Abstract
The development of clinical agents remains a costly and time-consuming process. Although identification of new uses of existing drugs has been recognized as a more efficient approach for drug discovery than development of novel drugs, little screening of drugs that might be used for a rare malignant tumor such as osteosarcoma (OS) has been performed. In this study, we attempted to identify new molecular targeted agents for OS by employing Screening Committee of Anticancer Drugs (SCADS) kits. To screen compounds for OS treatment, their effect on cell viability of the OS cell lines 143B, MG63, HOS, SAOS-2, and HUO9 were evaluated. Candidate drugs were narrowed down based on a global anti-proliferative effect against these five OS cell lines. After excluding cytotoxic compounds and compounds unsuitable for in vivo administration, cucurbitacin I was extracted. Cucurbitacin I has been found to have cytotoxic and anti-proliferative properties against several tumors through inhibition of signal transducer and activator of transcription 3 (STAT3) activation. Cucurbitacin I dose- and time-dependently inhibited the proliferation of all five OS cell lines. Following cucurbitacin I treatment, STAT3 was inactivated and analysis of Mcl-1, cleaved PARP and caspase-3 indicated apoptosis induction. Expression of cell cycle regulator proteins, such as phospho-cyclin D1, c-Myc and survivin, were suppressed. Finally, cucurbitacin I potently inhibited the tumor growth of human OS 143B cells in nude mice. Our in vitro and in vivo results suggest that STAT3 inhibition by cucurbitacin I will be an effective and new approach for the treatment of OS.
Keywords: STAT3, cucurbitacin I, osteosarcoma
Introduction
Osteosarocoma (OS) is well established as the most common primary malignant bone tumor. OS is usually observed in children, adolescents and young adults. OS treatment requires a multidisciplinary strategy of surgery and chemotherapy including radiotherapy (1). The identification of effective chemotherapy for the treatment of OS has led to significant improvement in patient outcome; the 5-year survival rate for patients with a localized tumor has reached ~70% (2). However, the 5-year event-free survival of metastatic OS is only ~20% (3–8). The combination of chemotherapeutic agents, such as doxorubicin, cisplatin, methotrexate, and ifosfamide, is widely accepted to have efficacy against OS (9–13). However, these agents for OS have been used for over ten years now and there is a continued need for new therapeutic approaches for further improvement of OS patient prognosis. Recently, the use of molecular-targeted cancer therapy has been receiving attention for various tumors, because of several potential advantages in features such as drug metabolism and accumulation, optimum doses, and side effects, over conventional anticancer agents (14). Molecular-targeted therapy is currently favored as a replacement for conventional OS therapies.
The development of clinical agents remains a costly and time-consuming process. Identification of new uses for existing drugs has been recognized as being a more efficient approach for drug discovery than the development of novel drugs. The aim of this study was to identify existing compounds that are capable of killing OS cells. First, we screened the anti-proliferative effects of 324 anticancer drugs using five OS cell lines and selected candidate agents for new OS treatment. Second, we investigated the intracellular mechanism of the anti-proliferative activity of the candidate agent and examined its inhibitory effect on tumor growth using an in vivo model.
Materials and methods
Osteosarcoma cell culture
Five human OS cell lines (143B, HOS, MG63, SAOS-2, and HUO9) were used in this study. 143B, HOS, MG63 were cultured in minimum essential media (MEM) (Gibco, Carlsbad, CA, USA) containing 10% fetal bovine serum (FBS), 100 U/ml penicillin and 100 mg/ml streptomycin (Invitrogen, Carlsbad, CA, USA). SAOS-2 was cultured in McCoy's 5A (modified) medium (Gibco) containing 15% FBS, 100 U/ml penicillin and 100 mg/ml streptomycin. HUO9 was cultured in RPMI-1640 medium (Gibco) containing 10% FBS, 100 U/ml penicillin and 100 mg/ml streptomycin. Cells were maintained as attached monolayers and were incubated in a humidified atmosphere with 5% CO2 at 37°C.
Chemical compounds
The Screening Committee of Anticancer Drugs (SCADS) compound library, containing 324 compounds in four 96-well microplates (http://gantoku-shien.jfcr.or.jp/), was kindly provided by Grant-in-Aid for Scientific Research on the Priority Area ‘Cancer’ from the Ministry of Education, Culture, Sports, Science and Technology of Japan. The compounds, mainly composed of antitumor drugs and kinase inhibitors, were provided at a concentration of 10 mM in dimethyl sulfoxide (DMSO) solution.
Cucurbitacin I (Sigma-Aldrich, St. Louis, MO, USA) was initially dissolved in DMSO and stored at −20°C. For the experiments, cucurbitacin I was diluted with culture media to the final concentration used.
Measurement of cell viability
For measurement of cell proliferation, the five human OS cell lines were placed in monolayer culture at a density of 3.0×104 cells/well (100 μl) and were treated with either diluent control (DMSO) or 10 mM of each compound in 96-well plates. Cell viability was measured using the Cell-Titer 96® AQueous One Solution Cell Proliferation Assay kit (Promega, Madison, WI, USA). After compound screening, candidate compounds were examined for their anti-proliferative effect in a 2D monolayer culture (as above) and a 3D collagen gel culture (cellmatrix type 1A; Nitta Gelatin Inc., Japan). After 24 h of incubation, the compounds, dissolved in DMSO, were added to the culture at the indicated final concentrations. The cells were then cultured for 24 h. Cell viability in 2D monolayers was measured using cell proliferation assay kit as above. Cell viability in 3D collagen gels was measured using the Cell-Titer-Glo™ Luminescent Cell Viability assay (Promega). For dose-response tests, cells were exposed to media with various concentrations (10 nM, 100 nM, 1.0 μM and 10 μM) of cucurbitacin I or DMSO (negative control) for 24 h. For time-response tests, cells were exposed to media with 10 mM cucurbitacin I or DMSO for 12, 24 or 48 h.
Flow cytometry
Cell cycle progression and apoptosis were analysed by flow cytometry. For apoptosis analysis, cells were incubated with cucurbitacin I (10 μM) for 24 h followed by Annexin V-FITC and propidium isodide (PI) double staining performed according to the manufacturer's instructions (Beckman Coulter, Miami, FL, USA).
