3 | Unknown | Unknown | 11/18 | 61% |
| Short stature | 10/16 | 2/4 | Unknown | Unknown | 12/20 | 60% |
| Decreased fetal movement | 6/15 | 3/4 | 2/2 | 4/4 | 15/25 | 60% |
| Gastroesophageal reflux | 8/14 | Unknown | Unknown | N/A | 8/14 | 57% |
| Excessive weight gain | 5/13 | 3/4 | Unknown | N/A | 8/17 | 47% |
| Temperature instability | 6/13 | Unknown | Unknown | N/A | 6/13 | 46% |
| Scoliosis/kyphosis | 7/14 | 1/4 | Unknown | Unknown | 8/18 | 44% |
| Chronic constipation | 4/11 | 1/4 | Unknown | N/A | 5/15 | 33% |
| Seizures | 2/13 | 1/4 | Unknown | N/A | 3/17 | 18% |
, only individuals with molecularly confirmed MAGEL2 mutation and detailed medical history included in this table.
, 7 subjects received formal testing; 6 more patients express symptoms of ASD. DD/ID, developmental delay/intellectual disability. F, female. M, male. N/A, not applicable.
On average, affected children sat independently at 19 months (range: 8-36 mo.), crawled at 24 months (range: 24-72 mo., patients 5 (10 years old) and 19 (15 y.o.) never crawled), walked at 39 months (range: 24-60 mo., patients 19 (15 y.o.) and 20 (20 y.o.) not walking), and spoke their first word at 56 months (range: 12-144 mo., patients 12 (10 y.o.), 19 (15 y.o.), and 20 (20 y.o.) not speaking). The level of intellectual disability ranged from mild to severe. Of the newly identified cases with both phenotypic information and a confirmed molecular diagnosis, seven were evaluated for ASD. Of these seven individuals, four received a formal diagnosis of ASD. An additional six subjects were described to manifest symptoms of ASD (denoted as asterisk in Table 1), however no formal evaluation was performed, and further assessment is necessary. An analysis of patient behavior identified a spectrum of abnormalities, including impulsive, compulsive, stubborn, and manipulative behaviors (seen in nine of 11 cases for which this information was available). Parents reported habitual skin picking or automutilation of varying severity in seven of 12 molecularly diagnosed individuals.
Neonatal hypotonia was identified as an early, initial physical phenotype displayed by patients with pathogenic variants in MAGEL2.1,3 Among the molecularly confirmed individuals of this study, 14 of 15 manifested neonatal hypotonia. Fifteen of 16 displayed feeding difficulties requiring special feeding techniques. Joint contractures were present in 15 of 18 of these cases. The severity of contractures ranged from affecting only the interphalangeal joints to fetal akinesia with severe arthrogryposis (present in individuals 5 and 6, discussed below). Additional abnormalities of the hands included tapering fingers, clinodactyly, camptodactyly, brachydactyly, and adducted thumbs (surgically corrected in patient 3) (Fig. 2). A further assessment of skeletal features showed 12 of 14 cases to have small hands, 8 of 15 to have small feet, and 10 of 16 cases to have small stature. Further, 7 of 14 cases were diagnosed with scoliosis or kyphosis. Sleep abnormalities were commonly seen, with 9 of 13 cases diagnosed with sleep apnea. Hypogonadism in the form of cryptorchidism and/or micropenis was present in 8 of 11 male cases and represents one of the earliest recognized physical features right after birth. In addition, Patient 18 (Table S3) is a 20-year-old female diagnosed with hypogonadotropic hypogonadism. Physical examination showed dysmorphic labial development. She had spontaneous menarche, but no spontaneous development of secondary sex characteristics. This was stimulated with estrogen supplementation at 18 years, and she now uses oral contraceptives. Eleven of 14 patients manifested eye abnormalities in the form of strabismus, esotropia, or myopia.
Figure 2. Hand phenotypes in patients with Schaaf-Yang syndrome.

