Introduction
Research suggests that income inequality may be a threat to population health, including both physical and mental health outcomes. Mechanisms by which income inequality is hypothesized to deleteriously affect health include psychosocial stress, such as through frustration induced by a heightened sense of relative deprivation, as well as reduced social cohesion and its sequelae, such as increased crime (Adjaye-Gbewonyo & Kawachi, 2012; Cifuentes et al., 2008; Kawachi & Subramanian, 2014; Pabayo, Kawachi, & Gilman, 2015). Ecological analyses among high-income countries indicate that income inequality may be more strongly correlated with mental illness (correlations of 0.73) than other health outcomes such as life expectancy, obesity, infant mortality, and homicide (Pickett & Wilkinson, 2015). However, much of the evidence linking income inequality to mental health outcomes fails to adequately address several important questions that might improve causal inference, including confounding and temporal order.
Major depression represents a growing segment of the global burden of disease. Major depressive disorder rose from the 15th leading cause of global disability-adjusted life years to the 11th leading cause between 1990 and 2010, and depressive disorders contribute more to years lived with disability than other mental and behavioral conditions (Murray et al., 2013). In addition, while depression results in major morbidity in its own right, including risk of suicide, it has also been linked to greater risk of physical ailments such as cardiovascular disease (Hare, Toukhsati, Johansson, & Jaarsma, 2014; Rumsfeld & Ho, 2005).
Studies on income inequality and depression or other mental health outcomes have drawn on analyses of ecological data (Bouffard & Dubé, 2013; Hiilamo, 2014; Messias, Eaton, & Grooms, 2011; Pickett & Wilkinson, 2015), which may be subject to the ecological fallacy or confounding by compositional characteristics of individuals in areas with different levels of inequality. A recent study by Hiilamo (2014) employed longitudinal data from municipalities in Finland for the years 1995 to 2010. Using fixed-effects methods, he examined whether changes in income inequality, as measured by the Gini coefficient, were associated with changes in depression. There was no association between changes in municipal Gini coefficients and antidepressant use, but, among older people, increases in municipal inequality were associated with decreases in antidepressant use. However, as noted in the limitations, the study was ecological. Therefore, it could not test whether municipal income inequality was associated with antidepressant use independently of individual income—that is, whether income inequality has a contextual effect on depression over and above the effect of income (Gravelle, Wildman, & Sutton, 2002).
Several studies have used data at multiple levels to attempt to assess the contextual effect of income inequality on depression while controlling for individual-level factors, but most have been cross-sectional. For example, an international study using the World Health Surveys found that income inequality at the national level was not associated with individual risk of depression (Rai, Zitko, Jones, Lynch, & Araya, 2013). Steptoe and colleagues observed a positive cross-sectional association between national income inequality and depressive symptoms among university students from 23 countries (Steptoe, Tsuda, Tanaka, & Wardle, 2007). A study based in the United Kingdom found income inequality to be associated with common mental disorders independently of individual income only among high-income individuals, while it had a protective association among low-income individuals (Weich, Lewis, & Jenkins, 2001).
Studies within the United States have generally found income inequality at the state, county, school, or neighborhood level to be associated with higher levels of depression or depressive symptomatology, but some results have been mixed or have failed to observe a detrimental effect of income inequality (Ahern & Galea, 2006; Goodman, Huang, Wade, & Kahn, 2003; Gresenz, Sturm, & Tang, 2001; Henderson, Liu, Diez Roux, Link, & Hasin, 2004; Muramatsu, 2003; Pabayo, Kawachi, & Gilman, 2014; Shi, Starfield, Politzer, & Regan, 2002; Sturm & Gresenz, 2002; Zimmerman & Bell, 2006). In a recent prospective study, Pabayo et al. (2014) examined the association between state-level income inequality in the U.S. and major depression measured three years later and observed that income inequality was associated with increased risk of depression among women but not among men.
There have been recent calls to expand the test of the income inequality hypothesis as it relates to mental health in low- and middle-income countries (LMICs), particularly since these countries tend to have higher levels of inequality compared to high-income countries (Burns, 2015; Lund, 2015). However, there is still debate over whether absolute income is of more importance for health in LMICs compared to relative income. For example, in LMICs where large proportions of the populations may still live in poverty, health may be largely determined by poverty and absolute income rather than by relative income and inequality; the latter, as some argue, may have more import in high-income countries where much of the population already has basic needs met. A study by Cifuentes et al. (2008) found that, controlling for individual-level factors, income inequality was associated with major depressive episodes among countries in the top third of the Human Development Index (a measure of national development and well-being) but not in countries with lower Human Development Indices.
Other studies of income inequality in LMICs are suggestive of potential health impacts on income inequality, however; thus, highlighting the need for further research on this issue Burns and Esterhuizen (2008) assessed the association between income inequality and presentation for treatment of psychosis in seven municipalities in a district in South Africa and found that municipality inequality was positively correlated with treated incidence of psychosis; however, the study was ecological and did not control for individual-level factors. Only a few multilevel studies controlling for compositional factors have been conducted within non-Western countries or in LMICs (Burns, 2015). Chiavegatto Filho, Kawachi, Wang, Viana, and Andrade found that income inequality among municipalities within Sao Paulo, Brazil—a middle-income country with high levels of inequality—was positively associated with depression. By contrast, Fernandez-Nino, Manrique-Espinoza, Bojorquez-Chapela, and Salinas-Rodriguez (2014) found no association between income inequality (at the locality, municipality, and state levels) and prevalence of depressive symptoms among older adults in Mexico. Again, these studies did not examine this relationship longitudinally, and it is therefore difficult to tease out the temporal order of any links between income inequality and depression which is necessary for causal inference.
In Africa, studies examining the association between mental health and income inequality are sparse (Burns & Esterhuizen, 2008; Cifuentes et al., 2008; Rai et al., 2013), although many African countries are among the nations with the highest levels of inequality worldwide (Kim, Kawachi, Hoorn, & Ezzati, 2008). The middle-income country of South Africa consistently tops the list of most unequal societies. The World Bank estimates its Gini coefficient at 0.63 as of 2011, ranking it as the most unequal country among those with available data for that year (World Bank, 2016). This high level of inequality reflects a legacy of colonialism and apartheid, but there is also evidence that income inequality has further increased in the post-apartheid era and in recent years (Bhorat, van der Westhuizen, & Jacobs, 2009; Leibbrandt, Finn, & Woolard, 2012; OECD, 2013; van der Berg, 2011). Thus, South Africa may be an important setting in which to examine the potential effects of income inequality on mental health.
Over 16% of South African adults are estimated to suffer from a common mental disorder, including depression, anxiety, or a substance use disorder (Lund, Kleintjes, Kakuma, Flisher, & Consortium, 2010; Williams et al., 2008), and estimates of the prevalence of major depression among adults range from about 3% for past year prevalence to nearly 10% for lifetime prevalence (Rai et al., 2013; Tomlinson, Grimsrud, Stein, Williams, & Myer, 2009; Williams et al., 2008). When looking at depressive symptomatology and not solely clinical depression, the estimated prevalence of depressive symptomatology is around 36% for women and 27% for men in South Africa (Ardington & Case, 2009; Tomlinson et al., 2009), illustrating a potentially high burden in this population.
