Abstract
Objectives
Bipolar disorder is associated with elevated risk of suicide attempts and deaths. Key aims of the International Society for Bipolar Disorders Task Force on Suicide included examining the extant literature on epidemiology, neurobiology and pharmacotherapy related to suicide attempts and deaths in bipolar disorder.
Methods
Systematic review of studies from 1 January 1980 to 30 May 2014 examining suicide attempts or deaths in bipolar disorder, with a specific focus on the incidence and characterization of suicide attempts and deaths, genetic and non-genetic biological studies and pharmacotherapy studies specific to bipolar disorder. We conducted pooled, weighted analyses of suicide rates.
Results
The pooled suicide rate in bipolar disorder is 164 per 100,000 person-years (95% confidence interval = [5, 324]). Sex-specific data on suicide rates identified a 1.7:1 ratio in men compared to women. People with bipolar disorder account for 3.4–14% of all suicide deaths, with self-poisoning and hanging being the most common methods. Epidemiological studies report that 23–26% of people with bipolar disorder attempt suicide, with higher rates in clinical samples. There are numerous genetic associations with suicide attempts and deaths in bipolar disorder, but few replication studies. Data on treatment with lithium or anticonvulsants are strongly suggestive for prevention of suicide attempts and deaths, but additional data are required before relative anti-suicide effects can be confirmed. There were limited data on potential anti-suicide effects of treatment with antipsychotics or antidepressants.
Conclusion
This analysis identified a lower estimated suicide rate in bipolar disorder than what was previously published. Understanding the overall risk of suicide deaths and attempts, and the most common methods, are important building blocks to greater awareness and improved interventions for suicide prevention in bipolar disorder. Replication of genetic findings and stronger prospective data on treatment options are required before more decisive conclusions can be made regarding the neurobiology and specific treatment of suicide risk in bipolar disorder.
Keywords: Bipolar disorder, suicide or suicide attempts, pharmacotherapy, prevalence, neurobiology
Introduction
The tragedy of suicide is not unique to bipolar disorder (BD), but it is an inescapable reality that people who struggle with the illness are at elevated risk of suicide attempts and suicide (Chen et al., 2009; Crump et al., 2013; Dennehy et al., 2011; Hoyer et al., 2000; Nordentoft et al., 2011; Novick et al., 2010; Ösby et al., 2001; Singhal et al., 2014; Tondo et al., 2003). To better understand this issue, the International Society for Bipolar Disorders (ISBD) launched a special task force with the goals of summarizing the rapidly expanding literature on suicide attempts and suicide deaths in BD, and contributing new data when possible. The ISBD Task Force on Suicide in BD included 20 experts from across 12 countries and focused on four key areas of review: (1) epidemiology and characteristics of suicide attempts and suicide in BD, (2) identifying factors associated with greater likelihood of suicide attempts or suicide in people with BD, (3) neurobiological correlates of suicide attempts and deaths in BD and (4) clinical interventions for BD as they pertain to impact on likelihood of suicide attempts or deaths. This specific article provides an introduction to the work of the task force, and reports on the findings in the areas of epidemiology, neurobiology and pharmacotherapy studies.
While other excellent reviews have been published over the years on suicide attempts and deaths in BD (Baethge and Cassidy, 2013; Gonda et al., 2012; Hawton et al., 2005; Malhi et al., 2013; Mathews et al., 2013; Pompili et al., 2013; Yerevanian and Choi, 2013), this paper provides an important contribution to the literature by being an updated review on the topic, and conducting pooled analyses of suicide rates that include large studies that were not part of prior analyses (Novick et al., 2010; Tondo et al., 2003).
Models for understanding suicide attempts and deaths in people with BD can be enhanced by incorporation of diagnosis-specific neurobiological data. The vast literature on the neurobiology of suicide and suicidal behavior has been extensively reviewed in other publications (Mann and Currier, 2010; Pandey and Dwivedi, 2010; Stanley and Stanley, 1989; Turecki et al., 2012; Van Heeringen and Mann, 2014); however, most studies have not specifically examined BD samples. Based on the understanding that the underlying neurobiology of BD is at least partially distinct from other major psychiatric conditions (Anderson et al., 2013; Fillman et al., 2014; Lan et al., 2014), it would be important to examine the neurobiology of suicide attempts and suicide deaths specific to BD samples. Rather than extrapolate findings from the broad literature on neurobiology of suicide that may be relevant to BD (Mathews et al., 2013), we chose to focus on studies specific to BD samples or when subjects with BD comprised the majority of the study population.
In a similar vein, there are numerous available clinical treatment guidelines for the management of BD (Goodwin, 2009; Grunze et al., 2009, 2010; Yatham et al., 2013), but these generally do not specifically discuss suicide prevention in a comprehensive manner. Clinical interventions related to suicide prevention include a broad range of strategies, both non-pharmacological and pharmacological. We sought to review the literature specifically focused on patients with BD, while acknowledging that many important aspects of suicide prevention are not necessarily diagnosis-specific.
Methods
Overall ISBD Task Force
Members of the ISBD Task Force on Suicide identified four key areas for review based on clinical and research relevance in BD: (1) epidemiology and characteristics of suicide attempts and suicide deaths, (2) associated clinical factors, (3) neurobiological correlates and (4) clinical interventions. Each area was reviewed by a work group comprising authors with particular expertise. Work groups provided a summary of the literature that was framed within a systematic review. We conducted a PubMed search of articles using keywords ‘bipolar disorder’ and ‘suicide attempts or suicide’ published between 1 January 1980 and 30 May 2014. This was supplemented by manual examination of reference lists of articles, recently published reviews on suicide or suicide attempts in BD (Baethge and Cassidy, 2013; Chesin and Stanley, 2013; Hauser et al., 2013; Malhi et al., 2013; Pompili et al., 2013; Saunders and Hawton, 2013; Yerevanian and Choi, 2013), and data available from the members own research groups. Studies were only included if they contained data specific to BD, as evidenced by BD being present in >80% of the entire sample, or a well-defined sub-sample with separately reported data. BD was defined by Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Classification of Diseases (ICD) criteria at the time in which the studies were conducted. We only included data that examined suicide attempts or suicide deaths, as studies solely examining suicidal ideation (SI) or non-suicidal self-injury were beyond the scope of the review. There were no limitations on the methodological designs of the studies reviewed, which included retrospective and prospective clinical studies, epidemiological surveys, analyses of health care administrative databases and reviews of suicide deaths. Using the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) framework for systematic review (Moher et al., 2009), we identified 1816 articles + 2 additional conference abstracts which were screened for inclusion and exclusion criteria, resulting in 364 full texts being assessed for eligibility by two investigators (A.S. and C.R.), with any discrepancies discussed. Two of these studies were included after task force members provided additional unpublished data on published studies that permitted satisfaction of eligibility criteria. In all, 127 articles were subsequently excluded based on the same criteria, resulting in 237 studies determined eligible for inclusion in the review.
Statistical analyses of suicide rates
In addition to a summary of the overall literature, all studies that specifically reported on rates of suicide within a BD sample were pooled by sample size and exposure years to calculate overall suicide rates.
We calculated pooled suicide rates weighted by sample size and weighted by exposure years (per 100 person-years) with 95% confidence intervals (CIs). A pooled suicide rate by sample size was calculated by assigning each study a weighting based on the number of subjects in that study as a percentage of the entire sample of studies, and calculating a weighted pooled suicide rate by sample size. Pooled suicide rate by exposure years was calculated by assigning each study a weighting based on the number of person-years (product of sample size × average duration of the study monitoring period) in that study as a percentage of the entire number of person-years of all studies, and calculating a weighted pooled suicide rate by exposure years. Both types of pooled analyses were reported to facilitate comparison with the available literature, which varies in methodology. We further calculated pooled suicide rates separately for men and women, using all studies in which sex-specific data was available.
Results
Section A: epidemiology
Suicide rates among persons with bipolar disorder
Based on articles published from 1945 to 2001, Tondo et al. (2003) conducted a pooled analysis of 28 studies that reported a 3.9% rate of suicide (828/21,484 BD subjects) during a mean follow-up of 9.93 years. This translated into a suicide rate of 0.395 per 100 person-years (95% CI = [0.321, 0.469]) and a standardized mortality ratio (SMR) compared to the general population of 22.1 (95% CI = [20.0, 24.1]). Since 2001, there have been a number of large studies that supplement the data on suicide rates in BD, and the results of our updated pooled analyses are shown in Table 1. The two largest recent studies took place in the United States and Britain. Among 32,360 BD subjects from US health databases, 0.23% died from suicide during a median follow-up of 2.7 years, resulting in a suicide rate of 0.084 per 100-person years (Simon et al., 2007). A similar suicide rate of 0.08 per 100 person-years (Osborn et al., 2008) was reported among 10,742 BD subjects in the UK general practice research database during a median follow-up of 4.7 years. Mostly, other large studies since 2001 provide similar results (Dennehy et al., 2011; Dutta et al., 2007; Gonzalez-Pinto et al., 2011; Nordentoft et al., 2011), with suicide rates ranging from 0.08 (Osborn et al., 2008) to 0.18 (Dutta et al., 2007) per 100 person-years. The exceptions are two large clinical samples which report much higher rates among BD inpatients from a private hospital (1.11 suicide deaths per 100 person-years) (Sani et al., 2011) and a specialized mood disorders outpatient clinic (0.69 suicide deaths per 100 person-years) (Tondo et al., 2007).
Table 1.
Pooled suicide rates (weighted) for people with bipolar disorder.
| Paper | Year | No. of suicides |
Duration (years) |
Exposurea
(person- years) |
Suicide rate (per 100 person years) |
Suicide rate— Male (per 100 person years) |
Suicide rate— Female (per 100 person years) |
|---|---|---|---|---|---|---|---|
| Morrison et al. | 1982 | 12/443 | 8.5 | 3766 | 0.319 | ||
|
| |||||||
| Martin et al. | 1985 | 0/19 | 9 | 171 | 0.000 | ||
|
| |||||||
| Weeke and Vaeth | 1986 | 17/417 | 7 | 2919 | 0.582 | ||
|
| |||||||
| Black et al. | 1988 | 7/586 | 7 | 4102 | 0.171 | ||
|
| |||||||
| Dingman et al. | 1988 | 1/19 | 15 | 285 | 0.351 | ||
|
| |||||||
| Friis et al. | 1991 | 2/14 | 7 | 98 | 2.041 | ||
|
| |||||||
| Newman and Bland | 1991 | 19/1429 | 4.8 | 6859 | 0.277 | ||
|
| |||||||
| Sharma and Marker | 1994 | 9/472 | 9 | 4248 | 0.212 | ||
|
| |||||||
| Koukopoulos et al. | 1995 | 5/89 | 2.8 | 245 | 2.043 | ||
|
| |||||||
| Thies-flechtner et al. | 1996 | 8/146 | 2.5 | 365 | 2.192 | ||
|
| |||||||
| Angst et al. | 1998 | 11/220 | 28 | 6160 | 0.179 | ||
|
| |||||||
| Bocchetta et al. | 1998 | 5/47 | 5.6 | 263 | 1.900 | ||
|
| |||||||
| Brodersen et al. | 2000 | 7/61 | 16 | 976 | 0.717 | ||
|
| |||||||
| Kallner et al. | 2000 | 7/106 | 8.2 | 869 | 0.805 | ||
|
| |||||||
| Kleindiesnt and Greil | 2000 | 1/85 | 2.5 | 213 | 0.471 | ||
|
| |||||||
| Ösby et al. | 2001 | 672/15,386 | 11.1 | 170,615 | 0.393 | 0.498 | 0.323 |
|
| |||||||
| Gladstone et al. | 2001 | 5/813 | 5 | 4065 | 0.123 | ||
|
| |||||||
| Dutta et al. | 2007 | 8/235 | 18.8 | 4422 | 0.181 | 0.369 | 0.040 |
|
| |||||||
| Simon et al. | 2007 | 73/32,360 | 2.7 | 87,372 | 0.084 | 0.171 | 0.071 |
|
| |||||||
| Tondo et al. | 2007 | 22/843 | 5.8 | 4889 | 0.450 | 0.686 | 0.257 |
|
| |||||||
| Osborn et al. | 2008 | 41/10,742 | 4.7 | 50,487 | 0.080 | ||
|
| |||||||
| Ilgen et al. | 2010 | 683/96,099 | 7 | 672,693 | 0.102 | ||
|
| |||||||
| Dennehy et al. | 2011 | 8/4360 | 1.3 | 5668 | 0.141 | 0.252 | 0.065 |
|
| |||||||
| Sani et al. | 2011 | 57/1765 | 2.9 | 5119 | 1.114 | 1.458 | 0.869 |
|
| |||||||
| Gonzalez-Pinto et al. | 2011 | 3/169 | 10 | 1690 | 0.178 | ||
|
| |||||||
| Nordentoft et al. | 2011 | 175/5927 | 18 | 106,686 | 0.164 | 0.210 | 0.129 |
|
| |||||||
| Total by Study | 1858/172,852 | 8.5 | 1,145,245 | ||||
|
| |||||||
| Pooled (by sample size) |
0.151b (0.023–0.471) | 0.324 (0–0.820) | 0.160 (0–0.472) | ||||
|
| |||||||
| Pooled (by exposure years) |
0.164c,d (0.005–0.324) | 0.366d (0–0.762) | 0.217d (0–0.482) | ||||
95% CI: confidence interval.
