Abstract
Background
We sought to identify factors associated with condom-use during anal intercourse among self-identified HIV-negative gay, bisexual, and other men who have sex with men (GBM) in Vancouver, Canada following “treatment as prevention” (TasP) scale-up in 2010.
Methods
Sexually-active GBM were recruited using respondent-driven sampling (RDS) from 2012–2014. We analyzed participants’ most recent sexual encounter with up to their last five sexual partners within the past six months. In addition to individual- and event-level explanatory factors, we assessed potential associations with TasP awareness, TasP-related prevention practice (viral load sorting), and TasP-related attitudes (HIV treatment optimism). Accounting for clustering at the RDS chain- and participant-level, factors associated with event-level condom-use versus non-use were determined using a multivariable generalised linear mixed model built using backward selection and AIC minimization.
Results
Of 513 participants, 436 GBM (85%) reported a total of 1196 anal sex events with 56% condom-use. The proportion of condom-protected sexual events decreased monthly over the study period (OR=0.95 per month, 95%CI:0.92–0.98). TasP practices and attitudes were significantly associated with lower odds of condom-use at the univariate level, but were no longer significant at multivariate level. In the multivariable model, event-level partner methamphetamine use (aOR=0.18, 95%CI:0.06–0.58), frequency of recent anal intercourse with that partner (aOR=0.97 per act, 95%CI:0.95–0.98) and time since first sex with that partner (aOR=0.97 per 6 months, 95%CI:0.95–0.99) were associated with lower odds of condom-use while event-level participant alcohol use (aOR=1.41, 95%CI:1.01–1.98) and no planned future sex with that partner (aOR=1.56, 95%CI:1.08–2.27) were associated with greater odds of condom-use. Event-level receptive-only (aOR=2.10, 95%CI:1.38–3.20) or insertive-only (aOR=2.53, 95%CI:1.64–3.90) sexual positions were associated with greater odds of condom-use compared with reporting both positions.
Conclusions
TasP-related factors were not the most salient predictors of GBM’s condom-use. Health promotion must consider associations between condomless anal sex and substance use and relational factors.
Keywords: condoms, HIV, prevention, gay men, substance misuse
SHORT SUMMARY
HIV-negative gay men’s condom-use during anal intercourse decreased monthly over the study period, and Treatment as Prevention related factors were not the most salient predictors.
INTRODUCTION
In Canada, gay, bisexual, and other men who have sex with men (GBM) accounted for over half of new HIV infections in 2014.[1] In 2010, the province of British Columbia (BC) adopted “treatment as prevention” (TasP) as the key strategy to reduce HIV morbidity and transmission through increased HIV testing and expansion of combination antiretroviral therapy (cART) to all persons living with HIV.[2] Approximately 18% of HIV-positive GBM are unaware of their infection,[1] and in BC, 86% of HIV-diagnosed GBM are on cART, of whom 84% have suppressed viral loads.[3] Although TasP has contributed to earlier HIV-diagnosis and a broader distribution of cART health benefits, there is concern that it may lead to risk compensation[4]. This is the idea that medical innovations intended to decrease adverse event probability could unintentionally lead to increased risky behaviours,[5] which could undermine the benefits combination HIV prevention approaches. It is essential to evaluate possible concomitant impacts of TasP scale-up on an existing prevention strategy such as condom-use.
During anal sex, correct and consistent condom-use is a highly cost-effective method to prevent HIV transmission and other sexually transmitted infections (STI).[6] Also, since TasP places the responsibility for ongoing treatment adherence upon HIV-positive individuals, condoms are a primary prevention strategy for HIV-negative GBM. Given BC’s expansion of TasP in 2010 to extend the reach of testing, cART, and reduce community viral load,[2] there are fundamental gaps in our current understanding of HIV-negative GBM’s condom-use.
Growing optimism regarding medical advancements in HIV treatment, a potential product of TasP promotion, may have implications for condom-use. Past research with HIV-negative GBM in Vancouver found that direct TasP awareness was not associated with risky sex, however this did not assess TasP-related attitudes or behaviours.[7] The limited studies on HAART optimism (a proxy of TasP-related attitudes),[8] and sexual risk among HIV-negative GBM offer contrary findings.[9] As a TasP-informed behavioural measure, viral load sorting is a prevention practice where HIV-negative individuals choose to only have condomless anal sex with partners who are HIV-positive with undetectable viral loads.[10] Research is needed that evaluates broadly possible TasP-associated factors and their impact on condom-use.
Most research investigating substance use and HIV/STI infection is based on situational or global-instead of event-level analyses.[11] Event-level analyses examine variables within the context of a specific sex event, yielding improved causal evidence.[11] Similar to previous research on GBM’s condom-use and HIV risk, we apply a syndemics theory framework, examining how psychosocial (individual-level), relational (partner-level) and situational (event-level) factors interact to increase HIV risk.[12] Using event-level data from HIV-negative GBM, our objectives were to 1) determine the prevalence of condom-use during anal intercourse, 2) evaluate any change over time in condom-use, and 3) identify individual-, partner-, and event-level factors associated with condom-use, with a particular focus on TasP-related factors.
