Abstract
Introduction
Nursing personnel have high risk for incidence of low back pain (LBP) followed by development of chronic pain and disability. Multiple risk factors such as patient handling, night shift work and lack of supporting work culture have been identified. In subacute LBP, high-fear avoidance is prognostic for more pain, disability and not returning to work. Lack of leisure-time physical activity predicts long-term sickness absence. The purpose of this study is to compare effectiveness of 6-month neuromuscular exercise and counselling in treating back pain in female nursing personnel with recurrent non-specific LBP pain compared with either (exercise or counselling) alone and a non-treatment control group.
Methods and analysis
The design is of a double-blinded four-arm randomised controlled trial with cost-effectiveness evaluation at 12 and 24 months. The study is conducted in 3 consecutive substudies. The main eligibility criteria are experience of LBP during the past 4 weeks with intensity of at least 2 (Numeric Rating Scale 0–10) and engagement in patient handling. Sample size was estimated for the primary outcome of pain intensity (visual analogue scale). Study measurements are outlined according to the model of International Classification of Functioning, Disability and Health, which incorporates the biopsychosocial processes assessed.
Ethics and dissemination
This study is carried out conforming to the guidelines of good scientific practice and provisions of the declaration of Helsinki. Increasing physical and mental capacity with interventions taking place immediately after working hours near the worksite may reduce development of chronic LBP and work disability in female nursing personnel with recurrent non-specific LBP.
Trial registration number
NCT04165698.
Keywords: Rehabilitation, Exercise, Education, Lumbar spine
Introduction
Low back pain (LBP) is a common occupational health problem in industrialised countries and the leading specific cause of years lived with disability.1 The lifetime prevalence of LBP is reported to be as high as 84%2 and 85–90% of the cases are classified as ‘non-specific’.3 The prevalence of chronic LBP pain is about 23%, with 11–12% of the population being disabled by it.2 The pain symptoms of about one-third of the population are episodic or recurrent rather than subacute or chronic.4 5 The costs of chronic LBP greatly exceed the costs of acute and subacute LBP,6 the costs of recurrent LBP probably account for between those of subacute and chronic LBP. The economic burden can be attributed to greater prescribing of pain-related medications and increased health resource utilisation.6
LBP in nursing personnel
Studies from across the globe have documented higher prevalence of LBP in nursing personnel compared with other occupations,7–9 the annual prevalence ranging from 45%10 to 77%.11 Nurses who engage in patient handling have especially high risk of developing persistent/chronic LBP.12 Persistent LBP in nurses causes considerable functional and work disability,8 and is a strong risk factor for long-term sickness absence13 and dropout from profession at early stages of their career.14 Furthermore, all but a few European countries are facing shortages of healthcare workers now, and will continue to do so in the future.15 Thus prevention of persistent LBP in nurses is a priority.
Biopsychosocial model in the treatment of LBP
Waddell16 introduced the biopsychosocial model over 25 years ago, to better understand the failures of strict biomedical informed treatment of LBP. The model has clearly not been successful in reducing LBP-related disability,1 however, according to an international expert paper,17 this may be a consequence of the mostly restrictive way the model has been understood and applied rather than a failure of the biopsychosocial model itself. Different interventions used to treat LBP may have differential effects on impairment, activity limitation and restricted participation.18 The WHO's International Classification of Functioning, Disability and Health (ie, the ICF-model) provides a useful reference to identify and quantify the biopsychosocial concepts contained in outcome assessment in clinical trials.19 Nursing personnel are part of a group of LBP patients who surely benefit from a multidisciplinary approach due to the high demands of their work on physical capacity,9 20 21 as well as workplace-related psychosocial stress factors.21–23
Prognostic factors of chronic non-specific LBP with emphasis on studies in nursing personnel
Knowledge of the prognostic physical, psychosocial and clinical factors with worse or better disease outcome serve as one base to plan effective interventions.24 Nursing includes a lot of heavy physical work that may be back breaking due to lifting and transferring patients, and that may lead to ergonomically poor postures such as from working in a stooped position with a twisted back.9 10 12 25 A systematic review25 showed that nursing activities conferred increased risk for, and were associated with, back disorders regardless of nursing technique, personal characteristics and non-work-related factors. Patient handling had the highest risk in a dose–response manner. Associations were strong, consistent, temporally possible, plausible, coherent and analogous to other exposure-outcomes, indicating a causal relationship.25 Thus patient handling could result in tissue damage leading to accelerated lumbar spine disease and LBP.26
Psychosocial factors are believed to influence the development of chronic LBP. The Fear Avoidance Model27 is widely used to explain how psychological factors (fear, beliefs, catastrophising and kinesiophobia) affect the experience of pain and the development of chronic pain and disability.28 There is clear predictive value of fear-avoidance beliefs (FABs) and future outcomes of LBP.29 30 A person with fear-avoidance behaviour will avoid physical activities expected to increased pain.31 Among healthcare workers with previous LBP, FABs were major risk factors for new episodes of LBP.32 In two recent reviews, a high score of FABs was prognostic for not returning to work,33 34 and more pain and disability34 in subacute patients with LBP up to 6 months in duration. A decrease in FAB score during treatment was also associated with less pain and disability at follow-up.34
The role of psychosocial factors at work in relation to LBP and its consequences is still controversial. The methodological problems in the majority of published studies have limited the result interpretations of former reviews.23 35 Night shift work, perceived lack of support from superiors and lack of supporting culture in the work unit have been associated with an increased risk of intense LBP21 and related sick leaves in nurses’ aides.22 More recently, psychological and social factors at work were associated with FABs about work, and they explained 39% of FABs in patients on sick leave due to neck or back pain.36
Individual risk factors with at least reasonable evidence of a causal relationship for the development of work-related musculoskeletal disorders, including LBP, are smoking, high body mass index and the presence of comorbidities.37 Changes in pain and disability at 3 months of the initial period had prognostic value on the development of chronic non-specific LBP (NSLBP) in workers on sick leave due to subacute NSLBP.24 Physical deconditioning38 in combination with psychosocial factors has been hypothesised to compromise recovery from LBP. However, there is a lack of longitudinal studies designed to specifically investigate physical activity (PA) as an independent prognostic factor for chronic NSLBP.39 The results from former reviews40 41 are limited in terms of poor quality of PA measurement and heterogeneity of study designs.
