Abstract
BACKGROUND
We evaluated the 12-month effects of the COPE (Creating Opportunities for Personal Empowerment) Healthy Lifestyles TEEN (Thinking, Emotions, Exercise, Nutrition) program versus an attention control program (Healthy Teens) on overweight/obesity and depressive symptoms in high school adolescents.
METHODS
A cluster randomized controlled trial was conducted. Participants were 779 culturally diverse adolescents in the US Southwest. COPE is a cognitive-behavioral skills-building intervention with 20 minutes of physical activity integrated into a health course and taught by teachers once a week for 15 weeks. Outcome measures included body mass index (BMI) and depressive symptoms.
RESULTS
COPE teens had a significantly lower BMI at 12 months (F1, 698 = 11.22, p = .001) than Healthy Teens (24.95 versus 25.48). There was a significant decrease in the proportion of overweight and obese COPE teens from baseline to 12 months (χ2= 5.40, p = .02) as compared to Healthy Teens. For youth who began the study with extremely elevated depressive symptoms, COPE teens had significantly lower depression at 12 months compared to Healthy Teens (COPE M=42.39; Healthy Teens M=57.90); (F1, 12 = 5.78, p = .03).
CONCLUSIONS
COPE can improve long-term physical and mental health outcomes in teens.
Keywords: mental health outcomes, obesity, depression, health beliefs, health behavior
Overweight/obesity and mental health disorders are 2 significant public health problems that threaten the health outcomes and academic performance of American adolescents.1,2 The prevalence of youth who are overweight/obese has increased dramatically over the past 2 decades, with approximately 17% being obese (ie, sex and age-specific body mass index [BMI] percentiles at or above the 95%) and 15% overweight (ie, sex and age-specific BMI percentiles between the 85th and 94.9th%).3 Findings from the national 2011 Youth Risk Behavior Survey (YRBS) indicated that the percentage of high school students who are obese increased during 2009–2011.4 Being overweight predisposes teens to adverse health outcomes compared to their non-overweight counterparts, including Type 2 diabetes, hypertension, dyslipidemia, sleep apnea, increased asthma symptoms and a shortened life span.5–7 Overweight and obese teens also have a higher prevalence of school and mental health problems, including academic problems, poor social skills, depressive disorders and a greater number of reported suicide attempts.8–14
Additionally, 15 million US children and teens have a mental health problem that interferes with their functioning at home or at school, yet less than 25% receive treatment.11,15 Depression among teens leads to disabling morbidity and significant mortality.16,17 Depressive symptoms severe enough to impair daily functioning are reported by 37% of girls and 20% of boys.1 Depressed teens also typically have ongoing altered psychosocial and academic functioning, even after these conditions resolve.18–21 The prevalence rates of obesity and mental health problems are even higher in Hispanic and African-American teens22,23, with the 2 conditions often co-existing.24,25
The latest YRBS data on obesity in teens show that more effective school-based programs are needed to improve adolescent health outcomes. However, even though high schools are an ideal setting to provide adolescents with needed skills to enhance their healthy lifestyle behaviors and mental health outcomes, there are few well-designed health promotion intervention studies that have measured both short- and more long-term physical and mental health outcomes.4 Most high school intervention studies have had major methodological flaws (eg, lack of attention to control or comparison groups, small sample sizes, large attrition rates, short-term follow-up) and have targeted only the measurement of a single health outcome, such as depression, substance use or obesity.25 Therefore, evidence is lacking to guide educational curricula regarding whether more comprehensive health promotion interventions delivered in high schools can improve and sustain a variety of positive health outcomes in adolescents.
The primary aim of this study, a cluster randomized controlled trial (RCT), was to evaluate the more long-term efficacy of the COPE (Creating Opportunities for Personal Empowerment) Healthy Lifestyles TEEN (Thinking, Emotions, Exercise, Nutrition) program, versus an attention control program (ie, Healthy Teens), on overweight/obesity and depressive symptoms of 14-to-16 year-old high school adolescents 12 months post-intervention. As reported in an earlier publication,26 immediately following the intervention, COPE teens had greater steps per day (p = .003) and a lower BMI than Healthy Teens (p = .01). COPE teens also demonstrated higher social skills (p < .05), including academic competence, and reported less alcohol use as well as had higher health course grades than Healthy Teens. In addition, for those teens with severe depressive symptoms at baseline, COPE teens scored significantly less on depressive symptom than Healthy Teens (p = .02). Six months following the intervention, COPE teens had a lower mean BMI than Healthy Teens (COPE=24.72, Healthy Teens=25.05, adjusted M=−0.34, 95% CI=−.56, −0.11). Further, the proportion of overweight was significantly different from pre-intervention to the 6-month follow-up with the COPE group decreasing the proportion of overweight teens versus an increase in overweight in the control adolescents (χ2=4.69, p = .03). Fewer COPE teens than Healthy Teens moved from the normal weight category to overweight and none became obese.24 Therefore, it was hypothesized that adolescents who received the COPE program would have less overweight/obesity and fewer depressive symptoms at 12 months following the intervention than teens receiving the Healthy Teens attention control program.
METHODS
Study Design and Setting
This study was a prospective, blinded, cluster RCT that tested the efficacy of the COPE Program in improving overweight/obesity and depressive symptoms in high school adolescents 12 months following completion of the intervention programs. Eleven high schools were chosen by district personnel within 2 school districts in the Southwest Region of the United States to participate in this study. The 11 schools were then randomly assigned to receive either the COPE program or the attention control Healthy Teens program by placing all of the school names in a hat and then using a random selection method. Participating classrooms within the randomly assigned COPE schools delivered the COPE program whereas participating classrooms within the randomly assigned attention control schools delivered the Healthy Teens program. Schools were not matched on any characteristic. To decrease the chance of cross-group contamination between teens in the same high school and limit threats to the study’s internal validity, random assignment of schools versus individual classrooms to study group was conducted.