MATERIALS AND METHODS
Study Protocol & Participants
Data are drawn from GBM in Metro Vancouver, the largest metropolitan area of BC. Participants were recruited between February 2012 and February 2014 using respondent-driven sampling (RDS).[13] As per RDS methodology, initial “seed” participants were recruited in-person through partner community agencies or online through advertisements on GBM sociosexual networking websites/apps.[14] Participants were remunerated $50 for their visit, and $10 for each of up to six additional recruits successfully enrolled in the study. Eligibility criteria included: being ≥16 years of age, gender identifying as a man, reporting sex with another man in the past six months, currently living in Metro Vancouver, and being able to complete the questionnaire in English. Written informed consent was secured at the study office in downtown Vancouver. Data were collected during a 90-minute study visit, which included a computer-assisted self-interview (CASI) regarding demographics, sexual behaviour, substance use, and psychosocial attributes, and a subsequent nurse-administered clinical questionnaire and biological specimen collection for HIV, syphilis and Hepatitis C testing. This analysis was limited to participants who self-identified as HIV-negative, that is they did not report being diagnosed previously with HIV. The following institutional Research Ethics approved the study protocol: University of British Columbia (H11-00691), Simon Fraser University (2011s0691), and the University of Victoria (11-459). Additional detail on the study protocol are published elsewhere.[15]
Outcome Variable
The primary outcome of this analysis was condom-protected anal intercourse versus any condomless anal intercourse as measured at each individual sexual episodes/encounters (i.e., event-level data). During the CASI, participants completed a “partner matrix” of a repeating set of questions about their last sexual encounter (event-level factors, see below) with each of up to their five most recent sexual partners within the past six months. Participants were only asked to report on one sexual event, the most recent one, with each of their recent sexual partners (to a maximum of five partners). Sexual encounters that did not include anal intercourse were excluded. Condom-use was coded as such so long as condoms were reported for all sexual positions in that event (receptive, insertive, or both). Otherwise, the outcome was coded as non-use.
Explanatory Variables
All data for explanatory variables were collected during the CASI. Individual-level factors were collected for demographics, psychosocial factors, and prevention practices and attitudes. Event-level factors were collected regarding the partner and the last sexual event with that partner. Each grouping of factors is described in greater detail below.
A number of TasP-related variables were considered. Participants were asked whether they had “heard of the term treatment as prevention” to assess awareness. Participants were asked whether they intentionally had “anal sex without condoms with HIV-positive guys who have low viral loads or are on HIV treatment” in the past six months to assess TasP-related prevention practice. Participants were asked whether they agreed or disagreed with the following statement to assess TasP-related attitude: “Knowing a sex partner’s viral load is just as important as knowing their HIV status”. Finally, participants completed a 12-item HAART optimism scale (study alpha = 0.79, scale range 12–48) with greater scores indicating great optimism.[8]
Demographic information was collected for age group, sexual orientation, race/ethnicity, annual income, and relationship status (single, not married/common-law, married/common-law). Participants also indicated the timing of their most recent HIV test. A series of potential HIV prevention or risk reduction practices (i.e., consistent condoms, strategic positioning, anal abstinence, serosorting, withdrawal, and asking HIV status before sex) were posited to participants who indicated whether they used these in the past six months or not.
A number of other psychosocial scales were included: 11-item Sexual Sensation Seeking Scale (revised) (range 11–44; study alpha = 0.78) with greater scores indicating more sexual sensation seeking,[16] 7-item personal subscale and a 6-item communal subscale for sexual altruism (zero-based average, range 0–4; study alpha = 0.73) with greater scores indicating more altruism,[17] 12-item Escape Motivation scale (range 12–48; study alpha = 0.89) with greater scores indicating more escape motivations,[18] and two 7-item subscales for anxious and depressive symptoms using the Hospital Anxiety and Depression Scale (range 0–21; study alphas = 0.84, 0.79, respectively) with greater scores indicating more anxiety and depression symptomology, respectively.[19] An example item from the Escape Motivation scale is, “When I am drunk or high, I will do anything with anyone.”, which participants rate on a 4-point Likert scale from Strongly Disagree (1) to Strongly Agree (4).
Event-level factors were collected for each partner and sexual event. Participants indicated the number of months since they first had sex with that partner (per 6-month period) and the number of times they had anal sex with this partner in the past 6 months (per act). Participants indicated the month and year of the last sexual event they had with each partner, which was used to conduct a change over time analysis (see below). For each sexual event, participants indicated their anal sex positions (receptive, insertive, or both), their level of certainty regarding their partner’s HIV status before sex, whether they would have sex with this partner again in the future, and whether they had received any goods, money, drugs or services in return for sex. Participants also reported on their own and their partners’ substance use for the two hours prior to and during the sexual encounter for a variety of substances (e.g., alcohol, marijuana, poppers, erectile dysfunction drugs (EDD), crystal methamphetamine, gamma-hydroxybutyrate (GHB), and ecstasy/MDMA).