Effectiveness of exercise and counselling interventions to prevent chronic NSLBP
Contemporary evidence on interventions to prevent chronic LBP emphasises the biopsychosocial approach.42 However, exercise and counselling interventions targeted to subacute patients are scarce compared with those for chronic patients. A former review43 stated there was moderate quality evidence that post-treatment exercise can reduce recurrences of back pain, however, the results of exercise treatment studies were conflicting and it was impossible to specify the content of an effective programme. A later review on subacute LBP44 reported conflicting evidence on effectiveness of intense physical conditioning combined with usual care compared with usual care alone.
Among the wide range of psychosocial risk factors, research has focused mainly on pain beliefs and coping skills, with disappointing results:45 (1) there is high-quality evidence for the absence of significant difference between those who received information and those who received usual care with reference to outcomes of pain, function, work issues and healthcare use, (2) cognitive behavioural therapy showed very low-quality evidence of moderate effectiveness for pain, function, quality of life, work issues and healthcare use, and (3) was probably not superior to physical conditioning. There is no evidence about the effects of lifting and transfer technique guidance on LBP and disability among the population in general,46 or among nurses in particular.47 However, guidance combined with physical training reduced disability among nurses with LBP,47 and reduced pain and improved self-evaluated future work ability in male railroad workers.48
Methods and analysis
Objective
This randomised controlled trial (RCT) primarily aims to compare the effectiveness of 6-month exercise and counselling programmes to treat pain in female nursing personnel with recurrent NSLBP compared with either (exercise or counselling) alone and a non-treatment control group. Effectiveness will be analysed after the 6-month interventions, and after 12 and 24 months of follow-up. Cost-effectiveness analyses will be conducted after 12 and 24 months of follow-up. The secondary aims are to compare the effectiveness of the interventions as well as individuals’ leisure-time PA on the outcome measures proposed according to the ICF-model.
Primary hypothesis
H1: Together, neuromuscular exercise (NME) and back counselling (BC) will have a stronger influence on intensity of LBP than either alone. This also applies to the other outcome measures within the framework of the ICF-model.
Secondary hypotheses
H2: NME will improve the motor control of lumbar neutral zone (NZ), trunk muscular strength and endurance, leg strength and agility, and decrease perceived musculoskeletal exertion and tiredness after work, and thus decrease LBP and movement control impairment by 30% compared with non-exercise groups (counselling-only and control).
H3: BC will improve the awareness and skills to avoid harmful loading of the back during work and leisure-time, help to better cope with episodes of LBP and increase leisure-time PA, and thus decrease intensity of LBP and fear avoidance by 30% when compared with non-counselling groups (exercise-only and control).
H4: Specific baseline characteristics of participants will moderate or predict the compliance in interventions, which will affect pretreatment to post-treatment changes in the targeted physical impairments, cognitions and behaviours.
Trial design
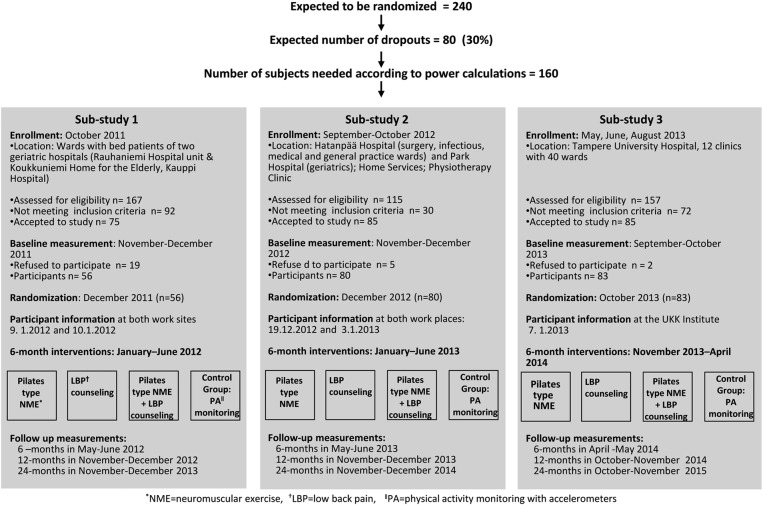
This study is an ongoing (not recruiting/finished with intervention periods/past 24-month follow-up measurements unfinished) double-blinded four-arm RCT of a 6-month intervention with a cost-effectiveness evaluation at 24 months. Participants were randomly assigned into one of four groups: (1) NME and BC for cognitive behavioural change, (2) NME-only, (3) BC-only and (4) control. The study is conducted in three parts (substudies 1–3), which started in three consecutive years (2011–2013) in the city of Tampere, Finland. Measurements are taken at baseline, immediately following the intervention (6 months), and after 12-month and 24-month follow-up periods. The study protocol and time frame of each substudy are presented in figure 1.
