Abstract
Objectives
To determine associations of unmet need for child or family health services with (1) adverse family financial and employment impacts and (2) child behavioral functioning problems among US children with autism spectrum disorder (ASD), developmental delay (DD), and/or intellectual disability (ID).
Method
This was a secondary analysis of parent-reported data from the 2009–10 National Survey of Children with Special Healthcare Needs linked to the 2011 Survey of Pathways to Diagnosis and Services. The study sample (n = 3,518) represented an estimated 1,803,112 US children aged 6–17 years with current ASD, DD, and/or ID (developmental disabilities). Dependent variables included adverse family financial and employment impacts, as well as child behavioral functioning problems. The independent variables of interest were unmet need for (1) child health services and (2) family health services. Multivariable logistic regression models were fit to examine associations.
Results
Unmet need for child and family health services, adverse family financial and employment impacts, and child behavioral functioning problems were prevalent among US children with developmental disabilities. Unmet needs were associated with an increased likelihood of adverse family employment and financial impacts. Unmet needs were associated with an increased likelihood of child behavioral functioning problems the following year; however, this association was not statistically significant.
Conclusion
Unmet needs are associated with adverse impacts for children with developmental disabilities and their families. Increased access to and coordination of needed health services following ASD, DD, and/or ID diagnosis may improve subsequent outcomes for children with developmental disabilities and their families.
INTRODUCTION
Children with developmental disabilities such as autism spectrum disorder (ASD), developmental delay (DD), and intellectual disability (ID) are likely to experience high need for health services, given the chronic and complex nature of their conditions.1–3 With 1 in 6 US children estimated to have a developmental disability4 and an increase in prevalence over recent years, these needs have significant consequences for the US health system. That is, as the prevalence of children with developmental disabilities increases more children will be encouraged and referred to use health services3,5 including medical and dental care, specialty care, prescription medications, mental healthcare, therapy services (e.g., physical, occupational, speech and language therapy), as well as communication aids or devices. Respite care, mental healthcare, and genetic counseling may also be sought by the child’s family to cope with and manage their child’s symptoms. Utilization of certain health services, particularly evidence-based treatments, may lead to better health outcomes for children with developmental disabilities.6,7
Although children with developmental disabilities may use more child and family health services than other children with special health care needs (CSHCN), they have a greater likelihood of experiencing unmet need for health services than other CSHCN.1,2,5,8–10 Unmet health service needs include myriad situations in which children and their families are unable to access needed health services for the child (e.g., prescription medication, therapy services) or the family (e.g., respite care, family mental healthcare). Unmet need for health services warrants attention for CSHCN—particularly children with developmental disabilities—in general and specialty care pediatric settings, as well as other service delivery settings (e.g., schools, public health agencies), because unmet need has been suggested to lead to poor adult health and functional status outcomes,11 which CSHCN with developmental disabilities are already prone to experience.12 Increased knowledge of which unmet health service needs are most prevalent among children with developmental disabilities may help health system administrators more effectively allocate resources toward reducing unmet need while helping clinicians and other service providers to more quickly identify and ameliorate unmet needs families of children with developmental disabilities are likely to experience. Previous research suggests children with developmental disabilities are most likely to experience unmet need for communication aids or devices, mental healthcare, home healthcare, and therapy services.2,9 Further research is needed to determine which family health services children with developmental disabilities are most likely to need and lack.
Unmet health service needs, which may be assuaged in pediatric care settings with patient-centered medical home models,13,14 can have immediate consequences for children and their families. One consequence of unmet health service needs may be adverse family employment and financial impacts. It is known that children with developmental disabilities experience more family financial and employment impacts (e.g., having a family member who needs to cut-back or stop working due to the child’s health condition, having a family that experiences financial problems due to the child’s health condition) than other CSHCN.8,10 The mechanism relating unmet needs to financial and employment impacts may perhaps be best illustrated through an example: envision a parent whose child has been diagnosed with ID and ASD who needs but is unable to access respite care. This parent may need to spend more time providing and coordinating care for her child, which would involve cutting back work hours. In turn, a reduction in work hours would result in lower household income, further straining family finances. Unmet health service needs can, thus, create detrimental family financial and employment impacts or worsen a family’s existing financial situation.
CSHCN with ASD are at particular risk for adverse family impacts: rates of adverse family impact are higher in CSHCN with ASD than among CSHCN with other developmental disabilities (e.g., developmental delay, attention-deficit/hyperactivity disorder [ADHD]); CSHCN with functional limitations; and CSHCN with emotional, developmental, or behavioral problems.15–17 High rates of unmet need among children with developmental disabilities may reflect the complex problems they experience.3,18 For instance, Kuo and colleagues8 found 56.8% of more complex CSHCN (i.e., children with three or more special healthcare needs, who used medical equipment, and who saw two or more subspecialists in the past year) had families that experienced financial problems and 48.8% had at least one unmet medical service need. Findings from another study suggest that increasing out-of-pocket medical expenditures are associated with a greater likelihood of unmet health service needs among children with and without special healthcare needs.18 Yet, associations between unmet needs and adverse family financial and employment impacts have not been examined among CSHCN with developmental disabilities more specifically.