Exposure years: sample size multiplied by duration of follow-up. For Osborn et al. (2008), Nordentoft et al. (2011) and Sani et al. (2011), we used mean duration of follow-up for the entire study sample, not specifically for those with bipolar disorder (the latter not being available).
Pooled mean, weighted by sample size, with 95% CI.
Pooled mean, weighted by exposure years, with 95% CI.
95% CI range included <0 was recorded as 0.
The effect of the newer data has been to increase the total sample size by eightfold and to lower the overall estimated suicide rate from that previously published (Tondo et al., 2003). Our pooled analysis weighted by sample size (total n = 172,852) identified a suicide rate of 0.151 per 100 person-years (95% CI = [0.023, 0.471]). The pooled analysis weighted by number of exposure years (total of 1,145,245 person-years) identified a suicide rate of 0.164 per 100 person-years (95% CI = [0.005, 0.324]). Using a smaller sample of only seven studies that included sufficient information to examine sex-effects, the pooled analysis weighted by exposure years identified a suicide rate among men of 0.366 per 100 person-years (95% CI = [0, 0.762]) and a suicide rate among women of 0.217 per 100 person-years (95% CI = [0, 0.482]). These rates are higher than the overall rate because only a non-representative subsample of studies reported data by sex.
Bipolar disorder suicides as a proportion of the population
Another aspect of suicide data in BD relates to the proportion of all suicides in a population comprising persons with BD. Large epidemiological samples from Taiwan, Japan, United States and Canada reported that 3.4–5.9% of all suicide deaths occurred among people with BD (Chen et al., 2009; Karch et al., 2006; Schaffer et al., 2014; Takizawa, 2012). Higher proportions were found in a large study of US Veterans (9.0% of suicides were among people with BD) (Ilgen et al., 2010), a national English sample (9.6% of all suicide deaths) (Clements et al., 2013), and among psychiatric outpatients (14% of all suicides) (Brown et al., 2000). A total of 47% of a consecutive Hungarian sample of suicide decedents retrospectively diagnosed with depression at the time of death were identified as having BD, mostly type II (Rihmer et al., 1990).
Suicides rates across diagnoses
Comparisons of suicide rates or SMRs between BD and unipolar depression have shown mixed results. Four studies reported higher SMRs for suicide in unipolar depression using data from large psychiatric inpatient or prison inmate registries (Baillargeon et al., 2009; Fazel et al., 2013; Hoyer et al., 2000; Ösby et al., 2001), while several other studies showed the opposite result of higher rates in BD among large outpatient, inpatient or broad clinical samples (Ilgen et al., 2010; Nordentoft et al., 2011; Sani et al., 2011; Singhal et al., 2014; Tondo et al., 2007). This reinforces the fact that there are additional moderating factors such as likelihood of hospitalization or incarceration, severity of illness, comorbidities and subject recruitment that likely influence the comparisons of suicide risk across mood disorder diagnoses.
Similarly, mixed results have also been reported related to differences in suicide risk between BD and schizophrenia groups. A number of studies report numerically higher rates of suicide in BD than schizophrenia (Barner-Rasmussen, 1986; Karch et al., 2006; Osborn et al., 2008; Sani et al., 2011), such as Osborn et al. (2008) who found that among 46,136 UK patients with severe mental illness, the adjusted hazard ratio for suicide death compared to the general population was 8.74 (95% CI = [5.80, 13.17]) for the BD group and 7.00 (95% CI = [4.78, 10.25]) for the schizophrenia group. In two large Asian epidemiological samples and a study of the Texas prison system (Baillargeon et al., 2009; Chen et al., 2009; Takizawa, 2012), the opposite trend was reported, with schizophrenia associated with a numerically higher relative risk or proportion of suicides compared to BD. While the studies of proportions of suicide by diagnosis are impacted by possible differences in the prevalence of each diagnosis, overall there is no clear signal from the literature that BD or schizophrenia are associated with substantially different suicide risks.
Specific methods of suicide
There is noteworthy similarity in the pattern of most common methods of suicide deaths across large studies in BD. Three studies each examined methods in >300 BD suicides from Taiwan, Sweden and the United Kingdom, and reported rates were 31.0–32.5% for hanging, 24.9–29.8% for self-poisoning and 13.7–18.9% for jumping (Chen et al., 2009; Hunt et al., 2006; Ösby et al., 2001). Table 2 summarizes the data on method of suicide deaths reported in nine BD studies across nine countries.
Table 2.
Summary of international data on method of suicide deaths in bipolar disorder studies.
| Paper | Hanging (%) |
Self-poisoning (%) |
Jumping (%) |
Gunshot wounds (%) |
Charcoal burning (%) |
Carbon monoxide (%) |
Stabbing/ cutting (%) |
Drowning (%) |
|---|---|---|---|---|---|---|---|---|
|
Ösby et al. (2001)
N = 672 (Sweden) |
31.0 | 30.0 | 13.7 | 5.2 | – | – | 2.7 | 11.0 |
|
| ||||||||
|
Chen et al. (2009)
N = 482 (Taiwan) |
32.2 | 24.9 | 17.4 | 0.2 | 13.5 | – | 2.1 | 4.8 |
|
| ||||||||
|
Hunt et al. (2006)
N = 391 (United Kingdom) |
32.5 | 27.4 | 18.9 | – | – | 4.3 | – | 6.9 |
|
| ||||||||
|
Schaffer et al. (2014)
N = 170 (Canada) |
17.1 | 33.5 | 30.0 | 2.4 | 1.2 | 2.9 | 2.9 | 2.9 |
|
| ||||||||
|
Rihmer et al. (1990)
N = 47 (Hungary) |
17.0 | 53.2 | 25.5 | – | – | – | – | – |
|
| ||||||||
|
Keks et al. (2009)
N = 35 (Australia) |
46.0 | 17.0 | 11.0 | – | – | 17.0 | – | – |
|
| ||||||||
|
Isometsä et al. (1994)
N = 31 (Finland) |
– | 35.5 | – | – | – | – | – | – |
|
| ||||||||
|
Gos et al. (2009)
N = 7 (Germany) |
28.6 | 42.9 | – | – | – | – | 14.3 | – |
|
| ||||||||
|
Dennehy et al. (2011)
N = 8 (United States) |
25.0 | 25.0 | – | 25.0 | – | – | – | – |
Ösby et al. (2001): n = 45 unknown method.
Chen et al. (2009): n = 16 unspecified method.
Hunt et al. (2006): Burning (n = 7); other = defined as cutting, electrocution, firearms and suffocation (n = 22).
Schaffer et al. (2014): n = 10 subway, train or car collisions, n = 3 fire, burns or electrocution and n = 6 plastic bag or helium gas.
Rihmer et al. (1990): other = defined as train, shooting and cutting (n = 1 each) but diagnosis unknown.
Keks et al. (2009): n = 3 unknown method; Jumping specifically ‘in front of vehicle’.
Isometsä et al. (1994): n = 20 unspecified method.
Gos et al. (2009): n = 1 electric shock.
Dennehy et al. (2011): n = 2 unknown method.
A study comparing 482 BD suicides in Taiwan to suicide deaths without a recorded psychiatric diagnosis (Chen et al., 2009) found that BD suicides were significantly more likely to occur via jumping (odds ratio [OR] = 2.2, 95% CI = [1.8, 2.7]) and significantly less likely to occur by charcoal burning (OR = 0.5, 95% CI = [0.4, 0.7]). Similarly, Ösby et al. compared 672 BD suicides with suicides from the general population and found that jumping was significantly more common in the BD group. Shooting was less common in the male BD group compared to males in the general population and self-poisoning was less common in the female BD group compared to females in the general population (Ösby et al., 2001). In a large Canadian sample of suicide deaths, rates of self-poisoning among those with BD were significantly higher (33.5% vs 17.4%) and rates of hanging were significantly lower (17.1% vs 29.7%) (Schaffer et al., 2014).
Isometsä et al. (1994) examined 31 BD suicides for specific prescriptions used in the 11 suicides that occurred by self-poisoning and found that 45% used neuroleptics, 18% used lithium, 18% used a combination of more than two benzodiazepines and 9% used a tricyclic antidepressant (TCA). Low rates of death due to lethal levels of lithium (2.9%) was also reported in a Toronto sample of 34 BD suicide deaths by self-poisoning, with carbamazepine being much more commonly present in lethal levels (20.6% of deaths), along with antipsychotics (32.4%), opioids (29.4%), benzodiazepines (26.5%) and diphenhydramine (14.7%) (Schaffer et al., 2012).
Frequency of suicide attempts among people with bipolar disorder
Numerous studies have reported on suicide attempt frequencies within BD samples, including a meta-analysis of 24 studies that compared suicide attempts in BD I and II patients (Novick et al., 2010). The prospective studies had follow-up periods ranging from 18 months to 44 years and reported an average suicide attempt frequency of 23.8% in BD I patients and 19.8% in BD II patients. Two prospective studies published after 2010 show comparable frequencies: a 22% suicide attempt frequency in a 5-year follow-up study of a combined BD I and II group (Altamura et al., 2010) and an 18.3% frequency in a 10 year follow-up study of BD I patients (Gonzalez-Pinto et al., 2011). The Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) sample of 4360 BD subjects had a 4.1% suicide attempt frequency during a mean follow-up period of 10 months (Dennehy et al., 2011).
The Novick et al. (2010) meta-analysis also included retrospective data, which yielded slightly higher lifetime suicide attempt frequencies of 36.3% in BD I patients and 32.4% in BD II. Large retrospective epidemiological studies published since 2010 have found frequencies of suicide attempts in BD samples that range from 22.9% to 25.6% (Merikangas et al., 2011; Sala et al., 2012). Higher frequencies were reported in large clinical samples (Dennehy et al., 2011; Dervic et al., 2011; Shabani et al., 2013) with the STEP-BD sample having a retrospective suicide attempt frequency of 36% (Dennehy et al., 2011). Ryu et al. (2010) found a low lifetime suicide attempt frequency of 13.1% among a Korean sample of BD inpatients.
The ratio of suicide attempts to suicide deaths is between 20 and 30 in the general population (Simon and Hales, 2006) but appears to be lower in BD samples. Tondo et al. (2007) identified a ratio of 13:1 indicating a lower ratio of attempts/deaths by suicide possibly due to stronger intent to die or use of more lethal methods. A large English study reported a 16:1 ratio in BD, lower than most major psychiatric disorders other than schizophrenia (Singhal et al., 2014).
Specific methods of suicide attempts in bipolar disorder
Self-poisoning was the most common method reported in each study of BD suicide attempters (D’Ambrosio et al., 2012; De Abreu et al., 2012; Oquendo et al., 2009; Ruengorn et al., 2012; Ryu et al., 2010; Tsai et al., 1999b). The proportion of suicide attempts by self-poisoning ranged from 29.8% to 80.1%, with a pattern of Asian countries (Thailand, Taiwan and Korea) reporting relatively lower proportions (29.8–34.2%) (Ruengorn et al., 2012; Ryu et al., 2010; Tsai et al., 1999b) and other areas of the world reporting relatively higher proportions (47.5–80.1%) (D’Ambrosio et al., 2012; De Abreu et al., 2012; Oquendo et al., 2009). Other methods cited in at least one study of BD suicide attempters include cutting (5.6–22.7%) (D’Ambrosio et al., 2012; Oquendo et al., 2009; Ruengorn et al., 2012; Ryu et al., 2010; Tsai et al., 1999b), jumping (4.8–13.2%) (D’Ambrosio et al., 2012; Oquendo et al., 2009; Ruengorn et al., 2012; Ryu et al., 2010), hanging (0.7–26.3%) (D’Ambrosio et al., 2012; Oquendo et al., 2009; Ruengorn et al., 2012; Ryu et al., 2010), drowning (0.2–16.7%) (Oquendo et al., 2009; Ruengorn et al., 2012; Tsai et al., 1999b; Yen et al., 2008), gas inhalation (2.8–5.7%) (D’Ambrosio et al., 2012; Tsai et al., 1999b), shooting (1.4–4.2%) (D’Ambrosio et al., 2012; Oquendo et al., 2009), self-immolation (1.3–2.1%) (Oquendo et al., 2009; Ryu et al., 2010) and intentional car accident (1.4%) (D’Ambrosio et al., 2012). Two studies reported on attempters using a combination of methods, with a Thai sample reporting 26.4% using two or more methods (Ruengorn et al., 2012; Ryu et al., 2010).
