Abstract
Background
Barriers to trauma care for rural populations are well documented, but little is known about the magnitude of urban-rural disparities in injury mortality. This study sought to quantify differences in injury mortality comparing rural and non-rural residents with traumatic injuries.
Methods
Using data from the 2009–2010 Nationwide Emergency Department Sample, multiple logistic regression analyses were conducted to estimate odds of death following traumatic injury for rural residents compared to non-rural residents, while controlling for age, sex, injury type and severity, comorbidities, trauma designation and Census region.
Results
Rural residents were 14% more likely to die, compared to non-rural residents (p < 0.001). Increased odds of death for rural residents were observed at Level I (OR = 1.20, p < 0.001), Level II (OR = 1.34, p < 0.001), and Level IV/non-trauma centers (OR = 1.23, p < 0.001). The disparity was greatest for injuries occurring in the South and Midwest (OR = 1.54, p < 0.001 and OR = 2.06, p < 0.001, respectively), and for cases with an injury severity scores less than nine, or unknown severity (OR = 2.09, <0.001 and OR = 1.31, p < 0.001, respectively).
Conclusions
Rural residents are significantly more likely than non-rural residents to die following traumatic injury. This disparity varies by trauma center designation, injury severity, and US Census region. Distance and time to treatment likely play a role in rural injury outcomes, along with regional differences in pre-hospital care and trauma system organization.
Background
Injury treatment at designated trauma centers can reduce mortality from traumatic injury,1–4 but the majority of US residents in rural areas do not have timely access to Level I or II trauma centers.5 Geographic barriers to trauma care are more likely to impact racial minorities and people living in poverty,6 paralleling established racial and socioeconomic disparities in trauma mortality.7–12 Rural residents face elevated risk of traumatic injury compared to non-rural residents,13, 14 and injury mortality rates are higher in rural communities than in urban and suburban settings.15, 16 While higher injury incidence in rural settings can explain at least some of the difference in injury mortality rates, variation in outcomes within injured populations likely plays a significant role in rural injury mortality rates.17
Several studies have examined urban/rural differences in mortality following injuries using samples from small geographic areas.18, 19 Lipsky, et al. found no geographic variation in trauma outcomes comparing trauma mortality in rural Northern California with the Los Angeles Metro area; however, the authors note that the rural emergency medical services (EMS) system examined was well organized and used enhanced EMS practices.18 Conversely, Svenson, et al. found that children from rural regions in Kentucky are more likely to die from traumatic injuries, compared to non-rural children with similar injuries.19
While existing studies demonstrate urban/rural differences in injury incidence13, 14 and mortality rates15, 16 using nationally representative data, we are not aware of any nationally representative studies exploring urban/rural variation in odds of death following injury for all injury mechanisms and types. This study used the Nationwide Emergency Department Sample (NEDS) from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project to analyze geographic differences in mortality among people with traumatic injury, based on the National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme.
Methods
Study Design
We performed a retrospective analysis of 2009–2010 NEDS data to determine if trauma mortality differs across urban/rural classification. The NEDS is an all payer sample of emergency department (ED) visits, including encounters resulting in discharge, transfer, admission, and/or death.20, 21 The 2009–2010 NEDS contains 57,445,348 ED records (unweighted), of which 8,949,530 include an injury as the primary diagnosis based on the National Trauma Data Standard (NTDS).22 The data are weighted based on geographic region, trauma center designation, urban-rural hospital location, teaching hospital status, and hospital ownership in order to provide a nationally representative sample of EDs. In addition to the stratification fields used to weight the sample, the NEDS includes administrative, diagnostic, and mortality outcomes data.21
Study Sample
Our analyses included ED encounters with injury as the primary or secondary diagnosis, based on International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes included in the NEDS data (ICD-9-CM 800–959.9). In accordance with the NTDS,22 we did not include encounters with superficial injury (ICD-9-CM 910–924.9), foreign body injury (ICD-9-CM 930–939.9) or late effects of injury (ICD-9-CM 905–909.9) as the only injury diagnosis. Records with missing urban-rural classification for the patient’s residence or unknown disposition from the hospital were excluded. We also excluded encounters that resulted in transfer to another hospital as transferred patients are likely to be represented in data from other EDs in the NEDS, and the NEDS does not include identifiers to facilitate tracking of patients across facilities.
Variables and Measurement
The primary outcome of interest was mortality following traumatic injury, including death in the ED or in the hospital following admission. The NEDS includes mortality as a categorical variable, with codes indicating that the patient died in the ED, died in the hospital, or did not die. The NEDS includes a separate variable for disposition from the ED, with codes indicating discharge, admission, transfer, death, or leaving against medical advice (AMA). For the purposes of this study, ED and hospital deaths were combined to create a single dichotomous variable for mortality. Encounters with an indication of death in the ED or in the hospital during the admission associated with the ED encounter were coded as deaths. Encounters with an indication of discharge from the ED, discharge from the hospital admission associated with the ED encounter, or leaving AMA were coded as non-deaths.
