Sir,
Oral ingestion of paraphenylenediamine (PPD) main toxic component of permanent hair dye, causes severe angioedema of the upper airway accompanied by a swollen, dry, hard and protruding tongue, and requires emergency airway management. PPD intoxication also results in multisystem involvement causing rhabdomyolysis and acute kidney injury (AKI), flaccid paralysis, severe gastrointestinal manifestations, cardiotoxicity and arrhythmias1. The mechanisms involved in kidney injury are a direct toxic effect against the renal tubules, rhabdomyolysis and myoglobinuria. This direct toxic effect on the kidney is due to the aromatic structure of PPD, which facilitates an easy absorption and concentration of PPD in the tubules, causing AKI. Propylene glycol and resurcitol are other potentially nephrotoxic agents of hair dye poisoning2,3.
The objective of this retrospective study was to describe the characteristics and the outcome of the patients with hair dye poisoning admitted at the intensive care unit (ICU) of a rural district hospital in India. This study was conducted from May 2010 to May 2013 in Balhalapalli Hospital, a 300-bed non-profit secondary level institution belonging to the Rural Development Trust (RDT) at Anantapur, in the State of Andhra Pradesh, in southern India.
The data were collected in relation to demographic details (age, sex, marital and socio-economic status) volume consumed; time to reach the hospital, clinical features, laboratory findings and outcomes. Tracheotomy was done for severe cervicofacial oedema with stridor. Demographic, clinical, radiological, and laboratory data were reviewed in all 102 patients during ICU stay. In 19 cases (18%) an emergency tracheostomy was performed. Forty eight (47%) patients presented with dark urine, and five (5%) developed acute renal failure. Total mortality was 5.9 per cent: two each due to cardiogenic shock (myocarditis), brain death following hypoxia; and renal and respiratory failure. All those patients who died consumed ≥ 60 ml of hair dye.
Chi-square test or Fisher's exact test was used for comparison of proportions. For continuous variables, mean, median and standard deviation were calculated, and compared by Student t test or non-parametric tests; if appropriate a bivariate analysis was conducted to identify prognostic variables for mortality. The considered variables were age, gender, hours prior to admission and the volume consumed. All variables that were significant in the bivariate analysis were included in a gender-adjusted logistic regression model.
During the study period, a total of 1262 poisoning cases were admitted, of whom 340 (27%) were due to organophosphates and 414 (33%) due to hair dye poisoning. The remaining 40 per cent were due to other pesticides and poisons. Of the 414 patients with hair dye poisoning, 102 (25%) required ICU admission.
Most patients were young women (n=80, 78.4%). There was no significant differences between men and women in age, marital status and overall mortality. Sixty five (63.7%) patients were married. Mean age of patients was 23.4 ± 7.6 yr. The time from the ingestion to hospital admission ranged from 45 min to 12 h, with a median value of 2.2 h. The volume of hair dye consumed ranged from 10 to 500 ml. In 19 cases (18%) an emergency tracheostomy was performed and 16 (16%) required endotracheal intubation. Overall, the sum of patient days at ICU was 261. Four patients were referred to a higher centre (3 of them for dialysis and 1 to ENT surgeon).
