Abstract
Little is known about how obesity susceptibility single nucleotide polymorphisms (SNPs) interact with moderate to vigorous physical activity (MVPA) in relation to BMI during adolescence, once obesogenic neighborhood factors are accounted for. In race stratified models, including European (EA; N=4977), African (AA; N=1726), and Hispanic Americans (HA; N=1270) from the National Longitudinal Study of Adolescent to Adult Health (1996; ages 12-21), we assessed the evidence for a SNP × MVPA interaction with BMI-for-age Z score, once accounting for obesogenic neighborhood factors including physical activity amenities, transportation and recreation infrastructure, poverty and crime. Eight SNP × MVPA interactions with suggestive significance (p<0.10; three in each EA, and AA, two in HA) were observed showing attenuation on BMI-for-age Z score in adolescents with ≥ 5 versus < 5 bouts/week MVPA, except for rs10146997 (near NRXN3). Findings were robust to the inclusion of neighborhood-level variables as covariates. These findings suggest that any attenuation from MVPA on a genetic susceptibility to obesity during adolescence is likely not operating through obesogenic neighborhood factors.
Keywords: Genetics of obesity, adolescence, BMI, African and Hispanic American, physical activity
INTRODUCTION
Adolescence is a high-risk period for weight gain that is often maintained or exacerbated into adulthood (Gordon-Larsen P et al. 2004; The et al. 2010). Physical activity (PA) is an effective behavior to prevent or reduce unwanted weight gain (Knowler et al. 2002; Singh et al. 2008; Hankinson et al. 2010). A growing literature suggests that neighborhood amenities, such as physical activity resources, green-space, as well as neighborhood socio-demographics are associated with the physical activity of residents (Block et al. 2004; Cummins et al. 2005; Frank et al. 2006; Gordon-Larsen et al. 2006; Moore and Diez Roux 2006; Oakes et al. 2007; Larson et al. 2009; Rodriguez et al. 2009; Boone-Heinonen et al. 2011). However, while the physical activity literature has included attention to neighborhood environment, few studies have examined gene by physical activity interactions and obesity in relation to obesogenic neighborhood factors.
Several genetic loci that influence body mass index (BMI) or obesity have been successfully identified primarily in European descent adults (Speliotes et al. 2010; Locke et al. 2015), but many generalize to other ethnic groups (Wen et al. 2012; Graff et al. 2013; Monda et al. 2013). Further, recent studies suggest that physical activity may modify a genetic susceptibility to obesity by attenuating the genetic effect on BMI (Andreasen et al. 2008; Sonestedt et al. 2009; Kilpelainen et al. 2011). The most notable study reported a weaker genetic effect on BMI from the FTO locus in more active compared to inactive individuals (Kilpelainen et al. 2011; Xi et al. 2011). Previously we examined the interaction of established obesity susceptibility SNPs with <5 vs.≥5 bouts moderate to vigorous physical activity (MVPA) per week in relation to BMI-for-age Z-scores in a nationally representative sample of European American (EA), African–American (AA) and Hispanic American (HA) adolescents (Richardson et al. 2014). We reported that higher moderate to vigorous physical activity (MVPA) per week attenuated the effect on BMI-for-age Z-score of variants in/near GNPDA2 and FTO in EA, in/near MAP2K5, LMX1B, and NRXN3 in AA, and in/near LZTR2 and LRRN6C in HA. Thus, we demonstrated a protective effect of MVPA on increased genetic susceptibility to obesity. However, the interaction between genetic variants and physical activity behaviors in relation to obesity has not previously accounted for the neighborhood environment. While it has been shown that the obesogenic environment is associated with obesity through decreased physical activity, it is not known how this can influence the PA-SNP interaction on obesity.
To address this gap in the literature, we used data from a US nationally representative, longitudinal cohort to determine whether established obesity SNPs interact with MVPA in relation to BMI-for-age Z score, once accounting for obesogenic neighborhood factors. We hypothesized that the interaction between obesity SNPs and MVPA in relation to BMI-for-age Z score inverse association would be influenced by accounting for neighborhood obesogenic features. In the current analysis, we selected SNPs from 39 obesity susceptibility SNPs that were found to have an interaction with MVPA that met suggestive statistical significance at p-value<0.10 using the current sample and based on the analyses previously performed (Richardson et al. 2014) and further tested for the independence of these interaction effects once adjusting for neighborhood environment elements, such as crime, population density, green space, physical activity resources, and neighborhood sociodemographics.
METHODS
Add Health
Participants
Add Health is a nationally representative cohort of adolescents (1994-95, n=20,745, aged 11-20 y, mean age 15.9 y) drawn from a probability sample of 80 US high schools and 52 US middle schools, representative of US schools in 1994-95 with respect to region, urban setting, school size, school type, and race or ethnic background. Wave II (1996, n = 14,738, aged 12-21 y, mean age 16.5 y) included by design Wave I adolescents still of school-age, including those currently in high school and high school drop outs. Oversampled subgroups include related and non-related adolescents sharing a Wave I household (n=5,524 Wave I respondents living in 2,639 households (Harris et al. 2006)), highly educated African Americans, and several race/ethnic subpopulations, including Chinese, Cubans, Puerto Ricans, and Filipinos. Wave III (2001-2002, n= 15,197, aged 18-27 y, mean age 22.3 y) and Wave IV (2008-2009, n=15,701, aged 23-32 y, mean age 28.9 y) followed all Wave I respondents, regardless of Wave II participation. The most recent data collection (Wave IV) included follow-up interviews from 15,701 respondents drawn from 19,962 of the original 20,745 Wave I respondents. Survey procedures have been described elsewhere (Resnick et al. 1997; Miller et al. 2004; Harris 2010) and were collected under written informed consent at each exam and protocols approved by Institutional Review Board at the University of North Carolina at Chapel Hill.
