Abstract
We recently reported that targeted deletion of Pannexin 1 in neural precursor cells of the ventricular zone impairs the maintenance of these cells in healthy and stroke-injured brain. Here we frame this exciting new finding in the context of our previous studies on Pannexin 1 in neural precursors as well as the close relationship between Pannexin 1 and purinergic receptors established by other groups. Moreover, we identify important gaps in our understanding of Pannexin 1 in neural precursor cell biology in terms of the underlying molecular mechanisms and functional/behavioural outcomes.
Keywords: neural precursor, ventricular zone, pannexin, ATP, cytoskeleton, proliferation, phagoptosis
Introduction
Pannexin 1 (Panx1) was discovered in 2000 (Panchin et al., 2000) through moderate sequence homology with invertebrate gap junction forming proteins, the innexins. Although the molecular mechanisms underlying Panx1 activation and modulation have not yet been fully characterized, work from various groups has identified several means, such as membrane depolarization, mechanical deformation and caspase cleavage of the C-terminal tail (reviewed in Chiu et al., 2014). Work in a variety of systems has established that Panx1 facilitates adenosine triphosphate (ATP) release (e.g. Bao et al., 2004; Schenk et al., 2008; Ransford et al., 2009), and can pass other ions and metabolites up to 1 kDa in size, likely through its activity as a single membrane channel (Sosinsky et al., 2011). Based on foundational work that ATP is a critical signalling molecule in ventricular zone (VZ) neural precursor cells (NPCs), through the activation of various purinergic (P2) receptors (recently reviewed in Cavaliere et al., 2015), our group investigated and established the expression of Panx1 in VZ NPCs in vitro (recently confirmed by Talaveron et al., 2015), where it regulates NPC proliferation, differentiation and migration (Wicki-Stordeur et al., 2012; Wicki-Stordeur and Swayne, 2013). Building on these discoveries, we recently reported our in vivo findings on the role of Panx1 in the VZ (Wicki-Stordeur et al., 2016). We deleted Panx1 in NPCs using an approach that consisted of intracerebroventricular injection of control and Cre-recombinase retroviruses co-expressing different fluorescent markers (Tashiro et al., 2006) in Panx1 floxed mice. This strategy allowed us to study NPC “maintenance” since we were able to monitor both Panx1-null and Panx1-expressing NPCs in the same environment over time. Deletion of Panx1 impaired NPC maintenance in the VZ niche, both in healthy and stroke-injured tissue. In contrast, Panx1-null VZ NPCs that had migrated to the peri-infarct cortex exhibited improved maintenance compared with Panx1-expressing NPCs. These results suggest that Panx1 is a key regulator of NPC biology, but there are several outstanding questions with respect to mechanism. For example, does Panx1 influence NPC biology through its channel function (ATP release, ion fluxes), or protein-protein interactions, or a combination of both? While the jury is still out on Panx1 ion selectivity (several reports suggest it is anion-selective, while others suggest it non-selectively passes anions and cations (reviewed in Chiu et al., 2014), we are currently undertaking experiments to investigate how exactly Panx1 regulates NPC biology. Here we review links between Panx1 and the regulation of NPCs biology from the existing literature. These include interactions with purinergic signalling and interactions with the cytoskeleton, which we outline below. Finally, we conclude with a discussion of another important outstanding question arising from this work: what might be the behavioural implications of Panx1 regulation of VZ NPCs?