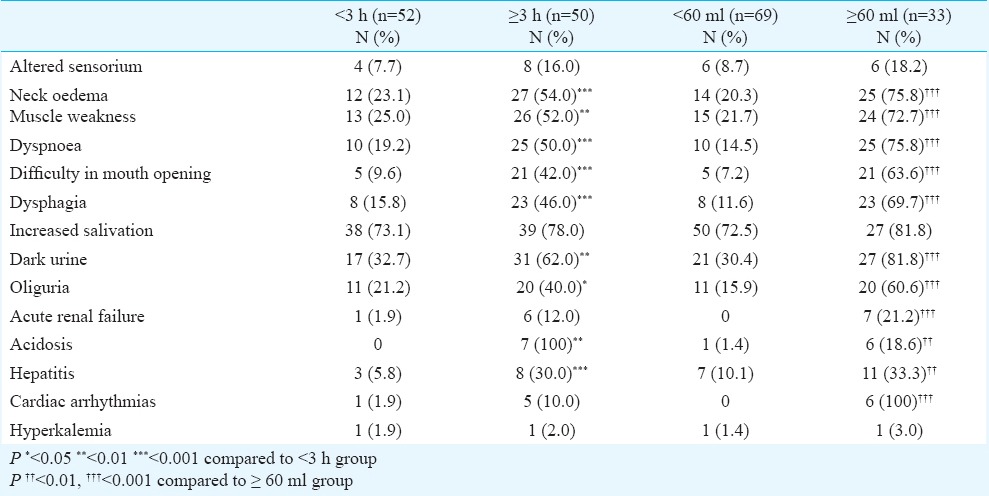
The comparison of clinical data between the patients admitted within the first three hours after the ingestion (n=52) and those admitted three or more hours after the ingestion (n=50) is shown in (Table I). The latter group presented with more severe symptoms. Similarly, those patients that took 60 ml or more also presented with severe symptoms than those who took less than 60 ml (Table I). This cut-off value corresponded to the 75th percentile of the sample. None of patients who took less than 60 ml presented acute renal failure and/or cardiac complications.
Table I.
Comparison of clinical data between patients admitted within <3 h and ≥3 h of ingestion, and between patients who consumed <60 ml and ≥60 ml
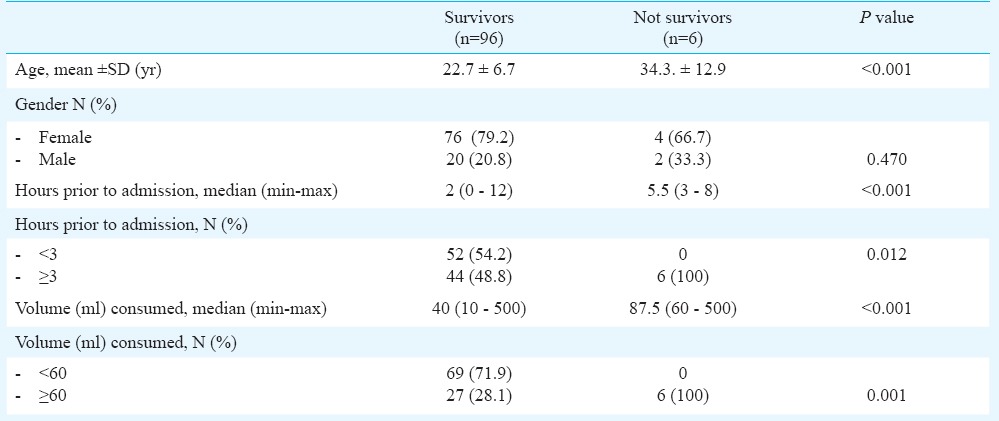
The analysis of factors potentially related with patients’ prognosis is shown in Table II. The average age of survivors was significantly lower than that of the non-survivors. Half of the survivors arrived to the hospital during the first two hours after ingestion, whereas the median time for arriving among non-survivors was more than two fold (5.5 h). Half of the survivors consumed 40 ml or less, whereas the median volume consumed by the non-survivors was 87.5 ml. All patients who died arrived to the hospital three or more hours after ingestion and consumed 60 or more ml of the dye.
Table II.
Bivariate analysis of factors potentially related with prognosis
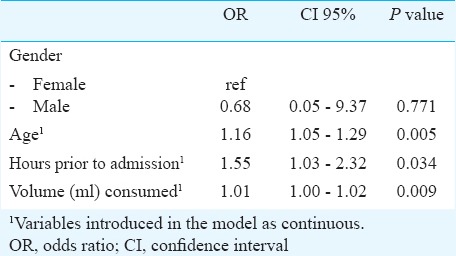
A logistic regression analysis was performed to identify the determinant factors for dying due to hair dye ingestion (Table III), showing that the longer time between ingestion and hospital admission and the higher volume of poison consumed were significant independent risk factors. Age was also related with a poorer prognosis. The interpretation of the adjusted odds ratios for these prognostic variables, considering them as continuous, was that for every hour that the patient came late after ingestion, the risk of death increased up to 55 per cent and for each 10 ml of consumed dye, the risk of death increased up to 10 per cent. In relation with the age, every year increased 16 per cent mortality (Data not shown).
