Abstract
Accountable care organizations (ACOs) have diverse contracting arrangements and have displayed wide variations in their performance. Using data from national surveys of 399 ACOs, we examined differences between the 228 commercial ACOs (those with commercial payer contracts) and the 171 noncommercial ACOs (those with only public contracts, such as with Medicare or Medicaid). Commercial ACOs were significantly larger and more integrated with hospitals, and had lower benchmark expenditures and higher quality scores, compared to noncommercial ACOs. Among all of the ACOs, there was low uptake of quality and efficiency activities. However, commercial ACOs reported more use of disease monitoring tools, patient satisfaction data, and quality improvement methods than did noncommercial ACOs. Few ACOs reported having high-level performance monitoring capabilities. About two-thirds of the ACOs had established processes for distributing any savings accrued, and these ACOs allocated approximately the same amount of savings to the ACOs themselves, participating member organizations, and physicians. Our findings demonstrate that ACO delivery systems remain at a nascent stage. Structural differences between commercial and noncommercial ACOs are important factors to consider as public policy efforts continue to evolve.
Over the past four years there has been a substantial increase in the number of accountable care organizations (ACOs)—groups of physicians, hospitals, and other providers that agree to be financially responsible for the total cost and quality of care for a defined patient population. Provider groups are entering into contractual agreements with both commercial (or private) payers and public payers, such as Medicare and Medicaid. Collectively, an estimated 838 ACOs currently cover an attributed population of about 28.3 million people nationwide.[1] With the federal government increasingly encouraging providers to participate in alternative payment models, some policy makers expect the number of beneficiaries attributed to ACOs to exceed 100 million at some point in the next five years.[2]
While much attention has been focused on ACO performance outcomes,[3,4] there is less information on how ACOs are internally structured to support delivery system reform and achieve performance benchmarks. Given the large variation in ACO outcomes to date, it is important that the organizations’ internal processes are well understood.[5] We focused on three areas to better understand the types and extent of organizational transformation that is occurring within ACOs.
First, ACO formation is subject to a range of organizational dynamics that result in particular structures, activities, and outcomes. Resource dependence theory holds that an organization’s behavior is strongly influenced by its ability to gain control of vital external resources that may be diffusely distributed across or held by multiple other organizations.[6] In the ACO context, partner organizations experience varying degrees of interdependence. One key strategy for mitigating any resulting risk is through consolidation of resources. Consequently, many providers are engaging in new regional partnerships, collaborations, and joint ventures with other providers. This is particularly the case with integrated delivery systems that contract with commercial payers in alternative payment models to control health care spending.[7,8]
As a consequence, these ACOs may be structured differently than ACOs that participate only in public payer programs, such as Medicare, and their constituent provider organizations may be more highly consolidated. The extent to which any structural changes may also translate into lower costs and improved health care quality remains unknown.
Second, a major organizational challenge for ACOs in transforming care is to effectively engage providers and patients in new models of service delivery. Institutional theory suggests that organizations strive to maintain their credibility and legitimacy in the face of changing societal norms and values.[9] In health care, this creates competing tensions between old and new delivery paradigms—the former characterized by a self-regulated, semi-autonomous, physician-dominated environment, and the latter characterized by shifts toward greater engagement of multidisciplinary clinical [please provide] teams and consumers; a focus on population health; and alternatives to volume-driven, fee-for-service physician compensation models. It is unclear to what extent ACOs are taking measures to shift their activities to align with these emerging paradigms of health care delivery, or whether such shifts might manifest themselves differently in ACOs that contract with commercial payers and those that contract only with public payers.
Third, ACOs are operating in relatively high-risk environments, particularly those organizations that may receive either bonuses (when their costs are less than an established baseline) or penalties (when their costs exceed the baseline). The extent to which ACOs can withstand financial adversity and improve their performance remains uncertain. “High-reliability organizations” are those that thrive in complex environments, consistently demonstrate error-free performance, and withstand threats to their viability.[10] Robust information technology systems, widely disseminated and continuous processes of quality improvement, care coordination, and monitoring systems that are sensitive enough to detect “weak signals” of potential failure are all key features of such organizations.[11] Attainment of these capabilities may be particularly challenging in ACO environments, where providers have limited previous experience in working together, and provider networks are only loosely organized.
In exploring these three areas empirically we sought to address the following questions. Do ACOs involved in commercial payer programs have different structures and outcomes than ACOs involved only in public programs? Are ACOs implementing changes to their provider compensation models and care management processes? Are ACOs adopting features of high-reliability organizations to support their sustainability in complex health care environments?
To address these questions, we investigated some of the mechanisms that Lawton Burns and Mark Pauly note can be used to affect change in ACOs.[12] These mechanisms include revising organizational structures (for example, forming physician-hospital organizations, centralizing contracting, and vertically integrating providers), altering provider compensation (such as shifting from volume- to value-based incentives or aligning payments with requirements in external contracts), implementing changes to improve quality (including the use of clinical decision support, disease registries, care coordination, patient engagement, data analytics, and electronic health records [EHRs]), and increasing efficiency (for example, through the use of “lean” production principles, removing low-value practices, or reducing hospitalizations and use of the emergency department [ED]).