In the present study, we sought to examine the potential association between area-level income inequality and individual-level depressive symptoms in South Africa using longitudinal data. Our study is unique in that it links detailed longitudinal microdata to area-level (district) changes in income inequality over a four-year period. We employ a fixed-effects approach that controls for unmeasured confounding and introduce a wide set of controls for individual and district characteristics. Although South Africa has some of the highest levels of income inequality worldwide (OECD, 2013) few studies have examined the relationship between income inequality and depressive symptoms here. This study contributes to the literature on income inequality and health by expanding our knowledge about the potential nature of this association in a highly unequal setting.
Methods
Data Sources and Sample
The source of individual- and household-level data for this study was the National Income Dynamics Study (NIDS), which is a nationally-representative, household, panel survey conducted by the Southern Africa Labour and Development Research Unit (National Income Dynamics Study, 2014). The sampling strategy was a stratified, two-stage cluster design, and the household response rate was 69% as described in detail previously (De Villiers et al., 2014; Southern Africa Labour and Development Research Unit, 2014a; Southern Africa Labour and Development Research Unit, 2014b; Southern Africa Labour and Development Research Unit, 2014c).
At the area level, district councils were used as the unit of analysis. South Africa is divided administratively into nine provinces, over 50 district councils and further into municipalities. District councils are primarily responsible for delivery of primary health care among other public services and vary widely in terms of characteristics such as demographics and urban-rural make-up, health indicators, et cetera (Day, Barron, Massyn, Padarath, & English, 2012; The Local Government System in South Africa, 2009; Massyn et al., 2014; Naledi, Barron, & Schneider, 2011). District-level data were drawn from two census data sources, South Africa's Community Survey 2007 (Minnesota Population Center, 2013) and Census 2011 (Statistics South Africa, 2014a). Census and Community Survey data have been used to analyze trends in national income inequality in South Africa in previous research (Yu, 2010). District variables in the present study were calculated according to the 2011 administrative boundaries for all 52 districts (Day, Gray, & Budgell, 2011; Day et al., 2012; Statistics South Africa, 2012). The Community Survey 2007 was a 2% random sample of South Africa's population conducted by Statistics South Africa, the administrative body that conducts censuses in South Africa, to provide population estimates between the 2001 and 2011 censuses at national and subnational levels (Minnesota Population Center, 2013; Statistics South Africa, 2007). Questions in the Community Survey 2007 are analogous to those in the census. Community Survey 2007 data were linked to the 2008 NIDS Wave 1 survey for the present analysis. The data from the Census 2011 was a 10% sample of the census containing over one million households and nearly 4.5 million individuals (Statistics South Africa, 2014b). Data from the census sample were linked to the 2012 NIDS Wave 3 survey.
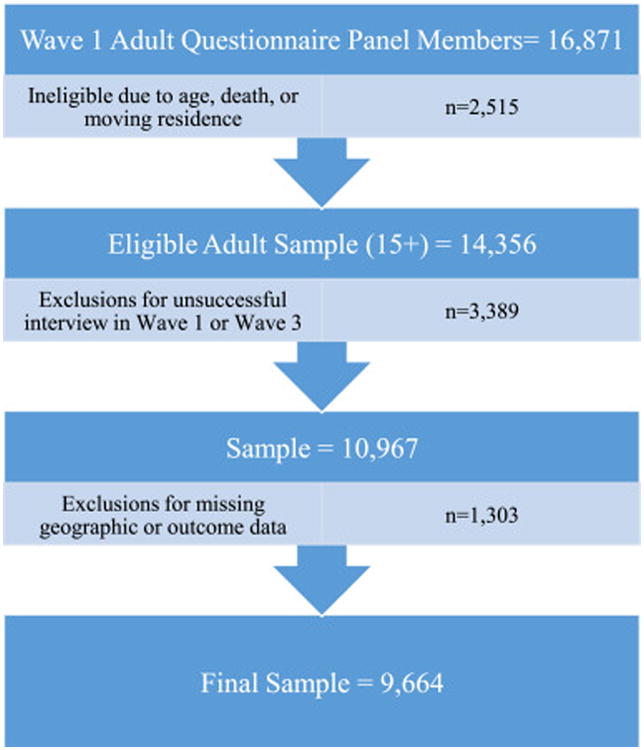
Of the original Wave 1 NIDS adult sample of 16,871 individuals, 2,515 panel members were considered ineligible because of: discrepant or incomplete age information or being under 15 years of age at the time of the Wave 1 interview (n=110), death by Wave 3 (n=1,208), living outside of South Africa in Wave 3 (n=43), or living in a different district council from their original Wave 1 district in Wave 3 (n=1,203). Of the eligible sample, 3,389 panel members were excluded for unsuccessful interviews in Wave 1 (n=1,056) or Wave 3 (n=2,618). Finally, 1,303 respondents were excluded due to missing or unknown geographic (district council) information in Wave 3 (n=27) or an incomplete depressive symptoms assessment in either Wave 1 (n= 54) or Wave 3 (n=1,252). The final sample contained 9,664 individuals (Figure 1).
Figure 1. Flowchart of sample selection.
Variables
Depressive Symptoms
The NIDS adult survey includes the Center for Epidemiological Studies Depression Scale Short Form (CES-D-10). The items ask respondents about the frequency of the following 10 symptoms over the past week: being unusually bothered, having trouble keeping their minds on current activities, feeling depressed, feeling that all activities were an effort, feeling hopeful about the future, feeling fearful, having restless sleep, being happy, feeling lonely, and being unable to get going. The responses are on a four-point Likert scale [rarely or none of the time (< 1 day), some or little of the time (1-2 days), occasionally or a moderate amount (3-4 days), all of the time (5-7 days)]. The CES-D-10 scale has been validated in a number of samples and performed similarly to the full-length CES-D (which has been widely used and validated to assess depressive symptomatology) in terms of reliability, predictive accuracy for depression, and assessment of severity of depressive symptoms among older adults, HIV-positive patients, and a sample of psychiatric patients (Andresen, Malmgren, Carter, & Patrick, 1994; Bjorgvinsson, Kertz, Bigda-Peyton, McCoy, & Aderka, 2013; Zhang et al., 2012).
CES-D-10 scores were calculated following procedures used in previous studies (Alaba & Chola, 2013; Meffert, McCulloch, Neylan, Gandhi, & Lund, 2015; Tomita, Labys, & Burns, 2015a, 2015b) to create scores ranging from 0 to 30, indicating increasing symptomatology. Individuals missing five or more items in the scale were excluded. For individuals missing four or fewer items, the mean score of the non-missing items was used to impute the values for the missing items, and this was summed with the other responses to create the score. Of the 9,664 adults in the sample, 125 individuals had one or more items in the scale imputed this way in Wave 1, while 86 had one or more items imputed in Wave 3. The internal consistency of the CES-D-10 scale in this sample measured using the standardized Cronbach's coefficient alpha was 0.75 in Wave 1 and 0.74 in Wave 3.