Participants
Youth 14–16 years old (mainly freshmen and sophomores) enrolled in required health education courses were recruited to participate in the study from 11 high schools in 2 school districts located in the Southwestern Region of the United States. The schools were selected for their diversity across race/ethnicity and varied economic status. Teens who could read and speak English and of any sex, ethnicity/race, or socioeconomic status were eligible for participation if they provided assent and their custodial parent gave consent for them to enroll in the study.
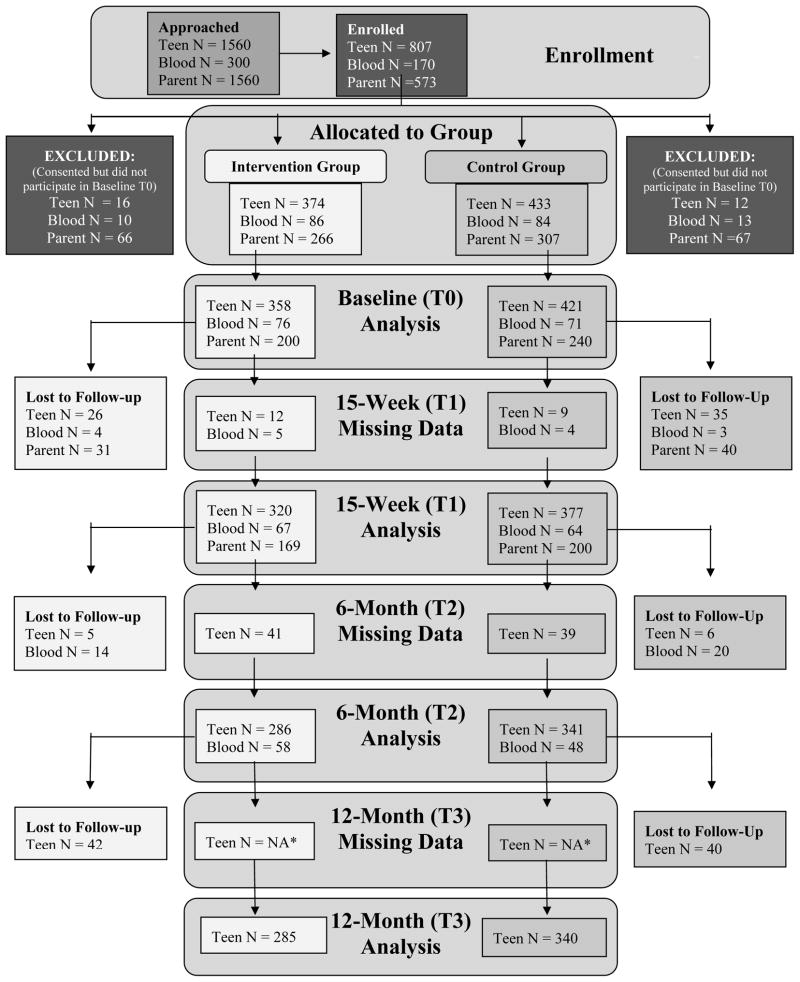
All teens in required health education courses in the participating high schools were invited to participate in the study. Specifics of the protocol are published elsewhere.16 Teens who returned a signed assent and parent consent were enrolled in the trial. Teen enrollment and participation in the study is outlined in Figure 1.
Figure 1.
Flow Diagram
Lost to Follow up= any participant who does not participate in the final data collection (T3);
*By definition, all missing data at the final time point are considered to be lost to follow up regardless of the reason.
All students in the health classes received either the COPE or Healthy Teens program. However, outcome measures were obtained only on the students enrolled in the trial. During the period from December 2009 to December 2012, 779 adolescents were enrolled in the study. Demographics of the adolescents are outlined in Table 1. Approximately two-thirds of the teens identified themselves as being Hispanic and slightly more than half were girls.
Table 1.
