Summary
Abdominal pain is a very common symptom in all age groups but retroperitoneal fibrosis is a rare differential diagnosis suspected in young patients presenting with nonspecific abdominal pain and symptoms of obstructive uropathy. Presented here is a case of a 16-year-old boy who presented with symptoms of persistent abdominal pain and a previous history of swelling in the left leg. A computed tomography (CT) scan suggested retroperitoneal fibrosis and an exploratory laparotomy and histopathological examination were performed for definitive diagnosis. This case report is intended to promote awareness of retroperitoneal fibrosis in young patients among health care providers.
Keywords: Retroperitoneal fibrosis, children, abdominal pain, obstructive uropathy
1. Introduction
Retroperitoneal fibrosis is a rare disorder characterized by the presence of a chronic mass of fibroinflammatory tissue, which usually starts by first entrapping the aorta and then gradually entrapping surrounding structures including the ureter, vena cava, psoas muscle, and other retroperitoneal tissues. The peak age for the incidence of retroperitoneal fibrosis is usually in the 60 s or 70 s. The average age at onset is 60 years, with a male-to-female ratio of 1.9:1 (1). Childhood presentation is extremely rare. The most common manifestations include abdominal pain, abdominal distension, lumbago, weight loss, and pitting edema in the lower extremities (1).
2. Case Report
A 16-year-old male presented with persistent abdominal pain and vomiting that began 15 days earlier. The patient also had a history of swelling in the left leg from 4 years prior. Findings from a systemic examination were unremarkable. There was no localised tenderness in the abdomen, no organomegaly, and no lymphadenopathy.
Laboratory results in the form of the complete blood count revealed microcytic hypochromic anemia (hemoglobin: 9 gm/dL) for the patient's age and sex while total leucocyte counts and platelet counts were within normal limits. A routine urine examination indicated a mild degree of proteinuria with 4–6 pus cells and 3–5 red blood cells per high power field. Blood urea nitrogen (BUN) was 128 mg/dL and creatinine was 1.8 mg/dL. Other biochemical results were within normal limits. Inflammatory markers in the serum were elevated, including C-reactive protein (CRP) at 1.2 mg/dL (normal: < 0.6 mg/dL) and an erythrocyte sedimentation rate (ESR) of 95 mm/h (normal: 0–20 mm/h), but immunoglobulin G4 (IgG4) was normal at 105 mg/dL (normal: 1–291 mg/dL). The patient tested negative for antinuclear antibodies (< 1.0 IU).
Ultrasonography of the abdomen showed right renal enlargement with grade 3 hydronephrosis and a small left kidney. No evidence of stones was noted. Computed tomography (CT) (Figure 1) suggested an irregularly shaped soft-tissue mass 10.5 × 9.1 × 8.9 cm in size in the presacral region. The mass was located more to the left and it extended along the left lateral pelvic wall, protruding in the left sacral foramina at levels S1–2 and S2–3. Iliac vessels on both sides abutted or were entrapped within the mass (L > R). Both ureters also entrapped by the mass. The left kidney was small, 7.6 cm in length and heterogeneously hyperdense with loss of corticomedullary differentiation. Prominent vascular collaterals were found in the subcutaneous plane of the anterior abdominal wall and the bilateral inguinal region and pelvis.
Figure 1.
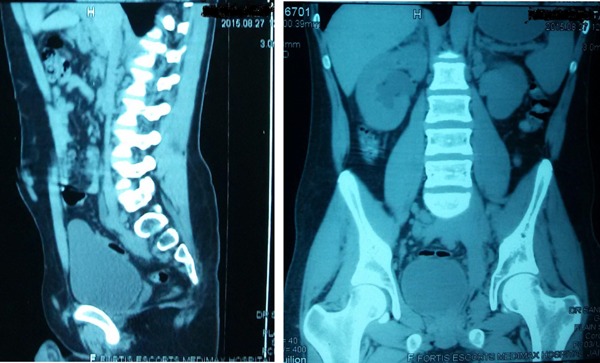
Computed tomography scan of the abdomen showing a retroperitoneal mass encasing the ureter and iliac vessels on both sides. The left kidney is 7.6 cm smaller in length and heterogeneously hyperdense.