Analyses
Data analysis began by limiting the analysis to participants and events that reported anal intercourse. Given multiple sexual events were reported by the same participant, known as “one with many”[20], we used a generalized linear mixed model with a random effect for participant to address clustering at that level.[21] We also included another random effect for RDS chain to address potential clustering given recruitment occurred within socio-sexual networks. As the outcome level was binary (condom-use versus non-use), we used a mixed effects logistic model. Univariate associations were prepared for all individual-level and event-level explanatory factors. A multivariable model was built using manual backward selection and Type III p-value and AIC minimization to select the optimal factors to retain in the final model.[22] Change over time in the proportion of anal sex events where condom-use was reported versus not (outcome) was assessed using a continuous variable for month (explanatory factor) in the same regression method described above. To allow for consistent power across months (as recruitment was slower at the beginning and end of the study period), events reported during or before February 2012 were collapsed together as were events reported during or after December 2013; all over events were grouped into the month in which they were reported to have occurred. All analyses were conducted using SAS® version 9.3 (SAS, North Carolina, United States).
RESULTS
A total of 524 self-identified HIV-negative GBM were recruited into the study. Of these, 513 completed the partner matrix with a total of 1,866 sexual encounters reported (mean=3.64/participant). Most participants reported at least one anal intercourse event (n=436/513, 85.0%), of whom 36.7% reported consistent condom-use across all of their anal intercourse events. Across the 1866 sexual encounters reported in the event-level data, most encounters included anal intercourse (n=1196/1886, 64.1%).
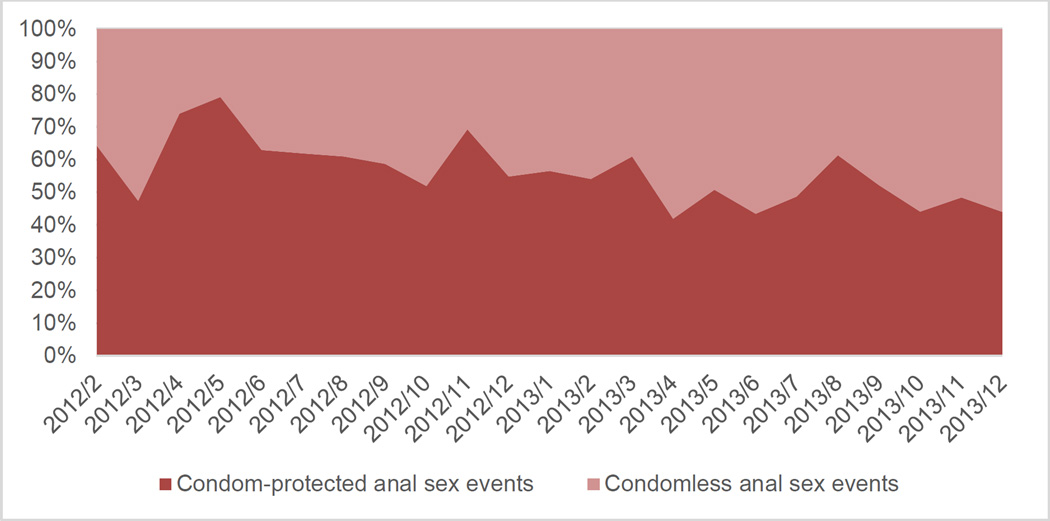
Of the 1196 anal sex events (ASE) used for these analyses, 55.5% reported condom-use. Figure 1 shows the proportion of events with reported condom-use across each month of the study period. The likelihood of condom-use decreased monthly over the study period (OR=0.95, 95% CI: 0.92–0.98). For example, 64.3% of ASEs reported condom-use in the first time period while only 44.0% of ASEs reported condom-use in the final time period. By sexual position, of the 1196 ASEs, 493 included only insertive anal sex roles (n=280/493, 56.8% with consistent condom-use), 453 included only receptive anal sex roles (n=286/453, 57.1% with consistent condom-use), and 250 included both anal sex roles. Of these 250 events, 234 reported either consistent condom-use or consistent non-use for both sexual positions (n=98, 39.2% reported consistent condom-use across both roles; n=136, 54.4% reported condomless anal sex in both roles). As such, only 16 of 250 dual sexual position events (6.4%), or 1.3% of all ASEs, reported differential condom-use across sexual positions.
Figure 1.
Proportion of condom-protected anal sex events reported over time (by month)
Notably, consistent condom-use during the 1196 ASEs varied by awareness of partner’s HIV status: 67.0% with unknown status partners (n=209/312 events), 56.2% for partners thought to be HIV-negative (n=181/322), 53.7% with partners thought to be certainly HIV-negative (n=255/475), 22.7% with partners thought to be certainly HIV-positive (n=17/75), and 16.7% with partners thought to be HIV-positive (n=2/12).
