Abstract
Background
Femoroacetabular impingement (FAI) is common with an estimated prevalence of 10–15% among young active individuals. The natural history of the disorder is progression to early osteoarthritis. Hip arthroscopy is recommended if conservative treatments fail; however, outcomes are unclear, particularly in highly active populations.
Aim
To evaluate the functional and vocational outcome of hip arthroscopy, as part of an evidence-based rehabilitation hip pain pathway, for the treatment of FAI in an active military population.
Methods
All patients in the defence rehabilitation hip pain pathway, with a confirmed diagnosis of FAI who failed conservative treatment, were assessed prior to surgery and at 2, 6 and 12 months postsurgery. Outcome measures included the Visual Analogue Scale (VAS) for hip pain, Non-Arthritic Hip Score (NAHS) for function, and vocational assessments including functional activity assessment (FAA) and Joint Medical Employment Standard for military employability and deployability.
Results
101 patients completed the study (mean age=33 years) (male:female:75:26) (Royal Navy/British Army/Royal Air Force: 13%/48%/39%). Outcomes demonstrated significant improvements with large effect size. Preoperative NAHS mean=62.9 (SD 16.4), 12-month postoperative NAHS mean=78.8 (18.3), mean improvement in NAHS=15.9 (95% CI 12.3 to 19.5, p<0.001). Preoperative VAS pain mean=51.3 (20.9), 12-month postoperative VAS pain=25.6 (24.5). Mean improvement 25.7 (95% CI 19.4 to 31.99, p<0.001). 73% of patients had a deployable medical category at 12 months postoperative.
Conclusions
These data confirm that hip arthroscopy as part of a structured evidence-based multidisciplinary care pathway produces significant and continued symptomatic, functional and vocational improvements over a 12-month period in a military population exposed to high intensity, weight-bearing exercise in uncontrolled and unforgiving environments.
Keywords: Hip, Rehabilitation, Arthroscopy
What are the new findings?
Hip arthroscopy for femoroacetabular impingement has excellent outcomes when part of a structured multidisciplinary evidence- based care pathway.
Vocational, as well as more relevant pain and functional, outcomes post arthroscopy are very good even in highly physically demanding military jobs.
How might it impact on clinical practice?
Pre and postoperative rehabilitation of femoroacetabular impingement is likely to play a significant role in outcome.
Introduction
Femoroacetabular impingement (FAI) as well as its related consequences such as labral and chondral tears is now recognised as a common disorder among the young active population with an estimated prevalence of 10–15%.1 It is becoming increasingly accepted that FAI is a potential precursor to early osteoarthritis of the hip, especially in young and active people.1–4
The management paradigm of this condition follows a traditional initial conservative approach with exercise-based rehabilitation. If rehabilitation treatments fail, then hip arthroscopy is often the next step in the treatment of these disorders; however, postoperative rehabilitation still remains an essential part of the management pathway. Hip arthroscopy requires a high degree of skill and has a significant risk of complication.5 The UK National Institute for Health and Care Excellence (NICE) guidance advises that the procedure ‘should only be performed by surgeons with specialist expertise in arthroscopic hip surgery’.6 The best evidence currently available suggests that surgical treatment with hip arthroscopy has a good outcome.7–15 These studies, however, have been limited by small numbers, retrospective design, short follow-ups, study in relatively inactive populations and limited reporting of postoperative rehabilitation interventions, with the potential bias of outcomes being reported by the same surgical teams and very limited use of vocational outcomes or outcomes relevant to a very-high functioning population.
The military population is very similar to a young sporting population in that it regularly undertakes high-intensity physical exercise; however, military exercise will often be load carrying (minimum army fitness requirement is to complete a paced 8 mile march carrying 30 kg) and may be in uncontrolled and unforgiving environments. In many ways, a military career is the ultimate test of outcome of the treatment of FAI. Since 2010, the defence rehabilitation services established an evidence-based hip pain best practice care pathway specifically to improve the diagnosis and management of FAI.
