Abstract
The home environment includes important social and physical contexts within which children develop. Poor physical home environments may be a potential source of stress for children through difficult daily experiences. Using a sub-sample from the Los Angeles Family and Neighborhood Survey (N = 425), we consider how the home physical environment affects stress-related immune system dysregulation in children ages 3–18 years. Results indicated that children in poorer quality homes had higher inflammation (measured by C-reactive protein). The associations were particularly strong for younger children. We also found that part of the home physical environment association with CRP worked through increased risk of obesity for children living in low-quality homes. Future research should assess how home physical environments could be improved to reduce stress and improve health outcomes in children.
Keywords: Stress, CRP, L.A.FANS, Housing, Poverty, Obesity
1. Introduction
A healthy and safe home environment is essential for promoting and protecting health and development during childhood. Children need stable, supportive social environments and access to resources within the home to enhance cognitive, emotional, and physical development (Bronfenbrenner, 2001). Alternatively, unstable, noisy, chaotic home environments have negative effects on children’s health (Dush et al., 2013) and development (Evans, 2003; Evans and English, 2002). Low-income children are more likely to face poor quality home environments, across multiple domains, than their wealthier counterparts (Bradley et al., 2001; Evans and English, 2002; Holupka and Newman, 2011); and, low-income parents are often forced to choose between healthy and affordable homes (Breysse et al., 2004). Thus, the home physical environment not only affects individual child well-being, but also is an important pathway through which socio-economic inequalities create child health and developmental disparities (Conley, 2001).
One reason proposed for the negative effects of poor home environments on child well-being is through increased exposure to stress (Conger and Donnellan, 2007). Biological changes may occur if the body is exposed to chronic stress (repeated stress response over time), resulting in dysregulation of the neuroendocrine and immune systems; these systems may be particularly sensitive during the formative years of childhood and adolescence (Bauer and Boyce, 2004; Pervanidou and Chrousos 2012). Dysregulation of children’s neuroendocrine and immune systems, in turn, is associated with poor health (Chen et al., 2006), cognitive (Keller et al., 2012), and socio-emotional (Evans and English, 2002) outcomes.
In this study, we consider how the home physical environment affects stress-related immune system dysregulation in children as indicated by increased low-grade inflammation levels (measured by C- reactive protein). We focus on the physical disorder in the home (e.g., hazards, crowding, dim lighting, clutter, uncleanliness) as a potentially important source of stress for children. Past research suggests important negative effects of the home physical environment on children’s socio-emotional outcomes (Evans et al., 2001b), but it is not yet clear whether these experiences result in physiological changes and biological embedding of childhood disadvantage. We assess potential differences in the association between physical home conditions and inflammation by child age, building on past evidence of age differences in SES associations with child health (Chen et al., 2006; Chen et al., 2002). We also consider the mediating role of obesity, given that low-quality home environments may contribute to obesity through decreased opportunities for activity and poor eating or sleeping habits; and higher body mass index (BMI), in turn, is associated with higher inflammation levels in children (Dowd et al., 2010; Visser et al., 2001).
We test these research hypotheses using data from the Los Angeles Family and Neighborhood Survey (L.A.FANS). The data are representative of households in L.A. County, a geographical area that includes the least affordable housing market of all metropolitan areas in the nation (California Housing Partnership Corporation, 2014). With increasing housing costs, low-income families in Los Angeles are forced to overspend and overcrowd with little hope for homeownership. It is no coincidence that the city with the least affordable housing market also has the second highest rate of overcrowded households among major U.S. cities, with 25.6% of all families living in crowded quarters (O’Hara, 2002). The situation is worse for children; in 2013, nearly half of L.A. children (46%) lived in cramped homes compared to the state average of 28% and the national average of 14% (Kids Count Data Center, 2014). Other aspects of the home environment, such as safety and access to outdoor areas, are likely to be sacrificed within this expensive housing market, with implications for children’s exposure to and ability to cope with chronic stress.
Our study provides new research on home physical conditions and child well-being, focusing on inflammation as an under-studied measure of exposure to chronic stress in children. The use of interviewer-rated home assessments and biomarker outcomes reduces biases related to parental reports. Of particular importance, we assess how associations differ by child age and when controlling for obesity. The findings from this study inform future research and policy related to housing and child well-being, and increase our understanding of how health inequalities begin during childhood.
2. Background
The household is a critical ecological context that affects children’s health and psychosocial development (Bronfenbrenner, 1995). Compared to more distal environments, home conditions may be particularly relevant for child well-being due to the daily, repeated interactions between children and their home environments (Bronfenbrenner, 1995; Bronfenbrenner and Evans, 2000). Physical characteristics of the home are an important part of this context because they influence children’s social interactions, health behaviors (sleeping, eating, physical activity), and exposure to environmental toxins (Evans, 2006). Social interactions may be impacted by the lack of adequate, organized space for members of the household to carry out daily activities.
A review of research indicates that crowded and inadequate housing increases tension, punitive punishment, aggression and conflict within the household (Evans, 2006). Physical disorder, such as lack of cleanliness and higher levels of clutter in the home, also may reflect social disorganization, with implications for children’s well-being (Dunifon et al., 2004). Social disorder related to physical conditions in the home can, in turn, lead to increased psychosocial stress in children. Recent research found that emotional chaos in the home (various indicators of commotion within the home) predicted stress (abnormal cortisol responses) in young, low-income children (Lumeng et al., 2014). Other research indicates poor housing conditions are associated with increased psychological distress among mothers (Evans et al., 2000), another social risk factor that may be associated with child stress in homes with poor physical conditions.
In addition to social relationships, low-quality physical housing environments may affect children’s health and stress-coping behaviors. Having an unsafe interior or exterior, no access to a yard or patio, crowding, and poorly-lit interiors reduce children’s creative play, ability to move about, and outdoor playtime (Maitland et al., 2013; Marino et al., 2012). These conditions can increase sedentary behaviors and reduce children’s ability to cope with the stressful environments (Wells and Evans, 2003). Research also suggests that more chaotic homes increase unhealthy, stress-related eating behaviors in young children (Lumeng et al., 2014). Crowded, inadequate and disorganized home environments also impact children’s sleep habits, directly and indirectly through increased psychosocial stress; and, poor sleep quality may contribute to elevated inflammation (Quist et al., 2015). Thus, lack of adequate home physical conditions may impact behaviors that increase inflammation and risk of obesity in children (McCurdy et al., 2010).
Finally, the home physical environment embodies environmental toxins that can be found in the air (dust, noise), walls (mold, lead paint), floor (unsafe objects), and other areas within the home. Children with environmental toxins (including noise) in the home have been observed to have worse developmental, physical health, and behavioral outcomes (Cohen and Spacapan, 1984; Evans, 2006; Koger et al., 2005; Krieger and Higgins, 2002); and elevated noise has been associated with biomarkers of stress in children (Evans et al., 2001a; Hohmann et al., 2013).
Existing empirical evidence supports the importance of ensuring a high quality home physical environment for child health (Leventhal and Newman, 2010). In a study of four housing characteristics (housing type, cost, quality, and stability) poor housing quality most consistently predicted low-income children’s emotional and behavioral problems and lower cognitive skills (Coley et al., 2013). Several studies indicate that household social and physical disorder (including hazardous, crowded, cluttered, and unclean homes) are associated with worse health in children (Breysse et al., 2004; Cutts et al., 2011; Delgado et al., 2002; Dush et al., 2013; Leventhal and Newman, 2010; Suglia et al., 2010).