The primary independent variable of interest for this study was urban-rural classification based on the National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme. The NEDS includes NCHS classification for each encounter based on the patient’s county of residence,23 and classifications are determined based on county population size and location within or outside of a metropolitan statistical area (MSA). NCHS classifications include large central metropolitan (at least one million residents, includes principal city in MSA), large fringe metropolitan (at least one million residents, in MSA), medium metropolitan (at least 250,000 residents, in MSA), small metropolitan (at least 50,000 residents, in MSA), micropolitan (between 10,000 to 49,999 residents, not In MSA), and noncore (fewer than 9,999 residents, not in MSA).23 Based on NCHS groupings, we collapsed the classifications to a dichotomous rural/non-rural measure, with micropolitan and noncore residences classified as rural, and all others classified as non-rural.23
Our analyses also included ED trauma designation, blunt and penetrating injury, injury severity, comorbidities, age, sex, and geographic region as covariates. The NEDS includes ED trauma designation based on American College of Surgeons designation of trauma centers and/or state designation with EDs coded as level I–III and a combined code for Level IV and non-trauma facilities.21 The NEDS masks trauma center designation when inclusion of this information in combination with other hospital features would make a hospital identifiable. Masked trauma centers ere coded as a combined Level I/II or Level I/II/III. Blunt and penetrating injuries were identified based on injury mechanism, which was extracted from medical records at each participating hospital using External Cause of Injury Codes (E-codes).24 Penetrating injuries included those with cutting or firearm as the mechanism. Blunt injuries included those caused by falls, machinery, motor vehicle traffic, cyclist, pedestrian, or being struck by an object. Blunt and penetrating injuries were included as separate dichotomous variables, and it was possible to have both or neither in a single observation. Injury severity in the NEDS is measured as the Injury Severity Score (ISS). Scores range from 1 to 75, and are calculated based on ICD-9-CM code using the method developed by Baker et al.25 ISS was categorized as 1–8, 9–15, 16–19, and 20 or greater. Records were coded as having an unknown ISS when the ISS could not be determined based on the available diagnosis codes. These records were included as unknown ISS in this analysis. Comorbidities were measured with the Charlson Comorbidity Index (CCI), which was calculated for each encounter based on selected diagnoses reported in the NEDS as ICD-9-CM codes.26 Charlson scores were coded as zero, one, and two or higher. Patient age and sex in the NEDS were extracted from billing data at each participating hospital.21 Age was coded as the patient’s age at the time of arrival in the ED, and was categorize as younger than 18, 18–24, 25–34, 35–44, 45–55, 54–65, and 65 or older. Patient sex was coded as male or female. Geographic region was coded as Northeast, South, Midwest, or West based the location of the treating hospital and US Census region.27
Statistical Analysis
All analyses were conducted using STATA 14.1 (StataCorp LP, College Station, TX), and using NEDS sampling and discharge weights to produce nationally representative patient-level estimates and standard errors. We tabulated population characteristics by urban/rural status, and tested differences between groups using χ2 test for categorical. Multiple logistic regressions were used to calculate odds ratios comparing odds of death from traumatic injury for rural and non-rural, while controlling for age, sex, injury severity, presence of blunt and penetrating trauma, comorbidities, trauma center designation, and US Census region. Models were then stratified by trauma center designation, injury severity, and Census region.
Results
Sample Characteristics
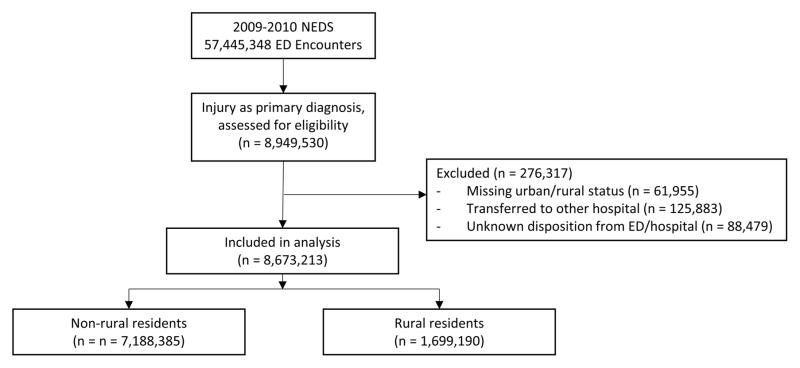
Of the 8,949,530 records identified as injury cases, we excluded records with missing urban-rural classification for the patient’s home address, unknown disposition for the ED, and with patients transferred to another medical facility (Figure 1). Patients excluded due to transfer disposition were less likely to have an ISS in the lowest category than the study sample (62.62% vs. 93.77%, p < 0.001), and more likely to be rural residents (36.82% vs. 18.83%, p < 0.001). Due to the large sample size, the distribution of ISS by rural residence was statistically significantly different for the exclusion categories, compared to the study sample, but the differences were not clinically meaningful.
