Abstract
Background
In 2009, Ohio’s Department of Public Safety established statewide geriatric triage criteria to be used by emergency medical services for injured patients age ≥70. Our goal was to evaluate the effect of the criteria on patient outcomes.
Design
A retrospective cohort study of the Ohio Trauma Registry.
Setting
All hospitals in Ohio.
Participants
Patients age ≥70 years in the Ohio Trauma Registry from January 2006 through December 2011, 3 years before and 3 years after criteria adoption.
Measurements
Primary outcomes were in-hospital mortality and discharge to home. Criteria effects were assessed using chi-square tests, multivariable logistic regression, interrupted time series plots and multivariable segmented regression models.
Results
We included 34,499 patients. After geriatric criteria adoption, the proportion of patients qualifying for trauma center transport increased from 44% to 58%, but EMS transport rates did not change (44% versus 45%). There was no difference in unadjusted mortality (7.1% versus 6.6%) (p=0.098). In adjusted analyses, subjects with ISS<10 demonstrated decreased mortality (3.0% versus 2.5%) (odds ratio 0.81; 95% CI 0.70–0.95; p=0.011). Discharge to home did increase in the adjusted analysis (odds ratio 1.06, 95% CI 1.01–1.11; p=0.016). There were no time-dependent changes for either outcome.
Conclusions
Although the proportion of older adults meeting criteria for trauma center transport substantially increased with geriatric triage criteria, there were no increases in trauma center transports. Adoption of statewide geriatric triage guidelines did not improve mortality in more severely injured older adults, but was associated with a small decrease in mortality in mild injury (ISS <10) and with an increase in patients discharged to home. Improving outcomes in injured older adults will require further attention to implementation and use of the geriatric-specific criteria.
Keywords: geriatric, trauma, triage
INTRODUCTION
Older adults aged 65 and over constitute 13% of the US population and account for over 25% of all hospital admissions for trauma.1,2 By 2050, 40% of all trauma patients will be older adults.3–5 Injured older adults suffer from increased morbidity and mortality compared to younger adults with similar injuries. They have higher acuity, longer hospital stays, and lower discharge rates, even in the setting of apparently minor injuries.1 They are also more likely to have chronic comorbid conditions and suffer from adverse events during hospitalizations.1,6,7 Despite these findings, injured older adults are less likely to be transported by emergency medical services (EMS) providers to a trauma center than younger adults.8,9 This discrepancy increases with advancing age and likely occurs for several reasons. Current adult trauma triage criteria, for example those used by the American College of Surgeons, fail to identify a large proportion of severely injured older adults.8–12 Even among patients who meet triage criteria, older adults are less likely to be transported to a trauma center than younger adults.8,9 As a result, injured older adults are less likely to receive trauma center care than similarly injured younger patients.10,13 This under-triage of older adults is associated with increased rates of morbidity and mortality.14
In Ohio, the Ohio Department of Public Safety (ODPS) houses the Division of Emergency Medical Services which serves as the administrative arm of the State Board of Emergency Medical, Fire, and Transportation Services. The primary tasks of the Division for fire and EMS services, include: certification of personnel, accreditation of training and continuing education services, collection of EMS run data, and regulation of medical transportation services. In addition, the Division serves as the “lead agency” for the state’s trauma system, including management of the trauma registry. Local EMS structures in Ohio vary widely and include services with EMS and fire combined, EMS alone, and volunteer EMS services. All have the same standards, accreditation process, continuing education requirements, and run data analyses.
In an effort to combat the phenomena among older adults described above, the Ohio Department of Public Safety (ODPS) established geriatric-specific EMS triage criteria in 2009 for patients age 70 and over based on an observed increase in severity-adjusted mortality at that age (Supplemental Table).15,16 These criteria were based on review of the Ohio Trauma Registry and were created by altering the standard adult criteria to better predict older adults’ injury severity and need for trauma center care.15–18 In Ohio, changes to the trauma triage rules reside as law within Ohio Administrative Code. For this manuscript, we define “adoption” of the criteria as their inclusion in the trauma triage rules and incorporation into Ohio Law on December 29, 2008. “Implementation” refers to the steps taken after adoption of the criteria. By Ohio law, each EMS provider must complete 2 hours of an approved Ohio Trauma triage course during each 3-year cycle for recertification. As a result, we expect all providers to have received geriatric triage training within 3 years of their adoption. Additional training on triage criteria may be provided at the individual or EMS agency level, but was not tracked for this manuscript.
Following recommended steps in the evaluation of a new risk-prediction instrument 19, after initial proof of concept evaluation using the Registry 16, the accuracy of the criteria were validated in a cohort identified after their adoption. In this cohort, the geriatric criteria demonstrate increased sensitivity while maintaining adequate specificity in identifying older adults’ need for trauma center care.17 The criteria demonstrated both incremental value over the previous adult criteria and potential clinical utility in that the improvement in sensitivity was large enough to substantially change predicted risk. However, their effect on patient outcomes (the next recommended step in evaluation of such criteria)19 has not yet been examined.
The goal of this study was to evaluate the effect of the adoption by ODPS of the Ohio geriatric triage criteria on patient-level outcomes. We hypothesized that mortality rates for injured patients aged 70 and over in Ohio would decrease after adoption and subsequent implementation of the new criteria. We also hypothesized that a greater proportion of injured older adults would be discharged to home with less requiring skilled nursing or rehabilitation care.
METHODS
We conducted a retrospective, observational cohort study of Ohio Trauma Registry patients from 2006 through 2011 which included 3 years of data before and 3 years after adoption of the geriatric criteria on December 28, 2008. We followed the STROBE Statement (Strengthening the Reporting of Observational studies in Epidemiology) checklist for cohort studies.20 Approval was received from the local Institutional Review Board with a waiver of informed consent.