Table 1 presents the descriptive statistics, univariate associations, and multivariate associations for condom-use for individual-level factors in our analysis. There was no significant difference in condom-use reported between participants who had heard of TasP compared with those who hadn’t (p=0.44). However, two other TasP-related factors were significantly associated with lower odds of condom-use at the univariate level: having reported use of viral load sorting as a prevention practice in the past six months (OR=0.18, 95% CI: 0.10–0.31) and reporting greater Treatment Optimism on the scale (OR=0.90, 95% CI: 0.87–0.93). Table 2 presents the descriptive statistics, univariate associations, and multivariate associations for condom-use for event-level and partner-level factors.
Table 1.
Individual-level factor descriptive statistics and associations with condom use versus non-use during anal sex events
| Participants | Anal Sex Events (ASE) |
Condom-protected ASE |
Univariate Associations |
Multivariate Associations* |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | OR | 95% CI | AOR | 95% CI | |||
| Age Categories | ||||||||||||
| 18–29 | 267 | 51.0 | 666 | 55.7 | 411 | 61.9 | Ref | |||||
| 30–44 | 165 | 31.5 | 362 | 30.3 | 174 | 26.2 | 0.55 | 0.38 | 0.81 | |||
| 45+ | 92 | 17.6 | 168 | 14.1 | 79 | 11.9 | 0.54 | 0.32 | 0.91 | |||
| Sexual Orientation | ||||||||||||
| Gay | 445 | 84.9 | 1051 | 87.9 | 580 | 87.4 | Ref | |||||
| Bisexual | 45 | 8.6 | 83 | 6.9 | 41 | 6.2 | 0.87 | 0.46 | 1.67 | |||
| Other | 34 | 6.5 | 62 | 5.2 | 43 | 6.5 | 2.04 | 0.93 | 4.47 | |||
| Race/Ethnicity | ||||||||||||
| White | 390 | 74.4 | 900 | 75.3 | 488 | 73.5 | Ref | |||||
| Asian | 60 | 11.5 | 123 | 10.3 | 80 | 12.1 | 1.52 | 0.86 | 2.67 | |||
| Aboriginal | 29 | 5.5 | 53 | 4.4 | 25 | 3.8 | 0.64 | 0.28 | 1.50 | |||
| Other | 45 | 8.6 | 120 | 10.0 | 71 | 10.7 | 1.08 | 0.60 | 1.94 | |||
| Annual Income ($CAD) | ||||||||||||
| <$30,000 | 313 | 59.7 | 694 | 58.0 | 414 | 62.4 | Ref | Ref | ||||
| ≥$30,000 | 211 | 40.3 | 502 | 42.0 | 250 | 37.7 | 0.64 | 0.45 | 0.91 | 0.65 | 0.46 | 0.93 |
| Relationship status | ||||||||||||
| Not partnered | 323 | 61.6 | 769 | 64.3 | 459 | 69.1 | Ref | |||||
| Partnered, but not married/common law | 110 | 21.0 | 250 | 20.9 | 134 | 20.2 | 0.74 | 0.48 | 1.14 | |||
| Partnered, and married/common law | 91 | 17.4 | 177 | 14.8 | 71 | 10.7 | 0.38 | 0.24 | 0.63 | |||
| Last HIV test | ||||||||||||
| <6 months ago | 198 | 48.4 | 542 | 58.3 | 294 | 56.5 | Ref | |||||
| 6 months – 2 years ago | 151 | 36.9 | 283 | 30.4 | 168 | 32.3 | 1.17 | 0.77 | 1.80 | |||
| >2 years ago | 33 | 8.1 | 53 | 5.7 | 29 | 5.6 | 0.99 | 0.44 | 2.23 | |||
| Never tested | 27 | 6.6 | 52 | 5.6 | 29 | 5.6 | 0.92 | 0.40 | 2.09 | |||
|
Prevention practices
(mutually exclusive; referent: don’t use) |
||||||||||||
| Consistent condoms “Always using condoms for anal sex” |
335 | 64.4 | 739 | 62.2 | 526 | 79.3 | 6.48 | 4.59 | 9.14 | 4.04 | 2.74 | 5.95 |
| Strategic positioning “Being the top for anal sex” |
138 | 26.5 | 344 | 29.0 | 149 | 22.5 | 0.48 | 0.33 | 0.70 | |||
| Anal abstinence “Having sex which doesn’t include anal sex” |
258 | 49.6 | 477 | 40.2 | 269 | 40.6 | 1.09 | 0.77 | 1.55 | |||
| Sero-sorting “Having anal sex without condoms only with guys I know are HIV- negative” |
182 | 35.0 | 476 | 40.1 | 192 | 29.0 | 0.31 | 0.22 | 0.44 | 0.50 | 0.35 | 0.73 |
| Withdrawal “Not letting my sex partners cum inside me” |
146 | 28.1 | 354 | 29.8 | 192 | 29.0 | 0.93 | 0.64 | 1.36 | |||
| Ask Status “Asking my sex partners about their HIV status before sex” |
326 | 62.7 | 793 | 66.8 | 418 | 63.1 | 0.73 | 0.51 | 1.06 | |||
|
TasP awareness: “heard of the term treatment as prevention” |
||||||||||||
| No | 299 | 57.2 | 699 | 58.5 | 381 | 57.5 | Ref | |||||
