Abstract
Introduction
Traumatic brain injury (TBI) is a major cause of death and disability worldwide. The deleterious effects of secondary brain injury may be attenuated by early pharmacological therapy in the emergency room and intensive care unit (ICU). Current medical management of acute TBI is primarily supportive, aimed at reducing intracranial pressure (ICP) and optimizing cerebral perfusion. There are no pharmacological therapies to date that have been unequivocally demonstrated to improve neurological outcomes after TBI.
Objectives
The purpose of this systematic review was to evaluate the recent clinical studies from January 2013 through November 2015 that investigated neuroprotective functional outcomes of pharmacological agents after TBI.
Methods
The following databases were searched for relevant studies: MEDLINE (OvidSP January Week 1, 2013–November Week 2 2015), Embase (OvidSP 2013 January 1–2015 November 24), and the unindexed material in PubMed (National Library of Medicine/National Institutes of Health [NLM/NIH]). This systematic review included only full-length clinical studies and case series that included at least five patients and were published in the English language. Only studies that examined functional clinical outcomes were included.
Results
Twenty-five of 527 studies met our inclusion criteria, which investigated 15 independent pharmacological therapies. Eight of these therapies demonstrated possible neuroprotective properties and improved functional outcomes, of which five were investigated with randomized clinical trials: statins, N-acetyl cysteine (NAC), Enzogenol, Cerebrolysin, and nitric oxide synthase inhibitor (VAS203). Three pharmacological agents did not demonstrate neuroprotective effects, and four agents had mixed results.
Conclusions
While there is currently no single pharmacological therapy that will unequivocally improve clinical outcomes after TBI, several agents have demonstrated promising clinical benefits for specific TBI patients and should be investigated further.
1 Introduction
Despite recent advances in the management of trauma patients with multiple injuries [1], traumatic brain injury (TBI) remains a leading cause of morbidity and mortality in young people [2]. A patient’s neurological status after TBI is greatly dependent on numerous factors, including severity of injury (mild, moderate, or severe), mechanism (blunt or penetrating injury), and other patient factors [3]. While there have been significant improvements in TBI-related mortality over the past 10 years [4], more than half of patients suffer a poor neurological outcome or death after a severe TBI [5].
Interestingly, epidemiological studies have demonstrated a shift in the population demographics in patients suffering TBI over the past 3 decades. Whereas the average age of patients suffering TBI was 25–29 years in the 1980s [6, 7] and 38 years in the 1990s [8], more recent studies have shown that the average TBI patient is currently 42–53 years of age [9–11]. In this older population, increased medical comorbidities and vulnerability to the systemic effects of brain injury may significantly worsen the magnitude of neurological injury after TBI.
Neurological injury after TBI can be mechanistically classified into two stages: primary and secondary injury. Primary brain injury occurs at the moment of focal impact. In the hours following the trauma, secondary brain injury may result from changes in cerebral blood flow and intracranial pressure (ICP), hypoxemia, systemic hypotension, and cerebral edema. This secondary injury may be attenuated by the initiation of neuroprotective strategies employed in the emergency room and intensive care unit (ICU). Neuroprotective agents that target specific and limited steps in the extensive chemical cascade that results from TBI have all failed to demonstrate an improvement in mortality or neurological outcomes. Currently, the treatment of acute TBI focuses on reducing ICP and optimizing cerebral perfusion pressure (CPP); however, these treatment approaches fail to address the effects of secondary brain injury.
Several pharmacological neuroprotective agents have recently been studied with varying degrees of success. In 2012, McConeghy and colleagues reviewed the findings of studies published to 2012 in which pharmacological therapies were used to treat TBI [12]. The authors concluded that no pharmacological agent was shown to definitively improve neurological outcomes after acute TBI. Several agents such as progesterone and ciclosporin (cyclosporine) had shown promise in earlier phase II studies, however the results of larger studies at that time were pending. Since that time, the results of progesterone phase III trials have been published, and several new pharmacological agents have also been studied in humans with acute TBI. Ciclosporin phase III trials have not yet started. The purpose of this systematic review was to evaluate the recent clinical studies from January 2013 through November 2015 that investigated neuroprotective functional outcomes of pharmacological agents after TBI. This study provides new information on the pharmacological agents that have recently generated the most interest and evaluation, and which of these agents may show the most promise for the future treatment of TBI.
2 Methods
2.1 Search Methodology
The following databases were searched for relevant studies: MEDLINE (OvidSP January Week 1, 2013–November Week 2 2015), Embase (OvidSP 2013 January 1–2015 November 24), and the unindexed material in PubMed [National Library of Medicine/National Institutes of Health (NLM/NIH)]. All searches were conducted on 24 November 2015. The databases were searched using both controlled vocabulary words and synonymous free-text words for the topic of interest (traumatic brain injuries) and a list of pharmacologic neuroprotective agents (ciclosporin, antioxidants, statins, estrogen, glucocorticoids, etc.). The search strategies were adjusted for the syntax appropriate for each database/platform, and the search was limited to articles published as case reports, clinical trials, controlled clinical trials, multicenter or observational studies, randomized controlled trials, and observational studies. The search strategy was also limited to articles published since January 2013 (see the electronic supplementary material for the MEDLINE search strategy).
2.2 Inclusion Criteria
This systematic review included only full-length clinical studies and case series that included at least five patients and were published in the English language. Only studies that examined functional clinical outcomes were included.
2.3 Study Selection
Two reviewers (SG and BG) independently evaluated the titles and abstracts of the retrieved articles. Abstracts that did not include sufficient information to determine eligibility for inclusion were retrieved for full-text evaluation. The two reviewers independently evaluated all full-text articles and determined eligibility; disagreements were resolved by consensus agreement.
2.4 Data Extraction and Analysis
The same two reviewers independently conducted study evaluation and data extraction. The data extracted included the study design, sample size (total and in each group), pharmacological intervention and treatment protocol, outcome measures, results, and conclusions. A qualitative summary composed of these descriptive properties was created for each included study.
3 Results
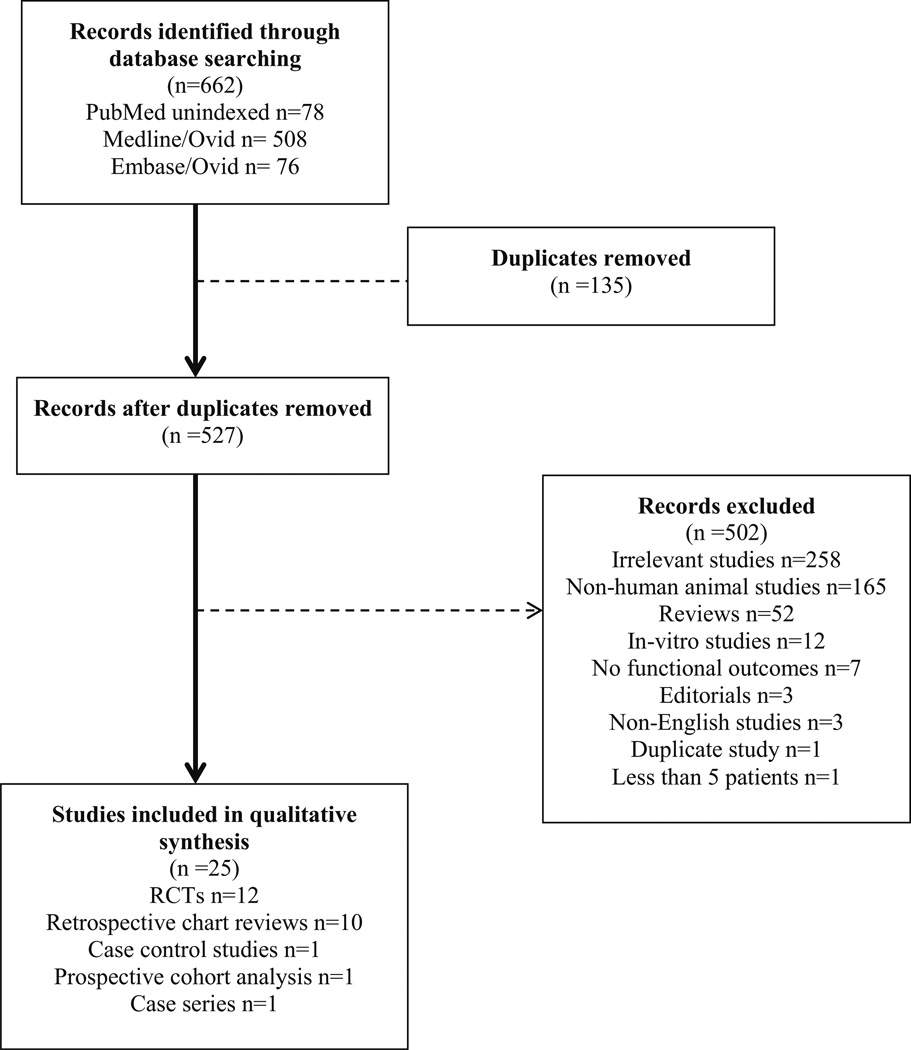
A total of 662 articles were retrieved from the systematic literature search. After removing the duplicates, 527 articles were then screened (Fig. 1). Of these articles, 502 were excluded because they were irrelevant (258 articles), non-human animal studies (165 articles), reviews (52 articles), in vitro studies (12 articles), reported either no outcomes or non-functional outcomes (7 articles), editorials (3 articles), were not written in English (3 articles), duplicate study published in two independent journals (1 article), or case series that included less than five patients (1 article). The 25 remaining studies were included in the analysis (Table 1): 12 randomized control trials (RCTs), 10 retrospective chart reviews, 1 case control study, 1 prospective cohort analysis, and 1 case series. In total, 15 independent pharmacological therapies were tested. Pharmacological therapies tested in at least two articles included progesterone (3 studies), ethanol (3 studies), growth hormone (GH) (3 studies), erythropoietin (3 studies), barbiturates (2 studies), and statins (2 studies). The remaining pharmacological therapies were each tested in one study, including glibenclamide, N-acetyl-l-cysteine (NAC), marijuana, Enzogenol, β-blockers, cerebrolysin, ciclosporin, anticonvulsants, and nitric oxide (NO) synthase inhibitor Antipterin (VAS203).