The Ohio Trauma Registry contains patient records from 87% of Ohio hospitals, which are legally required to submit information about injured patients presenting to emergency departments (EDs).21 The ODPS maintains this database and updates it annually with information entered by local trained personnel from both trauma centers and non-trauma centers.22 Patients eligible for inclusion in the Registry include those with an ICD-9-CM code for injury (ranging from 800.0 to 995.5) and at least one of the following: initial hospital admission longer than 48 hours, any transfer into or out of an ED or hospital, dead on arrival, or death following the start of evaluation or treatment. Exclusion criteria for the Registry include isolated hip fractures, delayed effects of injury, foreign body related complaints, and superficial abrasions.
All trauma registry patients ≥70 years of age who were brought to a hospital by EMS providers between January 1, 2006 and December 31, 2011 were eligible for inclusion in this study. Patients were excluded if they were not initially transported by EMS or were missing gender data.
In the case of patients transferred between different hospitals (e.g. from a non-trauma to a trauma center), a single injury event may be present more than once in the Registry. ODPS staff performed probabilistic linkage with LinkPlus version 8.2 (Centers for Disease Control and Prevention, Atlanta, GA) to create a single entry for each event.17,23 Patients with a documented disposition of “transfer to another institution” were matched to those at other hospitals with documented arrival sources of “arrival from another institution,” using gender, age, hospital identifier codes, dates of arrival and transfer (tolerance +/− 2 days), date of injury (tolerance +/− 4 days), and external cause of injury code (E-code). Weighted probabilities were used for each field and subjects were blocked on gender. After obtaining linkage scores, we retained those with >90% probability. We also manually inspected both matching and nonmatching records. There were a proportion of records below the 90% threshold which had equal matching values for all variables except E-code. We believed that such patients represented true matches and also included these in the study data set.17
Registry data provided to study investigators included patient demographic information, type of injury, information from the EMS medical record, and chart data from the ED and inpatient stay. EMS data included reason for transport, vital signs, EMS Glasgow coma score (GCS), and procedures performed. ED data included arrival source, vital signs, ED GCS, procedures performed in the ED, and ED disposition. Data from the inpatient records included type of hospital (either non-trauma center or Level I or II trauma center) abbreviated injury score (AIS) codes, injury severity score (ISS), length of intensive care unit (ICU) stays, operating room (OR) visits, international classification of diseases - 9th revision – clinical modification ( ICD-9-CM) codes, E-codes, and discharge disposition. Linkages from transferred patients were considered as a single entry for each traumatic event.
Race and ethnicity are reported using U.S. census categories, but were included as black, Hispanic, white, or other in the multivariable models due to low counts in several of the categories. Injury type was classified as blunt, penetrating, burns or asphyxia. Injury severity score was analyzed both as a continuous variable and at commonly accepted cutoffs of <10, 10–15, and >15.8,17,24 Using the provided data, including ICD-9-CM codes, AIS score, E-codes, GCS, and vitals, each patient was characterized as meeting or not meeting both the original adult and the geriatric triage criteria. Our methods for doing so have been previously described.17
For cases where there were multiple entries for the same value (e.g., GCS), we used the following hierarchy: EMS documented value, initial hospital ED value, and final hospital ED value (for patients who were transferred). For ISS, however, final hospital values were given priority, as the hospital receiving the transferred patient would have more thorough information about injury severity and ultimate disposition.
The primary outcome of interest was inpatient mortality, defined as death occurring in the ED or during the inpatient hospitalization. The secondary outcome was discharge to home which included patients discharged to home (with or without professional assistance), jail, shelters, protective services, and other unspecified discharge locations. Patients were not considered discharged to home if discharged to nursing home, rehabilitation facility, or another hospital.
Analyses were conducted with Stata (version 13; StataCorp, College Station, TX) and SAS version 9.3 (SAS Institute, Cary, North Carolina). Multiple imputation was used for missing data including GCS eye, verbal, and motor; EMS intubation, EMS cardiopulmonary resuscitation (CPR), EMS systolic blood pressure, EMS respiratory rate, and injury severity score.25 Before imputing GCS, we created a single set of GCS scores and vital signs using data from both EMS and the initial ED, if available, with EMS data having priority. Imputation was used when data for GCS was missing from both sources. Multiple imputation was performed with SAS-callable IVEware version 0.2 (Survey Research Center, Institute for Social Research, University of Michigan, Ann Arbor).26,27 Independent variables in the imputations included age, gender, race, type of injury, and discharge disposition. To have a robust imputation dataset and include age as a covariate in the imputation models, these values were imputed after application of all exclusion criteria except age.
The imputed data sets were combined using Rubin’s rules to account for variance within and between data sets.28 Descriptive statistics are reported overall and stratified by pre- and post-adoption of the geriatric triage criteria. Unadjusted trauma center transfer rates, mortality rates, and discharge to home before and after adoption of the geriatric criteria were compared using chi-square tests at significance of 0.05 and by calculating the difference in proportions with 95% CI of the difference.
For each outcome, we first created a multivariable logistic regression model with adoption of the geriatric criteria, gender, age, race, injury type (blunt, penetrating, burns or asphyxia), and ISS included as independent variables. Variables were chosen a priori based on those considered likely to affect the mortality outcome and available in the dataset. Continuous variables were tested for linearity in the logit and transformed or grouped as appropriate. Each model was tested for the presence of interactions and for fit. Effect of geriatric criteria adoption was identified by the inclusion of a time variable indicating injury before or after December 28, 2008. In addition to providing odds ratios, the adjusted effect of triage adoption on each outcome was calculated using the margins command in STATA.
For each outcome, we also created an interrupted time series plot demonstrating rates of each outcome by quarter. This was visually examined for trends and abrupt changes. Segmented regression analyses of interrupted time series were performed to evaluate the impact of the new geriatric triage criteria on rates of mortality and discharge to home.29 December 28, 2008 was used as the intervention point, with time measured in quarters over the study period, resulting in 24 quarters of observation. Quarters 1–12 comprise the period before the triage adoption, and quarters 13–24 comprise the period after the triage was adopted.