Figure 1.
Age ranged from zero to one hundred years, with a mean age of 35.43 years, and the sample was 46.43% female. Overall, 0.21% of observations resulted in death in the ED (0.05%) or hospital (0.21%). The vast majority of patients had an ISS between 1 and 8 (93.77%), while 3.47% had a score between 9 and 15, 0.54% between 16 and 19, 0.33% were 20 or higher, and 2.20% with unknown ISS. Most subjects had no comorbidities and a CCI of zero (90.47%), while 7.26% had a CCI of 1 and 2.27% had a score of 2 or higher. Modest differences in the distribution of age, sex, location of death, comorbidities and injury severity for rural and non-rural populations were statistically significant due to the size of the study sample, but these differences were not clinically significant (Table 1). Blunt injuries were observed in 55.47% of cases, and penetrating injuries were observed in 10.60% of cases. Rural residents were slightly less likely to have blunt injuries than non-rural residents (51.87% vs. 56.31%, p < 0.001), but the difference in penetrating injury was not clinically meaningful. Most ED encounters took place at Level IV/non-trauma centers (68.05%), followed by Level I (10.23%), Level II (8.34%), and Level III (6.15%). Encounters with masked trauma center level accounted for 7.23% of all records (2.41% Level I/II and 4.82% Level I/II/III). Rural residents were significantly less likely to receive treatment at a Level I, Level II, or masked trauma center (Level I/II or Level I/II/III) compared to non-rural residents (3.32% vs. 11.83%, 2.63% vs. 9.67%, 0.89% vs. 2.76%, and 2.10% vs 5.45%, respectively; p <0.001), and more likely to receive treatment at a Level IV trauma center or non-trauma center (85.61% vs. 63.98%, p < 0.001). The South Census region accounted for the largest proportion of observations (40.54%), followed by the Midwest (22.20%), Northeast (20.05%), and West (17.13%). Rural residents were more likely be in the South and Midwest regions (50.61% vs. 38.20%, and 29.71% vs. 21.25%, respectively, p < 0.001), and less likely to be in the Northeast and West regions (12.67% vs. 21.76%, and 10.00% vs. 18.78%, respectively, p < 0.001).
Table 1.
Population characteristics by urban/rural status
| Rural (%) | Non-rural (%) | p | |
|---|---|---|---|
| Age | |||
| Younger than 18 | 25.74 | 26.20 | <0.001 |
| 18–24 | 13.33 | 13.25 | <0.001 |
| 25–34 | 15.53 | 15.73 | <0.001 |
| 35–44 | 12.74 | 12.83 | <0.001 |
| 45–54 | 11.89 | 11.69 | <0.001 |
| 55–64 | 7.55 | 7.92 | <0.001 |
| 65 or older | 12.76 | 12.85 | <0.001 |
| Female | 46.48 | 46.17 | <0.001 |
| Mortality | |||
| ED | 0.05 | 0.05 | <0.001 |
| Hospital | 0.16 | 0.15 | <0.001 |
| Trauma Designation | |||
| Level I | 63.98 | 85.61 | <0.001 |
| Level II | 6.31 | 5.45 | <0.001 |
| Level III | 9.67 | 2.63 | <0.001 |
| Level IV/Non-Trauma | 11.83 | 3.32 | <0.001 |
| Trauma level masked (I or II) | 2.76 | 0.89 | <0.001 |
| Trauma level masked (I, II, or III) | 5.45 | 2.10 | <0.001 |
| ISS | |||
| 1–8 | 93.78 | 93.70 | <0.001 |
| 9–15 | 3.52 | 3.27 | <0.001 |
| 16–19 | 0.55 | 0.47 | <0.001 |
| 20 or higher | 0.32 | 0.35 | <0.001 |
| Missing | 1.82 | 2.20 | <0.001 |
| Blunt injury | 51.87 | 56.31 | |
| Penetrating injury | 11.15 | 10.47 | |
| Charlson Comorbidity Index | |||
| 0 | 91.59 | 90.21 | <0.001 |
| 1 | 6.42 | 7.45 | <0.001 |
| 1 or more | 1.99 | 2.33 | <0.001 |
| Census Region | |||
| Northeast | 21.76 | 12.67 | <0.001 |
| Midwest | 21.25 | 26.71 | <0.001 |
| South | 38.20 | 50.61 | <0.001 |
| West | 18.78 | 10.00 | <0.001 |
While urban-rural variation in the overall distribution of ISS was minimal, there were differences in rural/non-rural distribution of ISS when examined by trauma center level. At Level I centers, rural patients were more likely to have an ISS in the more severe categories compared to non-rural patients (15.24% vs. 4.55% with ISS 9–15, 5.52% vs. 1.14% with ISS 16–19, and 5.48% vs. 0.96% with ISS 20+; p < 0.001), and rural patients were less likely to have an ISS in the lowest severity category compared to non-rural patients (73.77% vs. 93.35% with ISS 1–8; p < 0.001). A similar pattern was observed at Level II centers (89.26% vs. 95.50% with ISS 1–8, 7.48% vs. 3.45% with ISS 9–15, 1.90% vs. 0.68% with ISS 16–19 and 1.36% vs. 0.37% with ISS 20+; p < 0.001). The distribution of injury severity at Level III and Level IV/Non-Trauma centers varied very little by urban-rural designation, but the differences were statistically significant (p < 0.001 at both levels).