Figure 1.
Enrollment of the study participants, setting and time points for screening, randomisation, and baseline and follow-up measurements in the three sub-studies.
Target population and recruitment
The target population is female nursing personnel from wards with bed patients or other nursing tasks that include patient lifting, transferring or otherwise awkward body postures for the lower back. In this paper, ‘nursing personnel’ refers to all healthcare professions listed in figure 1.
To be eligible, participants should fulfil the following criteria:
Woman aged 30–55 years;
Has worked at her current job for at least 12 months;
Intensity of LBP on Numeric Rating Scale (scale 0–10) at least two during the past 4 weeks.49
Exclusion criteria for the study are:
Serious former back injury (fracture, surgery, disc protrusion);
Chronic LBP defined by a physician or self-reporting of continuous LBP of 7 months or more;
Other serious disease or symptoms that limit participation in moderate intensity NME;
Engagement in neuromuscular-type exercise more than once a week;
Pregnant or recently delivered (<12 months).
To recruit participants, the head nurses of four municipal hospitals, a home service and physiotherapy unit, and a university hospital in Tampere, Finland, were contacted by an email letter that included short information on the study. After that they were reached by phone. All of the contacted units required a written study plan and a copy of the approval of the ethics committee for official permission to screen their personnel for the study. After that, meetings were arranged with the personnel of the wards and/or groups of head nurses. Short presentations on the eligibility and contents of the study were given, and screening questionnaires were spread out. In addition, the physicians of the occupational healthcare unit of Tampere city disseminated screening questionnaires to their patients (only nursing personnel) with LBP. Screening questionnaires were collected in ‘mail boxes’ within the wards when appropriate. Internal mail and prepaid envelopes were also used to collect questionnaires directly in the research institute conducting the study. Records of screening were maintained for both included and excluded individuals, to document the criteria for both. More information on screening of each substudy is given in figure 1.
Sample size calculations
Sample size was estimated for the primary outcome of pain intensity (visual analogue scale, VAS), with emphasis on the proportion (%) of patients with improved LBP on VAS. The minimal important change for VAS is expected to be 15 mm.50 Accordingly, it was expected that there would be a minimal difference of 20% units between the intervention groups in proportions of patients with improved VAS (at least 15 mm). The proportion of participants in controls with improved VAS was expected to be 15%. Thus, in order to detect a difference in main effects (ie, exercisers vs non-exercisers/counselling vs non-counselling) with a significance level of 0.05 and a power of 80%, at least 160 participants were needed for the study (40 in each study group). For compensation of probable loss of participants in follow-up, the aim was to recruit a total of 240 nurses.
Randomisation and blinding
A method of sequentially numbered sealed envelopes was used in all three substudies, to assign participants into four study groups. At baseline measurements, once a participant had consented to enter the study, an envelope (next in order) was opened and the participant was then offered the allocated study group as well as information relevant to practical participation. The personnel conducting study measurements will be blinded to group allocation. The statistician and the outcome assessors will be blind to group allocation until completion of the statistical analyses.
Interventions (treatment arms)
In all three substudies, the intervention groups of NME and BC were organised near the work places of the nurses. Group sessions were provided from Monday to Friday, starting 15 min later than the typical work shifts ended. For those allocated to the group of combined NME and BC, it was possible to participate first in exercise and, an hour later, in counselling. Leaders of both intervention groups listed the participating individuals at the beginning of each exercise/counselling session to monitor adherence.
The common feature of the two interventions (NME and BC) is that both aim at reducing the intensity and recurrence of LBP by improving the control of the lumbar NZ, and specifically avoiding full lumbar flexion.48 51 The theoretical basis of this is the hypothesis of micro-damage, which is linked to acute repetitive lumbar syndrome, occurring in spinal ligaments, discs, facets and capsules.52–55 As the damage exceeds a certain threshold due to high loads, many repetitions and/or insufficient rest, an acute inflammation is triggered.54 55 This, in turn, elicits hyperexcitability of lumbar muscles (ie, neuromuscular dysfunction) in order to protect the soft tissue from further damage.
Neuromuscular exercise
The overall aim of NME is to restore pain-induced disturbances of movement control, and to increase muscle strength and endurance needed in heavy nursing tasks. The learning objectives of the first 7 weeks is to learn the right performance technique and control of the lumbar NZ,48 51 56 and combining breathing to each exercise.57 At the second and third levels, the programme is progressive in terms of demands for coordination, balance,58 and muscular strength and endurance.59 General training principles and specific objectives of the key exercises and their progression are described in online supplementary additional file 1. The instructors of NME were experienced exercise leaders and were specially educated for the targets and contents of the programme.
bmjsem-2015-000098supp_appendix1.pdf (7.3MB, pdf)
During the first 8 weeks, the goal is to participate in instructed exercise sessions twice a week, and during the next 16 weeks, in one instructed session and one home session with the help of a digital video disc or booklet produced for the study. After 6 months of intervention, the participants are encouraged to continue exercising at home. In addition, two instructed exercise sessions are provided at the beginning of the active follow-up time from 7 to 12 months.