Beyond adverse family impacts, unmet child and family health service needs may lead to poorer functional outcomes among children with developmental disabilities. That is, children with developmental disabilities are more likely than children without developmental disabilities to experience greater functional impacts such as limited ability to crawl, walk, run, or play,1,3 and their optimal functioning may be further impaired by unmet need for health services (e.g., inability to access early intensive behavioral intervention services may lead to greater impairment in communication for children with ASD). Severe condition symptoms, comorbidity, and related functional impairment may, conversely, result in elevated unmet need among children with developmental disabilities (e.g., children with severe ADHD symptoms may experience difficulty accessing needed combined medication and behavioral intervention services resulting in poorer functioning over time). Past research using cross-sectional data has shown unmet need for child health services is associated with increased child functional impairment among CSHCN13 generally. Unmet mental healthcare needs for CSHCN—particularly those with emotional, developmental, or behavioral problems—and their family members have also been correlated with greater child functional impact. To better understand the temporal complexity of the relationship between functional impact and unmet health service needs for children with developmental disabilities, it is important to determine if unmet need for health services has an effect on child functioning.
Unmet need for child and family health services, adverse family financial and employment impacts, and child behavioral functioning problems have been individually demonstrated among US children with developmental disabilities,2,9 particularly among those with ASD.8,10,16,18 Yet, relationships among unmet needs, adverse family impact, and child behavioral functioning have not been previously explored. Understanding these relationships is important to improving healthcare quality and reducing healthcare disparities for the especially vulnerable and growing population of children with developmental disabilities.
Therefore, this study sought to determine (1) if unmet need for child or family health services was significantly associated with adverse family employment and financial impacts experienced during the same year and (2) if unmet need for child or family services were significantly associated with child behavioral functioning problems the following year among a nationally representative sample of school-aged children with ASD, DD, and/or ID (hereinafter referred to as children with developmental disabilities). Drawing on past research,1,3,10,13,15,17–21 we hypothesized unmet need for child or family health services would be positively associated with adverse family financial and employment impacts experienced in the same year and also with child behavioral functioning problems the following year among US children with developmental disabilities.
METHODS
Study Design and Data Source
This study was a secondary analysis of parent-reported data from the 2009–10 National Survey of Children with Special Healthcare Needs (NS-CSHCN) linked to the 2011 Survey of Pathways to Diagnosis and Services (Pathways). Pathways was a follow-up survey of CSHCN, identified by the CSHCN Screener,22 who were aged 6–17 years and diagnosed with ASD, DD, or ID by a doctor or other healthcare provider in the NS-CSHCN according to a parent or other caregiver (parent). After informed consent was obtained, the same parent reported all data on the child for each survey. The 2009–10 NS-CSHCN had a 25.5% response rate.23 Pathways had a weighted completion rate of 62%.24 Pathways was only administered in English. Detailed survey methodology has been previously documented.23,24
Study Sample
The study sample included 3,518 US children aged 6–17 years with special health care needs and current ASD, DD, and/or ID in 2011. Given the study’s focus on children with developmental disabilities, 514 children were excluded because the parent indicated the child did not have current ASD, DD, or ID.
Measures
Adverse family financial and employment impacts
In line with past research examining adverse family financial and employment impacts among children with developmental disabilities using the NS-CSHCN,10,17 five binary (yes/no) items from the NS-CSHCN were used to measure adverse family financial and employment impacts. These included if: (1) the family paid >$1000 in out-of-pocket medical expenses annually, (2) the family experienced financial problems due to the child’s health condition, (3) a family member cut-back and/or stopped working due to the child’s health condition, (4) a family member avoided changing jobs due to concerns about maintaining the child’s health insurance, and (5) a family member spent ≥11 hours weekly coordinating or providing the child’s care.
Child behavioral functioning problems
Child behavioral functioning problems were assessed by the brief Strengths and Difficulties Questionnaire (SDQ), a previously validated screening tool to identify emotional and behavioral problems in US children.25,26 Although children with certain developmental disabilities (e.g., ADHD) may be at greater risk of behavioral problems related to their condition’s symptoms, the SDQ captures behavioral functioning more broadly beyond the scope of a child’s developmental disability. Child behavioral functioning problems were defined based on parent agreement with the following five statements about the child’s behavior in the past six months, each rated on a three-point Likert scale (not true, somewhat true, certainly true): “Is [child] generally well behaved, does what adults request?; [Child] has many worries or often seems worried?; [Child] is often unhappy, depressed, or tearful?; [Child] gets along better with adults than with other children/youth?; and [Child] has good attention span, sees chores or homework through to the end?”. According to a prior validation study of the brief SDQ and related research, a summed score of ≥6 was used to determine child behavioral functioning problems.26,27 The brief SDQ was only included in Pathways.
Unmet need for health services
Two binary (yes/no) measures from the NS-CSHCN were used to assess unmet need for child and family health services during the past 12-months. Unmet need for child health services was determined if the child had ≥1 unmet need for 14 specific health services including preventive medical care, specialty care, preventive dental care, other dental care, prescription medication, therapy services (i.e., physical, occupational, or speech and language therapy), mental health services, substance use, home healthcare, vision care, hearing care, mobility care, communication services, and durable medical equipment. Unmet need for family health services was determined if the family had ≥1 unmet need for three support services including respite care, mental healthcare, and genetic counseling.
Predisposing, enabling, and need factors
Covariates were identified from previous research on unmet health service needs, adverse family financial and employment impacts, and child functional status among CSHCN.5,9,10 According to the Behavioral Model of Health Services Utilization,28 covariates were categorized as predisposing characteristics, enabling resources, or healthcare need factors. Predisposing factors included: child age (years), sex, and race/ethnicity. Enabling resources included child health insurance type, household income relative to federal poverty level (FPL), highest parent education level, census region, and family structure. Healthcare need factors were developmental disability type, functional limitations status as assessed by the CSHCN Screener item “Is your child limited or prevented in any way in [his/her] ability to do the things most children of the same age can do?”,22 and condition comorbidity based on 20 chronic conditions asked about (e.g., allergies, asthma, anxiety, depression). Developmental disability type categories were defined according to the frequency with which parents reported their child currently had ASD, DD, and/or ID when Pathways was administered. Specifically, 1441 children had DD only, 1420 had ASD with or without DD and/or ID, and 657 had ID with or without DD (only 46 children were reported to have ID without DD). Child age and developmental disability type were from Pathways, and all other covariates were from the NS-CSHCN.