Race/ethnicity
Because genetic biomarkers to determine ancestry were unavailable, we used a race/ethnicity variable constructed from respondent and parental survey items on ancestral background and family relationship status, creating a race/ethnicity variable with priority for agreement between participant and parental report. We used a three-category classification: non-Hispanic EA, non-Hispanic AA and HA. Within HA, we also classified subpopulation: Cuban, Puerto Rican, Central/South Americans, Mexican or Other Hispanic, as well as non-US-born (first generation immigrants) and US-born (second- or third-generation immigrants).
Genetic characterization
The current analyses focus on seven of 39 SNPs which display a suggestive interaction (p-value < 0.10) with MVPA on BMI (see Supplementary Table 1) in our previous work (Richardson et al. 2014). (One SNP had an interaction with MVPA in both Europeans and African ancestry individuals). At the time of our study, the 39 SNPs were previously identified in published GWAS for their association with BMI (33 variants), obesity (4 variants) and central adiposity (2 variants) in European-descent individuals (Lindgren et al. 2009; Meyre et al. 2009; Thorleifsson et al. 2009; Willer et al. 2009; Heid et al. 2010; Speliotes et al. 2010; Wen et al. 2012). Genotyping was performed using TaqMan assays and the ABI Prism 7900® Sequence Detection System (Applied Biosystems, Foster City, CA, USA). In prior work we also illustrate the marginal effects of these loci on BMI-for-age Z-scores (Richardson et al. 2014, see Supplemental Material) and BMI (Graff et al. 2012). The SNPs that we focused on in the current analyses were rs9939609 (in FTO), rs10938397 (near GNPDA2), rs10146997 (in NRXN3) in individuals of European ancestry, rs867559 (near LMX1B) and rs2241423 (in MAP2K5) and rs10146997 (in NRXN3) in individuals of African Ancestry, and rs10968576 (near LRRN6C) and rs543874 (near SEC16B and LZTR2) in individuals of Hispanic Ancestry.
BMI-for-age Z-score
Weight and height were measured during in-home surveys using standardized procedures. BMI (kg/m2) was calculated using measured height and weight assessed at Waves II or III when participants were aged 12–21 years, with priority for younger age at measurement (Wave II: n = 14 646) unless the respondent was not seen at Wave II (Wave III: n = 785) and was still between the ages of 12 and 21 years. Self-reported height and weight were substituted for those refusing measurement and/or weighing more than the scale capacity (Wave II n = 119; Wave III n =34). The Add Health self-reported weight and height correlate strongly with measured weight (r = 0.95) and height (r = 0.94) (Team 1999). Given the heterogeneity in growth during the age range of our study (12-21 years), we used BMI Z-scores (Z-BMI) based on the CDC age- and sex-matched growth charts as the outcome in all statistical analyses (Ogden et al. 2002). This is the appropriate approach for analyzing BMI in adolescents (Flegal and Ogden 2011).
MVPA
Weekly frequency occurrences (bouts) of leisure-time MVPA (skating and cycling, exercise, and active sports) were queried at Waves II and III using a standard, interviewer-administered activity recall based on validated questionnaires (Sallis et al. 1996). The questionnaire included activities relevant to adolescents at Wave II and was modified at Wave III to include age-appropriate activities; Wave III bouts were scaled for comparability with Wave II (Willett 1998). MVPA ranged between 0 and 16.5 bouts per week but was skewed with 50% of individuals having less than 5 bouts per week, making its use as a continuous variable less optimal. Adolescents were classified as achieving or not achieving five or more weekly sessions of MVPA (i.e. high MVPA was classified as =>5 bouts and low MVPA classified as <5 bouts per week). We selected MVPA from the same Wave in which we also selected height and weight, thus MVPA and BMI were matched temporally. We use 5 bouts of MVPA as the threshold because this is the recommendation for MVPA for adolescents at the time of study (American Cancer Society 2001; Physical Activity Guidelines Advisory Committee Report, 2008).
Neighborhood Environment Attributes
We used the Add Health Obesity and Neighborhood Environment database (ONEdata), a geographic information system (GIS)-derived dataset of time-varying neighborhood-level characteristics spatially and temporally linked to Add Health respondent residential locations in 1994-95 (Wave I) and in 2001-2002 (Wave III). Because the individual-level phenotype data (e.g. BMI-for-age Z-scores, MVPA, etc.) in Add Health respondents are at either Waves II (not Wave I) or III, we temporally matched the neighborhood-level and individual-level data for BMI-for-age Z-score and MVPA. When we used the individual-level data from 1996 (Wave II) we used neighborhood-level data from 1994-95 (Wave I) and when we used the individual-level data 2001-2002 we used the neighborhood-level data from Wave III. We used data created within a 3-km straight line distance (Euclidean buffer) around each respondent's residential location based on empirical evidence (Boone-Heinonen et al. 2011; Hillier et al. 2011) and block group, tract, and county attributes from time-matched U.S. Census and other data, which were merged with individual-level Add Health interview responses (Boone-Heinonen et al. 2010).