Back pain counselling
The theory of cognitive-behavioural learning is the frame for BC,60 61 and problem based learning the method to implement it. The main aims of BC are a positive change in PA-related FABs and behaviour, and improved self-efficacy in managing future episodes of LBP. The premises for the aforementioned positive changes are that participants learn less harmful ways to perform daily activities,48 51 gain positive experiences from PA,28 and discover that they can understand and rule their back pain.28 The key messages and learning tasks of the BC sessions are presented in online supplementary additional file 2.
bmjsem-2015-000098supp_appendix2.pdf (1.5MB, pdf)
The specific topics of the 10 counselling sessions are as follows: (1) The natural history of LBP—why do we experience pain? (2) Control of the lumbar NZ helps to avoid harmful loading; (3) You do not need to fear the pain; (4) Physical inactivity and sedentary behaviour are ‘poison’ for the back; (5) You have the same back 24 h a day; (6) Choose an active strategy to cope with LBP; (7) Take care of your well-being: sleep and nutrition in shift work; (8) Is sitting or standing problematic for your back? (9) Did you learn what you expected to? and (10) Rehearsal of the main topics 1–4 of BC. An additional session after 6-month follow-up measurements is provided to renew the personal Physical Activity Pie Chart (see online supplementary additional file 2).
The 6-month intervention includes the above described 10 structured group sessions, each lasting 45 min and including between sessions learning tasks for each topic. During the first 4 weeks of the intervention, participants are expected to attend BC sessions once a week, and after that, on every third week. Participants are provided with a personal folder, in which they gather the material of each group session including lectures and material for learning tasks. After the 6-month intervention and follow-up measurements, an additional counselling session is organised to reinforce the maintenance of possible new behaviours. Three specially educated physiotherapists will instruct the group sessions. They will discuss the contents and learning tasks of each topic before group sessions to ensure standard implementation during each substudy.
Feedback to study participants
Individuals in all substudies, and study groups (including the control group), will be provided with standard written information on their physical fitness (fitness category, change in fitness) after the 6-month follow-up measurements. Similarly, after the endpoint of the study (24-months) participants will be provided with a similar type of information on their fitness and objectively measured PA at all the four measurement points (the past 24-month feedback meeting of substudy 3 will take place in 3/2/2016).
Baseline and outcome measures and data collection time points
Outcome measures, outlined according to the ICF-model in table 1, are assessed at baseline, immediately after 6-month interventions and at follow-ups of 12 and 24 months. Participants missing their follow-up measurements are reached by the research secretary for a new measurement appointment. In addition to listed measures in table 1, demographic data (age, civil status, level of education), personal data related to work (nursing profession, working years at current position, type of work shift), smoking habits and hormonal status related to menopause, are assessed. Measurements related to development of research methods and collected at selected substudies are described at the end of table 1.
Table 1.
Outcome measurements of the NURSE-RCT and other data for methods development
| Domain | Measurement |
|---|---|
| Primary outcome | |
| Body structure and functions | |
| Low back pain | Pain intensity: visual analogue scale 0–100 mm during the past month* |
| Secondary outcomes | |
| Musculoskeletal pain |
|
| Musculoskeletal exertion† |
|
| Sleep and recovery from work† | Tiredness in the morning, tiredness during the day, sleepiness during the day, recovery after work: Numeric Rating Scale 1–5* |
| Mental well-being | Beck Depression Inventory (9 items)*‡ |
| Activity limitations | |
| Movement control dysfunction | MCI test battery* |
| Motor skill: static balance§ | One-leg stand |
| Motor skill: gross movement timing§ | Rhythm coordination test* |
| Range of motion: trunk§ | Trunk side-bending* |
| Range of motion: upper-body§ | Shoulder neck mobility* |
| Muscular fitness: trunk§ | Dynamic sit-ups |
| Body composition | Weight, height, body mass index |
| Motor skill: agility§ | Running figure of 8 functional fitness test* |
| Muscular fitness: upper-body and trunk§ | Modified push-ups; functional fitness test* |
| Muscular fitness: leg power§ | Vertical jump; functional fitness test* |
| Muscular fitness: leg strength§ | One-leg squat (forward); functional fitness test* |
| Aerobic fitness: walking | 6 min walk test; functional fitness test |
| Limitations in self-reported activities | Patient specific functional scale |
| Participation | |
| Physical activity and sedentary behaviour | Objective assessment with accelerometer for 7 days (Hookie AM20 tri-axial accelerometer, Traxmeet, Espoo, Finland) |
| Physical activity and exercise diary | Recorded for the 7 days when using the accelerometer |
| Physical activity recommendation¶ | Standard Finnish Questionnaire assessing the fulfilment of current recommendation for weekly physical activity |
| Health-related quality of life | Rand 36-item health survey questionnaire |
| Self-reported work ability† | WAI: four standard questions |
| Environmental factors | |
| Psychosocial factors at work† | Selected items of a Finnish questionnaire* |
| Individual factors | |
| Fear avoidance** | Fear-avoidance beliefs questionnaire* |
| Methods development | |
| Body structure and functioning | |
| Functioning of the autonomic nervous system (substudies 1 and 2) | Measurements of heart-rate variability during two working days and one leisure day |
| Activity limitations | |
| Physical functioning in nursing tasks | Ability to manage with heavy, task specific nursing duties including patient transfer: Numeric Rating Scale 0–10 with 21 selection points*‡ |
| Motion analysis (substudy 3) | IMU system (Valedo Research, Hocoma AG, Volketswil, Switzerland)†† |
*Assessment of test-retest repeatability.