Limited research also finds that home physical environments may be associated with increased levels of chronic stress in children. One study using an index of interviewer-assessed housing quality found that poorer quality home environments were associated with higher psychological distress (children’s behavioral problems reported by parents) and learned helplessness in third through fifth graders, net of family income (Evans et al., 2001b). Another study of predominantly white children from low-income, rural communities found cumulative risk (including an indicator of substandard housing) to be associated with higher blood pressure and neuroendocrine markers of stress in children between the ages of 8 and 10 years (Evans and English, 2002).
2.1. Housing and inflammation
This study aims to assess how children’s home quality is associated with a biomarker of chronic stress exposure that has not been extensively studied in children –low-grade inflammation. Inflammation is a normal part of the body’s response to a threat, increasing the production of, among other things, C-reactive protein (CRP). CRP is a sensitive marker of inflammation and levels normally rise quickly in response to a physiological threat – infection or injury – and then decline soon after the threat is resolved (Dowd et al., 2010). However, low levels of CRP indicate a dysregulated immune system and increase the risk of chronic disease (McDade, 2012).
During childhood, inflammation has been linked with depression (Kim et al., 2014; Miller and Cole, 2012) and, in some studies, cardiovascular risk factors in youth (Slopen et al., 2012). Further, elevated inflammation in childhood may increase the risk for adult inflammation (Fagundes et al., 2013; Miller et al., 2011).
Exposure to psychosocial stress has been posited as a cause of low-grade inflammation and part of the biological embedding of social and economic disadvantage (Milleret al., 2011). Recent studies of U.S. children have found associations between elevated CRP and living in high-risk neighborhoods (Broyles et al., 2012), experiencing maltreatment (Cicchetti et al., 2015; Danese et al., 2011; Gonzalez, 2013), and living in low-income families (Dowd et al., 2010). Among children in Avon, England, externalizing behavior at age 8 was associated with higher CRP at age 10 (Slopen et al., 2013a); and adverse life events from early to mid-childhood were associated with higher CRP at ages 10 and 15, with some of the effects mediated by obesity (Slopen et al., 2013b). These suggest that risky social and economic conditions may result in systemic inflammation during childhood.
Importantly, research has found that everyday sources of stress, not just traumatic events, may have physiological implications for children. Adolescents with higher daily stressors (Fuligni et al., 2009) and those experiencing lower levels of positive affect (Chiang et al., 2015) had higher levels of CRP. Further, an intervention study of 11-year old rural African American children found that a program aimed at reducing psychosocial stress in children significantly decreased inflammation, in part due to improved parenting in the treated group (Miller et al., 2014). These studies indicate the potential for non-traumatic, chronic psychosocial stress occurring in the home environment to contribute to dysregulated immune systems in children and adolescents.
In this study, we hypothesize that a poor quality home physical environment (HPE) will be associated with higher stress-related inflammation in children through increased exposure to chronic psychosocial stress. Housing research suggests that the overall quality of the home environment, rather than subscales or individual indicators, are more important for studies of psychosocial distress (Evans et al., 2000). Following cumulative risk theory (Barocas et al., 1985) and past research (Bradley et al., 2001; Evans et al., 2001b), we assess how the cumulative number of risky HPE factors, rather than one indicator alone, influences children’s inflammation levels.
Based on developmental theory (Bronfenbrenner, 1995), we also assess the role of child age in moderating the effect of the HPE on inflammation. Younger children are likely to spend more time at home and be less able to escape the threats that the physical environment presents than adolescents. Thus, a low-quality HPE may have a stronger effect on younger children’s inflammation. On the other hand, if biological differences by HPE emerge due to the accumulation of stress over time, then HPE may be more strongly associated with elevated inflammation in older children. Past studies of the SES-health gradient among children have found that the association varies by age as well as the specific health outcome under analysis (Chen et al., 2002, 2006). Studies of household income and inflammation in children to date have found no significant differences by age (Dowd et al., 2010), but the effects of home conditions have not been explored.
Finally, we test if the associations between the HPE and children’s inflammation are due to increased risk of obesity. We posit that low-quality HPE will be associated with higher obesity risk, as homes with unsafe exteriors or no outside space may reduce the chances for children to exercise. Further, disordered and unsafe interior home conditions may induce unhealthy eating and sedentary behaviors (i.e., TV watching and video games) as ways of coping with difficult home environments. We test whether obesity is a key pathway between the HPE and inflammation, since overweight children have higher levels of inflammation (Visser et al., 2001).
A recent review of research in this area found no studies of home physical characteristics and child obesity (Gundersen et al., 2011); however, one related study found cumulative risk exposure (including 3 indicators of poor physical conditions in the home as part of the broader index) was linked to weight change during childhood (Wells et al., 2010). Another study found various family stressors to be associated with increased risk of obesity in children and adolescents (Garasky et al., 2009). The results indicated no association between housing stressors (moving to cheaper housing, moving in with others, sending a child to live elsewhere, or spending greater than 30% of income on housing) and the risk for childhood obesity, but home physical conditions were not considered (Garasky et al., 2009).
3. Methods
3.1. Data
This study uses unique data from the Los Angeles Family and Neighborhood Survey (L.A.FANS), which includes measures of social and economic conditions at the household and parent levels, along with biomarkers in children. L.A.FANS was designed as a stratified probability sample of neighborhoods (census tracts), blocks within these neighborhoods, households within these blocks, and children and adults within these households (Sastry et al., 2006). Poor and very poor census tracts and households with children were oversampled. Wave 2 (2006–2008) includes the biomarker measure of inflammation –CRP obtained by licensed phlebotomists—in a random sub-sample of children ages 3–18. Wave 1 did not collect biomarkers and thus was not included in this study.
The analytical sample used in this study consists of children who participated in the blood spot collection (425 of the 600 randomly selected for participation) for whom sufficient blood was obtained (N = 414). Since CRP values above 10 mg/L are considered acute responses to infection or injury rather than a response to chronic stress (McDade, 2007), we limit our sample to children with CRP levels ≤10 mg/L (383 of the 414 cases). A further 30 cases were dropped due to missing independent variables resulting in a sample size of 353.
Descriptive and regression analyses were adjusted to account for unequal selection probability and the clustered survey design (Peterson et al., 2011). Weights were calculated by multiplying the wave 2 child weights by the blood spot specific weights to account for oversampling, attrition by wave 2 and non-response to the blood spot portion of the study. We applied the combined weights to the descriptive and regression results to provide analyses representative of children in L.A. County.
Table 1 below presents the weighted descriptive statistics for the analytical sample. The mean child age was 11 years and 22% of the children were obese based on BMI cutoffs by age and gender. Although the mean family income-to-poverty ratio was under 3 (less than 3 times the poverty line), it varied substantially (standard deviation = 3). Virtually all (96%) primary caregivers were mothers. Of these caregivers, 53% were immigrants, 63% were Hispanic, and 36% had less than a high school degree (Table 1).
Table 1.
Weighted descriptive statistics of children with CRP ≤10 mg/L, L.A.FANS Wave 2, N = 353.
| Variables | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|
| Home Physical Environment (HPE) Measures | ||||
| Total # HPE indicators | 1.3 | 1.5 | 0 | 8 |
| Lower home quality (2 + HPE indicators) | 34% | |||
| Lowest home quality (3 + HPE indicators) | 15% | |||
| Specific HPE indicators | ||||
| No patio or yard | 19% | |||
| Crowded | 20% | |||
| Unsafe inside house | 4% | |||
| Unsafe outside house | 3% | |||
| Dark inside house | 17% | |||
| No decorations on walls | 19% | |||
| Cluttered | 41% | |||
| Not clean | 18% | |||
| Child Characteristics | ||||
| Child age in years | 10.9 | 3.4 | 3 | 18 |
| Child obese | 22% | |||
| Child was sick in past few days | 12% | |||
| Child had infection in past 3 weeks | 3% | |||
| Child male | 53% | |||
| PCGa and Household Characteristics | ||||
| PCG is mother | 96% | |||
| PCG < high school degree | 36% | |||
| PCG U.S.-born | 47% | |||
| PCG non-Hispanic white | 25% | |||
| PCG Hispanic | 63% | |||
| PCG African American | 6% | |||
| PCG married | 59% | |||
| Family income to poverty ratio | 2.7 | 3.3 | 0 | 19.3 |
| Number of children in household | 2.5 | 1.1 | 1 | 7 |
Primary caregiver.