Interactions with Purinergic Signalling
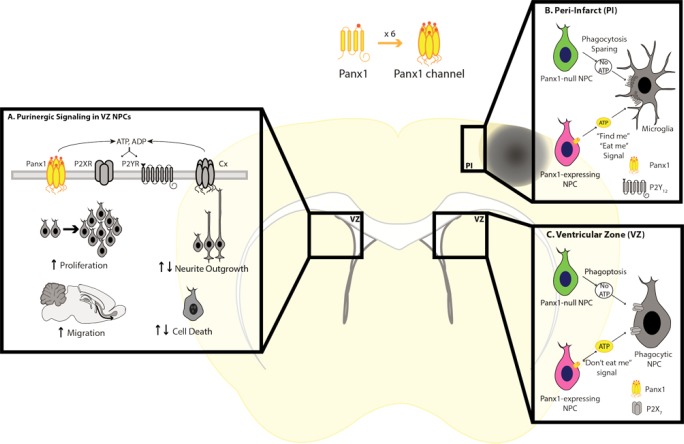
Several functional interactions between Panx1 and purinergic signalling have been described (reviewed in Baroja-Mazo et al., 2013) that could be related to this intriguing role of Panx1 in NPCs in the postnatal VZ and peri-infarct cortex (Figure 1). Panx1 facilitates the release of ATP and other nucleotides from a variety of cell types (reviewed in Lohman and Isakson, 2014), including NPCs in vitro (Wicki-Stordeur et al., 2012). ATP, in turn, binds to P2 receptors to elicit ionotropic (P2X) or metabotropic (P2Y) responses, which have been described to play a role in shaping NPC biology in a variety of ways. This work has been extensively reviewed elsewhere (Zimmermann, 2011; Cavaliere et al., 2015). Moreover, there is a reciprocal regulation of Panx1 by P2 receptors, in which P2 receptor activity elicits Panx1 channel activation, likely through increases in intracellular Ca2+ (Locovei et al., 2006; Pelegrin and Surprenant, 2006; Iglesias et al., 2008). Additionally, in certain cell types Panx1 forms a physical association with P2X7 (reviewed in Pelegrin and Surprenant, 2009; Boyce et al., 2014; Chiu et al., 2014). Early reports suggested a role for Panx1 as the large-pore component in the di-phasic activation of P2X7 (Pelegrin and Surprenant, 2006, 2007) but more recent studies found P2X7 large pore activity persisted in the absence of Panx1 (i.e., dye uptake persisted in the Panx1-/- scenario (Qu et al., 2011; Chiu et al., 2014)), suggesting there could be other factors that shape the Panx1/P2X7 relationship that are cell type and/or P2X7 isoform specific.
Figure 1.
Panx1 interaction with purinergic signalling and role in neural precursor cells (NPCs) in the ventricular zone (VZ) and peri-infarct cortex (PI).
(A) By facilitating adenosine triphosphate (ATP) release, Panx1 interaction with P2 receptors plays critical roles in NPC cellular behaviours. (B) In the peri-infarct cortex, deletion of Panx1 spares NPCs from phagocytic clearance by microglia, a process that involves P2Y12 receptors. (C) Within the ventricular zone, phagocytic NPCs with scavenger P2X7 receptors clear local NPCs; this mechanism is inhibited by ATP (“don’t eat me” signal) and therefore loss of Panx1 in NPCs makes them susceptible to elimination through “phagoptosis”. ADP: Adenosine diphosphate.
An intriguing new mode by which purinergic signalling regulates NPC maintenance has recently come to light that we have incorporated into our working model (Figure 1). According to this model, it is the expression of different purinergic receptors on different phagocytic cells in the VZ vs. the peri-infarct cortex environments that, in effect, “switches” the outcome of a Panx1-mediated ATP signal. In the healthy postnatal VZ, large numbers of NPCs are normally lost (Morshead and van der Kooy, 1992), likely through phagocytic clearance by neighbouring NPCs (Lu et al., 2011). This represents a newly recognized form of cell death known as “phagoptosis”, where the inability to display “don’t eat me” signals by cells results in their elimination (Brown and Neher, 2012). Phagocytic NPCs are regulated by a non-canonical P2X7-dependant mechanism that is inhibited by extracellular ATP (Lovelace et al., 2015). ATP dissociates the physical interaction between P2X7 and nonmuscle myosin heavy chain IIA, which is essential for the innate phagocytosis/scavenger function of P2X7 as shown both in vitro and in vivo (Gu et al., 2009, 2010, 2011). These recent findings along with the previously defined role of purinergic signalling in NPC maintenance and differentiation (Cavaliere et al., 2015), suggest that ATP could act as a survival (“do not eat me”) signal in the VZ. It has been well established that ATP is episodically released from VZ NPCs (for example see Lin et al., 2007). In our model, we propose that Panx1 represents a major mechanism for episodic ATP release. The model based on our experimental findings proposes that deletion of Panx1 (which facilitates the release of “don’t-eat-me ATP) renders NPCs susceptible to clearance via phagoptosis (Figure 1), accounting for the low number of Panx1 null NPCs observed in the VZ. Conversely, previous work has also shown that in the peri-infarct cortex, ATP acts as a “find-me/eat-me” signal (Patel et al., 2013) through the activation of microglial P2Y12 receptors. Therefore, the presence of Panx1 in NPCs that migrated into the peri-infarct cortex would render them vulnerable to phagoptosis (via mediating release of ATP, now acting as a “find-me/eat-me” signal). In summary, our model proposes that ATP acts as a “don’t-eat-me signal in the VZ, by disrupting physiological P2X7-mediated phagoptosis, while it acts as a “find-me/eat-me” signal in the peri-infarct cortex though activation of metabotropic puringergic receptors on microglia.