Statistical Analyses
Descriptive statistics, including weighted univariate and bivariate proportions with 95% confidence intervals, were computed for all measures. Chi-square tests were used to determine differences in the distribution of unmet need for child or family health services by predisposing, enabling, and need factors in the study sample. Chi-square tests were used to assess differences in the relative frequency of adverse family financial and employment impacts and child behavioral functioning problems by functional limitations status. Functional limitations status was used in these analyses as an indicator of impairment severity beyond what would typically be experienced by children with the given developmental conditions in 2009–10.
Logistic regression, including multivariable models controlling for predisposing, enabling, and need factors, was used to determine associations of unmet need for child or family health services with adverse family employment and financial impact and child behavioral functional problems. In multivariable analyses examining associations between unmet need for health services and behavioral functional problems the subsequent year, an additional composite measure was used to control for baseline behavioral problems in 2009–10. This measure was constructed based on past research20,27 using four items from the NS-CSHCN about whether children experienced a lot of difficulty with (1) learning, understanding, or paying attention; (2) speaking, communicating, or being understood; (3) feeling anxious or depressed; or (4) behavior problems, such as acting-out, fighting, bullying, or arguing. We also tested if functional limitations status significantly modified associations of unmet need for health services with adverse family financial and employment impacts as well as child behavioral functioning problems in the multivariable regression models, using a conventional alpha level of .05. Mean model variance inflation factors computed were <2 suggesting multicollinearity did not substantially affect model estimates. All analyses were weighted to account for the survey sampling design and were performed in Stata 14.1 (College Station, Texas).
RESULTS
Study Population
The study sample represented an estimated 1,803,112 US children (69.8% male) aged 6–17 years with ASD (36.2%), DD (46.5%), and/or ID (17.3%). Most children with developmental disabilities identified as white non-Hispanic (62.2%), had private health insurance (53.9%), had a parent with more than a high school education (67.8%), and had two biological or adoptive parents (52.2%) (Table 1). Many children with developmental disabilities experienced functional limitations (56.0%) and had three or more comorbid chronic conditions (47.9%).
Table 1.
Predisposing, Enabling, and Need Factors by Unmet Need for Child or Family Health Services Among US Children with Developmental Disabilities Aged 6–17 Years (n = 3,518)
| Overall | Any unmet child health service need | No unmet child health services need | Any unmet family health services need | No unmet family health services need | P-value any vs. no unmet child health services need | P-value any vs. no unmet family health services need | |
|---|---|---|---|---|---|---|---|
| Estimated number (% of sample) |
1,803,112 (100%) |
627,997 (35.5%) |
1,141,652 (64.5%) |
333,385 (18.5%) |
1,466,100 (81.5%) |
– | – |
| Predisposing factors | |||||||
| Age, y | .61 | .07 | |||||
| 6–8 (n = 632) | 19.0% | 17.1% | 20.3% | 12.4% | 20.5% | ||
| 9–11 (n = 1,089) | 30.6% | 33.4% | 30.7% | 33.5% | 31.0% | ||
| 12–14 (n = 992) | 27.6% | 25.2% | 26.2% | 25.1% | 26.5% | ||
| 15–17 (n = 805) | 23.4% | 24.3% | 22.8% | 29.0% | 22.1% | ||
| Sex | .58 | .39 | |||||
| Male (n = 2,436) | 69.8% | 70.9% | 69.2% | 72.5% | 69.1% | ||
| Female (n = 1,079) | 30.2% | 29.1% | 30.8% | 30.2% | 30.9% | ||
| Race/ethnicity | .76 | .75 | |||||
| Hispanic (n = 311) | 13.2% | 13.3% | 13.1% | 14.3% | 12.9% | ||
| White, non-Hispanic (n = 2,513) | 62.2% | 60.3% | 63.0% | 61.6% | 62.4% | ||
| Black, non-Hispanic (n = 305) | 15.7% | 17.8% | 14.8% | 13.1% | 16.3% | ||
| Other race, non-Hispanic (n = 358) | 8.9% | 8.6% | 9.1% | 11.0% | 8.5% | ||
| Enabling resources | |||||||
| Household income | .0009 | .46 | |||||
| 0%–99% FPL (n = 635) | 25.8% | 29.1% | 23.8% | 24.6% | 26.2% | ||
| 100%-199% FPL (n = 727) | 21.5% | 21.3% | 21.5% | 22.5% | 21.3% | ||
| 200%-399% FPL (n = 1,127) | 28.7% | 33.0% | 26.5% | 33.0% | 27.8% | ||
| ≥400% FPL (n = 1,029) | 23.9% | 16.6% | 28.3% | 19.9% | 24.8% | ||
| Health insurance type | .003 | .22 | |||||
| Any private (n = 2,139) | 53.9% | 46.9% | 57.9% | 49.0% | 54.9% | ||
| Public only or uninsured (n = 1,268) | 46.2% | 53.1% | 42.1% | 51.0% | 45.1% | ||
| Census region | .12 | .018 | |||||
| Northeast (n = 657) | 19.8% | 18.4% | 20.7% | 20.6% | 19.6% | ||
| Midwest (n = 810) | 24.8% | 24.2% | 25.5% | 19.4% | 26.0% | ||