Western blot analysis
After treatment with or without cucurbitacin I (10 μM) for 12 or 24 h, cells were lysed with radioimmunoprecipitation (RIPA) buffer (Millipore-Upstate, Temecula, CA, USA) supplemented with a protease inhibitor cocktail, 0.5 mM PMSF, and 0.2 mM Na3VO4. Proteins were separated by SDS-PAGE, and samples were adjusted to the same protein concentration before loading. Proteins were transferred to a nitrocellulose membrane, and blotted. Antibodies were obtained from the following sources and used at the dilutions recommended by the manufacturer: STAT3 and phospho-STAT3 antibodies 1:2,000 dilution (Cell Signaling Technology Beverly, MA, USA) and cleaved caspase-3, phospho-cyclin D1, c-Myc, Mcl-1, survivin and cleaved PARP antibodies 1:1,000 dilution (Cell Signaling Technology). The β-actin protein was assayed as a loading control.
Enzyme linked immunosorbent assay (ELISA)
The effect of cucurbitacin I on apoptosis was evaluated by measurement of caspase-3 activation. OS cells were cultured with or without cucurbitacin I (10 μM) for 24 h. Caspase-3 levels were determined using the Caspase-3 (Active) Human ELISA kit (Invitrogen) according to the manufacturer's instructions.
Growth of 143B xenografts in athymic nude mice with in vivo cucurbitacin I treatment
All animal experiments strictly followed the guidelines of Cedars-Sinai Medical Center and the National Institute of Health (NIH). 143B (6.0×106) human OS cells were inoculated subcutaneously into the back of female nude mice. Forty mice were randomly assigned to each of the following experimental groups: i) saline with DMSO (diluent-specific control); ii) 0.25 mg/kg cucurbitacin I; iii) 0.5 mg/kg cucurbitacin I; iv) 1.0 mg/kg cucurbitacin I. Saline or cucurbitacin I was administered three times a week intraperitoneally. Body weight and tumor size were measured every week, and the tumor volume was calculated using the following formula: V = lw2/2, where (l) is the length, (w) the width, and (V) is the volume as described previously (15). The treatment was stopped at 28 days. The total observation period from the start of treatment of the xenografts was 60 days.
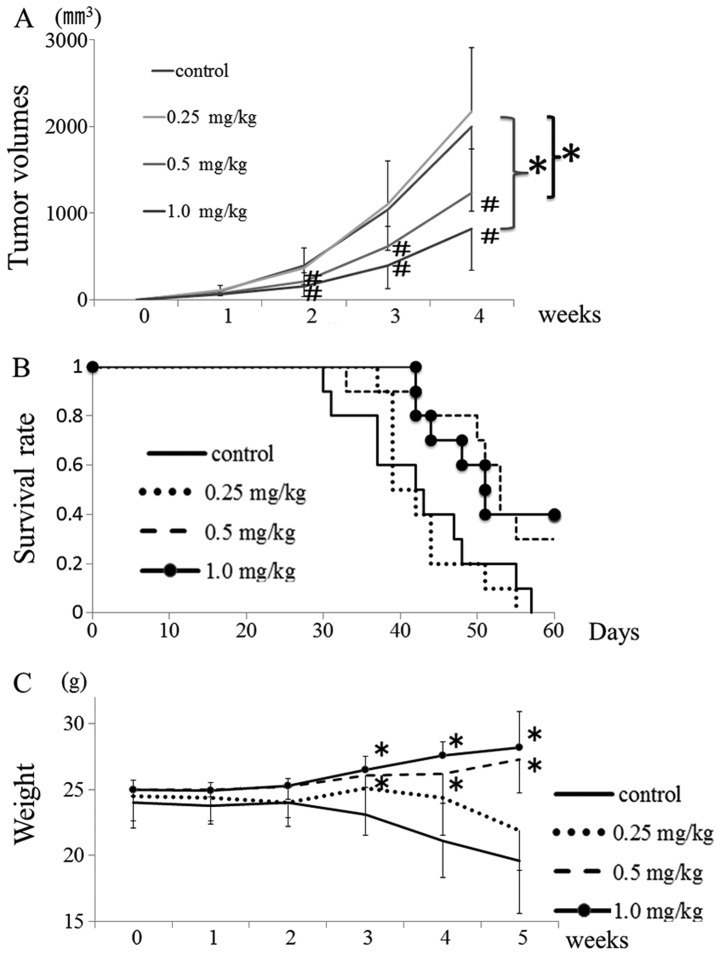
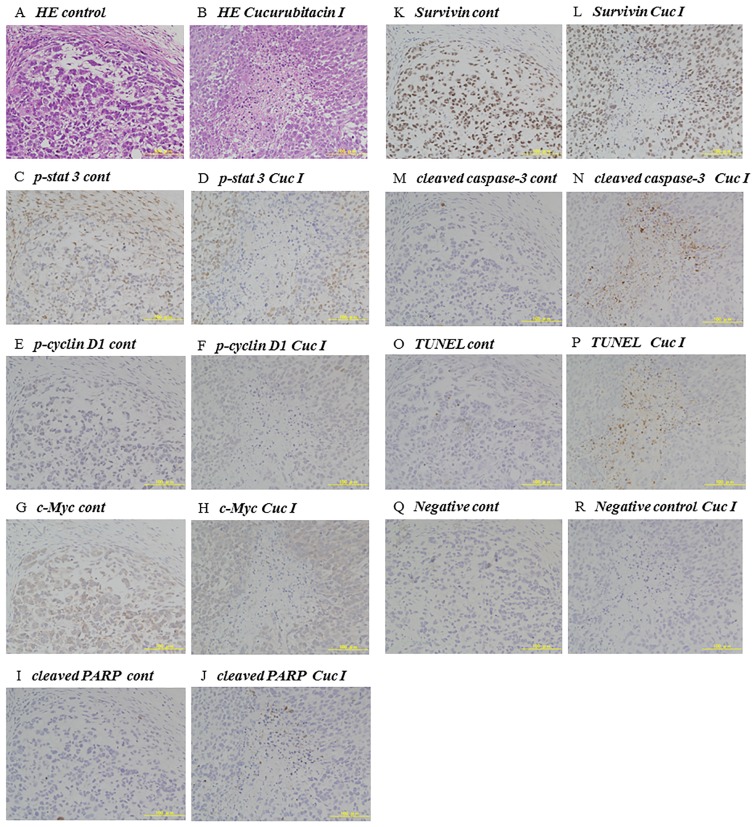
Histologic examination and terminal deoxynucleotide trans-ferase-mediated deoxyuridine triphosphate nick-end labeling (TUNEL) assay
For histologic examination, tumor samples were fixed in 4% paraformaldehyde phosphate buffer solution, embedded in paraffin and cut into 5-mm-thick sections. The sections were stained with hematoxylin-eosin and examined under a light microscope. Immunohistochemistry was carried out using antibodies obtained from the following sources and used at the dilutions recommended by the manufacturer: phospho-STAT3 antibodies 1:400 dilution (Cell Signaling Technology) and cleaved caspase-3 antibodies 1:300 dilution, phospho-cyclin D1 antibodies 1:200 dilution, c-Myc antibodies 1:200 dilution, surviving antibodies 1:400 dilution and cleaved PARP antibodies 1:50 dilution (Cell Signaling Technology). TUNEL staining was carried out on paraformaldehyde-fixed, paraffin-embedded sections using the ApopTag® Peroxidase In Situ Apoptosis Detection kit (Intergen, NY, USA) according to the manufacturer's instructions.