Our neighborhood recreational amenities data come from Dun and Bradstreet (D&B) from 1995 for Wave I and from 2001 for Wave III. D&B is a commercial source of business records by 8-digit Standard Industrial Classification (SIC) codes (Supplementary table listing SIC codes by each type) that has shown high overall agreement between commercial and field data (Boone et al. 2008). We captured neighborhood infrastructure derived from ESRI Streetmap data (2000) for Wave I and from Streetmap Pro data (July 2003, v.5.2) for Wave III from Environmental Systems Research Institute (ESRI, http://www.esri.com) in Redlands, CA. We characterized neighborhood crime using county-based FBI Uniform Crime report data from 1995 for Wave I and from 2001 for Wave III, and U.S. Census tract-level data from 1990 for Wave I and from 2000 for Wave III to characterize neighborhood sociodemographic characteristics. We used the U.S. Geological Service's National Land Cover Dataset derived from Fragstats [version 3.3 build 5] from 1992 for Wave I and from 2001 for Wave III to derive proportion of undeveloped land that is either natural or recreational, hereafter referred to as “green space”.
We used the above data sources to create three main categories of neighborhood environment factors. First, we included a set of neighborhood physical activity amenities, which included counts of physical activity facilities, including parks, public facilities such as community centers, and pay facilities such as golf courses and health centers. Second, we used a set of variables that characterize the neighborhood transportation and recreation infrastructure, which included counts of cul-de-sacs, green space, and alpha index (ratio of observed to maximum possible route alternatives between street nodes), with higher values of each indicating greater walkability. Third, we use a set of variables for neighborhood social characteristics, which included crime rates per 100,000 population within the county, and the percent of persons <150% of federal poverty level (1.5*federal poverty level (U.S Census Bureau 2009)). Further details about the methods used can be found elsewhere(Boone-Heinonen et al. 2010).
We have previously demonstrated an association between more obesogenic neighborhood environmental attributes with lower physical activity and higher obesity.(Gordon-Larsen et al. 2006; Nelson et al. 2006; Boone-Heinonen et al. 2010; Boone-Heinonen et al. 2010; Boone-Heinonen et al. 2010; Boone-Heinonen and Gordon-Larsen 2011; Boone-Heinonen et al. 2011; Richardson et al. 2011; Boone-Heinonen and Gordon-Larsen 2012).
Analytic sample
At Wave IV 58% (n = 12 066) of the original Wave I (n = 20 745) respondents provided samples, from which DNA was extracted and genotyped, and consent for banking and use in genetic studies. Individuals with DNA samples that had at least 80% of the 39 SNPs successfully genotyped (n = 11 448) and who were between the ages of 12 and 21 years at either Waves II or III were eligible (n = 9129). Among the 9129 eligible adolescents, we excluded the following participants: within monozygotic twin pairs, the twin with fewer genotyped loci (n = 139), individuals of Native American (n = 57), Asian (n = 437), or unclassified (n = 69) race/ethnicity due to insufficient sample size, pregnant (n=110), disabled (n = 47), and those with missing data for: geographic region (n = 67), BMI (n = 2), current smoking (n = 46), race/ethnicity (n = 43), MVPA (n = 1), screen time (i.e. hours per week spent for leisure computer, TV and video use) (n = 42), or environment data (n = 80). The final analytic sample included 7992 individuals (Supplementary Figure 1).
Statistical analysis
Descriptive analyses. We used means and proportions to describe individual-level characteristics and IQR to describe neighborhood-level characteristics (Table 1). All analyses were conducted using Stata, version 13.0 (Stata Corp, College Station, TX, USA. In race/ethnicity-stratified, multivariable models, we included a SNP × MVPA interaction term, and controlled for age, sex, current smoking status (≥1 cigarette every day for 30 days), screen time (hours of screen time from television, video and computer games per week), geographic region, and an indicator for self-reported heights and weights (n = 86), with additional controls in AA models: oversampling of highly educated AA families (n = 355), and in HA models: Hispanic ancestry: Cuban (n = 193), Puerto Rican (n = 224), Central/South American (n = 120), Mexican (n = 660), and other Hispanic (n = 103), and foreign born (n = 268). Sample design effects and familial relatedness were accounted for in all multivariable linear models using separate random effects for school and family. We selected SNPs that had an SNP by MVPA interaction at suggestive significance of p-value <0.10 in each race/ethnic group in the current sample (Supplementary Table 1). For the meta-analyzed sample, we looked for SNPs that were available for evaluation across all three race/ethnic groups, were directionally consistent across the three race/ethnic groups, and had suggestive significance of p-value <0.10. However, no SNPs met this criteria so we did not take any forward for evaluation with environmental factors in the meta-analyzed sample. To examine how including the neighborhood-level features changed the patterns of the SNP by MVPA interactions, used a forward stepwise addition in adjusting for each of the 3 categories of neighborhood environmental characteristics (see Supplementary Note): 1) physical activity resources: physical activity facilities, parks; 2) neighborhood infrastructure: green space, street connectivity; 3) neighborhood social factors: neighborhood poverty, and crime, with their separate interaction terms by MVPA and by SNP; and 4) all neighborhood resources and factors from 1), 2) and 3) above and their interaction with the respective SNP in the model. All models include the SNP by MVPA interaction with the indicated SNP. Model 1a only included the SNP by MVPA interaction without any of the neighborhood environmental factors and serves as the baseline model for comparison. Subsequent models build upon Model 1a. Model 1b adjusted for physical activity resources. Model 1c adjusted for physical activity resources and neighborhood infrastructure resources. Model 1d adjusted for physical activity resources, neighborhood infrastructure resources, and neighborhood social resources. Model 1e included the interactions of physical activity resources, neighborhood infrastructure resources, and neighborhood social resources with the respective SNP.
Table 1.