| South (n = 1,037) | 34.5% | 31.7% | 35.3% | 29.7% | 35.6% | ||
| West (n = 1,014) | 21.0% | 25.6% | 18.5% | 30.3% | 18.8% | ||
| Highest parental education level | .28 | .007 | |||||
| ≤High school (n = 699) | 32.2% | 29.6% | 33.6% | 21.2% | 34.8% | ||
| >High school (n = 2,819) | 67.8% | 70.5% | 66.4% | 78.8% | 65.2% | ||
| Family structure | .13 | .88 | |||||
| 2 parent biological or adopted (n = 2,152) | 52.2% | 49.8% | 54.0% | 53.0% | 52.0% | ||
| Single mother (n = 677) | 27.7% | 31.6% | 25.0% | 28.4% | 27.7% | ||
| Other (n = 668) | 20.0% | 18.6% | 21.0% | 18.6% | 20.4% | ||
| Healthcare need factors | |||||||
| Developmental disability type | .61 | < .001 | |||||
| DD (n = 1,441) | 46.5% | 44.7% | 48.1% | 28.0% | 50.8% | ||
| ASD (n = 1,420) | 36.2% | 36.7% | 35.4% | 26.5% | 34.0% | ||
| ID (n = 657) | 17.3% | 18.6% | 16.5% | 45.6% | 15.2% | ||
| Functional limitations status | < .001 | < .001 | |||||
| No (n = 1,524) | 44.0% | 31.8% | 51.0% | 21.7% | 49.1% | ||
| Yes (n = 1,994) | 56.0% | 68.2% | 49.0% | 78.3% | 50.9% | ||
| Comorbid chronic conditions | < .001 | < .001 | |||||
| ≥3 comorbid conditions (n = 1,615) | 47.9% | 59.4% | 41.1% | 76.3% | 41.4% | ||
| 2 comorbid conditions (n = 783) | 21.0% | 16.3% | 23.8% | 13.6% | 22.8% | ||
| 1 comorbid condition (n = 684) | 19.6% | 17.2% | 21.1% | 7.9% | 22.3% | ||
| No comorbid conditions (n = 436) | 11.5% | 7.2% | 14.1% | 2.2% | 13.6% | ||
Note. Not all proportions sum to 100% due to rounding.
Abbreviations: ASD, autism spectrum disorder; DD, developmental delay; FPL, federal poverty level; ID, intellectual disability.
Source: 2011 Survey of Pathways to Diagnosis and Services linked to the 2009–10 National Survey of Children with Special Health Care Needs.
Prevalence of Unmet Need for Health Services
Among children with developmental disabilities, 35.5% had any unmet child health service need and 18.5% had any unmet family health service need (Table 1). Therapy services and mental health services were the two most frequently reported unmet child health service needs among children with developmental disabilities: 12.4% (95% CI: 10.6–14.5%) had unmet therapy needs and 9.4% (95% CI: 7.8–11.4%) had unmet mental health service needs. Respite care and family mental healthcare were most common unmet family health service needs: 11.5 % (95% CI: 9.3–14.1%) had unmet respite care needs and 7.4% (95% CI: 5.8–9.5%) had unmet family mental healthcare needs. Low household income, having public health insurance only or being uninsured, having functional limitations, and having ≥3 comorbid conditions were positively associated with having any unmet child health service need among children with developmental disabilities. Living in the Western US, having a parent with more than a high school education, having ID, experiencing functional limitations, and having ≥3 comorbid conditions were positively associated with having any unmet family health service need among children with developmental disabilities (Table 1).
Prevalence of Adverse Family Financial and Employment Impacts and Child Behavioral Functioning Problems
The majority (71.4%) of children with developmental disabilities experienced one or more of five adverse family financial and employment impacts and 47.6% experienced two or more. Nearly half (45.0%) of children with developmental disabilities had a family member who cut-back or stopped working due to the child’s condition, and more than one-third (36.0%) had families that experienced financial problems due to the child’s condition (Figure 1). Among children with developmental disabilities, those with functional limitations were significantly more likely than those without functional limitations to have had their family spend 11 or more hours per week providing/coordinating the child’s care, cut-back or stop working due to the child’s health condition, and experience financial problems due to the child’s condition. Approximately one-quarter (24.5%) of children with developmental disabilities had behavioral functioning problems the following year, which did not vary significantly by functional limitations status.
Figure 1. Weighted Proportion and 95% Confidence Interval of US Children with Developmental Disabilities aged 6–17 years with Each Adverse Family Financial and Employment Impact and Child Behavioral Functioning Problems, by Functional Limitations Status.
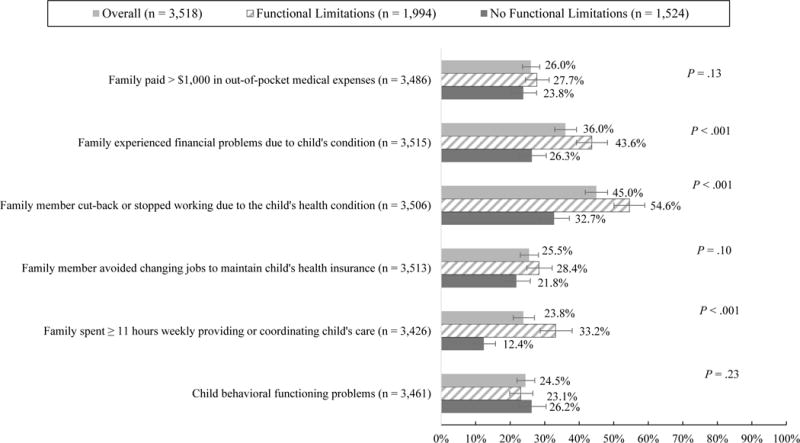
This figure shows the weighted proportion of US children with developmental disabilities aged 6–17 years overall and by functional limitations status that experienced each adverse family financial and employment impact as well as child behavioral functional problems. 95% confidence intervals for each weighted proportion and P-values from weighted chi-square tests comparing the distribution of each variable by functional limitations status are also displayed.