Study Data And Methods
Data
The National Survey of Accountable Care Organizations is an online survey that examines factors that influence the formation, implementation, and performance of ACOs.[13] Three cross-sectional waves of the survey have been conducted to date. Each wave includes a new cohort of ACOs that have not previously participated. Wave 1 was conducted between October 2012 and May 2013 and had 175 respondents. Wave 2 was conducted between September 2013 and March 2014 and had 96 respondents. Wave 3 was conducted between November 2014 and April 2015 and had 128 respondents. Questions added in waves 2 and 3 were asked in a follow-up survey conducted between November 2014 and April 2015 with 82 of the original wave 1 respondents. The overall response rate across all three waves was 64 percent. Further details about the survey methodology have been published previously[13] and are available in the online Appendix.[14]
For ACOs participating in Medicare ACO programs,[15] we matched publicly reported performance outcome data to survey responses. These data include information on expenditure benchmarks (derived from historical expenditures for the attributed population), savings and quality outcomes for each performance year in the program, and a range of indicators on beneficiaries’ demographic characteristics and health care utilization. We derived scores for quality outcomes from thirty-three reported measures in four domains (patient experience, care coordination, at-risk measures, and preventive care), using the methods outlined by the Centers for Medicare and Medicaid Services (CMS).[16] For indicators marked as pay-for-reporting only, we calculated performance scores using the CMS sliding-scale approach instead of awarding maximum points if ACOs’ performance on the indicators was satisfactory.
Our survey was approved by the Institutional Review Board at Dartmouth College. Informed consent was obtained from all participants.
Analysis
We examined responses to survey questions that pertained to the following four domains of interest: ACO structure and outcomes, provider compensation, quality activities, and efficiency processes. We defined a commercial ACO as an ACO that had at least one contract with a private payer (with or without Medicare or Medicaid contracts) and a noncommercial ACO as one that had contracts only with Medicare, Medicaid, or both. We present our data as means or as percentages. Statistical significance was assessed using two-sample t-tests for continuous variables and chi-square tests for categorical variables.
After performing descriptive analyses, we derived a set of organizational indices to characterize ACOs’ internal activities in three of the four domains in our conceptual framework (provider compensation, quality activities, and efficiency processes). The methods we used are outlined in Appendix Exhibit A2.[14] The ninety-three ACOs that participated in wave 1 of the survey but not the follow-up survey were excluded from this component of the analysis, because several questions of interest were not asked in the original survey.
Limitations
Limitations associated with the National Survey of Accountable Care Organizations have been discussed in previous work.[13,17] In particular, survey questions were directed to the single person in a given ACO deemed to be the most knowledgeable. It is possible that other people in the ACO might have responded differently and might have had more knowledge about some domains than the respondent. Further, although we tested for and ruled out nonresponse bias based on publicly available CMS data, we could not assess nonresponse bias in commercial ACOs because of a lack of public data sources.[13]
Our study focused on a cross-sectional survey conducted in the early period of ACOs’ contracting. The median duration from the date of implementation of the earliest ACO contract to the time of the survey was 11.6 months (interquartile range: 7.1–13.2 months). This time period was similar across all three survey waves and between commercial and noncommercial ACOs. Consequently, our ability to capture the dynamic nature of organizational transformation that might be occurring in these organizations was limited.
The analyses that we conducted included multiple comparisons. It is possible that some of the significant differences we report represent chance findings.
Study Results
Structural Characteristics And Outcomes
Of the 399 ACOs surveyed, 228 (57 percent) were commercial, and 171 (43 percent) were noncommercial (Exhibit 1). Seventy-five percent of the commercial ACOs had Medicare or Medicaid contracts in addition to their private payer contracts (for further details on contract status, see Appendix Exhibit A1).[14] Compared to noncommercial ACOs, commercial ACOs were significantly larger in terms of attributed Medicare beneficiaries (Exhibit 1)[please provide]). They were also more likely to include one or more hospitals and to be jointly led by physicians and one or more hospitals.
Exhibit 1.