This study aimed to prospectively record medium-term outcomes in an active military population with confirmed diagnoses of FAI which failed the conservative treatment element of the Defence Rehabilitation evidence-based best practice hip pain pathway and required hip arthroscopy intervention and postoperative rehabilitation. Particular attention was paid to investigating functional and vocational outcomes to assess whether surgical treatment and outcomes of FAI are compatible with an ongoing highly active and physically demanding military career.
Methods
Design
Consecutive patients with a clinical and imaging diagnosis of FAI who had failed conservative treatment were referred for arthroscopic hip surgery by one hip arthroscopy surgeon (RV) and were included in the study. Participants were assessed at baseline preoperatively and at follow-up at 2, 6 and 12 months postoperatively. Postoperative multidisciplinary (MDT) rehabilitation was a critical element to the treatment pathway and is detailed below as recommended by Grzybowski et al,16 and in line with Wahoff et al's17 recommendations. All patients gave informed consent. The chairman of the local research ethics committee deemed the study a service evaluation that did not require ethical approval.
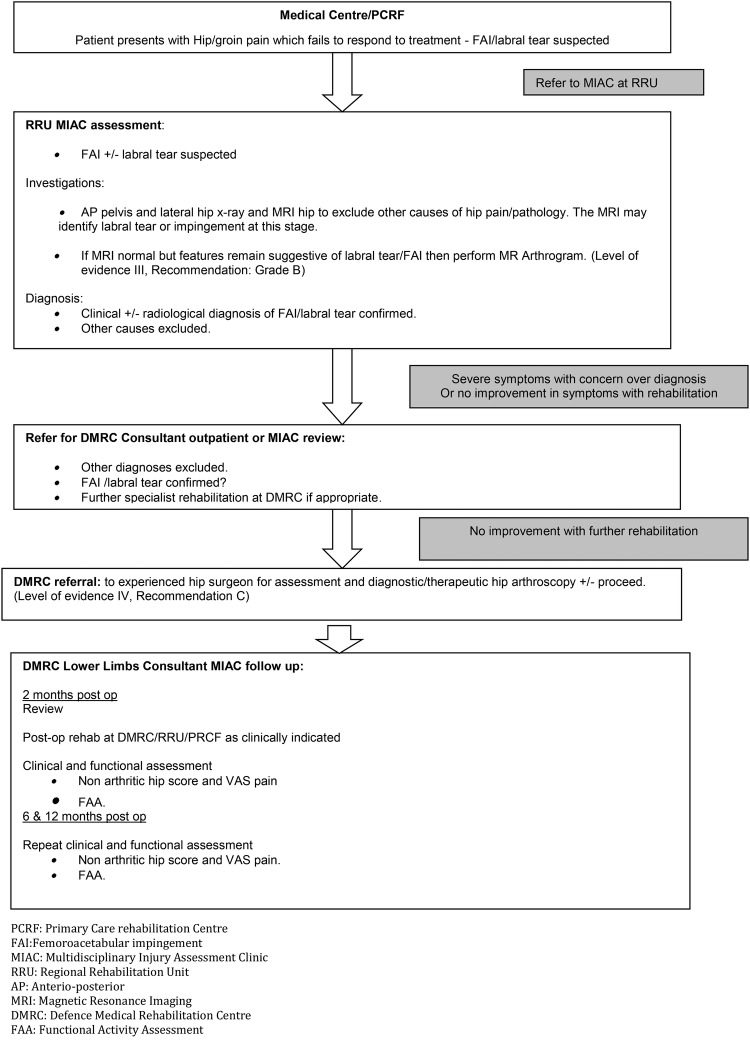
Patients were recruited from the defence rehabilitation hip pain pathway (figure 1). This is a best practice evidence-based care pathway that has been in place in defence rehabilitation since 2010. A diagnosis was made in patients having appropriate clinical symptoms and signs with imaging confirmation of the diagnosis. Symptoms of pain in the anterior groin/thigh, lateral thigh/greater trochanter area or buttock pain or pain in the ‘C’ sign region18 in the absence of spinal pathology were considered relevant. Clinical examination was assessed for a limited range of internal rotation or pain at end of range in the 90° hip-flexed position. The hip impingement sign with pain representing the patient's common symptoms on hip flexion, adduction and internal rotation with or without axial loading was also assessed. Clinical diagnoses were confirmed on imaging with X-ray and MRI±MR arthrogram. X-ray was used to identify typical FAI features such as cam and pincer deformities or acetabular dysplasia-associated with FAI and labral tears. The MRI was used to identify labral lesions including paralabral cysts, advanced cartilage lesions or labral tears and whether an effusion was present and FAI by measurement of the α angle.19 If the patient had a convincing clinical history and signs but normal X-ray and MRI, then MRA was used to diagnose labral tears or detachment by identification of intralabral contrast entry.