Fig. 1.
Study selection process. RCT randomized controlled trial
Table 1.
Characteristics of studies included in this systematic review
| Study, year | Study design | N | Intervention | Primary endpoints | Conclusions |
|---|---|---|---|---|---|
| Demonstrated neuroprotection | |||||
| Moreau et al. 2013 [16] |
Case–control | 50 | GH | Cognition, ADL, and QoL after 1 year of treatment |
GH therapy in TBI patients with GH deficiency may improve cognitive functions, ADL, and QoL functions |
| Devesa et al. 2013 [17] |
Case series | 13 | GH | Cognitive and behavioral function | GH therapy may improve cognitive and behavioral function after TBI regardless of whether or not the patient is GH-deficient |
| Gardner et al. 2015 [18] |
Retrospective chart review |
564 | GH | QoL scores and dimensions | GH replacement therapy resulted in long-term benefit in QoL in patients with TBI |
| Sanchez- Aguilar et al. 2013 [21] |
Randomized controlled trial |
36 | Rosuvastatin | 1. Effect of rosuvastatin on plasma levels of TNF, IL-1, 6 and 10 after 72 h after TBI 2. Amnesia, disorientation and disability at 6 months after TBI |
Statins may partially reduce proinflammatory mediators and may improve functional recovery after TBI |
| Orlando et al. 2013 [22] |
Retrospective chart review |
93 | Statins | In-hospital mortality, having at least one complication, and length of hospital stay [1 week |
Abrupt, unintended discontinuation of statin therapy is associated with an increased risk of mortality in the elderly TBI population |
| Nguyen et al. 2014 [28] |
Retrospective chart review |
446 | Marijuana | Mortality | A positive THC screen is associated with a decreased mortality after TBI |
| Mohseni et al. 2014 [31] |
Retrospective chart review |
662 | β-Blockers | In-hospital mortality | Pre-injury β-blockade improves survival following isolated severe |
| Hoffer et al. 2013 [34] |
Randomized controlled trial |
70 | NAC | Balance dysfunction, confusion, sensorineural hearing loss, headache, impaired memory and sleep disturbances |
NAC has beneficial effects on the severity and resolution of sequelae of blast-induced mild TBI (especially with early intervention) |
| Theadom et al. 2013 [36] |
Randomized controlled trial |
60 | Enzogenol | Cognitive failures and working and episodic memory at baseline, and 6, 12, and 16 weeks |
Enzogenol might reduce self- perceived cognitive failures 3–12 months after mild TBI |
| Chen et al. 2013 [38] |
Randomized controlled trial |
32 | Cerebrolysin | Differences in cognitive function including MMSE, and CASI scores at week 1, between baseline and week 4, and between baseline and week 12 |
Cerebrolysin improves cognitive function in patients with mild TBI at 3 months after injury, especially for long-term memory and drawing function |
| Stover et al. 2014 [41] |
Randomized controlled trial |
32 | Nitric oxide synthase inhibitor 4-amino- tetrahydrobiopterin (VAS203) |
ICP, CPP, brain metabolism, the therapy intensity level, and GOS- E after 6 months |
The significant improvement in clinical outcome indicates VAS203-mediated neuroprotection after TBI, but was associated with a risk of acute kidney injury at the highest dose |
| Did not demonstrate neuroprotection | |||||
| Ding et al. 2013 [46] |
Retrospective chart review |
70 | Glibenclamide | GCS on discharge, GOS on discharge, hospital and ICU length of stay |
Pretreatment and treatment with glibenclamide does not improve outcome in TBI patients with type II DM. |
| Aminmansour et al. 2014 [47] |
Randomized controlled trial |
100 | Ciclosporin | GOS-E and MMSE in the 3rd and 6th month after TBI |
Ciclosporin is not effective in improving consciousness or cognitive function after TBI |
| Gabriel and Rowe, 2014 [55] |
Prospective cohort analysis |
19 | Anticonvulsants | GOS-E, presence of early (0–7 days after TBI) or late (>8 days after TBI) seizures |
Long-term function outcomes in patients with TBI were not effected by treatment with PHT or LEV |
| Mixed results | |||||
| Shakeri et al. 2013 [61] |
Randomized controlled trial |
76 | Progesterone | Mortality rate, GCS on discharge, and GOS 3 months after discharge |
Progesterone improves neurological outcome in patients with severe TBI |
| Skolnick et al. 2014 [62] |
Randomized controlled trial |
1195 | Progesterone | GOS at 3 and 6 months, mortality rate at 1 and 3 months; Short- Form Health Survey scale at 3 and 6 months |
Progesterone treatment has no effect on clinical outcome in patients with moderate TBI |
| Wright et al. 2014 [63] |
Randomized controlled trial |
882 | Progesterone | Extended GOS at 6 months, mortality rate, Disability Rating Scale score |
Progesterone did not improve the outcome of patients with acute moderate-to-severe TBI |
| Raj et al. 2015 [65] |
Retrospective chart review |
405 | Ethanol | 6-month mortality and unfavorable neurological outcome (GOS 1–3) |
Low admission BAC (<2.3 %) demonstrated an independent risk reduction of 6-month mortality, and a trend towards improved long-term neurological outcome in BAC-positive patients |
| Pandit et al. 2014 [66] |
Retrospective chart review |
23,983 | Ethanol | Mortality | Ethanol intoxication is an independent predictor for mortality in patients with severe TBI, and is associated with higher complication rates |
| Scheyerer et al. 2014 [67] |
Retrospective chart review |
383 | Ethanol | Mortality | Patients with positive ethanol have a higher incidence of severe TBI and worse initial physiological parameters, but similar survival and hospital course, suggesting a possible neuroprotective role of ethanol |
| Majdan et al. 2013 [72] |
Retrospective chart review |
1172 | Barbiturates | ICP, use of vasopressors, and short- and long-term outcomes, including injury severity and treatment factors, mortality, and GOS |
The benefits of reduced ICP with barbiturates after TBI may be offset by marked hemodynamic instability. The use of barbiturates did not improve short- or long- term outcomes after TBI |
| Mellion et al. 2013 [73] |
Retrospective chart review |
36 | Barbiturates | Control of refractory intracranial hypertension, pediatric cerebral performance category scores at hospital discharge and at 3 months |
The addition of high-dose barbiturates achieved control of refractory intracranial hypertension in almost 30 % of treated children, and control of refractory intracranial hypertension was associated with an increased likelihood of an acceptable long-term outcome |
| Robertson et al. 2014 [75] |
Randomized controlled trial |
200 | Erythropoietin | GOS at 6 months after TBI, incidence of pulmonary complications, DVT and pulmonary embolism |
Erythropoietin administration in patients with TBI does not improve neurological outcomes or mortality. Maintenance of Hb concentration with hemotransfusions above 10 g/dl in TBI patients is not beneficial and may even be harmful |
| Aloizos et al. 2015 [76] |
Randomized controlled trial |
42 | Erythropoietin | Unfavorable neurological outcomes at 6 months (GOS-E 2–4, or death), probability of an equal, greater, or lesser GOS-E at 6 months, proportion of surviving patients with unfavorable neurological outcome (GOS-E 2–4) at 6 months, 6-month mortality |
Erythropoietin may be effective in limiting neuronal damage after TBI, resulting in lower mortality and improved neurological outcomes |
| Nichol et al. 2015 [77] |
Randomized controlled trial |
606 | Erythropoietin | Improvement in patients’ neurological status, summarized as a reduction in the proportion of patients with a GOS-E of 1–4 |
After moderate or severe TBI, erythropoietin did not reduce the number of patients with severe neurological dysfunction or increase the incidence of DVT |
GCS Glasgow Coma Scale, GOS Glasgow Outcome Score, GOS-E extended Glasgow Outcome Score, TBI traumatic brain injury, BAC blood alcohol concentration, ADL activities of daily living, QoL quality of life, GH growth hormone, PHT phenytoin, LEV levitiracetam, DM diabetes mellitus, NAC N-acetyl cysteine, ICP intracranial pressure, ICU intensive care unit, THC tetrahydrocannabinol, MMSE Mini–Mental State Examination, DVT deep vein thrombosis, CASI Cognitive Abilities Screening Instrument, TNF tumor necrosis factor, IL interleukin, ICP intracranial pressure, CPP cerebral perfusion pressure, Hb hemoglobin
Among the therapies recently tested, a neuroprotective benefit on functional outcomes after TBI was demonstrated with eight therapies: GH, statins, NAC, marijuana, Enzogenol, β-blockers, Cerebrolysin, and VAS203. No clinical benefit was demonstrated with administration of glibenclamide, ciclosporin, or anticonvulsants. Four agents demonstrated mixed results in recent studies, including progesterone, ethanol, barbiturates, and erythropoietin.
4 Pharmacological Agents with Demonstrated Neuroprotective Effects After TBI
4.1 Growth Hormone
Patients with TBI-induced damage to the anterior pituitary often demonstrate behavioral and cognitive impairment, which may be related to GH deficiency [13]. GH deficiency is commonly observed after TBI and may contribute to cognitive and behavioral dysfunction in these patients [14]. Furthermore, GH is thought to facilitate neurogenesis, neuronal differentiation, and survival of neurons after TBI, and may play a role in facilitating neuronal recovery in TBI patients without GH deficiency.