Characteristics of 399 accountable care organizations (ACOs) 2012–15, by commercial contract status
| Noncomme rcial ACOs |
Commer cial ACOs |
p value | |
|---|---|---|---|
| Contract arrangements | |||
| Current Medicare ACO contract | 91% | 62% | <0.001 |
| Current Medicaid ACO contract | 17 | 29 | 0.02 |
| Two or more private contracts | —a | 30 | —a |
| Leadership | |||
| Physician led | 60% | 47% | <0.001 |
| Hospital led | 7 | 5 | —b |
| Jointly led by physicians and one or more hospitals |
19 | 41 | —b |
| Other | 14 | 7 | —b |
| Hospital involvement | |||
| ACO includes at least one hospital | 47% | 71% | <0.001 |
| Previous experience with payment reform activities | |||
| Risk-based contractc | 28% | 50% | <0.001 |
| Bundled or episode-based payments | 22 | 31 | <0.01 |
| Pay-for-performance programs | 74 | 84 | 0.03 |
| Other risk-bearing contract | 37 | 50 | <0.001 |
| Physicians employed by the ACO (mean %) | |||
| Primary care physicians | 20 | 42 | <0.001 |
| Specialists | 14 | 38 | <0.001 |
| Types of providers available within the ACOd | |||
| Primary care | 95% | 97% | 0.54 |
| Routine specialty care | 53 | 73 | <0.001 |
| Pediatric health | 39 | 66 | <0.001 |
| Emergency care | 39 | 68 | <0.001 |
| Behavioral health | 33 | 48 | <0.01 |
| Mean health professionals per 1,000 Medicare beneficiaries in year 1e | |||
| Primary care physicians | 7.8 | 9.4 | 0.05 |
| Specialists | 12.8 | 17.8 | 0.04 |
| Nurse practitioners | 2.7 | 3.6 | 0.02 |
| Mean Medicare financial outcomes in year 1f | |||
| Attributed beneficiaries | 14,347 | 19,061 | 0.01 |
| Expenditure benchmark per beneficiary | $12,091 | $10,392 | <0.001 |
| Savings per beneficiary | $88 | $25 | 0.50 |
| Mean Medicare quality scores in year 1f | |||
| Overall quality | 70% | 74% | <0.001 |
| Patient experience | 87 | 89 | 0.03 |
| Preventive health | 71 | 71 | 0.93 |
| Care coordination | 65 | 72 | <0.001 |
| At-risk chronic disease measures | 58 | 64 | <0.001 |
SOURCE Authors’ analysis of data for 2012–15 from the National Survey of Accountable Care Organizations and from the Centers for Medicare and Medicaid Services. NOTES Survey data were available for 171 noncommercial and 228 commercial ACOs except where indicated. Year 1 refers to Medicare performance data for the first year of participation in the ACO program [please provide].
By definition noncommercial ACOs do not hold any private contracts[Please provide].
Statistical significance was based on the chi-square test for the overall question on leadership
Data were available for 123 noncommercial and 183 commercial ACOs (question not asked in the original survey).
Data were available for 160 noncommercial and 215 commercial ACOs (24 missing responses).
Medicare data were available for 121 noncommercial and 100 commercial ACOs.
Medicare data were available for 135 noncommercial and 113 commercial ACOs.
A larger proportion of commercial ACOs had previous experience with payment reform models and risk-based contracting and offered a greater breadth of specialized health services, compared to noncommercial ACOs (Exhibit 1). Of the 221 ACOs for which CMS data on providers were available, commercial ACOs had a higher density of primary care physicians and specialists than did noncommercial ACOs. Of the 248 ACOs for which CMS data on other topics were available, commercial ACOs had lower expenditure benchmarks per beneficiary and tended to achieve smaller savings in the Medicare programs but had significantly higher overall quality scores, compared to noncommercial ACOs.
Provider Compensation
Commercial ACOs reported higher rates of changes to their physician compensation model since becoming an ACO, compared to noncommercial ACOs (51 percent versus 28 percent) (further details shown in Appendix Exhibit A3-1). Overall, only a third of ACOs reported having a high level of ability to monitor financial performance. Less than half of ACOs were monitoring or reporting financial performance at the clinician level. Sixty-six percent had determined how savings would be distributed internally at the time of the survey (during the first year of an ACO contract).
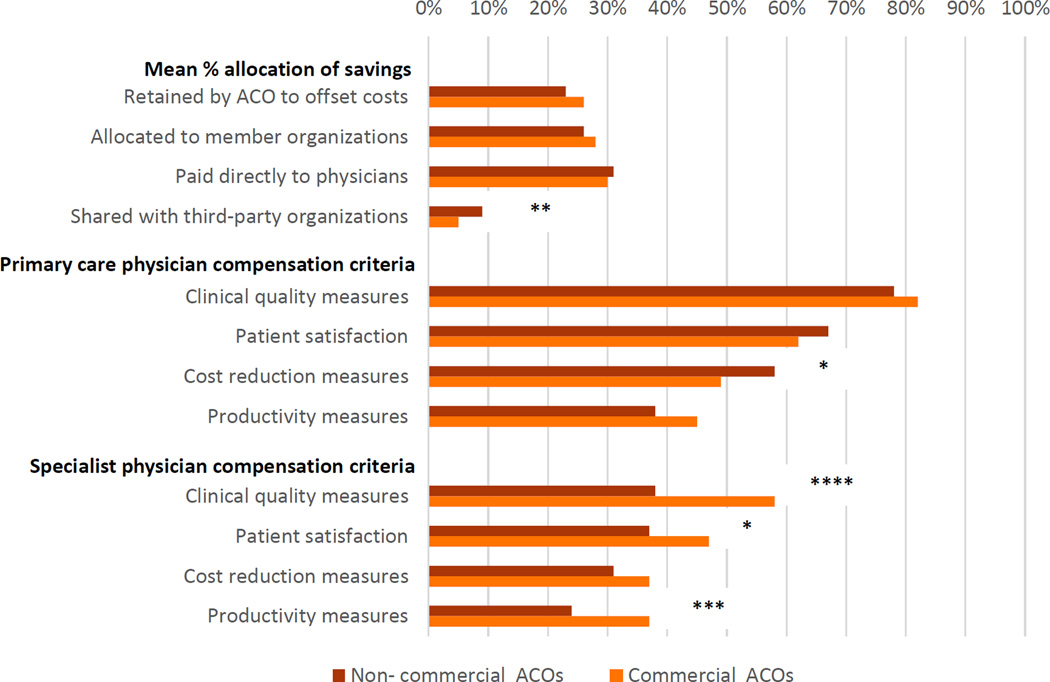
Of those ACOs with a plan in place, financial rewards were distributed roughly evenly among the ACO itself, participating member organizations, and physicians (Exhibit 2). There was a slightly greater mean allocation of rewards to third-party organizations in noncommercial ACOs than in commercial ACOs.