Several studies compared the frequency of non-violent vs violent methods, with the latter being less common and occurring in only 13.2–17.5% of suicide attempts among BD patients (De Abreu et al., 2012; Tsai et al., 1999b; Yen et al., 2008); however, there was little consistency across studies of the definition of violent or non-violent methods. Lethality of suicide attempts was reported in one study to be significantly greater among male BD attempters compared to female BD attempters (Zalsman et al., 2006).
Section B: neurobiology
Genetics and completed suicide in BD samples
A total of 16 genes have been shown to be differentially expressed in a BD suicide group when compared with a BD non-suicide group. Of these genes, 12 were identified in exclusively BD samples and 4 in samples with a majority of BD subjects. In a sample of 45 deaths of people with BD (22 suicides and 23 non-suicide deaths) derived from the Stanley Medical Research Institute (SMRI) Database, the prefrontal cortex expression of the following 10 genes were found to be down-regulated in BD suicides (Kim et al., 2007): transmembrane 4 L six family member 1 (TM4SF1); chitinase 3-like protein 1 (cartilage glycoprotein-39; CHI3L1); empty spiracles homolog 2 (Drosophila; EMX2); low-density lipoprotein receptor (LDLR); Zic family member 1 (odd-paired homolog, Drosophila; ZIC1); phospholipid scramblase 4 (PLSCR4); zinc fingers and homeoboxes, mRNA; cDNA DKFZp586B211 (from clone DKFZp586B211; ZHX2); tissue inhibitor of metalloproteinases (TIMP) metallopeptidase inhibitor 1 (TIMP1) and neuron navigator 2 (NAV2). In the same sample, the prefrontal cortex expression of the following three genes was up-regulated in BD suicides: tripartite motif-containing 23 (TRIM23); stress 70 protein chaperone, microsome-associated, 60 kDa (STCH) and gamma-aminobutyric acid (GABA) A receptor, alpha 5 (GABRAS).
In a more focused post-mortem genetic analysis of 14 BD suicides also derived from the SMRI database, significantly increased expression of acid phosphatase 1 (ACP1) in Brodmann area 46 was identified among those that died by suicide (Willour et al., 2012). A third study (Tochigi et al., 2008) on a sample of eight BD suicides from the SMRI dataset identified differential expression in the prefrontal cortex of dihydroorotase (CAD) and Na+/K+–ATPase alpha 3 subunit (ATP1A3). A fourth study using the SMRI dataset did not identify differential mRNA expression in the prefrontal cortex or allele frequency of Dopamine- and cAMP-regulated phosphoprotein of 32 kDa) (DARPP-32) between BD suicide and non-suicide deaths, those with schizophrenia and controls (Feldcamp et al., 2008). A novel study of DNA integrity reported a higher number of DNA strand breaks in the frontal cortex, pons, medulla and thalamus in an Indian sample of BD suicide deaths compared to accident victims with no psychiatric history (Mustak et al., 2010).
A number of other studies reported on genetic polymorphisms or gene expression in suicide samples that included a majority of BD subjects. In a small sample of 10 suicides, 9 of which had BD, De Luca et al. (2007) found lower expression of 5-HT2A mRNA but no difference in methylation of 5-HT2A receptor gene in the prefrontal cortex between suicide and non-suicide victims (De Luca et al., 2009). They also reported no association with tryptophan hydroxylase 2 (TPH2) promoter genotypes or haplotypes (De Luca et al., 2006). Dracheva (2008) used the SMRI sample and found 5-HT2CR mRNA editing variations to be associated with suicide, but no difference was found between BD and schizophrenia suicide groups.
Genetics and suicide attempts
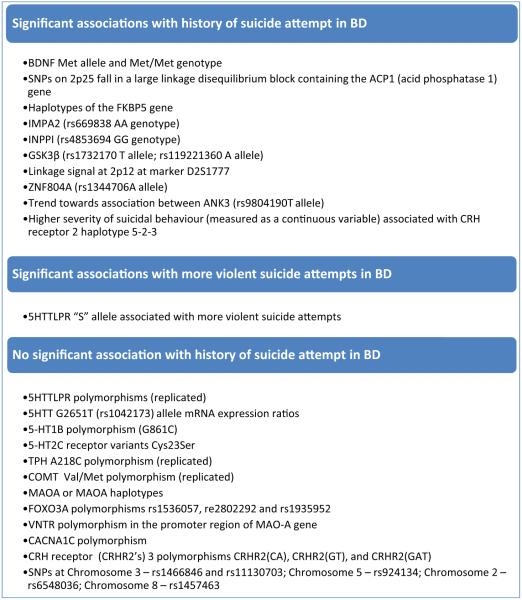
A number of studies examined for associations between specific genetic polymorphisms and a history of suicide attempt in BD samples. The principal findings are summarized in Figure 1.
Figure 1. Summary of findings on genetic associations with suicide attempts in studies of bipolar disorder.
Altamura et al. (2010), Baumann et al. (1999), Bellivier et al. (2000), Benedetti et al. (2011), Berrettini et al. (1986), Campos et al. (2010), D’Ambrosio et al. (2012), De Luca et al. (2005a, 2005b, 2006, 2009), Dowlatshahi et al. (1999), Dracheva et al. (2008), Evans et al. (2012), Feldcamp et al. (2008), Finseth et al. (2014), Jimenez et al. (2013), Kamali et al. (2012), Kim et al. (2002, 2007, 2008), Le-Niculescu et al. (2013), Leszczynska-Rodziewicz et al. (2014), Lopez et al. (2007), Mahon et al. (2012), Malloy-Diniz et al. (2011), Matsuo et al. (2010), Monfrim et al. (2014), Nery et al. (2014), Nery-Fernandes et al. (2012), Neves et al. (2008, 2010), Park et al. (2013), Perlis et al. (2012), Pinto et al. (2011), Pompili et al. (2008), Shabani et al. (2013), Sher et al. (2006, 2012), Singhal et al. (2014), Souery et al. (2001), Stange et al. (2014), Suttajit et al. (2013), Thibodeau et al. (2013), Tidemalm et al. (2014), Tochigi et al. (2008), Tsai et al. (1999a), Vuksan-Cusa et al. (2009) and Willour et al. (2012).
A well-designed series of studies investigating whole-blood (predominantly lymphocyte) gene expression levels in BD subjects identified a top biomarker candidate (blood levels of spermidine/spermine N1-acetyltransferase 1 [SAT1]) for conversion from no SI to a high SI state (Le-Niculescu et al., 2013) and identified significant predictive capacity for future hospitalization involving SI or acts. While replication of data is required, this approach is noteworthy for combining relatively accessible potential biomarkers with standard clinical assessments.
Non-genetic central and peripheral markers
There were no significant findings among studies of non-genetic markers and suicide deaths. Serum lipid or glucose levels during a past admission to hospital were not associated with suicide deaths in a Korean BD sample (Park et al., 2013). A post-mortem brain analysis of 15 BD suicides did not identify any difference in temporal cortex cAMP response element binding (CREB) levels between suicide and non-suicide deaths (Dowlatshahi et al., 1999). Another similar post-mortem brain study (Baumann et al., 1999) found no difference in mean number of noradrenergic neurons in the locus ceruleus.
A larger literature exists on potential non-genetic markers of suicide attempt in BD.
Neuroimaging studies found the following to be associated with a history of suicide attempts in BD: periventricular white matter and deep white matter hyperintensities (Pompili et al., 2008); lower fractional anisotropy in white matter of the left orbitofrontal region (Mahon et al., 2012) and decreased grey matter volume in dorsolateral prefrontal cortex (DLPFC), orbitofrontal cortex (OFC), anterior cingulate, superior temporal cortex, parieto-occipital cortex and basal ganglia (Benedetti et al., 2011). There were no differences reported in any regional corpus callosum areas among suicide attempters, but female BD patients with a history of suicide attempts had a significant inverse correlation between anterior genu area and impulsivity; a relationship that was not seen among BD non-suicide attempters (Matsuo et al., 2010). The lack of any differences in corpus callosum between BD suicide attempters and non-attempters has been replicated (Nery-Fernandes et al., 2012). All other imaging findings still require replication.
Two studies found no association between history of suicide attempts and cerebrospinal fluid (CSF) monoamine metabolites (Berrettini et al., 1986; Sher et al., 2006); however, these metabolites were negatively correlated with the maximum lethality of suicide attempt (Sher et al., 2006). One study identified significantly higher levels of corticotropin-releasing hormone in BD subjects with elevated suicide risk (Monfrim et al., 2014). Results were mixed with regard to the link between lipid levels and suicide attempts. Lower serum cholesterol (Tidemalm et al., 2014; Vuksan-Cusa et al., 2009), triglyceride (Vuksan-Cusa et al., 2009) and n-6 arachidonic acid (Evans et al., 2012) levels were reported in BD suicide attempters, but no such associations were identified in large Italian and Korean studies (D’Ambrosio et al., 2012; Kim et al., 2002). Significantly, higher bedtime salivary cortisol has been reported in BD suicide attempters compared to non-attempters, but no differences in morning cortisol were found (Kamali et al., 2012). Serum testosterone levels have been positively correlated with the number of suicide attempts in a sample of 67 BD subjects, even when controlling for sex (Sher et al., 2012). A small post-mortem study has shown that lower levels of the neurosteroid pregnenolone in the parietal cortex may be relevant to the neurobiology of suicide in BD and schizophrenia (Youssef et al., 2015).
Section C: clinical interventions in bipolar disorder
High risk time periods in relation to treatment contacts
The periods during and following hospital admission represent high risk times for suicide death among BD patients, with 14% of BD suicides occurring during an inpatient stay, with an additional 26% occurring within 6 weeks of discharge (Keks et al., 2009). In a large UK treated sample of BD suicides, 28.2% of deaths occurred within 3 months of discharge from hospital, a rate significantly higher than for other psychiatric diagnoses combined (Clements et al., 2013). There was also a significantly higher rate of last treatment contact in the week prior to death compared to other psychiatric diagnoses (61.3% vs 48.8%) (Clements et al., 2013). Barner-Rasmussen (1986) reported that among BD inpatients that died by suicide during or within 1 year of hospitalization, 32.8% died in hospital and 38% died within the first 2 weeks of discharge. A subsequent analysis of Danish epidemiological data (Hoyer et al., 2000) reported SMRs for completed suicide in BD to be highest during year 1 following first admission to hospital (SMR = 53.8), followed by years 1–3 (SMR = 20.2), years 3–5 (SMR = 14.9) and 5+ years (SMR = 10.7). A similarly designed Swedish study that additionally focused on age and sex differences (Ösby et al., 2001) reported first year post-admission suicide SMRs for males and females under 30 years old with BD to be 59.4 and 43.3, respectively. Among males, the SMR dropped in the older age groups, with an SMR = 31.9 in the over 65 age group. A different pattern was seen in females, with an increase in SMR with age, culminating in a SMR = 65.5 in the over 65 age group. For all age groups and both sexes, the SMRs were generally incrementally lower for longer follow-up time periods, up to > 5 years.
Suicide attempts have also been found to be significantly more common (OR = 3.57) during the year following inpatient psychiatric care (Tidemalm et al., 2014).
Duration of untreated illness
Consistent evidence from both clinical and epidemiological samples suggests that a longer duration of untreated BD illness is associated with an increased likelihood of suicide attempts (Altamura et al., 2010; Angst et al., 1998; Apfelbaum et al., 2013; Azorin et al., 2009; Bellivier et al., 2011). Altamura et al. (2010) reported that patients with greater than 2 years of untreated illness were more likely to attempt suicide and had a higher number of attempts during follow-up.
Type of first treatment contact
One study (Kessing and Munk-Jorgensen, 2004) reported that patients with BD whose first treatment contact included psychiatric admission were at increased risk of suicide compared to BD patients whose first treatment contact was on an outpatient basis.
Overall effect of treatment
An extensive literature addresses the impact of treatments for BD on suicide attempts or deaths. In a large trial of BD subjects receiving algorithm-guided pharmacotherapy plus interpersonal and social rhythm therapy (IPSRT)/intensive clinical management, pre-trial suicide attempt rate was 1.05/100 person-months, but significantly dropped to 0.31/100 person-months during acute treatment, and even further to 0.06/100 person-months during maintenance treatment (Rucci et al., 2002). Data from a BD US Veterans sample found discontinuation of a mood stabilizer resulted in a 16-fold increased rate of suicide behavior (Yerevanian et al., 2007a).