Statistical analysis
All in vitro experiments were repeated at least three times to ensure reproducibility. Data are expressed as the means ± SD. A non-parametric analysis of variance test (Mann-Whitney) was used to compare differences between two groups. Kaplan-Meier analysis was used to estimate survival time of treated mice. A repeated ANOVA or one-way ANOVA was used to compare tumor volume and weight. P-values are indicated in the figures. A p-value of <0.05 was considered statistically significant.
Results
Compound screening
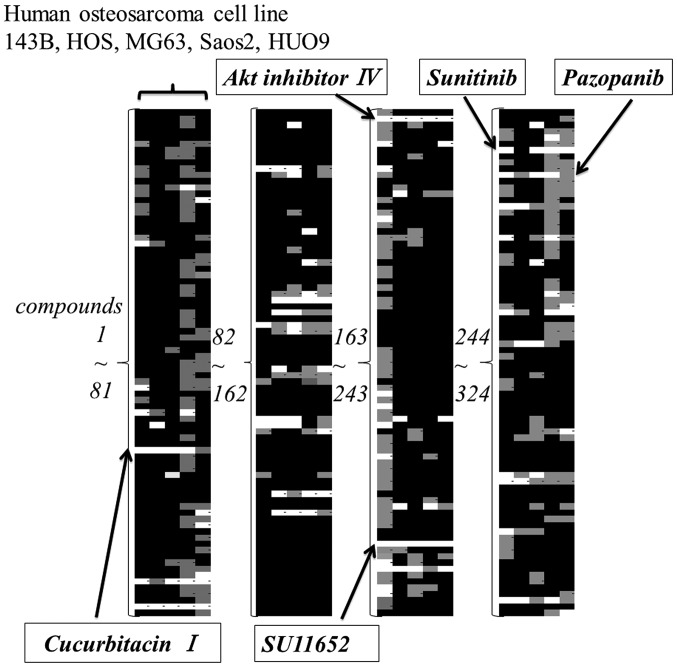
The anti-proliferative effect of 324 compounds against five OS cell lines was screened. The results were color-coded according to the percentage decrease in cell viability compared to control. White color indicated >50% reduction and a gray indicated from 20 to 50% reduction. Based on this color analysis, compounds that had a broad effect on 5 cell lines were narrowed down to pazopanib, sunitinib, cucurbitacin I, Akt-inhibitor IV, and SU11652 (Fig. 1). Cytotoxic compounds and compounds unsuitable for in vivo administration were excluded from this screening.
Figure 1.
Initial screening of the SCADS library for molecules that inhibit the cell viability of osteosarcoma cell lines. Five OS cell lines were treated for 24 h with compounds from the SCADS library and cell viability was evaluated. Compounds which had a broad effect on the five OS cell lines were selected by color imaging. Each column corresponds to an OS cell line (HUO9, 143B, HOS, Saos2 or MG63). White areas indicate >50% reduction in cell viability compared to the control, gray areas indicate a reduction of 20–50%, and black areas indicate a reduction of 0–20%. The compounds used in the assay/examined were cucurbitacin I, AKT inhibitor IV, SU11652, sunitinib and pazopanib.
Effect of identified compounds on cell viability
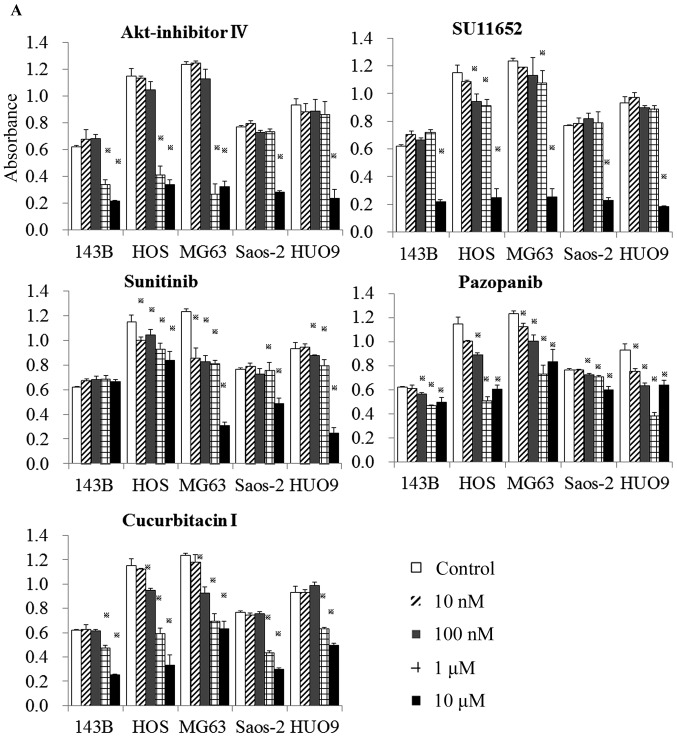
The 5 compounds were then examined more specifically for their effects on cell viability in 2D monolayer (Fig. 2A) and 3D collagen cultures (Fig. 2B).
Figure 2.
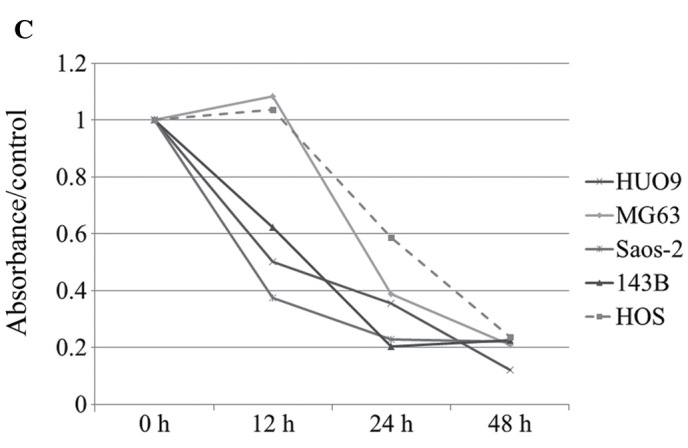
Effect of the selected compounds on cell viability of monolayer and 3D cultures of OS cell lines. (A) Analysis of the dose-dependent effect of the five selected compounds on the viability of five OS cell lines in monolayer culture. (B) Analysis of the dose-dependent effect of the five selected compounds on the viability of five OS cell lines in 3D collagen culture. (C) Time-dependent inhibition of the proliferation of five OS cell lines in monolayer culture by 10 μM of cucurbitacin I.