Individual- and neighborhood-level characteristics across race, the National Longitudinal Study of Adolescent to Adult Health
| European American | African American | Hispanic American | |
|---|---|---|---|
| N | 4,996 | 1,725 | 1,270 |
| Age, mean (SD), y | 16 (1.8) | 16 (1.9) | 17 (1.8) |
| Male sex, n (%) | 2,369 (47.4) | 771 (44.7) | 625 (49.2) |
| BMI1, mean (SD) | 23.0 (5.0) | 24.3 (5.8) | 24.0 (5.3) |
| BMI-for-age Z scores, mean (SD) | 0.31 (1.1) | 0.53 (1.1) | 0.48 (1.1) |
| MVPA ≥ 5 bouts per week2, n (%) | 3,177 (63.6) | 1,014 (58.8) | 741 (58.3) |
| Screen time, mean (SD), h/wk | 19.2 (16.9) | 27.7 (22.3) | 21.3 (17.8) |
| Current smoking, n (%) | 2,035 (40.7) | 320 (18.63) | 358 (28.2) |
| Geographic region, n (%) | |||
| West | 753 (15.1) | 244 (14.1) | 500 (39.4) |
| Midwest | 1,842 (36.9) | 330 (19.1) | 94 (7.4) |
| South | 1,642 (32.9) | 1,052 (61.0) | 492 (38.7) |
| Northeast | 760 (15.2) | 99 (5.7) | 184 (14.5) |
| PHYSICAL ACTIVITY RESOURCES3 | |||
| Counts of pay facilities, median4 (IQR) | 2.1 (0, 4.5) | 1.0 (0, 2.7) | 1.3 (0.6, 2.4) |
| Counts of public facilities, median (IQR) | 0 (0, 0.1) | 0.1 (0, 0.5) | 0.2 (0, 0.5) |
| Counts of parks, median (IQR) | 0 (0, 4.0) | 3.0 (0, 9) | 8.0 (6, 14) |
| NEIGHBOHROOD INFRASTRUCTURE | |||
| Green space (sq mile), median (IQR)5 | 0.4 (0.2, 0.01) | 0.3 (0.2, 0.5) | 0.2 (0.1, 0.3) |
| Alpha index, median (IQR) | 0.3 (0.2, 0.4) | 0.3 (0.3, 0.4) | 0.3 (0.2, 0.4) |
| Counts of cul de sacs, median (IQR)6 | 3.8 (1.6, 7.3) | 4.5 (2.2, 7.0) | 5.4 (2.9, 10.2) |
| NEIGHBOHROOD SOCIODEMOGRAPHICS | |||
| Percent population <100% FPL7 | 8.7 (4.6, 15.0) | 22.4 ( (10.6, 32.0) | 12.9 (7.0, 24.7) |
| Crime rate (%)8 | 4.4 (2.7, 5.9) | 6.3 (5.6, 8.3) | 6.2 (5.1, 7.7) |
Abbreviation: MVPA moderate to vigorous physical activity, BMI: Body Mass Index, FPL: federal poverty level
Unless otherwise indicated, data are presented as number (column percentage).
Calculated as weight in kilograms divided by height in meters squared.
Define how MVPA: Weekly frequency (bouts) of leisure-time MVPA (skating and cycling, exercise, and active sports) were queried using a standard, interviewer-administered activity recall. To explicitly test estimated effects for obesity susceptibility SNPs relative to the recommendation for MVPA for adolescents at the time of study (i.e., ≥5 bouts of MVPA week per week; American Cancer Society 2001), MVPA was dichotomized to high (≥5) vs. low (<5) bouts per week using the Wave at which height and weight were measured.
Spatially and temporally linked to respondents residential locations
Counts of Dunn & Bradstreet activity resources from 1996 for Wave I and from 2001 for Wave III within Euclidean 3km buffer per 10 km local and secondary roadways.
U.S. Geological Service's 1992 National Land Cover Dataset from 1992 for Wave I and from 2001 for Wave III using Fragstats [version 3.3 build 5] to derive proportion of recreational or undeveloped land (greenspace).
StreetMap 2000 data for Wave I and from Streetmap Pro (July 2003, v.5.2) for Wave III from Environmental Systems Research Institute (ESRI, www.esri.com) in Redlands, CA
U.S. Census-tract level data from 1990 for Wave 1 and from 2000 for Wave III.
National Archive of Criminal Justice Data at the county-level from 1995 for Wave I and from 2001 from Wave III.
Defined as the rate per 100,000 population. Show in the table as a percentage.
RESULTS
The Add Health adolescents were on average 16.4 years of age (ages 12-21 y, 47.5 % male) and had a mean BMI-for-age Z-score of 0.38 (Table 1), ranging from 0.31 in EA to 0.58 in AA. Approximately 60% of adolescents reported MVPA≥5 bouts per week. Counts of pay physical activity facilities were higher in EA neighborhoods but parks were higher among AA and HA neighborhoods. Infrastructure appeared similar across race/ethnicity, but the counts of cul-de-sacs were highest (mean 5.4) in HA neighborhoods. Finally, the percent of the population below the poverty level was highest among AA and lowest among EA (6.3% versus 4.4%).