EXHIBIT 2.
Compensation processes for providers in accountable care organizations (ACOs) 2012–15, by commercial contract status
Source/Notes: SOURCE Authors’ analysis of data for 2012–15 from the National Survey of Accountable Care Organizations. NOTES Complete data including numerators and denominators for each question and additional survey questions analyzed that are not shown in the exhibit [please provide] are available in Appendix Exhibit A3-1 (see Note 14 in text). The data on mean percentage allocation of savings applies only to those ACOs with a savings distribution plan in place. *p < 0.10 **p < 0.05 ***p < 0.01 ****p < 0.001
For the majority of ACOs, payments of savings to providers or member organizations were generally contingent on either their meeting performance benchmarks or the size of the attributed patient population. Similar proportions of commercial and noncommercial ACOs provided financial compensation to primary care physicians based on clinical quality measures (82 percent and 78 percent, respectively), patient satisfaction (62 percent and 67 percent, respectively) and cost-reduction measures (49 percent and 58 percent, respectively) (Exhibit 2). These measures tended to be used less commonly for specialist compensation, although a greater proportion of commercial ACOs than noncommercial ACOs compensated specialists based on clinical quality measures and productivity measures.
Quality Activities
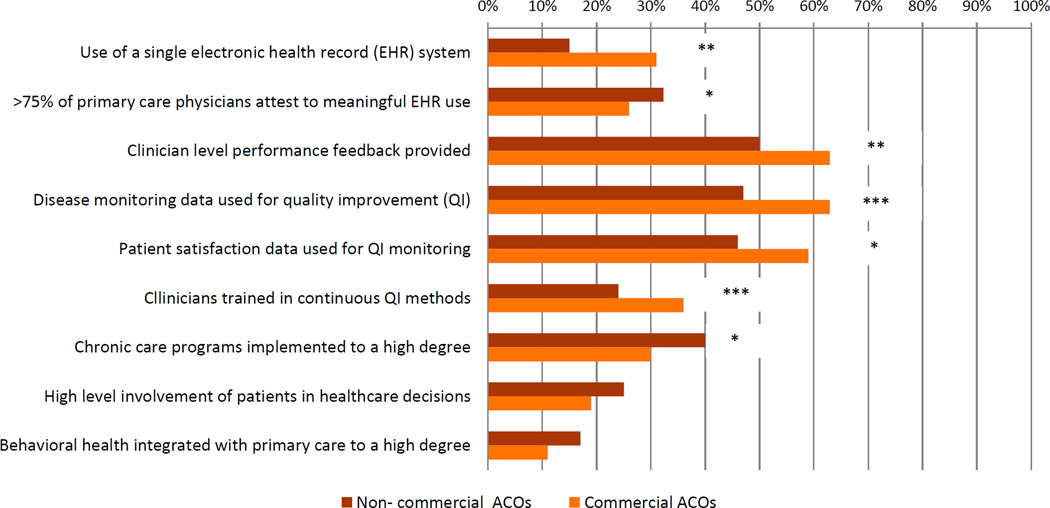
The majority of ACOs have invested in new staff for quality activities such as quality improvement, care coordination and analytics and information technology (further details shown in Appendix Exhibit A3-2). Despite this investment, overall EHR capacity appears to be low. A minority of commercial and noncommercial ACOs had single EHR systems (31 percent and 15 percent, respectively) and reported that more than 75 percent of their primary care physicians met criteria for meaningful use of the systems (26 percent and 33 percent, respectively) (Exhibit 3). Compared to noncommercial ACOs, commercial ACOs tended to have a higher degree of engagement in disease monitoring activities. Overall, a low proportion of ACOs considered that they had established high-level care coordination processes in terms of implementation of chronic care programs, involvement of patients in healthcare decisions and integration of behavioural health with primary health care (Exhibit 3 and Appendix Exhibit A3-2).
EXHIBIT 3.