Sensitivity analyses dichotomizing depressive symptoms using a cutoff score of 10, as has been used and validated in previous research (Andresen et al., 1994); Bjorgvinsson, Kertz, Bigda-Peyton, McCoy, & Aderka, 2013; Meffert et al., 2015; Tomita et al., 2015a, 2015b), were also run for comparison.
Income Inequality
The exposure of interest was district-level income inequality measured using the Gini coefficient (Subramanian, Kawachi, & Smith, 2007). We calculated district Gini coefficients in SAS (Cohen, N.d.) and Stata (Ineqdec0) from self-reported gross income estimated before deductions but including social grants as recorded in 12 categories in the Community Survey 2007 and Census 2011 (Lehohla 2008). Incomes were deflated to August 2012 prices and equivalized by dividing by the square root of household size. Additional details of these calculations are available in Appendix A. Gini coefficients were multiplied by a factor of 10 for use in the models.
In order to test for potentially non-linear effects of Gini coefficients, sensitivity analyses categorized Gini coefficients into five absolute categories based on the initial distribution of district Gini coefficients as well as into relative quartiles based on the distributions of district Gini coefficients in each time period.
Covariates
Covariates at the individual and household levels included, age, sex, population group (African, Coloured, White, Asian/Indian), education (no education, some general education and training, completed general education and training, some further education and training, completed further education and training, and higher education), log of monthly household income deflated to August 2012 levels, employment status (employed, unemployed, not economically active), marital status (currently married/living with partner, currently single), urban/rural location, and household receipt of any government grants (e.g. old age pension, child support grant). At the district level, covariates included log mean monthly household income, mean age, percent African, percent Coloured, percent female, percentage of adults aged 15+ years with no education, percentage of adults aged 15+ years with completed further education, percentage of adults aged 15+ years with higher education, percentage of adults aged 15-65 years who were unemployed, percentage of adults aged 15-65 years who were not economically active, and percentage of households that were rural.
Analysis
Data were cleaned and analyzed in SAS version 9.4 and Stata version 13.
Missing responses, responses of “don't know,” refusals to answer an item, or items that were not applicable to an individual were coded as missing for all variables. Given the low percentage of missing responses on covariates (<2%), those with missing covariates were excluded from all analyses, and complete–case analyses were conducted.
We first ran pooled cross-sectional models for Waves 1 and 3, using linear regression for the outcome CES-D-10 score. Pooled ordinary least squares models provide a picture of the cross-sectional association between income inequality and depression, pooling data from each time period to enhance power. This assumes the relationships between the variables do not change over time. These models exploit the variation both within and across individuals and districts to give a snapshot of the overall association between inequality across districts and the outcome during the time period; but, the results may be biased if there are unmeasured differences between individuals and districts that affect both inequality and depressive symptoms.
Therefore, to attempt to account for and assess potential unmeasured bias in the pooled cross-sectional models, we ran longitudinal models with individual fixed-effects. Fixed-effects regressions model only the within-individual changes in the outcome (depressive symptoms) over time in relation to within-individual, or in this case within-district, changes in the exposure (Gini coefficient). Each individual is essentially used as his or her own control by comparing his or her outcome at one time point under a given level of district inequality to his or her outcome at another time point under a different level of inequality. This therefore removes as sources of confounding all between-individual (and consequently between-district) differences, measured or unmeasured, that are fixed over time by factoring out between-individual variation and only examining the variation within individuals. Because only changes are modeled in fixed-effects regressions, all factors that remain constant over time do not contribute to the models. These models are conservative. However, while fixed-effects models account for time constant confounding, they cannot control for characteristics that change over time; therefore, several time-varying covariates, as described above, were also included in the models. Linear fixed-effects models were run for the continuous outcome CES-D-10 scores with the following generic model specification:
where t indicates wave, i indicates individuals, h indicates households, and j indicates districts. CESDtihj denotes individual-level depressive symptoms in Waves 1 and 3. β0 represents the intercept. Inequalitytj is the Gini coefficient for each district in each wave. Covariatestihj, Covariatesthj, and Covariatestj are vectors of individual, household, and district covariates, respectively. Wavet are the time fixed-effects. β6individualihj are the individual fixed-effects, and e0tihj are the error terms. The coefficient β1 is the main effect of interest.
For all models, 2011 administrative district boundaries were used. Standard errors were clustered by district. Sensitivity analyses using the dichotomous measure of high depressive symptoms used Poisson regression to estimate risk ratios, as this outcome was common in the sample (Cummings, 2009; Lumley, Kronmal, & Ma, 2006; Petersen & Deddens, 2008).
Results
Descriptive Statistics
Sample characteristics are shown in Table 1. The sample was 65% female and 80% African population group. The mean age at baseline was 38.9 years, and the mean size for households in the sample was 4.3 individuals. About 51% of households were rural, and at baseline over 60% of households received some type of government support (e.g., child support, old age pension); 18.6% of individuals were unemployed, and 60.8% of individuals were currently single. The mean Wave 1 CES-D-10 score was 8.1 out of 30, and 34.3% of the sample had high depressive symptoms (score ≥ 10) at baseline compared to a mean CES-D-10 score of 7.1 and prevalence of high depressive symptoms of 27.1% in Wave 3. The correlation between CES-D-10 scores across time was fairly low though significant [Pearson correlation between Wave 1 and 3 was 0.13 (p<0.0001)]. Average outcomes differed considerably by district (see Figure 2).
Table 1. Sample characteristics, Waves 1 and 3.
| Wave 1 | Wave 3 | |||
|---|---|---|---|---|
|
|
||||
| Sample Size | Proportion/Mean (Standard Deviation) | Sample Size | Proportion/Mean (Standard Deviation) | |
| Total | 9,664 | 9,664 | ||
| Female | 9,664 | 64.5% | 9,664 | 64.5% |
| Population group | 9,664 | 9,664 | ||
| African | 80.3% | 80.3% | ||
| Coloured | 14.8% | 14.8% | ||
| Asian/Indian | 1.1% | 1.1% | ||
| White | 3.7% | 3.7% | ||
| Age (years) | 9,664 | 38.9 (17.3) | 9,664 | 43.1 (17.3) |
| Highest Education level | 9,657 | 9,656 | ||
| No Education | 14.0% | 13.5% | ||
| Some General Education & Training | 35.5% | 31.6% | ||
| General Education & Training | 9.1% | 7.2% | ||
| Some Further Education & Training | 21.0% | 23.0% | ||
| Further Education & Training | 14.2% | 14.2% | ||
| Higher Education | 6.29% | 10.6% | ||
| Monthly household income (Rand) | 5,388 | 5,061.6 (8,682.7) | 5,986 | 5,874.2 (9,697.8) |
| Mean household size | 5,388 | 4.3 (2.6) | 5,986 | 4.4 (2.9) |
| Rural household | 5,388 | 51.0% | 5,986 | 50.9% |
| Percent of households receiving government | 5,369 | 60.6% | 5,983 | 62.8% |
| grants | ||||
| CES-D-10 score | 9,664 | 8.1 (4.8) | 9,664 | 7.1 (4.5) |
| High depressive symptoms | 9,664 | 34.3% | 9,664 | 27.1% |
| Employment status | 9,576 | 9,642 | ||
| Employed | 39.1% | 38.0% | ||
| Unemployed | 18.6% | 17.1% | ||
| Not economically active | 42.3% | 44.9% | ||
| Marital Status | 9,631 | 9,657 | ||
| Currently Married/Cohabiting | 39.2% | 38.6% | ||
| Currently single | 60.8% | 61.4% | ||
Figure 2. Cross-sectional scatter plots of district Gini coefficient (x-axis) and district-level summary of depressive symptoms (y-axis).