We identified three studies in which the potential neuroprotective properties of GH therapy after TBI were investigated in the setting of GH deficiency. In one case-control study, the effects of GH replacement therapy on cognition, activities of daily living (ADL), and quality of life (QoL) were investigated. GH replacement therapy was initiated in 23 patients (treatment) with cognitive and behavioral impairment, and severe GH deficiency (as defined by Prodam et al. [15]) present at least 1 year after TBI [16]. The initial dose of GH replacement therapy was 0.3 mg/day, and was progressively titrated up to achieve an insulin-like growth factor (IGF)-1 plasma level between 0 and +2 standard deviations (SDs) of the normal range for age. The treatment patients were compared with 27 matched controls who did not receive treatment. The mean Glasgow Coma Scale (GCS) score (i.e. TBI severity) in the treatment and control groups was 8.1 (SD 5.1) and 9.4 (SD 5.1), respectively. After 1 year of GH replacement therapy, the treatment group demonstrated a significant improvement (p < 0.05) in most cognitive functions, such as attention and executive function, and a non-significant trend (p < 0.07) towards improvement in spatial orientation and verbal memory test. Similar improvements were also demonstrated in ADL and four areas of QoL, including intellectual, psychological, functional, and personal domains. There was no significant association between the parameters improved by GH replacement therapy and severity of TBI. This study had several important limitations. The patients were not blinded or randomized, and treatment patients were selected based on specific criteria (i.e. severe GH deficiency), whereas most of the control patients had normal GH or only partial GH deficiency. Lastly, the small sample size (n = 50) precludes one from drawing clear conclusions, especially with regard to the effects of GH replacement therapy in patients with TBI of varying degrees of severity.
In a case-series study, the effects of GH therapy were investigated in 13 patients with cognitive and behavioral dysfunction present between 2.5 months and 11 years after severe TBI [17]. GH deficiency was identified in five patients, defined as peak GH values below 7.5 ng/mL in response to the GH-releasing hormone-arginine test. GH was initiated in all patients at 0.2 mg/day for 15 days, and subsequently increased to 0.8–1 mg/day depending on age, weight, and IGF-1 plasma levels. Patients were treated for a maximum of 8 consecutive months, where each 2 months of treatment were separated by 15 days without treatment. In all cases, a significant improvement in cognitive and behavioral function was demonstrated with GH therapy, regardless of whether the patient was GH-deficient. The patients’ cognitive function improved earlier and more significantly than motor function, and no undesirable side effects were observed. However, this study was limited to only a few cases (13), there was no adequate control group to compare, and the time to initiate treatment was highly variable (2.5 months to 11 years after TBI). Therefore, the specific effects of the hormone could not be precisely determined.
In a third study [18], the Pfizer International Metabolic Database was retrospectively reviewed, and patients with GH deficiency caused by TBI (n = 564) and non-functioning pituitary adenoma (n = 3773) were compared with regard to clinical characteristics at baseline and after 1 year of GH replacement therapy. QoL was examined after up to 8 years. The authors demonstrated that in TBI patients, there was a greater improvement in QoL at 1 year compared with patients with non-functioning pituitary adenoma, and the improvement was sustained over 8 years. Furthermore, TBI patients demonstrated normalized socialization after 1 year of GH replacement therapy, and normalized self-confidence and tenseness after 6 years. There was no normalization of tiredness or memory observed. The authors concluded that GH replacement therapy results in long-term clinical benefits in QoL in patients with TBI. Importantly, however, the authors did not address the patients’ severity of TBI in the study. Furthermore, this study was retrospectively conducted and, as with the other two studies, adequate conclusions cannot be drawn because patients were not randomized.
Although the effects of GH on facilitating neurogenesis, neuronal differentiation, and neuronal viability after TBI are well known, it is important to differentiate the potential of GH as a neuroprotective agent to improve functional outcomes from its use as a medical therapy in GH-deficient patients. Currently, very little is known about the effects of GH replacement in TBI patients without GH deficiency. Of the three recent studies, only one study [17] described the use of GH replacement therapy in eight patients with severe TBI without GH deficiency, and demonstrated improvements in cognitive and motor function. While these results are certainly intriguing, the small number of patients and lack of randomization precludes the ability to draw any conclusions regarding potential neuroprotective effects of GH. Moreover, none of the recent studies reviewed were RCTs, and were all therefore subject to important biases. While GH therapy is an interesting and potentially useful pharmacological therapy after TBI, it is currently unclear when therapy should be initiated, for how long, and which patients may benefit from its use. Large RCTs are needed to determine if GH therapy will have an important role in humans after TBI, especially in TBI patients without GH deficiency.
4.2 Statins
Previous studies in animal models of TBI have demonstrated that statin therapy results in long-lasting improvements in functional outcomes after TBI, and enhances neuronal survival in the hippocampus [19]. It has been proposed that statins induce neurogenesis and angiogenesis after brain injury, which may account for the observed neuroprotective effects in animal models [20]. However, few studies have examined the potential impact of statins on functional outcomes in humans after TBI.
Two recent studies, one RCT and one retrospective chart review, recently examined the neuroprotective effects of statins after TBI. The first study investigated whether rosuvastatin initiated within 24 h of moderate-to-severe TBI could reduce inflammatory cytokines and improve functional outcomes in humans [21]. Nineteen patients were randomized to receive rosuvastatin at a dose of 20 mg daily for 10 consecutive days, and 17 patients were administered placebo. Levels of tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, and IL-10 were measured prior to initiation of treatment and at 72 h after TBI. The levels of TNF-α were significantly reduced in the rosuvastatin group, but IL levels did not differ significantly between the groups. Moreover, treatment with rosuvastatin was associated with a reduction in disability score, indicating a favorable functional outcome at 3 and 6 months after TBI. No adverse effects associated with rosuvastatin treatment were observed. The results suggest that statins reduce proinflammatory mediators and improve functional outcomes after TBI in humans. However, it should be noted that these conclusions are based on a disability score at 3 and 6 months in a limited number of patients (n = 36).
A second study [22] retrospectively reviewed the charts of 93 TBI patients receiving chronic statin therapy, and compared the outcomes of patients who were either continued on statin therapy within 48 h of hospital admission (n = 46) or in whom statins were discontinued (n = 15). The primary outcome measures were in-hospital mortality, the incidence of at least one complication, and length of hospital stay of more than 1 week. The study demonstrated that patients who discontinued statin therapy had a fourfold higher mortality rate compared with patients who continued statins. Statin discontinuation did not have a higher complication rate or higher proportion of length of hospital stay >1 week. The authors concluded that abrupt, unintended discontinuation of statin therapy is associated with an increased risk of mortality in the elderly TBI population. Importantly, while this study demonstrated medical risks of abrupt discontinuation of statins, this does not imply that statins are neuroprotective or improve functional outcomes. Moreover, this study was limited by a retrospective study design (and lack of randomization) and small sample size. However, taken together, these studies suggest that statins are worth investigating further, and larger RCTs are needed to better assess the potential role of statins and optimal dose to provide clinical benefits after TBI.
4.3 Marijuana
Cannabinoid analogs have been shown to have neuroprotective properties in animal models by a reduction in glutamate neurotoxicity, free radical damage, and inflammation [23]. Preclinical studies in animal models of TBI have demonstrated that the cannabinoid analog dexanabinol is highly neuroprotective [24], and early phase I [25] and phase II [26] clinical trials have suggested that dexanabinol is safe and may improve the control of ICP. However, a multicenter, phase III RCT in 861 patients demonstrated that the administration of dexanabinol within 6 h of TBI was safe but was not efficacious in improving functional outcomes such as the 6-month extended Glasgow Outcome Score (GOS), mortality, improvement in ICP, or QoL [27]. Importantly, it should be noted that all patients in the phase III trial were administered a single dose of intravenous dexanabinol within 6 h of TBI, and the chronicity and timing of cannabinoid exposure may play an important role with regard to any potential neuroprotective effects.
A recent 3-year retrospective chart review studied whether a positive tetrahydrocannabinol (THC) screen on admission to a surgical ICU was associated with a reduced mortality after TBI [28]. Overall, 446 cases were identified, of which 82 (18.4 %) had a positive THC screen. The mortality rate in the THC-positive group was 2.4 % compared with 11.5 % in the THC-negative group (p < 0.05), and a THC-positive screen was independently associated with survival after TBI [odds ratio (OR] 0.224; p < 0.05). While the authors concluded that a positive THC screen is associated with a decreased mortality after TBI, these results should therefore be interpreted with caution. The study does not necessarily imply that the improvements in functional outcomes were the direct result of the pharmacological effects of THC. A THC-positive test does not specify the dose, timing, or chronicity of THC use prior to TBI. Furthermore, patients were not randomized and their use was limited to before the injury, therefore it is impossible to determine whether there is a clinical utility of THC treatment in the setting of TBI. While studies have demonstrated neuroprotective properties of marijuana (and other cannabinoid analogs) in animal models, more studies are needed to ascertain the potential benefits (if any exist) of cannabinoids in humans with TBI.
4.4 β-Blockers
Severe TBI is often associated with a tremendous catecholamine surge, known as ‘paroxysmal sympathetic storm’, which may result in worsening secondary brain damage and multi-organ failure [29]. The increased sympathetic activity reflects abnormally elevated plasma concentrations of the catecholamines epinephrine and norepinephrine in the first week after TBI, which subsequently leads to a pathologic vasoconstriction of cerebral vessels, reduced perfusion to the brain, and subsequent worsening of the brain injury. In recent years, there has been growing evidence to suggest that in-hospital treatment with β-blockers improve survival in patients after TBI [30]. It has been hypothesized that the beneficial neuroprotective effects of β-blockers result from a downregulation of the catecholamine surge that occurs after TBI.