Note: P-values were computed from weighted chi-square tests that compared children with functional limitations to children without functional limitations among the sample of children with developmental disabilities on the variables of interest.
Source: 2011 Survey of Pathways to Diagnosis and Services linked to the 2009–10 National Survey of Children with Special Health Care Needs
Associations of Unmet Need for Health Services with Adverse Family Financial and Employment Impacts
Results from unadjusted and adjusted analyses revealed unmet need for child or family health services were significantly associated with an increased likelihood of adverse family financial and employment impacts among children with developmental disabilities (Tables 2 & 3). The magnitude of these associations was consistently greater between any unmet need for family health services (versus any unmet need for child health services) and the adverse family financial and employment impacts. Functional limitations status did not significantly modify any associations of unmet need for health services with the family financial and employment impacts examined, according to multivariable regression model results (results available upon request).
Table 2.
Unadjusted Associations of Adverse Family Financial and Employment Impacts and Child Behavioral Functioning Problems with Unmet Need for Child or Family Health Services Among US Children with Developmental Disabilities: Weighted Proportions (95% CIs) and Odds Ratios (95% CIs)
| Family paid >$1,000 in annual out-of-pocket medical expenses (n = 1,280) |
Family experienced financial problems due to the child’s health condition (n = 1,382) |
Family member cut-back or stopped working due to the child’s health condition (n = 1,749) |
Family member avoided changing jobs to maintain the child’s health insurance (n = 1,045) |
Child’s family spent ≥11 hours per week providing/coordinating care for the child (n = 824) |
Child behavioral functioning problems (n = 1,019) |
|
|---|---|---|---|---|---|---|
| % Any unmet need for child health services (n = 2,665) |
30.1% (25.7% – 34.9%) |
53.4% (47.5% – 59.1%) |
56.5% (50.7% – 62.2%) |
30.7% (26.0% – 35.8%) |
33.7% (27.7% – 40.2%) |
25.8% (21.6% – 30.6%) |
| % No unmet need for child health services (n = 1,287) |
23.3% (20.4% – 26.4%) |
26.0% (22.9% – 29.4%) |
38.7% (35.0% – 42.4%) |
22.5% (19.5% – 25.8%) |
18.2% (15.4% – 21.5%) |
23.6% (20.6% – 27.0%) |
| aP-value | .0125 | < .001 | < .001 | .0045 | < .001 | .43 |
| OR Any unmet need for child health services |
1.42 (1.08 – 1.87) |
3.25 (2.43 – 4.34) |
2.06 (1.56 – 2.73) |
1.53 (1.40 – 2.04) |
2.28 (1.61 – 3.21) |
1.13 (0.84 – 1.51) |
| OR No unmet need for child health services | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
|
| ||||||
| % Any unmet need for family health services (n = 675) | 36.4% (29.4% – 44.0%) |
69.6% (62.4% – 75.9%) |
70.4% (62.7% – 77.0%) |
36.5% (29.4% – 44.2%) |
46.1% (37.4% – 55.2%) |
28.9% (22.5% – 36.1%) |
| % No unmet need for family health services (n = 3,342) | 23.6% (21.1% – 26.4%) |
28.3% (25.5% – 31.4%) |
39.3% (36.0% – 42.6%) |
23.0% (20.3% – 25.9%) |
18.6% (15.9% – 21.6%) |
23.5% (20.8% – 26.3%) |
| bP-value | .0005 | < .001 | < .001 | .0003 | < .001 | .13 |
| OR Any unmet need for family health services |
1.85 (1.30 – 2.62) |
5.79 (4.06 – 8.25) |
3.67 (2.53 – 5.33) |
1.93 (1.35 – 2.76) |
3.75 (2.49 – 5.63) |
1.32 (0.92 – 1.91) |
| OR No unmet need for family health services | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Abbreviations: CIs, confidence intervals; OR, odds ratio.
Weighted χ2 tests were conducted to determine significant differences in adverse family impacts and child behavioral functioning problems, by any unmet need for child health services.
Weighted χ2 tests were conducted to determine significant differences in adverse family impacts and child behavioral functioning problems, by any unmet need for family health services.
Source: 2011 Survey of Pathways to Diagnosis and Services linked to the 2009–10 National Survey of Children with Special Health Care Needs
Table 3.
Adjusted Associationsa of Adverse Family Financial and Employment Impacts and Child Behavioral Functioning Problems with Unmet Need for Child or Family Health Services Among US Children with Developmental Disabilities
| Family paid >$1,000 in annual out-of-pocket medical expenses | Family experienced financial problems due to the child’s health condition | Family member cut-back or stopped working due to the child’s health condition | Family member avoided changing jobs to maintain the child’s health insurance | Child’s family spent ≥11 hours per week providing/coordinating care for the child | Child behavioral functioning problemsb | |
|---|---|---|---|---|---|---|
| aOR (95% CI): Any unmet need for child health services (n = 1,287) |
1.81 (1.35 – 2.41) |
2.98 (2.25 – 3.96) |
1.83 (1.37 – 2.43) |
1.64 (1.22 – 2.21) |
1.75 (1.27 – 2.41) |
1.19 (0.88 – 1.61) |
| aOR (95% CI): No unmet need for child health services (n = 2,665) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| aP-value | < .001 | < .001 | < .001 | .001 | .001 | .26 |
|
| ||||||
| aOR (95% CI): Any unmet need for family health services (n = 675) |
2.02 (1.40 – 2.91) |
4.81 (3.36 – 6.88) |
2.91 (1.99 – 4.26) |
1.90 (1.34 – 2.69) |
2.69 (1.82 – 3.96) |
1.37 (0.97 – 1.94) |
| aOR (95% CI): No unmet need for family health services (n = 3,342) |
1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| bP-value | < .001 | < .001 | < .001 | < .001 | < .001 | .08 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
Odds ratios were adjusted for child age, sex, race/ethnicity, household income level, health insurance type, region of residence, highest parent education level, family structure, developmental disability type, functional limitations status, and condition comorbidity.