The segmented regression analysis model estimates the changes in levels and trends in our outcomes after the intervention. A major strength of the analysis is the controlling for baseline level and trend in the model. The terms in the time series model include: baseline level, baseline trend (change per quarter before intervention), level change (outcome change immediately after intervention), and trend change (change per quarter after intervention).29
In the multivariable segmented regression time series analyses, we adjusted for possible confounding by including aggregated quarterly values for: age, race/ethnicity (black, Hispanic, or white), burns/asphyxia injuries, penetrating injuries, and median ISS (square root transformed). Serial autocorrelation between error terms was assessed by visual inspection of residuals and assessment of Durbin-Watson statistics. Plots of the residuals did not show discernable patterns indicating autocorrelation. Segmented regression of interrupted time series models were constructed by means of the PROC AUTOREG procedure in SAS.
RESULTS
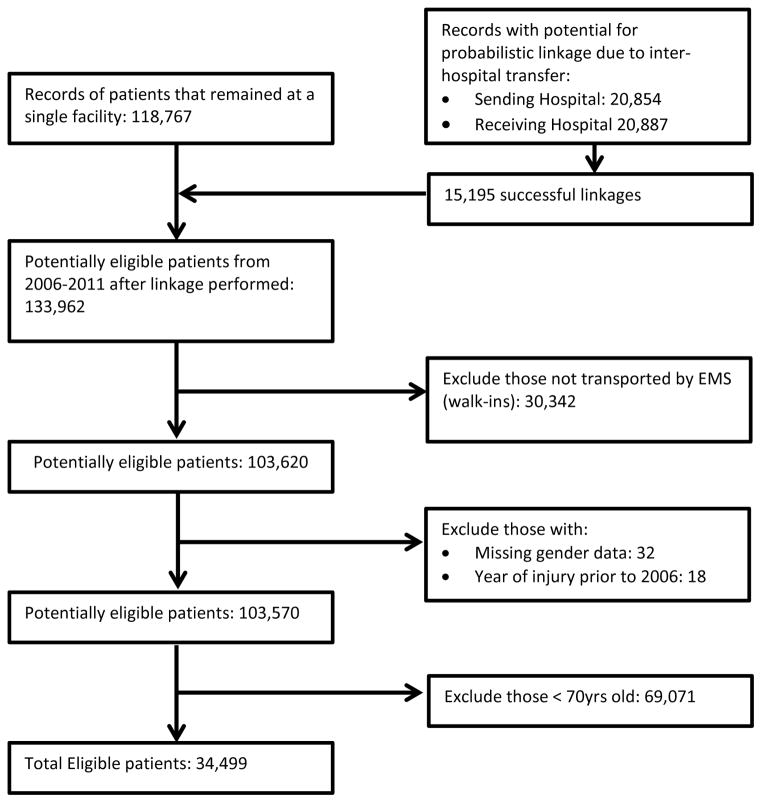
Study enrollment is described in Figure 1. Among 20,854 records indicating inter-hospital transfer, a total of 15,195 (73%) were linked. After application of all exclusion criteria except age ≥70, 103,570 patients remained for use in the imputation procedures. Missing data included GCS eye score (14%; n=14,186), GCS verbal score (14%; n=14,353), GCS motor score (12%, 12,413), intubation (40%; n=40,954), EMS CPR (12%; n=11,942), EMS assisted breathing (5%; n=5,299), systolic blood pressures (4%; n=4,298), respiratory rate (7%, n=7,021), and ISS (2%; n=2,026). There was no missing data for initial transport to a trauma center or discharge status. With application of the age criterion, there were 34,499 patients age ≥70 years included in the study, including 3,198 linked records.
Figure 1.
Flow diagram of study inclusion of patient records included in the Ohio Department of Public Safety trauma registry from 2006 through 2011.
Characteristics of the study population overall and stratified by adoption of geriatric triage criteria are shown in Table 1. Demographic data, mechanism of injury, and ISS distribution were similar for both time periods. Pre-adoption, 44% (95% CI 44–45%) of older adults met the adult triage criteria, indicating need for trauma center care. After adoption of the geriatric criteria, 58% (95% CI, 58–59%) met the new criteria and were appropriate for trauma center care (difference 14%, 95% CI of the difference 13–15%)(p<0.001). However, there were only minimal increases in the proportion of patients initially transported to a trauma center (1.0%, 95% CI of the difference 0.1 to 2.0%)(p=0.05) and in those transported or transferred to a trauma center at any time (2.4%, 95% CI of the difference 1.3 to 3.4%)( p<0.001).
Table 1.