Cucurbitacin I and Akt inhibitor IV demonstrated a dose-dependent and significant reduction in cell viability of all five OS cell lines in both monolayer and 3D cultures. Pazopanib displayed a weak reduction in the viability of 143B, Saos-2 and HUO9 cells in monolayer culture and of 143B, HOS and Saos-2 cells in 3D culture. SU11652, at a concentration of 10 μM, showed a broad inhibition of cell viability in monolayer and 3D cultures. Sunitinib had a weak effect on the viability of 143B cells in monolayer and of 143B and HOS cells in 3D culture (Fig. 2A and B). Sunitinib and SU11652 are established inhibitors of receptor tyrosine kinases that are essential for angiogenesis, tumor cell proliferation, and tumor cell survival. These inhibitors have been developed by Sugen (Redwood City, CA, USA). Sunitinib (SU11248) was made by replacement of chlorine in SU11562 with fluorine. Only sunitinib has been applied in clinical situations (16). Based on their above effects on cell viability, not only pazopanib but also sunitinib and SU11652 were excluded from further experiments.
Derivatives of cucurbitacin I (cucurbitacin B) and of Akt-inhibitor IV (three oral Akt-inhibitors) were then assayed for their effect on cell viability. The oral Akt-inhibitors, AZD5363, GDC0068 and GSK690693, had only a small inhibitory effect on cell viability and Akt-inhibitor IV exhibited toxicity in vivo (data not shown). Akt-inhibitors were therefore excluded from this study. The family Cucurbitaceae (cucurbitacin I and cucurbitacin B) demonstrated broad and significant inhibition of the viability of five OS cell lines in a dose-dependent manner. Compared to cucurbitacin B, viability of the OS cell lines Saos2 and MG63 was significantly decreased to a greater extent by cucurbitacin I when the cells were exposed to 10 μM of each agent for 48 h (data not shown). Therefore, subsequent experiments were performed using cucurbitacin I. Cucurbitacin I displayed similar results in the five OS cell lines in a time-dependent manner (Fig. 2C).
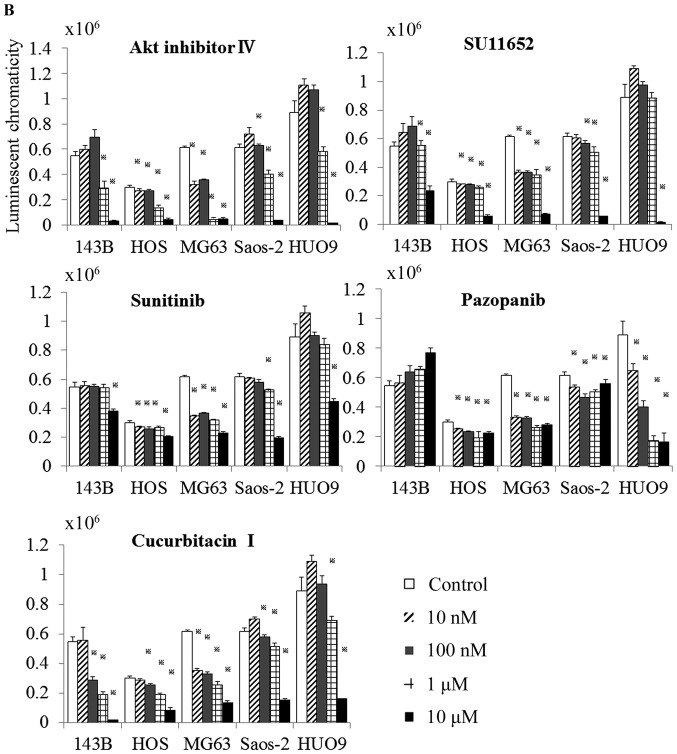
Cucurbitacin I induces apoptosis in osteosarcoma cells
Annexin V (x-axis) is a protein that binds to the phospholipid phosphatidylserine, but cannot enter the cell. Phosphatidylserine is located at the inner side of the membrane. However, upon apoptosis induction, its normal distribution in the cell is perturbed and it becomes exposed at the outer membrane. This feature is used in Annexin V staining for the detection of early apoptotic cells. The membrane-impermeable dye PI (y-axis) binds directly to the DNA, which is only possible upon membrane damage, occurring at late apoptotic or necroptotic events. The early apoptosis rate (red zone) increased in the cucurbitacin I treatment group compared to the control group in all five OS cell lines (143B 19.57 to 21.64%, HOS 27.89 to 56.41%, MG63 22.56 to 33.59%, HUO9 53.1 to 64.9%, Saos2 21.77 to 28.68%) (Fig. 3). These results confirmed that cucurbitacinI causes osteosarcoma cell death through apoptosis.
Figure 3.
Quantification of apoptotic cell populations. Depending on fluorescence intensity of Annexin V (x-axis) and propidium iodide (PI, y-axis), the populations can be distinguished into double-negative (healthy) cells, Annexin V-positive (early apoptotic cells) and double-positive (late apoptotic and necroptotic) cells.
Cell signaling mechanism of cucurbitacin I
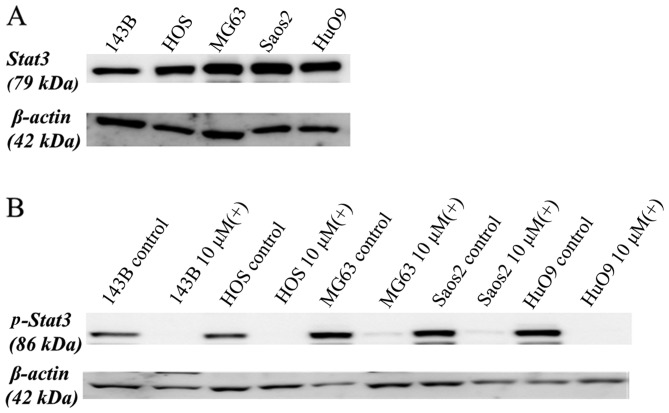
STAT3 is tyrosine phosphorylated and constitutively activated in many human cancer types (17–19). We first assayed STAT3 expression of the five human OS cell lines (143B, HOS, MG63, SAOS-2, and HUO9) by western blotting of the cell lysates with antibodies specific for STAT3. All five cell lines expressed high levels of STAT3 (Fig. 4A).