Models were additionally adjusted for whether or not children experienced serious overall difficulty in terms of having a lot of difficulty with any of the following: (1) learning, understanding, or paying attention; (2) speaking, communicating, or being understood; (3) feeling anxious or depressed; or (4) behavior problems, such as acting-out, fighting, bullying, or arguing.
Source: 2011 Survey of Pathways to Diagnosis and Services linked to the 2009–10 National Survey of Children with Special Health Care Needs
Among adverse family impacts, unmet need for child or family health services were both most strongly associated with the family experiencing financial problems due to the child’s health condition. Children with developmental disabilities with any unmet child health services need had 2.98 the adjusted odds (95% CI: 2.25–3.96) of having a family that experienced financial problems due to the child’s condition compared to those with no unmet child health service needs (53.4% versus 26.0%). Similarly, children with developmental disabilities with any unmet family health services need were more likely than those without unmet family health services need to have had a family that experienced financial problems due to the child’s health condition (69.6% versus 28.3%; adjusted odds ratio [aOR]: 4.81, 95% CI: 3.36–6.88).
Associations of Unmet Need for Health Services with Child Behavioral Functioning Problems
Children with developmental disabilities with any unmet need for child health services or family health services were more likely to have behavioral functioning problems compared to those without any unmet need for child health services (25.8% versus 23.6%) or family health services (28.9% versus 23.5%); however, the magnitude of these differences was relatively small. Results from unadjusted and adjusted analyses further indicated unmet needs were not significantly associated with behavioral functioning problems the subsequent year among children with developmental disabilities (Tables 2 & 3). Functional limitations status did not significantly modify associations of unmet need for health services with child behavioral functioning problems, according to multivariable regression model results (results available upon request).
DISCUSSION
This study aimed to determine if unmet need for child or family health services was significantly associated with adverse family employment and financial impacts the same year, and if unmet need for child or family services was significantly associated with child behavioral functioning problems the following year among a nationally representative sample of school-aged children with developmental disabilities. We found many children with developmental disabilities continue to experience unmet need for child and family health services, adverse family financial and employment impacts, and behavioral functioning problems. Unmet need for child and family health services were associated with a higher likelihood of adverse family financial and employment impacts in the same year. Associations of unmet need for child and family health services with child behavioral problems the following year were positive but not statistically significant. Together, these findings indicate unmet health services needs are associated with a wide variety of adverse impacts beyond the medical realm for US children with developmental disabilities and their families.
Estimates of any unmet need for child health services and any unmet need for family health services were somewhat higher than in past research on children with any learning or behavioral developmental disability3 or any neurologic condition.2 This may be due in part to methodological differences across studies regarding how unmet need for health services was measured and how study samples were defined. Previous research on the prevalence of unmet need for child and family health services specifically among children with ASD15 using 2005–06 NS-CSHCN data are, however, more consistent with this study’s findings. Findings from this study and past research suggest unmet need for child health services continue to affect a greater proportion of US children with developmental disabilities than unmet need for family health services.
One reason for this discrepancy may be that families of children with developmental disabilities are less likely to recognize their need for family-oriented health services than they are to recognize their child’s need for health services. As suggested by this study’s findings, recognition of unmet need for family health services among children with developmental disabilities may be facilitated by higher parent education level, region of residence (i.e., living in the West versus the Northeast), and the child’s special healthcare needs being more complex. Along with reducing unmet need for subgroups that may be more aware of their need for family health services, concurrent intervention may be needed to increase awareness of family health services and their potential benefits along with clear access lines to these services among subgroups that have previously been less affected by unmet need for family health services. Specifically, interventions aimed at (1) increasing awareness regarding the negative implications of unmet health service needs among families and health service providers and (2) enhancing communication between them about health service needs may benefit the health of children with developmental disabilities across the life course. Such interventions would require a component better enabling service providers to connect families with community resources addressing their children’s health service needs (e.g., following up with families once referrals are made, using a family navigator). In communities with less resources for children with developmental disabilities, interventions could take the form of capacity-building to teach existing providers to recognize and handle the service needs of CSHCN (e.g., speech and language therapy, respite care), or such interventions could employ approaches like telemedicine connecting families with expert providers elsewhere.
This study’s findings are fairly consistent with findings from past research on CSHCN with neurologic disorders2 and ASD9 indicating that unmet need for mental healthcare and therapy services may be greatest among US children with developmental disabilities. Findings from two prior studies additionally suggest the largest proportion of US CSHCN experience unmet need for respite care rather than other family health services.8,29 This study’s findings reinforce that unmet need for respite care relative to unmet need for family mental healthcare or genetic counseling may affect the largest number of CSHCN including those with developmental disabilities.
A combination of child, family, and health-system level factors may influence unmet need for these specific child and family health services among US children with developmental disabilities. High service costs and low local service availability, as well as health plan (i.e., insurance) problems have been shown to be common reasons for unmet mental healthcare and therapy needs among US CSHCN,14 including those with ASD.9 High service costs and low local service availability have also been frequently reported reasons for unmet respite care need among US CSHCN.9 Consequently, improved funding, availability, and reimbursement mechanisms for these specific types of child and family health services may help reduce unmet need among children with developmental disabilities and their families.