Mortality Odds
Overall, rural residents were 14% more likely to die, compared to non-rural residents when controlling for age, sex, ISS, CCI, injury type, trauma designation, and Census region (Table 2; OR = 1.14, p <0.001). Odds of death increased with each age category, relative to patients age 18 and younger, with and 88% increase in odds of death for patients age 18–24 (p < 0.001) to a more than six fold increase for patients age 65 or older (p < 0.001). Female patients were 44% less likely to die compared to otherwise similar male patients (p < 0.001). Compared to patients treated at Level IV/non-trauma centers, odds of death was highest for Level III centers (OR = 2.34, p < 0.001), followed by Level II centers (OR = 1.84, p < 0.001), and Level I centers (OR = 1.34, p < 0.001). The odds ratios for masked trauma centers were 1.80 (p < 0.001) for Level I/II centers, and 2.18 (p < 0.001) for Level I/II/III centers. Relative to patients with ISS 1–8, odds of death increased by 26.39 times (p < 0.001) for patients with ISS 9–15, 72.82 times for ISS 16–19, and 232.80 times for patients with ISS 20 or greater. Patients with unknown ISS were 5.80 times more likely to die than patients with ISS 1–8. Penetrating injuries were associated with a 4.37 times increase in odds of death (p < 0.001), while blunt injuries were not associated with increased odds of death. Patients with a Charlson score of 1 were 21% more likely to die than those with no comorbidities (p < 0.001), while those with 2 or more comorbidities were 2.36 times more likely to die (p < 0.001). Finally, patients in the Midwest region were 17% less likely to die than those in the Northeast (p < 0.001), while patients in the South were 8% more likely to die (p = 0.002). Odds of death did not vary for patients in the Western region (OR = 0.99, p = 0.828).
Table 2.
Odds ratios from logistic model
| Odds Ratio | 95% CI | p | |
|---|---|---|---|
| Rural/urban status | |||
| Non-rural | Ref | -- | -- |
| Rural | 1.14 | 1.09 – 1.19 | <0.001 |
| Age | |||
| Younger than 18 | Ref | -- | -- |
| 18–24 | 1.88 | 1.17 – 2.07 | <0.001 |
| 25–34 | 1.81 | 1.64 – 1.99 | <0.001 |
| 35–44 | 1.83 | 1.66 – 2.02 | <0.001 |
| 45–54 | 2.19 | 1.99 – 2.40 | <0.001 |
| 55–64 | 2.79 | 2.54 – 3.07 | <0.001 |
| 65 or older | 6.44 | 5.93 – 7.01 | <0.001 |
| Sex | |||
| Male | Ref | -- | -- |
| Female | 0.66 | 0.64 – 0.68 | <0.001 |
| Trauma Designation | |||
| Level I | 1.34 | 1.24 – 1.45 | <0.001 |
| Level II | 1.84 | 1.74 – 1.95 | <0.001 |
| Level III | 2.34 | 2.23 – 2.45 | <0.001 |
| Level IV/Non-Trauma | Ref | -- | -- |
| Trauma level masked (I or II) | 1.80 | 1.66 – 1.95 | <0.001 |
| Trauma level masked (I, II, or III) | 2.18 | 2.04 – 2.32 | <0.001 |
| ISS | |||
| 1–8 | Ref | -- | -- |
| 9–15 | 26.39 | 25.11 – 27.73 | <0.001 |
| 16–19 | 72.82 | 68.64 – 77.24 | <0.001 |
| 20 or higher | 232.80 | 220.13 – 246.20 | <0.001 |
| Unknown | 5.80 | 5.05 – 6.65 | <0.001 |
| Blunt injury | |||
| No | Ref | -- | -- |
| Yes | 1.05 | 1.00 – 1.10 | 0.063 |
| Penetrating injury | |||
| No | Ref | -- | -- |
| Yes | 4.37 | 4.11 – 4.65 | <0.001 |
| Charlson Comorbidity Index | |||
| 0 | Ref | -- | -- |
| 1 | 1.21 | 1.16 – 1.27 | <0.001 |
| 1 or more | 2.36 | 2.26 – 2.47 | <0.001 |
| Census Region | |||
| Northeast | Ref | -- | -- |
| Midwest | 0.83 | 0.79 – 0.88 | <0.001 |
| South | 1.08 | 1.03 – 1.13 | 0.002 |
| West | 0.99 | 0.94 – 1.05 | 0.828 |
When stratified by trauma designation and controlling for age, sex, ISS, CCI, injury type, and census region, rural residents were 20% more likely to die than non-rural residents at Level I trauma centers (p < 0.001; Table 3), 34% more likely to die at Level II centers (p < 0.001), and 23% more likely to die at Level IV/non-trauma centers (p < 0.001). Odds of death did not vary for rural residents at Level III trauma centers of masked trauma centers. When stratified by injury severity, odds of death were 31% higher for rural residents with ISS 1–8 compared to similar non-rural residents (p < 0.001), 10% higher for ISS 9–15 (p = 0.009), 21% higher for ISS 16–19 (p = 0.001), 10% higher for ISS 20 or higher (p = 0.046). Rural residents with unknown ISS were more than twice as likely to die as otherwise similar non-rural residents (OR = 2.09, p < 0.001). When stratified by Census region, rural residents in the Midwest were 21% more likely to die, and rural residents in the South were 11% more likely to die, compared to urban residents. There was no difference in odds of death for rural residents in the Northeast and South.