Baseline Findingsa and Demographics
| Characteristic | No. (%) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | COPE | Healthy Teens | ||||||
| (N = 779) | (N = 358) | (N = 421) | ||||||
| Age, mean (SD), yb | 14.74 | (.73) | 14.75 | (.76) | 14.74 | (.70) | .89 | |
| Sexc, N (%) | ||||||||
| Female | 402 | (51.60) | 195 | (54.50) | 207 | (49.20) | .14 | |
| Male | 377 | (48.40) | 163 | (45.50) | 214 | (50.80) | ||
| Ethnicityc, N (%) | ||||||||
| Hispanic or Latino | 521 | (68.30) | 271 | (77.40) | 250 | (60.50) | .00 | |
| Racec, N (%) | ||||||||
| American Native | 27 | (3.50) | 10 | (2.80) | 17 | (4.0) | .00 | |
| Asian | 31 | (4.0) | 7 | (2.0) | 24 | (5.70) | ||
| Black | 77 | (9.90) | 30 | (8.40) | 47 | (11.20) | ||
| White | 110 | (14.10) | 31 | (8.70) | 79 | (18.80) | ||
| Hispanic | 526 | (67.50) | 275 | (76.80) | 251 | (59.60) | ||
| Otherd | 8 | (1.0) | 5 | (1.40) | 3 | (.70) | ||
| BMI, mean (SD)b | 24.43 | (5.92) | 24.93 | (6.18) | 24.01 | (5.65) | .03 | |
| CDC BMI Categoriesc, N (%) | ||||||||
| Underweight | 14 | (1.80) | 1 | (.30) | 13 | (3.10) | .02 | |
| Healthy Weight | 433 | (55.60) | 196 | (54.70) | 237 | (56.30) | ||
| Overweight | 148 | (19.0) | 72 | (20.10) | 76 | (18.10) | ||
| Obese | 182 | (23.40) | 88 | (24.60) | 94 | (22.30) | ||
| Unreported | 2 | (.30) | 1 | (.30) | 1 | (.20) | ||
| Beck Youth Depression Inventory mean (SD) | ||||||||
| Depression | 46.55 | (9.57) | 46.55 | (10.20) | 46.55 | (9.02) | .99 | |
Abbreviations: BMI, body mass index; CDC, Centers for Disease Control and Prevention
unadjusted means
t-test
Chi-square
Other includes: Middle Eastern, Mexican/Irish/Cherokee/Caucasian, Erithrean, Mixed, Somali, Pakistani, and unreported
Interventions
The COPE/Healthy Lifestyles TEEN (Thinking, Emotions, Exercise and Nutrition) program is a manualized 15-session educational and cognitive-behavioral skills building program. Table 2 shows the major content in each COPE session. COPE is guided by Cognitive Theory (CT) with 20 minutes of physical activity (eg, dancing, walking, and kick boxing movements) as a component of each session. COPE teaches the adolescents that how they think is directly related to how they feel, and how to turn negative beliefs triggered by activating events into positive beliefs so that they feel emotionally better and engage in healthy behaviors. The COPE intervention was developed originally by the first author and pilot tested 3 times with white, Hispanic and African-American adolescents as a group intervention in high school settings. COPE also uses pedometers as cue recognition for increasing physical activity throughout the program and instructs students to increase their step counts by 10% each week regardless of baseline steps. The teens are instructed to keep track of their steps on a daily tracking sheet so that weekly averages can be monitored to determine if the teens met their weekly physical activity goal.
Table 2.
The COPE/Healthy Lifestyles Teen Program Content
| Session # | Session Content | Key Content in the COPE Intervention |
|---|---|---|
| 1 | Introduction of the COPE Healthy Lifestyles TEEN program and goals. | |
| 2 | Healthy Lifestyles and the Thinking, Feeling, Behaving triangle. | Cognitive-behavioral skills building (CBSB) |
| 3 | Self-esteem. Positive thinking/self-talk. | CBSB |
| 4 | Goal setting. Problem solving. | CBSB |
| 5 | Stress and Coping. | CBSB |
| 6 | Emotional and behavioral regulation. | CBSB |
| 7 | Effective communication. Personality and communication styles. | CBSB |
| 8 | Barriers to goal progression and overcoming barriers. Energy balance. Ways to increase physical activity and associated benefits. | CBSB and Physical Activity Information |
| 9 | Heart rate. Stretching. | Physical Activity information |
| 10 | Food groups and a healthy body. Stoplight diet: red, yellow & green. | Nutrition information |
| 11 | Nutrients to build a healthy body. Reading labels. Effects of media and advertising on food choices. | Nutrition information |
| 12 | Portion sizes. “super size.” Influence of feelings on eating. | Nutrition information |
| 13 | Social eating. Strategies for eating during parties, holidays, and vacations. | Nutrition information |
| 14 | Snacks. Eating out. | Nutrition information |
| 15 | Integration of knowledge and skills to develop a healthy lifestyle plan; Putting it all together | CBSB |
Teachers were provided with a full-day training workshop on COPE, which introduced Cognitive Theory, the framework used to create and develop the COPE content and program. During the training workshop, the teachers engaged in cognitive-behavioral skills building practice exercises with the facilitators. Teachers then integrated the manualized COPE sessions into their health course, once a week for 15 weeks. Teens received a COPE manual that contained the content of the program along with the homework/cognitive-behavioral skills building activities to help them put into practice the content that they were learning in class.
The Healthy Teens program is a 15-week attention control program to control for the time the health teachers in the COPE group spent delivering the experimental program to their students. Healthy Teens teachers also received a full-day training workshop on the Healthy Teens program content. The content was manualized and concentrated on common health issues for adolescents, including dental care, skin care, infectious diseases, and immunizations. The complete list of all session titles has been published.16 The control teens also received a manual with homework assignments each week that focused on the topics being covered in class. The control program was formatted similar to the COPE intervention and included the same number of sessions with no overlap of content.
Parent newsletters describing the content of the COPE program or the Healthy Teens program were sent home to the parents with the teens 4 times during each 15-week program. The teens were asked to review each newsletter with their parents as part of their health course homework assignments.
Assessment of Intervention Fidelity
Intervention fidelity was assessed by having observers rate approximately 25% of the teachers’ intervention sessions using a fidelity observation instrument that was developed for use in the study. An inter-rater reliability of 90% for the fidelity observations between raters was established.
Outcomes Assessment
The primary outcomes for this 12-month follow-up evaluation were BMI and depressive symptoms. Heights and weights were obtained to calculate the teens’ BMI. Height was measured with a stadiometer and weight was measured with a Tanita™ scale. The depression subscale of the Beck Youth Inventory II© (BYI-II), a widely used and valid and reliable instrument, was used to assess the teens’ self-reported depressive symptoms over time.17 Examples of item on the inventory include: “I think that my life is bad;” and “I have trouble doing things, and I feel lonely.” The scale score is calculated as the sum of the 20 items and standardized to a T score with a mean of 50 and a standard deviation of 10. The higher the youth’s T score, the higher the depressive symptomology the youth is experiencing. For example, the average norm for the sub-scale is <55; 55–59 indicates mildly elevated depressive symptomology; 60–69 is moderately elevated; and 70+ is extremely elevated. Teens’ responses on the depression subscale were immediately evaluated for suicidal risk at each data collection time point to provide immediate referral as necessary. Reliabilities for the BYI-II in this study ranged from .93 to .94.