Quality activities of accountable care organizations (ACOs) 2012–15, by commercial contract status
Source/Notes: SOURCE Authors’ analysis of data for 2012–15 from the National Survey of Accountable Care Organizations. NOTES Complete data including numerators and denominators for each question and additional survey questions analyzed that are not shown in the exhibit [please provide] are available in Appendix Exhibit A3-2 (see Note 14 in text). EHR is electronic health record. QI is quality improvement. *p < 0.10 **p < 0.05 ***p < 0.01
Efficiency Processes
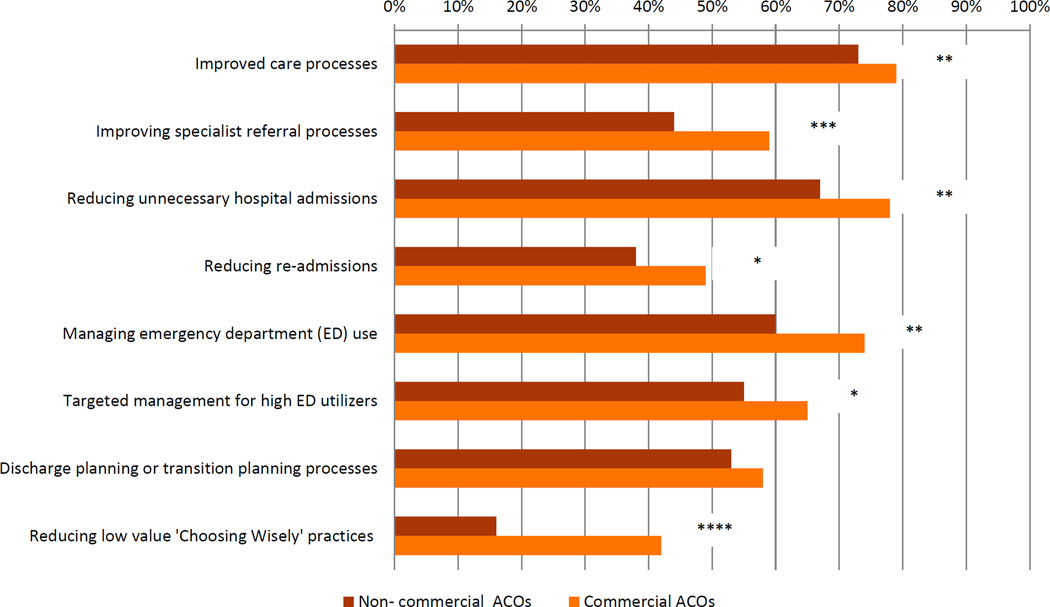
Compared to noncommercial ACOs, a greater proportion of commercial ACOs had taken action to improve efficiency in the areas of care processes (73 percent and 79 percent, respectively), unnecessary hospitalizations (67 percent and 78 percent, respectively), and specialist referral processes (44 percent and 59 percent, respectively) (Exhibit 4). A greater proportion of commercial ACOs were also investing in processes to reduce use of the ED and taking steps to reduce overuse of health care services identified by the Choosing Wisely campaign as having low value.[18]
EXHIBIT 4.
Efficiency processes of accountable care organizations (ACOs) 2012–15, by commercial contract status
Source/Notes: SOURCE Authors’ analysis of data for 2012–15 from the National Survey of Accountable Care Organizations. NOTES Complete data including numerators and denominators for each question and additional survey questions analyzed that are not shown in the exhibit [please provide] are available in Appendix Exhibit A3-3 (see Note 14 in text). “Low-value practices” are those identified by the Choosing Wisely campaign (see Note 18 in text). ED is emergency department. **p < 0.05 ***p < 0.01 ****p < 0.001
In general, neither commercial nor noncommercial ACOs were very active in trying to reduce costs in other areas, such as outpatient visits, use of imaging, and use of postacute care facilities (Appendix Exhibit A3-3).[14]
Composite Indices
Following correlation and principal component analyses, we derived a three-factor model with Eigenvalues of greater than 1.3 and 60 percent of the variance explained by these factors. From this model, we derived composite indices for provider compensation (Cronbach alpha: 0.85), quality activities (Cronbach alpha: 0.90), and efficiency processes (Cronbach alpha: 0.90). Appendix Exhibit A4 presents the variables included within each domain and shows how points were allocated to each variable.[14] Commercial ACOs had higher scores for quality activities (60.3 versus 56.0; p = 0.05), efficiency processes (50.1 versus 40.9; p < 0.01), and overall (51.5 versus 46.3; p <0.01). There were no significant differences in provider compensation (44.2 versus 42.1; p = 0.32).
Appendix Exhibit A5 outlines the normalized distribution of composite indices for ACOs by contract status for each index and overall.[14] Sensitivity analyses were conducted with mean and maximum values imputed for ACOs with missing responses. In those analyses there were negligible differences in overall index values.
Discussion
We analyzed survey data from a large, nationally representative sample of ACOs to examine the internal processes that ACOs are implementing to improve performance. Despite increasing scrutiny of ACOs’ ability to contain costs and improve health care quality, few studies have identified how the organizations are internally structuring their activities to achieve these goals. We focused on four domains (organizational structure, provider compensation, quality activities, and efficiency processes) and developed composite indices in the latter three domains to systematically characterize organizational activity. Four main findings emerged from our analyses.
