Summary
Infectious aortitis (IA) is a rare but life-threatening condition, and most commonly affects the abdominal aorta or thoracic aorta. Various microorganisms have been associated with infectious thoracic aortitis, most commonly Staphylococcus, Enterococcus, Streptococcus, and Salmonella species. Campylobacter fetus (C. fetus) has been seen as a cause of infective aortitis only in a few case reports. We report a rare case of infective aortitis of the abdominal aorta caused due to C. fetus bacteremia. While C. fetus infections usually occur in patients with immunosuppression, such as malignancy, or those with diabetes mellitus, but our patient was not immunocompromised. Furthermore, the IA occurred in the absence of an aortic aneurysm, unlike its usual presentation. Thus, it is extremely important to establish an early diagnosis of IA and find out the causative organism for appropriate medical treatment, because this condition is potentially life threatening.
Keywords: Aortitis, campylobacter fetus, aortic aneurysm, abdominal aorta
1. Introduction
Infectious aortitis (IA) is a rare but life-threatening condition, and most commonly affects the thoracic or the abdominal aorta (1). IA usually affects patients with atherosclerotic and/or aneurysmal disease and/or infective endocarditis (1). The epidemiology of aortitis, especially IA, as a distinct entity is poorly studied. The most common microorganisms causing IA are Staphylococcus, Enterococcus, Streptococcus, and Salmonella species (2). Cases of aortitis due to Mycobacterium tuberculosis have been observed in developing countries (3). Campylobacter fetus (C. fetus), a gram-negative bacilli has mostly been associated with endovascular and valve infections (4). We present a rare case of infectious aortitis associated with C. fetus bacteremia.
2. Case Report
A 66-year-old male with a medical history of hypertension, hyperlipidemia, gastroesophageal reflux disease (GERD), hypothyroidism and gout presented to the emergency room with a one-week history of back pain accompanied by fever and chills. The patient was initially suspected to have prostatitis as an outpatient and had failed treatment with oral levofloxacin. He denied having upper respiratory symptoms, difficulty breathing, diarrhea, recent intake of uncooked meat or intravenous drug use. Hematological workup revealed mild leukocytosis with white count of 13,000 and neutrophilia of 82%. There was elevation of acute inflammatory markers including erythrocyte sedimentation rate (ESR) of 90 and C-reactive protein (CRP) of 170. His chest X-ray and urinalysis were normal. Computed tomography (CT) scan of the abdomen and pelvis revealed focal wall thickening and fluid attenuation with inflammatory changes within and around the distal infrarenal abdominal aorta to proximal aortic bifurcation involving 7 cm in length, consistent with focal aortitis (Figure 1 and Figure 2)
Figure 1.
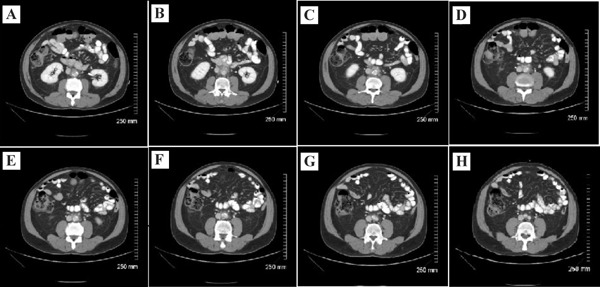
Contrast material enhanced sequential axial images of the abdomen via CT of the abdomen (A–H). There is nodular circumferential soft tissue thickening of the infra-renal aortic wall and the peri-aortic region with hazy peri-aortic inflammatory changes. The extent of the inflammatory changes involve the infra-renal aorta up to the more proximal aspect of the aortic bifurcation. Additionally, atherosclerotic changes of the infra-renal abdominal aorta are noted, consisting of calcified and non-calcified plaques.
Figure 2.