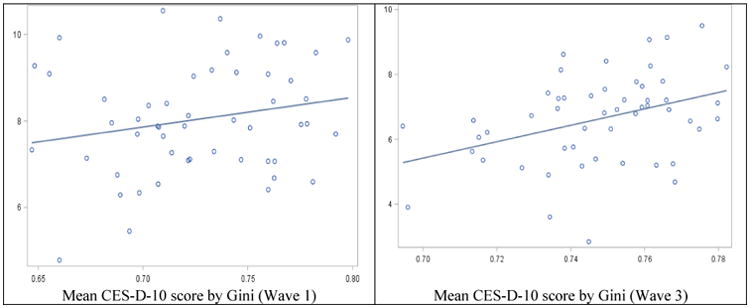
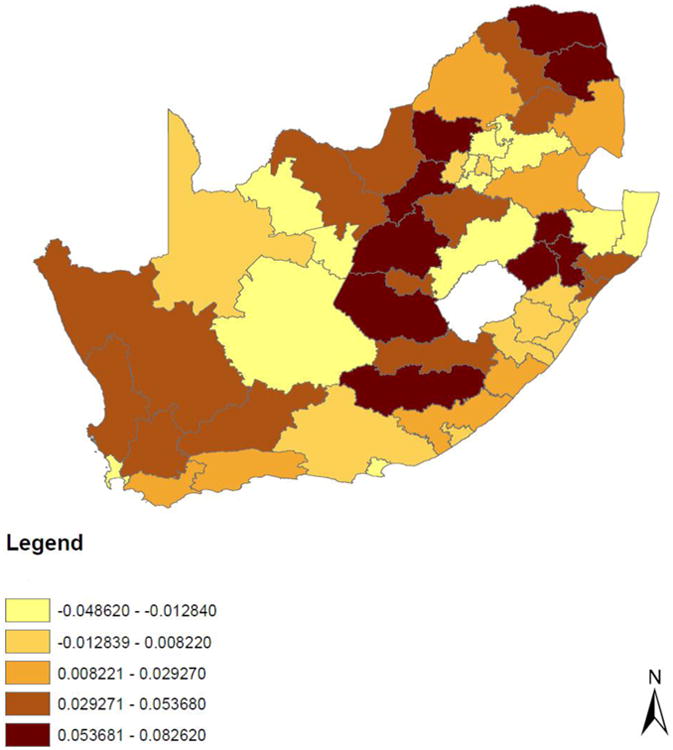
District Gini coefficients ranged from 0.65 to 0.80 in 2007 with a mean of 0.73 (see Appendix B). On average, district Gini coefficients increased by 0.02 to a mean of 0.75 (range 0.69-0.78) in 2011. The changes in district Gini coefficients between 2007 and 2011 ranged from -0.05 to 0.08 and are displayed in Figure 3. Although depressive symptoms decreased on average over time, and Gini coefficients increased on average, Figure 2 illustrates that there were positive cross-sectional correlations between district Gini coefficients and district rates of depressive symptoms in Waves 1 and 3. This association was further explored in the regressions discussed below.
Figure 3. Changes in District Council Gini Coefficients, South Africa 2007-2011.
Model Results
The results of pooled cross-sectional and longitudinal fixed-effects models are shown in Table 2. (Separate cross-sectional models for Waves 1 and 3 are available in Appendix C though the estimates for the association between district Gini coefficients and depressive symptoms did not differ statistically across waves in fully-adjusted interaction models.) Associations for covariates were in the expected directions: Female sex, lower levels of education, being single, lower household income (log), higher age, and African population group were associated with higher CES-D-10 scores. In addition, the coefficient for wave indicated a decline in depressive symptoms between Waves 1 and 3 of the survey, although inclusion of district-level covariates rendered this decline non-significant. Appendix C shows estimates for district-level covariates.
Table 2. Reression model coefficients for the outcome CES-D-10 score.
| Pooled cross-sectional models | Longitudinal fixed-effects models | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Covariates/Parameters | Model 1 | Model 2 | Model 3a | Model 1 | Model 2 | Model 3a |
| 10*District Gini Coefficient (Standard Error) | 1.10* (0.54) | 0.65 (0.38) | 0.50 (0.56) | 0.29 (0.60) | 0.30 (0.59) | -0.08 (0.97) |
| Wave 1 | Ref | Ref | Ref | Ref | Ref | Ref |
| Wave 3 (Standard Error) | -1.25*** (0.21) | -1.17*** (0.19) | -0.96 (0.61) | -1.08*** (0.17) | -1.05*** (0.17) | -0.95 (0.82) |
| Log household income (Standard Error) | -0.53*** (0.07) | -0.53*** (0.07) | -0.14 (0.09) | -0.16 (0.09) | ||
| Household size (Standard Error) | 0.05 (0.03) | 0.05* (0.02) | 0.04 (0.04) | 0.03 (0.04) | ||
| Urban | Ref | Ref | Ref | Ref | ||
| Rural (Standard Error) | -0.27 (0.20) | -0.34 (0.20) | ||||
| Does not receive government grants | Ref | Ref | Ref | Ref | ||
| Receives government grants (Standard Error) | -0.21 (0.14) | -0.24 (0.14) | -0.31 (0.18) | -0.35 (0.18) | ||
| Age (yrs) (Standard Error) | 0.04*** (0.00) | 0.04*** (0.00) | ||||
| African | Ref | Ref | ||||
| Coloured (Standard Error) | -1.58*** (0.29) | -1.08** (0.29) | ||||
| Asian/Indian (Standard Error) | -2.01*** (0.40) | -2.09*** (0.41) | ||||
| White (Standard Error) | -2.25*** (0.29) | -1.93*** (0.37) | ||||
| Male | Ref | Ref | ||||
| Female (Standard Error) | 0.52*** (0.07) | 0.54*** (0.08) | ||||
| No education | Ref | Ref | ||||
| Some general education & training (Standard Error) | -0.14 (0.14) | -0.22 (0.13) | ||||
| Completed general education & training (Standard Error) | -0.51** (0.18) | -0.60** (0.19) | ||||
| Some further education & training (Standard Error) | -0.50** (0.16) | -0.58** (0.16) | ||||
| Completed further education & training (Standard Error) | -0.78*** (0.18) | -0.86*** (0.17) | ||||
| Higher education (Standard Error) | -0.78*** (0.18) | -0.84*** (0.18) | ||||
| Currently single | Ref | Ref | Ref | Ref | ||
| Currently married/living with partner (Standard Error) | -0.48*** (0.07) | -0.46*** (0.07) | -0.55* (0.22) | -0.59* (0.22) | ||
| Not economically active | Ref | Ref | Ref | Ref | ||
| Employed (Standard Error) | -0.19 (0.10) | -0.16 (0.10) | -0.31 (0.17) | -0.23 (0.16) | ||
| Unemployed (Standard Error) | 0.01 (0.13) | 0.02 (0.13) | -0.17 (0.18) | -0.08 (0.16) | ||
Model 3 also controls for the following district covariates: Percent female, percent African, percent Coloured, mean age, log mean equivalized household income, percent with no education, percent with higher education, percent unemployed, percent not economically active, and percent rural (see Appendix C).