Affected patients manifest a spectrum of phenotypes, including contractures of the interphalangeal joints, camptodactyly, tapering of the fingers, brachydactyly, clinodactyly, and adducted thumbs. A, patient 2; B, patient 3; C, patient 4; D, patient 7; E, patient 9; F, patient 10, G, patient 11; H, patient 13; I, patient 14; J, patient 15; K, patient 17.
Of 18 molecularly confirmed postnatal cases, 16 are described to have a spectrum of varying facial dysmorphisms including malformations of the philtrum, ear position, nasal structure, frontal bossing and palpebral fissure length. As well, prognathia with a squared-off chin appears to be present in the majority of older children. As evidenced in figure 3, there is an appreciable variability of the degree of facial dysmorphisms previously mentioned, as well as bushy eyebrows and short noses.
Figure 3. Facial phenotype of individuals with Schaaf-Yang syndrome.
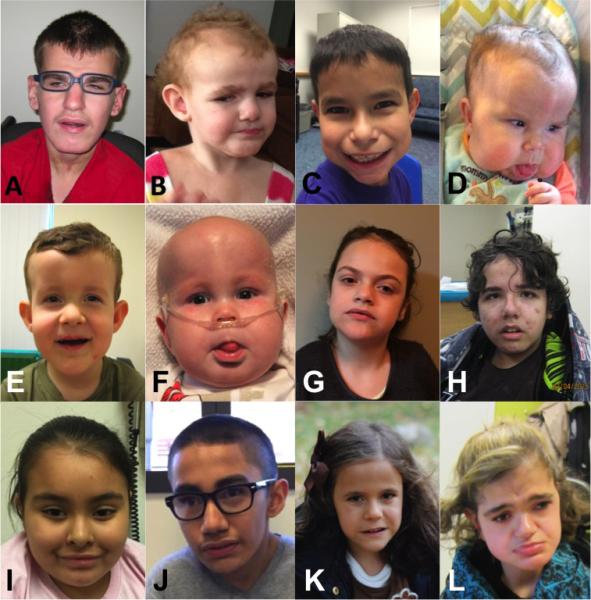
While several individuals manifest dysmorphic facial features, such as short noses, bushy eyebrows, and prognathism, the consistency of facial characteristics across individuals is limited. A, patient 1; B, patient 2; C, patient 3; D, patient 4; E, patient 7; F, patient 9; G, patient 10; H, patient 11; I, patient 13; J, patient 14; K, patient 15; L, patient 18.
Familial cases: Patients 1 and 2 are paternal cousins both carrying a deleterious c.1996dupC (p.Q666fs) variant in the MAGEL2 gene (Fig. 1B, pedigree on the upper left; Table S4), detected by clinical whole exome sequencing in the propositus (patient 1). Patient 1 is a 15-year-old male presenting characteristic phenotypes of SHFYNG specifically, neonatal hypotonia, feeding difficulties requiring assisted feeding techniques, contractures, hypotonia at the time of exam, and hypogonadism, among others (Fig. 3A). As well, he manifested cognitive and behavioral phenotypes typical of SHFYNG, namely DD/ID, ASD, and a behavioral profile including impulsivity, compulsivity, stubbornness, and manipulative behaviors. He did not have any indication of hyperphagia (Table S1). Patient 2 is a 6-year-old female, who shares several physical characteristics with her male cousin. She manifested neonatal hypotonia, feeding difficulties requiring assistance, contractures, and hypotonia at time of exam, among other phenotypes (Fig. 2A, 3B). As well, she manifested DD/ID and ASD, but no hyperphagia (Table S1). Using methylation sensitive digestion of the genomic DNA followed by PCR amplification and Sanger sequencing as previously described1, we confirmed that the c.1996dupC was present on his paternal MAGEL2 allele. Subsequent analysis revealed that his father and paternal grandmother were both carriers of the c.1996dupC (p.Q666fs) change, and that the mutation resided on their maternal chromosomes 15. This finding is consistent with their clinically unaffected status, based on the molecular mechanism of this disorder, caused by mutations of a paternally expressed, maternally imprinted gene. We then established that the proband’s paternal uncle and half-aunt were also carriers of the c.1996dupC (p.Q666fs) mutation, which they had inherited from their mother. Molecular analysis of the patient’s affected female cousin (Table S1; Patient 2) showed that she had inherited the c.1996dupC (p.Q666fs) mutation from her clinically unaffected carrier father.