We identified a retrospective chart review that examined in-hospital mortality in 662 patients with severe TBI, 159 of whom were exposed to pre-TBI β-blockade [31]. The study found that patients exposed to β-blockade and no β-blockade had a mortality rate of 13 and 22 %, respectively (p = 0.01). The absence of β-blockade exposure was a significant risk factor for mortality. The authors concluded that pre-injury β-blockade improved survival following isolated severe TBI; however, because the study was retrospective and not randomized, the optimal β-blocker, timing, or dose is not known. Moreover, the differences in mortality demonstrated in this study do not necessarily reflect the pharmacological effect of β-blockers. Indeed, the mechanism of the presumed neuroprotective effects of β-blockers is purely speculative and could not be definitely ascertained by this study. Prospective RCTs are needed before making any recommendations regarding their use in TBI patients.
4.5 N-acetyl-l-cysteine
NAC is a US FDA-approved pharmacological therapy that has been safely used in patients for more than 40 years. The neuroprotective benefits of NAC have been demonstrated in animal models of stroke and TBI [32, 33], and appear to be mediated by its antioxidant and anti-inflammatory properties [32]. The neuroprotective effects of NAC were studied in a double-blind, placebo-controlled RCT in solders suffering from signs of mild TBI after blast injury, including balance dysfunction, confusion, sensorineural hearing loss, headache, impaired memory, and sleep disturbances [34]. The primary outcome measured was the resolution of these symptoms 7 days after the blast exposure. After a baseline evaluation, 81 individuals were randomly assigned to receive either NAC or placebo for 7 days (4 g loading dose followed by 4 g for 4 days and 3 g for 3 days). By 7 days, the treatment group had a significantly higher resolution of symptoms compared with the placebo group (OR 3.6; p < 0.01). Secondary analysis demonstrated that the treatment patients had an 86 % chance of complete resolution of symptoms within 24 h of a blast TBI compared with 42 % of placebo patients. This was the first study to demonstrate the neuroprotective effects of NAC in humans with blast-induced mild TBI. Although these results seem promising, the study had a small sample size and the demonstrated clinical benefits of NAC were limited to mild TBI and blast injuries. The neuroprotective benefits of NAC should be further investigated in larger clinical trials with more extensive TBI and other mechanisms of injury.
4.6 Enzogenol
Enzogenol is a pine bark extract from New Zealand that has been shown to have antioxidant and anti-inflammatory properties [35]. A recent phase II RCT studied the efficacy of Enzogenol for improving cognitive function after mild TBI [36]. Sixty patients with cognitive dysfunction 3–12 months after mild TBI were randomized to receive either Enzogenol (1000 mg/day) or placebo for 6 weeks. Subsequently, all patients were administered Enzogenol for 6 weeks, followed by placebo for 4 weeks. Cognitive failures and working and episodic memory were assessed at baseline, and 6, 12, and 16 weeks. Enzogenol was safe and well tolerated and resulted in a significant reduction in cognitive failures after 6 weeks, with improvements in the frequency of self-reported cognitive failures. The authors concluded that Enzogenol might reduce self-perceived cognitive failures 3–12 months after mild TBI. Although the implications of this study are very promising, the sample size was small (n = 60), the measured outcomes were limited, and the clinical benefits were demonstrated only in mild TBI. Larger RCTs are needed to determine which patients may benefit from Enzogenol treatment after TBI.
4.7 Cerebrolysin
Cerebrolysin is a neurotrophic agent that mimics the endogenous actions of neurotrophic factors on neuroprotection and repair after injury, and has been successful in improving cognitive function in Alzheimer’s dementia and after stroke [37]. A recent double-blind, placebo-controlled, randomized phase II pilot study investigated the effects of Cerebrolysin on cognition in patients after mild TBI [38]. Patients were randomly assigned to receive either a once-daily intravenous infusion of Cerebrolysin at 30 mL over 60 min for 5 days, or placebo (same volume and administration of normal saline). The outcomes measures were differences in cognitive function, including Mini–Mental State Examination (MMSE), and Cognitive Abilities Screening Instrument (CASI) scores at 1 week, between baseline and week 4, and between baseline and week 12. The authors demonstrated that the CASI score difference in the treatment group between baseline and week 12 was 21, versus 7.6 in the control group (p < 0.05). Furthermore, drawing function and long-term memory were improved in the treatment group (p < 0.05). This study did not investigate whether Cerebrolysin resulted in any reduction in mortality, and the results were demonstrated in a small sample size (n = 32). However, larger RCTs should be conducted to further investigate the neuroprotective effects of Cerebrolysin, and to determine which patients may benefit from its use after TBI.
4.8 Nitric Oxide Synthase Inhibitor
NO is an important compound in promoting secondary brain injury after TBI by causing cerebral dilation and induction of the production of reactive nitrogen species [39], and inhibition of NO-mediated cascade has been shown to decrease ICP and improve outcomes in animal models of TBI [40]. We identified a phase IIa RCT that examined the neuroprotective effects of NO synthase inhibitor 4-amino-tetrahydrobiopterin (VAS203) [41]. Thirty-two patients were randomly assigned to one of three cohorts: patients in cohort 1 received three 12-h intravenous infusions of VAS203, followed by a 12-h infusionfree interval over 3 days (total dose 15 mg/kg); cohorts 2 and 3 were randomized to receive either VAS203 or placebo as an infusion for 48 or 72 h, respectively (total dose of 20 and 30 mg/kg). The primary endpoints were ICP, CPP, brain metabolism, the therapy intensity level, and extended GOS (GOS-E) after 6 months. No significant differences were observed between the treatment and control groups with regard to ICP, CPP, and brain metabolism. Therapy intensity level on day 6 was significantly decreased in VAS203-treated patients, and GOS-E after 6 months was significantly higher in the treatment group (p < 0.01); however, at the highest treatment dose, four of eight patients showed transient acute kidney injury (stage 2–3). Like Cerebrolysin, this study did not investigate whether VAS203 resulted in any reduction in mortality, and the results were demonstrated in a small sample size (n = 32). However, larger RCTs should be conducted to further investigate the neuroprotective effects of VAS203.
5 Pharmacological Agents with no Demonstrated Neuroprotective Effects After Traumatic Brain Injury (TBI)
5.1 Glibenclamide
The administration of glibenclamide, a sulfonylurea medication commonly used to treat hyperglycemia in patients with type II diabetes mellitus (DM), has been shown to improve neurological outcomes after stroke in humans [42], reduce secondary brain injury, and improve functional outcomes in animal models of TBI [43, 44]. Glibenclamide has been suggested to exert neuroprotective effects blocking the sulfonylurea receptor 1 (SUR1), a nonspecific water channel that plays an important role in the development of cytotoxic cerebral edema following TBI [45]. However, the role of glibenclamide in providing neuroprotective effects in humans after TBI is largely unknown.
A recent retrospective study examined whether glibenclamide treatment pre- and post-TBI in diabetic patients would have better neurological outcomes compared with diabetic TBI patients who were not treated with glibenclamide [46]. The authors identified 3453 TBI patients over an 11-year period, of which 32 non-surgical patients with type II DM were treated with glibenclamide at admission through discharge to control blood glucose (glibenclamide group). A second group of non-surgical diabetic TBI patients (n = 38) were treated with insulin to control their blood glucose level (insulin group). Neurological outcomes, as measured by GCS, GOS, length of hospital stay, and the development of progressive secondary hemorrhage, were compared between the two groups. The authors failed to demonstrate any improvement in neurological outcome in patients treated with glibenclamide. However, the study had several significant limitations, including its retrospective study design, long time span, small sample size, and the absence of long-term outcome follow-up. At this time there are insufficient data to draw adequate conclusions regarding the neuroprotective properties of glibenclamide.
5.2 Cyclosporin-A
In vitro and animal studies have demonstrated that ciclosporin confers neuroprotection by inhibiting calcineurin, thereby inhibiting NO-mediated glutamate neurotoxicity [47]. We identified a recent randomized, double-blind, placebo-controlled study [47] that randomly assigned patients to receive either ciclosporin 5 mg/kg/24 h via 250 mL DW 5 % (n = 50) during the first 8 h after TBI, or only 250 mL DW 5 % without ciclosporin (n = 50). The primary outcome measures were GOS-E and MMSE in the third and sixth month after TBI. The study demonstrated that there were no differences in GOS-E or MMSE after 3 and 6 months, and there were no increased adverse events in the treatment group. The authors concluded that ciclosporin is not effective in improving consciousness or cognitive function after TBI. At this time, there are insufficient data to recommend that ciclosporin be used to treat acute TBI.
5.3 Anticonvulsants
Anticonvulsants are commonly administered after TBI to prophylactically reduce the risk of early seizures [48]. Although phenytoin has historically been the agent of choice for post-TBI seizure prophylaxis [49], levetiracetam has emerged as an attractive alternative because of its simpler dosing regimen and more favorable side effect profile [50]. A prospective RCT [51] that compared phenytoin and levetiracetam after TBI failed to demonstrate any differences in seizure activity; however, patients who received levetiracetam had an improved Disability Rating Score and GOS-E at 6 months compared with patients who received phenytoin. This finding, combined with similar findings in earlier preclinical and clinical studies [52, 53], have led some experts to suggest that levetiracetam has neuroprotective properties [54]. However, the potential neuroprotective effects of anticonvulsant therapy and impact on functional outcomes after TBI are largely unknown.