Table 3.
Odds ratios for rural vs. urban residence, stratified by trauma center designation, injury severity, and Census region
| Odds Ratio | 95% CI | p | |
|---|---|---|---|
| Trauma center designation | |||
| Level I | 1.20 | 1.11 – 1.30 | <0.001 |
| Level II | 1.34 | 1.16 – 1.54 | <0.001 |
| Level III | 1.12 | 0.93 – 1.34 | 0.211 |
| Level IV/non-trauma | 1.23 | 1.15 – 1.31 | <0.001 |
| Masked I/II | 1.03 | 0.79 – 1.34 | 0.831 |
| Masked I/II/III | 1.05 | 0.84 – 1.30 | 0.665 |
| Injury severity | |||
| ISS 1–8 | 1.31 | 1.19 – 1.44 | <0.001 |
| ISS 9–15 | 1.10 | 1.03 – 1.19 | 0.009 |
| ISS 16–19 | 1.21 | 1.09 – 1.35 | 0.001 |
| ISS 20+ | 1.10 | 1.00 – 1.20 | 0.046 |
| Unknown ISS | 2.09 | 1.51 – 2.91 | <0.001 |
| Census Region | |||
| Northeast | 1.10 | 0.97 – 1.24 | 0.125 |
| Midwest | 1.21 | 1.11 – 1.31 | <0.001 |
| South | 1.11 | 1.04 – 1.18 | 0.002 |
| West | 1.11 | 0.97 – 1.28 | 0.130 |
Sensitivity Analyses
Sensitivity analyses were conducted to assess the impact of excluding patients leaving AMA, those with missing ISS, and those with masked trauma center designation. While individual coefficients varied by as much as 0.05 in each direction, the significance and direction of the results did not changes for any variable under any of the sensitivity analyses.
Discussion
This study demonstrates that rural residents are more likely to die from traumatic injury than non-rural residents when controlling for injury severity, presence of blunt and penetrating trauma, comorbidities, age, sex, and geographic region. This disparity was observed when examining mortality across all trauma designation levels combined, and was also observed at Level I, II and IV/non-trauma centers. The disparity persists across injury severity categories, though the association was less pronounced for the highest severity categories. The difference in odds of death for rural residents was present in the South and Midwest Census regions, and was not observed in the Northeast of West regions.
Our findings regarding the role of age, sex, injury severity, comorbidities, and injury type are consistent with prior studies examining determinants of injury mortality.28–36 We found that odds of death are higher for patients treated at Level I and II trauma centers. While this may seem inconsistent with established lifesaving ability of trauma center care,4 this is likely a reflection of trauma system organization and triage decisions, with the most critically injured patients receiving treatment at Level I and II centers.