A sizable proportion of suicides occur when BD patients are receiving no treatment (Ahearn et al., 2013; Angst et al., 1998; Schou and Weeke, 1988). Despite this, an analysis of several maintenance BD trials found no significant difference in rates of suicide attempts or deaths between active and placebo groups; however, the analysis was hampered by low base rates (Storosum et al., 2005). A more recent analysis of clinical trial data identified a significant effect of anti-manic treatments on lowering overall mortality rate during study follow-up periods (of which suicide comprised the most frequent cause of death), but the analysis was underpowered to directly examine the effect on suicide rates (Khan et al., 2013). In an Australian sample of 35 suicides among people with BD, only 48% were retrospectively considered to be at high risk of suicide, with pharmacological and psychosocial interventions not reaching benchmark standards in a majority of cases (Keks et al., 2009). Furthermore, evidence suggests a greater likelihood of complex polypharmacy being prescribed to BD patients with a history of suicide attempt (Weinstock et al., 2014). This underscores the imperative of matching clinical interventions to the needs of patients with BD, and the tremendous challenges at both clinical and research levels to understand what interventions are most effective for preventing suicide attempts and suicide in this population.
Lithium
The extensive literature on the impact of lithium use or discontinuation on both suicide attempts and suicide deaths in BD samples has been widely reviewed and meta-analyzed (Baldessarini and Tondo, 2008; Cipriani et al., 2005). Cipriani et al. (2013) recently published an updated systematic review and meta-analysis of suicide risk within randomized controlled trials (RCTs) of lithium for mood disorders and reported that lithium was significantly associated with a reduced risk of suicide compared to placebo (OR = 0.13, 95% CI = [0.03, 0.66]), but no significant reduction in risk of deliberate self-harm (which included both suicide attempts and non-suicidal self-injury) was identified (OR = 0.60, 95% CI = [−0.27, 1.32]). Other than lithium treatment being associated with a reduced risk of deliberate self-harm vs carbamazepine (OR = 0.14, 95% CI = [0.02, 0.83]), there were no significant drug–drug differences found. Only 19/48 trials in their analyses included BD participants only, and their reported comparisons among the BD-only trials were limited to one or two studies per comparison to placebo or other drugs, resulting in wide CIs and no significant results other than the lithium vs carbamazepine finding noted above.
Baldessarini and Tondo (2008) have similarly reported meta-analytic results of lower risk of suicidal acts during maintenance treatment with lithium compared to without lithium, calculating a number needed to treat (NNT) of 22.6 (95% CI = [21.0, 24.6]), and lower risk during treatment with lithium compared to anticonvulsants (risk ratio = 0.38, 95% CI = [0.33, 0.44]). This is further supported by data such as a nationwide Danish study including all patients treated with lithium (n = 13,186), irrespective of diagnosis, which found that continued lithium treatment was associ ated with reduced suicide risk, regardless of sex and age (Kessing et al., 2005). While these results are highly informative, and are supported by sophisticated neurobiological hypotheses for an anti-suicide effect (Benedetti et al., 2011; Halcomb et al., 2013; Kalkman, 2011), it is nonetheless important to incorporate prospective, comparative clinical data on the potential anti-suicide effects of lithium specifically among suicidal or high-risk patients with BD, the situation commonly faced in clinical practice. In a landmark study, Oquendo et al. (2011) conducted a long-term RCT of add-on lithium (mean duration 495 days) or valproate (mean duration 550 days) among 98 depressed or mixed BD patients with a history of suicide attempt. No suicide deaths occurred during the study and there were no significant differences between rates of suicide attempts between the two groups, but power limitations clearly impacted the results. STEP-BD data from 106 patients with a prospective suicide event (mostly commonly an attempt) found no significant association between lithium use, anti-convulsant use or atypical antipsychotic use and risk of suicide events, therefore not supporting the hypothesis of a specific anti-suicide effect of lithium (Marangell et al., 2008).
A Danish study reported that suicide rates were lower among BD patients who purchased a prescription for lithium compared to patients who purchased a prescription for an anticonvulsant, but suicide rates dropped considerably among patients who continued treatment of either type (Søndergård et al., 2008). Notably, patients on anticonvulsants who were switched to lithium or had lithium added had a reduced rate of suicide, but a switch or add-on in the other direction had no such effect.
The overall literature continues to suggest an anti-suicide effect of lithium in patients with BD compared to placebo or lithium discontinuation, but comparative randomized clinical trials have not yet confirmed the hypothesis of greater anti-suicide effect compared to other mood stabilizers, albeit with methodological and ethical limitations being a central factor. Furthermore, data are very much required in specific clinical situations to better inform the clinicians as to when to employ lithium vs other possible treatments as an anti-suicide treatment intervention and the expected magnitude of the clinical effect. Prospective controlled studies of lithium use with suicide-related outcomes during high-risk periods (e.g. mixed states, post-hospitalization) would be highly informative with direct clinical application. Similarly, the correlation between lithium level and anti-suicide effect remains understudied yet is of tremendous clinical importance.
Anticonvulsants
While lithium has received the bulk of attention, there is also a fairly extensive literature on anti-convulsants and risk of suicide attempts and deaths in BD (Ferrer et al., 2014).
In 2009, the US Food and Drug Administration (FDA) published a warning that 11 anticonvulsant medications carry an increased risk of suicidal thoughts or actions (US Department of Health and Human Services, 2009). This decision was made based on data from placebo-controlled trials in epilepsy, psychiatric disorders and other conditions. Subsequent to this warning, several studies were completed specific to BD. A meta-analysis of only psychiatric studies (Redden et al., 2011) found no difference in suicidal events between divalproex and placebo arms. A 30-year observational study of BD patients found no elevation in suicidal behavior among participants treated with anticonvulsants (Leon et al., 2012). Two large epidemiological samples of BD subjects also found no increased risk of suicide-related events with use of anticonvulsants (Arana et al., 2010; Reid, 2011), and one found significantly lower rates of suicide attempts compared to pretreatment among patients given any anticonvulsant, with the exception of topiramate or carbamazepine, for which reductions did not reach significant levels. (Gibbons et al., 2009). A further analysis of this latter dataset found that rates of suicide attempt were significantly higher during the month prior to initiations of an anticonvulsant as compared to the month after (Marcus et al., 2013). As reviewed earlier, BD patients who purchased additional prescriptions of anticonvulsants had fewer suicides than BD patients who only purchased one prescription (263 vs 528 suicide rate per 100,000 person-years, adjusted rate ratio = 0.28, 95% CI = [0.19, 0.41]) (Søndergård et al., 2008). The nearly fourfold higher risk of suicide reported in this study among subjects who purchased one prescription of an anticonvulsant compared to subjects who purchased one prescription of lithium complicates the interpretation of the literature comparing lithium to anticonvulsants (Søndergård et al., 2008), since there may be important baseline differences in these groups, perhaps driven by suicide risk impacting selection of treatment. Clinicians may be aware of the putative anti-suicide effects of lithium but also may be fearful of lithium toxicity in overdose or the risk of highly unstable patients not maintaining safe lithium levels thus leading to increased use of anticonvulsants among high-risk patients. When long-term treatment of lithium and anticonvulsants were compared, Danish patients who purchased ⩾ 6 anticonvulsants prescriptions had a substantial reduction in the risk of suicide (relative risk [RR] = 0.22, 95% CI = [0.11, 0.42], p < 0.0001) similar to patients who purchased ⩾ 6 lithium prescriptions (RR = 0.27, 95% CI = [0.12, 0.62], p = 0.006) (Smith et al., 2009).
Nonetheless, the available comparative literature, based primarily on non-randomized designs, does mostly find higher rates of suicidal events in patients on anticonvulsants compared to lithium, but this is not consistent across all studies (Ahearn et al., 2013). Baldessarini and Tondo (2009) reported nearly threefold higher rate of suicidal acts among BD subjects receiving anticonvulsants as compared to lithium. A large epidemiological sample also reported a nearly threefold increased adjusted risk of suicide deaths among BD patients receiving divalproex vs lithium (Goodwin et al., 2003). Collins and McFarland (2008) followed up with a similar study in which compared to lithium use, divalproex use was associated with a significantly higher risk of suicide attempts (hazard ratio [HR] = 1.6) but not completed suicides (HR = 1.5), gabapentin use was associated with higher risk of suicide deaths (HR = 2.6) but not attempts (HR = 1.6) and carbamazepine use had no significant effect on suicide attempts, with insufficient data on suicide deaths. A large US veterans study (n = 1306 BD patients) found no significant difference in rate of suicide attempts during periods of treatment with lithium monotherapy or divalproex monotherapy and also found the numerically lowest suicide rate to occur during treatment with the combination of lithium and divalproex (Ahearn et al., 2013). A separate large epidemiological study found a positive effect of gabapentin in reducing risk of suicide attempts in BD subjects (Gibbons et al., 2010). Several studies failed to find any significant difference in suicidal behavior between anticonvulsants and lithium, including both clinical (Oquendo et al., 2011; Yerevanian et al., 2007a) and epidemiological samples (Gibbons et al., 2009; Yerevanian et al., 2003), most notable of which is the Oquendo et al. RCT (Oquendo et al., 2011) previously reviewed that found no difference between valproate and lithium in a high-risk BD sample.
Antipsychotics
There is relatively sparse data examining antipsychotics and suicide attempts or suicide in patients with BD. Given the widespread use of both typical and atypical antipsychotics in the treatment of BD (Song et al., 2012; Vieta et al., 2013), this gap in the data is quite glaring.
Within a clinical sample of 161 US Veterans with BD, suicide attempts were significantly more common during periods of monotherapy treatment with typical antipsychotics vs atypical antipsychotics, but no differences were found when either class of antipsychotic was combined with mood stabilizers (Koek et al., 2012). There were also no significant differences in rates of suicide attempts during treatment periods with olanzapine, risperidone or quetiapine (Koek et al., 2012). This same group had also previously reported on a larger sample of veterans with BD and found that compared to periods in which patients received mood stabilizer monotherapy, suicide attempt rates were 9.4 times higher during periods of monotherapy treatment with an antipsychotic and 3.5 times higher during periods of combination treatment with a mood stabilizer plus antipsychotic (Yerevanian et al., 2007b), perhaps related to greater severity of illness. In a sub-analysis, the combination of antipsychotic plus divalproex was also significantly associated with higher suicide attempt rates than periods of treatment with divalproex monotherapy (Yerevanian et al., 2007b). In a similar analysis of a large VA hospital BD sample, Ahearn et al. (2013) identified higher rates of suicide attempts during periods of treatment with atypical antipsychotic monotherapy as compared to lithium monotherapy or divalproex monotherapy. A Danish report of n = 326 clozapine-treated BD patients (mean dose = 307 mg) identified significantly reduced hospital visits for intentional self-harm/overdose during a mean 544 days of follow-up compared to a similar duration of time prior to clozapine treatment (Nielsen et al., 2012). Any potential causal interpretation is limited by the non-randomized and non-replicated nature of these data, and unfortunately, the available clinical trials using antipsychotics in patients with BD do not adequately report on this issue.
Antidepressants
In the only prospective study of antidepressants and suicide events in BD, Marangell et al. (2008) in the STEP-BD study referenced earlier found a significant association between past 6-month use of antidepressant medication in 42 BD subjects and a suicide event. This association remained significant, although less so, even when mood state just prior to the suicide event was controlled for. However, as noted by the authors, the study was not designed to determine suicide risk, and the naturalistic treatment design does not allow for a determination of whether patients at higher risk of a suicide event were more likely to receive a prescription for an antidepressant. Two retrospective clinical studies have reported the same association between recent treatment with an antidepressant and likelihood of a suicide attempt (Raja et al., 2009; Yerevanian et al., 2007c), with one small study of elderly BD patients finding the opposite effect (Aizenberg et al., 2006).
Discussion
This paper highlights the complex literature that exists on suicide attempts and suicide deaths in BD. The historical paucity of data on suicide attempts and suicide specific to BD has given way to a more robust and growing literature from which a diagnosis-specific perspective on risk can be informed.
Suicide rates vary greatly across studies, but when all studies are pooled and weighted by exposure years, the calculated rate is 164 per 100,000 person-years, approximately 10-fold greater than the general population. Newer studies have had the effect of lowering the estimated suicide rate in BD compared to similar earlier analyses (Tondo et al., 2003), and also tilt the balance toward large epidemiological datasets. There is no doubt, however, that suicide rates vary across the course of a person’s illness, therefore, our results should only be considered as an estimate of risk over an extended period of time, as opposed to during a specific high-risk period for which individual studies may provide more meaningful data. The fact that shorter clinical studies often conducted during or near an episode of high illness burden, yield higher suicide rates is not surprising. These results show that the overall rate of suicide in BD is high and imply that this high rate further escalates during certain periods in the course of illness.
Sex-specific data on suicide rates from seven studies (n = 60,876 BD subjects) identified a 1.7:1 ratio in men compared to women. This finding supports one of the aspects of a diagnosis-specific approach, namely, that the influence of a factor such as sex should ideally be considered in the context of the illness, rather than using more general data on sex differences in suicide rates, which tend to identify a larger ratio.
The proportion of all suicides accounted for by people with BD varied considerably by sample composition, with a range of 3–14%. The comparison of suicide rates in BD compared to unipolar depression or schizophrenia also showed divergent results which were very much influenced by sample composition, with epidemiological samples identifying higher rates in BD compared to unipolar depression, but the opposite in inpatient or prison inmate samples.