| Yes | 224 | 42.8 | 496 | 41.5 | 282 | 42.5 | 1.15 | 0.81 | 1.63 | |||
|
TasP-related prevention practice: “Having anal sex without condoms with HIV-positive guys who have low viral loads or are on HIV treatment” |
||||||||||||
| Yes | 469 | 90.2 | 1028 | 86.5 | 625 | 94.3 | Ref | |||||
| No | 51 | 9.8 | 160 | 13.5 | 38 | 5.7 | 0.18 | 0.10 | 0.31 | |||
|
TasP-related attitude: “Knowing a sex partner’s viral load is just as important as knowing their HIV status” |
||||||||||||
| Disagree | 163 | 31.8 | 357 | 30.6 | 220 | 33.6 | Ref | Ref | ||||
| Agree | 349 | 68.2 | 811 | 69.4 | 434 | 66.4 | 0.75 | 0.51 | 1.09 | 0.70 | 0.47 | 1.03 |
| Psychosocial factors (mutually exclusive) | median | Q1,Q3 | median | Q1,Q3 | median | Q1,Q3 | OR | 95% CI | AOR | 95% CI | ||
| Treatment Optimism | 24 | 20, 27 | 24 | 20, 27 | 23 | 20, 25 | 0.90 | 0.87 | 0.93 | |||
| Sexual Sensation Seeking Scale | 30 | 28, 33 | 31 | 28, 34 | 30 | 28, 33 | 0.90 | 0.86 | 0.94 | |||
| Escape Motivation | 28 | 24, 32 | 29 | 25, 33 | 28 | 24, 32 | 0.96 | 0.93 | 0.98 | 0.96 | 0.93 | 0.99 |
| Sexual Altruism – Personal | 3.57 | 3, 4 | 3.43 | 3, 4 | 3.57 | 3, 4 | 2.25 | 1.60 | 3.16 | |||
| Sexual Altruism – Communal | 3.67 | 3, 4 | 3.50 | 3, 4 | 3.67 | 3, 4 | 2.35 | 1.80 | 3.08 | 1.64 | 1.22 | 2.21 |
| HAD – Anxiety | 8 | 5, 10 | 8 | 5, 10 | 8 | 5, 10 | 1.03 | 0.99 | 1.08 | |||
| HAD – Depression | 3 | 1, 6 | 3 | 1, 5 | 3 | 2, 6 | 1.05 | 1.00 | 1.11 | |||
95% CI = 95% confidence interval; OR = odds ratio; $CAD = Canadian dollars; Q1,Q3 = first quartile, third quartile values. Bolded text indicates statistical significant at p<0.05.
The multivariable model also includes event-level factors listed in Table 2.
Table 2.
Partner- and event-level factor descriptive statistics and associations with condom use versus non-use during anal sex events
| Anal Sex Events (ASE) |
Condom- Protected ASE |
Univariate Associations | Multivariate Associations* |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| median | Q1,Q3 | median | Q1,Q3 | OR | 95%CI | AOR | 95%CI | |||
|
Time since first sex with partner (for each 6 month period) |
4 | 1, 12 | 3 | 1, 8 | 0.96 | 0.93 | 0.98 | 0.97 | 0.95 | 0.99 |
|
Number of times of anal sex in P6M (for each episode) |
2 | 1, 5 | 1 | 1, 3 | 0.95 | 0.94 | 0.97 | 0.97 | 0.95 | 0.98 |
| n | % | n | % | OR | 95%CI | AOR | 95%CI | |||
| Sexual position(s) | ||||||||||
| Both insertive and receptive | 250 | 20.9 | 98 | 14.8 | Ref | Ref | ||||
| Receptive only | 493 | 41.2 | 280 | 42.2 | 2.09 | 1.43 | 3.06 | 2.10 | 1.38 | 3.20 |
| Insertive only | 453 | 37.9 | 286 | 43.1 | 2.72 | 1.85 | 4.01 | 2.53 | 1.64 | 3.90 |
| Aware of partner’s HIV status | ||||||||||
| No, I did not know his HIV status | 312 | 26.1 | 209 | 31.5 | Ref | |||||
| Yes, I was certain he was HIV-negative | 475 | 39.7 | 255 | 38.4 | 0.50 | 0.34 | 0.72 | |||
| Yes, I think he was HIV-negative | 322 | 26.9 | 181 | 27.3 | 0.63 | 0.42 | 0.95 | |||
| Yes, I was certain he was HIV-positive | 75 | 6.3 | 17 | 2.6 | 0.14 | 0.07 | 0.29 | |||
| Yes, I think he was HIV-positive | 12 | 1.0 | 2 | 0.3 | 0.12 | 0.02 | 0.78 | |||
| “Yes” to future sex with partner | ||||||||||
| Yes | 349 | 29.2 | 142 | 21.4 | Ref | Ref | ||||
| No | 847 | 70.8 | 522 | 78.6 | 2.64 | 1.93 | 3.62 | 1.56 | 1.08 | 2.27 |
| Transactional Sex (received something) | ||||||||||
| No | 1191 | 99.6 | 662 | 99.7 | Ref | |||||
| Yes | 39 | 3.3 | 22 | 3.3 | 0.97 | 0.44 | 2.17 | |||
|
Participant substance use
(mutually exclusive; referent: not used) |
||||||||||
| Any alcohol use | 466 | 39.2 | 295 | 44.7 | 1.58 | 1.17 | 2.14 | 1.41 | 1.01 | 1.98 |
| Any marijuana use | 232 | 19.6 | 125 | 19.0 | 1.00 | 0.68 | 1.47 | |||
| Any poppers use | 175 | 14.9 | 73 | 11.2 | 0.60 | 0.39 | 0.92 | |||