Future studies are now needed to address this putative role of Panx1 in regulating phagoptosis of NPCs in the VZ and peri-infarct cortex, as well as establish the precise molecular mechanisms involved in order to determine how this information could be used to strategize treatment paradigms seeking to improve outcomes after a stroke. Our results already suggest that it could be appropriate to target Panx1 in the peri-infarct cortex, perhaps coupling this intervention with other known ways to potentiate NPCs (such as supplementation of growth factors) that have proved to produce objective behavioural improvements in stroke models (Christie and Turnley, 2012). Moreover, the contributions of other ATP-release channels (i.e., LRRC8A, the maxi-anion channel, connexin hemi-channels, and CALHM1 (Sabirov and Okada, 2005; Abascal and Zardoya, 2012; Taruno et al., 2013; Burow et al., 2015)) to phagoptosis could also be investigated.
Interactions with the Cytoskeleton
Apart from the association with purinergic signaling, there are additional possible ways by which Panx1 function could regulate NPC maintenance in the VZ. Foundational work on the cellular and molecular biology of the channel revealed actin is not only critical for Panx1 trafficking and stability in the membrane but also binds directly to its C-terminus (Bhalla-Gehi et al., 2010). Additionally, we also have identified a large number of putative Panx1-interacting proteins in Neuro-2a (N2a) cells using immunoprecipitation coupled to mass spectrometry (Wicki-Stordeur and Swayne, 2013). We validated an interaction between Panx1 and actin, as well as the microfilament-associated protein Arp3 (from the Arp 2/3 complex), and reported that at least 10% of all identified Panx1 protein interaction partners fell under the GO term ‘Cytoskeleton’ (Wicki-Stordeur and Swayne, 2013). Associations with the cytoskeleton provide stability to plasma membrane populations of Panx1 (Bhalla-Gehi et al., 2010), and likely underlie its mechanosensitive nature (Bao et al., 2004; Seminario-Vidal et al., 2011). Whether Panx1 reciprocally regulates cytoskeleton function in NPCs is unknown; however, in other cell types, ATP released via Panx1 modulates actomyosin cytoskeleton dynamics (Bao et al., 2012), and reductions in Panx1 expression alter levels of the intermediate filament protein, vimentin (Penuela et al., 2012). Since cytoskeletal processes are key components of NPC maintenance, regulating behaviours such as cell division and fate specification (reviewed in Lian and Sheen, 2015; Mora-Bermudez and Huttner, 2015), it is feasible to suggest that Panx1 may act, in part, through cytoskeletal remodelling, to affect NPC maintenance. Future studies will investigate the molecular determinants of novel interactions, and explore the potential interplay with channel function.
Given the strong association between Panx1 and proteins involved in cell maintenance, it is notable that we detected no changes in the proliferation of Panx1-null NPCs via Ki67 immunoreactivity. Yet, it is possible that Panx1 deletion altered the cell cycle in such a way as to obscure differences in the Ki67 signal (reviewed in Scholzen and Gerdes, 2000). For example, if Panx1 deletion caused cell cycle elongation or stalling within an active phase (G1, S, G2), rather than cell cycle exit (G0), these Panx1-null NPCs would remain Ki67-positive, but possess limited proliferative capacity when compared to their Panx1-expressing counterparts. It is also possible that at the time of our analyses, the small number of remaining Panx1-null NPCs had recovered from, or had become resistant to the effects of Panx1 deletion, perhaps through compensatory mechanisms (Lohman and Isakson, 2014), or normal heterogeneity of gene expression within the NPC population (Johnson et al., 2015). Future studies addressing the role of Panx1 in cell proliferation in NPCs in vivo could assess additional cell cycle or proliferation markers (e.g. BrdU), alternative time points following Panx1 deletion, and/or analyses of cell cycle length.