From our previously published work we selected the SNP × MVPA associations with p<0.10 (Richardson et al. 2012). In European Americans there were three: rs10938397 (near GNPDA2), rs9939609 (in FTO) and rs10146997 (near NRXN3). In rs10938397 and rs9939609, high MVPA (≥ 5 bouts per week) attenuated the risk allele effect on BMI-for-age Z score, while in rs10146997 the risk allele effect on BMI-for-age Z score increased for adolescents with high versus low MVPA. In Hispanic Americans we identified two SNP × MVPA associations at p<0.10; rs10968576 (in LRRN6C) and rs543874 (in/near LZTR2 and SEC16B), both of which attenuated BMI-for-age Z score. For African Americans, rs2241423 (in MAP2K5), rs10968576 (in LRRN6C), and rs867559 (near LMX1B) showed p<0.10 for interaction (Supplementary Table 2, Model a). All three were negatively associated with BMI-for-age Z score.
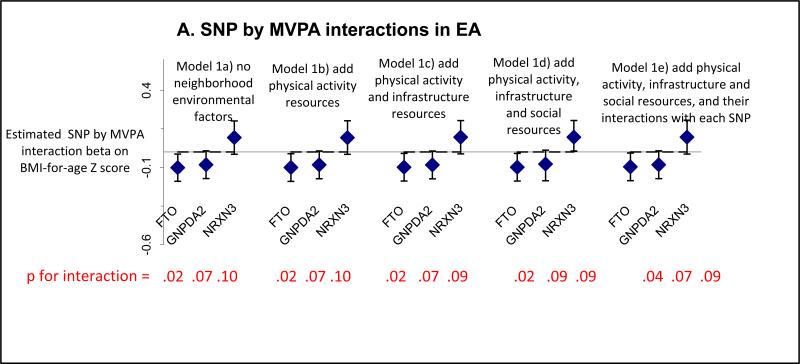
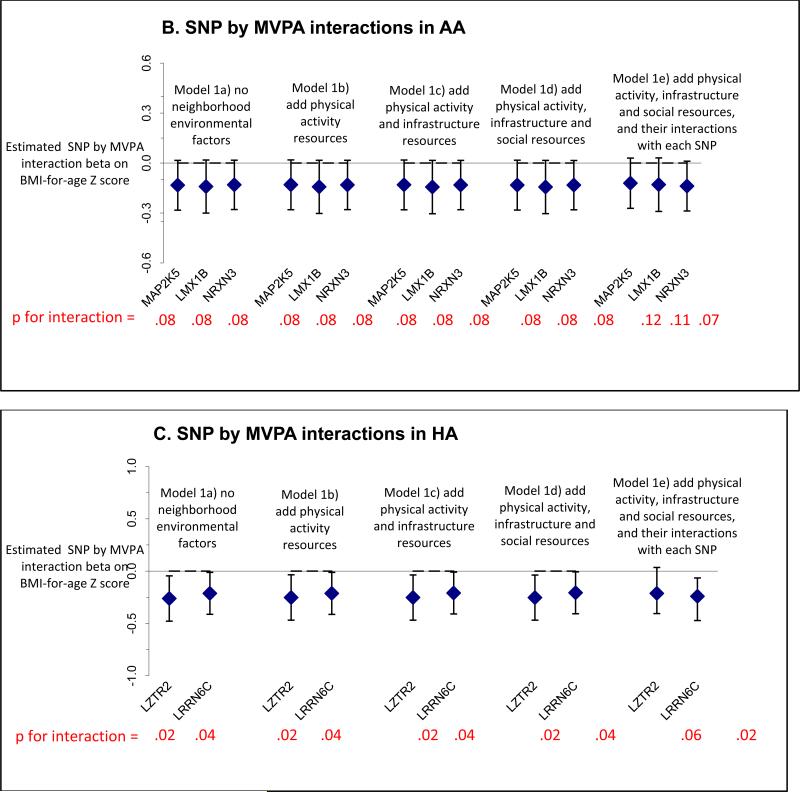
Extending our previously published work, we tested the SNPs that showed empirical evidence for interaction with MVPA relative to BMI-for-age Z score at p<0.10 again and further adjusted for the three categories of neighborhood-level environmental factors (described above) including: counts of physical activity resources, neighborhood infrastructure, and neighborhood sociodemographics. Further adjustment of the SNP × MVPA interactions with the neighborhood-level environmental factors had little influence on the effect estimates (see Figure 1 & Supplementary Table 2, Models b-e). Model e includes the two-way interactions between physical activity and neighborhood-level environmental factors, as well as neighborhood-level environmental factors and each SNP. The SNP × MVPA changed little by including these two way interactions with neighborhood-level environmental factors and SNP. None of the neighborhood-level environmental factors × SNP interactions were significant except for with three SNPs with neighborhood poverty including LRRN6C in HA, NRXN3 in EA, and MAP2K5 in AA. However, excluding the interactions of these SNPs with MVPA did not change their interactions with neighborhood poverty.
Figure 1.
The estimated interaction effects for moderate to vigorous physical activity (MVPA) with the indicated SNPs by race/ethnicity (A. European ancestry [EA], B. African ancestry [AA], C. Hispanic ancestry [HA]) on BMI-for-age Z-score, before and after adjusting for neighborhood environmental factorsa.