Our findings also suggest that injury mortality varies by Census region, with patients treated in the South region facing higher odds of death than in other regions, and with larger urban-rural disparities in mortality observed in the Midwest and South. Distance from trauma centers and travel time are likely significant contributors to this pattern. Nearly all of Northeast region falls within a sixty minute drive of a Level I or II trauma center, while other regions have larger rural populations living more than an hour from trauma care.5 Treatment in the Midwest region does not predict higher odds of death, but rural residents in the Midwest face a greater disparity in mortality than rural residents in the South. This may be due to variation in time to treatment for rural residents across regions. While many rural residents in the both regions live more than an hour from a Level I or II trauma center, time to trauma center care is longer in the Midwest than in the South.5 Treatment in the West region does not predict mortality, and we did not observe a disparity in mortality for rural residents in the West region. Again, this is likely due to travel times, which are longer in the West than in any other Census region.5 Travel times in the West region may be long enough that patients are dying in transit (and not included in the NEDS), while similar patients in other regions die in the ED. Differences in EMS system structure and pre-hospital care also likely contribute to regional variation in injury mortality,37–39 including the presence of well-organized EMS systems in the West region, as noted by Lipsky, et al.18
Approximately 20% of the US population live in rural areas and face elevated risk of death from injury.23 This increased risk of death may result in part from differences in injury incidence,13, 14 but our findings suggest that differences in injury response also contribute to injury mortality in rural populations, including documented barriers to trauma center access for the majority of rural residents.5 Our findings are consistent with prior studies indicating that rural residents are more likely to die from injury that non-rural residents.19, 40 While our findings are not consistent with the overall findings of Lipsky et al., we do find variation in mortality across trauma designation levels, with no disparity found at Level III and IV trauma centers, which may support a similar conclusion that well organized EMS systems reduce mortality in populations with limited trauma center access.18
These findings suggest a significant disparity in outcomes following traumatic injury, with rural populations experiencing worse outcomes than non-rural populations. Due to the geographic distribution of various demographic groups in the US, this disparity may disproportionately impact racial minorities and people living in poverty.6 Little is known about the causal pathway for this disparity. Time to treatment is presumed to be a significant factor in trauma outcomes,41 and would disparately impact rural populations,5, 6 but evidence for the relationship between pre-hospital time and mortality is widely variable.30, 32, 42–52 Other factors, such as community-level wealth and insurance coverage,53–55 may also contribute to geographic disparities in injury mortality. Further research is needed to examine the potentially complex network of factors that determine injury outcomes for rural residents.
Limitations
The NEDS is one of several retrospective data sets commonly used to examine injury outcomes. We selected the NEDS for use in this analysis due to the inclusion of urban-rural residence at the patient level. Urban-rural residence is either not included, or missing for most observations in other data sets commonly used to examine injury outcomes.56, 57 While the NEDS is the best data set available for this study, there are several limitations. Injury severity and comorbidity measures are based on diagnostic codes included in the NEDS. While each observation can include up to 15 diagnostic codes, this may not capture all relevant co-morbid conditions, and it is likely that CII scores based on NEDS data are artificially low. The use of diagnostic codes to estimate injury severity has been validated as a strong predictor of injury mortality58, but the inclusion of other severity indicators, such as Glascow Coma Score, would enhance our ability to control for injury characteristics. While the NEDS uses a stratified sampling strategy to produce a nationally representative sample, there are likely state level effects that are not reflected in this approach, including differences in EMS system organization. The NEDS does not include any measure of distance or travel time. Distance and travel time are closely related to rural residence status,5, 6 and may determine time to definitive care and the trauma designation of the treating hospital. Finally, the NEDS only contains data on ED encounters for patients who are alive upon arrival, and does not include pre-hospital deaths. This limitation may exclude the most severely injured patients who died prior to hospital arrival. If increased distance from a trauma center increases risk of death, then severely injured rural residents may disproportionately be excluded from the NEDS, which would decrease the observed magnitude of the difference in mortality between rural and non-rural residents.
Our findings are limited by the number of records excluded due to unknown disposition from the ED or transfer to another hospital. Rural residents were more likely to be excluded due to hospital transfer, which is consistent with standard hospital transfer protocols for patients with severe injury arriving at Level III trauma centers, Level IV trauma centers, or non-trauma facilities.59 If these transfers represent a more severely injured subset of patients, these exclusions are likely to attenuate our findings as the most severely injured rural residents are not represented.
Next Steps
In light of the disparity demonstrated in this study, future studies should explore differences in cause-specific mortality by urban-rural status, especially for penetrating injuries, that are most likely to benefit from rapid delivery of definitive care.30, 32 Researchers should also evaluate the role of distance and travel time as they relate to mortality for rural residents, both for patients receiving care in the ED and for those who die prior to hospital arrival. As a more detailed understanding of the mortality disparity develops, researchers should explore differences in mortality within the rural population and examine the role of EMS and trauma center characteristics on trauma outcomes for rural residents.
Conclusion
Rural residents have significantly increased risk of death from traumatic injury compared to non-rural residents when treated at Level I or II trauma centers, even when controlling for injury severity and comorbidities. This disparity indicates a need to improve the response to and treatment of traumatic injuries in rural communities. Further research should explore distance and travel time to definitive hospital care as a determinant of disparity in mortality, as well as the role of pre-hospital care.
Acknowledgments
This research supported by Agency for Healthcare Research and Quality NSRA training grant #T32HS000029.
Footnotes
Presented February 1, 2016 at the Academic Surgical Congress, Jacksonville, FL
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Molly P. Jarman, Email: mjarman2@jhu.edu, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management, 624 N Broadway, Baltimore, MD 21205, 919-389-8513 (phone), 410-614-2797 (fax).
Renan C. Castillo, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management.
Anthony R. Carlini, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management.
Lisa M. Kodadek, Johns Hopkins University School of Medicine, Department of Surgery.