Figure 1.
Defence rehabilitation hip pain care pathway.
Once the diagnosis was confirmed, patients were treated conservatively with rehabilitation. Patients were treated with weekly outpatient physiotherapy sessions for 6 weeks with concurrent exercise rehabilitation with the exercise rehabilitation instructor (ERI) at the primary care rehabilitation facility. If symptoms failed to improve, then patients were referred for further intensive inpatient rehabilitation (5 hours per day, 5 days per week, for 2–3 weeks) at one of the 16 military regional rehabilitation units or at the Defence Medical Rehabilitation Centre (DMRC), Headley Court.
FAI rehabilitation, as per the defence rehabilitation hip pain pathway, was delivered by a MDT of healthcare professionals including doctor, physiotherapist, ERI± occupational therapist. Rehabilitation included assessment and treatment of reduced/altered muscle strength, muscle activation and timing abnormalities, muscle imbalance abnormalities, poor hip, pelvis, lumbar/pelvic or thoracolumbar dissociation and control, gait abnormalities, abnormal proprioception, core muscle weakness, anterior multidirectional translation of the hip joint and obesity/weight management issues.
Patients were reviewed after completing up to 3 months of rehabilitation, as described above. Those with no significant symptomatic and functional improvement were referred for hip arthroscopy surgery (figure 1) and were entered into the study. Patients were excluded from the study if other significant diagnoses were apparent that explained the patient's symptoms, that is, radiographic hip osteoarthritis, or that the patient improved significantly with conservative management and did not require hip arthroscopy.
The study was designed so that only one experienced hip arthroscopist, as per NICE guidelines,20 performed all the operations to minimise the effects of different surgical standards and techniques on outcome. Baseline outcome measures were recorded by the rehabilitation team preoperatively. Patients were reviewed 6 weeks postoperatively by the surgical team and then at 2, 6 and 12 months by the military rehabilitation team, independent of the surgical team, at which point outcome measures were recorded.
Initial postoperative rehabilitation was prescribed by the surgical team, which included protecting the integrity of the repaired tissue, restoring range of motion, restoring normal gait pattern and weight-bearing status and progressively increasing muscle strength. Patients were reviewed by the surgical team, to ensure wound healing and exclude complications, at 6 weeks and then discharged to the care of the MDT military rehabilitation team who reviewed the patient at the 2-month point. At this review, patients were referred for further residential multidisciplinary rehabilitation at DMRC, Headley Court. This rehabilitation initially followed the principles of postoperative rehabilitation (as noted above) and then progressed to a more individualised hip and groin programme which included restoration of muscular endurance/strength, cardiovascular endurance, normal movement patterns and muscle balance, proprioception, balance, normal firing and activation patterns for stability and optimisation of neuromuscular control. This then progressed to the restoration of running, sports and military activities.