First, commercial ACOs are structured differently from noncommercial ACOs in terms of patient numbers, location, level of hospital integration, breadth of specialty services provided in house, provider-to-patient ratios, and benchmark spending. From a resource dependency perspective, these factors are seen as critical drivers of organizational sustainability. The substantially lower benchmark spending and higher efficiency index of commercial ACOs suggests that they are considerably “leaner” organizations when entering Medicare ACO programs, compared to noncommercial ACOs, and that they may have already implemented efficiency processes.[19] This may also explain why the magnitude of savings is generally greater for noncommercial ACOs during their initial Medicare performance years.[20]
The drivers of higher efficiency in commercial ACOs may also be the result of a more mature engagement with private payers, compared to noncommercial ACOs that may have less flexible arrangements with public payers. Organizations that became commercial ACOs may have previously entered into less intensive activities with payers, such as using bundled payments and other alternative payment models, before taking on more intensive risk-based contracting as ACOs. Compared to noncommercial ACOs, commercial ACOs may also have greater opportunities and requirements for efficiency gains with private payers in terms of the ability to bear greater risk,[17] negotiate price discounts, and implement supply-side controls (such as preauthorizations).[8] Their awareness of and active engagement in processes to reduce utilization of hospitals and low-value health care practices associated with the Choosing Wisely campaign[18] are examples of this and are consistent with a recent evaluation of the Pioneer ACOs that found modest reductions in low-value services.[21]
Second, in terms of provider compensation, the majority of ACOs now provide some financial incentives to physicians to lower costs and raise quality, and there appears to be a higher degree of change in physician compensation models in commercial ACOs than in noncommercial ACOs. This finding contrasts with the results of a study from the early 2000s that found that only 25 percent of Californian physician organizations were offering physicians financial incentives based on reduced spending for hospital services and referrals.[22] However, the question remains whether such incentives are sufficient or even necessary to influence cost and quality outcomes. Andrew Ryan and coauthors found that although practices participating in an ACO provide higher compensation for better performance on quality metrics, the proportion of that funding was less than 5 percent of overall compensation, and salary and compensation for productivity measures remain dominant.[23]
Drawing on institutional theory, it seems that ACOs to date have minimally disrupted the status quo in provider compensation reform. Furthermore, a low proportion of ACOs reported having strong financial or quality monitoring systems. Thus, having the correct size and type of incentives is not enough: The lack of an adequate infrastructure to implement these incentives remains a major barrier.
Third, the implementation of quality activities still appears to be in an early stage for all ACOs, with only a modest uptake of performance monitoring and quality improvement processes observed. This suggests that engaging providers in these activities takes time. In addition, it remains unclear what are the best ways to motivate front-line providers to engage in quality improvement activities. It is possible that when modest financial incentives for performance improvements are combined with quality improvement activities, this may produce greater change in organizational practices than each one on their own.[24] Greater attention to behavioral economic principles may be helpful in shedding light on how financial, behavioral, and social factors may interact with one another to influence organizational culture.[25,26]
Fourth, despite intensive policy efforts to improve information management systems, ACOs still have limited capacity to make optimal use of these systems. Although EHR adoption, the use of decision support and data analytics, and integration of information between providers are all considered essential building blocks to delivery system reform, only a minority of ACOs (both commercial and noncommercial) said that they had a high level of capability in these areas.[27] The immature stage of development of information technology in ACOs could substantially limit delivery system transformation. This raises concerns that ACOs lack some of the essential tools needed to become high-reliability organizations.
Policy Implications
This study builds on previous work that showed a wide spectrum of ACO structures, capabilities, and outcomes.[28] It suggests that the establishment of support mechanisms for noncommercial ACOs, which are typically smaller than commercial ACOs, may be a critical factor in their sustainability. In terms of extrinsic factors, a public-sector steward such as Medicare may play a central role in promoting delivery system reform. This contrasts with the provider-dominated integrated delivery networks of the 1990s.[12] Noncommercial ACOs may be engaging in Medicare programs as a low-risk opportunity to build internal capacity to better manage risk-based contracting.[29]
This finding underscores the pivotal role played by the public sector in stimulating provider engagement in ACO and other alternative payment and care delivery models.[30–32] Alignment with private-sector payment models remains a major barrier to delivery system reform, and state-led initiatives such as Maryland’s all-payer rate-setting system for hospital costs could serve as a model for future all-payer ACOs.[33] Such demonstration initiatives—when combined with large-scale public policy changes, including provisions of the Medicare Access and CHIP Reauthorization Act of 2015—may accelerate attainment of a tipping point for substantive shifts away from traditional delivery system models.[34]
Although federal Medicare programs appear essential, it remains to be seen whether ACOs can successfully establish internal processes to support their sustainability. While a command-control structure may support the establishment of certain capabilities such as uniform information technology systems, this structure may not be ideal for changing providers’ organizational culture.[35,36] Conversely for smaller ACOs with a potentially less hierarchical structure than larger ACOs, their size may afford them additional opportunities to engage providers more closely. However, smaller ACOs may lack the ability to invest in common infrastructure to support system changes. It is likely that a combination of initiatives, simultaneously driven by central administration and by local front-line providers, is needed to strike the right balance in promoting organizational change.
Conclusion
The movement toward accountable care is highly dynamic. For some health care providers it is engendering rapid organizational transformation, while for others it presents an opportunity to gain valuable experience with risk-based contracting. The role of public and private payers, the establishment of essential organizational infrastructure, and the level of provider engagement internally are important factors that influence the sustainability of the nascent ACO movement. Given the heterogeneous nature of ACOs, it is likely that judicious alignment of external policy programs and internal organizational factors will be needed to promote successful outcomes.