Methods of suicide were quite similar across epidemiological studies of BD suicide deaths, with the most common method being hanging, followed by self-poisoning and jumping. Clinical samples generally had higher proportions of death by self-poisoning, which suggests an opportunity for medication-related means restriction strategies to be highly relevant in clinical settings.
Many studies report suicide attempt rates in BD and newer data had not materially changed the identified rate of attempts. Higher rates were generally found in retrospective studies as compared to prospective designs. Self-poisoning was the most common method of suicide attempt, but the proportion of attempts via self-poisoning was much lower in Asian samples.
The vast majority of studies on the neurobiology of suicide attempts or suicide do not specifically examine BD. Despite this, there is a small but growing body of evidence, primarily in the field of genetics, which should be considered hypothesis-generating. There are only a handful of small genetic studies specific to suicide deaths in BD and no replicated findings; however, 16 genes have been reported to be differentially expressed in BD suicide vs non-suicide groups.
Several structural brain imaging studies identified correlates of suicide attempts in exclusively BD samples, but replication is not yet available. There were no significant replicated peripheral marker findings in a modest selection of studies of suicide attempts or death in BD. As the development of neurobiological models of suicide risk in general continues to be an area of active study, it is imperative that further data specific to BD be reported whenever possible, to allow for growth in this important but underdeveloped area.
Given the high rates of suicide attempts and suicide deaths in BD, having effective clinical interventions in the hands of the clinician is paramount. Most of the available literature has focused on lithium and anticonvulsants, for which there are numerous studies. While the methodological limitations of retrospective or non-randomized designs continue to impact the strength of the conclusions, the available data support the view that treatment with lithium or anticonvulsants significantly reduces the risk of suicide attempts and suicide deaths in people with BD. This conclusion is more cautious than prior publications (Cipriani et al., 2005; Wasserman et al., 2012), especially with regard to the putative anti-suicide effects of lithium. Our caution stems from the identification of remaining gaps in the extant data, especially with regard to prospective, randomized and head-to-head trials. In order to substantiate a claim of a direct anti-suicide effect in BD that is present with lithium but not other treatments, a high level of evidence is required, and at this stage, it is important to not only highlight the strong evidence that supports lower risk of suicide during lithium treatment compared to lithium discontinuation or placebo but also to identify the limits of retrospective studies to accurately compare anti-suicide effect of lithium vs other treatments, for which only minimal prospective data exist. The BD-specific literature on other treatments such as atypical antipsychotics, antidepressants, electroconvulsive therapy or psychotherapeutic interventions is very sparse, which is concerning given their frequent use, and argues for the importance of focusing on these in future studies.
There is also a dearth of clinical intervention studies on high suicide-risk BD patients. While the methodological challenges for such studies are quite significant, it is imperative that further efforts be made to launch multi-center clinical trials in high-risk scenarios. Furthermore, RCTs that are conducted during higher risk periods (e.g. bipolar depression, mixed states and post-hospitalization) should whenever possible incorporate comprehensive assessments of suicidal behavior specifically, as SI alone is an insufficient proxy.
Limitations
There are a number of important limitations that should be considered. First, as with any review of the literature, the results are dependent on the available data. Our reported pooled suicide rates included studies with a variety of different methodologies and study characteristics, which in the case of clinical studies likely to occur during higher risk periods of time in the course of illness. Non-hospital-based samples and those with BD type II are likely to have been less well represented. Furthermore, reporting bias must be considered, especially for neurobiological studies for which multiple genetic or non-genetic markers may have been examined within a given study, but only the positive findings reported. Second, while we attempted to provide some information on data collection throughout the review, the variability inherent in such a broad literature did not permit a full description of methodological variance for each study reviewed. This variability most critically relates to the reporting of suicide attempts and deaths, which vary in terms of method of ascertainment and classification system used (e.g. level of lethality of suicidal behavior; probable vs definite suicide definitions). This limitation is especially relevant when interpreting findings across countries, regions and time periods. Another related limitation is that suicidal behavior may be under-reported in clinical and epidemiological studies; therefore, the true rate of suicidal behavior—both attempts and deaths—may be underestimated in our review (Valtonen et al., 2006). Most studies from which either neurobiological or clinical data were available were not specifically designed with suicide attempts or deaths as the primary measure, so methodological heterogeneity is a significant issue in interpretation of results. Fourth, the reported data examined subjects diagnosed with BD, which cannot adequately address issues related to misdiagnosis or change in diagnosis over time, which can be especially common in epidemiological samples, and in relation to BD type II. Nevertheless, this issue impacts most BD studies and does not discount the value of the data when studying rigorously defined BD. Finally, much of the available literature is derived from North America, Europe and East Asia, and the generalizability of findings to other regions in the world remains a question for further consideration.
Conclusion
An expansive literature on suicide attempts and suicide deaths in BD permits increasingly accurate estimates of risk of suicide attempts and deaths. However, gaps do remain, pointing out the need for more diverse geographic representation in the BD suicide literature, as well as a focus on state-dependent suicide risk estimates. A growing wealth of data also exists on suicide attempts and suicide in BD, yet there is limited direct data on the neurobiological aspects. Even for clinical interventions, the robust data on lithium and anticonvulsants are in contrast with the paucity of data on other interventions, and the interpretation of extant literature is limited by insufficient controlled and comparative data. Given the known risks of inaction and benefits of action, it is imperative that mental health providers and researchers continue to make grand efforts to tackle this area of need.
Acknowledgements
The authors wish to thank the International Society for Bipolar Disorders executive and staff who assisted with the organization of the task force, and the students and researchers who assisted with the literature review and provided statistical work (Jessika Lenchyshyn, BSc, McMaster University, and Randy Rovinski, MSc, University of Toronto). Partial findings were presented during symposia at the 16th Annual Conference of the International Society for Bipolar Disorders.
Funding
Partial support for this project was provided by the Brenda Smith Bipolar Disorder Research Fund, Sunnybrook Health Sciences Centre and University of Toronto.
Footnotes
Declaration of interest
Dr Schaffer has in the past received speakers’ bureau honoraria, advisory panel funding and/or research grants from Bristol-Myers Squibb, Eli Lilly Canada, Lundbeck Canada, Otsuka, Pfizer Canada and Sunovion. Dr Moreno has received grant support or served as a speaker for Abbott, Aché, Lundbeck, EMS and Eurofarma. Dr Sinyor has received grant support from the American Foundation for Suicide Prevention, Physicians’ Services Incorporated (PSI) Foundation and the Brenda Smith Bipolar Disorder Research Fund. Dr Tondo has received funding from private donors to Aretaeus Association and to McLean Hospital. Dr Kessing has within the preceding 3 years been a consultant for Lundbeck and AstraZeneca. Dr Ha has no financial disclosures to report. Dr Isometsä has received honoraria from Servier for lecturing in educational meetings. Dr Turecki has no financial disclosures to report. Ms Reis has no financial disclosures to report. Dr Cassidy has no financial disclosures to report. Dr Azorin has received research support and has acted as consultant and/or served on a speaker’s bureau for Bristol-Myers Squibb, Janssen, Lilly, Lundbeck, Roche and Sanofi-Aventis. Dr Goldstein has received research support from NIMH, NIDA, NICHD, The Pittsburgh Foundation and Royalties from Guilford Press. Dr Weizman has no financial disclosures to report. Dr Beautrais has no financial disclosures to report. Dr Chou has no financial disclosures to report. Dr Diazgranados has no financial disclosures to report. Dr Levitt has received research grants from Janssen Ortho, AstraZeneca, Great West Life Insurance, and Eli Lilly Canada and has acted as a consultant for Janssen Ortho. Dr Zarate is listed as a coinventor on a patent application for the use of ketamine and its metabolites in major depression. He has assigned his rights in the patent to the US government but will share a percentage of any royalties that may be received by the government. Dr Rihmer has in the past received speakers’ bureau honoraria, advisory board funding or travel support from AstraZeneca, Janssen, Lundbeck, Lilly, Servier-EGIS, Richer and TEVA-Biogal. Dr Yatham has been a member of advisory boards and/or received research grants and/or been a speaker for AstraZeneca, DSP, Janssen, Lilly, GSK, Bristol-Myers Squibb, Lundbeck, Novartis, Servier, Sunovion and Pfizer.
References
- Ahearn EP, Chen P, Hertzberg M, et al. Suicide attempts in veterans with bipolar disorder during treatment with lithium, divalproex, and atypical antipsychotics. Journal of Affective Disorders. 2013;145:77–82. doi: 10.1016/j.jad.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizenberg D, Olmer A, Barak Y. Suicide attempts amongst elderly bipolar patients. Journal of Affective Disorders. 2006;91:91–94. doi: 10.1016/j.jad.2005.12.013. [DOI] [PubMed] [Google Scholar]
- Altamura AC, Dell’Osso B, Berlin HA, et al. Duration of untreated illness and suicide in bipolar disorder: A naturalistic study. European Archives of Psychiatry and Clinical Neuroscience. 2010;260:385–391. doi: 10.1007/s00406-009-0085-2. [DOI] [PubMed] [Google Scholar]
- Anderson D, Ardekani BA, Burdick KE, et al. Overlapping and distinct gray and white matter abnormalities in schizophrenia and bipolar I disorder. Bipolar Disorders. 2013;15:680–693. doi: 10.1111/bdi.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angst J, Sellaro R, Angst F. Long-term outcome and mortality of treated versus untreated bipolar and depressed patients: A preliminary report. International Journal of Psychiatry in Clinical Practice. 1998;2:115–119. doi: 10.3109/13651509809115343. [DOI] [PubMed] [Google Scholar]
- Apfelbaum S, Regalado P, Herman L, et al. Comorbidity between bipolar disorder and cluster B personality disorders as indicator of affective dysregulation and clinical severity. Actas Españolas de Psiquiatría. 2013;41:269–278. [PubMed] [Google Scholar]
- Arana A, Wentworth CE, Ayuso-Mateos JL, et al. Suicide-related events in patients treated with antiepileptic drugs. The New England Journal of Medicine. 2010;363:542–551. doi: 10.1056/NEJMoa0909801. [DOI] [PubMed] [Google Scholar]
- Azorin JM, Kaladjian A, Adida M, et al. Risk factors associated with lifetime suicide attempts in bipolar I patients: Findings from a French National Cohort. Comprehensive Psychiatry. 2009;50:115–120. doi: 10.1016/j.comppsych.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Baethge C, Cassidy F. Fighting on the side of life: A special issue on suicide in bipolar disorder. Bipolar Disorders. 2013;15:453–456. doi: 10.1111/bdi.12097. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Penn JV, Thomas CR, et al. Psychiatric disorders and suicide in the nation’s largest state prison system. Journal of the American Academy of Psychiatry and the Law. 2009;37:188–193. [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L. Lithium and suicidal risk. Bipolar Disorders. 2008;10:114–115. doi: 10.1111/j.1399-5618.2008.00550.x. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L. Suicidal risks during treatment of bipolar disorder patients with lithium versus anticonvulsants. Pharmacopsychiatry. 2009;42:72–75. doi: 10.1055/s-0028-1103291. [DOI] [PubMed] [Google Scholar]