Outcome measures
Outcome measures included the Visual Analogue Scale (VAS) for pain in the affected hip,21 the Non-Arthritic Hip Score (NAHS)22 and the functional activity assessment (FAA),23 all of which are valid and reliable outcome measures and appropriate to this active military population. The VAS for pain is an internationally recognised and established outcome measure for the assessment of pain. The minimally clinically important improvement for the VAS is 15.3 mm.24 The NAHS is a valid outcome measure for pain and function for the hip. It is scored from 0 to 100 (bad–good). This is a relevant outcome measure in a young active population with hip pathology as it covers high-level sporting activities (football, rugby, tennis) as well as heavy daily activities such as moving furniture and therefore avoids the ceiling affect in a young functional population that occurs using the Harris hip score,25 which has ‘unlimited walking’ or ‘stairs without using railing’ as the highest level of activity or the Western Ontario and McMasters (WOMAC) osteoarthritis index26 where the most strenuous activities are walking upstairs and downstairs.
The FAA is a validated vocational outcome tool23 specific to military populations where the patient grades their function-related to typical work and military duties ranging from 1=fully fit, 2=fit for trade and restricted military duties, 3=unfit for trade but fit for restricted military duties, 4=unfit for all but sedentary duties and 5=off all duties.
Finally, the patient's Joint Medical Employment Standard was also recorded at their 12-month postoperative review to assess vocational outcome. This is a medical officer completed assessment of the patient's actual ability to complete all, including arduous, military duties.
Statistical analysis
Statistical analysis was completed on SPSS. Data were tested for normality and analysed accordingly using either parametric or non-parametric tests including the paired t-test, sign test or Wilcoxon signed-rank test. Significance was reported as p<0.05.
Results
Demographics
One hundred and one patients (male:female, 75:26) with a mean age of 33 years (range 20–50) were entered into the study. They all had arthroscopic hip surgery for a diagnosis of FAI, which had failed conservative rehabilitation management in a period between January 2010 and October 2012, and all completed 12-month postoperative follow-up. Forty-eight per cent of patients were in the British Army and 39% and 13% were in the Royal Air Force and Royal Navy, respectively (table 1).
Table 1.
Patient demographics
| Participants (n) | 101 |
| Male (%) | 74 |
| Age (years): mean (range) | 33 (20–50) |
| Service (%; Royal Navy:British Army:Royal Air Force) | 13:48:39 |
Exclusions
A further four patients started the study and had hip arthroscopy but did not complete 12 months follow-up as they made no clinically significant improvements. Three of these had further hip resurfacing surgery at a mean of 8.6 months postarthroscopy (range 6–11 months) and one went for total hip replacement at 6 months. Four other patients were also referred for consideration of hip arthroscopy; one declined and three were assessed to have significant osteoarthritis (OA) by the surgeon and therefore did not progress to arthroscopy, but had other hip surgery (2 times hip resurfacing and one total hip replacement).
Outcomes
Of those who completed the 12-month follow-up, VAS for hip pain was recorded at baseline (preoperatively) and at 12-month follow-up (n=92). The mean baseline score was 51.30 mm (SD: 20.9) and mean 12-month score was 25.60 mm (24.5) with a statistically significant mean improvement of 25.7 mm (95% CI 19.4 to 31.99), p<0.001 a large effect size of 1.23 (table 2).
Table 2.
Results
| Outcome | N | Baseline: mean (SD) | 12-month: mean (SD) | Improvement: mean (95% CI) | p Value |
|---|---|---|---|---|---|
| VAS | 92 | 51.3 (20.9) | 25.6 (24.5) | 25.7 (19.4 to 31.99) | <0.001 |
| NAHS | 95 | 62.9 (16.4) | 78.8 (18.3) | 15.9 (12.27 to 19.54) | <0.001 |
| FAA | 97 | 2.77 (0.95) | 2.18 (1.1) | 0.59 (0.35 to 0.84) | <0.001 |
FAA, functional activity assessment; NAHS, Non-Arthritic Hip Score; VAS, Visual Analogue Scale.
Minimal clinically important improvement (MCII) in VAS for hip pain is regarded as an improvement of 15 mm.24 Improvements in 55 (60%) patients were greater than the MCII. A further 14 (15%) improved but by less than the MCII, 16 (17%) patients showed worsening of VAS scores and 7 (8%) had no change.