Supplementary Material
Acknowledgments
The findings from this study were presented to the Quality and Value Interest Group at the AcademyHealth Annual Research Meeting, Boston, Massachusetts, June 25, 2016. The authors gratefully acknowledge funding from the Commonwealth Fund (Grant No. 20150034). David Peiris and Madeleine Phipps-Taylor were supported by Commonwealth Fund Harkness Fellowships in Healthcare Policy and Practice. Valerie Lewis was supported by a grant from the Robert Wood Johnson Foundation’s Changes in Health Care Financing and Organization initiative (Grant No. 72646). Carrie H Colla received support from the Dartmouth Clinical and Translational Science Institute, through an award from the National Center for Advancing Translational Sciences (Award No. UL1TR001086).
Biographies
David Peiris (dpeirishsph.harvard.edu) is a Harkness Fellow at the Harvard T. H. Chan School of Public Health, in Boston, Massachusetts.
Madeleine C. Phipps-Taylor was a 2014–2015 Harkness Fellow at the School of Public Health at the University of California, Berkeley.
Courtney A. Stachowski is a research project specialist at the Dartmouth Institute for Health Policy and Clinical Practice, in Lebanon, New Hampshire.
Lee-Sien Kao was a health policy fellow at the Dartmouth Institute for Health Policy and Clinical Practice.
Stephen M. Shortell is a professor in and dean of the School of Public Health at the University of California, Berkeley.
Valerie A. Lewis is an assistant professor of health policy at the Dartmouth Institute for Health Policy and Clinical Practice.
Meredith B. Rosenthal is a professor of health economics and policy in the Department of Health Policy and Management at the Harvard T. H. Chan School of Public Health.
Carrie H. Colla is an associate professor of health policy at the Dartmouth Institute for Health Policy and Clinical Practice.
Notes
- 1.Muhlestein D, McClellan M. Accountable care organizations in 2016: private and public-sector growth and dispersion. [cited 2016 Aug 5];Health Affairs Blog [blog on the Internet] 2016 Apr 21; Available from: http://healthaffairs.org/blog/2016/04/21/accountable-care-organizations-in-2016-private-and-public-sector-growth-and-dispersion/ [Google Scholar]
- 2.Muhlestein D, Gardner P, Caughey W, de Lisle K. Projected growth of accountable care organizations. Salt Lake City (UT): Leavitt Partners, LLC; 2015. Dec, [please provide] [Google Scholar]
- 3.Nyweide DJ, Lee W, Cuerdon TT, Pham HH, Cox M, Rajkumar R, et al. Association of Pioneer Accountable Care Organizations vs traditional Medicare fee for service with spending, utilization, and patient experience. JAMA. 2015;313(21):2152–2161. doi: 10.1001/jama.2015.4930. [DOI] [PubMed] [Google Scholar]
- 4.McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance differences in year 1 of Pioneer Accountable Care Organizations. N Engl J Med. 2015;372(20):1927–1936. doi: 10.1056/NEJMsa1414929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colla CH, Wennberg DE, Meara E, Skinner JS, Gottlieb D, Lewis VA, et al. Spending differences associated with the Medicare Physician Group Practice Demonstration. JAMA. 2012;308(10):1015–1023. doi: 10.1001/2012.jama.10812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hillman AJ, Withers MC, Collins BJ. Resource dependence theory: a review. J Manage. 2009;35(6):1404–1427. [Google Scholar]
- 7.Shortell SM, Wu FM, Lewis VA, Colla CH, Fisher ES. A taxonomy of accountable care organizations for policy and practice. Health Serv Res. 2014;49(6):1883–1899. doi: 10.1111/1475-6773.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song Z, Chokshi DA. The role of private payers in payment reform. JAMA. 2015;313(1):25–26. doi: 10.1001/jama.2014.15904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodrick E, Reay T. An institutional perspective on accountable care organizations. Med Care Res Rev. 2016 Mar 30; doi: 10.1177/1077558716641832. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Pronovost PJ, Berenholtz SM, Goeschel CA, Needham DM, Sexton JB, Thompson DA, et al. Creating high reliability in health care organizations. Health Serv Res. 2006;41(4 Pt 2):1599–1617. doi: 10.1111/j.1475-6773.2006.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vogus TJ, Singer SJ. Creating highly reliable accountable care organizations. Med Care Res Rev. 2016 Mar 28; doi: 10.1177/1077558716640413. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Burns LR, Pauly MV. Accountable care organizations may have difficulty avoiding the failures of integrated delivery networks of the 1990s. Health Aff (Millwood) 2012;31(11):2407–2416. doi: 10.1377/hlthaff.2011.0675. [DOI] [PubMed] [Google Scholar]
- 13.Colla CH, Lewis VA, Shortell SM, Fisher ES. First national survey of ACOs finds that physicians are playing strong leadership and ownership roles. Health Aff (Millwood) 2014;33(6):964–971. doi: 10.1377/hlthaff.2013.1463. [DOI] [PubMed] [Google Scholar]
- 14.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 15.The ACOs with Medicare contracts in this survey participated in either the Shared Savings Program or the Pioneer model. Pioneer ACOs share with Medicare a proportion of any savings or losses relative to an expenditure benchmark (“two-sided risk”). ACOs in the Shared Savings Program can take on two-sided risk, but they also have the option of sharing only in a proportion of savings (not losses) in the first three years of participation (“one-sided risk”).