Given the risk of bleeding from prominent vascular collaterals present in the subcutaneous plane of the anterior abdominal wall and the inaccessibility of a deep-seated mass, a biopsy was performed via an exploratory laparotomy rather than a laparoscopic procedure. There was a hard, irregular, and poorly circumscribed mass at the base of the bladder that encased both ureters and iliac vessels. The left ureter had a thick wall and narrow lumen. A biopsy sample was submitted for histopathology examination. A DJ stent was placed on both sides to relieve obstruction. Biopsy of the mass revealed several irregular greyish white pieces of soft tissue 0.6 × 0.4 cm in size. Microscopically, the mass consisted of mainly fibroadipose tissue with few congested blood vessels and chronic infiltration by non-specific inflammatory cells. Evidence of tuberculosis or malignancy was not evident.
Corticosteroids were started to treat retroperitoneal fibrosis, and the patient responded well. One month after the start of treatment, the patient became clinically asymptomatic and his creatinine level returned to normal (0.7 mg/dL). Another CT scan is planned for follow up.
3. Discussion
Cases of retroperitoneal fibrosis have previously been reported, but the current case is unusual. This case has been for 2 reasons: to promote awareness regarding the overlooked features of retroperitoneal fibrosis and to prompt consideration of retroperitoneal fibrosis in young patients as well.
Retroperitoneal fibrosis was first described by Albarran, a French urologist, as ureter obstruction by retroperitoneal tissue (2), but Ormond (3) defined it as an established clinical disease. The cause of retroperitoneal fibrosis is not readily understood. About three-fourths of cases are idiopathic while other cases may be related to retroperitoneal injury, drug therapy with methysergide, β-blockers and haloperidol, or genetic factors. The incidence of the idiopathic form has been reported to be 0.1 per 100,000 person-years, with a prevalence of 1.4 per 100,000 (4). This disease usually occurs in elderly patients, but it has also been reported in children. Males are affected more often than females (1).
Most frequently, the patient presents with nonspecific symptoms like dull abdominal pain and features of chronic renal failure, hypertension, pain, a backache, weight loss, and an abdominal mass (5). In the current case, the patient presented with features of a urinary tract obstruction and renal failure. However, the patient also had a past history of swelling in the left leg. At the time, ultrasonography of the perforators was performed, but the results were normal and the patient was advised to wear stockings. That swelling might be part of the disease process, but this disease entity is very rare, so health care providers seldom consider retroperitoneal fibrosis. When a patient presents with nonspecific symptoms or symptoms of obstructive uropathy and elevated ESR and CRP, retroperitoneal fibrosis should be considered. Biopsy is the gold standard for diagnosis but a CT scan and magnetic resonance imaging (MRI) scan should also done to rule out secondary causes (6).
Recently, the concept of a correlation between IgG4 and idiopathic retroperitoneal fibrosis has been proposed. Zen et al. (7) studied 17 patients with retroperitoneal fibrosis and immunohistochemistry revealed numerous IgG4-positive plasma cell infiltrates in 10 cases (IgG4-related) but only a few positive cells in 7 cases (non-IgG4-related). Serologically, serum IgG and IgG4 levels were significantly higher in cases of IgG4-related retroperitoneal fibrosis. The current patient had normal serum IgG4 levels, and the patient's condition may have fallen into the category of non-IgG4-related retroperitoneal fibrosis.
Secondary retroperitoneal fibrosis is treated by treating the underlying cause while idiopathic cases of retroperitoneal fibrosis are treated by excising the mass with ureterolysis and administering corticosteroid therapy (8). Immunosuppression with azathioprine and mycophenolate mofetil and hormonal treatment with tamoxifen are also cited as treatment modalities for retroperitoneal fibrosis (9–11).