Italics indicates p<0.10.
Bold indicates p<0.05.
indicates p<0.05.
indicates p<0.01.
indicates p<0.001.
Models are linear, and fixed-effects models use individual fixed effects. Standard errors are clustered by district.
Contrary to our hypothesis, district-level income inequality was not associated with CES-D-10 scores in fully-adjusted, pooled cross-sectional or longitudinal fixed-effects models (Table 2). In fixed-effects models adjusting for other covariates, there were no statistically significant interactions between income inequality and income, baseline age (50+ years, vs. 15-49), or population group; models stratified by sex also revealed no significant estimates for the association between income inequality and depressive symptoms for either sex (results available upon request). Sensitivity analyses for the dichotomous measure of high depressive symptoms produced similar results (see Appendix C). Sensitivity analyses using categorical Gini coefficients also failed to show significant associations between income inequality and depressive symptoms in models adjusted for other covariates.
Discussion
Income inequality was not associated with depressive symptoms in this sample from South Africa, a country with one of the highest income inequality levels. Despite previous research showing positive associations between income inequality and depression, as detailed in a recent review (Pickett & Wilkinson, 2015), a number of other studies have failed to observe an association between income inequality and mental health outcomes including depression, or have noted that contextual factors explain a relatively small proportion of the variance in mental illness (Fernandez-Nino et al., 2014; Gresenz et al., 2001; Pabayo et al., 2015; Rai et al., 2013).
We offer several explanations for the lack of association between depressive symptoms and income inequality in this analysis. First and foremost, our findings may indicate that there is, in fact, no causal relationship between income inequality and depression, at least in South Africa. It is possible, for example, that compared to populations in high-income countries, South Africans are more tolerant of high levels of income inequality because of their hopes and expectations for a better future in a post-apartheid setting.
Alternatively, our analysis may not have captured the relevant etiologic period for the impact of income inequality on depression. To further examine this issue, we conducted sensitivity analyses matching Gini coefficients from the Census 2001 (Minnesota Population Center, 2013; Statistics South Africa, 2003) to the 2008 NIDS survey (7-8 year lag) and Gini coefficients from the Community Survey 2007 to the 2012 NIDS survey (5-6 year lag). However, associations between Gini coefficients and depressive symptoms, controlling for other factors, continued to remain statistically non-significant. If the etiologic period is longer, we may have missed an association, and additional follow-up would be warranted.
Another potential explanation may be that there are ceiling effects for the impact of income inequality on health, and that there was insufficient variability between districts and over time to detect effects. The districts in South Africa all had very high levels of inequality, ranging from 0.65 to 0.80 during the four years examined. It may be that at such levels of inequality, any additional increases over time or moderate differences between districts may have little impact on depressive symptoms.
A further consideration is that the Gini coefficient does not provide information on the nature of the income distribution in an area. Multiple income distributions may give rise to the same Gini coefficient (Burns, 2015; Rasella, Aquino, & Barreto, 2013). It may be that in the states or countries in which associations between income inequality and health have been observed, Gini coefficients correspond to particular structures of the income distribution which differ from those in South Africa. Or, as has been previously suggested in neo-materialist hypotheses and observed by Cifuentes et al. (2008), income inequality may matter in high-income countries with low levels of poverty and not in low- or middle-income countries with high levels of poverty, where the effects of poverty and individual income may be more significant (Cifuentes et al., 2008). Therefore, it could be that in South Africa, the material impacts of absolute income may be of more relevance to depressive symptoms than relative income.
Lastly, the effects of income inequality may operate at various geographic scales depending on whether people compare themselves to others at the national, regional, municipal, or local level and on how society and resources are organized. If there is high residential segregation, as is the case in some areas of South Africa (Bradlow, Bolnick, & Shearing, 2011; Tomita & Burns, 2013; Tomita et al., 2015b), smaller areal units of analysis for income inequality may not capture the full range of society members to which individuals compare themselves (Chiavegatto Filho et al., 2013). Therefore, it is not clear whether districts are the most appropriate level of analysis for income inequality; however, we do not see an indication that they would not be.
Our results also suggest that depressive symptoms decreased in this sample over time. This decline may be related to secular trends or other changes in demographic characteristics, such as increases in income or improvements in the economy.
Consistent with theories on social support and depression (Berkman & Glass, 2000; Berkman & Krishna, 2014; Kawachi & Berkman, 2001), as well as with results from other studies (Cifuentes et al., 2008; Fernandez-Nino et al., 2014; Rai et al., 2013; Tomita et al., 2015b), individuals who were married or partnered, or who became married or partnered had reduced levels of depressive symptoms in our sample. Additionally, consistent with social determinants of health frameworks and other studies (Allen, Balfour, Bell, & Marmot, 2014; Ardington & Case, 2009; Berkman & Kawachi, 2014; Glymour, Avendano, & Kawaachi, 2014; Hong, Knapp, & McGuire, 2011; Lynch & Kaplan, 2000; Rai et al., 2013; Tomita & Burns, 2013; Tomita et al., 2015b; Tomlinson et al., 2009), depressive symptoms in our sample tended to decrease with increasing income and education. Income inequality did not interact with income in supplementary analyses. Some studies have likewise failed to observe interactions between income inequality and measures of socioeconomic status in relation to depression (Pabayo et al., 2014; Rai et al., 2013), while others have observed interactions (Weich et al., 2001).
We also found depressive symptoms to be higher among those of African population group compared to those of other population groups in this sample. This would be consistent with a social determinants of health framework, since black Africans in South Africa were the most economically and socially marginalized under the apartheid system (Tomita et al., 2015b; van der Berg, 2011). Some others have observed a similar racial pattern with depression and depressive symptoms in South Africa; however, this has not been consistent (Ardington & Case, 2009; Tomita & Burns, 2013; Tomita et al., 2015b; Tomlinson et al., 2009). As has been consistently noted in the depression literature (Ardington & Case, 2009; Fernandez-Nino et al., 2014; Rai et al., 2013; Tomita & Burns, 2013; Tomita et al., 2015b; Tomlinson et al., 2009), being female was associated with higher depressive symptoms in our sample.
Limitations
There are a number limitations to this study. District boundaries changed slightly in 2011 resulting in 52 rather than 53 district councils. The 2011 boundaries were used throughout this analysis for consistency. However, in the Community Survey 2007, data below the municipality level was not available, and district management areas within each district were grouped. This limited our ability to account for district boundary changes due to within-municipality boundary changes or changes in district management areas. However, this issue only affected districts Vhembe, Mopani, Ehlanzeni, West Rand, City of Tshwane, Waterberg, and Bojanala. Models run excluding these districts produced similar findings.