3.2. Measures
Inflammation is measured by the plasma equivalent concentration (in mg/L) of C-reactive protein (CRP) levels obtained from assaying reconstituted dried blood spots (McDade, 2007). Using a high sensitivity enzyme immunoassay, low levels of CRP can be detected in the blood. As previously stated, our outcome of interest is chronic, low-grade inflammation as a measure of physiological stress response in children. Thus, we limit our sample to children with CRP ≤ 10 mg/L. Although this cutoff has been established in studies of adults, it has been consistently used in research on children due to the lack of established cut offs for children (Broyles et al., 2012; Murasko, 2008; Warnberg et al., 2007).
The independent variables of interest are measures of the child’s home physical environment (HPE), including, whether the home: had no patio or yard, was unsafe inside, was unsafe outside, was dark/minimally lit, had little or monotonous décor, was crowded, was cluttered, and was unclean. The first measure (no patio/yard) was reported by the primary caregiver, while the other measures were observed by interviewers while they were in the home. Interviewers were trained and had a guide to follow during this observation process (Appendix A). Prompts were given for what the interviewers should look for in the home environment. Unsafe conditions in the home were indicated by the presence of one or more potentially dangerous health or structural hazards such as broken glass, peeling paint, or frayed electrical wires. The external home environment, including the yard, patio, porch, and/or exterior halls and stairs, was also rated for safety. Examples of unsafe exterior conditions included unlit entrance or stairway, broken steps, or large ditches. Households were considered crowded if there were many people living in a very small house or apartment, if it was difficult to find a private place to interview respondents, or if there were frequent interruptions and people bumping into each other. Clutter was indicated by the disorganization of objects in the home; such as, a vacuum cleaner, schoolwork, or shoes and socks left out. Cleanliness of homes was assessed by the level of trash, dirty dishes, or dust in visible rooms (Peterson et al., 2011).
These interviewer observations are similar to those used to measure the physical environment in the HOME scale (Bradley and Caldwell, 1979; Wen-jui, Leventhal and Linver, 2004) and in other studies of housing quality (Evans et al., 2000). Following past research on housing quality (Coley et al., 2013; Evans et al., 2000), these variables were dichotomized to reflect a negative home characteristic and then added together to produce a measure of the number of low-quality HPE indicators, ranging from 0 to 8. Research suggests that an overall housing quality index is more reliable than any specific indicator or subscale (Evans et al., 2000). We conducted a factor analysis and found one factor emerged for these 8 indicators. In addition to number of risk factors, we further characterized low-quality HPE as two or more and three or more low-quality indicators to test for threshold effects that may not be captured with a linear measure. As Table 1 shows, in this sample, the mean number of low-quality HPE indicators was 1.3, with 34% of children experiencing two or more and 15% three or more low-quality HPE conditions.
Child obesity, a potentially important predictor of inflammation and mediator of the HPE effects, was defined based on BMI (weight (kg)/height (m)2). Height and weight were measured by trained interviewers and BMI z-scores were calculated using age- and gender-specific growth curves of a reference population. We categorized a child as obese if their z-score was ≥95th percentile ≥95th percentile (Cole et al., 2000; Kuczmarski et al., 2002). In regression models we included a dummy variable for child obesity, with overweight or normal BMI as the omitted category. Including child overweight as a separate category from normal BMI did not change the results; and, the effect of overweight status was not significantly different from normal BMI.
Family income was included in regression models to assess the HPE effects net of economic status. In L.A.FANS, total family income sums all earned and transfer income (including income from government cash benefits and food stamps) and missing income data was imputed (Peterson et al., 2011). Using total family income, we calculated the income-to-poverty ratio by dividing income by the federal poverty line (FPL) for a given family size in the year for which the income was reported (the year prior to the survey year). In regression models we controlled for whether the measure included an imputed income component.
Other independent variables were child and primary caregiver control variables. Child-level controls included: child age, gender, recent illnesses (dummy), and recent infection (dummy). Primary caregiver controls included: immigrant status (born in the U.S.), race/ethnicity (White, Latino, African American, other), education (less than high school degree), self-reported depression (reported being depressed or on anti-depressants in the past year), marital status (married, separated/divorced, cohabiting, never married, widowed), number of children in the household, and number of years in the current home. Neighborhood poverty category was also included. L.A.FANS defined neighborhood poverty by the percent of the population living in poverty: very poor (the top 10% of the neighborhood poverty distribution), poor (those in the 60–89 percentiles of neighborhoods), and non-poor (those in the bottom 60% of the neighborhood poverty distribution) (Sastry et al., 2006).
3.3. Statistical methods
In developing our multivariate regression models, we logged the CRP measure and conducted Tobit regression analysis to account for censoring of the CRP values below the detectable level, consistent with past research in this area (Dowd et al., 2010). Standard errors were adjusted for heteroskedasticity and we used the cluster command in Stata to account for clustering of the data at the survey strata level. Research suggests that adjusting for clustering at higher geographic levels also accounts for clustering at lower levels, including the household level (Angeles et al., 2005; Cameron and Miller, 2015).
All regression analyses include the weights and control variables previously described. We report regression coefficients, which can be interpreted as percent change in CRP for each unit change in the independent variable. We conducted two-tailed tests of p < 0.05 for statistical significance.
Obesity mediation was assessed by entering the obesity variable sequentially to illustrate changes in associations between CRP and the independent variables when obesity was included. We also conducted Sobel-Goodman mediation tests to assess the statistical significance of obesity as a mediator of our HPE measures and family income.
To test for age moderation effects, we created child age*HPE interaction terms and included them in the regression models along with the main effect and control variables. We assessed the significance of the interaction terms, and the joint significance of the interaction terms with the HPE main effect variables when considering evidence of moderation.
4. Results
We first provide descriptive statistics for CRP and key child characteristics in L.A.FANS and in a national sample, the National Health and Nutrition Examination Survey (NHANES) during the same time period (2006–2008). We provide the NHANES data as a reference group, given the limited population-level data on CRP levels in children. Mean CRP among all children in the L.A.FANS sample is 2.5, compared to 1.7 in the U.S. (Table 2). When limited to those ≤10 mg/L, the focus of this study, mean CRP values are 1.1 in L.A. FANS and 0.93 in NHANES. Given that obesity and Mexican-American origin have been linked with higher CRP levels in children (Dowd et al., 2010), the higher CRP values in L.A.FANS may be due to the higher percentage of Hispanic and obese children in L.A. compared with the nation as a whole (see Table 2).
Table 2.