Clinical characteristics and outcomes of 34,449 geriatric trauma patients ≥ 70 years old in the Ohio trauma registry from 2006 – 2011, overall and stratified by adoption of geriatric triage criteria*
| Older adults aged ≥70 years (n=34,499) | Before triage criteria adopted (n=15,664) | After triage criteria adopted (n=18,835) | |
|---|---|---|---|
| Demographics | |||
| Median (IQR) age | 82 (77–87) | 82 (77–87) | 82 (77–87) |
| Male gender | 31% (10,755) | 31% (4,788) | 32% (5,967) |
| Race/Ethnicity | |||
| White | 90% (31,031) | 92% (14,345) | 89% (16,686) |
| Black | 4.7% (1,624) | 5.1% (792) | 4.4% (832) |
| Hispanic | 0.3% (105) | 0.3% (39) | 0.4% (66) |
| Other | 0.9% (306) | 1.0% (153) | 0.8% (151) |
| Undocumented | 4.2% (1,433) | 2.1% (333) | 5.8% (1,100) |
| Mechanism of Injury | |||
| Blunt | 99% (34,049) | 99% (15,462) | 99% (18,587) |
| Penetrating | 0.8% (266) | 0.7% (114) | 0.8% (152) |
| Burns | 0.5% (157) | 0.5% (75) | 0.4% (82) |
| Asphyxial | 0.1% (27) | 0.1% (13) | 0.1% (14) |
| Injury Severity | |||
| ISS >15 | 14% (5,001) | 16% (2,489) | 13% (2,512) |
| ISS 10–15 | 14% (4,795) | 13% (2,082) | 14% (2,713) |
| ISS <10 | 72% (24,703) | 71% (11,093) | 72% (13,610) |
| Median (IQR) ISS | 5 (4–10) | 6 (4–10) | 5 (4–10) |
| Proportion meeting trauma triage criteria | |||
| Geriatric triage criteria | 58% (20,010) | 57% (8,984) | 58% (11,026) |
| Adult triage criteria | 44% (15,347) | 44% (6,972) | 44% (8,375) |
| Hospital measures | |||
| Inter-hospital Transfers | 9.3% (3,198) | 8.4% (1,310) | 10% (1,888) |
| Initial transport to a trauma center (level 1 or 2) | 45% (15,459) | 44% (6,928) | 45% (8,531) |
| Any transport to a trauma center (level 1 or 2) | 53% (18,418) | 52% (8156) | 54% (10,262) |
| ICU Stay ≥ 1 day | 17% (5,761) | 14% (2,181) | 19% (3,580) |
| OR visits (≤48hrs) | 13% (4,480) | 12% (1,926) | 14% (2,554) |
| Discharge status | |||
| Home† | 35% (12,014) | 37% (5,350) | 38% (6,664) |
| Medical facility ‡ | 58% (20,147) | 59% (9,214) | 58% (10,933) |
| Mortality | 6.8% (2,338) | 7.1% (1,100) | 6.6% (1,238) |
Values are percentage(n) or median (IQR)
Discharge to home includes home, home with professional assistance, jail/prison, against medical advice or other non-medical facility (shelter, home hospice, etc.)
Discharge to medical facility includes extended care facility, nursing home, skilled nursing facility, rehabilitation facility, or transfer to another hospital
IQR=interquartile range; ISS=Injury severity score; ICU=intensive care unit; OR=operating room
There were also no differences in transport rates among the subgroup who met triage criteria. In the pre-adoption data, 48% (95% CI, 47–49%) (n=3,362 of 6,972) of patients meeting adult criteria and 48% (95% CI 48–50%) (n=4,361 of 8,984) of those meeting what would ultimately be the geriatric criteria were initially transported to a trauma center. After geriatric criteria adoption, only 48% (95% CI, 47–49%) (n=5,322 of 11,026) of those who met geriatric criteria were transported to a trauma center. Similar results were seen when identifying the rate of those transported or transferred to a trauma center at any time. In the pre-adoption data, 57% (95% CI, 56–58%) (n=3,972 of 6,972) of those meeting adult criteria and 59% (95% CI 58–60%) (n=5,302 of 8,984) meeting what would ultimately be the geriatric criteria were transported to a trauma center. After geriatric criteria adoption, only 60% (95% CI, 59–60%) (n=6,575 of the 11,026) of those who met geriatric criteria were ultimately transported to a trauma center.
The unadjusted mortality rate did not significantly change after adoption. Mortality was 7.1% (95% CI, 6.6%–7.4%) pre-adoption and 6.6% (95% CI, 5.9%–6.6%) post-adoption (difference −0.4%, 95% CI of the difference −0.1 to 0.1%)(p=0.098). Results of the multivariable logistic regression analysis for mortality are shown in Table 2. ISS was not linear in the logit and was initially included in the model using the square root of ISS. However, an interaction existed between the square root of ISS and geriatric criteria adoption. This substantially complicated the interpretation of the effect of the geriatric criteria. For clarity, we converted ISS to a 3-level variable. An interaction continued to exist. When accounting for this interaction term, adoption of the geriatric criteria was associated with a significant decrease in mortality among older adults with ISS<10 (OR 0.81, 95% CI 0.70–0.95)(Table 4). Adjusted mortality in this ISS<10 group decreased from 3.0% (95% CI, 2.7–3.3%) to 2.5% (95% CI, 2.2–2.7%). There were no changes in mortality among those with ISS 10–15 (5.0%[95% CI, 4.1–6.1] pre- to 5.8% [95% CI, 4.9–6.7%] post-intervention) or ISS >15 (27% [95% CI, 25–29%] pre- to 30% [95% CI, 28–32%] post-intervention).
Table 2.
Multivariable logistic regression models identifying the effect of geriatric triage criteria adoption on mortality Note that odds ratios for geriatric triage criteria adopted and ISS must be interpreted with consideration of the interaction between them.
| Variable | Level | Odds Ratio | 95% CI | p-value | |
|---|---|---|---|---|---|
| Geriatric Triage Criteria adopted | No | Ref | |||
| Yes | 0.81 | 0.70 | 0.95 | 0.011 | |
| Gender | Female | Ref | |||
| Male | 1.80 | 1.64 | 1.98 | <.0001 | |
| Age(years) | 1.02 | 1.01 | 1.03 | <.0001 | |
| Race/Ethnicity | Other | Ref | |||
| Black | 1.00 | 0.75 | 1.32 | 0.9928 | |
| Hispanic | 0.87 | 0.36 | 2.11 | 0.7537 | |
| White | 0.98 | 0.80 | 1.19 | 0.8261 | |
| Injury Type | Blunt | Ref | |||
| Burns/Asphyxial | 7.80 | 5.41 | 11.25 | <.0001 | |
| Penetrating | 7.12 | 5.26 | 9.65 | <.0001 | |
| Injury severity score | ISS <10 | Ref | |||
| ISS 10–15 | 1.79 | 1.42 | 2.24 | <.0001 | |
| ISS >15 | 11.89 | 10.28 | 13.75 | <.0001 | |
| Interaction of triage criteria adoption and ISS | Triage adopted and ISS < 10 | Ref | |||
| Triage adopted and ISS 10–15 | 1.36 | 1.00 | 1.83 | 0.0475 | |
| Triage adopted and ISS >15 | 1.34 | 1.09 | 1.64 | 0.0048 | |
ISS = Injury Severity Score; CI = Confidence Interval; Ref=referent
Table 4.