Statistical Analysis
A power analysis for the outcomes was conducted to determine sample size for this study, based on published research and pilot data. Baseline measures that were significantly different between the 2 groups were entered as covariates in the analyses. Specifically, there were more Hispanic teens and a higher BMI in the COPE group. COPE teens also had lower acculturation and watched more hours of television on a school day. To allow for follow-up attrition, the sample size was increased by 25%. A marginal model approach to repeated measures ANCOVA was conducted to evaluate the study’s outcomes. Baseline values of the dependent variable were used as a covariate in the analysis. In addition, there were significant baseline differences between the groups on race/ethnicity (greater percentage of Hispanic teens in COPE), acculturation (COPE teens had lower assimilation and greater integration and separation), and hours of television watched on a school day (COPE teens watched more television). Thus, the analyses also controlled for these variables. The marginal model was run using a mixed model to incorporate random effects and to adjust the standard errors for the clustering or correlation among observations due to students nested within classes. Tests of overall main effects and the group x time interaction were followed by planned contrasts among cell means, testing (1) group differences at 12 months and (2) group differences in the degree of change from baseline to 12 months and from 6 months to 12 months. To investigate the effects of the continuous moderators (age, income, and public assistance) on the intervention over time, 3-way interactions were created. For significant interactions, contrasts were used to aid in the interpretation using Cohen and Cohen’s suggestion that the mean and one standard deviation above and one standard deviation below the mean of the moderator be used.27 Analyses were performed using all available data (ie, intent to treat), including participants who subsequently dropped out of the study. Statistical analyses were conducted using SAS Proc Mixed for continuous outcomes and Proc Genmod, (ie, GEE models), was used for outcomes with limited dispersion, such as the proportion overweight (SAS Institute, Inc., Cary, North Carolina, Version 9.2). Effect sizes for treatment differences and differences over time were computed using the formula for Cohen’s d.
RESULTS
Approximately 50% of eligible teens participated in the study (Figure 1). Recruitment from the various high schools ranged from 20.88% to 66.47%. Recruitment for Cohorts 1 through 3 was 44.85%, 44.78%, and 62.17% respectively.
Twelve-month Effects on Overweight and Obesity
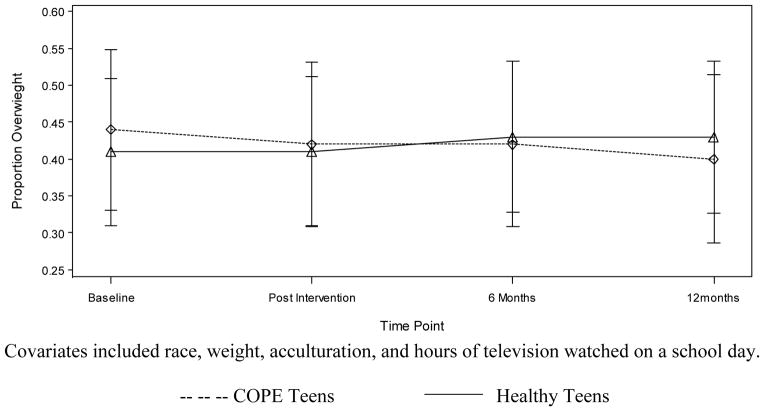
There was a significant decrease in the proportion of overweight and obese COPE teens from baseline to 12 months (χ2 = 5.40, p = .02) as compared to youth participating in Healthy Teens (Figure 2). COPE participants decreased from .4408 to .4043 whereas Healthy Teens participants increased from .4101 to .4318, adjusting for the covariates (Figure 2). The COPE teens had significantly lower BMI values at 12 months (F1, 698 = 11.22, p = .001, ES = 3.35) than the Healthy Teens (COPE adj M=24.95, SE = .115 vs. Healthy Teens adj M=25.48, SE = .105). Furthermore, only 4.8% (N = 7) of the COPE teens who were in the healthy weight category at baseline progressed to the overweight category at 12 months and none moved to being obese. On the other hand, 8.6% (N = 17) of the Healthy Teens youth progressed to the overweight category and 2% (N = 4) moved to the obese category during the same time frame. There also was a significant difference in the rate of change between in BMI values from immediately post-intervention to 12 months (F1, 698 = 5.50, p = .02, ES = 2.34) with the Healthy Teens group having a greater BMI increase (COPE post adj M=24.57, SE = .056 to COPE 12 month adj M=24.95, SE =.115 vs. Healthy Teens post adj M=24.78, SE = .051 to Healthy Teens 12 month adj M = 25.48, SE = .105).
Figure 2. Proportion of Overweight Adolescents at 12 Months Post-intervention.
Covariates included race, weight, acculturation, and hours of television watched on a school day.