Abbreviations: EA: European Americans; AA: African Americans: HA: Hispanic Americans a The 3 categories of neighborhood environmental factors are defined as follows: 1) physical activity resources, which included counts of physical activity facilities, parks, public facilities such as community centers, pay facilities such as golf courses and health centers; 2) transportation and recreation infrastructure (labeled in the graphs as infrastructure resources), which included counts of cul-de-sacs, green space (the proportion of undeveloped land that is either natural or recreational, derived from the U.S. Geological Service's National Land Cover Dataset based on Fragstats [version 3.3 build 5] from 1992 for Wave I and from 2001 for Wave III), and alpha index (ratio of observed to maximum possible route alternatives between street nodes), with higher values of each indicating greater walkability; and 3) a set of neighborhood social characteristics variables (labeled in the graphs as social resources), which included crime rates per 100,000 population within the county, and the percent of persons <150% of federal poverty level (1.5*federal poverty level [U.S. Census Bureau 2009]). Further details about the methods used can be found elsewhere [Boone et al Health Place. 2010]. All models include the SNP by MVPA interaction with the indicated SNP. Model 1a only included the SNP by MVPA interaction without any of the neighborhood environmental factors and serves as the baseline model for comparison. Subsequent models build upon Model 1a. Model 1b adjusted for physical activity resources. Model 1c adjusted for physical activity resources and neighborhood infrastructure resources. Model 1d adjusted for physical activity resources, neighborhood infrastructure resources, and neighborhood social resources. Model 1e included the interactions of physical activity resources, neighborhood infrastructure resources, and neighborhood social resources with the respective SNP.
Discussion
Previous reports suggest that physical activity may attenuate the association of genetics on obesity. In the current analysis, we further investigated the interaction of moderate-to-vigorous physical activity and the obesity loci independent of the context of neighborhood environments. For loci where we found some suggestion of effect modification from physical activity on BMI-for-age Z-score (p-value for interaction < 0.10) we further adjusted for the neighborhood-level environmental factors. These factors had little influence on the effect estimates, suggesting that irrespective of neighborhood environments, physical activity may still have the potential to attenuate the influence of genetic susceptibility on obesity.
Studies that have investigated the interaction of genetic obesity susceptibility loci and physical activity on BMI have primarily been conducted among adults of European descent (Andreasen et al. 2008; Sonestedt et al. 2009; Kilpelainen et al. 2011; Liu et al. 2011; Ahmad et al. 2013). Most have focused on the locus in the FTO gene, reporting an attenuation on BMI for active individuals of European ancestry carrying at least one copy of the risk allele for FTO, and have noted a stronger association among those living in North America (Kilpelainen et al. 2011). Two other studies illustrated that increased physical activity can diminish the effect incurred by genetic predisposition (quantified using a genetic risk score comprised of 12 independent variants) on BMI and obesity. Variants in or near FTO and also SEC16B demonstrated the largest magnitude of effect to the risk score, both showing at least nominally significant associations with BMI and obesity. Again, the association was primarily driven by cohorts of European ancestry from North America (Ahmad et al. 2013). The latter observation suggests an environmental component that is exacerbating the interaction in those from North America. Xi et al 2011 found associations of 5 obesity risk SNPs (including FTO and GNPDA2) only in children who had moderate-to-low physical activity levels or engaged in sedentary behavior, regardless of which risk alleles they carried. The results indicated that encouraging less sedentary behavior and higher levels of physical activity could alleviate the influence of risk alleles on genetic predisposition to childhood obesity, thereby serving as a promising prevention strategy. Our purpose in the current study, was to take a closer look at some of the neighborhood environmental factors with potential influence on the previously identified nominally significant SNP × MVPA interactions in relation to BMI (two of which were FTO and GNPDA2) in adolescents from North America. Our results suggest that other neighborhood environmental factors did little to diminish or counteract the estimates.
There have been few studies examining the influence of various environmental factors, other than physical activity, on genetic obesity risk. Two studies of adult twins in the US and Denmark found a decrease in the heritability in BMI with increasing income (adjusted for insurance coverage and education level) and education, respectively (Johnson and Krueger 2005; Johnson et al. 2011). A similar result was seen in adolescent (aged 11-14) twins from Finland, where genetic variance in adolescent BMI was lower in families with highly educated parents (Lajunen et al. 2012). This makes understanding the complex interplay between genetic and environmental factors influencing obesity risk particularly important in the current obesogenic environment (Kirk et al. 2010).
We conducted a power analysis using SNPs in/near NRXN3, FTO, GNPDA2) in European ancestry individuals, finding power of 99% for the identifying a main effect and between 18-20% for identifying an interaction. While this is relative low power for finding an interaction, the statistical power to test the significant interactions is typically about 5-times lower that to test main effect. The interactions of FTO and GNPDA2 with physical activity have been seen in adult and childhood studies (Kilpelainen et al. 2011;Xi et al. 2011;Ahmad et al. 2013), lending support our findings. While the results should be interpreted with caution because of low power, they still could have potential meaning given the challenges of identifying and interactions particularly with genetic factors.
While our study capitalizes on an ancestrally diverse nationally representative cohort measured during a unique period of the lifecycle, there are limitations. First, established obesity loci in all racial/ethnic groups is lacking, particularly for HA. Second, interaction estimation has greater random error than main effect estimations due to smaller sample size (Greenland 2009) and this is especially a limitation in non-European ancestry populations. Third, we rely on self-reported physical activity behaviors. With objective measures of energy expenditure, we might have increased power to detect associations of interest, due to precision of measurement. Also, there may be more complex interactions such as gene by gene and/or gene by unmeasured environmental influences that might affect BMI. Fourth, we focus on residential neighborhood environments and do not account for other environments where participants likely spent time, such as school. Fifth, we lack ancestral informative markers to account for population admixture. Sixth, in our cross-sectional analysis we are unable to assess temporal relationships with MVPA behavior patterns and BMI change over time. Finally, we are unaware of another adolescent sample with the kind of neighborhood data that would allow us to replicate the models we have run here. Instead, we put these results out in the literature is in hopes that other will have an interest in also pursuing the modifications and influence from neighborhood and obesogenic environment on genetics and behaviors. Despite these limitations our study capitalizes on an ethnically diverse adolescent population and well-established obesity loci to investigate the joint role of MVPA and established obesity variants on BMI, with adjustment for neighborhood factors known to influence physical activity.