Weighted descriptive statistics for children ages 3–18 years National Health and Nutrition Examination Survey (NHANES) and L.A.FANS Wave 2.
| Meana | Std. dev.a | Minb | Maxa | % CRP ≤10 mg/L | Mean age | % Male | % Hispanic | % Obese | |
|---|---|---|---|---|---|---|---|---|---|
| NHANES (2005–2008) | |||||||||
| All (N = 4304) | 1.7 | 5.7 | 0.1 | 136 | 96% | 12 | 51% | 19% | 12% |
| CRP ≤10 mg/L | 0.93 | 1.7 | 0.1 | 10 | 12 | 51% | 18% | 12% | |
| L.A.FANS (2006–2008) | |||||||||
| All (N = 404) | 2.5 | 5.4 | 0.078 | 63 | 95% | 11 | 51% | 60% | 25% |
| CRP ≤10 mg/L | 1.1 | 1.9 | 0.078 | 10 | 11 | 53% | 61% | 22% | |
All CRP values in mg/L.
Determined by the lab’s lowest detection level.
Turning to the regression results, Table 3 shows the associations between the HPE measures and CRP in children with CRP ≤10 mg/L. As Model 1 shows, the total number of low-quality HPE indicators was associated with CRP, independent of income and other socio-demographic controls, increasing CRP by 11% with each additional indicator. Models 2 and 3 indicate the significance of HPE threshold effects; children in homes with two or more low-quality HPE indicators had, on average, 30% higher CRP than those with 0 or 1 indicator. Those in the riskiest home environments (3+ low-quality HPE indicators) had 62% higher CRP than those in homes with 0–2 negative HPE indicators.
Table 3.
Weighted Tobit regression models of CRP in Children 3–18 years with CRP≤10 mg/L. L.A.FANS Wave 2, N = 353.
| Models
| |||||
|---|---|---|---|---|---|
| Variables | (1) | (2) | (3) | (4) | (5) |
| Home Physical Environment (HPE) | |||||
| Total low-quality HPE indicators | 0.11** | ||||
| (0.028) | |||||
| 2+ low-quality HPE indicators | 0.29** | 0.20* | |||
| (0.040) | (0.100) | ||||
| 3+ low-quality HPE indicators | 0.62** | 0.34* | |||
| (0.075) | (0.14) | ||||
| Child characteristics | |||||
| Obese | 0.87* | 0.83* | |||
| (0.34) | (0.35) | ||||
| Age | −0.014 | −0.014 | −0.011 | −0.016 | −0.015 |
| (0.031) | (0.032) | (0.033) | (0.037) | (0.037) | |
| Recently ill | −0.092 | −0.092 | −0.13 | 0.059 | 0.041 |
| (0.80) | (0.77) | (0.79) | (0.73) | (0.74) | |
| Infection in past 3 weeks | 0.90 | 0.93 | 0.82 | 0.55 | 0.51 |
| (0.50) | (0.48) | (0.48) | (0.65) | (0.64) | |
| Male | −0.57** | −0.57* | −0.55** | −0.55* | −0.54** |
| (0.22) | (0.23) | (0.21) | (0.21) | (0.20) | |
| PCGa and Household Controls | |||||
| PCG U.S. born | −0.093** | −0.081** | −0.081 | 0.068 | 0.047 |
| (0.018) | (0.021) | (0.050) | (0.11) | (0.12) | |
| PCG Hispanicb | −0.12 | −0.12 | −0.17 | −0.15 | −0.19 |
| (0.26) | (0.27) | (0.27) | (0.17) | (0.19) | |
| PCG African Americanb | −0.26 | −0.30 | −0.13 | −0.26 | −0.17 |
| (0.34) | (0.32) | (0.33) | (0.31) | (0.31) | |
| PCG other raceb | −0.66** | −0.71** | −0.73** | −0.52** | −0.55** |
| (0.089) | (0.086) | (0.11) | (0.056) | (0.088) | |
| Family income-to-poverty ratio | −0.027 | −0.031** | −0.029* | −0.019 | −0.019 |
|
| |||||
| (0.015) | (0.011) | (0.014) | (0.0099) | (0.011) | |
| Log likelihood | −424 | −424 | −422 | −410 | −410 |
|
| |||||
| Sobel-Goodman mediation tests: Income by HPE | n.s. | n.s. | n.s. | ||
| HPE by obesity | * | ** | |||
| Income by obesity | ** | ** | |||
Robust standard errors in parentheses.
p < 0.01,
p < 0.05.
PCG = Primary caregiver. All control variables included in models; insignificant household and PCG controls not shown for brevity.
Ref: non-Hispanic white.
In Models 2 and 3, the family income-to-poverty ratio (IPR) was significantly associated with lower CRP, although the effect was quite small. Moving from being at the poverty line (IPR = 1) to income two times the poverty line (IPR = 2) was associated with a 3% decline in CRP. Although the small association between income and CRP could be due to mediation by HPE, we found no evidence of mediation in supplemental analyses (reported at the bottom of Table 3). Most other control variables were not associated with inflammation, with the exception of child gender (boys had lower inflammation, on average, than girls) and primary caregiver’s (PCG) immigrant status (in some models). The effect of PCG “other race” was also significant, but few of our sample children had PCGs in this category (6%).
Models 4 and 5 present the results from regression models controlling for child obesity. Not surprisingly, obese children had significantly higher CRP than overweight and normal BMI children. We also found evidence that obesity mediated part of the HPE effects, with significant attenuation of the HPE indicators when controlling for obesity and significant Sobel-Goodman tests (reported at the bottom of Table 3). Obesity mediated the small effect of income as well.
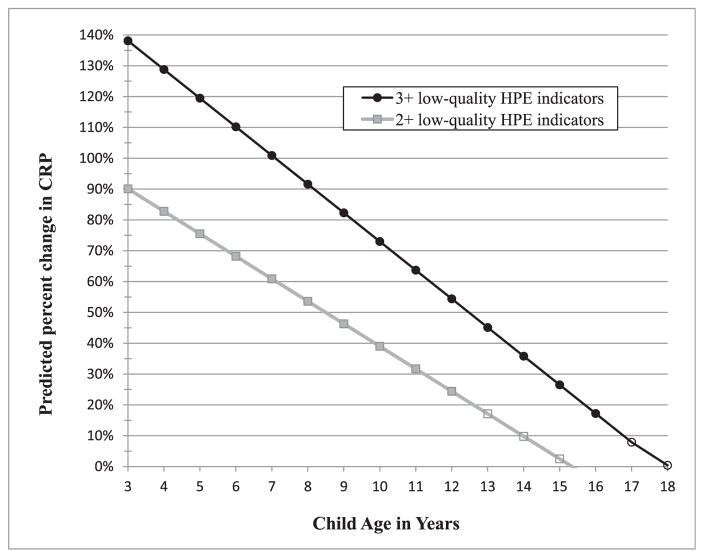
Table 4 shows our results when assessing the role of child age as a moderator of the HPE effects. We found negative age interactions and joint significance of the HPE threshold variables with the age interactions (F-tests indicated at the bottom of Table 4). The negative interaction effects indicate that the associations between the HPE and children’s CRP become smaller with increasing child age. The joint effect of the HPE and age interaction variables remained significant even when controlling for obesity (Table 4, Models 9 & 10).
Table 4.
Weighted Tobit regression models of CRP in Children 3–18 years with CRP≤10 mg/L including home physical environment* child age interaction effects. L.A.FANS Wave 2, N = 353.
| Variables | Models
|
|||
|---|---|---|---|---|
| Age interactions
|
Controlling for child obesity
|
|||
| (7) | (8) | (9) | (10) | |
| 2+ low-quality HPE indicators | 1.12** (0.38) | 0.94** (0.27) | ||
| 3+ low-quality HPE indicators | 1.66** (0.34) | 1.09* (0.54) | ||
| Age* HPE interaction | −0.073 (0.037) | −0.093** (0.029) | −0.065* (0.030) | −0.066 (0.039) |
| Child age | 0.0056 (0.027) | 0.0025 (0.037) | 0.0016 (0.036) | −0.0050 (0.042) |
| Child obese | 0.85* (0.34) | 0.81* (0.38) | ||
| F-test joint significance HPE main effects and HPE* age interaction terms | ** | ** | ** | * |
Robust standard errors in parentheses.
p < 0.01,
p < 0.05.