-- -- -- COPE Teens ——— Healthy Teens
Age was a significant moderator of the impact of the intervention on BMI. COPE teens aged 14 had a smaller increase in BMI from 6 months to 12 months (F1, 404 = 4.60, p = .03, ES = 2.14) than the 14 year-old members of the Healthy Teens group (COPE 6 months adj M=25.18, SE=.156 to COPE 12 month adj M=25.29, SE=.203 vs. Healthy Teens 6 months adj M=25.26, SE=.154 to Healthy Teens 12 month adj M=25.83, SE=.199). In addition, COPE participants aged 15 years had significantly lower BMI values at 12 months (F1, 404 = 8.99, p = .003, ES=2.99) than participants in Healthy Teens aged 15 years (COPE adj M=24.94, SE=.239 vs. Healthy Teens adj M=25.85, SE=.187). Age again was a significant moderator, with COPE teens aged 14 years having a lower body mass percentile at 12 months (F1, 404 = 4.84, p = .03, ES=2.199) (COPE adj M=69.62, SE=1.046 vs. Healthy Teens adj M=72.84, SE=1.027), a greater decrease from 6 months to 12 months (F1, 404 = 6.36, p = .01, ES=2.522) (COPE 6 months adj M=73.85, SE=.875 to COPE 12 month adj M=69.62, SE=1.046 vs. Healthy Teens 6 months adj M=72.19, SE=.866 to Healthy Teens 12 month adj M=78.84, SE=1.027) and a greater decrease from post to 12 months (F1, 404 = 6.87, p = .01, ES=2.621) than Healthy Teens (COPE post adj M=73.09, SE=.875 to COPE 12 month adj M=69.62, SE=1.046 vs. Healthy Teens post adj M=72.65, SE=.584 to Healthy Teens 12 month adj M=78.84, SE=1.027).
Income also was a significant moderator, with high-income COPE participants having lower BMI values at 12 months (F1, 388 = 6.33, p = .01, ES=2.52) than high-income healthy teens (COPE adj M=24.92, SE=.187 vs. Healthy Teens adj M=25.43, SE=.206). The change in body mass percentile from immediately post-intervention to 12 months approached statistical significance (F1, 698 = 3.53, p = .06, ES=1.88) with a greater decrease for the COPE teens than for the Healthy Teens (COPE post adj M=71.28, SE=.377 to COPE 12 month adj M=63.73, SE=.617 vs. Healthy Teens post adj M=71.22, SE=.345 to Healthy Teens 12 month adj M=70.12, SE=.565). Being on public assistance also was a significant moderator with COPE teens on public assistance having a greater decline in body mass percentile from post to 12 months (F1, 407= 4.62, p = .03, ES=2.15) than Healthy Teens on public assistance (COPE post adj M=74.68, SE=2.878 to COPE 12 month adj M=71.02, SE=2.975 vs. Healthy Teens post adj M=66.62, SE=3.008 to Healthy Teens 12 month adj M=66.15, SE=3.114).
Twelve-month Effects on Depressive Symptoms
Although the COPE group as a whole had significantly higher T scores on the Beck Depression Inventory at 12 months (F1, 690 = 5.60, p = .001, ES=2.37) than the Healthy Teen group (adj M=47.52, SE=.417 versus adj M=46.18, SE=.381 respectively), the one point difference was not clinically meaningful with both groups having depressive scores in the normal range.
However, for teens who began the study with extremely elevated depression scores, COPE teens had significantly lower depressive symptom scores that fell into the normal range at 12 months compared to the Healthy Teens group whose depression scores remained in the depressed range (COPE =42.39; Healthy Teens M=57.90). (F1, 12 = 5.78, p = .03) (Table 3). In addition, when assessing moderators, those participants who came from high-income families showed a significant difference between the COPE and Healthy Teen groups where depressive symptoms for the Healthy Teens increased from 6 months to 12 months and COPE teens remained stable (F1, 381 = 4.09, p = .04, ES=2.122) (COPE 6 months adj M=46.18, SE=.912 to COPE 12 month adj M=46.38 SE=.878 versus Healthy Teens post adj M=45.94, SE=.630 to Healthy Teens 12 month adj M=46.61, SE=.626).
Table 3.
Sub-Group Analysis of Teens with Severe Depression at Baseline
| COPE | Healthy Teen | ||||||
|---|---|---|---|---|---|---|---|
| Time Point | N | Estimated Meana | Standard Error | N | Estimated Meana | Standard Error | p-value |
| Baseline | 12 | 12 | |||||
| Post-Intervention | 10 | 44.43 | 5.53 | 11 | 66.23 | 5.12 | .02 |
| 6-Month Follow-up | 8 | 48.98 | 5.30 | 11 | 62.87 | 4.89 | .10 |
| 12-Month Follow-up | 9 | 42.39 | 3.94 | 9 | 57.90 | 3.77 | .03 |
Adjusted for baseline differences
At the 12-month follow-up evaluation, 69.6% (N = 197) of teens found information from the program helpful. Specific comments included: “Instead of getting angry and taking it out on other people, I know how to deal with it in a healthy way,” “I always look at the nutrition facts so I found the healthy eating part most helpful,” “It helped me make life choices like exercise and eat healthy; also it helped me set goals for myself but goals that I know I can accomplish,” “It helped me talk about my problems,” and “Stress is a huge part of every teen’s life and the sections on stress and goal setting helped me organize my life.” Forty-eight percent (N = 135) of the teens indicated they changed a behavior as a result of the COPE program with changes such as “I continued to be positive about life and to stop saying ‘I can’t’ to everything,” “I do more exercise than I did before I started the cope program,” “I’ve been doing better at school; I brought up all my F’s to B’s & C’s,” “I’ve stayed positive about myself and everyone else; I say a positive thing to my family and myself,” “Instead of stressing, I talk to my parents and it makes me feel better,” and “Not arguing with my parents.”
When the teens were asked about family changes as a result of the program, 22.6% (N = 64) indicated their families had made changes. Examples include “They learned from me as I learned from COPE and they’re interested about healthy food choices,” “They have replaced fats and sugar with fruits and vegetables,” “They cook baked meals instead of fried,” “They have spent more time with us,” “We all go exercising at 6 pm every day,” and “They also lost weight.”