Patients 5 and 6 are fetal cases from two separate pregnancies, affected with fetal akinesia and severe arthrogryposis (Fig. 1B, pedigree on the upper right). Analysis via whole-exome sequencing revealed that both fetuses harbored a deleterious variant, c.1996delC (p.Q666fs), in the MAGEL2 gene. Patient 5 was a female fetus presenting with fetal akinesia, noted on prenatal ultrasound examination (Table S1; Fig. S1A, S1B). Upon consultation, the family elected to terminate the pregnancy at 21 weeks and four days gestation. Post-mortem examination identified contractures, overlapping digits, and rocker bottom feet, as well as retro-micrognathia and gnatho-palatoschisis. Patient 6, a male sibling of patient 5, also presented with fetal akinesia (Table S1; Fig. S1C, S1D), and the family elected to terminate the pregnancy at 14 weeks and six days gestation. Post-mortem examination identified similar phenotypic expression with contractures, overlapping digits, and retro-micrognathia. Moreover, patient 6 manifested multiple pterygia and bilateral congenital talipes equinovarus. The c.1996delC (p.Q666fs) variant identified in patient 5 and 6 was found to be inherited from the unaffected father and unaffected paternal grandmother. Moreover, the variant was found not to be present in the healthy sibling to these fetuses.
Patients 16, 17 and 18 are paternal cousins (Fig. 1B, lower pedigree). Whole exome sequencing identified the c.1996dupC (p.Q666fs) mutation in the proband (patient 16) and patient 18. Molecular analysis confirmed the mutation in patient 17, the proband’s father, and one paternal uncle. Sanger sequencing identified the mutation in a chorion villi sample of a fetal sibling of patient 17 (Fig. 1B, lower pedigree), who shows a clenched fist on ultrasound examination at 29+6 weeks of gestation. Patients 16, 17, and 18 manifested phenotypes consistent with SHFYNG, most notably neonatal hypotonia, feeding difficulties requiring assisted feeding techniques, DD/ID, dysmorphic facial features, and contractures (Table S3; Fig. 2K, 3L). Patient 16, a deceased nine-month-old male, passed with an unknown cause of death, though suspect for apnea.
In order to get an appreciation of the prevalence of Schaaf-Yang syndrome among samples submitted for clinical WES, we analyzed the data available from the Baylor Miraca Genetics and the GeneDx laboratories. As of February 2016, the two laboratories have analyzed a combined total of 15,360 proband exomes. Of these 15,360 individuals, 13 were identified to have pathogenic truncating variants in MAGEL2. When filtering for those manifesting developmental delay and/or intellectual disability and hypotonia, seven of 3,820 individuals were identified to have pathogenic MAGEL2 variants. When filtering for male individuals with DD and/or ID and hypogonadism, four of 162 individuals were identified as positive for MAGEL2 truncating variants. This analysis is limited by the phenotypes listed at the time of sample submission.
Discussion
In this report, we present 18 individuals with phenotypic characteristics of SHFYNG, all of whom have molecularly confirmed truncating mutations in MAGEL2. The consistency of clinical features among affected individuals, and the segregation of clinical phenotypes with the presence of the respective MAGEL2 mutations on the paternal allele in three families, provides evidence of the pathogenicity of these mutations. Furthermore, the consistency of clinical features suggests a clinically recognizable syndrome, characterized by neonatal hypotonia, feeding difficulties, contractures, and developmental delay.