All control variables included in all models but not shown for brevity.
To provide an interpretation of the age effects, Fig. 1 shows the predicted percent change in CRP by age for children who were exposed to two or more and three or more low-quality HPE indicators. These effects were calculated based on results from Models 7 and 8. As the figure illustrates, young children had the highest predicted increases in CRP in these risky home environments, with substantially higher CRP among children in households with three or more low-quality HPE indicators. Although the effect size decreased with age, it remained significant through age 16 for children living in homes with three or more low-quality HPE indicators. The effects were smaller, but still strong, for those exposed to two or more low-quality HPE indicators. The association between CRP and 2+ HPE indicators became insignificant after age 12.
Fig. 1.
Predicted percent change in CRP by child age for children 3–18 years with CRP ≤10 mg/L. Based on results from Models (7) & (8).
5. Discussion
Despite general improvements in living conditions of children in the U.S. over the past 40 years, research suggests that large inequalities in home quality remain (Bradley et al., 2001; Conley, 2001; Evans et al., 2005). Recent findings suggest that housing conditions are critical to understanding the lives of low-income families with children and that housing quality, compared to other housing measures, is most strongly associated with child emotional, behavioral and cognitive development (Coley et al., 2013).
In this study, we considered how housing conditions measured as the home physical environment (HPE) contributed to inequalities in biological markers of stress in children. Our outcome, low-grade inflammation assessed by CRP levels, is an important indicator of a dysregulated immune system linked to exposure to chronic stress (Kemeny, 2009). Elevated inflammation is also currently being explored as a potential correlate of depression in children (Heim and Binder, 2012), as well as other health conditions that emerge during childhood and later in the life course (Crosswell et al., 2014; Slopen et al., 2012).
Using data from Los Angeles County, we found that a substantial portion of children (34%) experienced two or more physical risk factors in their HPE, and 15% lived in homes with 3 or more physical risk factors. The total number of low-quality HPE indicators and categorical risk level (2 + and 3+ low-quality indicators) were associated with higher CRP levels net of control variables. The effect of living in a home with three or more risk factors was particularly high, increasing CRP by an estimated 62%.
We also explored the role of obesity in mediating the associations between the HPE and CRP. Our results partially supported this hypothesis, with some of the HPE effects working through increased risk of child obesity. Further analyses indicated that the HPE had an important effect on obesity net of the control variables. This may reflect, in part, cumulated biological responses to chronic stressors and stress-coping behaviors (e.g., unhealthful eating, TV-watching) among children with low-quality HPE. It may also be that low-quality HPE restricted the physical activity of children. Both psychosocial stress and reduced activity have the potential to increase obesity risk in children (Wilson and Sato, 2014).
It is important to note that living in homes with multiple physical risk factors was associated with 20–30% higher CRP when controlling for obesity. Thus, the physical conditions of the home were associated with immune system dysregulation in children that reflected not only increases in adiposity, but also immune system changes potentially related to exposure to chronic psychosocial stressors (Charmandari et al., 2012; Kemeny, 2009).
The negative HPE effects were particularly pronounced in younger children, with smaller, but still significant associations in adolescents. This finding is consistent with prior research on housing and children’s emotional and behavioral outcomes (Coley et al., 2013). These findings may indicate that young children are particularly vulnerable to household disadvantage because the majority of their time is spent in the home and, unlike adolescents, they are unable to escape poor home conditions (West, 1997; West and Sweeting, 2004). It may also be that young children are more susceptible to the psychosocial threats related to poor physical qualities in the home than are older children.
There are many challenges to conducting research on bio-social processes. One such challenge is the lack of adequate data, including longitudinal data and large, population-based samples, particularly among children. This study focused on children from L.A. County and provided a snapshot of their home environment and physiological health at one point in time. This limits the generalizability to only children in L.A., and also carries the risk of null findings due to small numbers, less variability, and potential measurement error in estimating associations. The relatively small sample size (N = 353) also makes sub-population analyses difficult. Although child age interactions with HPE were statistically significant, the age-specific effects should be viewed with caution due to the relatively small number of children at each age.
In our models, socio-demographic variables that should reflect disadvantage and stress exposure, such as low primary caregiver education and single-parent households were not associated with inflammation, unlike studies of other health outcomes in children (Goodman et al., 2005; Schmeer, 2012). This may be due to sample size or because the sample was 60% Hispanic and had a large percent of immigrant households. It may also be that inflammation is more sensitive to proximate stressors, rather than larger socioeconomic conditions. For example, parental education was not associated with CRP in a national sample of children (Dowd et al., 2010), neighborhood poverty was not associated with elevated CRP in a sample of Louisiana children (Broyles et al., 2012), and little is known about associations between family structure and inflammation in children. Thus, more research is required to establish which social and demographic characteristics of children’s environments are associated with inflammation.
This study is also limited by relying on interviewer assessed home quality. Although interviewers were trained and given guidelines to follow during their rating process, we do not have a measure of inter-rater reliability to determine how successful the training was in producing consistent results across interviewers. We tested models including interviewer effects, and the results were unchanged. The use of biomarker data collected by technicians for our dependent variable eliminated concerns about error in the dependent variable being correlated with interviewer observations. Further, past research suggests that interviewer-rated home observations are preferred over respondents’ reports of home qualities (Evans et al., 2001b).
Despite the limitations, this research contributes to our understanding of health inequalities in children and the potential role of chronic stress underlying these inequalities. More specifically, our research suggests that housing conditions, and the related home environment, have potentially important implications for child well-being, net of other social and economic characteristics of the family. The finding that younger children had higher risks of elevated inflammation in homes with poor physical conditions suggests that biological embedding of disadvantage may begin early in the life course.
This research also points to the need to address housing issues as part of policies and programs aimed at improving child health. Although social structures, such as socio-economic position and race/ethnicityclearly shape individuals’ health status, living conditions are more amenable to targeted policy efforts. Further research is needed to assess whether policies and programs that provide housing assistance to improve the home physical environment could reduce stress and improve health outcomes in children within existing structural constraints.
Acknowledgments
We thank Narayan Sastry and Chris Peterson for access to the L.A. FANS biomarker data and helpful advice related to using these data. This research was funded in part by a K01 grant awarded to Schmeer through the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) of the National Institutes of Health (NIH), 5 K01 HD077063-02. Support for this project also was provided through a seed grant awarded to Schmeer by the Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver NICHD of NIH, P2CHD058484, and a Center for Poverty Research Small Grant from the University of California, Davis. Funding for the Small Grants Competition was made possible in part by grant number AE00102 from the U.S. Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver NICHD, the NIH, or the Department of Health and Human Services.
Appendix A
Pebley, Anne R., and Narayan Sastry. 2004. “The Los Angeles Family and Neighborhood Survey: Field Interviewer Manual.” Santa Monica, CA.
Excerpt from the Field Interviewer Manual (Pp. 8–163—8–166) [All text is quoted directly from the manual. Italics added to indicate instructions guiding the interviewer’s observations.]:
Now you will take the computer back from the respondent and answer some observation questions about the household. Tell respondents you have a few administrative things to take care of on the computer that will take you a few minutes—that they can take a break until you finish.