DISCUSSION
The hypothesis that COPE teens would have a lower BMI than the Healthy Teens at the 12-month post-intervention follow-up was supported. Further, there were fewer COPE teens (4.8%) who moved into the overweight category and none who became obese during the 12-month study versus the group of Healthy Teens in which over 10% of the students moved from a healthy weight category to being overweight or obese. Thus, the positive effects found for COPE on BMI at 6-months following the intervention were sustained for 12 months following the intervention. One of the explanations for the significant and clinically meaningful difference in BMI between the 2 groups at the 12-month follow-up assessment is that COPE students were averaging over 4000 more self-reported pedometer steps per day than Healthy Teens at the end of the intervention phase of the study.26 Feedback from teens at the 12-month follow-up assessment time point indicated that many of them continued to be physically active, citing activities such as taking walks with their parents and exercising more. Additionally, although diet inventories were not kept, student evaluations included numerous comments indicating that the teens and their families had adopted healthier eating habits. In addition, because prior research has indicated that adolescent healthy lifestyle beliefs are related to their behaviors,28 the intensive cognitive-behavioral skills building component of this intervention may have been key in sustaining lifestyle behavior changes such as increased physical activity and better nutritional eating patterns, which was content that was emphasized in the COPE intervention.
Although total group mean depression scores for the COPE group were not lower than the Healthy Teens group and both groups’ symptoms were in the normal range, COPE students who began the study with severely elevated depressive symptoms had significantly lower depressive scores that fell into the normal range than the Healthy Teens students at 12 months post-intervention, versus those in the attention control group whose symptoms remained elevated. This is an important finding given that the majority of adolescents with depression do not receive any treatment.29,30 The COPE intervention is based on Cognitive Theory, 31–34 and includes all 12 key concepts used in cognitive-behavior therapy, the gold standard evidence-based treatment for a variety of mental health disorders, including depression.35–38 In the COPE intervention, the thinking, feeling, behaving triangle is a major area of emphasis and is integrated throughout the entire program. The teens are taught that how they think directly relates to how they feel and how they behave, and they are provided with many case-based examples in which they also are instructed in and conduct practice sessions on how to engage in positive thinking using the “ABCs” (A=Activator event, B=Belief, C=Consequences of the belief). On the open-ended program evaluation by COPE students, hundreds of comments specifically indicated that the COPE program helped them in dealing effectively with stress and anger as well as feeling better about themselves.
Prior studies using just the first 7 cognitive-behavioral skills building sessions from the 15-session COPE Healthy Lifestyles TEEN program with depressed and anxious adolescents in individual, group and classroom format have resulted in substantial declines in depression, anxiety, anger, and disruptive behavior as well as improvements in self-esteem.39,40 The 12-month depression finding in this study also replicates our prior research in which marked decreases in depression and anxiety were found in high school and college students with baseline elevated depressive symptoms when the COPE healthy lifestyles program was delivered within classroom settings.41,42
Findings from this study support that COPE had a positive impact on physical activity, BMI, psychosocial outcomes, and grade performance in high school adolescents. To our knowledge, this is the first study to show improvements over time in multiple outcomes with a teacher-delivered cognitive-behavioral skills building intervention integrated into high school health education curriculum. Whereas other studies have found short-term positive effects on health knowledge and BMI with multi-component interventions that typically include nutrition education, physical activity and behavior modification,13 our study indicates that multiple immediate, 6- and 12-month outcomes can be positively impacted by teaching adolescents cognitive-behavioral skills, which include cognitive reappraisal, emotional and behavioral regulation, stress and coping, and learning how to set goals and problem solve barriers to living a healthy lifestyle.
Some limitations existed in this study, which included self-reported data by the teens on depression and only approximately 50% of the eligible teens participated. Further, even though random assignment was used to allocate schools to treatment group, the 2 groups of students were different on some variables at baseline. However, those variables were controlled as covariates in the analyses. Teens also were not assessed on any mental health treatment being received outside of the study. Another limitation was that study team fidelity observations of intervention implementation by the teachers revealed decreases in fidelity at least once in approximately half of the classrooms, which may have diminished the potency of the COPE program. With full intervention fidelity by the teachers in the COPE group, the positive effects for the COPE program may have been even larger. Therefore, future studies with the COPE intervention should provide monitoring of fidelity as well as ongoing strategies to support implementation fidelity and quality.43 In addition, given that only the COPE teens received 20 minutes of physical activity in their intervention sessions, it is unclear which of the intervention components were largely accountable for the positive outcomes.
Conclusions
Findings from this study indicated that a manualized cognitive-behavioral skills building healthy lifestyle program delivered by teachers in high school classrooms can have a multitude of positive short and more long-term outcomes, including improvement of BMI and prevention of overweight/obesity in addition to decreasing depression in teens who report severe depressive symptomatology. The routine integration of COPE into high school health courses has great potential to improve physical health, mental health and academic outcomes in high-risk adolescents.
IMPLICATIONS FOR SCHOOL HEALTH
Teachers were used to deliver the COPE Program in this study because it is more feasible and cost-effective to have the intervention integrated into required health courses rather than plan for school districts to hire additional personnel to deliver the program. Thus, the COPE intervention is easily scalable and can be offered in high schools across the nation. At a time when many schools are under budget constraints and are eliminating physical education teachers, COPE offers an approach to enhancing healthy lifestyle behaviors and reducing overweight/obesity in teens, including 20 minutes of physical activity that can be implemented in classrooms, which any high school teacher can incorporate into their school day. In addition, because COPE also includes evidence-based cognitive-behavioral skills building in a format that can be delivered by teachers, social skills and depressive symptoms can be improved in those teens at highest risk for poor academic performance. Furthermore, research supports that teachers may be better at sustaining longer-term positive outcomes because they can reinforce content in their classrooms and throughout the course curriculum.42
Human Subjects Approval Statement
This project was reviewed and approved by Arizona State University’s (IRB Protocol Number 1001004756) and The Ohio State University’s (IRB Protocol Number 2011B0356) Institutional Review Board (IRB). An independent data and safety monitoring board monitored the research.