Similar significant improvements were seen in the NAHS. The mean baseline score (n=95) was 62.9 (16.4) and 12-month follow-up was 78.8 (18.3). A significant mean improvement of 15.9 (12.27 to 19.54) a large effect size of 0.97 was observed (table 2).
The mean FAA at baseline was 2.77 (0.95) and at 12-month follow-up was 2.18 (1.1) (n=97). This represented a significant improvement (mean=0.59; 95% CI 0.35 to 0.839) in the FAA, a medium effect size of 0.62 (table 2). Fifty-one patients improved by one level or more on the FAA, 31 did not change and 15 deteriorated. At baseline, only 40 (41%) patients scored at FAA of 1 or 2 (fit for most military duties) however by 12-month follow-up this had increased to 69 (71%).
At the 12-month follow-up, 74 of 101 patients had a formal medical employability standard assessing them fully fit for military duties (n=46) or fit for military duties including deployment with some limitations. Only six had been medically discharged.
Outcomes were also assessed at the 2-month and 6-month postoperative follow-up. There were significant improvements in VAS pain, NAHS and FAA between baseline and 2 months and baseline and 6 months. There was also significant improvement between 2 and 6 months; however, there were no significant improvements between 6 and 12 months, indicating a plateau of improvement at the 6-month point.
Owing to the anatomical and physical variations in sexes, an analysis to compare outcomes between males and females was undertaken. This demonstrated no significant differences in pain outcome (VAS) (p=0.102) or pain and function via the NAHS (p=0.886). A similar analysis between military service was undertaken due to the different military roles and physical stress that personnel from each service typically undertakes; again, there were no significant differences (VAS pain, p=0.238; NAHS, p=0.375). Analysis of the effect of age on outcome revealed that it also had no significant effect.
Discussion
This study has demonstrated that hip arthroscopy as part of an evidence-based care pathway, in the management of FAI, can produce significant improvements during a 12-month period in symptoms, function and employability. Our population was a young and active military cohort of patients exposed to regular sport and physical training as well as arduous physical tasks in potentially uncontrolled and unforgiving environments.
Although previous studies have investigated outcomes in sporting populations, this is the first study to explore such a procedure in a military population, which is exposed to highly physically demanding tasks, often involving significant loads. It is also the first study to explore occupational outcomes.
The minimum fitness requirement for Army personnel is to be able to complete a paced 8 mile march carrying 30 kg of weight. This study of outcome of FAI extends previous studies by assessing the outcome of the surgery as part of a multidisciplinary care pathway, which includes structured intensive inpatient preoperative and postoperative rehabilitation (figure 1). In this pathway, although the surgical team clearly has a pivotal role, diagnosis, preoperative rehabilitation, postoperative assessment and rehabilitation were all carried out by a multidisciplinary rehabilitation team remote and independent of the surgical team. This model of care is well suited to the elite sporting environment and it is also important to highlight that in this study all hip arthroscopies were carried out by ‘surgeons with specialist expertise in arthroscopic hip surgery’ as per the NICE guidance;6 they were also carried out by a single surgeon (RV) for all patients to prevent variations in outcome related to surgical technique and experience.
The outcomes demonstrated significant improvements over time across all symptomatic, functional and occupational measures. What is of particular interest in these results is that with a comprehensive preoperative and postoperative rehabilitation programme, the peak improvement was reached at 6 months with no further significant improvements in patient-reported outcomes between 6 and 12 months, which is contrary to the widely held belief that complete recovery from hip arthroscopy takes 12–18 months.28 This cohort was 76% male, which reflects the proportion of men and women in the UK military. There was no significant difference comparing outcomes between males and females.