The Community Survey excluded residents of certain types of institutions and collective living quarters (Lehohla, 2008; Statistics South Africa, 2012, 2014), which may affect some district-level covariates, though the estimates from the Community Survey 2007 and Census 2011 are still very similar and highly correlated. Additionally, South African census data have been reported to have high numbers of households reporting no income (Yu, 2010). In the Census 2011, about 15% of households reported no income, and in the Community Survey 2007 nearly 13% reported no income. In the NIDS sample, however, less than 1% of households had zero income in the fully imputed data, suggesting that while census data sources may be the most reliable and representative at subnational levels, unlike detailed economic surveys, they may not capture all sources of income. Thus, Gini coefficients may appear higher in census sources. Nevertheless, we do not expect these households to be distributed differentially across census datasets, and therefore this should not bias our results.
An additional consideration is that the Gini coefficients used in this study were based on pre-tax income available in the Census and Community Survey, but it is possible that comparisons of post-tax income are more relevant. However, in sensitivity analyses using Gini coefficients calculated from the NIDS survey, which estimates post-tax household income, estimates still failed to support our hypothesis.
The question of how well the CES-D-10 performs in this sample and others should also be considered (Cole, Rabin, Smith, & Kaufman, 2004). Our standardized measures of internal consistency for the CES-D-10 were around 0.75 in this sample, which is lower than has been recorded in other studies (Bjorgvinsson et al., 2013; Meffert et al., 2015). When we excluded the two reverse-coded items (happiness and hope), standardized Cronbach's alpha values increased to 0.84 in Wave 1 and 0.80 in Wave 3. However, even with depressive symptoms scores excluding the items on hope and happiness, our results showed the same patterns as those reported here.
It is worth noting that the 2010 FIFA World Cup for association football/soccer took place in South Africa in the middle of the study period. Mega-events such as the World Cup may have effects on the local economy as well as quality of life (du Plessis & Maennig, 2011; Kaplanidou et al., 2013). If any such effects are lasting and not uniform across districts, this could bias our results. However, while inequality levels appeared slightly higher and seemed to have a smaller increase in the nine mostly urban districts with World Cup venues, depressive scores were similar at both time points, and fixed-effects models excluding those districts continued to produce non-significant results for the association between income inequality and depressive symptoms, even with similar standard errors.
A major limitation of the study is that due to attrition and missing data, the sample may not be representative of the South African population, and there may be risk of selection bias. At baseline, those excluded from the sample differed from those included in the sample on several demographics including education levels, marital status, and income. However, those excluded from the sample did not differ significantly from those included in terms of CES-D-10 scores at baseline (see Appendix D). Nevertheless, it is possible, for example, that in Wave 3, people who were missing or who did not complete the CES-D-10 scale had higher depressive symptomatology, which could account for the apparent decline in depression scores over time; furthermore, people who moved may have done so for reasons related to the exposure or outcome. However, sensitivity analyses applying NIDS panel weights that account for and adjust for attrition over time produced qualitatively similar results to those presented here. Moreover, we conducted sensitivity analyses to address missing data by using an “intent-to-treat” method for the exposure (Modern Epidemiology, 2008), in which all panel members, including those who moved or had missing district information at follow-up, were treated as though they remained in their original district. To address missingness in the outcome variable, we ran sensitivity analyses assuming two extremes, a “worst-case” and “best-case” scenario, in order to estimate the bounds for the range of associations that might be observed in the data. One scenario was that all those with missing or incomplete CES-D-10 scores had the highest CES-D-10 score possible (30), and the other was that all those with missing or incomplete CES-D-10 scores had the lowest CES-D-10 score possible (0). In each scenario, using an intent-to-treat method for the exposure, fixed-effects models continued to show no association between changes in income inequality and changes in depressive symptoms.
Finally, while the fixed-effects design helps to reduce the risk of confounding by controlling for all unmeasured time-constant factors, the possibility of unmeasured time-varying confounding still remains. Therefore, causal interpretations cannot be made.
Conclusion
In conclusion, our study used a longitudinal, fixed-effects design in a large sample from a highly unequal African country to examine whether changes in district income inequality were associated with changes in depressive symptoms, while controlling for individual-level factors. Our results suggest that changes in income inequality during this time period were not associated with depressive symptoms in the middle-income country of South Africa. Future research exploring longer lag periods, effect modifiers, other geographic levels, and measures of inequality which provide more information about the shape of the income distribution, may provide additional insights. As they stand, however, our results do not provide support for the income inequality hypothesis.
Supplementary Material
Highlights.
District income inequality increased on average in South Africa from 2007 to 2011.
Depressive symptoms decreased among NIDS sample members between 2008 and 2012.
Changes in district inequality were not associated with changes in depressive symptoms.
Acknowledgments
Kafui Adjaye-Gbewonyo received training-grant support from National Research Service Award T32 HL 098048I CVD Epidemiology Training Program in Behavior, the Environment and Global Health, as well as the Initiative for Maximizing Student Diversity GM055353-13 through the National Institutes of Health. Mauricio Avendano was supported by the European Research Council (ERC) (grant No 263684), the National Institute on Aging (Award Numbers R01AG040248, R01AG037398), and the European Union's Horizon 2020 research and innovation programme under grant agreement No. 667661. The authors would also like to acknowledge Simo Goshev and the other members of Data Science Services at Institute for Quantitative Social Science at Harvard University for support with statistical questions; Stata Technical Support for assistance with Stata-related queries; and Michelle Chinhema and the rest of the NIDS team for support with data questions.
Contributor Information
Kafui Adjaye-Gbewonyo, Email: kafuig@post.harvard.edu.
Mauricio Avendano, Email: mavendan@hsph.harvard.edu.
S. V. Subramanian, Email: svsubram@hsph.harvard.edu.
Ichiro Kawachi, Email: ikawachi@hsph.harvard.edu.