Acknowledgments
This study was funded by the National Institutes of Health/National Institute of Nursing Research 1R01NR012171.
Contributor Information
Bernadette Mazurek Melnyk, Email: melnyk.15@osu.edu, Dean and Professor, College of Nursing, Professor of Pediatrics and Psychiatry, College of Medicine, The Ohio State University, 1585 Neil Avenue, Columbus, OH 43210, Phone: (614) 292-4844, Fax: (614) 292-4535.
Diana Jacobson, Email: Diana.Jacobson@asu.edu, Assistant Professor, Arizona State University College of Nursing & Health Innovation, 500 North 3rd Street, Phoenix, AZ 85004.
Stephanie A. Kelly, Email: kelly.901@osu.edu, Assistant Professor, The Ohio State University, 1585 Neil Avenue, Columbus, OH 43210.
Michael J. Belyea, Email: Michael.Belyea@asu.edu, Research Professor, Arizona State University College of Nursing & Health Innovation, 500 North 3rd Street, Phoenix, AZ 85004.
Gabriel Q. Shaibi, Email: Gabriel.Shaibi@asu.edu, Associate Professor and Southwest Borderlands Scholar, Arizona State University College of Nursing & Health Innovation, 500 North 3rd Street, Phoenix, AZ 85004.
Leigh Small, Email: lsmall2@vcu.edu, Department Chair and Associate Professor, Family and Community Health Nursing, Virginia Commonwealth University School of Nursing, P.O. Box 980567, Richmond, VA 23298-0567.
Judith A. O’Haver, Email: johaver@phoenixchildrens.com, Phoenix Children’s Medical Group - Dermatology, 1919 E Thomas Rd, Phoenix, AZ 85016-7710.
Flavio Francisco Marsiglia, Email: marsiglia@asu.edu, Distinguished Foundation Professor of Cultural Diversity and Health, School of Social Work Director of the Southwest Interdisciplinary Research Center (SIRC), School of Social Work - College of Public Programs, Arizona State University, 411 N. Central Ave., Suite 720, Phoenix, AZ 85004.
References
- 1.Centers for Disease Control and Prevention. Youth risk behavior surveillance- United States, 2005. MMWR Surveill Summ. 2006;55(SS-5):1–107. [PubMed] [Google Scholar]
- 2.Evans D, Seligman M. Introduction. In: Evans DL, Foa EB, Gur R, Hendin H, O’Brien CP, Seligman ME, et al., editors. Treating and Preventing Adolescent Mental Health Disorders: What We Know and What We Don’t Know. New York, NY: Oxford University Press; 2005. pp. xxv–xl. [Google Scholar]
- 3.Falkner NH, Neumark-Sztainer D, Story M, Jeffery RW, Beuhring T, Resnick MD. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9(1):32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 4.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance – United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109(4):704–712. doi: 10.1542/peds.109.4.704. [DOI] [PubMed] [Google Scholar]
- 6.Freedman D, Dietz W, Srinivasan S, Berenson G. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–1185. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 7.Stabouli S, Kotsis V, Papamichael C, Constantopoulos A, Zakopoulos N. Adolescent obesity is associated with high ambulatory blood pressure and increased carotid intimal-medial thickness. J Pediatr. 2005;147(5):651–656. doi: 10.1016/j.jpeds.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med. 2003;157(12):1206–1211. doi: 10.1001/archpedi.157.12.1206. [DOI] [PubMed] [Google Scholar]
- 9.Goodman E, Whitaker R. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;109(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 10.Sjöberg RL, Nilsson KW, Leppert J. Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics. 2005;116(3):e389–392. doi: 10.1542/peds.2005-0170. [DOI] [PubMed] [Google Scholar]
- 11.Stein RE, Zitner LE, Jensen PS. Interventions for adolescent depression in primary care. Pediatrics. 2006;118(2):669–682. doi: 10.1542/peds.2005-2086. [DOI] [PubMed] [Google Scholar]
- 12.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 13.Bell S, Morgan S. Children’s attitudes and behavioral intentions toward a peer presented as obese. Does a medical explanation for the obesity make a difference? J Pediatr Psychol. 2002;25:137–145. doi: 10.1093/jpepsy/25.3.137. [DOI] [PubMed] [Google Scholar]
- 14.Finkelstein EA, Brown DS, Wrage LA, Allaire BT, Hoerger TJ. Individual and aggregate years of life lost associated with overweight and obesity. Obesity. 2010;18(2):333–339. doi: 10.1038/oby.2009.253. [DOI] [PubMed] [Google Scholar]
- 15.Melnyk BM, Moldenhauer Z, editors. The KySS Guide to Child and Adolescent Mental Health Screening, Early Intervention and Health Promotion. Cherry Hill, NJ: National Association of Pediatric Nurse Practitioners; 2006. [Google Scholar]
- 16.Melnyk BM, Kelly S, Jacobson D, Belyea M, Shaibi M, Small L, et al. The COPE health lifestyles TEEN randomized controlled trial with culturally diverse high school adolescents: baseline characteristics and methods. Contemp Clin Trials. 2013;36:41–53. doi: 10.1016/j.cct.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beck JS, Beck AT, Jolly JB, Steer RA. Beck Youth Inventories for Children and Adolescents: Manual. 2. San Antonio, TX: Harcourt Assessment; 2005. [Google Scholar]
- 18.Bernal P, Estroff DB, Aboudarham JF, Murphy M, Keller A, Jellinek MS. Psychosocial morbidity: the economic burden in a pediatric health maintenance organization sample. Arch Pediatr Adolesc Med. 2000;154(3):261–266. doi: 10.1001/archpedi.154.3.261. [DOI] [PubMed] [Google Scholar]