The outcome measures were carefully chosen to be specific to the population being studied. In previous studies, outcome measures that are not relevant to a young active population such as the modified Harris Hip score (highest level of function ‘unlimited walking’ or ‘stairs without a rail’ which has a ceiling effect in a sporting or military population)25 27 29 or the WOMAC26 were used. Previous studies have generally been retrospective reviews of outcome30 31 or smaller case series32 and all have failed either to provide significant detail of the preoperative or postoperative role of rehabilitation in the management of FAI as recommended16 or investigated vocational outcomes.12 13 27 29 30
Two published studies have reported long-term follow-up over 10 years.29 31 However, the study by McCarthy et al31 is a retrospective study, which is more susceptible to bias, with only 56% of patients completing final outcome assessments (NAHS), and the study by Byrd and Jones29 was small (n=50), had multiple mixed hip pathologies and used the modified Harris hip score as its main outcome, which has the limitations in young active populations as explained above.
In a recent study by Kemp et al,28 in a slightly older (mean age 36 years) general population with an approximate mean activity of 4.5 hours per week, the severity of chondropathy at arthroscopy was a predictor of outcome. Patients with severe chondropathy (Outerbridge grade III-IV)33 had significantly worse hip disability and outcome scores. In the Kemp et al study, grades of chondropathy were associated with increasing age. Grades of chondropathy were not specifically recorded in our study; however, age was. Interestingly, we found that in this cohort age had no effect on outcome, indicating that there are perhaps other independent factors that affect the degree of chondropathy.
Limitations
The main limitation of this study is that there was no control group. Also, we cannot ascertain the independent influence of dedicated postoperative multidisciplinary rehabilitation in this cohort. Further studies could compare standard preoperative and postoperative outpatient rehabilitation with the more comprehensive rehabilitation programme provided for this military cohort.
Conclusion
This study indicates that in a military population, with appropriate clinical MDT inpatient postoperative rehabilitation, maximal patient-reported clinical and vocational outcomes can be reached within 6 months.
Footnotes
Contributors: ANB contributed to the study design, data collection, data analysis, manuscript production and review of manuscript. JN contributed to the data collection, manuscript production and review of manuscript. AR contributed to data analysis, manuscript production and review of manuscript. RB-D was involved in data collection, data analysis and review of manuscript. RV contributed to study design, manuscript production and review of manuscript. JMH was involved in data collection, data analysis, manuscript production and review of manuscript.
Competing interests: None declared.
Ethics approval: The MoD research ethics committee reviewed this study and confirmed it as a service evaluation and that it did not require research ethics.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Leunig M, Ganz R. [Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis]. Unfallchirurg 2005:108:9–10, 12–17. [DOI] [PubMed] [Google Scholar]
- 2.Ganz R, Parvizi J, Beck M et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112–20. [DOI] [PubMed] [Google Scholar]
- 3.Murphy S, Tannast M, Kim YJ et al. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res 2004;429:178–81. [DOI] [PubMed] [Google Scholar]
- 4.Jäger M, Wild A, Westhoff B et al. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci 2004;9:256–63. 10.1007/s00776-004-0770-y [DOI] [PubMed] [Google Scholar]
- 5.Weber AE, Harris JD, Nho SJ. Complications in hip arthroscopy: a systematic review and strategies for prevention. Sports Med Arthrosc 2015;23:187–93. 10.1097/JSA.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 6.National Institute for Health and Care Excellence; Interventional proceedure guidance [IPG408]. Sep 2011.