Behavioural Implications
Our study raised additional exciting questions. For example, might Panx1 also regulate VZ NPC behaviours during development? A correlation exists between Panx1 expression levels and the proliferative capacity of VZ NPCs, both of which are extremely robust during early brain development and decline with age (Ray et al., 2005; Conover and Shook, 2011). While current Panx1 knock-out models do not exhibit overt defects and can readily reproduce, a recent study reported the first human disease linked to a reduced-function variant of PANX1 (Shao et al., 2016). The affected individual demonstrated significant developmental abnormalities including severe intellectual disability. Although behavioural characterization of constitutive Panx1 knock-out models remains far from exhausted, behavioural dysfunction detected so far includes a tendency to anxiety-related responses and hippocampus-dependent memory impairments, the latter possibly explained by the potently increased long term potentiation (LTP) and reducedlong term depression (LTD) observed in the absence of Panx1 (Prochnow et al., 2012; Ardiles et al., 2014). The contrast between the severe abnormalities found in the human case carrying the reduced-function variant of PANX1 and the constitutive Panx1 knock-out mice could be explained by development of compensatory mechanisms or redundancy of biological systems (Penuela et al., 2013; Bond and Naus, 2014). Considering the enriched expression of Panx1 in the brain encompasses pyramidal cells and interneurons (especially parvalbumin-positive cells) in the cerebral cortex and hippocampus, as well as Purkinje cells in the cerebellum (Ray et al., 2005; Vogt et al., 2005; Zoidl et al., 2007), generation of conditional and/or inducible Panx1 knock-outs, or knock-in of the reduced-function mutant, will help to enable precise analyses of age- and cell-type dependent effects of Panx1. This includes potentially investigating the effects of Panx1 deletion in hippocampal NPCs. We demonstrated Panx1 expression in hippocampal neurosphere cultures (Wicki-Stordeur et al., 2012), yet this has not been further investigated in vivo. In light of the fact that most behavioural abnormalities tested in Panx1 knock-out models are hippocampus-dependent, the implications of Panx1 in hippocampal NPC biology, in health and injury, represents an potentially important area of future study.
It should also be noted that the mouse model used (Dvoriantchikova et al., 2012) in our study also contains a passenger mutation that inactivates caspase-11, also known as caspase-4 and Ich-3 (Vanden Berghe et al., 2015). Because there is virtually no detectable caspase-11 expression in the brain under basal conditions (Wang et al., 1996; Van de Craen et al., 1997), it is difficult to know how this would affect our results in the uninjured control mice where there is not any caspase-11 activation, if it were present, and we see a robust effect of knocking out Panx1. We cannot rule out the possibility, however, that caspase-11 could be upregulated after stroke or other brain injury. That said, a major strength of our experimental paradigm was that it allowed comparison of Panx1-nulll and Panx1-expressing NPCs within the same animal (and therefore same conditions and environment), rather than comparisons between Panxl knock-out and wild type animals on different backgrounds. Still, future studies could examine whether caspase-11 is appreciably expressed or up-regulated in NPCs following brain injury.
We also have yet to determine the behavioural consequences of Panx1 deletion from VZ NPCs. Although the constitutive Panx1 knock-out models have thus far demonstrated few obvious defects, a recent study found impaired olfactory learning in Panx1 deficient mice (Kurtenbach et al., 2014). This is interesting given that adult-born VZ NPCs migrate to the olfactory bulb (OB) in rodents, where they differentiate and specialize into OB interneurons (for review see Lledo et al., 2006; Ming and Song, 2011). Adult-born neurons are also found in the piriform and entorhinal cortices (Shapiro et al., 2009), with the latter sending direct projections to the hippocampus where olfactory and emotional information are consolidated (Kaut et al., 2003). Impaired addition of adult-born neurons to these OB networks results in impoverished odour discrimination and odour-associated perceptual learning (Moreno et al., 2009). It is feasible to suggest that Panx1 deletion from VZ NPCs could similarly reduce addition of OB neurons, given that Panx1 promotes NPC maintenance within the VZ. Thus, behavioural tests directed towards odour discrimination, learning, memory and spatial navigation tasks, in combination with genetic manipulations, may help to determine the functional impact of Panx1 on VZ NPCs.
Concluding Remarks
Panx1 represents a novel molecular player in brain plasticity and neural regeneration thanks to its enrichment in the central nervous system and interactions with purinergic and cytoskeletal signalling. Future studies unraveling molecular mechanisms and investigating its potential role in phagoptosis and animal behaviour will help us to better understand the role of this channel in NPC homeostasis and neuronal development.
Footnotes
Funding: Research in the Swayne lab was supported by operating grants to LAS from the Natural Sciences and Engineering Research Council of Canada (NSERC Discovery Grant), the Canadian Institutes of Health Research (CIHR Grant MOP142215), The Scottish Rite Charitable Foundation of Canada and the University of Victoria Division of Medical Sciences and by infrastructure grants from the Canadian Foundation for Innovation (CFI) and the British Columbia Knowledge Development Fund (BCKDF). LAS was supported by a Michael Smith Foundation for Health Research and British Columbia Schizophrenia Society Foundation Scholar Award. JCSA was supported by a University of Victoria Fellowship Graduate Award. LEWS was supported by a Vanier Canada Graduate Scholarship (NSERC).