†Standard questionnaire developed by the Finnish Institute of Occupational Health, Finland.
‡Assessment of construct validity.
§Standard method developed by the UKK Institute, Tampere, Finland.
¶Standard method developed by the UKK Institute and National Institute of Health and Well-being, Finland.
**Finnish version, translated and validated by Orton, Helsinki, Finland.
††Assessment of validity of IMU to detect MCIs and their changes.
IMU, inertial measurement unit; MCI, movement control impairment; NURSE-RCT, prevention of chronic low back pain in female nurses; WAI, Work Ability Index.
Data analysis
The between-group differences at 6-month, 12-month and 24-month follow-up will be analysed by generalised linear mixed models. The analyses are based on a 2×2 factorial design (1=exercise and counselling, 2=exercise only, 3=counselling only and 4=control) as the factor variables. The baseline measurements and selected individual, clinical, physical and psychosocial factors indicating associations with the outcome measures will be used as confounding variables according to the strength of their impact.
Selected items of psychosocial factors at work, smoking and use of hormone-replacement therapy will be used as known confounding factors in all statistical analysis of effectiveness. All participants are invited to all follow-up measurements regardless of lacking participation in interventions. The results will be analysed primarily according to an intention-to-treat principle. With a view to adjust for the possible bias due to incomplete data, the missing values will be imputed and statistical analyses performed using a multiple imputation strategy.
Cost-effectiveness analysis
Cost-effectiveness analysis will be based on self-report diaries recoded for the past 6 months before the study, and for each later 6-month period up to 24 months. The diary includes information on use of pain medication for LBP, visits to physician/physiotherapist/other treatment due to LBP and sickness absences due to LBP. To evaluate cost-effectiveness, the differences between groups will be analysed via a non-parametric bootstrap approach. Cost-effectiveness will be expressed in terms of the incremental cost-effectiveness ratio, which indicates the amount of money required to decrease intensity of LBP and increase quality-adjusted life years.
Ethics and dissemination
This study is carried out confirming to the guidelines of good scientific practice and provisions of the Finnish Medical Research Act (declaration of Helsinki). The aim of the study, as well as risks and benefits, were clarified in a written information letter to those recruited to the study. They were encouraged to continue their usual PA and seek any medical or other treatments when needed. All participants gave their written consent to a research secretary at the beginning of the baseline measurements. Approval for the study protocol was received from the Ethical Committee of Pirkanmaa Hospital District (ETL code R08157).
Significance of the study
Municipal hospitals are stressful work environments and shift work places an additional strain on nursing personnel. The physical load of patient handling is considerable and one of the main reasons for dropout of profession at early stages of career.14 LBP is more common among nurses than any other occupational group, with high rates of sickness absence and early retirement. There is no doubt that effective interventions to tackle this worldwide problem are needed. Increasing physical and mental capacity with interventions taking place immediately after working hours near the worksite may represent a useful approach for reducing development of chronic pain and work disability in female nurses.
The main aims of the Pilates type NME are to improve the movement control of lumbar NZ and neuromuscular fitness of nurses, who are engaged in strenuous patient lifting, transferring or otherwise awkward body postures at their work. The rationale is based on the revolution hypothesis of chronic back pain by Panjabi,52 which is strongly connected to sensorimotor aspects of the spinal stabilising system55 (see methods). The main effects of NME are proposed to induce positive biological effects on the body including experience of pain62 and mental health.63 The specific mode of inhaling and exhaling during each exercise is expected to have positive effects on the autonomic nervous system.64
The rationale of the BC is to provide new ideas, experiences and skills to perform nursing tasks in a more back-friendly way,51 which will help to avoid reinjury and related new episodes of LBP, and to adopt the same safe manners in everyday life outside work. Encouragement and advice for self-care and management of pain is the way to increase self-efficacy to better cope with future pain episodes.28 Promotion of active work commuting and leisure-time PA, as well as introducing the multiple positive health effects of PA aim at reducing fear of pain related to physical activities.
Strengths and weaknesses of the study
The biopsychosocial approach with wide range of measurements including outcome measures, and prognostic or/and moderating factors are the major strengths of the present study. Objective measurements of PA, sedentary behaviour and physical fitness offer a valuable novel opportunity to study their prognostic value for physical functioning, workability and quality of life among nurses with recurrent NSLBP. The former experience of the present authors in conducting interventions to reduce LBP48 51 as well as other musculoskeletal injuries65 66 is an advantage that helps to design relevant and up-to-date contents to the interventions, and to manage their implementation.
The study was not designed to change the work or work environment of the participating female nurses. In addition, the workplaces were different in each substudy and even within substudies. Thus it is possible that the differences in work and work environment will have an effect on the results of this study, despite the possibility of controlling many of them with the broad range of data gathered. The shift work of many of the participants is a challenge that may increase the number of dropouts during the study, and thus jeopardise the feasibility and credibility of the interventions.