| Any EDD use | 91 | 7.7 | 37 | 5.7 | 0.59 | 0.32 | 1.08 | |||
| Any crystal methamphetamine use | 51 | 4.3 | 10 | 1.5 | 0.21 | 0.09 | 0.52 | |||
| Any GHB use | 32 | 2.7 | 11 | 1.7 | 0.50 | 0.20 | 1.23 | |||
| Any ecstasy/MDMA use | 39 | 3.3 | 16 | 2.4 | 0.60 | 0.27 | 1.35 | |||
|
Partner substance use
(mutually exclusive; referent: not used) |
||||||||||
| Any alcohol use | 426 | 35.8 | 264 | 40.0 | 1.37 | 1.01 | 1.85 | |||
| Any marijuana use | 207 | 17.5 | 107 | 16.2 | 0.80 | 0.55 | 1.17 | |||
| Any poppers use | 183 | 15.6 | 87 | 13.3 | 0.74 | 0.50 | 1.11 | |||
| Any EDD use | 42 | 3.6 | 16 | 2.5 | 0.53 | 0.23 | 1.21 | |||
| Any crystal methamphetamine use | 52 | 4.4 | 8 | 1.2 | 0.18 | 0.07 | 0.45 | 0.18 | 0.06 | 0.58 |
| Any GHB use | 29 | 2.5 | 11 | 1.7 | 0.66 | 0.26 | 1.68 | |||
| Any ecstasy/MDMA use | 34 | 2.9 | 14 | 2.1 | 0.63 | 0.27 | 1.46 | |||
Q1,Q3 = first quartile, third quartile values; OR = odds ratio; 95% CI = 95% confidence interval; EDD = erectile dysfunction drugs; GHB = gamma-hydroxybutyric; MDMA = 3,4-methylenedioxymethamphetamine. Bolded text indicates statistical significant at p<0.05.
The multivariable model also includes individual-level factors listed in Table 1.
The multivariable generalized linear mixed effect logistic regression model for event-level condom-use versus non-use is shown in the far right columns of Table 1 and Table 2. Significantly greater odds of condom-use was associated with reporting consistent condom-use as a recent preventive practice (aOR=4.04, 95% CI:2.74–5.95), greater Communal Sexual Altruism scale scores (aOR=1.64, 95% CI:1.22–2.21), reporting only a receptive (aOR=2.10, 95% CI:1.38–3.20) or insertive anal sex role (aOR=2.53, 95% CI:1.64–3.90) versus both, reporting no future plan to have sex with that partner (aOR=1.56, 95% CI:1.08–2.27), and reporting their own use of alcohol before or during sex (aOR=1.41, 95% CI:1.01–1.98). Significantly lower odds of condom-use was associated with reporting an annual income of greater than $30,000 CAD (aOR=0.65, 95% CI:0.46–0.93), reporting sero-sorting as a recent preventive practice (aOR=0.50, 95% CI:0.35–0.73), reporting greater Escape Motivation scale scores (aOR=0.96, 95% CI:0.93–0.99), having first had sex with that partner longer ago (aOR=0.97 per 6-month period, 95% CI:0.95–0.99), having had more recent anal sex with that partner (aOR=0.97 per act, 95% CI:0.95–0.98), and reporting crystal methamphetamine use by their partner (aOR=0.18, 95% CI: 0.06–0.58).
DISCUSSION
Our study was conducted in Vancouver, where major efforts regarding TasP promotion and rollout have been underway since 2010.[2] We analyzed 1886 recent anal intercourse events reported by 513 self-reported HIV-negative GBM and determined a 55.5% overall prevalence of event-level condom-use during anal intercourse. However, condom-use decreased significantly over the study period, which provides some indication of an ecological or cultural shift away from condom-use for some GBM.[23] We examined associations between condom-use and various TasP-related factors. In our study, TasP awareness was not associated with event-level condom-use, which may indicate the limitations of this measure as an explanatory factor of risk compensation.[4–5] Although not significant in our multivariable model, we found significantly lower odds of condom-use reported by GBM who reported viral load sorting and greater HAART optimism (TasP-related prevention practice and attitudes) at the univariable level. Our findings add to a growing number of studies suggesting that greater uptake and confidence in HIV treatment coincide with sexual risk compensation among GBM.[9] These findings reflect an accurate perception of GBM that treatment reduces the risk of HIV transmission.