Previously reported patients with deletions encompassing MAGEL2, but not the SNORD116@ cluster on chromosome 15q, appear to have milder phenotypes than those individuals with truncating MAGEL2 mutations.5,6 Buiting et al. described a patient with deletion of MAGEL2, who presented with transient hypotonia and feeding difficulties during infancy.6 He had kyphosis and manifested a slight delay in fine and gross motor skills. The concept that a deletion of the entire gene could have milder effects than a truncating mutation is intriguing. As MAGEL2 is a one-exon gene, one could speculate that truncating mutations may result in a truncated protein, which then could have a dominant-negative effect. Alternatively, the deletion of the entire paternal copy of this imprinted gene, including its promoter, could lead to leaky expression of the maternal copy of the gene. This has been suggested based on studies of Magel2 m+/p− mice.7 Indeed, further investigation of individuals with MAGEL2 deletions is necessary and may broaden the phenotypic spectrum associated with MAGEL2 mutations.
To further delineate the clinical phenotype associated with MAGEL2 truncating variants, we report prominent early phenotypes of fetal akinesia, neonatal hypotonia, feeding difficulties requiring assisted feeding techniques, and DD/ID. Sleep apnea, gastroesophageal reflux, and decreased fetal movement are frequently reported in SHFYNG. These symptoms may be observed due to the muscular dysfunction associated with the early hypotonia. Importantly, twenty-three of 28 postnatal individuals with molecularly confirmed MAGEL2 mutations reported to date manifest contractures of their interphalangeal joints, a phenotype rarely reported among individuals with PWS8–10, providing further evidence that the prevalence of certain phenotypes may be markedly different between SHFYNG and PWS.
Although the infantile phenotype of SHFYNG is profoundly similar to PWS, the majority of patients with point mutations in MAGEL2 appear not to go through the later nutritional stages of PWS.11 In particular, most individuals appear not to progress to phase 3, which is characterized by hyperphagia. Further, only eight of 17 molecularly confirmed individuals had excessive weight gain, typically associated with PWS. Interestingly, patient one described here and the recently described siblings of Soden et al. (CMH382 and CMH382) had unusual body habitus with increased abdominal girth.3 Body composition and patterns of adiposity have not been studied in individuals with MAGEL2 mutations, but this should be considered, taking into consideration the murine phenotype of Magel2 loss-of-function. The mice are not significantly overweight, but do have increased adiposity with altered metabolism in adulthood.12 Strikingly, ten of 13 patients tested to date carry a diagnosis of ASD, and six are reported to manifest autistic behaviors. This is a marked contrast to the 27% of PWS cases diagnosed with ASD.13 Notable cognitive behavioral characteristics were described as being impulsive, compulsive, varying degrees of stubbornness, and being manipulative. Detailed neuropsychological phenotyping would be warranted to further delineate the behavioral phenotypes of individuals with MAGEL2 loss-of-function. Of note, a Magel2-deficient mouse model manifests deficits in social recognition and social interaction.14
It is readily apparent that patients with truncating mutations of MAGEL2 express different levels of severity. On one hand, there are multiple patients with relatively mild contractures, only affecting the interphalangeal joint. On the other hand, there are cases of fetal akinesia, with severely decreased fetal movement and arthrogryposis multiplex, as seen in patient 5 and 6 (Table S1; Fig. S1). Indeed, several individuals who appeared to be affected with SHFYNG died during childhood. Reported causes of death included apnea, aspiration pneumonia with subsequent medical complications, and sudden infant death syndrome. However, further investigation of the natural course of SHFYNG and its associated mortality is necessary.