Impacts of the study
The target group of the present study is such that the risk of new episodes of LBP is high. Thus, the risk of gradual decrease in physical functioning, work ability and quality of life is increased. If the described interventions, designed to recurrent NSLBP, turn out to be effective in reducing pain and improving pain-related behaviour at reasonable costs, they will offer new ‘ready to use practical tools’ to prevent sickness absence and early retirement in nursing personnel as well as in other women workers with jobs that are physically strenuous for the back.
Physical therapists are health professionals who are mainly responsible for conducting both exercise and counselling interventions among patients with LBP with or without the help of experts in psychosocial problems. The described interventions provide rationale and materials for this purpose. In addition, the prospective evaluations of the predictive factors for adverse/positive outcomes at 24 months will provide knowledge on the usefulness of the study measurements (PA, fitness, questionnaires) among female nursing personnel as practical screening tools for early detection of those with increased risk of persistent LBP and in need of targeted interventions.
Footnotes
Funding: The study has been funded by the Social Insurance Institution of Finland 37/26/2011 and Pirkanmaa Hospital District, Tampere, Finland 9K127 and 9M099.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Ethical Committee of Pirkanmaa Hospital District, Tampere, Finland.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balagué F, Mannion AF, Pellisé F et al. Non-specific low back pain. Lancet 2012;379:482–91. 10.1016/S0140-6736(11)60610-7 [DOI] [PubMed] [Google Scholar]
- 3.Krismer M, van Tulder M, Low Back Pain Group of the Bone and Joint Health Strategies for Europe Project. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific). Best Pract Res Clin Rheumatol 2007;21:77–91. 10.1016/j.berh.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 4.Lemeunier N, Leboeuf-Yde C, Gagey O. The natural course of low back pain: a systematic critical literature review. Chiropr Man Therap 2012;20:33 10.1186/2045-709X-20-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamcan O, Mannion AF, Eisenring C et al. The course of chronic and recurrent low back pain in the general population. Pain 2010;150:451–7. 10.1016/j.pain.2010.05.019 [DOI] [PubMed] [Google Scholar]
- 6.Gore M, Sadosky A, Stacey BR et al. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012;37:E668–77. 10.1097/BRS.0b013e318241e5de [DOI] [PubMed] [Google Scholar]
- 7.Hignett S. Work-related back pain in nurses. J Adv Nurs 1996;23:1238–46. 10.1046/j.1365-2648.1996.13423.x [DOI] [PubMed] [Google Scholar]
- 8.Harcombe H, Herbison GP, McBride D et al. Musculoskeletal disorders among nurses compared with two other occupational groups. Occup Med (Lond) 2014;64:601–7. 10.1093/occmed/kqu117 [DOI] [PubMed] [Google Scholar]
- 9.Yassi A, Lockhart K. Work-relatedness of low back pain in nursing personnel: a systematic review. Int J Occup Environ Health 2013;19:223–44. 10.1179/2049396713Y.0000000027 [DOI] [PubMed] [Google Scholar]
- 10.Smedley J, Egger P, Cooper C et al. Manual handling activities and risk of low back pain in nurses. Occup Environ Med 1995;52:160–3. 10.1136/oem.52.3.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karahan A, Kav S, Abbasoglu A et al. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs 2009;65:516–24. 10.1111/j.1365-2648.2008.04905.x [DOI] [PubMed] [Google Scholar]
- 12.Holtermann A, Clausen T, Jørgensen MB et al. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand J Work Environ Health 2013;39:164–9. 10.5271/sjweh.3329 [DOI] [PubMed] [Google Scholar]
- 13.Andersen LL, Clausen T, Mortensen OS et al. A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int Arch Occup Environ Health 2012;85:615–22. 10.1007/s00420-011-0709-5 [DOI] [PubMed] [Google Scholar]
- 14.Faber A, Giver H, Strøyer J et al. Are low back pain and low physical capacity risk indicators for dropout among recently qualified eldercare workers? A follow-up study. Scand J Public Health 2010;38:810–16. 10.1177/1403494810379891 [DOI] [PubMed] [Google Scholar]
- 15.Bevan S QT, McGee R, Mahdon M et al. Fit for work—musculoskeletal disorders in the European workforce. London: The Work Foundation, 2009. [Google Scholar]
- 16.Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine 1987;12:632–44. 10.1097/00007632-198709000-00002 [DOI] [PubMed] [Google Scholar]
- 17.Pincus T, Kent P, Bronfort G et al. Twenty-five years with the biopsychosocial model of low back pain—is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine 2013;38:2118–23. 10.1097/BRS.0b013e3182a8c5d6 [DOI] [PubMed] [Google Scholar]
- 18.Ayis S, Arden N, Doherty M et al. Applying the impairment, activity limitation, and participation restriction constructs of the ICF model to osteoarthritis and low back pain trials: a reanalysis. J Rheumatol 2010;37:1923–31. 10.3899/jrheum.091332 [DOI] [PubMed] [Google Scholar]
- 19.Brockow T, Cieza A, Kuhlow H et al. Identifying the concepts contained in outcome measures of clinical trials on musculoskeletal disorders and chronic widespread pain using the International Classification of Functioning, Disability and Health as a reference. J Rehabil Med 2004;(44 Suppl):30–6. 10.1080/16501960410015371 [DOI] [PubMed] [Google Scholar]