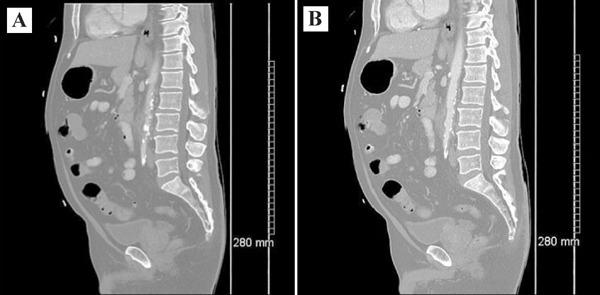
Contrast material enhanced sagittally reconstructed images of the abdomen and pelvis (A and B). There is evidence of diffuse circumferential soft tissue wall thickening of the abdominal aorta with surrounding peri-aortic inflammatory hazy changes. The superior extent of the inflammatory changes begin approximately at the proximal aspect of the infra-renal aorta and extend inferiorly just beyond the aortic bifurcation. Additionally, atherosclerotic changes of the infra-renal abdominal aorta are noted, consisting of calcified and non-calcified plaques.
He was admitted to the hospital, blood cultures were drawn and intravenous (IV) meropenem and ciprofloxacin were started empirically. Blood cultures returned positive for gram-negative rods eventually identified as C. fetus. While hospitalized, the patient received meropenem for 12 days, and ciprofloxacin for 9 days, which were eventually switched to gentamicin with final identification of C. fetus. Repeat blood cultures remained negative. A cardiac echocardiogram done did not reveal valvular vegetations or other abnormalities and repeat CT of the abdomen & pelvis showed stable focal aortitis with no signs of aortic aneurysmal dilatation or dissection. The patient's back pain significantly improved over time and a peripheral intravenous central catheter was placed anticipating long-term antibiotic therapy. His discharge medications included IV meropenem and IV gentamicin in addition to his home medications - aspirin, amlodipine, olmesartan, levothyroxine, atorvastatin, colchicine, pantoprazole and rosuvastatin. The patient's repeat blood cultures and CT of the abdomen remained stable.
3. Discussion
IA also known by bacterial, microbial, or cryptogenic aortitis, or mycotic or infected aneurysm, is a rare entity in the antibiotic era. It can affect the thoracic as well as the abdominal aorta. IA is frequently related to infectious endocarditis, occurring in 86% cases in the pre-antibiotic era (1). Infectious aortitis has mostly been described in the thoracic aorta in the literature rather than the abdominal aorta. There are only a few cases in the literature describing IA in the absence of an aneurysm or rupture. If it is left untreated, an infected nonaneurysmal aorta (typically with atherosclerosis) will likely progress to a mycotic aneurysm (2).
The most common pathogens associated with infective thoracic aortitis are Gram-positive bacteria, such as Staphylococcus, Enterococcus and Streptococcus species, causing 60% of the infections. On the other hand, infective abdominal aortitis is most frequently caused by Gram-negative bacilli, most commonly the Salmonella species (1). Campylobacter has been reported to cause infective abdominal aortitis in a few case reports (3–7). Patients with underlying chronic debilitating illness, e.g., diabetes, thalassemias, malignancy, cardiac conditions, or cirrhosis, are at increased risk for C. fetus bloodstream infections (8). The mechanisms of infections include i) bacteremic seeding on an existing atherosclerotic plaque; ii) septic emboli from infective endocarditis; iii) contiguous infective focus extending to the abdominal wall; and iv) direct bacterial inoculation at the time of trauma (penetrating injury). The virulence of C. fetus is thought to be mainly related to its production of a high-molecular-weight surface protein, which acts as a microcapsule with high affinity for the vascular endothelium (9). Blaser et al reported that C. fetus strains were serum resistant, which explains the high affinity of the organism to endothelial tissues (10).