In summary, our findings show little influence from residential neighborhood environmental factors on any attenuation of a genetic effect on BMI from MVPA during adolescence, in that effect sizes remained relatively unchanged. Further we found similar results of unchanged effect sizes for tested loci in African, Hispanic and European ancestry groups in the study. To the extent that other large genetic consortia have access to neighborhood environment data, it would be worthwhile to replicate these findings in larger samples of adolescents.
Supplementary Material
Highlights.
Obesity susceptibility SNPs may interact with physical activity to attenuate increased BMI.
The obesogenic environment might change this interaction.
We tested the interaction of eight SNPs each with physical activity once the obesogenic neighborhood was accounted for.
Neighborhood-level factors did not influence SNP × MVPA interactions.
Physical activity may attenuate genetic influences on BMI in any environment.
Acknowledgements
This work was funded by National Institutes of Health grant R01HD057194. P.G.L., K.E.N., E.M.L., L.A.L, A.S.R, K.L.Y., and M.G. contributed to study design, A.S.R. and M.G. performed the data analysis, and P.G.L., K.E.N., A.Y.L., E.M.L., L.A.L, K.M.H., K.L.Y., and M.G. contributed to writing the manuscript, all other authors provided critical evaluation of the manuscript. A.S.R, K.L.Y., M.G., K.E.N., and P.G.L. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). We thank Amy Perou of the BioSpecimen Processing facility and Amanda Floyd Beaty and Michael Andre of the Mammalian Genotyping Core at University of North Carolina at Chapel Hill. We are grateful to the Carolina Population Center (R24 HD050924) for general support. There were no potential or real conflicts of financial or personal interest with the financial sponsors of the scientific project.
Abbreviations
- EA
non-Hispanic European American
- AA
non-Hispanic African American
- HA
Hispanic American
- BMI
body mass index
- PA
physical activity
- SNPs
single-nucleotide polymorphisms
- GWAS
genome-wide associated studies
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmad S, Rukh G, et al. Gene x physical activity interactions in obesity: combined analysis of 111,421 individuals of European ancestry. PLoS Genet. 2013;9(7):e1003607. doi: 10.1371/journal.pgen.1003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen CH, Stender-Petersen KL, et al. Low physical activity accentuates the effect of the FTO rs9939609 polymorphism on body fat accumulation. Diabetes. 2008;57(1):95–101. doi: 10.2337/db07-0910. [DOI] [PubMed] [Google Scholar]
- Block JP, Scribner RA, et al. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Boone-Heinonen J, Casanova K, et al. Where can they play? Outdoor spaces and physical activity among adolescents in U.S. urbanized areas. Prev Med. 2010;51(3-4):295–298. doi: 10.1016/j.ypmed.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Evenson KR, et al. Built and socioeconomic environments: patterning and associations with physical activity in U.S. adolescents. Int J Behav Nutr Phys Act. 2010;7:45. doi: 10.1186/1479-5868-7-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P. Life stage and sex specificity in relationships between the built and socioeconomic environments and physical activity. J Epidemiol Community Health. 2011;65(10):847–852. doi: 10.1136/jech.2009.105064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P. Obesogenic environments in youth: concepts and methods from a longitudinal national sample. Am J Prev Med. 2012;42(5):e37–46. doi: 10.1016/j.amepre.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P, et al. Environment and Physical Activity Dynamics: The Role of Residential Self-selection. Psychol Sport Exerc. 2011;12(1):54–60. doi: 10.1016/j.psychsport.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171(13):1162–1170. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Guilkey DK, et al. Residential self-selection bias in the estimation of built environment effects on physical activity between adolescence and young adulthood. Int J Behav Nutr Phys Act. 2010;7:70. doi: 10.1186/1479-5868-7-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Popkin BM, et al. What neighborhood area captures built environment features related to adolescent physical activity? Health Place. 2010;16(6):1280–1286. doi: 10.1016/j.healthplace.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone JE, Gordon-Larsen P, et al. Validation of a GIS facilities database: quantification and implications of error. Ann Epidemiol. 2008;18(5):371–377. doi: 10.1016/j.annepidem.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S, Stafford M, et al. Neighbourhood environment and its association with self rated health: evidence from Scotland and England. J Epidemiol Community Health. 2005;59(3):207–213. doi: 10.1136/jech.2003.016147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL. Childhood Obesity: Are We All Speaking the Same Language? Adv Nutr March 2011 Adv Nutr vol. 2011;2:159S–166S. doi: 10.3945/an.111.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank L, Sallis J, et al. Many pathways from land use to health. J Am Plan Assn. 2006;72:75–87. [Google Scholar]
- Gordon-Larsen P, Adair LS, et al. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. American Journal of Clinical Nutrition. 2004;80(3):569–575. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, et al. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Graff M, Fernandez-Rhodes L, et al. Generalization of adiposity genetic loci to US Hispanic women. Nutr Diabetes. 2013;3:e85. doi: 10.1038/nutd.2013.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Interactions in epidemiology: relevance, identification, and estimation. Epidemiology. 2009;20(1):14–17. doi: 10.1097/EDE.0b013e318193e7b5. [DOI] [PubMed] [Google Scholar]
- Hankinson AL, Daviglus ML, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304(23):2603–2610. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM. An integrative approach to health. Demography. 2010;47(1):1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, et al. The National Longitudinal Study of Adolescent Health (Add Health) twin data. Twin Res Hum Genet. 2006;9(6):988–997. doi: 10.1375/183242706779462787. [DOI] [PubMed] [Google Scholar]