- 20.Schlossmacher R, Amaral FG. Low back injuries related to nursing professionals working conditions: a systematic review. Work 2012;41(Suppl 1):5737–8. 10.3233/WOR-2012-0935-5737 [DOI] [PubMed] [Google Scholar]
- 21.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med 2004;61:398–404. 10.1136/oem.2003.008482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of sickness absence: a three month prospective study of nurses’ aides. Occup Environ Med 2003;60:271–8. 10.1136/oem.60.4.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hartvigsen J, Lings S, Leboeuf-Yde C et al. Psychosocial factors at work in relation to low back pain and consequences of low back pain; a systematic, critical review of prospective cohort studies. Occup Environ Med 2004;61:e2. [PMC free article] [PubMed] [Google Scholar]
- 24.Heymans MW, van Buuren S, Knol DL et al. The prognosis of chronic low back pain is determined by changes in pain and disability in the initial period. Spine J 2010;10:847–56. 10.1016/j.spinee.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 25.Roffey DM, Wai EK, Bishop P et al. Causal assessment of workplace manual handling or assisting patients and low back pain: results of a systematic review. Spine J 2010;10:639–51. 10.1016/j.spinee.2010.04.028 [DOI] [PubMed] [Google Scholar]
- 26.Seidler A, Euler U, Bolm-Audorff U et al. Physical workload and accelerated occurrence of lumbar spine diseases: risk and rate advancement periods in a German multicenter case-control study. Scand J Work Environ Health 2011;37:30–6. 10.5271/sjweh.3121 [DOI] [PubMed] [Google Scholar]
- 27.Waddell G, Newton M, Henderson I et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52:157–68. 10.1016/0304-3959(93)90127-B [DOI] [PubMed] [Google Scholar]
- 28.Linton SJ, Shaw WS. Impact of psychological factors in the experience of pain. Phys Ther 2011;91:700–11. 10.2522/ptj.20100330 [DOI] [PubMed] [Google Scholar]
- 29.Wideman TH, Asmundson GG, Smeets RJ et al. Rethinking the fear avoidance model: toward a multidimensional framework of pain-related disability. Pain 2013;154:2262–5. 10.1016/j.pain.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lundberg M, Grimby-Ekman A, Verbunt J et al. Pain-related fear: a critical review of the related measures. Pain Res Treat 2011;2011:494196 10.1155/2011/494196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leeuw M, Goossens ME, Linton SJ et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007;30:77–94. 10.1007/s10865-006-9085-0 [DOI] [PubMed] [Google Scholar]
- 32.Jensen JN, Karpatschof B, Labriola M et al. Do fear-avoidance beliefs play a role on the association between low back pain and sickness absence? A prospective cohort study among female health care workers. J Occup Environ Med 2010;52:85–90. 10.1097/JOM.0b013e3181c95b9e [DOI] [PubMed] [Google Scholar]
- 33.Wertli MM, Rasmussen-Barr E, Weiser S et al. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. Spine J 2014;14:816–36.e4. 10.1016/j.spinee.2013.09.036 [DOI] [PubMed] [Google Scholar]
- 34.Wertli MM, Rasmussen-Barr E, Held U et al. Fear-avoidance beliefs—a moderator of treatment efficacy in patients with low back pain: a systematic review. Spine J 2014;14:2658–78. 10.1016/j.spinee.2014.02.033 [DOI] [PubMed] [Google Scholar]
- 35.Macfarlane GJ, Pallewatte N, Paudyal P et al. Evaluation of work-related psychosocial factors and regional musculoskeletal pain: results from a EULAR Task Force. Ann Rheum Dis 2009;68:885–91. 10.1136/ard.2008.090829 [DOI] [PubMed] [Google Scholar]
- 36.Myhre K, Røe C, Marchand GH et al. Fear-avoidance beliefs associated with perceived psychological and social factors at work among patients with neck and back pain: a cross-sectional multicentre study. BMC Musculoskelet Disord 2013;14:329 10.1186/1471-2474-14-329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med 2010;53:285–323. 10.1002/ajim.20750 [DOI] [PubMed] [Google Scholar]
- 38.Verbunt JA, Smeets RJ, Wittink HM. Cause or effect? Deconditioning and chronic low back pain. Pain 2010;149:428–30. 10.1016/j.pain.2010.01.020 [DOI] [PubMed] [Google Scholar]
- 39.Hendrick P, Milosavljevic S, Hale L et al. The relationship between physical activity and low back pain outcomes: a systematic review of observational studies. Eur Spine J 2011;20:464–74. 10.1007/s00586-010-1616-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hendrick P, Te Wake AM, Tikkisetty AS et al. The effectiveness of walking as an intervention for low back pain: a systematic review. Eur Spine J 2010;19:1613–20. 10.1007/s00586-010-1412-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin CW, McAuley JH, Macedo L et al. Relationship between physical activity and disability in low back pain: a systematic review and meta-analysis. Pain 2011;152:607–13. 10.1016/j.pain.2010.11.034 [DOI] [PubMed] [Google Scholar]
- 42.Weiner BK. Spine update: the biopsychosocial model and spine care. Spine 2008;33:219–23. 10.1097/BRS.0b013e3181604572 [DOI] [PubMed] [Google Scholar]