Compared with more commonly used period prevalence measures, our use of event-level data provide better evidence for temporal causality and more salient predictors of condom-use. Particularly with regards to substance use, event-level crystal methamphetamine use was linked to condomless sex in our study, as in a recent event-level systematic review.[11] This review also identified binge drinking (≥5 alcoholic drinks per occasion) with condomless sex, while our study recognized alcohol use as a protective factor. Our study instrument was not able to distinguish between any and binge use of alcohol. As such, our protective finding likely reflects the varied levels of and reasons for alcohol use in social-sexual settings,[12] and indicates that health promotion and research need to distinguish between binge and non-binge drinking.
Partner familiarity or relational closeness, which was captured in our analysis by longer time since first sex, greater sexual experience, and future intentions to have sex with that partner, continues to drive a certain proportion of condom non-use.[24] Prior research demonstrates that condom-use is habitual across partner types and sexual positions,[21] and that most HIV infections occurred within the context of main partnerships given reduced condom-use, increased sexual versatility, and more frequent sex.[25] Indeed, we found that individuals reporting both anal sex positions were significantly less likely to report condom-use than those men reporting engaging in only one position.
Longitudinal research has demonstrated that GBM are challenged to maintain any prevention practice over time, which degrades their effectiveness.[26] Interventions and health promotion programs that improve condom-use must focus on appropriate and consistent use.[27] Fortunately, we found that men who reported intentional consistent condom-use as a prevention strategy had four times greater odds of condom-use at the event-level. Condoms provide prevention for many STIs, but the TasP- and HAART-related attitudes and seroadaptive practices of men with lower odds of condom-use in our study reflect intentional consideration to reduce their possibility of acquiring HIV, potentially without (equal) concern for other STIs. In lieu of condom-use, HIV pre-exposure prophylaxis (PrEP) offers the only other effective primary prevention intervention to limit onward sexual transmission of acute HIV infection within sexual networks with low/no condom-use.[28] However, none of our participants reported PrEP use, which was not approved for use in Canada nor was there a publicly funded access program during the study period.[29] Sero-sorting as a risk reduction strategy was also associated with condom non-use, emphasizing the importance of interventions that support disclosure between sexual partners, and appropriate adherence to HIV testing guidelines. Efforts to improve modifiable attitudes such as sexual altruism may provide such an opportunity to improve safer sex practices.
Our study had a number of limitations. Participants were only asked to report on their most recent sex with a partner (one event per partner), which was intended to reduce recall bias by limiting the time between survey data and sexual event, but may have introduced order bias. Despite the significance of partner-level factors in our findings, we were unable to distinguish between different romantic or emotional partner types, such as those with a main partner(s) versus casual extra-relational partners. It is important to note that these analyses focused exclusively on events where anal intercourse was reported, and the patterns observed may differ if non-anal intercourse events were included. Finally, given the multilevel nature of the data, future research could explore statistical interactions between individual-level traits and event-level factors.
In conclusion, our work demonstrates that condom-use may be decreasing among Vancouver GBM, but that TasP-related attitudes and practices were not the most salient predictors of event-level condom-use. As such, health promotion must promote frank dialogue regarding HIV status, relational factors, and substance use. Crystal methamphetamine may require more specific programming to reduce problematic substance use, given its repeated significance in research.[11] Future prospective longitudinal research must evaluate within-person change over time in condom-use, substance use, sexual behaviour and attitudes, and the relationships between these factors. Research must also determine whether these population-level changes have impacted other STI transmission rates.
REFERENCES
- 1.Public Health Agency of Canada (PHAC) Estimates of HIV Incidence, Prevalence and Proportion Undiagnosed in Canada, 2014. Ottawa, Canada: 2015. Nov, [Accessibility verified 2015 Dec 18]. Available from http://healthycanadians.gc.ca/publications/diseases-conditions-maladies-affections/hiv-aids-estimates-2014-vih-sida-estimations/alt/hiv-aids-estimates-2014-vih-sida-estimations-eng.pdf. [Google Scholar]
- 2.Johnston C. Shifting the paradigm: The history of the Vancouver STOP HIV/AIDS Project. Vancouver, Canada: 2013. Available from: http://www.catie.ca/sites/default/files/stop_EN_2013_10_07.pdf. [Google Scholar]
- 3.HIV Monitoring Quarterly Report for British Columbia: Third Quarter 2015. Vancouver, Canada: 2015. [Accessibility verified 2015 Dec 18]. BC Centre for Excellence in HIV/AIDS. Available from: http://www.cfenet.ubc.ca/sites/default/files/uploads/publications/centredocs/bc-monitoring-report-15q3-corrected-d.pdf. [Google Scholar]