Odds of death for mildly, moderately, and severely injured geriatric patients after geriatric triage criteria adoption accounting for the interaction between adoption and injury severity
| Injury severity | Odds Ratio | 95% CI | p-value | |
|---|---|---|---|---|
| ISS <10 | 0.814 | 0.695 | 0.954 | 0.011 |
| ISS 10–15 | 1.103 | 0.854 | 1.426 | 0.4518 |
| ISS >15 | 1.092 | 0.959 | 1.242 | 0.1832 |
ISS = Injury Severity Score; OR = Odds Ratio; CI = Confidence Interval
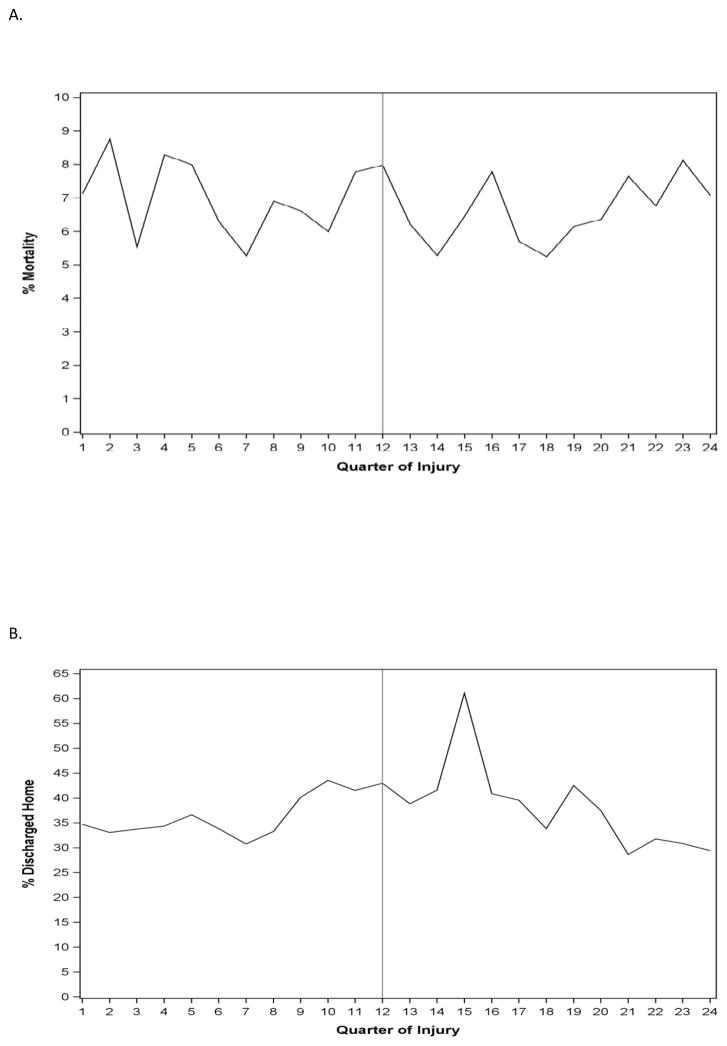
Figure 2a demonstrates mortality over time before and after the geriatric criteria were adopted. In the univariable time series model, there was no significant baseline trend (p=0.72), level change after adoption (p=0.17), or trend change after adoption (p=0.18). Checks for negative autocorrelation (p=0.58) and positive autocorrelation (p=0.42) indicated that no corrections for autocorrelation needed to be made. In the multivariable time series analysis (Table 2), there were no significant baseline trends (p=0.82), post-adoption level change (p=0.80), or post-adoption trend changes (p=0.77) for mortality.
Figure 2.
Proportion of study patients with (A) in-hospital mortality and (B) discharge to home by quarter of injury. Quarter 1 is the 1st quarter of 2006, quarter 24 is the 4th quarter of 2011, and the quarter 12 reference line is the time of adoption of Ohio’s geriatric triage criteria.
For the secondary outcome, there were only minimal unadjusted increases in discharge to home, from 34% (95% CI 33–35%) pre-adoption to 35% (95% CI, 35–35%) post-adoption (difference 1.2%, 95% CI of the difference 0.2–2.2%)(p=0.02). For the multivariable models, we excluded patients with in-hospital mortality and used the same independent variables as above. Results of the multivariable logistic regression analysis for discharge to home are shown in Table 3. There were no significant interactions in this model. Geriatric criteria adoption was associated with greater odds of discharge to home (odds ratio 1.06, 95% CI 1.01–1.10)(p=0.016). Adjusted discharge to home was 36% (95% CI, 36–37%) before and 38% (95% CI, 37–38%) after adoption of the criteria.
Table 3.