- 43.Choi BK, Verbeek JH, Tam WW et al. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev 2010;(1):CD006555 10.1002/14651858.CD006555.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schaafsma FG, Whelan K, van der Beek AJ et al. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013;8:CD001822 10.1002/14651858.CD001822.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ramond-Roquin A, Bouton C, Gobin-Tempereau AS et al. Interventions focusing on psychosocial risk factors for patients with non-chronic low back pain in primary care—a systematic review. Fam Pract 2014;31:379–88. 10.1093/fampra/cmu008 [DOI] [PubMed] [Google Scholar]
- 46.Martimo KP, Verbeek J, Karppinen J et al. Effect of training and lifting equipment for preventing back pain in lifting and handling: systematic review. BMJ 2008;336:429–31. 10.1136/bmj.39463.418380.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Warming S, Ebbehøj NE, Wiese N et al. Little effect of transfer technique instruction and physical fitness training in reducing low back pain among nurses: a cluster randomised intervention study. Ergonomics 2008;51:1530–48. 10.1080/00140130802238606 [DOI] [PubMed] [Google Scholar]
- 48.Suni J, Rinne M, Natri A et al. Control of the lumbar neutral zone decreases low back pain and improves self-evaluated work ability: a 12-month randomized controlled study. Spine 2006;31:E611–20. 10.1097/01.brs.0000231701.76452.05 [DOI] [PubMed] [Google Scholar]
- 49.Dionne CE, Dunn KM, Croft PR et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine 2008;33:95–103. 10.1097/BRS.0b013e31815e7f94 [DOI] [PubMed] [Google Scholar]
- 50.Ostelo RW, Deyo RA, Stratford P et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 2008;33:90–4. 10.1097/BRS.0b013e31815e3a10 [DOI] [PubMed] [Google Scholar]
- 51.Suni JH, Taanila H, Mattila VM et al. Neuromuscular exercise and counseling decrease absenteeism due to low back pain in young conscripts: a randomized, population-based primary prevention study. Spine 2013;38:375–84. 10.1097/BRS.0b013e318270a12d [DOI] [PubMed] [Google Scholar]
- 52.Panjabi MM. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J 2006;15:668–76. 10.1007/s00586-005-0925-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Courville A, Sbriccoli P, Zhou BH et al. Short rest periods after static lumbar flexion are a risk factor for cumulative low back disorder. J Electromyogr Kinesiol 2005;15:37–52. 10.1016/j.jelekin.2004.06.005 [DOI] [PubMed] [Google Scholar]
- 54.Le P, Solomonow M, Zhou BH et al. Cyclic load magnitude is a risk factor for a cumulative lower back disorder. J Occup Environ Med 2007;49:375–87. 10.1097/JOM.0b013e318046eb0b [DOI] [PubMed] [Google Scholar]
- 55.Solomonow M. Neuromuscular manifestations of viscoelastic tissue degradation following high and low risk repetitive lumbar flexion. J Electromyogr Kinesiol 2012;22:155–75. 10.1016/j.jelekin.2011.11.008 [DOI] [PubMed] [Google Scholar]
- 56.Cholewicki J, Panjabi MM, Khachatryan A. Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture. Spine 1997;22:2207–12. 10.1097/00007632-199710010-00003 [DOI] [PubMed] [Google Scholar]
- 57.Hodges PW, Eriksson AE, Shirley D et al. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech 2005;38:1873–80. 10.1016/j.jbiomech.2004.08.016 [DOI] [PubMed] [Google Scholar]
- 58.Taube W, Gruber M, Gollhofer A. Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiol (Oxf) 2008;193:101–16. 10.1111/j.1748-1716.2008.01850.x [DOI] [PubMed] [Google Scholar]
- 59.Kavcic N, Grenier S, McGill SM. Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises. Spine 2004;29:2319–29. 10.1097/01.brs.0000142222.62203.67 [DOI] [PubMed] [Google Scholar]
- 60.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000;85:317–32. 10.1016/S0304-3959(99)00242-0 [DOI] [PubMed] [Google Scholar]
- 61.Vlaeyen JW, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain 2012;153:1144–7. 10.1016/j.pain.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 62.Sluka KA, O'Donnell JM, Danielson J et al. Regular physical activity prevents development of chronic pain and activation of central neurons. J Appl Physiol 2013;114:725–33. 10.1152/japplphysiol.01317.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Helgadóttir B, Forsell Y, Ekblom Ö. Physical activity patterns of people affected by depressive and anxiety disorders as measured by accelerometers: a cross-sectional study. PLoS ONE 2015;10:e0115894 10.1371/journal.pone.0115894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gockel M, Lindholm H, Niemistö L et al. Perceived disability but not pain is connected with autonomic nervous function among patients with chronic low back pain. J Rehabil Med 2008;40:355–8. 10.2340/16501977-0172 [DOI] [PubMed] [Google Scholar]
- 65.Pasanen K, Parkkari J, Pasanen M et al. Neuromuscular training and the risk of leg injuries in female floorball players: cluster randomised controlled study. BMJ 2008;337:a295 10.1136/bmj.a295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Parkkari J, Taanila H, Suni J et al. Neuromuscular training with injury prevention counselling to decrease the risk of acute musculoskeletal injury in young men during military service: a population-based, randomised study. BMC Med 2011;9:35 10.1186/1741-7015-9-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2015-000098supp_appendix1.pdf (7.3MB, pdf)
bmjsem-2015-000098supp_appendix2.pdf (1.5MB, pdf)