The objective of these questions is to collect information about the physical environment and factors that may have an impact on children. You will read these questions to yourself and base your answers on what you know or have seen—do not explore the home in an attempt to better or more completely answer the questions. Do not discuss your observations with anyone in the household. This may be difficult if you see a hazard you feel could put a child at risk of injury. In cases such as these, talk to your FS.
Unsafe interior
The first of these household observation questions appears below:
ENVIRONMENT INSIDE HOME IS UNSAFE FOR YOUNG CHILDREN, ONE OR MORE POTENTIALLY DANGEROUS HEALTH OR STRUCTURAL HAZARDS. (EX: FRAYED ELECTRICAL WIRES, MICE OR RATS, GLASS, POISONS, FALLING PLASTER, BROKEN STAIRS, PEELING PAINT, CLEANING MATERIALS LEFT OUT, FLAMES AND HEAT WITHIN REACH OF YOUNG CHILD.)
Note the things in the interior of the house that might be dangerous to a young child and that you can actually see. However, remember that you are not doing a safety inspection—you’re looking for things that create an obvious health or safety risk to a child. Look for signs that would indicate health or structural hazards. For example, you may not see a mouse but you may notice mouse droppings. Or if none of the kitchen cabinets have doors on them, you may assume that the child could have access to any hazardous materials that are in the cabinets. Or if the face plates are missing from sockets and electrical switches, consider that hazardous as well. Remember that for this question you are only recording your observations about the inside of the house. If you see any of the items mentioned in the examples on the outside of the house or in the hallways or other common areas of an apartment building but do not see anything hazardous inside the home, indicate “No” for this question.
Unsafe exterior
The next question asks about the outside of the home:
ENVIRONMENT OUTSIDE HOME (YARD, PATIO, ENTRYWAY OR PORCH, HALLS AND STAIRS) IS UNSAFE FOR YOUNG CHILDREN. (EX: UNLIT ENTRANCE OR STAIRWAY, BROKEN STEPS, BROKEN GLASS, BROKEN TOYS, LARGE DITCHES, ALCOHOL OR DRUG PARAPHENALIA).
For this question, note those things on the outside of the house may be dangerous to a young child. In addition to the examples given in the question, rusty metal objects, discarded refrigerators with doors attached, and discarded condoms may be considered hazardous and pose an obvious health or safety risk to a child. If you see any of the items mentioned in the examples on the inside of the house but do not see anything hazardous outside the home or in the hallways or other common areas of an apartment building, answer “No” for this question.
Lighting
The next question is about the amount of light in the home:
INSIDE OF HOME IS DARK. (EX: DARK ROOMS OR DRAPES)
We ask this question because dark rooms with little light are less stimulating to a child. Answer.
“Yes” if the room or rooms you have seen have relatively little light or are fairly dark.
Décor
For the next question, you will need to determine if the house visually stimulating:
HOUSEHOLD HAS NO DECORATION OR DECOR IS MONOTONOUS. (EX: NO PICTURES OR NICK-NACKS, NO PLANTS, NO OR VERY LITTLE FURNITURE IN LIVING ROOM OR DINING ROOM)
You are not rating the respondent’s taste in decor. A respondent may live in a house that uses a lot of colors that you find unappealing, but it may still be visually stimulating. If the house has no pictures on the walls or no knickknacks, plants, sculptures, statues, or other items or color schemes that draw your eye, answer “Yes.”
Crowding
In the next question, you will need to determine if the house is crowded:
INSIDE OF HOME IS CROWDED. (EX: MANY PEOPLE LIVING IN A VERY SMALL HOUSE OR APARTMENT, DIFFICULT TO FIND A PRIVATE PLACE TO INTERVIEW RESPONDENTS, FREQUENT INTERRUPTIONS AND PEOPLE BUMPING INTO EACH OTHER).
If there are many people living in a small household (as indicated on the household roster) but you do not feel it is crowded, answer “No.” However, if the interview was interrupted or others were observing or distracting you or the respondent because there is no private space, answer “Yes.”
Clutter
Now you will need to assess the amount of clutter:
ALL VISIBLE ROOMS OF HOUSE/APARTMENT ARE MINIMALLY CLUTTERED OR NOT CLUTTERED AT ALL. (EX: VISIBLE ROOMS ARE NEAT OR ARE MINIMALLY CLUTTERED WITH CLOTHES, VACUUM CLEANER, CHILDREN’S SCHOOL WORK, SHOES AND SOCKS, OTHER OBJECTS).
Clutter may be a hazard to children, so observe the amount of disorder in the home’s physical environment. Look to see if toys, clothes, books, dishes, or other items are out of place—for instance, they are on the floor, tables, shelves, or scattered throughout the house. If there are small children, you will probably see some clutter—the amount of clutter may grow, the longer you remain in the household. Observe and record what you see.
Cleanliness
The next question asks about the cleanliness of the home:
ALL VISIBLE ROOMS OF THE HOUSE/APARTMENT ARE CLEAN OR REASONABLY CLEAN. (EX: NO TRASH STREWN AROUND, NO OR FEW DIRTY DISHES IN KITCHEN, FLOOR AND FURNITURE HAVE BEEN CLEANED OR DUSTED FAIRLY RECENTLY).
A clean home provides a healthier environment for children. Notice if there are empty food containers, newspapers, junk mail, catalogues, magazines, etc., on the tables, countertops, floors, or strewn about may indicate a house that is not very clean. Notice the trash—is it overflowing? Does it have an odor? If there is a baby in the house, there may be an odor if a diaper needs to be changed or the lid to the diaper pail or trash is not airtight. If you see dust in the corners, dirty dishes stacked on the counters or table, or other signs of a dirty environment, answer “No” for this question. If the household is reasonably clean, answer “Yes.”