In a prospective cohort analysis [55], 19 patients who received either phenytoin (n = 14) or levetiracetam (n = 5) for more than 48 h for severe TBI were contacted by telephone for GOS-E evaluation at least 6 months after severe TBI. The primary endpoints were GOS-E and the presence of early (0–7 days after TBI) or late (>8 days after TBI) seizures. The authors found no differences in GOS-E scores 6 months or more after severe TBI, and no differences in the rate of early or late seizures. The authors concluded that long-term functional outcomes in patients with TBI were not affected by treatment with phenytoin or levetiracetam. Therefore, at this time there is insufficient evidence to recommend either phenytoin or levetiracetam therapy in patients after TBI.
6 Pharmacological Agents with Mixed Results After TBI
6.1 Progesterone
In the past decade, the potential neuroprotective effects of progesterone after TBI have gained increasing attention [56, 57]. Progesterone rapidly crosses the blood–brain barrier and has several properties that make for a potentially useful pharmacological therapy after TBI, including antioxidant, anti-inflammatory, and remyelination effects after injury [58]. Two small RCTs clearly demonstrated improved outcomes with progesterone administration after TBI, which subsequently paved the way for larger RCTs [59, 60]. In one study published in 2008, Xiao and colleagues conducted a prospective, randomized, placebocontrolled trial in which 159 patients were randomized to receive either progesterone or placebo after TBI [59], and found that progesterone improved neurological outcomes for up to 6 months. In the other study, published in 2007, Wright and colleagues conducted a phase II, randomized, double-blind, placebo-controlled trial in which 100 patients were randomized to receive either progesterone or placebo after TBI [60]. These investigators demonstrated that patients who received progesterone had a lower 30-day mortality than controls, and moderate TBI survivors were more likely to have a moderate or good outcome.
Three of the 25 clinical studies we identified explored the potential neuroprotective properties of progesterone therapy after TBI. In the first study, treatment was initiated in 76 male patients within the first 6 h after trauma, with associated diffuse axonal injury and a GCS ≤8 [61]. Either medroxyprogesterone tablets (treatment) at a dose of 1 mg kg−1 or placebo (control) were administered every 12 h via a nasogastric tube for 5 days. The authors demonstrated that patients with a GCS between 5 and 8 who were administered progesterone had a better GOS than control patients (p < 0.05). Patients with a GCS <5 in both groups had a poor outcome, including 12 patient deaths (31.6 %) in the progesterone group and 17 (44.7 %) in the control group (not significant).
In a phase III, multinational, placebo-controlled trial (SYNAPSE), 1195 patients with severe TBI (defined as GCS ≤8 and at least one reactive pupil) were randomly assigned to receive progesterone or placebo [62]. Treatment was initiated within 8 h after the injury and consisted of a loading dose of 0.71 mg kg−1 h−1 for 1 h, followed by 0.5 mg kg−1 h−1 for 119 h. The primary outcome measure was the GOS score at 6 months after the injury. Secondary outcome measures included GOS score at 3 months, mortality at 1 and 6 months, and GOS-E score. Primary and secondary efficacy analyses failed to demonstrate any clinical benefit of progesterone in patients with severe TBI.
In a phase III, double-blind, placebo-controlled RCT (PROTECT III), the efficacy of early intravenous administration of progesterone after acute TBI was investigated [63]. Treatment was initiated within 4 h after injury in patients with a GCS of between 4 and 12, which consisted of a 1-h loading dose of 0.71 mg/kg/h, 71 h of a maintenance infusion of 0.5 mg/kg/h, and a 24-h infusion taper. A total of 882 of the planned 1140 patients underwent randomization before the trial was stopped due to a lack of favorable outcomes in the progesterone versus placebo groups (51 vs. 55.5 %, respectively). Phlebitis or thrombophlebitis was more frequent in the progesterone group, and no differences in mortality rates were observed between the two groups. Despite promising preclinical and early RCTs, the results of the two recent large phase III studies have failed to demonstrate any improvement in functional outcomes with progesterone treatment after TBI. In light of these studies, progesterone treatment after TBI cannot be recommended at this time.
6.2 Ethanol
Ethanol is a known inhibitor of N-methyl-d-aspartate (NMDA) receptor-mediated glutamate neurotoxicity, and studies have suggested that ethanol may have significant neuroprotective effects in the setting of TBI [64]. Previous studies on the effects of acute or chronic ethanol intoxication have yielded inconsistent results.
We identified three recent retrospective chart reviews that examined the effects of ethanol on mortality after TBI. In the first study [65], 405 patients were retrospectively grouped according to blood alcohol concentration (BAC) on hospital admission after TBI: no BAC (n = 99), low BAC (<2.3 %, n = 140), and high BAC (>2.3 %, n = 166). The primary outcome measures included 6-month mortality and unfavorable neurological outcome (GOS 1–3). The authors found that low BAC independently reduced the risk of 6-month mortality compared with no BAC or high BAC, and there was a trend towards a reduced risk of 6-month unfavorable outcome in patients with positive BAC compared with negative BAC. The authors concluded that a positive BAC after TBI may have neuroprotective effects with respect to both mortality and neurological outcomes.
A second recent study [66] retrospectively reviewed the charts of 23,983 patients with severe TBI, and examined the effects of ethanol intoxication on in-hospital complications and mortality. It was demonstrated that the 5461 (22.8 %) patients who tested positive for ethanol intoxication were more likely to have in-hospital complications (p = 0.001) and a higher mortality rate (p = 0.01) compared with patients who were not intoxicated. These investigators concluded that ethanol intoxication was an independent predictor for mortality in patients with severe TBI, and is associated with higher complication rates.
A third study [67] retrospectively reviewed 383 charts and grouped patients according to BAC (>0.5 %, defined as ‘positive’; and <0.5 %, defined as ‘negative’). The primary endpoint in this study was mortality. The authors demonstrated that patients in the ethanol-positive group had significantly lower GCS (9.64 vs. 12 points; p = 0.005), increased lactate, and a lower mean arterial pressure on admission. No differences in mortality rate were observed between the ethanol-positive and ethanol-negative patients (19.6 vs. 21.5 %). Similarly, hospital stay (15.29 vs. 17.55 days) and duration of ICU treatment (8.53 vs. 8.36 days) were similar between groups. As patients with a positive ethanol test had a higher incidence of severe TBI and worse physiological parameters on admission, yet similar hospital course and survival rates, the authors concluded that ethanol might have a neuroprotective role in the setting of TBI.
At this time, it is difficult to draw conclusions regarding the possible neuroprotective properties of ethanol. All of the studies were observational and retrospective, and their use was limited to before the injury. Performing an RCT with ethanol would likely be impractical for ethical reasons, and it is therefore difficult to ascertain how ethanol might be used in future treatment after TBI.
6.3 Barbiturates
Intracranial hypertension is common in TBI patients [68] and, if not corrected, is associated with secondary brain injury and worsened outcomes. Barbiturates are a non-surgical treatment that have been used since the 1970s to lower ICP [69]. Although the exact mechanism is poorly understood, the effects of barbiturates on lowering ICP have been attributed to the inverse steal phenomenon, a reduction in cerebral oxygen consumption and metabolism, and free radical oxygen scavenging [54]. Despite its effects in lowering ICP, prospective RCTs performed in the 1980s demonstrated that barbiturate use after TBI is associated with an increase in risk of infection, as well as increased cardiovascular and pulmonary complications [70, 71]. Therefore, although the effects of barbiturate treatment on functional outcomes in select subgroups of TBI patients are uncertain, experts have recommended against the prophylactic use of barbiturate coma in the treatment of TBI.
We identified two recent retrospective studies that examined the neuroprotective effects of barbiturates after TBI. In the first study, the charts of 1172 patients with severe TBI were retrospectively reviewed in 13 centers across five European countries, and investigated the effects of barbiturates on ICP, use of vasopressors, and short- and long-term outcomes [72]. Short-term outcome measures included injury severity and treatment factors, mortality, and GOS. Patients were categorized into three groups, depending on barbiturate dose. The authors demonstrated that <20 % of patients with severe TBI were administered barbiturates, and 6 % were administered high doses. High-dose barbiturates resulted in a 69 % decrease in ICP but significant hemodynamic instability and increased use of vasopressors. The use of barbiturates had no effect on short- or long-term outcomes after TBI.
In a second retrospective chart review [73], 36 cases were reviewed in which high-dose barbiturates were administered for refractory intracranial hypertension after severe TBI in children for at least 6 h. The primary outcome measures were control of refractory intracranial hypertension and pediatric cerebral performance category scores at hospital discharge and at 3 months. It was noted that 10 patients (28 %) achieved control of their refractory intracranial hypertension, 10 patients survived, and survival was more common in patients with controlled intracranial hypertension. Nineteen of the 22 surviving patients had an acceptable neurological outcome (pediatric cerebral performance category <3) at 3 months or longer, and only three returned to normal function. Lastly, control of refractory intracranial hypertension was associated with a better pediatric cerebral performance category score and a more than twofold increase in acceptable long-term outcomes compared with patients who had refractory intracranial hypertension despite high-dose barbiturates. However, it should be noted that because the study was retrospective and not placebo-controlled, it is impossible to ascertain whether the improvement in clinical outcomes were associated with the reduction in ICP or possible neuroprotective properties of barbiturate therapy. At this point, it seems clear that barbiturate therapy should not be used indiscriminately in all TBI patients. While some patients with refractory intracranial hypertension after TBI may benefit from its use, definitive conclusions cannot be drawn at this time.