Patients may present with fevers, chills, abdominal pain, and back pain. The patient may be asymptomatic, if he has no aneurysm formation. Leukocytosis and neutrophilia is seen in patients. ESR and CRP will also be elevated. Pentraxin-3 (PTX-3) is another promising potential biomarker for IA. Blood cultures can help isolate the microorganism, like in our case. Due to its association with infective endocarditis (IE), an echocardiogram is recommended to rule out IE. CT with contrast is the initial imaging method of choice (11). Magnetic resonance imaging (MRI) with gadolinium contrast enhancement or positron emission tomography (PET) scan can also be used. Invasive aortography is reserved for cases in which diagnosis of acute aortic syndrome cannot be excluded by noninvasive methods and carries the risk of rupture of the fragile aortic wall. The possible complications include aneurysm formation, if the patient does not have an already existent aneurysm. Complications of the aneurysm include rupture and bleeding, aortic thrombosis with distal embolisation, aortic dissection and aortic insufficiency. Acute coronary syndromes can occur in patients with involvement of coronaries (11).
As soon as the diagnosis is suspected, broad-spectrum intravenous antibiotics should be initiated. A longer course should be considered for immunosuppressed patients and if biochemical parameters of inflammation do not return to normal. Resection of the infected aorta can be performed with the intent of confirming the diagnosis, controlling sepsis, controlling hemorrhage (if rupture occurred), and reconstruction of the arterial vasculature. While surgery is recommended for most cases of infective aortitis, our patient was treated only with intravenous antibiotics because of the absence of aneurysm and clinical improvement with appropriate antibiotic therapy. It is important to identify the organism and initiate appropriate antibiotic therapy. C. fetus has been known to infect prosthetic joints and heart valves. In a case series of 21 patients with C. fetus bacteremia, all isolates were susceptible to amoxicillin, amoxicillin-clavulanate, imipenem, and gentamicin. Based on their study results, the authors suggest that imipenem should be preferred as first-line therapy for severe C. fetus infection, such as meningitis or endovascular infections (12). Gentamicin has low MICs for C. fetus isolates, and no gentamicin-resistant C. fetus isolates were seen in a report from Quebec (13,14). Based on microbiological data and clinical experience with treatment of C. fetus bacteremia, the use of a regimen that includes gentamicin has been advocated (15). Our patient responded well to gentamycin therapy. Endovascular techniques need further studies and longer follow-up periods in order to better define their role in IA management.
Factors apparently associated with a poor prognosis are advanced age, diagnosis delay, gram-negative bacilli infection, immunosuppression, thoracic location, and complication occurrence (such as rupture, embolization, or septic shock). Some authors recommend close medical follow-up that includes old and new biomarkers, serial blood cultures and imaging techniques (16) while others do not perform such approaches, and recommend only clinical surveillance (17).
Our patient presented with infective aortitis in the absence of formation of an aneurysm. He was found to have C. fetus bacteremia along with the aortitis in the absence of any underlying chronic debilitating illnesses. The patient showed an elevated leukocyte count and elevated ESR and CRP. The patient was diagnosed on the basis of the CT scan which showed focal aortitis in the absence of an aneurysm formation. Gentamycin has low MIC for treatment of C. fetus and our patient responded well to gentamycin therapy. Serial follow up CT scans showed resolution and no aneurysm formation was observed.
In conclusion, we report a rare case of infective aortitis of the abdominal aorta caused due to C. fetus bacteremia. It is extremely important to establish an early diagnosis of IA and find out the causative organism to institute antibiotic therapy and prevent fatal complications.