Nucleotides c.1990-1996 represent a sequence of seven cytosines, which appears to represent a mutational hotspot, with a total of 13 molecularly confirmed individuals from eight families with a c.1996dupC, and five individuals from two families with a c.1996delC pathogenic variant. The fact that the two cases of fetal akinesia reported herein carried the same pathogenic variant (c.1996delC; p.Q666fs) as the three siblings with prenatally lethal arthrogryposis multiplex, reported by Mejlachowicz et al.4, suggests that some genotype-phenotype correlations may exist. In this context, it is worth noting that neither missense mutations in MAGEL2, nor mutations of the MAGEL2 promoter have been reported to date. These may provide further information regarding genotype-phenotype correlation.
While we are able to present the clinical phenotypes of 18 molecularly confirmed patients, the ability to gain complete medical history and background can prove troublesome. Due to familial geographic location, lack of historical medical information, and availability of care, not all phenotypes can be assessed. Moreover, the age of an individual can predict the availability of phenotypic information, such as the diagnosis of ASD, characteristic cognitive behaviors, and hypogonadism in males. While male hypogonadism can often be noted clinically, even at the time of birth, via the observation of cryptorchidism and/or micropenis, female hypogonadism is not as readily recognizable. As mentioned, patient 18 is the oldest presented female and the only female reported with hypogonadism to date. She was diagnosed with hypogonadotropic hypogonadism and presented dysmorphic labial development, identifiable upon pubertal maturation. A systematic, endocrinological assessment of individuals with SHFYNG has not been reported to date.
Given the phenotypic overlap between PWS and SHFYNG, testing for mutations in MAGEL2 should be considered in the context of PWS-like phenotypes, but negative PWS methylation analysis. In fact, during infancy, PWS was considered high on the differential diagnosis for most of the individuals reported herein. While SHFYNG and PWS share an appreciable amount of common features, and no specific feature appears to be exclusive of one or the other condition, the presence of contractures at birth makes SHFYNG more likely, while the development of hyperphagia in childhood appears to be more characteristic of PWS. The overlap and the distinction between the two syndromes has been described previously.15
PWS and PWS-like phenotype usually represent sporadic disorders, with single individuals affected within a given family. This report of 18 individuals includes three families carrying a truncating MAGEL2 mutation leading to SHFYNG. The familial association highlights the importance of parental testing, determination of the allelic location of the mutation, and the challenges for genetic counseling. Unlike “regular” autosomal dominant disorders, the imprinted nature of this condition can phenotypically skip several generations, as long as the mutation resides on the maternal (imprinted) chromosome. However, the chances for offspring of male individuals carrying a deleterious MAGEL2 mutation to be clinically affected are 50%.
For several individuals and their families reported herein, making a molecular diagnosis puts an end to a long diagnostic odyssey. It allows families to connect with each other for the exchange of experience and knowledge, and for emotional support. In particular, these families have connected via social media, providing support to families with newly identified individuals, showing the important role of family advocacy, especially in rare disorders such as Schaaf-Yang syndrome.
Current trials are underway to evaluate oxytocin as a potential therapeutic for PWS (clinicaltrials.gov). Oxytocin therapy has been shown as effective in mice null for Magel2, and may be beneficial for humans expressing truncating mutations of MAGEL2 as well.14,16 Having families connected together will allow for a quick dissemination of updated knowledge and faster enrollment into potential clinical trials.
Supplementary Material
Acknowledgments
This work was supported by the Joan and Stanford Alexander Family (CPS), and the Foundation for Prader-Willi Research (CPS). This research is supported by the Intellectual and Developmental Disabilities Research Center (1U54 HD083092). We are indebted to the patients and their families for their willingness to participate in our study.
Footnotes
Supplementary information is available at the Genetics in Medicine website.