- 19.Melnyk BM, Brown HE, Jones DC, Kreipe R, Novak J. Improving the mental/psychosocial health of US children and adolescents: outcomes and implementation strategies from the national KySS Summit. J Pediatr Health Care. 2003;17(6 Suppl):S1–S24. doi: 10.1016/j.pedhc.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Wells KB, Kataoka SH, Asarnow JR. Affective disorders in children and adolescents: addressing unmet need in primary care settings. Biol Psychiatry. 2001;49(12):1111–1120. doi: 10.1016/s0006-3223(01)01113-1. [DOI] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 22.Isasi CR, Whiffen A, Campbell E, Florez Y, Freeman K, Wylie-Rosett J. High prevalence of obesity among inner-city adolescent boys in the Bronx, New York: forgetting our boys. Prev Chronic Dis. 2011;8(1):A23. [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr. 2011;2:23–31. doi: 10.3945/an.110.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flegal KM, Ogden CL, Carroll MD. Prevalence and trends in overweight in Mexican-American adults and children. Nutr Rev. 2004;62(7 Pt 2):S144–S148. doi: 10.1111/j.1753-4887.2004.tb00085.x. [DOI] [PubMed] [Google Scholar]
- 25.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity. 2008;16(5):1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 26.Melnyk BM, Jacobson D, Kelly S, Belyea M, Shaibi G, Small L, et al. Promoting healthy lifestyles in high school adolescents: a randomized controlled trial. Am J Prev Med. 2013;45(4):407–415. doi: 10.1016/j.amepre.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen J, Cohen P. Applied Multiple Regression/Correlation for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- 28.Melnyk BM, Kelly S, Jacobson D, Arcoleo K, Shaibi G. Improving physical activity, mental health outcomes, and academic retention of college students with Freshman 5 to Thrive: COPE/Healthy Lifestyles. J AM Acad Nurse Prac. 2014;26(6):314–322. doi: 10.1002/2327-6924.12037. [DOI] [PubMed] [Google Scholar]
- 29.US Department of Health and Human Services. Mental Health: A Report of the Surgeon General. US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; Rockville, MD: 1999. [Google Scholar]
- 30.Kataoka SH, Zhang L, Wells K. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 31.Ellis A. Reason and Emotion in Psychotherapy. New York, NY: Lyle Stuart; 1962. [Google Scholar]
- 32.Seligman MEP. Helplessness: On Depression, Development and Death. San Francisco, CA: Freeman; 1975. [Google Scholar]
- 33.Skinner BF. Science and Human Behavior. NewYork, NY: Macmillan; 1953. [Google Scholar]
- 34.Lewinsohn PM. Manual of instructions for the behavioral ratings used for the observation of interpersonal behavior. In: Mash EJ, Terdal LG, editors. Behavior Therapy Assessment. Springer Publishing Company; New York, NY: 1974. pp. 335–345. [Google Scholar]
- 35.American Academy of Pediatrics. Evidence-based child and adolescent psychosocial interventions. Pediatrics. 2010;125(3 Suppl):S128. doi: 10.1542/peds.2010-0788H. [DOI] [Google Scholar]
- 36.Weersing VR, Iyengar S, Kolko DJ, Birmaher B, Brent DA. Effectiveness of cognitive-behavioral therapy for adolescent depression: a benchmarking investigation. Behav Ther. 2006;37(1):36–48. doi: 10.1016/j.beth.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for adolescent depression: a meta-analytic investigation of changes in effect size estimates. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1403–1413. doi: 10.1097/chi.0b013e3180592aaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beck AT, Dozois DJ. Cognitive therapy: current status and future directions. Annu Rev Med. 2011;62(1):397–409. doi: 10.1146/annurev-med-052209-100032. [DOI] [PubMed] [Google Scholar]
- 39.Lusk P, Melnyk BM. The brief cognitive-behavioral COPE intervention for depressed adolescents: outcomes and feasibility of delivery in 30-minute outpatient visits. J Am Psychiatr Nurses Assoc. 2011;17(3):226–236. doi: 10.1177/1078390311404067. [DOI] [PubMed] [Google Scholar]
- 40.Melnyk BM, Kelly S, Lusk P. Outcomes and feasibility of a manualized cognitive-behavioral skills building intervention: group COPE for depressed and anxious adolescents in school. J Child Adolesc Psychiatr Nurs. 2014;27(1):3–13. doi: 10.1111/jcap.12058. [DOI] [PubMed] [Google Scholar]
- 41.Melnyk BM, Jacobson D, Kelly S, O’Haver J, Small L, Mays M. Improving mental health, healthy lifestyle choices and physical health of Hispanic adolescents with the school based COPE/Healthy Lifestyles TEEN program: a randomized controlled pilot study. J Sch Health. 2009;79(12):575–584. doi: 10.1111/j.1746-1561.2009.00451.x. [DOI] [PubMed] [Google Scholar]
- 42.Melnyk BM, Small L, Morrison-Beedy D, Strasser A, Spath L, Kreipe R, et al. Mental health correlates of healthy lifestyle attitudes, choices, & behaviors in overweight teens. J Pediatr Health Care. 2006;20(6):401–406. doi: 10.1016/j.pedhc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Kelly SA, Oswalt K, Melnyk BM, Jacobson D. Comparison of intervention fidelity between COPE TEEN and an attention-control program in a randomized controlled trial. Health Educ Res. 2015;30(2):233–247. doi: 10.1093/her/cyu065. [DOI] [PMC free article] [PubMed] [Google Scholar]