Multivariable logistic regression model identifying the effect of geriatric triage criteria adoption on discharge to home in injured older adults
| Variable | Level | Odds Ratio | 95% CI | p-value | |
|---|---|---|---|---|---|
| Geriatric Triage Criteria adopted | No | Ref | |||
| Yes | 1.06 | 1.01 | 1.11 | 0.162 | |
| Gender | Female | Ref | |||
| Male | 1.26 | 1.20 | 1.33 | <0.001 | |
| Age(years) | 0.96 | 0.96 | 0.97 | <0.001 | |
| Race/Ethnicity | Other | Ref | |||
| Black | 1.18 | 1.02 | 1.37 | 0.0254 | |
| Hispanic | 1.05 | 0.69 | 1.60 | 0.8179 | |
| White | 1.02 | 0.92 | 1.14 | 0.6569 | |
| Injury Type | Blunt | Ref | |||
| Burns/Asphyxial | 1.17 | 0.81 | 1.68 | 0.4111 | |
| Penetrating | 2.00 | 1.45 | 2.77 | <0.001 | |
| Injury Severity | ISS <10 | Ref | |||
| ISS 10–15 | 0.93 | 0.87 | 1.00 | 0.0487 | |
| ISS >15 | 0.85 | 0.78 | 0.91 | <0.001 | |
ISS = Injury Severity Score; CI = Confidence Interval; Ref=referent
Figure 2b demonstrates discharge to home over time before and after the geriatric criteria were adopted. In the univariable time series model, there was no significant baseline trend (p=0.06) or level change after adoption (p=0.11). There was a significant trend change in the proportion of discharges home after adoption (p=0.001). There was an estimated 2.5% quarterly adoption in the proportion of discharges to home when compared with the trend before adoption. Checks for negative autocorrelation (p=0.64) and for positive autocorrelation (p=0.36) indicated that no corrections for autocorrelation needed to be made. In the multivariable time series analysis, there were no significant baseline trends (p=0.64), post-adoption level changes (p=0.22) or post-adoption trend changes (p=0.37) for discharge to home.
DISCUSSION
Injured older adults have worse morbidity and mortality than younger adults and derive significant benefit from appropriate care in designated trauma centers.1,17,24 Despite this, older adults are less likely to be transported to a trauma center by EMS providers.8,9 Ohio’s geriatric triage criteria for EMS providers were adopted as one attempt to address the persistent undertriage in this population.16,18 The criteria have been shown to improve sensitivity from 61% to 93% in identifying geriatric patients in need of trauma center care.17 However, despite this greater sensitivity, we found only a small decrease in mortality among injured older adults in the three years after their adoption. This benefit was confined to the ISS<10 group where mortality decreased from 3% to 2.5% after controlling for demographics, injury type, and injury severity. No mortality benefit was identified in groups with higher ISS. Additionally, there were no specific time-related trends in mortality in the interrupted time series plot or segmented regression analysis, indicating that the failure to find a substantial difference in outcome was not due to pre-adoption trends or to a lag in implementation of the criteria.
The failure to improve outcomes for more severely injured patients is of uncertain etiology and could reflect failure to increase rates of transport to trauma centers, a ceiling effect (i.e., inability to affect outcome in the most severely injured older adults), or other factors. Historically, under-triage has been at least partially the result of poor sensitivity when applying standard adult criteria to older adults.8,10,17 However, we have previously demonstrated that the Ohio geriatric triage criteria perform similarly in older adults as the adult criteria do in younger adults.17 As a result, the most likely reason for the minimal effect on mortality seen on this study is the lack of substantial changes in transport rates to trauma centers after guideline adoption. Although 14% more older adults met criteria for trauma center transport after adoption, initial transport rates to a trauma center by EMS increased only 1.0% and ultimate transport rates (e.g. either initial EMS transport or subsequent transfer to a trauma center from a local hospital) increased only 2.4%. This small increase in initial transport is not clearly related to the new criteria as rates did not change among those meeting adult criteria pre-intervention (58%) and geriatric criteria post-intervention (58%). However, the rate of ultimate transport increased from 57% of those meeting adult criteria pre- to 60% of those meeting geriatric criteria post-intervention. This finding is consistent with past evidence demonstrating persistent undertriage of older adults, even when criteria for trauma center transport are met.8 Compliance with CDC field triage guidelines is less likely for older patients and results in decreased trauma center transfer rates for those older than 65, with those older than 80 being 89% less likely to receive care at a level I trauma center.8 The reasons behind this lack of change in transport rates are not clear and could include geographic, patient, EMS provider, EMS system, and local facility factors. For example, differential rural vs. urban distribution of population by age would affect availability of trauma centers. Reluctance to transfer older adults to a trauma center could be a result of EMS factors or even factors at local non-trauma hospitals. Patient preference (e.g. concerns over being transported farther a field or desires for different intensity of care) could also play a role. Further work, incorporating both quantitative and qualitative methods, will be required to better understand these factors and identify appropriate remedies.
Interestingly, the mortality benefit seen in the ISS<10 group occurred even without increases in trauma center transfer rates either in the entire group with ISS<10 or in the subset of those with ISS<10 who met geriatric triage criteria. This raises the concern that the observed decrease in mortality, although statistically significant in the setting of a large sample size, may have been due to chance. As a result, this should be viewed as a preliminary finding. Nevertheless, older adults with mild injury have been shown to suffer worse outcomes than their younger adult counterparts.1 As those with ISS<10 make up the majority of injured older patients, even small benefits in mortality would be associated with large absolute numbers of patients benefitting. This subgroup should be particularly examined in the setting of further work which aims to decrease under-triage and increase guideline compliance among EMS providers.
In-hospital mortality is not alone an adequate indicator of acceptable outcomes in older adults after trauma.30 Discharge to a skilled nursing facility is associated with poor-long term outcomes in older adults.31,32 We hypothesized that the triage criteria would result in an increase in the proportion of injured older adults discharged home. We did identify a small increase in such patients, after adjusting for patient factors. Likely, the same factors which affect mortality as an outcome also affected discharge status.