Conflicts of interest: None declared.
References
- Abascal F, Zardoya R. LRRC8 proteins share a common ancestor with pannexins, and may form hexameric channels involved in cellcell communication. Bioessays. 2012;34:551–560. doi: 10.1002/bies.201100173. [DOI] [PubMed] [Google Scholar]
- Ardiles AO, Flores-Munoz C, Toro-Ayala G, Cardenas AM, Palacios AG, Munoz P, Fuenzalida M, Saez JC, Martinez AD. Pannexin 1 regulates bidirectional hippocampal synaptic plasticity in adult mice. Front Cell Neurosci. 2014;8:326. doi: 10.3389/fncel.2014.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao BA, Lai CP, Naus CC, Morgan JR. Pannexin1 drives multicellular aggregate compaction via a signaling cascade that remodels the actin cytoskeleton. J Biol Chem. 2012;287:8407–8416. doi: 10.1074/jbc.M111.306522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao L, Locovei S, Dahl G. Pannexin membrane channels are mechanosensitive conduits for ATP. FEBS Lett. 2004;572:65–68. doi: 10.1016/j.febslet.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Baroja-Mazo A, Barbera-Cremades M, Pelegrin P. The participation of plasma membrane hemichannels to purinergic signaling. Biochim Biophys Acta. 2013;1828:79–93. doi: 10.1016/j.bbamem.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Bhalla-Gehi R, Penuela S, Churko JM, Shao Q, Laird DW. Pannexin1 and pannexin3 delivery, cell surface dynamics, and cytoskeletal interactions. J Biol Chem. 2010;285:9147–9160. doi: 10.1074/jbc.M109.082008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond SR, Naus CC. The pannexins: past and present. Front Physiol. 2014;5:58. doi: 10.3389/fphys.2014.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce AK, Wicki-Stordeur LE, Swayne LA. Powerful partnership: crosstalk between pannexin 1 and the cytoskeleton. Front Physiol. 2014;5:27. doi: 10.3389/fphys.2014.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GC, Neher JJ. Eaten alive! Cell death by primary phagocytosis: ‘;phagoptosis’. Trends Biochem Sci. 2012;37:325–332. doi: 10.1016/j.tibs.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Burow P, Klapperstuck M, Markwardt F. Activation of ATP secretion via volume-regulated anion channels by sphingosine-1-phosphate in RAW macrophages. Pflugers Arch. 2015;467:1215–1226. doi: 10.1007/s00424-014-1561-8. [DOI] [PubMed] [Google Scholar]
- Cavaliere F, Donno C, D’Ambrosi N. Purinergic signaling: a common pathway for neural and mesenchymal stem cell maintenance and differentiation. Front Cell Neurosci. 2015;9:211. doi: 10.3389/fncel.2015.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu YH, Ravichandran KS, Bayliss DA. Intrinsic properties and regulation of Pannexin 1 channel. Channels (Austin) 2014:8. doi: 10.4161/chan.27545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie KJ, Turnley AM. Regulation of endogenous neural stem/progenitor cells for neural repair-factors that promote neurogenesis and gliogenesis in the normal and damaged brain. Front Cell Neurosci. 2012;6:70. doi: 10.3389/fncel.2012.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conover JC, Shook BA. Aging of the subventricular zone neural stem cell niche. Aging Dis. 2011;2:49–63. [PMC free article] [PubMed] [Google Scholar]
- Dvoriantchikova G, Ivanov D, Barakat D, Grinberg A, Wen R, Slepak VZ, Shestopalov VI. Genetic ablation of Pannexin1 protects retinal neurons from ischemic injury. PLoS One. 2012;7:e31991. doi: 10.1371/journal.pone.0031991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu BJ, Saunders BM, Jursik C, Wiley JS. The P2X7-nonmuscle myosin membrane complex regulates phagocytosis of nonopsonized particles and bacteria by a pathway attenuated by extracellular ATP. Blood. 2010;115:1621–1631. doi: 10.1182/blood-2009-11-251744. [DOI] [PubMed] [Google Scholar]
- Gu BJ, Saunders BM, Petrou S, Wiley JS. P2X(7) is a scavenger receptor for apoptotic cells in the absence of its ligand, extracellular ATP. J Immunol. 2011;187:2365–2375. doi: 10.4049/jimmunol.1101178. [DOI] [PubMed] [Google Scholar]