Ease of access to needed community-based services (i.e., difficulties and/or frustration in accessing needed services such as medical care and special education services due to barriers like finances or transportation), not unmet need for child and family health services per se, has been shown to be associated with a reduced likelihood of adverse family financial and employment impacts among CSHCN with ASD.17 This study extends past research by demonstrating that unmet child health services need and unmet family health services need are each associated with an increased likelihood of adverse family financial and employment impacts among children with developmental disabilities more broadly, and also that unmet need for family versus child health services is more strongly associated with the likelihood of these impacts among children with developmental disabilities. Certain adverse family financial and employment impacts including the child’s family experiencing financial problems, needing to cut-back or stop working due to the child’s health condition, and spending 11 or more hours per week coordinating or providing care for the child had the strongest associations with unmet need for child and family health services among children with developmental disabilities in this study. These findings suggest that lacking needed family health services may be more strongly correlated with financial problems and needing to spend more time providing care for the child rather than out-of-pocket medical expenses and concerns related to the child’s health insurance coverage. Further research—perhaps employing qualitative methods—is needed to disentangle the temporal nature of these relationships for children with developmental disabilities and their families.
Numerous past studies have found poorer child functioning to be positively correlated with unmet need for health services among US CSHCN8,13,14,18,19,29 and children with developmental disabilities.1–3,5,9,15 Yet, these studies have not examined the effects of unmet health services need on child health and functional status over time. Albeit a relatively short two-year time period, this study found there was not a statistically significant association between unmet need for child or family health services with child behavioral problems the following year. These associations may be due to other factors not assessed, such as sustained receipt of evidence-based treatments (e.g., applied behavioral analysis for CSHCN with ASD), parent wellbeing, or school environment, which may better explain variation in subsequent child behavioral problems than unmet need. The brief SDQ measure has been shown to be most valid and reliable when completed by multiple informants (versus one parent alone) and for older children (13–17 years); therefore, measurement error may have biased this study’s findings more toward the null hypothesis.26,27
This study has a number of limitations that should be considered in interpreting its findings. First, data on unmet need for health services as well as adverse family financial and employment impacts were cross-sectional, limiting the ability to draw causal inference regarding their associations. Specifically, it is unclear if children have more unmet need because services are too expensive or if unmet need itself causes adverse financial and employment impacts for their families. Factors such as limited service availability and barriers to accessing services may also contribute to unmet need. Additionally, there are a number of social and educational services (e.g., Temporary Assistance for Needy Families benefits, Supplemental Nutrition Assistance Program benefits) that may contribute to improved health outcomes for children with developmental disabilities but were not directly assessed in the surveys used. Consequently, our ability to draw completely inclusive inferences in terms of unmet need and associations with adverse family financial and employment impacts is limited. Because data used in this study were observational, temporal associations between unmet need and child behavioral functioning problems the subsequent year should also be interpreted cautiously. Other variables not included in the data set or unaccounted for in our analyses may alter these associations. The approximately two-year time period between when unmet need was assessed in 2009–10 and when child behavioral functioning was assessed in 2011 was also relatively short to determine temporal associations, particularly given the chronic nature of symptoms in children with developmental disabilities. For these reasons, future research using longitudinal data on children with developmental disabilities, specifically their unmet need for various health services, family impacts, and behavioral functioning, is needed to better determine the mechanism by which this child subpopulation may experience more optimal health outcomes.
Additionally, the study sample did not include children with all types of developmental disabilities, younger children (<6 years), and children of parents who could not complete the survey in English. Children with developmental disabilities are commonly diagnosed in early childhood, during which time their need for health services may be less apparent to parents, and children with other types of developmental disabilities have been shown to experience less unmet health services need than children with ASD or ID.3 Further, children whose parents have limited English proficiency may be more prone to experience delayed diagnosis and to not recognize their child’s health service needs.30 For these reasons, we expect that the inclusion of these groups may have altered study findings. It should be acknowledged that while the study’s measure of child behavioral functioning—the brief SDQ—has been validated26,27 to identify emotional and behavioral problems, it does not capture the broad complexity of behavioral functioning in children with developmental disabilities that could potentially be gathered through clinical observation. Last, all study measures parent-reported, thus, limiting the ability to determine how concordant parent perceptions of the constructs examined are with those of other parties who may be affected such as children and service providers.
Despite these limitations, this study is one of the first to demonstrate associations of unmet need for child and family health services with adverse family financial and employment impacts among a nationally representative sample of children with developmental disabilities. Findings from this study also suggest that unmet need for child or family health services may not be significantly associated with child behavioral functioning problems over a relatively short time-period for children with developmental disabilities. In all, these findings highlight the importance of recognizing need for both child and family health services among children with developmental disabilities and helping their families to overcome obstacles accessing these services. Unmet health service needs may be reduced among children with developmental disabilities as more medical systems move to adapt comprehensive care delivery models (e.g., the patient-centered medical home model) and simultaneous efforts are made to increase family and provider awareness about the negative implications of unmet needs while enhancing communication about these needs and the utilization of strategies to meet health service needs.13,14 Within the broader system of care for CSHCN, the education, public health, and child welfare systems must also employ models with components akin to those comprising the patient-centered medical home model such as family-centered care and care coordination to ensure that children with developmental disabilities and their families receive the array of health services needed to optimize their quality of life over time.
Acknowledgments
The authors thank Brianna Sinche, MPH, for her assistance with initial data analyses.