- 16.Centers for Medicare and Medicaid Services. Baltimore (MD): CMS; [cited 2016 Aug 5]. Medicare Shared Savings Program quality measure benchmarks for the 2014 reporting year [Internet] Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/MSSP-QM-Benchmarks.pdf. [Google Scholar]
- 17.Lewis VA, Colla CH, Schpero WL, Shortell SM, Fisher ES. ACO contracting with private and public payers: a baseline comparative analysis. Am J Manag Care. 2014;20(12):1008–1014. [PubMed] [Google Scholar]
- 18.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 19.Sutherland S, Egan B, Davis R, Rutledge V, Sinopoli A. Diving into the pool of ACO quality measures: MSSP year 2 performance metrics. [cited 2016 Aug 8];Health Affairs Blog [blog on the Internet] 2015 Dec 21; Available from: http://healthaffairs.org/blog/2015/12/21/diving-into-the-pool-of-aco-quality-measures-mssp-year-2-performance-metrics/ [Google Scholar]
- 20.McClellan M, Kocot SL, White R. Medicare ACOs continue to show care improvements—and more savings are possible. [cited 2016 Aug 8];Health Affairs Blog [blog on the Internet] 2015 Nov 4; Available from: http://healthaffairs.org/blog/2015/11/04/medicare-acos-continue-to-show-care-improvements-and-more-savings-are-possible/ [Google Scholar]
- 21.Schwartz AL, Chernew ME, Landon BE, McWilliams J. Changes in low-value services in year 1 of the Medicare Pioneer Accountable Care Organization program. JAMA Intern Med. 2015;175(11):1815–1825. doi: 10.1001/jamainternmed.2015.4525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenthal MB, Frank RG, Buchanan JL, Epstein AM. Transmission of financial incentives to physicians by intermediary organizations in California. Health Aff (Millwood) 2002;21(4):197–205. doi: 10.1377/hlthaff.21.4.197. [DOI] [PubMed] [Google Scholar]
- 23.Ryan AM, Shortell SM, Ramsay PP, Casalino LP. Salary and quality compensation for physician practices participating in accountable care organizations. Ann Fam Med. 2015;13(4):321–324. doi: 10.1370/afm.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson JC. Theory and practice in the design of physician payment incentives. Milbank Q. 2001;79(2):149–177. III. doi: 10.1111/1468-0009.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Emanuel EJ, Ubel PA, Kessler JB, Meyer G, Muller RW, Navathe AS, et al. Using behavioral economics to design physician incentives that deliver high-value care. Ann Intern Med. 2016;164(2):114–119. doi: 10.7326/M15-1330. [DOI] [PubMed] [Google Scholar]
- 26.Conrad DA. The theory of value-based payment incentives and their application to health care. Health Serv Res. 2015;50(Suppl 2):2057–2089. doi: 10.1111/1475-6773.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larson BK, Van Citters AD, Kreindler SA, Carluzzo KL, Gbemudu JN, Wu FM, et al. Insights from transformations under way at four Brookings-Dartmouth accountable care organization pilot sites. Health Aff (Millwood) 2012;31(11):2395–2406. doi: 10.1377/hlthaff.2011.1219. [DOI] [PubMed] [Google Scholar]
- 28.Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law. 2015;40(4):647–668. doi: 10.1215/03616878-3149976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewis VA, Colla CH, Schpero WL, Shortell SM, Fisher ES. ACO contracting with private and public payers: a baseline comparative analysis. Am J Manag Care. 2014;20(12):1008–1014. [PubMed] [Google Scholar]
- 30.Takach M, Townley C, Yalowich R, Kinsler S. Making multipayer reform work: what can be learned from medical home initiatives. Health Aff (Millwood) 2015;34(4):662–672. doi: 10.1377/hlthaff.2014.1083. [DOI] [PubMed] [Google Scholar]
- 31.Rajkumar R, Conway PH, Tavenner M. CMS—engaging multiple payers in payment reform. JAMA. 2014;311(19):1967–1968. doi: 10.1001/jama.2014.3703. [DOI] [PubMed] [Google Scholar]
- 32.Pham HH, Pilotte J, Rajkumar R, Richter E, Cavanaugh S, Conway PH. Medicare’s vision for delivery-system reform—the role of ACOs. N Engl J Med. 2015;373(11):987–990. doi: 10.1056/NEJMp1507319. [DOI] [PubMed] [Google Scholar]
- 33. CMS.gov. Baltimore (MD): Centers for Medicare and Medicaid Services; [cited 2016 Aug 8]. Maryland all-payer model [Internet] [last updated 2015 Feb 6;]. Available from: https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/ [Google Scholar]
- 34.Rosenthal MB. Physician payment after the SGR— the new meritocracy. N Engl J Med. 2015;373(13):1187–1189. doi: 10.1056/NEJMp1507757. [DOI] [PubMed] [Google Scholar]
- 35.Anderson DG, Morris DE. Characteristics of successful “super ACOs”. Healthc Financ Manage. 2015;69(6):98–100. [PubMed] [Google Scholar]
- 36.Scheffler RM. Accountable care organizations: integrated care meets market power. J Health Polit Policy Law. 2015;40(4):639–645. doi: 10.1215/03616878-3149964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.