Figure 4.
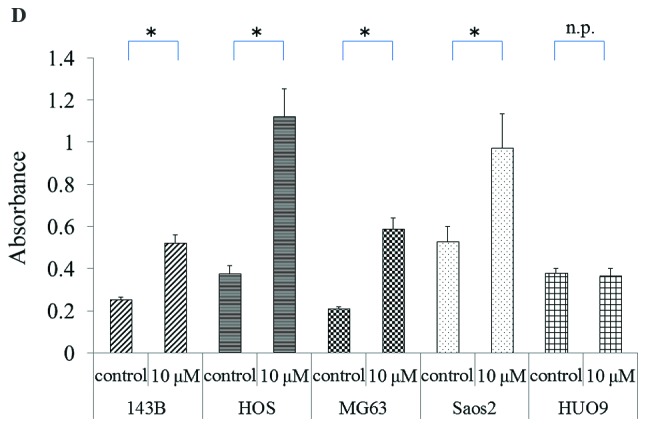
Analysis of the effect on cell signaling of osteosarcoma cell lines by cucurbitacin I. (A) Western blot analysis of STAT3 expression in the five OS cell lines. β-actin was used as a loading control. (B) The effect of incubation of the five OS cell lines with vehicle (−) or cucurbitacin I (10 μM; +) for 12 h on phosphorylated STAT3 (p-STAT3) was analyzed by western blotting with an anti-p-STAT3 antibody. β-actin was used as a loading control. (C) The effect of incubation of the five OS cell lines with vehicle (−) or cucurbitacin I (10 μM; +) for 24 h on the anti-apoptotic factor, Mcl-1, the apoptotic product, cleaved PARP, cleaved caspase-3 and the signaling molecules phospho-cyclin D1, c-Myc and survivin that regulate proliferation, was analyzed by western blotting. β-actin was used as a loading control. (D) The effect of incubation of the five OS cell lines with vehicle (control) or cucurbitacin I (10 μM) for 24 h on the activation of caspase-3 was analyzed using an ELISA.
These five human OS cell lines were then treated with or without 10 μM of cucurbitacin I for 12 h, following which, the cell lysates were analyzed by western blotting with antibodies specific for phospho-STAT3. As shown in Fig. 4B, cucurbitacin I suppressed the levels of phosphorylated STAT3 in all five cell lines.
STAT3-mediated signals are involved in regulation of the apoptotic pathway. Caspase-3, a member of the caspase family that plays a central role in apoptosis, is primarily responsible for the cleavage of PARP during cell death and receives inhibitory signals from Mcl-1. The effect of cucurbitacin I on PARP cleavage, cleaved caspase-3 and Mcl-1 was analyzed by western blotting, and its effect on activated caspase-3 was measured using ELISA. Cucurbitacin I clearly downregulated Mcl-1 protein levels and upregulated cleavage of the PARP protein in all OS cell lines treated for 24 h (Fig. 4C). As shown in Fig. 4D, activated caspase-3 was observed in all OS cell lines, except for HUO9 cells, that were treated with cucurbitacin I for 24 h. Thus, cucurbitacin I induced apoptosis in human OS cells.
The effect of cucurbitacin I on cell cycle regulator proteins, such as phospho-cyclin D1, c-Myc and survivin, was also investigated by western blotting with each specific antibody. Phospho-cyclin D1 plays a role as a cell cycle regulator. c-Myc is a key regulator of cellular proliferation and growth factor stimulation. Survivin is a member of the inhibitors of apoptosis protein family and inhibits cell death through interference with both caspase-dependent and -independent cell apoptosis. As shown in Fig. 4C, cucurbitacin I clearly downregulated phospho-cyclin D1, c-Myc and survivin levels following treatment for 24 h.
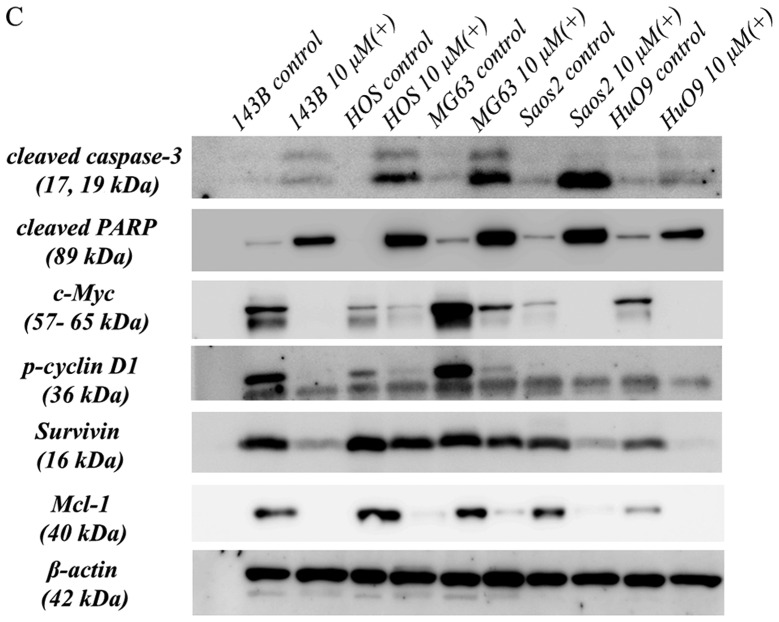
Cucurbitacin I inhibits growth and induces apoptosis in mice with tumors
To determine the effect of cucurbitacin I on tumor growth inhibition, we evaluated time-dependent changes in 143B xenografts in vivo following cucurbitacin I treatment. Fig. 5A shows that, in the absence of cucurbitacin I, the growth of the 143B tumor was highly aggressive, but that treatment with 0.5 or 1.0 mg/kg of cucurbitacin I significantly and dose-dependently inhibited the tumor growth. Furthermore, treatment with 0.5 and 1.0 mg/kg of cucurbitacin I improved overall survival rate, and body weight significantly increased over time (Fig. 5B and C). In addition, the tumor was histopathologically evaluated after 14 days of treatment with 1.0 mg/kg cucurbitacin I. Cucurbitacin I suppressed phospho-STAT3 phospho-cyclin D1, survivin and c-Myc expression in the 143B tumor. Moreover, the phospho-STAT3-negative area was positive by TUNEL, cleaved caspase-3 and cleaved PARP in immunohistochemical analysis. Thus, suppression of tumor cell growth signal by cucurbitacin I administration led to tumor cell apotosis (Fig. 6).
Figure 5.