Surgical treatment includes temporary decompression by percutaneous nephrostomy or ureteral stenting for obstructive uropathy, and definitive treatment includes open or laparoscopic ureterolysis, anterior transposition or omental wrapping of the involved ureter, and more recently, ureterolysis and omental wrapping with Gore-Tex, excision of the ureter and reanastomosis, fashioning of a posterior preperitoneal flap, and renal autotransplantation (12,13).
The prognosis for retroperitoneal fibrosis usually depends on the underlying cause and the degree of renal impairment at the time of presentation. Usually, the idiopathic form has a good prognosis (14) while the malignant form has a poor prognosis. Even if the idiopathic form has a good prognosis, lifelong follow up is required to monitor recurrence and complications.
In conclusion, this case report is intended to promote awareness of retroperitoneal fibrosis in young patients among health care providers. Definitive diagnosis should be based on a CT scan or MRI findings along with a biopsy.
References
- 1. An LM, Xu YF, Zhang ZL. Clinical features and prognostic analysis of retroperitoneal fibrosis in 32 patients. Beijing Da Xue Bao. 2012; 44:265-269. (in Chinese) [PubMed] [Google Scholar]
- 2. Albarran J. Rétention rénale par périurétérite. Libération externe de l'uretère. Assoc Fr Urol. 1905; 9:511-517. [Google Scholar]
- 3. Ormond JK. Bilateral ureteral obstruction due to envelopment and compression by an inflammatory retroperitoneal process. J Urol. 1948; 59:1072-1079. [DOI] [PubMed] [Google Scholar]
- 4. Thongprayoon C, Spanuchart I, Cheungpasitporn W, Kangwanpornsiri A. Idiopathic retroperitoneal fibrosis: A challenging case in a rare disease. N Am J Med Sci. 2014; 6:237-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koep L, Zuidema GD. The clinical significance of retroperitoneal fibrosis. Surgery. 1977; 81:250-257. [PubMed] [Google Scholar]
- 6. Liu H, Zhang G, Niu Y, Jiang N, Xiao W. Retroperitoneal fibrosis: A clinical and out-come analysis of 58 cases and review of literature. Rheumatol Int. 2014; 34:1665-1670. [DOI] [PubMed] [Google Scholar]
- 7. Zen Y, Onodera M, Inoue D, et al. Retroperitoneal fibrosis: A clinicopathologic study with respect to immunoglobulin G4. Am J Surg Pathol. 2009; 33:1833-1839. [DOI] [PubMed] [Google Scholar]
- 8. Baker LR, Mallison WJ, Gregory MC, Menzies EA, Cattell WR, Whitfield HN, Hendry WF, Wickham JE, Joekes AM. Idiopathic retroperitoneal fibrosis: A retrospective analysis of sixty cases. Br J Urol. 1987; 60:497-503. [DOI] [PubMed] [Google Scholar]
- 9. Dedeoglu F, Rose CD, Athreya BH, Conard K, Grissom L, Magnusson M. Successful treatment of retroperitoneal fibrosis with tamoxifen in a child. J Rheum. 2001; 28:1693-1695. [PubMed] [Google Scholar]
- 10. Van Bommel EF. Retroperitoneal fibrosis. Neth J Med. 2002; 60:231-242. [PubMed] [Google Scholar]
- 11. Swartz RD, Lake AM, Roberts WW, Faerber GJ, Wolf JS., Jr Idiopathic retroperitoneal fibrosis: A role for mycophenolate mofetil. Clin Nephrol. 2008; 69:260-268. [DOI] [PubMed] [Google Scholar]
- 12. Safioleas M, Safioleas P, Stamatakos M, Safioleas C. Retroperitoneal fibrosis obstructing the ureter: A new technique to prevent stenosis recurrence. Surgery. 2008; 143:299-300. [DOI] [PubMed] [Google Scholar]
- 13. Fugita OE, Jarrett TW, Kavoussi P, Kavoussi LR. Laparoscopic treatment of retroperitoneal fibrosis. J Endourol. 2002; 16:571-574. [DOI] [PubMed] [Google Scholar]
- 14. Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet. 2006; 367:241-251. [DOI] [PubMed] [Google Scholar]