References
- 1. Revest M, Decaux O, Cazalets C, Verohye JP, Jego P, Grosbois B. Thoracic infectious aortitis: Microbiology, pathophysiology and treatment. Rev Med Interne. 2007; 28:108-115. (in French) [DOI] [PubMed] [Google Scholar]
- 2. Lopes RJ, Almeida J, Dias PJ, Pinho P, Maciel MJ. Infectious thoracic aortitis: A literature review. Clin Cardiol. 2009; 32:488-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bossone E, Pluchinotta FR, Andreas M, Blanc P, Citro R, Limongelli G, Della Corte A, Parikh A, Frigiola A, Lerakis S, Ehrlich M, Aboyans V. Aortitis. Vascul Pharmacol. 2016; 80:1-10. [DOI] [PubMed] [Google Scholar]
- 4. Morrison VA, Lloyd BK, Chia JK, Tuazon CU. Cardiovascular and bacteremic manifestations of Campylobacter fetus infection: Case report and review. Rev Infect Dis. 1990; 12:387-392. [DOI] [PubMed] [Google Scholar]
- 5. Blabey RG, Jr, Parry MF, Bull SM, Weed CB. Mycotic aneurysm of the abdominal aorta: Successful management of Campylobacter fetus aortitis. Conn Med. 1983; 47:129-130. [PubMed] [Google Scholar]
- 6. Anolik JR, Mildvan D, Winter JW, Puttlitz D, Rubenstein S, Lozman H. Mycotic aortic aneurysm. A complication of Campylobacter fetus septicemia. Arch Intern Med. 1983; 143:609-610. [DOI] [PubMed] [Google Scholar]
- 7. File TM, Jr, Barnishan J, Fass RJ. Campylobacter fetus sepsis with mycotic aortic aneurysm. Arch Pathol Lab Med. 1979; 103:143-145. [PubMed] [Google Scholar]
- 8. Guerrant RL, Lahita RG, Winn WC, Jr, Roberts RB. Campylobacteriosis in man: Pathogenic mechanisms and review of 91 bloodstream infections. Am J Med. 1978; 65:584-592. [DOI] [PubMed] [Google Scholar]
- 9. Fujihara N, Takakura S, Saito T, Iinuma Y, Ichiyama S. A case of perinatal sepsis by Campylobacter fetus subsp. fetus infection successfully treated with carbapenem — case report and literature review. J Infect. 2006; 53:e199-e202. [DOI] [PubMed] [Google Scholar]
- 10. Blaser MJ, Newell DG, Thompson SA, Zechner EL. Pathogenesis of Campylobacter fetus. In: Campylobacter 3rd ed. (Nachmakin S, Blaser MJ, eds). ASM Press, Washington, DC, USA; 2008. pp.401-428. [Google Scholar]
- 11. Gornik HL, Creager MA. Aortitis. Circulation. 2008; 117:3039-3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gazaigne L, Legrand P, Renaud B, Bourra B, Taillandier E, Brun-Buisson C, Lesprit P. Campylobacter fetus bloodstream infection: Risk factors and clinical features. Eur J Clin Microbiol Infect Dis. 2008; 27:185-189. [DOI] [PubMed] [Google Scholar]
- 13. Tremblay C, Gaudreau C, Lorange M. Epidemiology and antimicrobial susceptibilities of 111 Campylobacter fetus subsp. fetus strains isolated in Quebec, Canada from 1983 to 2000. J Clin Microbiol. 2003; 41:463-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tremblay C, Gaudreau C. Antimicrobial susceptibility testing of 59 strains of Campylobacter fetus subsp. fetus. Antimicrob Agents Chemother. 1998; 42:1847-1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Morrison VA, Lloyd BK, Chia JK, Tuazon CU. Cardiovascular and bacteremic manifestations of Campylobacter fetus infection: Case report and review. Rev Infect Dis. 1990; 12:387-392. [DOI] [PubMed] [Google Scholar]
- 16. Foote EA, Postier RG, Greenfield RA, Bronze MS. Infectious aortitis. Curr Treat Options Cardiovasc Med. 2005; 7:89-97. [DOI] [PubMed] [Google Scholar]
- 17. Hsu RB, Tsay YG, Wang SS, Chu SH. Surgical treatment for primary infected aneurysm of the descending thoracic aorta, abdominal aorta, and iliac arteries. J Vasc Surg. 2002; 36:746-750. [DOI] [PubMed] [Google Scholar]