Use of the Registry introduces limitations expected with previously collected data. Entry and abstraction is done by staff at the local hospital level, and some degree of inconsistency with abstraction is possible. However this is mitigated by personnel training and use of a data dictionary. There is also a possibility of selection bias, as less severely injured patients who were discharged from the hospital in under 48 hours were not included in the registry. This could affect our results, particularly since we found that patients with ISS <10 experienced the greatest decrease in mortality. In relying on registry data we were also unable to determine specific factors leading to transport or lack of transport of individual patients to a trauma center. This will require a complete multivariable analysis and potentially qualitative analysis at the level of the EMS agency in subsequent work. Finally, the use of registry data does not directly identify the accuracy of the geriatric criteria when applied real-time by providers in the field. Factors complicating implementation, for example failure to accurately apply the criteria, could affect accuracy but cannot be measured in the current study. In addition, the reproducibility and interrater reliability of subjective factors in the criteria have not been assessed.
The before-and-after study design also cannot account for unmeasured secular trends or temporal changes which could have influenced results. For example, if care of trauma patients in general improved over the study period, mortality may have decreased independent of the change in geriatric triage criteria. The time series analyses provide some reassurance that this was not the case as there was no pre-intervention trend in improving outcome for the 3 years prior to the intervention.
In conclusion, we demonstrated that adoption of statewide geriatric triage guidelines for EMS providers did not improve mortality in moderate to severely injured older adults, but was associated with a small decrease in mortality in those with mild injury (ISS <10). There was a small increase in the proportion of patients discharged to home. Although the proportion of older adults recommended for transport to a trauma center substantially increased with the new criteria, there were only minimal increases in transport and transfer rates. Improving outcomes in injured older adults will likely require additional study and attention to implementation and use of the geriatric-specific triage criteria.
Supplementary Material
Acknowledgments
Disclosures of funding: JMC was partially funded by a 2013 Trauma Grant from the Ohio Department of Public Safety and was supported in part by 1K23AG038351-01 from the National Institute on Aging. BI was supported by an Ohio State University College of Medicine Roessler Scholarship.
The authors acknowledge the assistance of the following from the Ohio Department of Public Safety, Division of Emergency Medical Services in the obtaining of the initial data set and the conduct of the data set matching: Tim Erskine, EMT-P, BA, Chief, Trauma and Research, Sue Morris, EMT-P, BA, EMS & Trauma Program data manager; and Ryan Frick, MPH, epidemiologist.
JMC: ODPS grant on trauma funded this work.
MNS: NIH and AHRQ grants on EMS and trauma. Not directly related to this work.
Conflict of Interest Disclosures
| Elements of Financial/Personal Conflicts | *Author 1 JMC |
Author 2 NVB |
Author 3 MWH |
Author 4 BI |
||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | x | X | X | X | ||||
| Grants/Funds | x | X | X | X | ||||
| Honoraria | x | X | X | X | ||||
| Speaker Forum | x | X | X | X | ||||
| Consultant | x | X | X | X | ||||
| Stocks | x | X | X | X | ||||
| Royalties | x | X | X | X | ||||
| Expert Testimony | x | X | X | X | ||||
| Board Member | x | X | X | X | ||||
| Patents | x | X | X | X | ||||
| Personal Relationship | x | X | X | X | ||||
| Elements of Financial/Personal Conflicts | *Author 5 SK |
Author 6 DCE |
Author 7 SD |
Author 8 ARP. |
||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | x | X | X | X | ||||
| Grants/Funds | x | X | X | X | ||||
| Honoraria | x | X | X | X | ||||
| Speaker Forum | x | X | X | X | ||||
| Consultant | x | X | X | X | ||||
| Stocks | x | X | X | X | ||||
| Royalties | x | X | X | X | ||||
| Expert Testimony | x | X | X | X | ||||
| Board Member | x | X | X | X | ||||
| Patents | x | X | X | X | ||||
| Personal Relationship | x | X | X | X | ||||
| Elements of Financial/Personal Conflicts | *Author 9 MNS |
Etc. | ||||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | x | |||||||
| Grants/Funds | x | |||||||
| Honoraria | x | |||||||
| Speaker Forum | x | |||||||
| Consultant | x | |||||||
| Stocks | x | |||||||
| Royalties | x | |||||||
| Expert Testimony | x | |||||||
| Board Member | x | |||||||
| Patents | x | |||||||
| Personal Relationship | x | |||||||
For “yes” x mark(s): give brief explanation below:
Footnotes
Meetings: The paper was presented at the annual meeting of the American College of Physicians, Boston, MA. October, 2015.
Author Contributions: JMC: Designed the study, oversaw the data analysis and interpretation, and authored the manuscript.
NVB: Performed the data analysis and assisted with data interpretation and manuscript preparation.
MWH: Assisted with interpretation of the data and manuscript preparation.
BI: Assisted with study design, prepared the database for analysis, and assisted with manuscript preparation.
SK: Assisted with interpretation of the data and manuscript preparation.
DCE: Assisted with interpretation of the data and manuscript preparation.
SD: Assisted with study design and data analysis.
ARP: Assisted with data analysis and manuscript preparation.
MNS: Assisted with interpretation of the data and manuscript preparation.
Sponsor’s Role: NONE
Contributor Information
Jeffrey M. Caterino, Department of Emergency Medicine, The Ohio State University Wexner Medical Center, Columbus, OH.
Nicole V. Brown, Center for Biostatistics, The Ohio State University, Columbus, OH.
Maya W. Hamilton, The Ohio State University College of Medicine, Columbus, OH.
Brian Ichwan, Stanford University Medical Center, Department of Emergency Medicine, Stanford, CA.
Salman Khaliqdina, Department of Emergency Medicine, The Ohio State University Wexner Medical Center, Columbus, OH.
David C. Evans, Department of Surgery, The Ohio State University Wexner Medical Center, Columbus, OH.
Subrahmanyan Darbha, Department of Emergency Medicine, The Ohio State University Wexner Medical Center, Columbus, OH.
Ashish R. Panchal, Department of Emergency Medicine, The Ohio State University Wexner Medical Center, Columbus, OH.