- Barner-Rasmussen P. Suicide in psychiatric patients in Denmark, 1971–1981. II. Hospital utilization and risk groups. Acta Psychiatrica Scandinavica. 1986;73:449–455. doi: 10.1111/j.1600-0447.1986.tb02710.x. [DOI] [PubMed] [Google Scholar]
- Baumann B, Danos P, Diekmann S, et al. Tyrosine hydroxylase immunoreactivity in the locus coeruleus is reduced in depressed non-suicidal patients but normal in depressed suicide patients. European Archives of Psychiatry and Clinical Neuroscience. 1999;249:212–219. doi: 10.1007/s004060050089. [DOI] [PubMed] [Google Scholar]
- Bellivier F, Szoke A, Henry C, et al. Possible association between serotonin transporter gene polymorphism and violent suicidal behavior in mood disorders. Biological Psychiatry. 2000;48:319–322. doi: 10.1016/s0006-3223(00)00891-x. [DOI] [PubMed] [Google Scholar]
- Bellivier F, Yon L, Luquiens A, et al. Suicidal attempts in bipolar disorder: Results from an observational study (EMBLEM) Bipolar Disorders. 2011;13:377–386. doi: 10.1111/j.1399-5618.2011.00926.x. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Radaelli D, Poletti S, et al. Opposite effects of suicidality and lithium on gray matter volumes in bipolar depression. Journal of Affective Disorders. 2011;135:139–147. doi: 10.1016/j.jad.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Berrettini WH, Nurnberger JI, Jr, Narrow W, et al. Cerebrospinal fluid studies of bipolar patients with and without a history of suicide attempts. ANNALS of the New York Academy of Sciences. 1986;487:197–201. doi: 10.1111/j.1749-6632.1986.tb27899.x. [DOI] [PubMed] [Google Scholar]
- Black DW, Winokur G, Nasrallah A. Effect of psychosis on suicide risk in 1,593 patients with unipolar and bipolar affective disorders. The American Journal of Psychiatry. 1988;145:849–852. doi: 10.1176/ajp.145.7.849. [DOI] [PubMed] [Google Scholar]
- Bocchetta A, Ardau R, Burrai C, et al. Suicidal behavior on and off lithium prophylaxis in a group of patients with prior suicide attempts. Journal of Clinical Psychopharmacology. 1998;18:384–389. doi: 10.1097/00004714-199810000-00006. [DOI] [PubMed] [Google Scholar]
- Brodersen A, Licht RW, Vestergaard P, et al. Sixteen-year mortality in patients with affective disorder commenced on lithium. The British Journal of Psychiatry. 2000;176:429–433. doi: 10.1192/bjp.176.5.429. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Campos SB, Miranda DM, Souza BR, et al. Association of polymorphisms of the tryptophan hydroxylase 2 gene with risk for bipolar disorder or suicidal behavior. Journal of Psychiatric Research. 2010;44:271–274. doi: 10.1016/j.jpsychires.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Chen YY, Lee MB, Chang CM, et al. Methods of suicide in different psychiatric diagnostic groups. Journal of Affective Disorders. 2009;118:196–200. doi: 10.1016/j.jad.2009.05.020. [DOI] [PubMed] [Google Scholar]
- Chesin M, Stanley B. Risk assessment and psychosocial interventions for suicidal patients. Bipolar Disorders. 2013;15:584–593. doi: 10.1111/bdi.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: Updated systematic review and meta-analysis. British Medical Journal. 2013;346:F3646. doi: 10.1136/bmj.f3646. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Pretty H, Hawton K, et al. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: A systematic review of randomized trials. The American Journal of Psychiatry. 2005;162:1805–1819. doi: 10.1176/appi.ajp.162.10.1805. [DOI] [PubMed] [Google Scholar]
- Clements C, Morriss R, Jones S, et al. Suicide in bipolar disorder in a national English sample, 1996–2009: Frequency, trends and characteristics. Psychological Medicine. 2013;43:2593–2602. doi: 10.1017/S0033291713000329. [DOI] [PubMed] [Google Scholar]
- Collins JC, McFarland BH. Divalproex, lithium and suicide among Medicaid patients with bipolar disorder. Journal of Affective Disorders. 2008;107:23–28. doi: 10.1016/j.jad.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Crump C, Sundquist K, Winkleby MA, et al. Comorbidities and mortality in bipolar disorder: A Swedish national cohort study. JAMA Psychiatry. 2013;70:931–939. doi: 10.1001/jamapsychiatry.2013.1394. [DOI] [PubMed] [Google Scholar]
- D’Ambrosio V, Salvi V, Bogetto F, et al. Serum lipids, metabolic syndrome and lifetime suicide attempts in patients with bipolar disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2012;37:136–140. doi: 10.1016/j.pnpbp.2011.12.009. [DOI] [PubMed] [Google Scholar]
- De Abreu LN, Nery FG, Harkavy-Friedman JM, et al. Suicide attempts are associated with worse quality of life in patients with bipolar disorder type I. Comprehensive Psychiatry. 2012;53:125–129. doi: 10.1016/j.comppsych.2011.03.003. [DOI] [PubMed] [Google Scholar]
- De Luca V, Hlousek D, Likhodi O, et al. The interaction between TPH2 promoter haplotypes and clinical-demographic risk factors in suicide victims with major psychoses. Genes, Brain, and Behavior. 2006;5:107–110. doi: 10.1111/j.1601-183X.2005.00182.x. [DOI] [PubMed] [Google Scholar]
- De Luca V, Likhodi O, Kennedy JL, et al. Differential expression and parent-of-origin effect of the 5-HT2A receptor gene C102T polymorphism: Analysis of suicidality in schizophrenia and bipolar disorder. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2007;144:370–374. doi: 10.1002/ajmg.b.30458. [DOI] [PubMed] [Google Scholar]
- De Luca V, Tharmalingam S, King N, et al. Association study of a novel functional polymorphism of the serotonin transporter gene in bipolar disorder and suicidal behaviour. Psychopharmacology. 2005a;182:128–131. doi: 10.1007/s00213-005-0046-z. [DOI] [PubMed] [Google Scholar]
- De Luca V, Tharmalingam S, Sicard T, et al. Gene-gene interaction between MAOA and COMT in suicidal behavior. Neuroscience Letters. 2005b;383:151–154. doi: 10.1016/j.neulet.2005.04.001. [DOI] [PubMed] [Google Scholar]
- De Luca V, Viggiano E, Dhoot R, et al. Methylation and QTDT analysis of the 5-HT2A receptor 102C allele: Analysis of suicidality in major psychosis. Journal of Psychiatric Research. 2009;43:532–537. doi: 10.1016/j.jpsychires.2008.07.007. [DOI] [PubMed] [Google Scholar]
- Dennehy EB, Marangell LB, Allen MH, et al. Suicide and suicide attempts in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Journal of Affective Disorders. 2011;133:423–427. doi: 10.1016/j.jad.2011.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dervic K, Carballo JJ, Baca-Garcia E, et al. Moral or religious objections to suicide may protect against suicidal behavior in bipolar disorder. Journal of Clinical Psychiatry. 2011;72:1390–1396. doi: 10.4088/JCP.09m05910gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingman CW, McGlashan TH. Characteristics of patients with serious suicidal intentions who ultimately commit suicide. Hospital & Community Psychiatry. 1988;39:295–299. doi: 10.1176/ps.39.3.295. [DOI] [PubMed] [Google Scholar]
- Dowlatshahi D, MacQueen GM, Wang JF, et al. G Protein-coupled cyclic AMP signaling in postmortem brain of subjects with mood disorders: Effects of diagnosis, suicide, and treatment at the time of death. Journal of Neurochemistry. 1999;73:1121–1126. doi: 10.1046/j.1471-4159.1999.0731121.x. [DOI] [PubMed] [Google Scholar]
- Dracheva S, Patel N, Woo DA, et al. Increased serotonin 2C receptor mRNA editing: A possible risk factor for suicide. Molecular Psychiatry. 2008;13:1001–1010. doi: 10.1038/sj.mp.4002081. [DOI] [PubMed] [Google Scholar]
- Dutta R, Boydell J, Kennedy N, et al. Suicide and other causes of mortality in bipolar disorder: A longitudinal study. Psychological Medicine. 2007;37:839–847. doi: 10.1017/S0033291707000347. [DOI] [PubMed] [Google Scholar]
- Evans SJ, Prossin AR, Harrington GJ, et al. Fats and factors: Lipid profiles associate with personality factors and suicidal history in bipolar subjects. PLoS ONE. 2012;7:e29297. doi: 10.1371/journal.pone.0029297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Wolf A, Geddes JR. Suicide in prisoners with bipolar disorder and other psychiatric disorders: A systematic review. Bipolar Disorders. 2013;15:491–495. doi: 10.1111/bdi.12053. [DOI] [PubMed] [Google Scholar]
- Feldcamp LA, Souza RP, Romano-Silva M, et al. Reduced prefrontal cortex DARPP-32 mRNA in completed suicide victims with schizophrenia. Schizophrenia Research. 2008;103:192–200. doi: 10.1016/j.schres.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Ferrer P, Ballarin E, Sabate M, et al. Antiepileptic drugs and suicide: A systematic review of adverse effects. Neuroepidemiology. 2014;42:107–120. doi: 10.1159/000356807. [DOI] [PubMed] [Google Scholar]
- Fillman SG, Sinclair D, Fung SJ, et al. Markers of inflammation and stress distinguish subsets of individuals with schizophrenia and bipolar disorder. Translational Psychiatry. 2014;4:e365. doi: 10.1038/tp.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finseth PI, Sonderby IE, Djurovic S, et al. Association analysis between suicidal behaviour and candidate genes of bipolar disorder and schizophrenia. Journal of Affective Disorders. 2014;163:110–114. doi: 10.1016/j.jad.2013.12.018. [DOI] [PubMed] [Google Scholar]
- Friis S, Hauff E, Island TK, et al. The Ulleval acute ward follow-up study: a personal 7-year follow-up of patients with functional psychosis admitted to the acute ward of a catchment area. Psychopathology. 1991;24:316–327. doi: 10.1159/000284732. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hur K, Brown CH, et al. Relationship between antiepileptic drugs and suicide attempts in patients with bipolar disorder. Archives of General Psychiatry. 2009;66:1354–1360. doi: 10.1001/archgenpsychiatry.2009.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons RD, Hur K, Brown CH, et al. Gabapentin and suicide attempts. Pharmacoepidemiology and Drug Safety. 2010;19:1241–1247. doi: 10.1002/pds.2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladstone GL, Mitchell PB, Parker G, et al. Indicators of suicide over 10 years in a specialist mood disorders unit sample. The Journal of Clinical Psychiatry. 2001;62:945–951. doi: 10.4088/jcp.v62n1205. [DOI] [PubMed] [Google Scholar]
- Gonda X, Pompili M, Serafini G, et al. Suicidal behavior in bipolar disorder: Epidemiology, characteristics and major risk factors. Journal of Affective Disorders. 2012;143:16–26. doi: 10.1016/j.jad.2012.04.041. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Pinto A, Barbeito S, Alonso M, et al. Poor long-term prognosis in mixed bipolar patients: 10-year outcomes in the Vitoria prospective naturalistic study in Spain. Journal of Clinical Psychiatry. 2011;72:671–676. doi: 10.4088/JCP.09m05483yel. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Fireman B, Simon GE, et al. Suicide risk in bipolar disorder during treatment with lithium and divalproex. The Journal of the American Medical Association. 2003;290:1467–1473. doi: 10.1001/jama.290.11.1467. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Evidence-based guidelines for treating bipolar disorder: Revised second edition—Recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology. 2009;23:346–388. doi: 10.1177/0269881109102919. [DOI] [PubMed] [Google Scholar]
- Gos T, Gunther K, Bielau H, et al. Suicide and depression in the quantitative analysis of glutamic acid decarboxylase-Immunoreactive neuropil. Journal of Affective Disorder. 2009;113:45–55. doi: 10.1016/j.jad.2008.04.021. [DOI] [PubMed] [Google Scholar]
- Grunze H, Vieta E, Goodwin GM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: Update 2009 on the treatment of acute mania. The World Journal of Biological Psychiatry. 2009;10:85–116. doi: 10.1080/15622970902823202. [DOI] [PubMed] [Google Scholar]
- Grunze H, Vieta E, Goodwin GM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: Update 2010 on the treatment of acute bipolar depression. The World Journal of Biological Psychiatry. 2010;11:81–109. doi: 10.3109/15622970903555881. [DOI] [PubMed] [Google Scholar]
- Halcomb ME, Gould TD, Grahame NJ. Lithium, but not valproate, reduces impulsive choice in the delay-discounting task in mice. Neuropsychopharmacology. 2013;38:1937–1944. doi: 10.1038/npp.2013.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser M, Galling B, Correll CU. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: A systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disorders. 2013;15:507–523. doi: 10.1111/bdi.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, et al. Suicide and attempted suicide in bipolar disorder: A systematic review of risk factors. Journal of Clinical Psychiatry. 2005;66:693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- Hoyer EH, Mortensen PB, Olesen AV. Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. The British Journal of Psychiatry. 2000;176:76–82. doi: 10.1192/bjp.176.1.76. [DOI] [PubMed] [Google Scholar]
- Hunt IM, Kapur N, Robinson J, et al. Suicide within 12months of mental health service contact in different age and diagnostic groups: National clinical survey. The British Journal of Psychiatry. 2006;188:135–142. doi: 10.1192/bjp.188.2.135. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert AS, Ignacio RV, et al. Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry. 2010;67:1152–1158. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- Isometsä ET, Henriksson MM, Aro HM, et al. Suicide in bipolar disorder in Finland. The American Journal of Psychiatry. 1994;151:1020–1024. doi: 10.1176/ajp.151.7.1020. [DOI] [PubMed] [Google Scholar]