Adil H. Haider, Brigham and Women’s Hospital, Division of Trauma, Burn and Surgical Critical Care, Brigham and Women’s Hospital, Harvard Medical School and Harvard T.H. Chan School of Public Health, Center for Surgery and Public Health.
References
- 1.Glance LG, Osler TM, Mukamel DB, Dick AW. Impact of trauma center designation on outcomes: is there a difference between Level I and Level II trauma centers? J Am Coll Surg. 2012;215:372–8. doi: 10.1016/j.jamcollsurg.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 2.Garwe T, Cowan LD, Neas B, Cathey T, Danford BC, Greenawalt P. Survival benefit of transfer to tertiary trauma centers for major trauma patients initially presenting to nontertiary trauma centers. Acad Emerg Med. 2010;17:1223–32. doi: 10.1111/j.1553-2712.2010.00918.x. [DOI] [PubMed] [Google Scholar]
- 3.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Doucet J, et al. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (injury severity score > 15) J Am Coll Surg. 2006;202:212–5. doi: 10.1016/j.jamcollsurg.2005.09.027. quiz A45. [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 5.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, et al. Access to trauma centers in the United States. JAMA : the journal of the American Medical Association. 2005;293:2626–33. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 6.Hsia R, Shen YC. Possible geographical barriers to trauma center access for vulnerable patients in the United States: an analysis of urban and rural communities. Archives of surgery (Chicago, Ill : 1960) 2011;146:46–52. doi: 10.1001/archsurg.2010.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haider AH, Weygandt PL, Bentley JM, Monn MF, Rehman KA, Zarzaur BL, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74:1195–205. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Losonczy LI, Weygandt PL, Villegas CV, Hall EC, Schneider EB, Cooper LA, et al. The severity of disparity: increasing injury intensity accentuates disparate outcomes following trauma. Journal of health care for the poor and underserved. 2014;25:308–20. doi: 10.1353/hpu.2014.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singer MB, Liou DZ, Clond MA, Bukur M, Mirocha J, Margulies DR, et al. Insurance-and race-related disparities decrease in elderly trauma patients. J Trauma Acute Care Surg. 2013;74:312–6. doi: 10.1097/TA.0b013e31826fc899. [DOI] [PubMed] [Google Scholar]
- 10.Salim A, Ottochian M, DuBose J, Inaba K, Teixeira P, Chan LS, et al. Does insurance status matter at a public, level I trauma center? J Trauma. 2010;68:211–6. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 11.Arthur M, Hedges JR, Newgard CD, Diggs BS, Mullins RJ. Racial disparities in mortality among adults hospitalized after injury. Med Care. 2008;46:192–9. doi: 10.1097/MLR.0b013e31815b9d8e. [DOI] [PubMed] [Google Scholar]
- 12.Bowman SM, Martin DP, Sharar SR, Zimmerman FJ. Racial disparities in outcomes of persons with moderate to severe traumatic brain injury. Med Care. 2007;45:686–90. doi: 10.1097/MLR.0b013e31803dcdf3. [DOI] [PubMed] [Google Scholar]
- 13.Coben JH, Tiesman HM, Bossarte RM, Furbee PM. Rural-urban differences in injury hospitalizations in the U.S., 2004. Am J Prev Med. 2009;36:49–55. doi: 10.1016/j.amepre.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Tiesman H, Zwerling C, Peek-Asa C, Sprince N, Cavanaugh JE. Non-fatal injuries among urban and rural residents: the National Health Interview Survey, 1997–2001. Inj Prev. 2007;13:115–9. doi: 10.1136/ip.2006.013201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meit M, Knudson A, Gilbert T, Yu AT, Tanenbaum E, Elizabeth O, et al. The 2014 Update of the Rural-Urban Chartbook. Rural Health Research & Policy Centers; 2014. [Google Scholar]
- 16.Myers SR, Branas CC, French BC, Nance ML, Kallan MJ, Wiebe DJ, et al. Safety in numbers: are major cities the safest places in the United States? Ann Emerg Med. 2013;62:408–18. e3. doi: 10.1016/j.annemergmed.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. Am J Public Health. 2004;94:1689–93. doi: 10.2105/ajph.94.10.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lipsky AM, Karsteadt LL, Gausche-Hill M, Hartmans S, Bongard FS, Cryer HG, et al. A comparison of rural versus urban trauma care. Journal of emergencies, trauma, and shock. 2014;7:41–6. doi: 10.4103/0974-2700.125639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Svenson JE, Spurlock C, Nypaver M. Factors associated with the higher traumatic death rate among rural children. Ann Emerg Med. 1996;27:625–32. doi: 10.1016/s0196-0644(96)70167-1. [DOI] [PubMed] [Google Scholar]