References
- Angeles G, Guilkey DK, Mroz TA. The impact of community-level variables on individual-level outcomes: theoretical results and applications. Sociol Methods Res. 2005;34(1):76–121. [Google Scholar]
- Barocas R, Seifer R, Sameroff AJ. Defining environmental risk - multiple dimensions of psychological vulnerability. Am J Community Psychol. 1985;13(4):433–447. doi: 10.1007/BF00911218. [DOI] [PubMed] [Google Scholar]
- Bauer Amy M, Thomas Boyce W. Prophecies of childhood: how children’s social environments and biological propensities affect the health of populations. Int J Behav Med. 2004;11(3):164–175. doi: 10.1207/s15327558ijbm1103_5. [DOI] [PubMed] [Google Scholar]
- Bradley Robert H, Caldwell Bettye M. Home observations for measurement of the environment – revision of the preschool scale. Am J Ment Defic. 1979;84(3):235–244. [PubMed] [Google Scholar]
- Bradley Robert H, Corwyn Robert F, Harriette Pipes McAdoo, Cynthia García Coll. The home environments of children in the United States Part I: variations by age, ethnicity, and poverty status. Child Dev. 2001;72(6):1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- Breysse P, Farr N, Galke W, Lanphear B, Morley R, Bergofsky L. The relationship between housing and health: children at risk. Environ Health Perspect. 2004;112(15):1583–1588. doi: 10.1289/ehp.7157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The bioecological model from a life course perspective: reflections of a participant observer. In: Moen P, Elder J, Glen H, Lüscher K, Bronfenbrenner U, editors. Examining Lives in Context: Perspectiveson the Ecology of Human Development. American Psychological Association; Washington, D.C: 1995. pp. 599–618. [Google Scholar]
- Bronfenbrenner U. The bioecological theory of human development. In: Smelser N, Baltes P, editors. International Encyclopedia of the Social and Behavioral Sciences. Elsevier; New York: 2001. [Google Scholar]
- Bronfenbrenner U, Evans GW. Developmental science in the 21st century: emerging questions, theoretical models, research designs and empirical findings. Soc Dev. 2000;9(1):115–125. [Google Scholar]
- Broyles ST, Staiano AE, Drazba KT, Gupta AK, Sothern M, Katzmarzyk PT. Elevated C-Reactive protein in children from risky neighborhoods: evidence for a stress pathway linking neighborhoods and inflammation in children. Plos One. 2012;7(9) doi: 10.1371/journal.pone.0045419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Housing Partnership Corporation; California Housing Partnership Corporation, editor. How Los Angeles County’s Housing Market Is Failing to Meet the Needs of Low-income Families. 2014. California Housing Partnership Corporation. [Google Scholar]
- Cameron AC, Miller DL. A Practitioner’s guide to cluster-robust inference. J Hum Resour. 2015;50(2):317–372. [Google Scholar]
- Charmandari E, Achermann JC, Carel JC, Soder O, Chrousos GP. Stress response and child health. Sci Signal. 2012;5(248) doi: 10.1126/scisignal.2003595. [DOI] [PubMed] [Google Scholar]
- Chen E, Martin AD, Matthews KA. Socioeconomic status and health: do gradients differ within childhood and adolescence? Soc Sci Med. 2006;62(9):2161–2170. doi: 10.1016/j.socscimed.2005.08.054. [DOI] [PubMed] [Google Scholar]
- Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: how and why do these relationships change with age? Psychol Bull. 2002;128(2):295–329. doi: 10.1037/0033-2909.128.2.295. [DOI] [PubMed] [Google Scholar]
- Chiang JJ, Bower JE, Almeida DM, Irwin MR, Seeman TE, Fuligni AJ. Socioeconomic status, daily affective and social experiences, and inflammation during adolescence. Psychosom Med. 2015;77(3):256–266. doi: 10.1097/PSY.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Handley ED, Rogosch FA. Child maltreatment, inflammation, and internalizing symptoms: investigating the roles of C-reactive protein, gene variation, and neuroendocrine regulation. Dev Psychopathol. 2015;27(2):553–566. doi: 10.1017/S0954579415000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon, Spacapan Shirlynn. The social psychology of noise. In: Jones DM, Chapman AJ, editors. Noise and Society. John Wiley & Sons; Chichester: 1984. [Google Scholar]
- Cole Tim J, Bellizzi Mary C, Flegal Katherine M, Dietz William H. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ Br Med J. 2000;320(7244):1240–1240. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley D. A room with a view or a room of one’s own? Housing and social stratification. Sociol Forum. 2001;16(2):263–280. [Google Scholar]
- Coley RL, Leventhal T, Lynch AD, Kull M. Relations between housing characteristics and the well-being of low-income children and adolescents. Dev Psychol. 2013;49(9):1775–1789. doi: 10.1037/a0031033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Donnellan MB. Annual Review of Psychology. Annual Reviews; Palo Alto: 2007. An interactionist perspective on the socioeconomic context of human development; pp. 175–199. [DOI] [PubMed] [Google Scholar]
- Crosswell AD, Bower JE, Ganz PA. Childhood adversity and inflammation in breast cancer survivors. Psychosom Med. 2014;76(3):208–214. doi: 10.1097/PSY.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, Geppert J, de Cuba SE, Heeren T, Coleman S, Rose-Jacobs R, Frank DA. Us housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, Caspi A, Williams B, Ambler A, Sugden K, Mika J, Arseneault L. Biological embedding of stress through inflammation processes in childhood. Mol Psychiatry. 2011;16(3):244–246. doi: 10.1038/mp.2010.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado J, Ramirez-Cardich ME, Gilman RH, Lavarello R, Dahodwala N, Bazan A, Rodriguez V, Cama RI, Tovar M, Lescano A. Risk factors for burns in children: crowding, poverty, and poor maternal education. Inj Prev. 2002;8(1):38–41. doi: 10.1136/ip.8.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd JB, Zajacova A, Aiello AE. Predictors of inflammation in U.S. Children aged 3–16 years. Am J Prev Med. 2010;39(4):314–320. doi: 10.1016/j.amepre.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunifon R, Duncan GJ, Brooks-Gunn J. The long-term impact of parental organization and efficiency. In: Kalil A, DeLeire T, editors. Family Investments in Children’s Potential: Resources Parenting Behaviors that Promote Success. Lawrence Erlbaum Assoc Publ; Mahwah: 2004. [Google Scholar]
- Dush CMK, Schmeer KK, Taylor M. Chaos as a social determinant of child health: reciprocal associations? Soc Sci Med. 2013;95:69–76. doi: 10.1016/j.socscimed.2013.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans Gary W. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol. 2003;39(5):924–933. doi: 10.1037/0012-1649.39.5.924. [DOI] [PubMed] [Google Scholar]
- Evans GW. Child development and the physical environment. Annu Rev Psychol vol. 2006;57:423–451. doi: 10.1146/annurev.psych.57.102904.190057. [DOI] [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Dev. 2002;73(4):1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Evans GW, Lercher P, Meis M, Ising H, Kofler WW. Community noise exposure and stress in children. J Acoust Soc Am. 2001a;109(3):1023–1027. doi: 10.1121/1.1340642. [DOI] [PubMed] [Google Scholar]
- Evans GW, Saltzman H, Cooperman JL. Housing quality and Children’s socioemotional health. Environ Behav. 2001b;33(3):389–399. [Google Scholar]
- Evans GW, Wells NM, Chan HYE, Saltzman H. Housing quality and mental health. J Consult Clin Psychol. 2000;68(3):526–530. doi: 10.1037//0022-006x.68.3.526. [DOI] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children’s socioemotional adjustment. Psychol Sci. 2005;16(7):560–565. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- Fagundes CP, Glaser R, Kiecolt-Glaser JK. Stressful early life experiences and immune dysregulation across the lifespan. Brain Behav Immun. 2013;27:8–12. doi: 10.1016/j.bbi.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Telzer EH, Bower J, Cole SW, Kiang L, Irwin MR. A preliminary study of daily interpersonal stress and C-Reactive protein levels among adolescents from latin American and European backgrounds. Psychosom Med. 2009;71(3):329–333. doi: 10.1097/PSY.0b013e3181921b1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garasky S, Stewart SD, Gundersen C, Lohman BJ, Eisenmann JC. Family stressors and child obesity. Soc Sci Res. 2009;38(4):755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Gonzalez A. The impact of childhood maltreatment on biological systems: implications for clinical interventions. Paediatr Child Health. 2013;18(8):415–418. [PMC free article] [PubMed] [Google Scholar]
