Nerve guidance channels for peripheral nerve injury: Over the past decade, nerve guidance channels (NGCs) have emerged as a promising technology for regenerating gap injuries in peripheral nerves. Nerve gap injuries resulting from neurodegeneration and trauma, such as car accidents and battlefield wounds, affect hundreds of thousands of people annually. Motivated by suboptimal results obtained with the current gold standard of autologous grafting (i.e., autografts), various commercially available NGCs composed of synthetic and biomaterials are now alternatively available (Jia et al., 2014; Jones et al., 2016).
A key advantage of nerve repair via NGCs is the ability to both customize material properties and mimic native biological design of peripheral nerve. Various NGC characteristics including geometry (e.g., channel shape and fascicular structure), mechanical properties (e.g., elasticity), biological properties (e.g., biocompatibility and bio-degradability) and biological supplements (e.g., growth factors and nerve supporting cells) may be controlled. Common methods for NGC fabrication include wet chemistry and field-driven material assembly approaches, such as dip-molding and electrospinning, respectively. These approaches enable access to a wide materials palette, and as a result, NGCs made of synthetic polymers, biomaterials and conductive materials have been examined (Lewitus et al., 2011; Jones et al., 2016).
State of the art nerve repair and associated challenges: State of the art NGCs fabricated via conventional approaches are typically linear, bioresorbable channels containing physical cues (e.g., aligned fibers) and biological supplements, such as neurotrophic factors, extracellular matrix hydrogels and nerve supporting cells (e.g., Schwann cells or stem cells). As a result, current research areas include: 1) understanding the influence of NGC characteristics on regenerative outcome; 2) decoupling the effects of multiple NGC characteristics on regenerative outcome; 3) improving regenerative outcome relative to autograft-based repair in terms of critical nerve gap size and functional return; and 4) applying NGCs to complex nerve gap injuries, such as bifurcating nerve pathways. However, the limitations in controlling multi-material assembly and integration, especially that of biological supplements, is a critical challenge. Thus, a computer-aided multi-material NGC biomanufacturing paradigm would be highly desirable (Figure 1).
Figure 1.
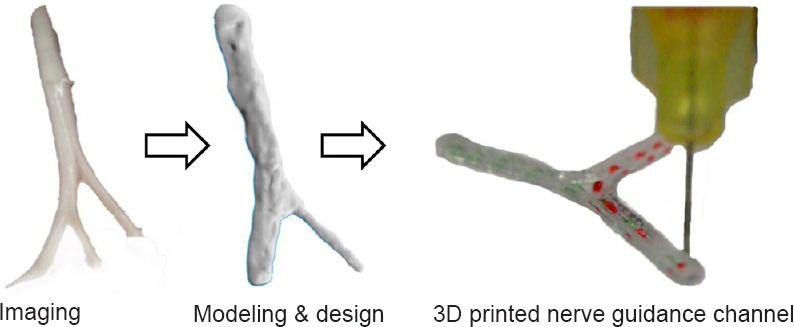
The extrusion-based 3D bioprinted nerve guidance channel (NGC) paradigm.
3D bioprinting as an enabling NGC biomanufacturing paradigm: Here we discuss the promise of multi-material extrusion-based 3D bioprinting, a form of additive manufacturing, for accelerating the pace of research, discovery, and translation of NGC technology (Johnson et al., 2015, 2016). We recently demonstrated the promise of NGC 3D bioprinting via both customizing scaffold geometry and programming the integration of physical and biochemical cues using a bifurcating nerve gap injury model (Johnson et al., 2015). Multi-material extrusion-based 3D bioprinting is compatible with standard materials and biological supplements used for NGC fabrication. Most importantly, the 3D bioprinting approach offers: 1) computer-aided design and modeling of physical (e.g., grooves and microchannels) and biological cues; and 2) personalization of scaffold geometry via imaging data inputs (Figure 1). Thus, 3D bioprinting is an emerging paradigm for unified design, prototyping, and biofabrication of personalized NGCs (Johnson et al., 2015).
Computer-aided control of geometry, physical cues, biological supplements and gradients: Currently, the integration of NGC physical characteristics, biological supplements (e.g., luminal “fillers”, surface micro-patterning, Schwann cell or stem cell inclusion), and mechanisms for controlled release of neurotrophic factors is approached through a material design-driven paradigm. This approach has provided a number of advances including the matching of NGC degradation rates to rates of peripheral nerve regeneration and the identification of both physical and biochemical regenerative cues. However, the ability to fully utilize and evaluate the expansive set of materials and cues available requires a complementary material assembly-driven paradigm.