References
- Adjaye-Gbewonyo K, Kawachi I. Use of the Yitzhaki Index as a test of relative deprivation for health outcomes: a review of recent literature. Social Science and Medicine. 2012;75(1):129–137. doi: 10.1016/j.socscimed.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Ahern J, Galea S. Social context and depression after a disaster: the role of income inequality. Journal of Epidemiology and Community Health. 2006;60(9):766–770. doi: 10.1136/jech.2006.042069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaba O, Chola L. The social determinants of multimorbidity in South Africa. International Journal for Equity in Health. 2013;12:63. doi: 10.1186/1475-9276-12-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. International Review of Psychiatry. 2014;26(4):392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Ardington C, Case A. Health: Analysis of the NIDS Wave 1 Dataset: National Income Dynamics Study 2009 [Google Scholar]
- Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- Berkman LF, Kawachi I. A Historical Framework for Social Epidemiology: Social Determinants of Population Health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social Epidemiology. Second. New York: Oxford University Press; 2014. pp. 1–16. [Google Scholar]
- Berkman LF, Krishna A. Social Network Epidemiology. In: Berkman LF, Kawachi I, Glymour MM, editors. Social Epidemiology. Second. New York: Oxford University Press; 2014. pp. 234–289. [Google Scholar]
- Bhorat H, van der Westhuizen C, Jacobs T. Income and Non-Income Inequality in Post-Apartheid South Africa: What Are the Drivers and Possible Policy Interventions. 2009 Retrieved from South Africa. [Google Scholar]
- Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- Bouffard L, Dubé M. L'inégalité de revenus : un « virus » qui affecte la santé mentale et le bonheur. Sante Mentale Au Quebec. 2013;38(2):215. doi: 10.7202/1023997ar. [DOI] [PubMed] [Google Scholar]
- Bradlow B, Bolnick J, Shearing C. Housing, institutions, money: the failures and promise of human settlements policy and practice in South Africa. Environment and Urbanization. 2011;23(1):267–275. [Google Scholar]
- Burns JK. Poverty, inequality and a political economy of mental health. Epidemiology and Psychiatric Sciences. 2015;24(2):107–113. doi: 10.1017/S2045796015000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK, Esterhuizen T. Poverty, inequality and the treated incidence of first-episode psychosis: an ecological study from South Africa. Social Psychiatry and Psychiatric Epidemiology. 2008;43(4):331–335. doi: 10.1007/s00127-008-0308-2. [DOI] [PubMed] [Google Scholar]
- Chiavegatto Filho AD, Kawachi I, Wang YP, Viana MC, Andrade LH. Does income inequality get under the skin? A multilevel analysis of depression, anxiety and mental disorders in Sao Paulo, Brazil. Journal of Epidemiology and Community Health. 2013;67(11):966–972. doi: 10.1136/jech-2013-202626. [DOI] [PubMed] [Google Scholar]
- Cifuentes M, Sembajwe G, Tak S, Gore R, Kriebel D, Punnett L. The association of major depressive episodes with income inequality and the human development index. Social Science and Medicine. 2008;67(4):529–539. doi: 10.1016/j.socscimed.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Cohen PN. Gini Code. N.d. Retrieved from http://www.terpconnect.umd.edu/∼pnc/gini.sas.
- Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychol Assess. 2004;16(4):360–372. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- Cummings P. Methods for estimating adjusted risk ratios. The Stata Journal. 2009;9(2):175–196. [Google Scholar]
- Day C, Barron P, Massyn N, Padarath A, English R. District Health Barometer 2010/11. Durban: Health Systems Trust; 2012. [Google Scholar]
- Day C, Gray A, Budgell E. Health and Related Indicators. In: Padarath A, English R, editors. South African Health Review 2011. Durban: Health Systems Trust; 2011. [Google Scholar]
- De Villiers L, Brown M, Woolard I, Daniels R, Leibbrandt M. National Income Dynamics Study Wave 3 User Manual. Cape Town: Southern Africa Labour and Development Research Unit; 2014. [Google Scholar]
- du Plessis S, Maennig W. The 2010 FIFA World Cup high-frequency data economics: Effects on international tourism and awareness for South Africa. Development Southern Africa. 2011;28(3):349–365. doi: 10.1080/0376835x.2011.595994. [DOI] [Google Scholar]
- Fernandez-Nino JA, Manrique-Espinoza BS, Bojorquez-Chapela I, Salinas-Rodriguez A. Income inequality, socioeconomic deprivation and depressive symptoms among older adults in Mexico. PLoS One. 2014;9(9):e108127. doi: 10.1371/journal.pone.0108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour MM, Avendano M, Kawaachi I. Socioeconomic Status and Health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Second. New York: Oxford University Press; 2014. pp. 17–62. [Google Scholar]
- Goodman E, Huang B, Wade TJ, Kahn RS. A multilevel analysis of the relation of socioeconomic status to adolescent depressive symptoms: does school context matter? The Journal of Pediatrics. 2003;143(4):451–456. doi: 10.1067/S0022-3476(03)00456-6. [DOI] [PubMed] [Google Scholar]
- Gresenz CR, Sturm R, Tang L. Income and Mental Health: Unraveling Community and Individual Level Relationships. The Journal of Mental Health Policy and Economics. 2001;4:197–203. [PubMed] [Google Scholar]
- Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. European Heart Journal. 2014;35(21):1365–1372. doi: 10.1093/eurheartj/eht462. [DOI] [PubMed] [Google Scholar]
- Henderson C, Liu X, Diez Roux AV, Link BG, Hasin D. The effects of US state income inequality and alcohol policies on symptoms of depression and alcohol dependence. Social Science and Medicine. 2004;58(3):565–575. doi: 10.1016/s0277-9536(03)00228-4. [DOI] [PubMed] [Google Scholar]
- Hiilamo H. Is income inequality ‘toxic for mental health’? An ecological study on municipal level risk factors for depression. PLoS One. 2014;9(3):e92775. doi: 10.1371/journal.pone.0092775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong J, Knapp M, McGuire A. Income-related inequalities in the prevalence of depression and suicidal behaviour: a 10-year trend following economic crisis. World Psychiatry. 2011;10:40–44. doi: 10.1002/j.2051-5545.2011.tb00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplanidou K, Karadakis K, Gibson H, Thapa B, Walker M, Geldenhuys S, Coetzee W. Quality of Life, Event Impacts, and Mega-Event Support among South African Residents before and after the 2010 FIFA World Cup. Journal of Travel Research. 2013;52(5):631–645. [Google Scholar]
- Kawachi I, Berkman L. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Subramanian SV. Income Inequality. In: Berkman LF, Kawachi I, Glymour MM, editors. Social Epidemiology. Second. New York: Oxford University Press; 2014. pp. 126–152. [Google Scholar]
- Kim D, Kawachi I, Hoorn SV, Ezzati M. Is inequality at the heart of it? Cross- country associations of income inequality with cardiovascular diseases and risk factors. Social Science and Medicine. 2008;66(8):1719–1732. doi: 10.1016/j.socscimed.2007.12.030. [DOI] [PubMed] [Google Scholar]
- Lehohla P. Community Survey 2007 Unit Records Metadata. Pretoria: Statistics South Africa; 2008. [Google Scholar]
- Leibbrandt M, Finn A, Woolard I. Describing and decomposing post-apartheid income inequality in South Africa. Development Southern Africa. 2012;29(1):19–34. [Google Scholar]
- The Local Government System in South Africa. 2009 Retrieved from http://www.kunnat.net/fi/palvelualueet/projektit/pohjoinen-etela/kuntatietoa/etela_afrikka/Documents/The%20Local%20Government%20System%20in%20South%20Africa.doc.