- Gu BJ, Rathsam C, Stokes L, McGeachie AB, Wiley JS. Extracellular ATP dissociates nonmuscle myosin from P2X(7) complex: this dissociation regulates P2X(7) pore formation. Am J Physiol Cell Physiol. 2009;297:C430–439. doi: 10.1152/ajpcell.00079.2009. [DOI] [PubMed] [Google Scholar]
- Iglesias R, Locovei S, Roque A, Alberto AP, Dahl G, Spray DC, Scemes E. P2X7 receptor-Pannexin1 complex: pharmacology and signaling. Am J Physiol Cell Physiol. 2008;295:C752–760. doi: 10.1152/ajpcell.00228.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MB, Wang PP, Atabay KD, Murphy EA, Doan RN, Hecht JL, Walsh CA. Single-cell analysis reveals transcriptional heterogeneity of neural progenitors in human cortex. Nat Neurosci. 2015;18:637–646. doi: 10.1038/nn.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaut KP, Bunsey MD, Riccio DC. Olfactory learning and memory impairments following lesions to the hippocampus and perirhinal-entorhinal cortex. Behav Neurosci. 2003;117:304–319. doi: 10.1037/0735-7044.117.2.304. [DOI] [PubMed] [Google Scholar]
- Kurtenbach S, Whyte-Fagundes P, Gelis L, Kurtenbach S, Brazil E, Zoidl C, Hatt H, Shestopalov VI, Zoidl G. Investigation of olfactory function in a Panx1 knock out mouse model. Front Cell Neurosci. 2014;8:266. doi: 10.3389/fncel.2014.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian G, Sheen VL. Cytoskeletal proteins in cortical development and disease: actin associated proteins in periventricular heterotopia. Front Cell Neurosci. 2015;9:99. doi: 10.3389/fncel.2015.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JH, Takano T, Arcuino G, Wang X, Hu F, Darzynkiewicz Z, Nunes M, Goldman SA, Nedergaard M. Purinergic signaling regulates neural progenitor cell expansion and neurogenesis. Dev Biol. 2007;302:356–366. doi: 10.1016/j.ydbio.2006.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lledo PM, Alonso M, Grubb MS. Adult neurogenesis and functional plasticity in neuronal circuits. Nat Rev Neurosci. 2006;7:179–193. doi: 10.1038/nrn1867. [DOI] [PubMed] [Google Scholar]
- Locovei S, Wang J, Dahl G. Activation of pannexin 1 channels by ATP through P2Y receptors and by cytoplasmic calcium. FEBS Lett. 2006;580:239–244. doi: 10.1016/j.febslet.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Lohman AW, Isakson BE. Differentiating connexin hemichannels and pannexin channels in cellular ATP release. FEBS Lett. 2014;588:1379–1388. doi: 10.1016/j.febslet.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovelace MD, Gu BJ, Eamegdool SS, Weible MW, 2nd, Wiley JS, Allen DG, Chan-Ling T. P2X7 receptors mediate innate phagocytosis by human neural precursor cells and neuroblasts. Stem Cells. 2015;33:526–541. doi: 10.1002/stem.1864. [DOI] [PubMed] [Google Scholar]
- Lu Z, Elliott MR, Chen Y, Walsh JT, Klibanov AL, Ravichandran KS, Kipnis J. Phagocytic activity of neuronal progenitors regulates adult neurogenesis. Nat Cell Biol. 2011;13:1076–1083. doi: 10.1038/ncb2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ming GL, Song H. Adult neurogenesis in the mammalian brain: significant answers and significant questions. Neuron. 2011;70:687–702. doi: 10.1016/j.neuron.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora-Bermudez F, Huttner WB. Novel insights into mammalian embryonic neural stem cell division: focus on microtubules. Mol Biol Cell. 2015;26:4302–4306. doi: 10.1091/mbc.E15-03-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno MM, Linster C, Escanilla O, Sacquet J, Didier A, Mandairon N. Olfactory perceptual learning requires adult neurogenesis. Proc Natl Acad Sci U S A. 2009;106:17980–17985. doi: 10.1073/pnas.0907063106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morshead CM, van der Kooy D. Postmitotic death is the fate of constitutively proliferating cells in the subependymal layer of the adult mouse brain. J Neurosci. 1992;12:249–256. doi: 10.1523/JNEUROSCI.12-01-00249.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchin Y, Kelmanson I, Matz M, Lukyanov K, Usman N, Lukyanov S. A ubiquitous family of putative gap junction molecules. Curr Biol. 2000;10:R473–474. doi: 10.1016/s0960-9822(00)00576-5. [DOI] [PubMed] [Google Scholar]