Resources
Facebook group for affected families: www.facebook.com/MAGEL2
References
- 1.Schaaf CP, Gonzalez-Garay ML, Xia F, et al. Truncating mutations of MAGEL2 cause Prader-Willi phenotypes and autism. Nat Genet. 2013;45(11):1405–1408. doi: 10.1038/ng.2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holm VA, Cassidy SB, Butler MG, et al. Prader-Willi Syndrome : Consensus Diagnostic Criteria. Pediatrics. 1993;91(2):398–402. [PMC free article] [PubMed] [Google Scholar]
- 3.Soden SE, Saunders CJ, Willig LK, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6(265):1–14. doi: 10.1126/scitranslmed.3010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mejlachowicz D, Nolent F, Maluenda J, et al. Truncating Mutations of MAGEL2, a Gene within the Prader-Willi Locus, Are Responsible for Severe Arthrogryposis. Am J Hum Genet. 2015:1–5. doi: 10.1016/j.ajhg.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanber D, Giltay J, Wieczorek D, et al. A paternal deletion of MKRN3, MAGEL2 and NDN does not result in Prader-Willi syndrome. Eur J Hum Genet. 2009;17(5):582–590. doi: 10.1038/ejhg.2008.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buiting K, Di Donato N, Beygo J, et al. Clinical phenotypes of MAGEL2 mutations and deletions. Orphanet J Rare Dis. 2014;9(1):40. doi: 10.1186/1750-1172-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matarazzo V, Muscatelli F. Natural breaking of the maternal silence at the mouse and human imprinted Prader-Willi locus: A whisper with functional consequences. Rare Dis. 2013;1(e27228):1–7. doi: 10.4161/rdis.27228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denizot S, Boscher C, Le Vaillant C, Roze JC, Gras Le Guen C. Distal Arthrogryposis and Neonatal Hypotonia: an Unusual Presentation of Prader–Willi Syndrome ( PWS ) J Perinatol. 2004;24:733–734. doi: 10.1038/sj.jp.7211185. [DOI] [PubMed] [Google Scholar]
- 9.Bigi N, Faure J, Coubes C, et al. Prader-Willi syndrome : is there a recognizable fetal phenotype ? Prenat Diagn. 2008 Jan;28:796–799. doi: 10.1002/pd. [DOI] [PubMed] [Google Scholar]
- 10.Haugen G, Ronnestad A, Kroken M. Variations in fetal phenotype in Prader-Willi syndrome. Prenat Diagn. 2009;29:294. doi: 10.1002/pd.2207. [DOI] [PubMed] [Google Scholar]
- 11.Miller JL, Lynn CH, Driscoll DC, et al. Nutritional phases in Prader-Willi syndrome. Am J Med Genet Part A. 2011 Apr;155:1040–1049. doi: 10.1002/ajmg.a.33951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bischof JM, Stewart CL, Wevrick R. Inactivation of the mouse Magel2 gene results in growth abnormalities similar to Prader-Willi syndrome. Hum Mol Genet. 2007;16(22):2713–2719. doi: 10.1093/hmg/ddm225. [DOI] [PubMed] [Google Scholar]
- 13.Bennett JA, Germani T, Haqq AM, Zwaigenbaum L. Autism spectrum disorder in Prader-Willi syndrome: A systematic review. Am J Med Genet Part A. 2015;167A:2936–2944. doi: 10.1002/ajmg.a.37286. [DOI] [PubMed] [Google Scholar]
- 14.Meziane H, Schaller F, Bauer S, et al. An Early Postnatal Oxytocin Treatment Prevents Social and Learning Deficits in Adult Mice Deficient for Magel2, a Gene Involved in Prader-Willi Syndrome and Autism. Biol Psychiatry. 2014;78:85–94. doi: 10.1016/j.biopsych.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Fountain MD, Schaaf CP. Prader-Willi Syndrome and Schaaf-Yang Syndrome : Neurodevelopmental Diseases Intersecting at the MAGEL2 Gene. Diseases. 2016;4 doi: 10.3390/www.mdpi.com/journal/diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fountain MD, Schaaf CP. MAGEL2 and Oxytocin—Implications in Prader-Willi Syndrome and Beyond. Biol Psychiatry. 2015;78(2):78–80. doi: 10.1016/j.biopsych.2015.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.