- 4.Sullivan PS, Carballo-Diéguez A, Coates T, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–399. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilde G. Target Risk: Dealing with the Danger of Death, Disease, and Damage in Everyday Decisions. Ontario, Canada: PDE Publications; 1994. [Google Scholar]
- 6.Beyrer C, Sullivan PS, Sanchez J, et al. A call to action for comprehensive HIV services for men who have sex with men. Lancet. 2012;380:424–438. doi: 10.1016/S0140-6736(12)61022-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carter A, Lachowsky N, Rich A, et al. Gay and bisexual men's awareness and knowledge of treatment as prevention: findings from the Momentum Health Study in Vancouver, Canada. J Int AIDS Soc. 2015;18(1) doi: 10.7448/IAS.18.1.20039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van de Ven P, Crawford J, Kippax S, et al. A scale of optimism-skepticism in the context of HIV treatments. AIDS Care. 2000;12:171–176. doi: 10.1080/09540120050001841. [DOI] [PubMed] [Google Scholar]
- 9.Chen Yiyun. Treatment-related optimistic beliefs and risk of HIV transmission: a review of recent findings (2009–2012) in an Era of treatment as prevention. Curr HIV/AIDS Rep. 2013;10:79–88. doi: 10.1007/s11904-012-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van de Ven P, Mao L, Fogarty A, et al. Undetectable viral load is associated with sexual risk taking in HIV serodiscordant gay couples in Sydney. AIDS. 2005;19(2):179–184. doi: 10.1097/00002030-200501280-00010. [DOI] [PubMed] [Google Scholar]
- 11.Vosburgh H, Mansergh G, Sullivan PS, et al. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- 12.Mustanski BS, Newcomb ME, Du Bois SN, et al. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volz E, Heckathorn DD. Probability based estimation theory for respondent driven sampling. J Official Statistics. 2008;24(1):79. [Google Scholar]
- 14.Lachowsky NJ, Lal A, Forrest JI, et al. Including Online-Recruited Seeds: A Respondent-Driven Sample of Men Who Have Sex With Men. J Med Int Res. 2016;18(3) doi: 10.2196/jmir.5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore DM, Cui Z, Lachowsky N, et al. HIV Community Viral Load and Factors Associated With Elevated Viremia Among a Community-Based Sample of Men Who Have Sex With Men in Vancouver, Canada. J AIDS. 2016;72(1):87–95. doi: 10.1097/QAI.0000000000000934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalichman S, Rompa D. Sexual sensation seeking and sexual compulsivity scales: reliability, validity and predicting HIV risk behavior. J Pers Assess. 1995;65:586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 17.Nimmons D, Folkman S. Other-sensitive motivations for safer sex among gay men: expanding paradigms for HIV prevention. AIDS Behav. 1999;3:313–324. [Google Scholar]
- 18.McKirnan DJ, Vanable PA, Ostrow DG, et al. Expectancies of sexual “escape” and sexual risk among drug-and alcohol-involved gay and bisexual men. J Subst Abuse. 2001;13:137–154. doi: 10.1016/s0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- 19.Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rich AJ, Lachowsky NJ, Cui Z, et al. Event-level analysis of anal sex roles and sex drug use among gay and bisexual men in Vancouver, British Columbia, Canada. Arch Sex Behav. 2015 doi: 10.1007/s10508-015-0607-0. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lachowsky NJ, Dewey CE, Dickson NP, et al. Habitual condom use across partner type and sexual position among younger gay and bisexual men: findings from New Zealand HIV behavioural surveillance 2006–2011. Sex Transm Infect. 2015;91:445–450. doi: 10.1136/sextrans-2014-051759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lima VD, Harrigan R, Murray M, et al. Differential impact of adherence on long-term treatment response among naive HIV-infected individuals. AIDS. 2008;22:2371–2380. doi: 10.1097/QAD.0b013e328315cdd3. [DOI] [PubMed] [Google Scholar]
- 23.Darbes LA, Chakravarty D, Neilands TB, et al. Sexual risk for HIV among gay male couples: a longitudinal study of the impact of relationship dynamics. Arch Sex Behav. 2014;43:47–60. doi: 10.1007/s10508-013-0206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phillip AN, Cambiano V, Nakagawa F, et al. Increased HIV incidence in men who have sex with men despite high levels of ART-indicated viral suppression: analysis of an extensively documented epidemic. PLoS ONE. 2013;8(2):e55312. doi: 10.1371/journal.pone.0055312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sullivan PS, Salazar L, Buchbinder S, et al. Estimating the proportion of HIV transmission from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 26.McFarland W, Chen YH, Nguyen B, et al. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16:121–131. doi: 10.1007/s10461-011-9936-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Emetu RE, Marshall A, Sanders SA, et al. A novel, self-guided, home-based intervention to improve condom use among young men who have sex with men. J Amer College Health. 2014;62:118–124. doi: 10.1080/07448481.2013.856914. [DOI] [PubMed] [Google Scholar]
- 28.Hojilla JC, Koester KA, Cohen SE, et al. Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: a qualitative analysis of counseling notes. AIDS Behav Published Online First. 2015 Apr 3; doi: 10.1007/s10461-015-1055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lachowsky NJ, Lin SY, Hull MW, et al. Pre-exposure Prophylaxis Awareness Among Gay and Other Men who have Sex with Men in Vancouver, British Columbia, Canada. AIDS Behav. 2016;20(7):1408–1422. doi: 10.1007/s10461-016-1319-8. [DOI] [PMC free article] [PubMed] [Google Scholar]