Extrusion-based 3D bioprinting offers a one-pot NGC manufacturing approach for the programmable integration of synthetic materials, biomaterials, cells and growth factors based on bio-CAD templates derived from medical imaging data (Murphy and Atala, 2014; Johnson et al., 2015). Medical imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI), are commonly used for template development. However, the process of reconstructing a 3D model from 2D segmented imaging data can be an arduous process. To overcome this barrier, we recently demonstrated that highly accurate 3D computer models of peripheral nerve can be obtained by a complementary technique, 3D structured light scanning (SLS). Although SLS requires a direct view of the tissue using either cadaver models or the patient's nerves (healthy or injured), the resultant models are assembled from 3D segmented data which enables accurate surface reconstruction. We recently found SLS assists computer-aided design and manufacturing of personalized NGCs for complex, bifurcating nerve injuries (Johnson et al., 2015).
An important step in computer-aided manufacturing of straight and un-supplemented NGCs was recently made using photo-polymerizable polymers via stereolithography (SLA) (Pateman et al., 2015). This work suggested promise for the use of extrusion-based 3D bioprinting for NGC manufacturing which would enable the one-pot fabrication of integrated multi-material NGCs via coordinated extruders. It is well established that extrusion-based 3D bioprinting is a highly biocompatible manufacturing process (Murphy and Atala, 2014). We recently demonstrated that extrusion-based 3D bioprinting enables the fabrication of NGCs with complex geometry based on medical imaging data (SLS) which contain precisely embedded physical cues and biological supplements. Interestingly, we found the 3D printing process parameters could be tuned to achieve a longitudinal physical cue which caused aligned neurite outgrowth (Johnson et al., 2015).
Precision gradient programming via 3D bioprinting for enhanced regenerative outcomes: The incorporation of biological supplements (cues) in NGCs (e.g., extracellular matrix proteins, neurotrophic factors and supporting cells) is an active area of research. It has been shown that the incorporation and controlled release of neurotrophic factors can increase the magnitude of axonal regeneration (Faroni et al., 2015) and facilitate the regeneration of large nerve gaps (Chiono and Tonda-Turo, 2015). The incorporation of Schwann cells and neurotrophic factors has been shown to enhance nerve regeneration relative to controls that lacked such supplements (May et al., 2013). It was also shown that NGCs supplemented with luminal gelatin-based hydrogels led to increased neurite outgrowth (Gnavi et al., 2014). In addition, studying the effects of geometric distribution (uniform vs. gradients) and temporal release profiles remains a highly active area of research (Johnson et al., 2015). However, the variation in fabrication approaches and complexity of nerve regeneration make it difficult to definitively determine the effects of geometric and temporal patterning of biological factors on functional outcomes in vivo.
It has been established that hydrogel microstructure is influenced by many processing parameters including ionic strength, pH and additives (Spivey et al., 2012), and the current techniques for embedding biological supplements in NGCs widely vary. The introduction of biological supplements is typically done via manual injection, manual insertion, dip-coating or conventional seeding. Promising material design-driven approaches are continuing to emerge for direct incorporation of biological supplements into scaffold materials (Dinis et al., 2014). Thus, given the complexity of the nerve regeneration process, there is a need for highly repeatable and controlled biomanufacturing strategies to develop a fundamental understanding of the regenerative process as well as to further optimize clinical regenerative outcomes.
We recently demonstrated the concept of incorporating dual-component gradients in a bifurcating NGC for mixed nerve injury regeneration using extrusion-based 3D bioprinting (Johnson et al., 2015). Our 3D bioprinting approach enabled each path to be supplemented with a specific gradient of neurotrophic factors to promote selective regeneration. Specifically, the sensory and motor paths were supplemented with nerve growth factor (NFG) and glial cell-derived neurotrophic factor (GDNF), respectively. We also demonstrated the ability to 3D print Schwann cells and other neuronal cells at high viability using the same approach (Johnson et al., 2016). We found via in vitro studies that the 3D printed NGF gradients were a chemotractant for axonal growth and GDNF gradients increased Schwann cell migration rates. The functional outcome of in vivo studies was assessed by Catwalk analysis studies and revealed significant improvement in the functional return of the limbs treated with the gradient-containing NGCs. Importantly, the results suggest two major conclusions: 1) extrusion-based 3D bioprinting offers the ability to develop NGCs for the regeneration of bifurcating mixed nerve injuries; and 2) 3D bioprinting enables controlled and programmable augmentation of NGCs with biological supplements (cues) in gradient configurations for enhanced regenerative outcomes.