- Patel AR, Ritzel R, McCullough LD, Liu F. Microglia and ischemic stroke: a double-edged sword. Int J Physiol Pathophysiol Pharmacol. 2013;5:73–90. [PMC free article] [PubMed] [Google Scholar]
- Pelegrin P, Surprenant A. Pannexin-1 mediates large pore formation and interleukin-1beta release by the ATP-gated P2X7 receptor. EMBO J. 2006;25:5071–5082. doi: 10.1038/sj.emboj.7601378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelegrin P, Surprenant A. Pannexin-1 couples to maitotoxin- and nigericin-induced interleukin-1beta release through a dye uptake-independent pathway. J Biol Chem. 2007;282:2386–2394. doi: 10.1074/jbc.M610351200. [DOI] [PubMed] [Google Scholar]
- Pelegrin P, Surprenant A. The P2X(7) receptor-pannexin connection to dye uptake and IL-1beta release. Purinergic Signal. 2009;5:129–137. doi: 10.1007/s11302-009-9141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penuela S, Gehi R, Laird DW. The biochemistry and function of pannexin channels. Biochim Biophys Acta. 2013;1828:15–22. doi: 10.1016/j.bbamem.2012.01.017. [DOI] [PubMed] [Google Scholar]
- Penuela S, Gyenis L, Ablack A, Churko JM, Berger AC, Litchfield DW, Lewis JD, Laird DW. Loss of pannexin 1 attenuates melanoma progression by reversion to a melanocytic phenotype. J Biol Chem. 2012;287:29184–29193. doi: 10.1074/jbc.M112.377176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochnow N, Abdulazim A, Kurtenbach S, Wildforster V, Dvoriantchikova G, Hanske J, Petrasch-Parwez E, Shestopalov VI, Dermietzel R, Manahan-Vaughan D, Zoidl G. Pannexin1 stabilizes synaptic plasticity and is needed for learning. PLoS One. 2012;7:e51767. doi: 10.1371/journal.pone.0051767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y, Misaghi S, Newton K, Gilmour LL, Louie S, Cupp JE, Dubyak GR, Hackos D, Dixit VM. Pannexin-1 is required for ATP release during apoptosis but not for inflammasome activation. J Immunol. 2011;186:6553–6561. doi: 10.4049/jimmunol.1100478. [DOI] [PubMed] [Google Scholar]
- Ransford GA, Fregien N, Qiu F, Dahl G, Conner GE, Salathe M. Pannexin 1 contributes to ATP release in airway epithelia. Am J Respir Cell Mol Biol. 2009;41:525–534. doi: 10.1165/rcmb.2008-0367OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray A, Zoidl G, Weickert S, Wahle P, Dermietzel R. Site-specific and developmental expression of pannexin1 in the mouse nervous system. Eur J Neurosci. 2005;21:3277–3290. doi: 10.1111/j.1460-9568.2005.04139.x. [DOI] [PubMed] [Google Scholar]
- Sabirov RZ, Okada Y. ATP release via anion channels. Purinergic Signal. 2005;1:311–328. doi: 10.1007/s11302-005-1557-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenk U, Westendorf AM, Radaelli E, Casati A, Ferro M, Fumagalli M, Verderio C, Buer J, Scanziani E, Grassi F. Purinergic control of T cell activation by ATP released through pannexin-1 hemichannels. Sci Signal. 2008;1:ra6. doi: 10.1126/scisignal.1160583. [DOI] [PubMed] [Google Scholar]
- Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000;182:311–322. doi: 10.1002/(SICI)1097-4652(200003)182:3<311::AID-JCP1>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- Seminario-Vidal L, Okada SF, Sesma JI, Kreda SM, van Heusden CA, Zhu Y, Jones LC, O’Neal WK, Penuela S, Laird DW, Boucher RC, Lazarowski ER. Rho signaling regulates pannexin 1-mediated ATP release from airway epithelia. J Biol Chem. 2011;286:26277–26286. doi: 10.1074/jbc.M111.260562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Q, Lindstrom K, Shi R, Kelly J, Schroeder A, Juusola J, Levine KL, Esseltine JL, Penuela S, Jackson MF, Laird DW. A germline variant in PANX1 has reduced channel function and is associated with multisystem dysfunction. J Biol Chem. 2016;291:12432–12443. doi: 10.1074/jbc.M116.717934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro LA, Ng K, Zhou QY, Ribak CE. Subventricular zone-derived, newly generated neurons populate several olfactory and limbic forebrain regions. Epilepsy Behav 14 Suppl. 