- Lumley T, Kronmal R, Ma S. Relative Risk Regression in Medical Research: Models, Contrasts, Estimators, and Algorithms. UW Biostatistics Working Paper Series 2006 [Google Scholar]
- Lund C. Poverty, inequality and mental health in low- and middle-income countries: time to expand the research and policy agendas. Epidemiology and Psychiatric Sciences. 2015;24(2):97–99. doi: 10.1017/S2045796015000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Kleintjes S, Kakuma R, Flisher AJ Consortium, M. H. R. P. Public sector mental health systems in South Africa: inter-provincial comparisons and policy implications. Social Psychiatry and Psychiatric Epidemiology. 2010;45(3):393–404. doi: 10.1007/s00127-009-0078-5. [DOI] [PubMed] [Google Scholar]
- Lynch J, Kaplan G. Socioeconomic Position. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- Massyn N, Day C, Peer N, Padarath A, Barron P, English R. District Health Barometer 2013/14. Durban: Health Systems Trust; 2014. [Google Scholar]
- Meffert SM, McCulloch CE, Neylan TC, Gandhi M, Lund C. Increase of perceived frequency of neighborhood domestic violence is associated with increase of women's depression symptoms in a nationally representative longitudinal study in South Africa. Social Science and Medicine. 2015;131:89–97. doi: 10.1016/j.socscimed.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messias E, Eaton WW, Grooms AN. Economic grand rounds: Income inequality and depression prevalence across the United States: an ecological study. Psychiatric Services. 2011;62(7):710–712. doi: 10.1176/ps.62.7.pss6207_0710. [DOI] [PubMed] [Google Scholar]
- Minnesota Population Center. Integrated Public Use Microdata Series, International: Version 6.2. 2013 [Machine-readable database]. from University of Minnesota. [Google Scholar]
- Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3rd. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- Muramatsu N. County-Level Income Inequality and Depression among Older Americans. HSR: Health Services Research. 2003;38(6):1863–1884. doi: 10.1111/j.1475-6773.2003.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Abdalla S. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2013;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Naledi T, Barron P, Schneider H. Primary Health Care in SA Since 1994 and Implications of the New Vision for PHC Re-Engineering. In: Padarath A, English R, editors. South African Health Review 2011. Durban: Health Systems Trust; 2011. [Google Scholar]
- National Income Dynamics Study. What is NIDS. 2014 Retrieved from http://www.nids.uct.ac.za/about/what-is-nids.
- OECD. OECD Economic Surveys: South Africa 2013. Paris: OECD Publishing; 2013. [Google Scholar]
- Pabayo R, Kawachi I, Gilman SE. Income inequality among American states and the incidence of major depression. Journal of Epidemiology and Community Health. 2014;68(2):110–115. doi: 10.1136/jech-2013-203093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabayo R, Kawachi I, Gilman SE. US State-level income inequality and risks of heart attack and coronary risk behaviors: longitudinal findings. International Journal of Public Health. 2015;60(5):573–588. doi: 10.1007/s00038-015-0678-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol. 2008;8:9. doi: 10.1186/1471-2288-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Social Science and Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Rai D, Zitko P, Jones K, Lynch J, Araya R. Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. British Journal of Psychiatry. 2013;202(3):195–203. doi: 10.1192/bjp.bp.112.112482. [DOI] [PubMed] [Google Scholar]
- Rasella D, Aquino R, Barreto ML. Impact of income inequality on life expectancy in a highly unequal developing country: the case of Brazil. Journal of Epidemiology and Community Health. 2013;67(8):661–666. doi: 10.1136/jech-2012-201426. [DOI] [PubMed] [Google Scholar]
- Rumsfeld JS, Ho PM. Depression and cardiovascular disease: a call for recognition. Circulation. 2005;111(3):250–253. doi: 10.1161/01.CIR.0000154573.62822.89. [DOI] [PubMed] [Google Scholar]
- Shi L, Starfield B, Politzer R, Regan J. Primary Care, Self-rated Health, and Reductions in Social Disparities in Health. HSR: Health Services Research. 2002;37(3):529–550. doi: 10.1111/1475-6773.t01-1-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2008, Wave 1 [dataset] Version 5.2. 2014a Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2010-2011, Wave 2 [dataset] Version 2.2. 2014b Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2012, Wave 3 [dataset] Version 1.2. 2014c Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Statistics South Africa. Census 2001: Metadata. Pretoria: Statistics South Africa; 2003. [Google Scholar]
- Statistics South Africa. Census 2011 Statistical Release - P0301.4. Pretoria: Statistics South Africa; 2012. [Google Scholar]
- Statistics South Africa. Census 2011 10% Sample Metadata. Pretoria: Statistics South Africa; 2014a. [Google Scholar]
- Statistics South Africa. South Africa - South African Census 2011 v1.1 [MRDF] 2014b Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Steptoe A, Tsuda A, Tanaka Y, Wardle J. Depressive Symptoms, Socio-Economic Background, Sense of Control, and Cultural Factors in University Students from 23 Countries. International Journal of Behavioral Medicine. 2007;14(2):97–107. doi: 10.1007/BF03004175. [DOI] [PubMed] [Google Scholar]
- Sturm R, Gresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ: British Medical Journal. 2002;324(7328):20. doi: 10.1136/bmj.324.7328.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Kawachi I, Smith GD. Income inequality and the double burden of under- and overnutrition in India. Journal of Epidemiology and Community Health. 2007;61(9):802–809. doi: 10.1136/jech.2006.053801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Burns JK. A multilevel analysis of association between neighborhood social capital and depression: evidence from the first South African National Income Dynamics Study. Journal of Affective Disorders. 2013;144(1-2):101–105. doi: 10.1016/j.jad.2012.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Labys CA, Burns JK. Depressive Symptoms Prior to Pregnancy and Infant Low Birth Weight in South Africa. Maternal and Child Health Journal. 2015a doi: 10.1007/s10995-015-1732-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Labys CA, Burns JK. A multilevel analysis of the relationship between neighborhood social disorder and depressive symptoms: evidence from the South African National Income Dynamics Study. American Journal of Orthopsychiatry. 2015b;85(1):56–62. doi: 10.1037/ort0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Grimsrud AT, Stein DJ, Williams DR, Myer L. The epidemiology of major depression in South Africa: Results from the South African Stress and Health study. South African Medical Journal. 2009;99(5):368–373. [PMC free article] [PubMed] [Google Scholar]
- van der Berg S. Current poverty and income distribution in the context of South African history. Economic History of Developing Regions. 2011;26(1):120–140. [Google Scholar]
- Weich S, Lewis G, Jenkins SP. Income inequality and the prevalence of common mental disorders in Britain. British Journal of Psychiatry. 2001;178:222–227. doi: 10.1192/bjp.178.3.222. [DOI] [PubMed] [Google Scholar]
- Williams DR, Herman A, Stein DJ, Heeringa SG, Jackson PB, Moomal H, Kessler RC. Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychological Medicine. 2008;38(2):211–220. doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. GINI index (World Bank estimate) 2016 Retrieved from http://data.worldbank.org/indicator/SI.POV.GINI?order=wbapi_data_value_2011+wbapi_data_value+wbapi_data_value-first&sort=desc.
- Yu D. Stellenbosch Economic Working Papers. Stellenbosch: University of Stellenbosch; 2010. Poverty and inequality trends in South Africa using different survey data. [Google Scholar]
- Zimmerman FJ, Bell JF. Income inequality and physical and mental health: testing associations consistent with proposed causal pathways. Journal of Epidemiology and Community Health. 2006;60(6):513–521. doi: 10.1136/jech.2005.040154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, O'Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, et al. Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