Funding Disclosure: The Medical Research Foundation of Oregon funded this project. Dr. Zuckerman’s effort was also funded by #1K23MH095828 from the National Institute of Mental Health. The funders had no involvement in the study design, data collection or analysis, results interpretation, in writing the manuscript, or in the decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Boulet SL, Boyle CA, Schieve LA. Health care use and health and functional impact of developmental disabilities among US children, 1997–2005. Arch Pediatr Adolesc Med. 2009;163(1):19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- 2.Bitsko RH, Visser SN, Schieve LA, Ross DS, Thurman DJ, Perou R. Unmet health care needs among CSHCN with neurologic conditions. Pediatrics. 2009;124(Suppl 4):S343–51. doi: 10.1542/peds.2009-1255D. [DOI] [PubMed] [Google Scholar]
- 3.Schieve LA, Gonzalez V, Boulet SL, et al. Concurrent medical conditions and health care use and needs among children with learning and behavioral developmental disabilities, national health interview survey, 2006–2010. Res Dev Disabil. 2012;33(2):467–476. doi: 10.1016/j.ridd.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 4.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127(6):1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- 5.Nageswaran S, Parish SL, Rose RA, Grady MD. Do children with developmental disabilities and mental health conditions have greater difficulty using health services than children with physical disorders? Matern Child Health J. 2011;15(5):634–641. doi: 10.1007/s10995-010-0597-4. [DOI] [PubMed] [Google Scholar]
- 6.Stein DS, Blum NJ, Barbaresi WJ. Developmental and behavioral disorders through the life span. Pediatrics. 2011;128(2):364–373. doi: 10.1542/peds.2011-0266. [DOI] [PubMed] [Google Scholar]
- 7.Weitlauf AS, McPheeters ML, Peters B, et al. Therapies for children with autism spectrum disorder: Behavioral interventions update. Vanderbilt Evidence-Based Practice Center. 2014 Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed]
- 8.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165(11):1020–1026. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012;16(5):1081–1091. doi: 10.1007/s10995-011-0833-6. [DOI] [PubMed] [Google Scholar]
- 10.Vohra R, Madhavan S, Sambamoorthi U, St Peter C. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. 2014;18(7):815–826. doi: 10.1177/1362361313512902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hargreaves DS, Elliott MN, Viner RM, Richmond TK, Schuster MA. Unmet health care need in US adolescents and adult health outcomes. Pediatrics. 2015;136(3):513–520. doi: 10.1542/peds.2015-0237. [DOI] [PubMed] [Google Scholar]
- 12.Quach J, Jansen PW, Mensah FK, Wake M. Trajectories and outcomes among children with special health care needs. Pediatrics. 2015;135(4):e842–50. doi: 10.1542/peds.2014-2431. [DOI] [PubMed] [Google Scholar]
- 13.Litt JS, McCormick MC. Care coordination, the family-centered medical home, and functional disability among children with special health care needs. Acad Pediatr. 2015;15(2):185–190. doi: 10.1016/j.acap.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Miller JE, Nugent CN, Gaboda D, Russell LB. Reasons for unmet need for child and family health services among children with special health care needs with and without medical homes. PLoS One. 2013;8(12):e82570. doi: 10.1371/journal.pone.0082570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the united states, 2005–2006. Pediatrics. 2008;122(6):e1149–58. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- 16.Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129(4):617–623. doi: 10.1542/peds.2011-2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zuckerman KE, Lindly OJ, Bethell CD, Kuhlthau K. Family impacts among children with autism spectrum disorder: The role of health care quality. Acad Pediatr. 2014;14(4):398–407. doi: 10.1016/j.acap.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karaca-Mandic P, Choi-Yoo SJ, Lee J, Scal P. Family out-of-pocket health care burden and children’s unmet needs or delayed health care. Acad Pediatr. 2014;14(1):101–108. doi: 10.1016/j.acap.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Inkelas M, Raghavan R, Larson K, Kuo AA, Ortega AN. Unmet mental health need and access to services for children with special health care needs and their families. Ambul Pediatr. 2007;7(6):431–438. doi: 10.1016/j.ambp.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 20.Simon AE, Pastor PN, Reuben CA, Huang LN, Goldstrom ID. Use of mental health services by children ages six to 11 with emotional or behavioral difficulties. Psychiatr Serv. 2015;66(9):930–937. doi: 10.1176/appi.ps.201400342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lindly OJ, Sinche BK, Zuckerman KE. Variation in educational services receipt among US children with developmental conditions. Acad Pediatr. 2015;15(5):534–543. doi: 10.1016/j.acap.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: Development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. Frequently asked questions: 2009–2010 national survey of children with special health care needs. 2011 Available at: http://www.cdc.gov/nchs/data/slaits/NSCSHCNfaqs2009.pdf.
- 24.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. Frequently asked questions: 2011 survey of pathways to diagnosis and services. 2013 Available at: http://www.cdc.gov/nchs/data/slaits/PathwaysFAQ.pdf.
- 25.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Gruber M, Sampson N. Validation studies of mental health interview survey. report presented to the center for disease control december 21, 2006. 2006 [Google Scholar]
- 27.Pastor PN, Reuben CA, Duran CR. Identifying emotional and behavioral problems in children aged 4–17 years: United states, 2001–2007. Natl Health Stat Report. 2012;(48):1–17. [PubMed] [Google Scholar]
- 28.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647–653. doi: 10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- 29.Nageswaran S. Respite care for children with special health care needs. Arch Pediatr Adolesc Med. 2009;163(1):49–54. doi: 10.1001/archpediatrics.2008.504. [DOI] [PubMed] [Google Scholar]
- 30.Magnusson D, Palta M, McManus B, Benedict RE, Durkin MS. Capturing unmet therapy need among young children with developmental delay using national survey data. Acad Pediatr. 2015 doi: 10.1016/j.acap.2015.05.003. [DOI] [PubMed] [Google Scholar]