2009;1:74–80. doi: 10.1016/j.yebeh.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosinsky GE, Boassa D, Dermietzel R, Duffy HS, Laird DW, MacVicar B, Naus CC, Penuela S, Scemes E, Spray DC, Thompson RJ, Zhao HB, Dahl G. Pannexin channels are not gap junction hemichannels. Channels (Austin) 2011;5:193–197. doi: 10.4161/chan.5.3.15765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talaveron R, Fernandez P, Escamilla R, Pastor AM, Matarredona ER, Saez JC. Neural progenitor cells isolated from the subventricular zone present hemichannel activity and form functional gap junctions with glial cells. Front Cell Neurosci. 2015;9:411. doi: 10.3389/fncel.2015.00411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taruno A, Vingtdeux V, Ohmoto M, Ma Z, Dvoryanchikov G, Li A, Adrien L, Zhao H, Leung S, Abernethy M, Koppel J, Davies P, Civan MM, Chaudhari N, Matsumoto I, Hellekant G, Tordoff MG, Marambaud P, Foskett JK. CALHM1 ion channel mediates purinergic neurotransmission of sweet, bitter and umami tastes. Nature. 2013;495:223–226. doi: 10.1038/nature11906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashiro A, Zhao C, Gage FH. Retrovirus-mediated single-cell gene knockout technique in adult newborn neurons in vivo. Nat Protoc. 2006;1:3049–3055. doi: 10.1038/nprot.2006.473. [DOI] [PubMed] [Google Scholar]
- Van de Craen M, Vandenabeele P, Declercq W, Van den Brande I, Van Loo G, Molemans F, Schotte P, Van Criekinge W, Beyaert R, Fiers W. Characterization of seven murine caspase family members. FEBS Lett. 1997;403:61–69. doi: 10.1016/s0014-5793(97)00026-4. [DOI] [PubMed] [Google Scholar]
- Vanden Berghe T, Hulpiau P, Martens L, Vandenbroucke RE, Van Wonterghem E, Perry SW, Bruggeman I, Divert T, Choi SM, Vuylsteke M, Shestopalov VI, Libert C, Vandenabeele P. Passenger mutations confound interpretation of all genetically modified congenic mice. Immunity. 2015;43:200–209. doi: 10.1016/j.immuni.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt A, Hormuzdi SG, Monyer H. Pannexin1 and Pannexin2 expression in the developing and mature rat brain. Brain Res Mol Brain Res. 2005;141:113–120. doi: 10.1016/j.molbrainres.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Wang S, Miura M, Jung Y, Zhu H, Gagliardini V, Shi L, Greenberg AH, Yuan J. Identification and characterization of Ich-3, a member of the interleukin-1beta converting enzyme (ICE)/Ced-3 family and an upstream regulator of ICE. J Biol Chem. 1996;271:20580–20587. doi: 10.1074/jbc.271.34.20580. [DOI] [PubMed] [Google Scholar]
- Wicki-Stordeur LE, Swayne LA. Panx1 regulates neural stem and progenitor cell behaviours associated with cytoskeletal dynamics and interacts with multiple cytoskeletal elements. Cell Commun Signal. 2013;11:62. doi: 10.1186/1478-811X-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicki-Stordeur LE, Dzugalo AD, Swansburg RM, Suits JM, Swayne LA. Pannexin 1 regulates postnatal neural stem and progenitor cell proliferation. Neural Dev. 2012;7:11. doi: 10.1186/1749-8104-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicki-Stordeur LE, Sanchez-Arias JC, Dhaliwal J, Carmona-Wagner EO, Shestopalov VI, Lagace DC, Swayne LA. Pannexin 1 differentially affects neural precursor cell maintenance in the ventricular zone and peri-infarct cortex. J Neurosci. 2016;36:1203–1210. doi: 10.1523/JNEUROSCI.0436-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann H. Purinergic signaling in neural development. Semin Cell Dev Biol. 2011;22:194–204. doi: 10.1016/j.semcdb.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Zoidl G, Petrasch-Parwez E, Ray A, Meier C, Bunse S, Habbes HW, Dahl G, Dermietzel R. Localization of the pannexin1 protein at postsynaptic sites in the cerebral cortex and hippocampus. Neuroscience. 2007;146:9–16. doi: 10.1016/j.neuroscience.2007.01.061. [DOI] [PubMed] [Google Scholar]