- Goodman E, McEwen BS, Huang B, Dolan LM, Adler NE. Social inequalities in biomarkers of cardiovascular risk in adolescence. Psychosom Med. 2005;67(1):9–15. doi: 10.1097/01.psy.0000149254.36133.1a. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12(501):e54–e63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- Heim Christine, Binder Elisabeth B. Current research trends in early life stress and depression: review of human studies on sensitive periods, gene–environment interactions, and epigenetics. Exp Neurol. 2012;233(1):102–111. doi: 10.1016/j.expneurol.2011.10.032. [DOI] [PubMed] [Google Scholar]
- Hohmann C, Grabenhenrich L, de Kluizenaar Y, Tischer C, Heinrich J, Chen CM, Keil T. Health effects of chronic noise exposure in pregnancy and childhood: a systematic review initiated by ENRIECO. Int J Hyg Environ Health. 2013;216(3):217–229. doi: 10.1016/j.ijheh.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Holupka C Scott, Newman Sandra J. The housing and neighborhood conditions of America’s children: patterns and trends over four decades. Hous Policy Debate. 2011;21(2):215–245. [Google Scholar]
- Keller PS, El-Sheikh M, Granger DA, Buckhalt JA. Interactions between salivary cortisol and alpha-amylase as predictors of children’s cognitive functioning and academic performance. Physiol Behav. 2012;105(4):987–995. doi: 10.1016/j.physbeh.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Kemeny ME. Psychobiological responses to social threat: evolution of a psychological model in psychoneuroimmunology. Brain Behav Immun. 2009;23(1):1–9. doi: 10.1016/j.bbi.2008.08.008. [DOI] [PubMed] [Google Scholar]
- Kids Count Data Center. Children Living in Crowded Housing. Annie E. Casey Foundation; Baltimore, MD: 2014. [Google Scholar]
- Kim JW, Szigethy EM, Melhem NM, Saghafi EM, Brent DA. Inflammatory markers and the pathogenesis of pediatric depression and suicide: a systematic review of the literature. J Clin Psychiatry. 2014;75(11):1242–1253. doi: 10.4088/JCP.13r08898. [DOI] [PubMed] [Google Scholar]
- Koger Susan M, Schettler Ted, Weiss Bernard. Environmental toxicants and developmental disabilities: a challenge for psychologists. Am Psychol. 2005;60(3):243–255. doi: 10.1037/0003-066X.60.3.243. [DOI] [PubMed] [Google Scholar]
- Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Leventhal Tama, Newman Sandra. Housing and child development. Child Youth Serv Rev. 2010;32(9):1165–1174. [Google Scholar]
- Lumeng JC, Miller A, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, Vazquez DM. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72. doi: 10.1016/j.appet.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maitland C, Stratton G, Foster S, Braham R, Rosenberg M. A place for play? the influence of the home physical environment on children’s physical activity and sedentary behaviour. Int J Behav Nutr Phys Activity. 2013;10 doi: 10.1186/1479-5868-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino AJ, Fletcher EN, Whitaker RC, Anderson SE. Amount and environmental predictors of outdoor playtime at home and school: a cross-sectional analysis of a national sample of preschool-aged children attending Head Start. Health Place. 2012;18(6):1224–1230. doi: 10.1016/j.healthplace.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdy LE, Winterbottom KE, Mehta SS, Roberts JR. Using nature and outdoor activity to improve Children’s health. Curr Problems Pediatr Adolesc Health Care. 2010;40(5):102–117. doi: 10.1016/j.cppeds.2010.02.003. [DOI] [PubMed] [Google Scholar]
- McDade TW. Measuring immune function: markers of cell-mediated immunity and inflammation in dried blood spots. In: Ice GH, James GD, editors. Measuring Stress in Humans: a Practical Guide for the Field. Vol. 49. 2007. pp. 181–207. [Google Scholar]
- McDade TW. Early environments and the ecology of inflammation. Proc Natl Acad Sci U S A. 2012;109:17281–17288. doi: 10.1073/pnas.1202244109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Brody GH, Yu TY, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proc Natl Acad Sci U S A. 2014;111(31):11287–11292. doi: 10.1073/pnas.1406578111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Cole SW. Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biol Psychiatry. 2012;72(1):34–40. doi: 10.1016/j.biopsych.2012.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murasko JE. Male-female differences in the association between socioeconomic status and atherosclerotic risk in adolescents. Soc Sci Med. 2008;67(11):1889–1897. doi: 10.1016/j.socscimed.2008.09.018. [DOI] [PubMed] [Google Scholar]
- O’Hara Kate. How Are We Housed? the Continuing Struggle for Decent, Affordable Housing in Los Angeles 1990–2000. Southern California Association of Non-Profit Housing; 2002. [Google Scholar]
- Pervanidou Panagiota, Chrousos George P. Metabolic consequences of stress during childhood and adolescence. Metabolism. 2012;61(5):611–619. doi: 10.1016/j.metabol.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Peterson CE, Pebley AR, Sastry N, Yuhas K, Ghosh-Dastidar B, Haas AC, Bitler MP. Corporation, R, editor. Working Paper. RAND Corporation; 2011. The Los Angeles familyand neighborhood survey, wave 2 User’s guide and codebook; pp. 1–131. [Google Scholar]
- Quist JS, Sjodin A, Chaput JP, Hjorth MF. Sleep and cardiometabolic risk in children and adolescents. Sleep Med Rev. 2015;29:76–100. doi: 10.1016/j.smrv.2015.09.001. [DOI] [PubMed] [Google Scholar]
- Sastry Narayan, Ghosh-Dastidar Bonnie, Adams John, Pebley Anne R. The design of a multilevel survey of children, families, and communities: the Los Angeles Family and Neighborhood Survey. Soc Sci Res. 2006;35(4):1000–1024. [Google Scholar]
- Schmeer KK. Family structure and obesity in early childhood. Soc Sci Res. 2012;41(4):820–832. doi: 10.1016/j.ssresearch.2012.01.007. [DOI] [PubMed] [Google Scholar]
- Slopen N, Koenen KC, Kubzansky LD. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: a systematic review. Brain Behav Immun. 2012;26(2):239–250. doi: 10.1016/j.bbi.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Slopen N, Kubzansky LD, Koenen KC. Internalizing and externalizing behaviors predict elevated inflammatory markers in childhood. Psycho-neuroendocrinology. 2013a;38(12):2854–2862. doi: 10.1016/j.psyneuen.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Slopen N, Kubzansky LD, McLaughlin KA, Koenen KC. Childhood adversity and inflammatory processes in youth: a prospective study. Psychoneuroendocrinology. 2013b;38(2):188–200. doi: 10.1016/j.psyneuen.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Duarte CS, Sandel MT, Wright RJ. Social and environmental stressors in the home and childhood asthma. J Epidemiol Community Health. 2010;64(7):636–642. doi: 10.1136/jech.2008.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Low-grade systemic inflammation in overweight children. Pediatrics. 2001;107(1):e13. doi: 10.1542/peds.107.1.e13. [DOI] [PubMed] [Google Scholar]
- Warnberg J, Nova E, Romeo J, Moreno LA, Sjostrom M, Marcos A. Lifestyle-related determinants of inflammation in adolescence. Br J Nutr. 2007;98:S116–S120. doi: 10.1017/S0007114507839614. [DOI] [PubMed] [Google Scholar]
- Wells NM, Evans GW. Nearby nature: a buffer of life stress among rural children. Environ Behav. 2003;35(3):311–330. http://dx.doi.org/10.1177/0013916503035003001. [Google Scholar]
- Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. Am J Public Health. 2010;100(12):2507–2512. doi: 10.2105/AJPH.2009.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen-jui Han, Leventhal Tama, Linver Miriam R. The home observation for measurement of the environment (HOME) in middle childhood: a study of three large-scale data sets. Parent Sci Pract. 2004;4(2/3):189–210. [Google Scholar]
- West P. Health inequalities in the early years: is there equalisation in youth? Soc Sci Med. 1997;44(6):833–858. doi: 10.1016/s0277-9536(96)00188-8. [DOI] [PubMed] [Google Scholar]
- West P, Sweeting H. Evidence on equalisation in health in youth from the West of Scotland. Soc Sci Med. 2004;59(1):13–27. doi: 10.1016/j.socscimed.2003.12.004. [DOI] [PubMed] [Google Scholar]
- Wilson SM, Sato AF. Stress and paediatric obesity: what we know and where to go. Stress Health. 2014;30(2):91–102. doi: 10.1002/smi.2501. [DOI] [PubMed] [Google Scholar]