In vivo antitumor effect of cucurbitacin I. Athymic nude mice with 143B xenografts were treated with vehicle (control), 0.25, 0.5 or 1 mg/kg of cucurbitacin I as described in Materials and methods. (A) The effect on tumor growth was assayed. Data are mean tumor volumes ± standard deviation (SD, error bars) of four mice per group. *p<0.01 (0.5 or 1.0 mg/kg vs. control by repeated ANOVA). A significant difference (#p<0.05; 0.5 and 1.0 mg/kg vs. control at the 2-, 3- and 4-week time-points by one-way ANOVA). (B) The survival rate was analyzed by Kaplan-Meier analysis. A significant difference (#p<0.01 by log-rank test). (C) Body weight was analyzed at the indicated time-points. A significant difference (*p<0.05; 0.5 and 1.0 mg/kg vs. control at the 2-, 3- and 4-week time-points by one-way ANOVA).
Figure 6.
Immunohistochemical analysis of cucurbitacin I-treated tumors. Representative 143B tumors of athymic nude mice were immunohistochemically analyzed on day 14 after administration of control (A, C, E, G, I, K, M, O and Q) or 1.0 mg/kg cucurbitacin I (B, D, F, H, J, L, N, P and R). (A and B) Hematoxylin-eosin (H&E) staining. (C and D) Immunohistochemical staining of phospho-STAT3. (E and F) p-cyclin D1. (G and H) c-Myc. (I and J) Cleaved PARP. (K and L) Suvivin. (M and N) Cleaved caspase-3. (O and P) TUNEL assay. (Q and R) Negative control.
Discussion
Progress in the development of therapeutic agents for primary musculoskeletal malignant tumors including OS has been much slower than that for molecular targeted agents for other cancers. This is because, firstly, the disease prevalence rate is extremely low, and, secondly, the tumor tissues are formed heterogeneously by various cells. Although screening of a compound library to detect agents for tumor treatment is not difficult, few such screenings have been performed for rare malignant tumors such as OS (20). The rarity of these tumors may result in an economic disadvantage for pharmaceutical companies and difficulty in performing clinical trials. In this study, we attempted to identify new target molecules for OS through cell-based screening using the SCADS inhibitor kit and five OS cell lines. We selected cucurbitacin I among many candidates based on its ability to inhibit the viability of the five OS cell lines.
The cucurbitacins have been used for centuries as unpurified molecules in folk medicine for their anti-inflammatory analgesic effects. However, little was known about the biological activities of the cucurbitacins for a long time. Recently, the derivatives of cucurbitacin: B, D, E and Q, have been widely recognized for their anti-proliferative activity in in vitro studies using endothelial cells, leukemias, and a variety of solid cancer cell lines (18,21–24). Cucurbitacin I has been found to have anti-proliferative properties against adenocarcinoma cells (25,26), nasopharyngeal carcinoma cells (27), anaplastic large cell lymphoma (28), and non-small cell carcinoma (29). In this study, we first demonstrated that cucurbitacin I inhibited viability of human OS cell lines in monolayer and collagen 3D cultures. A similar result was previously shown for cucurbitacin B in combination with methotrexate, which showed promising anti-proliferative activity against human OS (30). However, in this study, comparison of the effect of cucurbitacin I and cucurbitacin B alone in vitro indicated that cucurbitacin I showed greater inhibition of tumor cell viability than cucurbitacin B.
Initial studies suggested that cucurbitacin I was a selective inhibitor of janus kinase (JAK)/STAT3 activation (22) and that it reduced the levels of activated STAT3 in human cancer cell lines including pancreatic, lung and breast carcinomas (25). STAT3 is a critical mediator of oncogenic signaling, and is activated in many human cancers (19,31–33), including in 82% of prostate cancers (34), 70% of breast cancers (35), >90% of head and neck cancers (36), and >50% of lung cancers (37). In OS cell lines and tissues, STAT3 and phospho-STAT3 are overexpressed (38). Furthermore, activation of STAT3 signaling induces the expression of specific genes such as phosphocyclin D1, c-Myc, Mcl-1, and survivin, which may stimulate cell proliferation and anti-apoptosis, and promote tumor growth (29). In the tumors investigated, aberrant STAT3 activation has been demonstrated to be required for tumor cell growth and survival (19,39,40).
In this study, STAT3 was highly expressed in the OS cell lines and cucurbitacin I suppressed phospho-STAT3 expression. Our results indicated that cucurbitacin I treatment suppressed the expression of anti-apoptotic factors, such as Mcl-1, and enhanced apoptotic factors such as caspase-3 and cleaved PARP. Additionally, cucurbitacin I also inhibited the expression of the cell proliferation factors, survivin, c-Myc and phospho-cyclin D1 (Fig. 4). These changes in expression of the downstream targets of STAT3 signaling led to an increase in apoptosis and a decrease in the proliferation of OS cells. Moreover, the phospho-STAT3 negative area of tumors in vivo was positive by TUNEL assay in immunohistochemical analysis indicating apoptosis (Fig. 6). We successfully demonstrated cucurbitacin I induced tumor cell death by demonstrating an increase in apoptosis and a decrease in proliferative signaling via inactivation of STAT3. These findings may explain why administration of purified cucurbitacin I to athymic nude mice with human OS xenografts resulted in significant inhibition of tumor growth and improvement in the overall survival rate. It has also been shown that inhibition of STAT3-dependent signaling pathways can reverse tumor growth in experimental systems with few effects on normal cells (18,19). In this study, the administration of 0.5 or 1.0 mg/kg of cucurbitacin I showed inhibition of tumor growth without body weight decrease. It was therefore considered that cucurbitacin I did not have a severe toxic effect.
In conclusion, we demonstrated significant inhibition of tumor growth and improvement in the overall survival rate in vivo by cucurbitacin I treatment. These effects resulted from inactivation of STAT3, leading to the induction of apoptosis and the suppression of proliferative signaling mediated by signaling molecules such as survivin, c-Myc and phospho-cyclin D1. These results shed light on a therapeutic strategy by which cucurbitacin I might be used as a clinical agent and suggest that STAT3 might be used as a therapeutic target for OS treatment.
Acknowledgements
We would like to express our thanks to the SCADS Inhibitor kit, Screening Committee of Anticancer Drugs that was supported by a Grant-in-Aid for Scientific Research on Innovative Areas, Scientific Support Programs for Cancer Research, from The Ministry of Education, Culture, Sports, Science and Technology, Japan.