6.4 Erythropoietin
Erythropoietin has been shown to possess anti-inflammatory and anti-apoptic properties, and has neuroprotective effects in animal models [74]. We identified three recent RCTs that investigated the neuroprotective effects of erythropoietin after TBI. In the first study [75], 200 patients who were unable to follow commands and were identified within 6 h of TBI were enrolled. The study had two objectives: to assess the effects of early administration of erythropoietin, and to compare the effect of two hemoglobin transfusion thresholds on neurological outcome. A factorial (2 × 2) randomization design was used to compare the administration of erythropoietin or placebo, and separately compared the effects of a hemoglobin transfusion threshold of 7 versus 10 g dl−1. The primary outcome measured was GOS at 6 months after TBI. The authors failed to demonstrate a significant difference between study groups with regard to neurological outcome and mortality; however, the incidence of thromboembolic events was significantly greater in patients with a transfusion threshold of 10 g dl−1 compared with 7 g dl−1 (21.8 vs. 8.1 %, respectively; p < 0.01). The authors concluded that erythropoietin administration is ineffective in providing neuroprotection in human TBI, and that maintaining hemoglobin concentrations with transfusion is not beneficial and may even be harmful in TBI patients.
In a second recent RCT [76], 42 patients admitted to the ICU within 6 h of severe TBI were randomized to receive either 10,000 IU of erythropoietin (n = 24) or placebo (n = 18) for 7 consecutive days. The primary outcomes of the study were unfavorable neurological outcomes at 6 months (GOS-E 2–4, or death), probability of an equal, greater, or lesser GOS-E at 6 months, proportion of surviving patients with an unfavorable outcome (GOS-E 2–4 at 6 months), and 6-month mortality. The study demonstrated that six patients (42 %) died within the first 2 weeks; two (8.3 %) in the intervention group and four (22.2 %) in the control group (p < 0.01). Patients in the control group had a lower rate of good outcomes (GOS-E 6.6 vs. 4.2, respectively; p < 0.005). The authors concluded that erythropoietin may be effective in limiting neurological damage after TBI, resulting in lower mortality and improved neurological outcomes.
In a third, larger RCT, 606 patients were randomized in the first 24 h after moderate or severe TBI to receive either 40,000 IU of erythropoietin (n = 308) or saline solution (n = 298) subcutaneously once weekly for a maximum of three doses [77]. The primary outcome measure was an improvement in neurological status, summarized as a reduction in the proportion of patients with a GOS-E of 1–4. The study demonstrated that erythropoietin did not reduce the proportion of patients with a GOS-E level of 1–4, nor did erythropoietin increase the 6-month mortality of the occurrence of deep vein thrombosis (DVT). Although the early study demonstrated promising results with erythropoietin administration after TBI, the two more recent, larger, phase III trials failed to demonstrate the neuroprotective properties of erythropoietin, and even suggested that erythropoietin may cause harm. Therefore, in light of these recent studies, the administration of erythropoietin is not recommended after TBI.
7 Conclusions
TBI often results in devastating individual disability and a significant burden on society related to long-term care. Therefore, neuroprotective pharmacological agents that can be used to reduce or eliminate secondary brain injury after TBI are greatly needed. We reviewed 15 potential pharmacological agents that were recently investigated in 25 clinical studies. While there is currently no single pharmacological therapy that will unequivocally improve clinical outcomes after TBI, several agents have demonstrated promising clinical benefits for specific TBI patients. However, the positive studies are limited and many of the conclusions are based on retrospective studies or prospective studies conducted in a small sample size. Importantly, several agents such as cannabinoids, progesterone, and erythropoietin have demonstrated potential neuroprotective effects in preclinical and early clinical trials, but failed to show any improvement in functional outcomes after TBI in larger, phase III trials. Prospective RCTs are widely regarded as the ‘gold standard’ for measuring the efficacy of a particular intervention, and employ strict inclusion, exclusion, and treatment criteria that result in a high degree of ‘internal validity’ [78]. However, RCTs compare therapeutic agents with placebo, and not with existing treatment options that are more reflective of clinical practice. Therefore, these RCTs may have a limited external validity. As such, many experts have argued that RCTs should be supplemented by more modern statistical techniques, such as comparative effectiveness research, in order to draw more meaningful conclusions regarding the effectiveness of an agent [78]. Moreover, differences in outcomes may reflect differences in the studies’ treatment protocols, and better definition of inclusion criteria, triggers for intervention, or treatment targets may help aid in the identification of more effective drug treatments. The evidence we provided in this updated systematic review of the literature may greatly contribute to the interpretation of the recent literature and design of future studies.
Key Points.
While there is currently no single pharmacological therapy that will unequivocally improve clinical outcomes after traumatic brain injury (TBI), several agents have demonstrated promising clinical benefits for specific TBI patients.
The positive studies are limited, however, and many of the conclusions are based on retrospective studies or prospective studies conducted in a small sample size.
More randomized control trials are needed to investigate which pharmacological agents have the most neuroprotective benefits on functional outcomes after TBI, and to identify which patients may benefit most from their use.
Acknowledgments
Funding Shaun Gruenbaum is an Investigative Medicine MD to PhD Program graduate student. This publication was made possible by Clinical and Translational Science Awards (CTSA) Grant number UL1 TR000142 from the National Center for Advancing Translational Science (NCATS), a component of the NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s40263-016-0355-2) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards
Conflicts of interest Shaun Gruenbaum, Alexander Zlotnik, Benjamin Gruenbaum, Denise Hersey, and Federico Bilotta declare no conflicts of interest.
Contributor Information
Shaun E. Gruenbaum, Email: shaun.gruenbaum@yale.edu.
Alexander Zlotnik, Email: zlotnika@bgu.ac.il.
Benjamin F. Gruenbaum, Email: benjamin.gruenbaum@yale.edu.
Denise Hersey, Email: denise.hersey@yale.edu.
Federico Bilotta, Email: bilotta@tiscali.it.
References
- 1.Kirkpatrick AW, Ball CG, D’Amours SK, Zygun D. Acute resuscitation of the unstable adult trauma patient: bedside diagnosis and therapy. Can J Surg. 2008;51(1):57–69. [PMC free article] [PubMed] [Google Scholar]
- 2.Lu C, Xia J, Bin W, Wu Y, Liu X, Zhang Y. Advances in diagnosis, treatments, and molecular mechanistic studies of traumatic brain injury. Biosci Trends. 2015;9(3):138–148. doi: 10.5582/bst.2015.01066. [DOI] [PubMed] [Google Scholar]
- 3.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 4.Gerber LM, Chiu YL, Carney N, Hartl R, Ghajar J. Marked reduction in mortality in patients with severe traumatic brain injury. J Neurosurg. 2013;119(6):1583–1590. doi: 10.3171/2013.8.JNS13276. [DOI] [PubMed] [Google Scholar]
- 5.Marmarou A, Lu J, Butcher I, McHugh GS, Mushkudiani NA, Murray GD, et al. IMPACT database of traumatic brain injury: design and description. J Neurotrauma. 2007;24(2):239–250. doi: 10.1089/neu.2006.0036. [DOI] [PubMed] [Google Scholar]
- 6.Levin HS, Saydjari C, Eisenberg HM, Foulkes M, Marshall LF, Ruff RM, et al. Vegetative state after closed-head injury. A Traumatic Coma Data Bank report. Arch Neurol. 1991;48(6):580–585. doi: 10.1001/archneur.1991.00530180032013. [DOI] [PubMed] [Google Scholar]
- 7.Murray LS, Teasdale GM, Murray GD, Miller DJ, Pickard JD, Shaw MD. Head injuries in four British neurosurgical centres. Br J Neurosurg. 1999;13(6):564–569. doi: 10.1080/02688699943060. [DOI] [PubMed] [Google Scholar]
- 8.Murray GD, Teasdale GM, Braakman R, Cohadon F, Dearden M, Iannotti F, et al. The European Brain Injury Consortium survey of head injuries. Acta Neurochir. 1999;141(3):223–236. doi: 10.1007/s007010050292. [DOI] [PubMed] [Google Scholar]
- 9.Stocchetti N, Paterno R, Citerio G, Beretta L, Colombo A. Traumatic brain injury in an aging population. J Neurotrauma. 2012;29(6):1119–1125. doi: 10.1089/neu.2011.1995. [DOI] [PubMed] [Google Scholar]