- 7.Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Am J Orthop 2008;37:608–12. [PubMed] [Google Scholar]
- 8.Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy 2006;22:95–106. [DOI] [PubMed] [Google Scholar]
- 9.Philippon MJ, Weiss DR, Kuppersmith DA et al. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med 2010;38:99–104. 10.1177/0363546509346393 [DOI] [PubMed] [Google Scholar]
- 10.Bedi A, Chen N, Robertson W et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy 2008;24:1135–45. 10.1016/j.arthro.2008.06.001 [DOI] [PubMed] [Google Scholar]
- 11.Lovett Carter D, Kennedy N. What are athletes’ perceptions of rehabilitation outcome one year post hip arthroscopy? J Sport Rehabil 2014;23:339–50. [PubMed] [Google Scholar]
- 12.Fabricant PD, Fields KG, Taylor SA et al. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 2015;97:537–43. 10.2106/JBJS.N.00266 [DOI] [PubMed] [Google Scholar]
- 13.Nielsen TG, Miller LL, Lund B et al. Outcome of arthroscopic treatment for symptomatic femoroacetabular impingement. BMC Musculoskelet Disord 2014;15:394 10.1186/1471-2474-15-394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reiman MP, Thorborg K. Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? Br J Sports Med 2015;49:782–4. 10.1136/bjsports-2014-093821 [DOI] [PubMed] [Google Scholar]
- 15.Casartelli NC, Leunig M, Maffiuletti NA et al. Return to sport after hip surgery for femoroacetabular impingement: a systematic review. Br J Sports Med 2015;49:819–24. 10.1136/bjsports-2014-094414 [DOI] [PubMed] [Google Scholar]
- 16.Grzybowski JS, Malloy P, Stegemann C et al. Rehabilitation following hip arthroscopy—a systematic review. Front Surg 2015;2:21 10.3389/fsurg.2015.00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wahoff M, Dischiavi S, Hodge J et al. Rehabilitation after labral repair and femoroacetabular decompression: criteria-based progression through the return to sport phase. Int J Sports Phys Ther 2014;9:813–26. [PMC free article] [PubMed] [Google Scholar]
- 18.Byrd JWT. Operative hip arthroscopy. Springer Science & Business Media, 2005:1. [Google Scholar]
- 19.Nötzli HP, Wyss TF, Stoecklin CH et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002;84:556–60. 10.1302/0301-620X.84B4.12014 [DOI] [PubMed] [Google Scholar]
- 20.NICE. Arthroscopic femoro-acetabular surgery for hip impingment. London: NICE, 2007. [Google Scholar]
- 21.Langley GB, Sheppeard H. The visual analogue scale: its use in pain measurement. Rheumatol Int 1985;5:145–8. 10.1007/BF00541514 [DOI] [PubMed] [Google Scholar]
- 22.Christensen CP, Althausen PL, Mittleman MA et al. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res 2003;406:75–83. [DOI] [PubMed] [Google Scholar]
- 23.Roberts AJ, Franklyn-Miller AD, Etherington J. A new functional outcome assessment tool for military musculoskeletal rehabilitation: a pilot validation study. PM R 2011;3:527–32. 10.1016/j.pmrj.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 24.Tubach F, Ravaud P, Baron G et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis 2005;64:29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737–55. [PubMed] [Google Scholar]
- 26.Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum 1989;18(Suppl 2):14–17. 10.1016/0049-0172(89)90010-3 [DOI] [PubMed] [Google Scholar]
- 27.Byrd JWT, Jones KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med 2009;37:2140–3. 10.1177/0363546509337705 [DOI] [PubMed] [Google Scholar]
- 28.Kemp JL, Makdissi M, Schache AG et al. Hip chondropathy at arthroscopy: prevalence and relationship to labral pathology, femoroacetabular impingement and patient-reported outcomes. Br J Sports Med 2014;48:1102–7. 10.1136/bjsports-2013-093312 [DOI] [PubMed] [Google Scholar]
- 29.Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res 2010;468:741–6. 10.1007/s11999-009-0841-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res 2009;467:747–52. 10.1007/s11999-008-0656-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCarthy JC, Jarrett BT, Ojeifo O et al. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res 2011;469:362–71. 10.1007/s11999-010-1559-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh PJ, O'Donnell JM. The outcome of hip arthroscopy in Australian football league players: a review of 27 hips. Arthroscopy 2010;26:743–9. 10.1016/j.arthro.2009.10.010 [DOI] [PubMed] [Google Scholar]
- 33.OUTERBRIDGE RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br 1961;43-B:752–7. [DOI] [PubMed] [Google Scholar]