References
- 1.Picci P. Osteosarcoma (osteogenic sarcoma) Orphanet J Rare Dis. 2007 Jan 27; doi: 10.1186/1750-1172-2-6. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyers PA, Heller G, Healey J, Huvos A, Lane J, Marcove R, Applewhite A, Vlamis V, Rosen G. Chemotherapy for nonmetastatic osteogenic sarcoma: The Memorial Sloan-Kettering experience. J Clin Oncol. 1992;10:5–15. doi: 10.1200/JCO.1992.10.1.5. [DOI] [PubMed] [Google Scholar]
- 3.Harris MB, Gieser P, Goorin AM, Ayala A, Shochat SJ, Ferguson WS, Holbrook T, Link MP. Treatment of metastatic osteosarcoma at diagnosis: A Pediatric Oncology Group Study. J Clin Oncol. 1998;16:3641–3648. doi: 10.1200/JCO.1998.16.11.3641. [DOI] [PubMed] [Google Scholar]
- 4.Bacci G, Ferrari S, Longhi A, Forni C, Zavatta M, Versari M, Smith K. High-grade osteosarcoma of the extremity: Differences between localized and metastatic tumors at presentation. J Pediatr Hematol Oncol. 2002;24:27–30. doi: 10.1097/00043426-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Meyers PA, Heller G, Healey JH, Huvos A, Applewhite A, Sun M, LaQuaglia M. Osteogenic sarcoma with clinically detectable metastasis at initial presentation. J Clin Oncol. 1993;11:449–453. doi: 10.1200/JCO.1993.11.3.449. [DOI] [PubMed] [Google Scholar]
- 6.Pacquement H, Kahfa C, Fagnou C, Demaille MC, Brunat-Mentigny M, Sariban E, Perel Y, Zucker JM. Metastatic osteogenic sarcoma (OS) at diagnosis. Study of 73 cases from the French Society of Pediatric Oncology (SFOP) between 1980 and 1990. Eur J Cancer. 1997;33:S124. doi: 10.1016/S0959-8049(97)85082-4. [DOI] [Google Scholar]
- 7.Marina NM, Pratt CB, Rao BN, Shema SJ, Meyer WH. Improved prognosis of children with osteosarcoma metastatic to the lung(s) at the time of diagnosis. Cancer. 1992;70:2722–2727. doi: 10.1002/1097-0142(19921201)70:11<2722::AID-CNCR2820701125>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 8.Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: Imaging features. Cancer. 1999;86:1602–1608. doi: 10.1002/(SICI)1097-0142(19991015)86:8<1602::AID-CNCR31>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 9.Baum ES, Gaynon P, Greenberg L, Krivit W, Hammond D. Phase II study of cis-dichlorodiammineplatinum (II) in childhood osteosarcoma: Children's Cancer Study Group Report. Cancer Treat Rep. 1979;63:1621–1627. [PubMed] [Google Scholar]
- 10.Cores EP, Holland JF, Wang JJ, Sinks LF. Doxorubicin in disseminated osteosarcoma. JAMA. 1972;221:1132–1138. doi: 10.1001/jama.221.10.1132. [DOI] [PubMed] [Google Scholar]
- 11.Jaffe N, Paed D, Farber S, Traggis D, Geiser C, Kim BS, Das L, Frauenberger G, Djerassi I, Cassady JR. Favorable response of metastatic osteogenic sarcoma to pulse high-dose methotrexate with citrovorum rescue and radiation therapy. Cancer. 1973;31:1367–1373. doi: 10.1002/1097-0142(197306)31:6<1367::AID-CNCR2820310611>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Marti C, Kroner T, Remagen W, Berchtold W, Cserhati M, Varini M. High-dose ifosfamide in advanced osteosarcoma. Cancer Treat Rep. 1985;69:115–117. [PubMed] [Google Scholar]
- 13.Nitschke R, Starling KA, Vats T, Bryan H. Cis-diamminedichloroplatinum (NSC-119875) in childhood malignancies: A Southwest Oncology Group study. Med Pediatr Oncol. 1978;4:127–132. doi: 10.1002/mpo.2950040208. [DOI] [PubMed] [Google Scholar]
- 14.Hamakawa H, Nakashiro K, Sumida T, Shintani S, Myers JN, Takes RP, Rinaldo A, Ferlito A. Basic evidence of molecular targeted therapy for oral cancer and salivary gland cancer. Head Neck. 2008;30:800–809. doi: 10.1002/hed.20830. [DOI] [PubMed] [Google Scholar]
- 15.Sun J, Blaskovich MA, Knowles D, Qian Y, Ohkanda J, Bailey RD, Hamilton AD, Sebti SM. Antitumor efficacy of a novel class of non-thiol-containing peptidomimetic inhibitors of farnesyltransferase and geranylgeranyltransferase I: Combination therapy with the cytotoxic agents cisplatin, Taxol, and gemcitabine. Cancer Res. 1999;59:4919–4926. [PubMed] [Google Scholar]
- 16.Sun L, Liang C, Shirazian S, Zhou Y, Miller T, Cui J, Fukuda JY, Chu JY, Nematalla A, Wang X, et al. Discovery of 5-[5-fluoro-2-oxo-1,2-dihydroindol-(3Z)-ylidenemethyl]-2,4-dimethyl-1H-pyrrole-3-carboxylic acid (2-diethylaminoethyl) amide, a novel tyrosine kinase inhibitor targeting vascular endothelial and platelet-derived growth factor receptor tyrosine kinase. J Med Chem. 2003;46:1116–1119. doi: 10.1021/jm0204183. [DOI] [PubMed] [Google Scholar]
- 17.Bowman T, Yu H, Sebti S, Dalton W, Jove R. Signal transducers and activators of transcription: Novel targets for anticancer therapeutics. Cancer Control. 1999;6:427–435. [PubMed] [Google Scholar]
- 18.Turkson J, Jove R. STAT proteins: Novel molecular targets for cancer drug discovery. Oncogene. 2000;19:6613–6626. doi: 10.1038/sj.onc.1204086. [DOI] [PubMed] [Google Scholar]
- 19.Bowman T, Garcia R, Turkson J, Jove R. STATs in oncogenesis. Oncogene. 2000;19:2474–2488. doi: 10.1038/sj.onc.1203527. [DOI] [PubMed] [Google Scholar]
- 20.Shoemaker RH. The NCI60 human tumour cell line anticancer drug screen. Nat Rev Cancer. 2006;6:813–823. doi: 10.1038/nrc1951. [DOI] [PubMed] [Google Scholar]
- 21.Jayaprakasam B, Seeram NP, Nair MG. Anticancer and antiinflammatory activities of cucurbitacins from Cucurbita andreana. Cancer Lett. 2003;189:11–16. doi: 10.1016/S0304-3835(02)00497-4. [DOI] [PubMed] [Google Scholar]