Table III.
Logistic regression analysis of factors potentially related with prognosis
Patients with symptomatic hypocalcaemia, including tetany or seizures, would need intravenous correction of calcium4. The complications include the risk of death due to cervico facial oedema, renal failure and myocarditis5,6.If the patient arrives within the first six hours after ingestion, the treatment of poisoning is to be focused on the decrease of absorption with activated charcoal (2 g/kg diluted with 200 ml of water). The induction of emesis is contraindicated because if PPD comes in contract with mucosa it causes severe edematous reaction7.
To avoid the acute kidney injury (AKI) associated with rhabdomyolysis, early aggressive fluid therapy with crystalloids is required8,9,10. Bicarbonate therapy is reserved only when there is severe acidemia8,10. Further, bicarbonate may worsen the degree of hypocalcaemia, especially if hypovolemia is corrected8. For forced diuresis, mannitol is used because experimental studies showed it to be renoprotective8. Furosemide is another diuretic used to convert anuric to oliguric renal failure8. Dialysis per se is purely a supportive intervention as the PPD is not dialyzable. In our experience, although some of our patients presented with transient increase of hepatic transaminases, none of them developed hepatic failure.
In conclusion, our study showed that most patients who consumed hair dye were young women. Those who survived were younger than non-survivors and reached hospital within three hours after ingestion. Thus, age, volume of dye consumed and time between ingestion and hospital admission were significant factors determining the outcome.
Acknowledgment
The authors thank the RDT management for support in this study; The Medical Record Department of RDT Hospital Bathalapalli for providing all the patient records; and the ICU nurses for helping in recording proforma sheets.
Footnotes
Conflicts of Interest: None.
References
- 1.Abdelraheema M, Hamdoukb M, Zijlstra EE. Paraphenylenediamine (Hair Dye) Poisoning in Children. Arab J Nephrol Transplant. 2010;3:39–43. [Google Scholar]
- 2.Kumar PA, Talari K, Dutta TK. Super vasomol hair dye poisoning. Toxicol Int. 2012;19:77–8. doi: 10.4103/0971-6580.94503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sampathkumar K, Sooraj YS, Ajeshkumar RP, Mahaldar AR, Muthiah R. Rhabdomyolysis due to hair dye poisoning: An emerging threat. Indian J Crit Care Med. 2007;11:212–4. [Google Scholar]
- 4.Chrispal A, Begum A, Ramya I, Zachariah A. Hair dye poisoning- an emerging problem in the tropics: An experience from a tertiary care hospital in South India. Trop Doct. 2010;40:100–3. doi: 10.1258/td.2010.090367. [DOI] [PubMed] [Google Scholar]
- 5.Mary Nirmala S, Ganesh R. Hair dye - An emerging suicidal agent: Our experience. Otolaryngol Online J. 2012;2:1–11. [Google Scholar]
- 6.Sampathkumar K, Yesudas S. Hair dye poisoning and the developing world. J Emerg Trauma Shock. 2009;2:129–31. doi: 10.4103/0974-2700.50749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaik NA, Jayasundaram E. Gastric lavage in hair dye (Super Vasmol 33) poisoning: A friend or foe. J Emerg Trauma Shock. 2012;5:276. doi: 10.4103/0974-2700.99712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis - an overview for clinicians. Crit Care. 2005;9:158–69. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan FY. Rhabdomyolysis: a review of the literature. Neth J Med. 2009;67:272–83. [PubMed] [Google Scholar]
- 10.Scharman EJ, Troutman WG. Prevention of kidney injury following rhabdomyolysis: a systematic review. Ann Pharmacother. 2013;47:90–105. doi: 10.1345/aph.1R215. [DOI] [PubMed] [Google Scholar]