Manish N. Shah, Berbee Walsh Department of Emergency Medicine, The University of Wisconsin-Madison, Madison, WI.
References
- 1.Keller JM, Sciadini MF, Sinclair E, et al. Geriatric trauma: demographics, injuries, and mortality. Journal of orthopaedic trauma. 2012;26:e161–5. doi: 10.1097/BOT.0b013e3182324460. [DOI] [PubMed] [Google Scholar]
- 2.Bonne S, Schuerer DJ. Trauma in the older adult: epidemiology and evolving geriatric trauma principles. Clinics in geriatric medicine. 2013;29:137–50. doi: 10.1016/j.cger.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Morris JA, Jr, Smith GS, et al. Acute hospital costs of trauma in the United States: implications for regionalized systems of care. The Journal of trauma. 1990;30:1096–101. doi: 10.1097/00005373-199009000-00005. discussion 101–3. [DOI] [PubMed] [Google Scholar]
- 4.Administration on Aging (AoA) [Accessed 04/21/2015];Projected Future Growth of the Older Population. at http://www.aoa.acl.gov/Aging_Statistics/future_growth/future_growth.aspx.
- 5.Campbell JW, Degolia PA, Fallon WF, et al. In harm’s way: Moving the older trauma patient toward a better outcome. Geriatrics. 2009;64:8–13. [PubMed] [Google Scholar]
- 6.McGwin G, Jr, MacLennan PA, Fife JB, et al. Preexisting conditions and mortality in older trauma patients. JTrauma. 2004;56:1291–6. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 7.Meldon SW, Reilly M, Drew BL, et al. Trauma in the very elderly: a community-based study of outcomes at trauma and nontrauma centers. JTrauma. 2002;52:79–84. doi: 10.1097/00005373-200201000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Nakamura Y, Daya M, Bulger EM, et al. Evaluating age in the field triage of injured persons. Annals of emergency medicine. 2012;60:335–45. doi: 10.1016/j.annemergmed.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma MH, MacKenzie EJ, Alcorta R, et al. Compliance with prehospital triage protocols for major trauma patients. JTrauma. 1999;46:168–75. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 10.Lane P, Sorondo B, Kelly JJ. Geriatric trauma patients-are they receiving trauma center care? AcadEmergMed. 2003;10:244–50. doi: 10.1197/aemj.10.3.244. [DOI] [PubMed] [Google Scholar]
- 11.Goodmanson NW, Rosengart MR, Barnato AE, et al. Defining geriatric trauma: when does age make a difference? Surgery. 2012;152:668–74. doi: 10.1016/j.surg.2012.08.017. discussion 74–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scheetz LJ. Effectiveness of prehospital trauma triage guidelines for the identification of major trauma in elderly motor vehicle crash victims. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2003;29:109–15. doi: 10.1067/men.2003.59. [DOI] [PubMed] [Google Scholar]
- 13.Phillips S, Rond PC, III, Kelly SM, et al. The failure of triage criteria to identify geriatric patients with trauma: results from the Florida Trauma Triage Study. JTrauma. 1996;40:278–83. doi: 10.1097/00005373-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Rogers Amelia, BS, Rogers Frederick, MD, MS, Bradburn Eric, DO, Krasne Margaret, Lee John, MD, Wu Daniel, DO, Edavettal Mathew, MD, Horst Michael., PHD Old and Undertriaged: A Lethal Combination. doi: 10.1177/000313481207800628. [DOI] [PubMed] [Google Scholar]
- 15.Ohio Department of Public Safety. OAC 4765–14 with new geriatric triage criteria. http://wwwpublicsafetyohiogov/links/ems_oac4765_14_geriatric_triage_details09pdf.
- 16.Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. AmJEmergMed. 2010;28:151–8. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 17.Ichwan B, Darbha S, Shah MN, et al. Geriatric-specific triage criteria are more sensitive than standard adult criteria in identifying need for trauma center care in injured older adults. Ann Emerg Med. 2015;65:92–100. e3. doi: 10.1016/j.annemergmed.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Werman HA, Erskine T, Caterino J, et al. Development of statewide geriatric patients trauma triage criteria. Prehospital and disaster medicine. 2011;26:170–9. doi: 10.1017/S1049023X11006315. [DOI] [PubMed] [Google Scholar]
- 19.Hlatky MA, Greenland P, Arnett DK, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–16. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Journal of clinical epidemiology. 2008;61:344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Ohio Department of Public Safety. Ohio Trauma Registry Annual Data Reports 2001–2002. http://wwwemsohiogov/trauma/OTR/OTR%20ANNUAL%20REPORT%202001_2002%20FINALPDF.
- 22.Enright MC, Day NP, Davies CE, et al. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. JClinMicrobiol. 2000;38:1008–15. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 24.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. NEnglJMed. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 25.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. AcadEmergMed. 2006;13:314–24. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Raghunathan TELJ, Wan Howewyk J, Solengberger PW. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 27.IVEware: Imputation and variance estimation version 0.2 software user guide. University of Michigan; 2011. [Accessed 6/1/2015, 2015]. at ftp://ftp.isr.umich.edu/pub/src/smp/ive/ive21_user.pdf. [Google Scholar]
- 28.Rubin M. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 29.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. Journal of clinical pharmacy and therapeutics. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 30.Perdue PW, Watts DD, Kaufmann CR, et al. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. JTrauma. 1998;45:805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 31.Davidson GH, Hamlat CA, Rivara FP, et al. Long-term survival of adult trauma patients. JAMA. 2011;305:1001–7. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 32.Claridge JA, Leukhardt WH, Golob JF, et al. Moving beyond traditional measurement of mortality after injury: evaluation of risks for late death. Journal of the American College of Surgeons. 2010;210:788–94. 94–6. doi: 10.1016/j.jamcollsurg.2009.12.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.