- 22.Duncan KLK, Duncan MD, Alley MC, Sausville EA. Cucurbitacin E-induced disruption of the actin and vimentin cytoskeleton in prostate carcinoma cells. Biochem Pharmacol. 1996;52:1553–1560. doi: 10.1016/S0006-2952(96)00557-6. [DOI] [PubMed] [Google Scholar]
- 23.Sun J, Blaskovich MA, Jove R, Livingston SK, Coppola D, Sebti SM. Cucurbitacin Q: A selective STAT3 activation inhibitor with potent antitumor activity. Oncogene. 2005;24:3236–3245. doi: 10.1038/sj.onc.1208470. [DOI] [PubMed] [Google Scholar]
- 24.Rivat C, Rodrigues S, Bruyneel E, Piétu G, Robert A, Redeuilh G, Bracke M, Gespach C, Attoub S. Implication of STAT3 signaling in human colonic cancer cells during intestinal trefoil factor 3 (TFF3) - and vascular endothelial growth factor-mediated cellular invasion and tumor growth. Cancer Res. 2005;65:195–202. [PubMed] [Google Scholar]
- 25.Blaskovich MA, Sun J, Cantor A, Turkson J, Jove R, Sebti SM. Discovery of JSI-124 (cucurbitacin I), a selective Janus kinase/signal transducer and activator of transcription 3 signaling pathway inhibitor with potent antitumor activity against human and murine cancer cells in mice. Cancer Res. 2003;63:1270–1279. [PubMed] [Google Scholar]
- 26.Iwanski GB, Lee DH, En-Gal S, Doan NB, Castor B, Vogt M, Toh M, Bokemeyer C, Said JW, Thoennissen NH, et al. Cucurbitacin B, a novel in vivo potentiator of gemcitabine with low toxicity in the treatment of pancreatic cancer. Br J Pharmacol. 2010;160:998–1007. doi: 10.1111/j.1476-5381.2010.00741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lui VWY, Yau DMS, Wong EYL, Ng YK, Lau CPY, Ho Y, Chan JP, Hong B, Ho K, Cheung CS, et al. Cucurbitacin I elicits anoikis sensitization, inhibits cellular invasion and in vivo tumor formation ability of nasopharyngeal carcinoma cells. Carcinogenesis. 2009;30:2085–2094. doi: 10.1093/carcin/bgp253. [DOI] [PubMed] [Google Scholar]
- 28.Shi X, Franko B, Frantz C, Amin HM, Lai R. JSI-124 (cucur-bitacin I) inhibits Janus kinase-3/signal transducer and activator of transcription-3 signalling, downregulates nucleophosmin-anaplastic lymphoma kinase (ALK), and induces apoptosis in ALK-positive anaplastic large cell lymphoma cells. Br J Haematol. 2006;135:26–32. doi: 10.1111/j.1365-2141.2006.06259.x. [DOI] [PubMed] [Google Scholar]
- 29.Jing N, Tweardy DJ. Targeting Stat3 in cancer therapy. Anticancer Drugs. 2005;16:601–607. doi: 10.1097/00001813-200507000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Lee DH, Thoennissen NH, Goff C, Iwanski GB, Forscher C, Doan NB, Said JW, Koeffler HP. Synergistic effect of low-dose cucurbitacin B and low-dose methotrexate for treatment of human osteosarcoma. Cancer Lett. 2011;306:161–170. doi: 10.1016/j.canlet.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bromberg JF, Wrzeszczynska MH, Devgan G, Zhao Y, Pestell RG, Albanese C, Darnell JE., Jr Stat3 as an oncogene. Cell. 1999;98:295–303. doi: 10.1016/S0092-8674(00)81959-5. [DOI] [PubMed] [Google Scholar]
- 32.Yu H, Jove R. The STATs of cancer - new molecular targets come of age. Nat Rev Cancer. 2004;4:97–105. doi: 10.1038/nrc1275. [DOI] [PubMed] [Google Scholar]
- 33.Darnell JE. Validating Stat3 in cancer therapy. Nat Med. 2005;11:595–596. doi: 10.1038/nm0605-595. [DOI] [PubMed] [Google Scholar]
- 34.Mora LB, Buettner R, Seigne J, Diaz J, Ahmad N, Garcia R, Bowman T, Falcone R, Fairclough R, Cantor A, et al. Constitutive activation of Stat3 in human prostate tumors and cell lines: Direct inhibition of Stat3 signaling induces apoptosis of prostate cancer cells. Cancer Res. 2002;62:6659–6666. [PubMed] [Google Scholar]
- 35.Dolled-Filhart M, Camp RL, Kowalski DP, Smith BL, Rimm DL. Tissue microarray analysis of signal transducers and activators of transcription 3 (Stat3) and phospho-Stat3 (Tyr705) in node-negative breast cancer shows nuclear localization is associated with a better prognosis. Clin Cancer Res. 2003;9:594–600. [PubMed] [Google Scholar]
- 36.Leeman RJ, Lui VW, Grandis JR. STAT3 as a therapeutic target in head and neck cancer. Expert Opin Biol Ther. 2006;6:231–241. doi: 10.1517/14712598.6.3.231. [DOI] [PubMed] [Google Scholar]
- 37.Song L, Turkson J, Karras JG, Jove R, Haura EB. Activation of Stat3 by receptor tyrosine kinases and cytokines regulates survival in human non-small cell carcinoma cells. Oncogene. 2003;22:4150–4165. doi: 10.1038/sj.onc.1206479. [DOI] [PubMed] [Google Scholar]
- 38.Ryu K, Choy E, Yang C, Susa M, Hornicek FJ, Mankin H, Duan Z. Activation of signal transducer and activator of transcription 3 (Stat3) pathway in osteosarcoma cells and overexpression of phosphorylated-Stat3 correlates with poor prognosis. J Orthop Res. 2010;28:971–978. doi: 10.1002/jor.21088. [DOI] [PubMed] [Google Scholar]
- 39.Niu G, Heller R, Catlett-Falcone R, Coppola D, Jaroszeski M, Dalton W, Jove R, Yu H. Gene therapy with dominant-negative Stat3 suppresses growth of the murine melanoma B16 tumor in vivo. Cancer Res. 1999;59:5059–5063. [PubMed] [Google Scholar]
- 40.Duncan MD, Duncan KL. Cucurbitacin E targets proliferating endothelia. J Surg Res. 1997;69:55–60. doi: 10.1006/jsre.1997.5028. [DOI] [PubMed] [Google Scholar]