Conclusions and future directions: The state of the art of nerve repair via NGCs involves the application of degradable conduits containing physical cues and biological supplements. Thus, the ability to rapidly regenerate injuries over large gap distances hinges on developing a fundamental understanding of the effect of biological cues on regenerative outcomes and applying high precision biomanufacturing strategies for programmable integration of biological supplements (e.g., gradients). Computer-aided manufacturing approaches, such as extrusion-based 3D bioprinting which offer the ability to interweave multiple materials based on anatomical design, show significant promise for accelerating the pace of research, discovery, and translation of NGCs.
This work was supported by the Maryland Stem Cell Research Fund (2013-MSCRFE-146-00) (to XJ) and in part by the National Institute of Health (R01HL118084) (to XJ).
References
- Chiono V, Tonda-Turo C. Trends in the design of nerve guidance channels in peripheral nerve tissue engineering. Prog Neurobiol. 2015;131:87–104. doi: 10.1016/j.pneurobio.2015.06.001. [DOI] [PubMed] [Google Scholar]
- Dinis TM, Vidal G, Jose RR, Vigneron P, Bresson D, Fitzpatrick V, Marin F, Kaplan DL, Egles C. Complementary effects of two growth factors in multifunctionalized silk nanofibers for nerve reconstruction. PLoS One. 2014;9:e109770. doi: 10.1371/journal.pone.0109770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faroni A, Mobasseri SA, Kingham PJ, Reid AJ. Peripheral nerve regeneration: Experimental strategies and future perspectives. Adv Drug Deliver Rev. 2015;82-83:160–167. doi: 10.1016/j.addr.2014.11.010. [DOI] [PubMed] [Google Scholar]
- Gnavi S, di Blasio L, Tonda-Turo C, Mancardi A, Primo L, Ciardelli G, Gambarotta G, Geuna S, Perroteau I. Gelatin-based hydrogel for vascular endothelial growth factor release in peripheral nerve tissue engineering. J Tissue Eng Regen M. 2014 doi: 10.1002/term.1936. doi: 10.1002/term.1936. [DOI] [PubMed] [Google Scholar]
- Jia X, Romero-Ortega MI, Teng YD. Peripheral nerve regeneration: mechanism, cell biology, and therapies. Biomed Res Int 2014. 2014:145304. doi: 10.1155/2014/145304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B, Lancaster K, Hogue IB, Meng F, Kong YL, Enquist L, McAlpine M. 3D printed nervous system on a chip. Lab Chip. 2016;16:1393–1400. doi: 10.1039/c5lc01270h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BN, Lancaster KZ, Zhen G, He J, Gupta MK, Kong YL, Engel EA, Krick KD, Ju A, Meng F, Enquist LW, Jia X, McAlpine MC. 3D printed anatomical nerve regeneration pathways. Adv Funct Mater. 2015;25:6205–6217. doi: 10.1002/adfm.201501760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, Eisenberg HM, Jia X. Advances and future applications of augmented peripheral nerve regeneration. Int J Mol Sci. 2016;17:1494. doi: 10.3390/ijms17091494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewitus D, Vogelstein RJ, Zhen G, Choi YS, Kohn J, Harshbarger S, Jia X. Designing tyrosine-derived polycarbonate polymers for biodegradable regenerative type neural interface capable of neural recording. IEEE Trans Neural Syst Rehabil Eng. 2011;19:204–212. doi: 10.1109/TNSRE.2010.2098047. [DOI] [PubMed] [Google Scholar]
- May F, Buchner A, Schlenker B, Gratzke C, Arndt C, Stief C, Weidner N, Matiasek K. Schwann cell-mediated delivery of glial cell line-derived neurotrophic factor restores erectile function after cavernous nerve injury. Int J Urol. 2013;20:344–348. doi: 10.1111/iju.12078. [DOI] [PubMed] [Google Scholar]
- Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32:773–785. doi: 10.1038/nbt.2958. [DOI] [PubMed] [Google Scholar]
- Pateman CJ, Harding AJ, Glen A, Taylor CS, Christmas CR, Robinson PP, Rimmer S, Boissonade FM, Claeyssens F, Haycock JW. Nerve guides manufactured from photocurable polymers to aid peripheral nerve repair. Biomaterials. 2015;49:77–89. doi: 10.1016/j.biomaterials.2015.01.055. [DOI] [PubMed] [Google Scholar]
- Spivey EC, Khaing ZZ, Shear JB, Schmidt CE. The fundamental role of subcellular topography in peripheral nerve repair therapies. Biomaterials. 2012;33:4264–4276. doi: 10.1016/j.biomaterials.2012.02.043. [DOI] [PubMed] [Google Scholar]