- Heid IM, Jackson AU, et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet. 2010;42(11):949–960. doi: 10.1038/ng.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier A, Cannuscio C, et al. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geography. 2011;32:712–729. [Google Scholar]
- Johnson W, Krueger RF. Genetic effects on physical health: lower at higher income levels. Behav Genet. 2005;35(5):579–590. doi: 10.1007/s10519-005-3598-0. [DOI] [PubMed] [Google Scholar]
- Johnson W, Kyvik KO, et al. Education modifies genetic and environmental influences on BMI. PLoS One. 2011;6(1):e16290. doi: 10.1371/journal.pone.0016290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpelainen TO, Qi L, et al. Physical activity attenuates the influence of FTO variants on obesity risk: a meta- analysis of 218,166 adults and 19,268 children. PLoS Med. 2011;8(11):e1001116. doi: 10.1371/journal.pmed.1001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk SF, Cramm CL, et al. The state of obesity management for women giving birth in Atlantic Canada. Matern Child Health J. 2010;14(3):453–458. doi: 10.1007/s10995-009-0455-4. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lajunen HR, Kaprio J, et al. Genetic and environmental influences on BMI from late childhood to adolescence are modified by parental education. Obesity (Silver Spring) 2012;20(3):583–589. doi: 10.1038/oby.2011.304. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, et al. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lindgren CM, Heid IM, et al. Genome-wide association scan meta-analysis identifies three Loci influencing adiposity and fat distribution. PLoS Genet. 2009;5(6):e1000508. doi: 10.1371/journal.pgen.1000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G, Zhu H, et al. Influence of common variants in FTO and near INSIG2 and MC4R on growth curves for adiposity in African- and European-American youth. Eur J Epidemiol. 2011;26(6):463–473. doi: 10.1007/s10654-011-9583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke AE, Kahali B, et al. Genetic studies of bosy mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyre D, Delplanque J, et al. Genome-wide association study for early-onset and morbid adult obesity identifies three new risk loci in European populations. Nat Genet. 2009;41(2):157–159. doi: 10.1038/ng.301. [DOI] [PubMed] [Google Scholar]
- Miller WC, Ford CA, et al. Prevalence of chlamydial and gonococcal infections among young adults in the United States. JAMA. 2004;291(18):2229–2236. doi: 10.1001/jama.291.18.2229. [DOI] [PubMed] [Google Scholar]
- Monda KL, Chen GK, et al. A meta-analysis identifies new loci associated with body mass index in individuals of African ancestry. Nat Genet. 2013;45(6):690–696. doi: 10.1038/ng.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96(2):325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson MC, Gordon-Larsen P, et al. Built and social environments associations with adolescent overweight and activity. Am J Prev Med. 2006;31(2):109–117. doi: 10.1016/j.amepre.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Oakes JM, Forsyth A, et al. The effects of neighborhood density and street connectivity on walking behavior: the Twin Cities walking study. Epidemiol Perspect Innov. 2007;4:16. doi: 10.1186/1742-5573-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Kuczmarski RJ, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee Report. U.S. Department of Health and Human Services; Washington, DC: 2008. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Richardson AS, Boone-Heinonen J, et al. Neighborhood fast food restaurants and fast food consumption: a national study. BMC Public Health. 2011;11:543. doi: 10.1186/1471-2458-11-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson AS, North KE, et al. Moderate to vigorous physical activity interactions with genetic variants and body mass index in a large US ethnically diverse cohort. Pediatr Obes. 2014;9(2):e35–e46. doi: 10.1111/j.2047-6310.2013.00152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez DA, Evenson KR, et al. Land use, residential density, and walking. The multi-ethnic study of atherosclerosis. Am J Prev Med. 2009;37(5):397–404. doi: 10.1016/j.amepre.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Strikmiller PK, et al. Validation of interviewer- and self-administered physical activity checklists for fifth grade students. Med Sci Sports Exerc. 1996;28(7):840–851. doi: 10.1097/00005768-199607000-00011. [DOI] [PubMed] [Google Scholar]
- Singh AS, Mulder C, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- Sonestedt E, Roos C, et al. Fat and carbohydrate intake modify the association between genetic variation in the FTO genotype and obesity. Am J Clin Nutr. 2009;90(5):1418–1425. doi: 10.3945/ajcn.2009.27958. [DOI] [PubMed] [Google Scholar]
- Speliotes EK. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 2010;42:937–948. doi: 10.1038/ng.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team AHB. Biomarkers in Wave III of the Add Health Study. L. E. Manhart; 1999. p. 57. [Google Scholar]
- The NS, Suchindran C, et al. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–2047. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorleifsson G, Walters G, et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nature Genetics. 2009;41(1):18–24. doi: 10.1038/ng.274. [DOI] [PubMed] [Google Scholar]
- S Census Bureau U. 2009 [Google Scholar]
- Wen W, Cho YS, et al. Meta-analysis identifies common variants associated with body mass index in east Asians. Nat Genet. 2012;44(3):307–311. doi: 10.1038/ng.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willer CJ. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat. Genet. 2009;41:25–34. doi: 10.1038/ng.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett WC, editor. Nutritional Epidemiology. Oxford University Press; New York: 1998. [Google Scholar]
- Xi B, Wang C, et al. Influence of physical inactivity on associations between single nucleotide polymorphisms and genetic predisposition to childhood obesity. Am J Epidemiology. 1. 2011;173(11):1256–62. doi: 10.1093/aje/kwr008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.