- 10.Myburgh JA, Cooper DJ, Finfer SR, Venkatesh B, Jones D, Higgins A, et al. Epidemiology and 12-month outcomes from traumatic brain injury in australia and new zealand. J Trauma. 2008;64(4):854–862. doi: 10.1097/TA.0b013e3180340e77. [DOI] [PubMed] [Google Scholar]
- 11.Muehlschlegel S, Carandang R, Ouillette C, Hall W, Anderson F, Goldberg R. Frequency and impact of intensive care unit complications on moderate-severe traumatic brain injury: early results of the Outcome Prognostication in Traumatic Brain Injury (OPTIMISM) Study. Neurocrit Care. 2013;18(3):318–331. doi: 10.1007/s12028-013-9817-2. [DOI] [PubMed] [Google Scholar]
- 12.McConeghy KW, Hatton J, Hughes L, Cook AM. A review of neuroprotection pharmacology and therapies in patients with acute traumatic brain injury. CNS Drugs. 2012;26(7):613–636. doi: 10.2165/11634020-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Falleti MG, Maruff P, Burman P, Harris A. The effects of growth hormone (GH) deficiency and GH replacement on cognitive performance in adults: a meta-analysis of the current literature. Psychoneuroendocrinology. 2006;31(6):681–691. doi: 10.1016/j.psyneuen.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Agha A, Rogers B, Sherlock M, O’Kelly P, Tormey W, Phillips J, et al. Anterior pituitary dysfunction in survivors of traumatic brain injury. J Clin Endocrinol Metab. 2004;89(10):4929–4936. doi: 10.1210/jc.2004-0511. [DOI] [PubMed] [Google Scholar]
- 15.Prodam F, Pagano L, Corneli G, Golisano G, Belcastro S, Busti A, et al. Update on epidemiology, etiology, and diagnosis of adult growth hormone deficiency. J Endocrinol Invest. 2008;31(9 Suppl):6–11. [PubMed] [Google Scholar]
- 16.Moreau OK, Cortet-Rudelli C, Yollin E, Merlen E, Daveluy W, Rousseaux M. Growth hormone replacement therapy in patients with traumatic brain injury. J Neurotrauma. 2013;30(11):998–1006. doi: 10.1089/neu.2012.2705. [DOI] [PubMed] [Google Scholar]
- 17.Devesa J, Reimunde P, Devesa P, Barbera M, Arce V. Growth hormone (GH) and brain trauma. Horm Behav. 2013;63(2):331–344. doi: 10.1016/j.yhbeh.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 18.Gardner CJ, Mattsson AF, Daousi C, Korbonits M, Koltowska-Haggstrom M, Cuthbertson DJ. GH deficiency after traumatic brain injury: improvement in quality of life with GH therapy: analysis of the KIMS database. Eur J Endocrinol. 2015;172(4):371–381. doi: 10.1530/EJE-14-0654. [DOI] [PubMed] [Google Scholar]
- 19.Mahmood A, Goussev A, Kazmi H, Qu C, Lu D, Chopp M. Long-term benefits after treatment of traumatic brain injury with simvastatin in rats. Neurosurgery. 2009;65(1):187–191. doi: 10.1227/01.NEU.0000343540.24780.D6. (discussion 91-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu D, Goussev A, Chen J, Pannu P, Li Y, Mahmood A, et al. Atorvastatin reduces neurological deficit and increases synaptogenesis, angiogenesis, and neuronal survival in rats subjected to traumatic brain injury. J Neurotrauma. 2004;21(1):21–32. doi: 10.1089/089771504772695913. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez-Aguilar M, Tapia-Perez JH, Sanchez-Rodriguez JJ, Vinas-Rios JM, Martinez-Perez P, de la Cruz-Mendoza E, et al. Effect of rosuvastatin on cytokines after traumatic head injury. J Neurosurg. 2013;118(3):669–675. doi: 10.3171/2012.12.JNS121084. [DOI] [PubMed] [Google Scholar]
- 22.Orlando A, Bar-Or D, Salottolo K, Levy AS, Mains CW, Slone DS, et al. Unintentional discontinuation of statins may increase mortality after traumatic brain injury in elderly patients: a preliminary observation. J Clin Med Res. 2013;5(3):168–173. doi: 10.4021/jocmr1333w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoles E, Belkin M, Schwartz M. HU-211, a nonpsychotropic cannabinoid, produces short- and long-term neuroprotection after optic nerve axotomy. J Neurotrauma. 1996;13(1):49–57. doi: 10.1089/neu.1996.13.49. [DOI] [PubMed] [Google Scholar]
- 24.Shohami E, Biegon A. Novel approach to the role of NMDA receptors in traumatic brain injury. CNS Neurol Disord Drug Targets. 2014;13(4):567–573. doi: 10.2174/18715273113126660196. [DOI] [PubMed] [Google Scholar]
- 25.Brewster ME, Pop E, Foltz RL, Reuschel S, Griffith W, Amselem S, et al. Clinical pharmacokinetics of escalating i.v. doses of dexanabinol (HU-211), a neuroprotectant agent, in normal volunteers. Int J Clin Pharmacol Ther. 1997;35(9):361–365. [PubMed] [Google Scholar]
- 26.Knoller N, Levi L, Shoshan I, Reichenthal E, Razon N, Rappaport ZH, et al. Dexanabinol (HU-211) in the treatment of severe closed head injury: a randomized, placebo-controlled, phase II clinical trial. Crit Care Med. 2002;30(3):548–554. doi: 10.1097/00003246-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Maas AI, Murray G, Henney H, 3rd, Kassem N, Legrand V, Mangelus M, et al. Efficacy and safety of dexanabinol in severe traumatic brain injury: results of a phase III randomised, placebocontrolled, clinical trial. Lancet Neurol. 2006;5(1):38–45. doi: 10.1016/S1474-4422(05)70253-2. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen BM, Kim D, Bricker S, Bongard F, Neville A, Putnam B, et al. Effect of marijuana use on outcomes in traumatic brain injury. Am Surg. 2014;80(10):979–983. [PubMed] [Google Scholar]
- 29.Clifton GL, Ziegler MG, Grossman RG. Circulating cate-cholamines and sympathetic activity after head injury. Neurosurgery. 1981;8(1):10–14. doi: 10.1227/00006123-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Arbabi S, Campion EM, Hemmila MR, Barker M, Dimo M, Ahrns KS, et al. Beta-blocker use is associated with improved outcomes in adult trauma patients. J Trauma. 2007;62(1):56–61. doi: 10.1097/TA.0b013e31802d972b. (discussion 61-2) [DOI] [PubMed] [Google Scholar]
- 31.Mohseni S, Talving P, Wallin G, Ljungqvist O, Riddez L. Preinjury beta-blockade is protective in isolated severe traumatic brain injury. J Trauma Acute Care Surg. 2014;76(3):804–808. doi: 10.1097/TA.0000000000000139. [DOI] [PubMed] [Google Scholar]
- 32.Sekhon B, Sekhon C, Khan M, Patel SJ, Singh I, Singh AK. N-Acetyl cysteine protects against injury in a rat model of focal cerebral ischemia. Brain Res. 2003;971(1):1–8. doi: 10.1016/s0006-8993(03)02244-3. [DOI] [PubMed] [Google Scholar]
- 33.Hicdonmez T, Kanter M, Tiryaki M, Parsak T, Cobanoglu S. Neuroprotective effects of N-acetylcysteine on experimental closed head trauma in rats. Neurochem Res. 2006;31(4):473–481. doi: 10.1007/s11064-006-9040-z. [DOI] [PubMed] [Google Scholar]
- 34.Hoffer ME, Balaban C, Slade MD, Tsao JW, Hoffer B. Amelioration of acute sequelae of blast induced mild traumatic brain injury by N-acetyl cysteine: a double-blind, placebo controlled study. PloS One. 2013;8(1):e54163. doi: 10.1371/journal.pone.0054163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shand B, Strey C, Scott R, Morrison Z, Gieseg S. Pilot study on the clinical effects of dietary supplementation with Enzogenol, a flavonoid extract of pine bark and vitamin C. Phytother Res. 2003;17(5):490–494. doi: 10.1002/ptr.1181. [DOI] [PubMed] [Google Scholar]
- 36.Theadom A, Mahon S, Barker-Collo S, McPherson K, Rush E, Vandal AC, et al. Enzogenol for cognitive functioning in traumatic brain injury: a pilot placebo-controlled RCT. Eur J Neurol. 2013;20(8):1135–1144. doi: 10.1111/ene.12099. [DOI] [PubMed] [Google Scholar]
- 37.Masliah E, Diez-Tejedor E. The pharmacology of neurotrophic treatment with Cerebrolysin: brain protection and repair to counteract pathologies of acute and chronic neurological disorders. Drugs Today (Barc) 2012;48(Suppl A):3–24. doi: 10.1358/dot.2012.48(Suppl.A).1739716. [DOI] [PubMed] [Google Scholar]
- 38.Chen CC, Wei ST, Tsaia SC, Chen XX, Cho DY. Cerebrolysin enhances cognitive recovery of mild traumatic brain injury patients: double-blind, placebo-controlled, randomized study. Br J Neurosurg. 2013;27(6):803–807. doi: 10.3109/02688697.2013.793287. [DOI] [PubMed] [Google Scholar]
- 39.Guzik TJ, West NE, Pillai R, Taggart DP, Channon KM. Nitric oxide modulates superoxide release and peroxynitrite formation in human blood vessels. Hypertension. 2002;39(6):1088–1094. doi: 10.1161/01.hyp.0000018041.48432.b5. [DOI] [PubMed] [Google Scholar]
- 40.Terpolilli NA, Zweckberger K, Trabold R, Schilling L, Schinzel R, Tegtmeier F, et al. The novel nitric oxide synthase inhibitor 4-amino-tetrahydro-L-biopterine prevents brain edema formation and intracranial hypertension following traumatic brain injury in mice. J Neurotrauma. 2009;26(11):1963–1975. doi: 10.1089/neu.2008.0853. [DOI] [PubMed] [Google Scholar]
- 41.Stover JF, Belli A, Boret H, Bulters D, Sahuquillo J, Schmutzhard E, et al. Nitric oxide synthase inhibition with the antipterin VAS203 improves outcome in moderate and severe traumatic brain injury: a placebo-controlled randomized phase IIa trial (NOSTRA) J Neurotrauma. 2014;31(19):1599–1606. doi: 10.1089/neu.2014.3344. [DOI] [PubMed] [Google Scholar]
