Clostridium difficile infection (CDI) is the leading cause of infectious diarrhea in the developed world and the incidence and severity of CDI began increasing at the turn of the 21st century. “Fulminant” CDI refers to illness that is life-threatening and, importantly, 36–75% of those who develop fulminant CDI have had recent surgery.1,2
Initial treatment of CDI depends on severity of infection and involves oral metronidazole, vancomycin or fidaxomicin. For CDI which is not responding to medical management, early surgical consultation is recommended with the gold standard surgical intervention being total abdominal colectomy and end ileostomy.1 In 2011, however, Neal and colleagues published the novel technique of performing diverting loop ileostomy with colonic lavage and postoperative antegrade vancomycin enemas in patients with severe CDI. They reported preservation of the colon in 93% of patients in addition to reduced mortality (19% vs 50%, odds ratio 0.24) when compared to matched historical patients treated with total abdominal colectomy.3 Although their outcomes interested many in the surgical community, critics have cited concerns over study design, small sample size, and results that have not been reliably replicated.1
We present the case of a 77 year old male who developed severe CDI after taking ciprofloxacin for prostatitis. He underwent emergent diverting loop ileostomy with colonic lavage and antegrade vancomycin enemas resulting in control of his severe colitis. Colonoscopy five months later showed nonspecific colitis and inflammation. He was referred to our facility three months later regarding ileostomy reversal, after his health had returned to baseline. One year after his index operation, he underwent technically uneventful ileostomy reversal. He had early return of bowel function on postoperative day one with loose bowel movements and, by postoperative day two, he felt well and was tolerating a full liquid diet. On the morning of postoperative day three, he was febrile, tachycardic and began having watery diarrhea. Several hours later, he was hypotensive with altered mental status, a markedly distended abdomen, a white blood cell count of 4.5 k/μl, a lactic acid of 5.5 mmol/L and rising serum creatinine. Abdominal plain film showed colonic distension and no pneumoperitoneum. He then required vasopressors for persistent hypotension and broad-spectrum antibiotics were initiated for concern for anastomotic leak. He developed respiratory distress requiring emergent intubation along with central and arterial line placement. His C. difficile test came back positive and a CT scan was consistent with recurrent C. difficile colitis (Fig. 1A & B). That evening, he was taken emergently for exploratory laparotomy and total abdominal colectomy. A short segment enterectomy also was performed due to a single enterotomy. His bowels were left in discontinuity and an Abthera was placed with plans for re-exploration. The following day, he remained acidotic on a bicarbonate drip with increasing pressor requirements and multisystem organ failure requiring high flow oscillating ventilator use as well as continuous dialysis. Based on the severity of his illness, his family elected to withdraw vasopressor and ventilator support. He was extubated and expired shortly thereafter, five days after his ileostomy reversal. Final pathology showed pseudomembranous enteritis and pseudomembranous colitis.
Fig. 1.
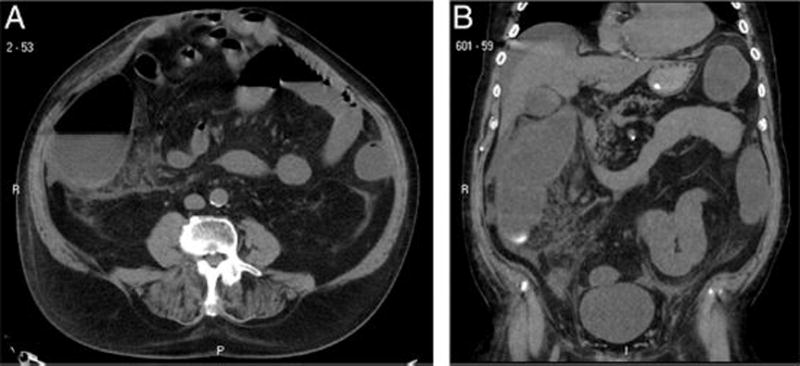
Abdominal computed tomography scan of patient. Representative (A) axial and (B) coronal images showing inflammation and fat stranding around the cecum and ascending colon, consistent with recurrent C. difficile colitis.
This case highlights several questions including appropriate timing of ileostomy reversal and testing for persistent C. difficile. Neal and colleagues did not discuss their criteria for determining when and on whom to perform ileostomy reversal in their series. At the time of initial publication, fifteen of their nineteen surviving patients (79%) had undergone ileostomy reversal. Because diverting loop ileostomy and colonic lavage is a new approach to managing fulminant CDI, there is not yet any long-term follow up data regarding recurrence of CDI after ileostomy reversal. Neal and colleagues did not report subsequent testing for C. difficile prior to ileostomy reversal, nor did they document any immediate recurrences after reversal. Abe and colleagues, however, published a case report in Japan, in which a 69 year old man developed fulminant and fatal CDI several days after ileostomy closure in an ileostomy formed for reasons unrelated to CDI.2 There have been other reports of CDI after ileostomy closure and one series found a statistically significant association of postoperative CDI with delayed ileostomy closure (>6 months from index procedure, p=0.003).4
After this alarming case of fatal recurrence of CDI, we recommend counseling patients about the risk of C. difficile recurrence prior to offering ileostomy closure to those who had their stomas initially created for treatment of CDI. A high index of suspicion as well as a multidisciplinary approach including surgeons and gastroenterologists is necessary for swift diagnosis and treatment of this postoperative complication. Additionally, we are looking into the possibility of perioperative fecal transplantation to both prevent and treat recurrent CDI after ileostomy reversal.
References
- 1.Steele SR, McCormick J, Melton GB, et al. Practice parameters for the management of clostridium difficile infection. Dis Colon Rectum. 2015;58(1):10–24. doi: 10.1097/DCR.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 2.Abe I, Kawamura YJ, Sasaki J, Konishi F. Acute fulminant pseudomembranous colitis which developed after ileostomy closure and required emergent total colectomy: A case report. J Med Case Rep. 2012;6 doi: 10.1186/1752-1947-6-130. 130-1947-6-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neal MD, Alverdy JC, Hall DE, et al. Diverting loop ileostomy and colonic lavage: An alternative to total abdominal colectomy for the treatment of severe, complicated clostridium difficile associated disease. Ann Surg. 2011;254(3):423–7. doi: 10.1097/SLA.0b013e31822ade48. discussion 427–9. [DOI] [PubMed] [Google Scholar]
- 4.Rubio-Perez I, Leon M, Pastor D, et al. Increased postoperative complications after protective ileostomy closure delay: An institutional study. World J Gastrointest Surg. 2014;6(9):169–174. doi: 10.4240/wjgs.v6.i9.169. [DOI] [PMC free article] [PubMed] [Google Scholar]