- Jimenez E, Arias B, Mitjans M, et al. Genetic variability at IMPA2, INPP1 and GSK3beta increases the risk of suicidal behavior in bipolar patients. European Neuropsychopharmacology. 2013;23:1452–1462. doi: 10.1016/j.euroneuro.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Kalkman HO. Circumstantial evidence for a role of glutamine-synthetase in suicide. Medical Hypotheses. 2011;76:905–907. doi: 10.1016/j.mehy.2011.03.005. [DOI] [PubMed] [Google Scholar]
- Kallner G, Lindelius R, Petterson U, et al. Mortality in 497 patients with affective disorders attending a lithium clinic or after having left it. Pharmacopsychiatry. 2000;33:8–13. doi: 10.1055/s-2000-7965. [DOI] [PubMed] [Google Scholar]
- Kamali M, Saunders EF, Prossin AR, et al. Associations between suicide attempts and elevated bedtime salivary cortisol levels in bipolar disorder. Journal of Affective Disorders. 2012;136:350–358. doi: 10.1016/j.jad.2011.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karch DL, Barker L, Strine TW. Race/ethnicity, substance abuse, and mental illness among suicide victims in 13 US states: 2004 data from the National Violent Death Reporting System. Injury Prevention. 2006;12:ii22–ii27. doi: 10.1136/ip.2006.013557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keks NA, Hill C, Sundram S, et al. Evaluation of treatment in 35 cases of bipolar suicide. Australian & New Zealand Journal of Psychiatry. 2009;43:503–508. doi: 10.1080/00048670902873680. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Munk-Jorgensen P. Does type of first contact in depressive and bipolar disorders predict subsequent hospitalisation and risk of suicide? Journal of Affective Disorders. 2004;83:65–71. doi: 10.1016/j.jad.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Søndergård L, Kvist K, et al. Suicide risk in patients treated with lithium. Archives of General Psychiatry. 2005;62:860–866. doi: 10.1001/archpsyc.62.8.860. [DOI] [PubMed] [Google Scholar]
- Khan A, Faucett J, Morrison S, et al. Comparative mortality risk in adult patients with schizophrenia, depression, bipolar disorder, anxiety disorders, and attention-deficit/hyperactivity disorder participating in psychopharmacology clinical trials. JAMA Psychiatry. 2013;70:1091–1099. doi: 10.1001/jamapsychiatry.2013.149. [DOI] [PubMed] [Google Scholar]
- Kim B, Kim CY, Hong JP, et al. Brain-derived neurotrophic factor Val/Met polymorphism and bipolar disorder. Association of the Met allele with suicidal behavior of bipolar patients. Neuropsychobiology. 2008;58:97–103. doi: 10.1159/000162356. [DOI] [PubMed] [Google Scholar]
- Kim S, Choi KH, Baykiz AF, et al. Suicide candidate genes associated with bipolar disorder and schizophrenia: An exploratory gene expression profiling analysis of post-mortem prefrontal cortex. BMC Genomics. 2007;8:413. doi: 10.1186/1471-2164-8-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YK, Lee HJ, Kim JY, et al. Low serum cholesterol is correlated to suicidality in a Korean sample. Acta Psychiatrica Scandinavica. 2002;105:141–148. doi: 10.1034/j.1600-0447.2002.10352.x. [DOI] [PubMed] [Google Scholar]
- Kleindienst N, Greil W. Differential efficacy of lithium and carbamazepine in the prophylaxis of bipolar disorder: Results of the MAP study. Neuropsychobiology. 2000;42(Suppl 1):2–10. doi: 10.1159/000054844. [DOI] [PubMed] [Google Scholar]
- Koek RJ, Yerevanian BI, Mintz J. Subtypes of antipsychotics and suicidal behavior in bipolar disorder. Journal of Affective Disorders. 2012;143:27–33. doi: 10.1016/j.jad.2012.05.053. [DOI] [PubMed] [Google Scholar]
- Koukopoulos A, Reginaldi D, Minnai G, et al. The long term prophylaxis of affective disorders. In: Gessa G, Fratta W, Pani L, editors. Depression and Mania: From Neurobiology to Treatment. Raven Press; New York: 1995. pp. 127–147. [PubMed] [Google Scholar]
- Lan MJ, Chhetry BT, Oquendo MA, et al. Cortical thickness differences between bipolar depression and major depressive disorder. Bipolar Disorders. 2014;16:378–388. doi: 10.1111/bdi.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le-Niculescu H, Levey DF, Ayalew M, et al. Discovery and validation of blood biomarkers for suicidality. Molecular Psychiatry. 2013;18:1249–1264. doi: 10.1038/mp.2013.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Solomon DA, Li C, et al. Antiepileptic drugs for bipolar disorder and the risk of suicidal behavior: A 30-year observational study. The American Journal of Psychiatry. 2012;169:285–291. doi: 10.1176/appi.ajp.2011.11060948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leszczynska-Rodziewicz A, Szczepankiewicz A, Narozna B, et al. Possible association between haplotypes of the FKBP5 gene and suicidal bipolar disorder, but not with melancholic depression and psychotic features, in the course of bipolar disorder. Journal of Neuropsychiatric Disease and Treatment. 2014;10:243–248. doi: 10.2147/NDT.S54538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez VA, Detera-Wadleigh S, Cardona I, et al. Nested association between genetic variation in tryptophan hydroxylase II, bipolar affective disorder, and suicide attempts. Biological Psychiatry. 2007;61:181–186. doi: 10.1016/j.biopsych.2006.03.028. [DOI] [PubMed] [Google Scholar]
- Mahon K, Burdick KE, Wu J, et al. Relationship between suicidality and impulsivity in bipolar I disorder: A diffusion tensor imaging study. Bipolar Disorders. 2012;14:80–89. doi: 10.1111/j.1399-5618.2012.00984.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi GS, Bargh DM, Kuiper S, et al. Modeling bipolar disorder suicidality. Bipolar Disorders. 2013;15:559–574. doi: 10.1111/bdi.12093. [DOI] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, de Moraes PH, et al. The 5-HTTLPR polymorphism, impulsivity and suicide behavior in euthymic bipolar patients. Journal of Affective Disorders. 2011;133:221–226. doi: 10.1016/j.jad.2011.03.051. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Currier DM. Stress, genetics and epigenetic effects on the neurobiology of suicidal behavior and depression. European Psychiatry. 2010;25:268–271. doi: 10.1016/j.eurpsy.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marangell LB, Dennehy EB, Wisniewski SR, et al. Case-control analyses of the impact of pharmacotherapy on prospectively observed suicide attempts and completed suicides in bipolar disorder: Findings from STEP-BD. Journal of Clinical Psychiatry. 2008;69:916–922. doi: 10.4088/jcp.v69n0605. [DOI] [PubMed] [Google Scholar]
- Marcus SM, Lu B, Lim S, et al. Suicide attempts in patients with bipolar disorder tend to precede, not follow, initiation of antiepileptic drugs. Journal of Clinical Psychiatry. 2013;74:630–631. doi: 10.4088/JCP.12l08334. [DOI] [PubMed] [Google Scholar]
- Martin RL, Cloninger CR, Guze SB, et al. Mortality in a follow-up of 500 psychiatric outpatients. II. Cause-specific mortality. Archives of General Psychiatry. 1985;42:58–66. doi: 10.1001/archpsyc.1985.01790240060006. [DOI] [PubMed] [Google Scholar]
- Mathews DC, Richards EM, Niciu MJ, et al. Neurobiological aspects of suicide and suicide attempts in bipolar disorder. Translational Neuroscience. 2013;4:203–216. doi: 10.2478/s13380-013-0120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo K, Nielsen N, Nicoletti MA, et al. Anterior genu corpus callosum and impulsivity in suicidal patients with bipolar disorder. Neuroscience Letters. 2010;469:75–80. doi: 10.1016/j.neulet.2009.11.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He JP, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archives of General Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Monfrim X, Gazal M, De leon PB, et al. Immune dysfunction in bipolar disorder and suicide risk: Is there an association between peripheral corticotropin-releasing hormone and interleukin-1β? Bipolar Disorders. 2014;16:741–747. doi: 10.1111/bdi.12214. [DOI] [PubMed] [Google Scholar]
- Morrison JR. Suicide in a psychiatric practice population. Journal of Clinical Psychiatry. 1982;43:348–352. [PubMed] [Google Scholar]
- Mustak MS, Hegde ML, Dinesh A, et al. Evidence of altered DNA integrity in the brain regions of suicidal victims of Bipolar Depression. Indian Journal of Psychiatry. 2010;52:220–228. doi: 10.4103/0019-5545.70974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nery-Fernandes F, Rocha MV, Jackowski A, et al. Reduced posterior corpus callosum area in suicidal and non-suicidal patients with bipolar disorder. Journal of Affective Disorders. 2012;142:150–155. doi: 10.1016/j.jad.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Nery FG, Miranda-Scippa A, Nery-Fernandes F, et al. Prevalence and clinical correlates of alcohol use disorders among bipolar disorder patients: Results from the Brazilian Bipolar Research Network. Comprehensive Psychiatry. 2014;55:1116–1121. doi: 10.1016/j.comppsych.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Neves FS, Malloy-Diniz LF, Romano-Silva MA, et al. Is the serotonin transporter polymorphism (5-HTTLPR) a potential marker for suicidal behavior in bipolar disorder patients? Journal of Affective Disorders. 2010;125:98–102. doi: 10.1016/j.jad.2009.12.026. [DOI] [PubMed] [Google Scholar]
- Neves FS, Silveira G, Romano-Silva MA, et al. Is the 5-HTTLPR polymorphism associated with bipolar disorder or with suicidal behavior of bipolar disorder patients? American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2008;147:114–116. doi: 10.1002/ajmg.b.30563. [DOI] [PubMed] [Google Scholar]
- Newman SC, Bland RC. Suicide risk varies by subtype of affective disorder. Acta Psychiatr Scandinavica. 1991;83:420–426. doi: 10.1111/j.1600-0447.1991.tb05568.x. [DOI] [PubMed] [Google Scholar]
- Nielsen J, Kane JM, Correll CU. Real-world effectiveness of clozapine in patients with bipolar disorder: Results from a 2-year mirror-image study. Bipolar Disorders. 2012;14:863–869. doi: 10.1111/bdi.12018. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Archives of General Psychiatry. 2011;68:1058–1064. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: A review and meta-analysis of the evidence. Bipolar Disorders. 2010;12:1–9. doi: 10.1111/j.1399-5618.2009.00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Carballo JJ, Rajouria N, et al. Are high-lethality suicide attempters with bipolar disorder a distinct phenotype? Archives of Suicide Research. 2009;13:247–256. doi: 10.1080/13811110903044385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy HC, Currier D, et al. Treatment of suicide attempters with bipolar disorder: A randomized clinical trial comparing lithium and valproate in the prevention of suicidal behavior. The American Journal of Psychiatry. 2011;168:1050–1056. doi: 10.1176/appi.ajp.2011.11010163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn D, Levy G, Nazareth I, et al. Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophrenia Research. 2008;99:134–138. doi: 10.1016/j.schres.2007.11.025. [DOI] [PubMed] [Google Scholar]
- Ösby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Archives of General Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- Pandey GN, Dwivedi Y. What can post-mortem studies tell us about the pathoetiology of suicide? Future Neurology. 2010;5:701–720. doi: 10.2217/fnl.10.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Yi KK, Na R, et al. No association between serum cholesterol and death by suicide in patients with schizophrenia, bipolar affective disorder, or major depressive disorder. Behavioral and Brain Functions. 2013;9:45. doi: 10.1186/1744-9081-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis RH, Ruderfer D, Maussion G, et al. Bipolar disorder and a history of suicide attempts with a duplication in 5HTR1A. The American Journal of Psychiatry. 2012;169:1213–1214. doi: 10.1176/appi.ajp.2012.12050592. [DOI] [PubMed] [Google Scholar]
- Pinto C, Souza RP, Lioult D, et al. Parent of origin effect and allelic expression imbalance of the serotonin transporter in bipolar disorder and suicidal behaviour. European Archives of Psychiatry and Clinical Neuroscience. 2011;261:533–538. doi: 10.1007/s00406-011-0192-8. [DOI] [PubMed] [Google Scholar]
- Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: A systematic review of the literature. Bipolar Disorders. 2013;15:457–490. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- Pompili M, Innamorati M, Mann JJ, et al. Periventricular white matter hyperintensities as predictors of suicide attempts in bipolar disorders and unipolar depression. Progress in NeuroPsychopharmacology & Biological Psychiatry. 2008;32:1501–1507. doi: 10.1016/j.pnpbp.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Raja M, Azzoni A, Koukopoulos AE. Psychopharmacological treatment before suicide attempt among patients admitted to a psychiatric intensive care unit. Journal of Affective Disorders. 2009;113:37–44. doi: 10.1016/j.jad.2008.04.024. [DOI] [PubMed] [Google Scholar]