- 42.Kunte H, Schmidt S, Eliasziw M, del Zoppo GJ, Simard JM, Masuhr F, et al. Sulfonylureas improve outcome in patients with type 2 diabetes and acute ischemic stroke. Stroke. 2007;38(9):2526–2530. doi: 10.1161/STROKEAHA.107.482216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zweckberger K, Hackenberg K, Jung CS, Hertle DN, Kiening KL, Unterberg AW, et al. Glibenclamide reduces secondary brain damage after experimental traumatic brain injury. Neuroscience. 2014;272:199–206. doi: 10.1016/j.neuroscience.2014.04.040. [DOI] [PubMed] [Google Scholar]
- 44.Patel AD, Gerzanich V, Geng Z, Simard JM. Glibenclamide reduces hippocampal injury and preserves rapid spatial learning in a model of traumatic brain injury. J Neuropathol Exp Neurol. 2010;69(12):1177–1190. doi: 10.1097/NEN.0b013e3181fbf6d6. [DOI] [PubMed] [Google Scholar]
- 45.Simard JM, Woo SK, Schwartzbauer GT, Gerzanich V. Sulfonylurea receptor 1 in central nervous system injury: a focused review. J Cereb Blood Flow Metab. 2012;32(9):1699–1717. doi: 10.1038/jcbfm.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ding J, Yuan F, Guo JY, Chen H, Tian HL. Influence of glibenclamide on outcome in patients with type 2 diabetes and traumatic brain injury. Clin Neurlo Neurosurg. 2013;115(10):2166–2169. doi: 10.1016/j.clineuro.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 47.Aminmansour B, Fard SA, Habibabadi MR, Moein P, Norouzi R, Naderan M. The efficacy of cyclosporine-a on diffuse axonal injury after traumatic brain injury. Adv Biomed Res. 2014;3:35. doi: 10.4103/2277-9175.125031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Temkin NR. Antiepileptogenesis and seizure prevention trials with antiepileptic drugs: meta-analysis of controlled trials. Epilepsia. 2001;42(4):515–524. doi: 10.1046/j.1528-1157.2001.28900.x. [DOI] [PubMed] [Google Scholar]
- 49.Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323(8):497–502. doi: 10.1056/NEJM199008233230801. [DOI] [PubMed] [Google Scholar]
- 50.Rowe AS, Goodwin H, Brophy GM, Bushwitz J, Castle A, Deen D, et al. Seizure prophylaxis in neurocritical care: a review of evidence-based support. Pharmacotherapy. 2014;34(4):396–409. doi: 10.1002/phar.1374. [DOI] [PubMed] [Google Scholar]
- 51.Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. 2010;12(2):165–172. doi: 10.1007/s12028-009-9304-y. [DOI] [PubMed] [Google Scholar]
- 52.Taylor S, Heinrichs RJ, Janzen JM, Ehtisham A. Levetiracetam is associated with improved cognitive outcome for patients with intracranial hemorrhage. Neurocrit Care. 2011;15(1):80–84. doi: 10.1007/s12028-010-9341-6. [DOI] [PubMed] [Google Scholar]
- 53.Wang H, Gao J, Lassiter TF, McDonagh DL, Sheng H, Warner DS, et al. Levetiracetam is neuroprotective in murine models of closed head injury and subarachnoid hemorrhage. Neurocrit Care. 2006;5(1):71–78. doi: 10.1385/NCC:5:1:71. [DOI] [PubMed] [Google Scholar]
- 54.Chen HI, Malhotra NR, Oddo M, Heuer GG, Levine JM, LeRoux PD. Barbiturate infusion for intractable intracranial hypertension and its effect on brain oxygenation. Neurosurgery. 2008;63(5):880–886. doi: 10.1227/01.NEU.0000327882.10629.06. (discussion 6-7) [DOI] [PubMed] [Google Scholar]
- 55.Gabriel WM, Rowe AS. Long-term comparison of GOS-E scores in patients treated with phenytoin or levetiracetam for posttraumatic seizure prophylaxis after traumatic brain injury. Ann Pharmacother. 2014;48(11):1440–1444. doi: 10.1177/1060028014549013. [DOI] [PubMed] [Google Scholar]
- 56.Deutsch ER, Espinoza TR, Atif F, Woodall E, Kaylor J, Wright DW. Progesterone’s role in neuroprotection, a review of the evidence. Brain Res. 2013;1530:82–105. doi: 10.1016/j.brainres.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 57.Wei J, Xiao GM. The neuroprotective effects of progesterone on traumatic brain injury: current status and future prospects. Acta Pharmacol Sin. 2013;34(12):1485–1490. doi: 10.1038/aps.2013.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shakeri M, Boustani MR, Pak N, Panahi F, Salehpour F, Lotfinia I, et al. Effect of progesterone administration on prognosis of patients with diffuse axonal injury due to severe head trauma. Clin Neurol Neurosurg. 2013;115(10):2019–2022. doi: 10.1016/j.clineuro.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 59.Xiao G, Wei J, Yan W, Wang W, Lu Z. Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Crit Care. 2008;12(2):R61. doi: 10.1186/cc6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49(4):391–402. doi: 10.1016/j.annemergmed.2006.07.932. (e1-2) [DOI] [PubMed] [Google Scholar]
- 61.Shakeri M, Boustani MR, Mahdkhah A. Effect of progesterone administration on prognosis of patients with diffuse axonal injury due to severe head trauma. Neurosurg Q. 2013;24(4):282–285. doi: 10.1016/j.clineuro.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 62.Skolnick BE, Maas AI, Narayan RK, van der Hoop RG, MacAllister T, Ward JD, et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371(26):2467–2476. doi: 10.1056/NEJMoa1411090. [DOI] [PubMed] [Google Scholar]
- 63.Wright DW, Yeatts SD, Silbergleit R, Palesch YY, Hertzberg VS, Frankel M, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457–2466. doi: 10.1056/NEJMoa1404304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kelly DF. Alcohol and head injury: an issue revisited. J Neurotrauma. 1995;12(5):883–890. doi: 10.1089/neu.1995.12.883. [DOI] [PubMed] [Google Scholar]
- 65.Raj R, Skrifvars MB, Kivisaari R, Hernesniemi J, Lappalainen J, Siironen J. Acute alcohol intoxication and long-term outcome in patients with traumatic brain injury. J Neurotrauma. 2015;32(2):95–100. doi: 10.1089/neu.2014.3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pandit V, Patel N, Rhee P, Kulvatunyou N, Aziz H, Green DJ, et al. Effect of alcohol in traumatic brain injury: is it really protective? J Surg Res. 2014;190(2):634–639. doi: 10.1016/j.jss.2014.04.039. [DOI] [PubMed] [Google Scholar]
- 67.Scheyerer MJ, Dutschler J, Billeter A, Zimmermann SM, Sprengel K, Werner CM, et al. Effect of elevated serum alcohol level on the outcome of severely injured patients. Emerg Med J. 2014;31(10):813–817. doi: 10.1136/emermed-2013-202804. [DOI] [PubMed] [Google Scholar]
- 68.Cormio M, Gopinath SP, Valadka A, Robertson CS. Cerebral hemodynamic effects of pentobarbital coma in head-injured patients. J Neurotrauma. 1999;16(10):927–936. doi: 10.1089/neu.1999.16.927. [DOI] [PubMed] [Google Scholar]
- 69.Levin AB, Duff TA, Javid MJ. Treatment of increased intracranial pressure: a comparison of different hyperosmotic agents and the use of thiopental. Neurosurgery. 1979;5(5):570–575. doi: 10.1227/00006123-197911000-00005. [DOI] [PubMed] [Google Scholar]
- 70.Schwartz ML, Tator CH, Rowed DW, Reid SR, Meguro K, Andrews DF. The University of Toronto head injury treatment study: a prospective, randomized comparison of pentobarbital and mannitol. Can J Neurol Sci. 1984;11(4):434–440. doi: 10.1017/s0317167100045960. [DOI] [PubMed] [Google Scholar]
- 71.Ward JD, Becker DP, Miller JD, Choi SC, Marmarou A, Wood C, et al. Failure of prophylactic barbiturate coma in the treatment of severe head injury. J Neurosurg. 1985;62(3):383–388. doi: 10.3171/jns.1985.62.3.0383. [DOI] [PubMed] [Google Scholar]
- 72.Majdan M, Mauritz W, Wilbacher I, Brazinova A, Rusnak M, Leitgeb J. Barbiturates use and its effects in patients with severe traumatic brain injury in five European countries. J Neurotrauma. 2013;30(1):23–29. doi: 10.1089/neu.2012.2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mellion SA, Bennett KS, Ellsworth GL, Moore K, Riva-Cambrin J, Metzger RR, et al. High-dose barbiturates for refractory intracranial hypertension in children with severe traumatic brain injury. Pediatr Crit Care Med. 2013;14(3):239–247. doi: 10.1097/PCC.0b013e318271c3b2. [DOI] [PubMed] [Google Scholar]
- 74.Siren AL, Fratelli M, Brines M, Goemans C, Casagrande S, Lewczuk P, et al. Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci USA. 2001;98(7):4044–4049. doi: 10.1073/pnas.051606598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47. doi: 10.1001/jama.2014.6490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aloizos S, Evodia E, Gourgiotis S, Isaia EC, Seretis C, Baltopoulos GJ. Neuroprotective effects of erythropoietin in patients with severe closed brain injury. Turk Neurosurg. 2015;25(4):552–558. doi: 10.5137/1019-5149.JTN.9685-14.4. [DOI] [PubMed] [Google Scholar]
- 77.Nichol A, French C, Little L, Haddad S, Presneill J, Arabi Y, et al. Erythropoietin in traumatic brain injury (EPO-TBI): a double-blind randomised controlled trial. Lancet. 2015;386(10012):2499–2506. doi: 10.1016/S0140-6736(15)00386-4. [DOI] [PubMed] [Google Scholar]
- 78.Concato J, Peduzzi P, Huang GD, O’Leary TJ, Kupersmith J. Comparative effectiveness research: what kind of studies do we need? J Invest Med. 2010;58(6):764–769. doi: 10.231/JIM.0b013e3181e3d2af. [DOI] [PubMed] [Google Scholar]