- Redden L, Pritchett Y, Robieson W, et al. Suicidality and divalproex sodium: Analysis of controlled studies in multiple indications. Annals of General Psychiatry. 2011;10:1. doi: 10.1186/1744-859X-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid S. Current use of antiepileptic drugs is associated with an increased risk of suicidality in people with depression but not in people with epilepsy or bipolar disorder. Evidence-Based Mental Health. 2011;14:3. doi: 10.1136/ebmh.14.1.3. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Barsi J, Arato M, et al. Suicide in subtypes of primary major depression. Journal of Affective Disorders. 1990;18:221–225. doi: 10.1016/0165-0327(90)90039-b. [DOI] [PubMed] [Google Scholar]
- Rucci P, Frank E, Kostelnik B, et al. Suicide attempts in patients with bipolar I disorder during acute and maintenance phases of intensive treatment with pharmacotherapy and adjunctive psychotherapy. The American Journal of Psychiatry. 2002;159:1160–1164. doi: 10.1176/appi.ajp.159.7.1160. [DOI] [PubMed] [Google Scholar]
- Ruengorn C, Sanichwankul K, Niwatananun W, et al. A risk-scoring scheme for suicide attempts among patients with bipolar disorder in a Thai patient cohort. Psychology Research and Behavior Management. 2012;5:37–45. doi: 10.2147/PRBM.S30878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu V, Jon DI, Cho HS, et al. Initial depressive episodes affect the risk of suicide attempts in Korean patients with bipolar disorder. Yonsei Medical Journal. 2010;51:641–647. doi: 10.3349/ymj.2010.51.5.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Goldstein BI, Morcillo C, et al. Course of comorbid anxiety disorders among adults with bipolar disorder in the U.S. population. Journal of Psychiatric Research. 2012;46:865–872. doi: 10.1016/j.jpsychires.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sani G, Tondo L, Koukopoulos A, et al. Suicide in a large population of former psychiatric inpatients. Psychiatry and Clinical Neurosciences. 2011;65:286–295. doi: 10.1111/j.1440-1819.2011.02205.x. [DOI] [PubMed] [Google Scholar]
- Saunders KE, Hawton K. Clinical assessment and crisis intervention for the suicidal bipolar disorder patient. Bipolar Disorders. 2013;15:575–583. doi: 10.1111/bdi.12065. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Sinyor M, Howlett A, et al. Suicide by overdose in a bipolar disorder cohort; 5th Biennial conference of the international society for bipolar disorders; Istanbul, Turkey. Mar, 2012. pp. 14–17. [Google Scholar]
- Schaffer A, Sinyor M, Reis C, et al. Suicide in bipolar disorder: Characteristics and subgroups. Bipolar Disorders. 2014;16:732–740. doi: 10.1111/bdi.12219. [DOI] [PubMed] [Google Scholar]
- Schou M, Weeke A. Did manic-depressive patients who committed suicide receive prophylactic or continuation treatment at the time? The British Journal of Psychiatry. 1988;153:324–327. doi: 10.1192/bjp.153.3.324. [DOI] [PubMed] [Google Scholar]
- Shabani A, Teimurinejad S, Kokar S, et al. Suicide risk factors in Iranian patients with bipolar disorder: A 21-month follow-up from BDPF study. Iranian Journal of Psychiatry and Behavioral Sciences. 2013;7:16–23. [PMC free article] [PubMed] [Google Scholar]
- Sharma R, Markar HR. Mortality in affective disorder. Journal of Affective Disorders. 1994;31:91–96. doi: 10.1016/0165-0327(94)90112-0. [DOI] [PubMed] [Google Scholar]
- Sher L, Carballo JJ, Grunebaum MF, et al. A prospective study of the association of cerebrospinal fluid monoamine metabolite levels with lethality of suicide attempts in patients with bipolar disorder. Bipolar Disorders. 2006;8:543–550. doi: 10.1111/j.1399-5618.2006.00319.x. [DOI] [PubMed] [Google Scholar]
- Sher L, Grunebaum MF, Sullivan GM, et al. Testosterone levels in suicide attempters with bipolar disorder. Journal of Psychiatric Research. 2012;46:1267–1271. doi: 10.1016/j.jpsychires.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Hunkeler E, Fireman B, et al. Risk of suicide attempt and suicide death in patients treated for bipolar disorder. Bipolar Disorders. 2007;9:526–530. doi: 10.1111/j.1399-5618.2007.00408.x. [DOI] [PubMed] [Google Scholar]
- Simon RI, Hales RE. The American Psychiatric Publishing Textbook of Suicide Assessment and Management. American Psychiatric Publishing; Arlington, VA: 2006. [Google Scholar]
- Singhal A, Ross J, Seminog O, et al. Risk of self-harm and suicide in people with specific psychiatric and physical disorders: Comparisons between disorders using English national record linkage. Journal of the Royal Society of Medicine. 2014;107:194–204. doi: 10.1177/0141076814522033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith EG, Søndergård L, Lopez AG, et al. Association between consistent purchase of anticonvulsants or lithium and suicide risk: A longitudinal cohort study from Denmark, 1995–2001. Journal of Affective Disorders. 2009;117:162–167. doi: 10.1016/j.jad.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Søndergård L, Lopez AG, Andersen PK, et al. Mood-stabilizing pharmacological treatment in bipolar disorders and risk of suicide. Bipolar Disorders. 2008;10:87–94. doi: 10.1111/j.1399-5618.2008.00464.x. [DOI] [PubMed] [Google Scholar]
- Song JY, Yu HY, Kim SH, et al. Assessment of risk factors related to suicide attempts in patients with bipolar disorder. The Journal of Nervous and Mental Disease. 2012;200:978–984. doi: 10.1097/NMD.0b013e3182718a07. [DOI] [PubMed] [Google Scholar]
- Souery D, Van Gestel S, Massat I, et al. Tryptophan hydroxylase polymorphism and suicidality in unipolar and bipolar affective disorders: A multicenter association study. Biological Psychiatry. 2001;49:405–409. doi: 10.1016/s0006-3223(00)01043-x. [DOI] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, da Silva Magalhaes PV, et al. Extreme attributions predict suicidal ideation and suicide attempts in bipolar disorder: Prospective data from STEP-BD. World Psychiatry. 2014;13:95–96. doi: 10.1002/wps.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley M, Stanley B. Biochemical studies in suicide victims: Current findings and future implications. Suicide and Life-Threatening Behavior. 1989;19:30–42. doi: 10.1111/j.1943-278x.1989.tb00364.x. [DOI] [PubMed] [Google Scholar]
- Storosum JG, Wohlfarth T, Gispen-de Wied CC, et al. Suicide risk in placebo-controlled trials of treatment for acute manic episode and prevention of manic-depressive episode. The American Journal of Psychiatry. 2005;162:799–802. doi: 10.1176/appi.ajp.162.4.799. [DOI] [PubMed] [Google Scholar]
- Suttajit S, Paholpak S, Choovanicvong S, et al. Correlates of current suicide risk among Thai patients with bipolar I disorder: Findings from the Thai Bipolar Disorder Registry. Neuropsychiatric Disease and Treatment. 2013;9:1751–1757. doi: 10.2147/NDT.S52519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takizawa T. Suicide due to mental diseases based on the Vital Statistics Survey Death Form. Nihon Koshu Eisei Zasshi. 2012;59:399–406. [PubMed] [Google Scholar]
- Thibodeau MA, Welch PG, Sareen J, et al. Anxiety disorders are independently associated with suicide ideation and attempts: Propensity score matching in two epidemiological samples. Depress Anxiety. 2013;30:947–954. doi: 10.1002/da.22203. [DOI] [PubMed] [Google Scholar]
- Thies-Flechtner K, Muller-Oerlinghausen B, Seibert W, et al. Effect of prophylactic treatment on suicide risk in patients with major affective disorders. Data from a randomized prospective trial. Pharmacopsychiatry. 1996;29:103–107. doi: 10.1055/s-2007-979553. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Haglund A, Karanti A, et al. Attempted suicide in bipolar disorder: Risk factors in a cohort of 6086 patients. PLoS ONE. 2014;9:E94097. doi: 10.1371/journal.pone.0094097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tochigi M, Iwamoto K, Bundo M, et al. Gene expression profiling of major depression and suicide in the prefrontal cortex of postmortem brains. Neuroscience Research. 2008;60:184–191. doi: 10.1016/j.neures.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Tondo L, Isacsson G, Baldessarini R. Suicidal behaviour in bipolar disorder: Risk and prevention. CNS Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- Tondo L, Lepri B, Baldessarini RJ. Suicidal risks among 2826 Sardinian major affective disorder patients. Acta Psychiatrica Scandinavica. 2007;116:419–428. doi: 10.1111/j.1600-0447.2007.01066.x. with additional written communication from Tondo L. [DOI] [PubMed] [Google Scholar]
- Tsai SJ, Hong CJ, Wang YC. Tryptophan hydroxylase gene polymorphism (A218C) and suicidal behaviors. Neuroreport. 1999a;10:3773–3775. doi: 10.1097/00001756-199912160-00010. [DOI] [PubMed] [Google Scholar]
- Tsai SY, Lee JC, Chen CC. Characteristics and psychosocial problems of patients with bipolar disorder at high risk for suicide attempt. Journal of Affective Disorders. 1999b;52:145–152. doi: 10.1016/s0165-0327(98)00066-4. [DOI] [PubMed] [Google Scholar]
- Turecki G, Ernst C, Jollant F, et al. The neurodevelopmental origins of suicidal behavior. Trends in Neurosciences. 2012;35:14–23. doi: 10.1016/j.tins.2011.11.008. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services Suicidal behavior and ideation and antiepileptic drugs. 2009 Available at: www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm100190.htm (accessed 30 May 2014)
- Valtonen HM, Suominen K, Mantere O, et al. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disorders. 2006;8:576–585. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- Van Heeringen K, Mann JJ. The neurobiology of suicide. The Lancet. 2014;1:63–72. doi: 10.1016/S2215-0366(14)70220-2. [DOI] [PubMed] [Google Scholar]
- Vieta E, Langosch JM, Figueira ML, et al. Clinical management and burden of bipolar disorder: Results from a multinational longitudinal study (WAVE-bd) The International Journal of Neuropsychopharmacology. 2013;16:1719–1732. doi: 10.1017/S1461145713000278. [DOI] [PubMed] [Google Scholar]
- Vuksan-Cusa B, Marcinko D, Nad S, et al. Differences in cholesterol and metabolic syndrome between bipolar disorder men with and without suicide attempts. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2009;33:109–112. doi: 10.1016/j.pnpbp.2008.10.017. [DOI] [PubMed] [Google Scholar]
- Wasserman D, Rihmer Z, Rujescu D, et al. The European Psychiatric Association (EPA) guidance on suicide treatment and prevention. European Psychiatry. 2012;27:129–141. doi: 10.1016/j.eurpsy.2011.06.003. [DOI] [PubMed] [Google Scholar]
- Weeke A, Vaeth M. Excess mortality of bipolar and unipolar manic-depressive patients. Journal of Affective Disorders. 1986;11:227–234. doi: 10.1016/0165-0327(86)90074-1. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Gaudiano BA, Epstein-Lubow G, et al. Medication burden in bipolar disorder: A chart review of patients at psychiatric hospital admission. Psychiatry Research. 2014;216:24–30. doi: 10.1016/j.psychres.2014.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willour VL, Seifuddin F, Mahon PB, et al. A genome-wide association study of attempted suicide. Molecular Psychiatry. 2012;17:433–444. doi: 10.1038/mp.2011.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: Update 2013. Bipolar Disorders. 2013;15:1–44. doi: 10.1111/bdi.12025. [DOI] [PubMed] [Google Scholar]
- Yen CF, Cheng CP, Ko CH, et al. Suicidality and its association with insight and neurocognition in Taiwanese patients with bipolar I disorder in remission. The Journal of Nervous and Mental Disease. 2008;196:462–467. doi: 10.1097/NMD.0b013e3181775a3d. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Choi YM. Impact of psychotropic drugs on suicide and suicidal behaviors. Bipolar Disorders. 2013;15:594–621. doi: 10.1111/bdi.12098. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J. Lithium, anticonvulsants and suicidal behavior in bipolar disorder. Journal of Affective Disorders. 2003;73:223–228. doi: 10.1016/s0165-0327(02)00302-6. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J. Bipolar pharmacotherapy and suicidal behavior. Part I: Lithium, divalproex and carbamazepine. Journal of Affective Disorders. 2007a;103:5–11. doi: 10.1016/j.jad.2007.05.019. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J. Bipolar pharmacotherapy and suicidal behavior. Part 3: Impact of antipsychotics. Journal of Affective Disorders. 2007b;103:23–28. doi: 10.1016/j.jad.2007.05.018. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J, et al. Bipolar pharmacotherapy and suicidal behavior. Part 2: The impact of antidepressants. Journal of Affective Disorders. 2007c;103:13–21. doi: 10.1016/j.jad.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Youssef NA, Bradford DW, Kilts JD, et al. Exploratory investigation of biomarker candidates for suicide in schizophrenia and bipolar disorder. Crisis. 2015;36:46–54. doi: 10.1027/0227-5910/a000280. [DOI] [PubMed] [Google Scholar]
- Zalsman G, Braun M, Arendt M, et al. A comparison of the medical lethality of suicide attempts in bipolar and major depressive disorders. Bipolar Disorders. 2006;8:558–565. doi: 10.1111/j.1399-5618.2006.00381.x. [DOI] [PubMed] [Google Scholar]