- 20.Owens PL, Barrett ML, Gibson TB, Andrews RM, Weinick RM, Mutter RL. Emergency department care in the United States: a profile of national data sources. Ann Emerg Med. 2010;56:150–65. doi: 10.1016/j.annemergmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 21.Healthcare Cost and Utilization Project. Introduction to the HCUP. Nationwide Emergency Department Sample (NEDS); 2011. [Google Scholar]
- 22.American College of Surgeons. National Trauma Data Standard: Data Dictionary. 2015 [Google Scholar]
- 23.Ingram DD, Franco SJ. NCHS Urban–Rural Classification Scheme for Counties. 2014 [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Matrix of E-code groupings. 2011 [Google Scholar]
- 25.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 27.United States Census Bureau. Census Regions and Divisions of the United States. 1985 [Google Scholar]
- 28.Sorenson SB. Gender disparities in injury mortality: consistent, persistent, and larger than you’d think. Am J Public Health. 2011;101(Suppl 1):S353–8. doi: 10.2105/AJPH.2010.300029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Downing SR, Oyetunji TA, Greene WR, Jenifer J, Rogers SO, Jr, Haider AH, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? J Trauma. 2011;70:130–4. doi: 10.1097/TA.0b013e3182032b34. discussion 4–5. [DOI] [PubMed] [Google Scholar]
- 30.Swaroop M, Straus DC, Agubuzu O, Esposito TJ, Schermer CR, Crandall ML. Pre-hospital transport times and survival for Hypotensive patients with penetrating thoracic trauma. Journal of emergencies, trauma, and shock. 2013;6:16–20. doi: 10.4103/0974-2700.106320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El-Menyar A, El-Hennawy H, Al-Thani H, Asim M, Abdelrahman H, Zarour A, et al. Traumatic injury among females: does gender matter? J Trauma Manag Outcomes. 2014;8:8. doi: 10.1186/1752-2897-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban Level I trauma center. Ann Emerg Med. 2013;61:167–74. doi: 10.1016/j.annemergmed.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 33.Lehmann R, Beekley A, Casey L, Salim A, Martin M. The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. American journal of surgery. 2009;197:571–4. doi: 10.1016/j.amjsurg.2008.12.037. discussion 4–5. [DOI] [PubMed] [Google Scholar]
- 34.Tohira H, Jacobs I, Mountain D, Gibson N, Yeo A. Systematic review of predictive performance of injury severity scoring tools. Scandinavian journal of trauma, resuscitation and emergency medicine. 2012;20:63. doi: 10.1186/1757-7241-20-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thompson HJ, Rivara FP, Nathens A, Wang J, Jurkovich GJ, Mackenzie EJ. Development and validation of the mortality risk for trauma comorbidity index. Annals of surgery. 2010;252:370–5. doi: 10.1097/SLA.0b013e3181df03d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bamvita JM, Bergeron E, Lavoie A, Ratte S, Clas D. The impact of premorbid conditions on temporal pattern and location of adult blunt trauma hospital deaths. J Trauma. 2007;63:135–41. doi: 10.1097/TA.0b013e318068651d. [DOI] [PubMed] [Google Scholar]
- 37.Govindarajan P, Lin L, Landman A, McMullan JT, McNally BF, Crouch AJ, et al. Practice variability among the EMS systems participating in Cardiac Arrest Registry to Enhance Survival (CARES) Resuscitation. 2012;83:76–80. doi: 10.1016/j.resuscitation.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 38.MacKenzie EJ, Carlini AR. Characterizing Local EMS Systems. Washington, DC: National Highway Transportation Safety Board; 2013. [Google Scholar]
- 39.Whitney JR, Werner S, Wilson S, Sanddal N, Conditt V, Sale P, et al. Rural trauma and emergency medical service challenges in a sample of Western States. Journal of trauma nursing : the official journal of the Society of Trauma Nurses. 2010;17:158–62. doi: 10.1097/JTN.0b013e3181f52258. [DOI] [PubMed] [Google Scholar]
- 40.Baker SP, Whitfield RA, O’Neill B. Geographic variations in mortality from motor vehicle crashes. N Engl J Med. 1987;316:1384–7. doi: 10.1056/NEJM198705283162206. [DOI] [PubMed] [Google Scholar]
- 41.Rogers FB, Rittenhouse KJ, Gross BW. The golden hour in trauma: dogma or medical folklore? Injury. 2015;46:525–7. doi: 10.1016/j.injury.2014.08.043. [DOI] [PubMed] [Google Scholar]
- 42.Eachempati SR, Robb T, Ivatury RR, Hydo LJ, Barie PS. Factors associated with mortality in patients with penetrating abdominal vascular trauma. The Journal of surgical research. 2002;108:222–6. doi: 10.1006/jsre.2002.6543. [DOI] [PubMed] [Google Scholar]
- 43.Pons PT, Markovchick VJ. Eight minutes or less: does the ambulance response time guideline impact trauma patient outcome? J Emerg Med. 2002;23:43–8. doi: 10.1016/s0736-4679(02)00460-2. [DOI] [PubMed] [Google Scholar]
- 44.Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, et al. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55:235–46. e4. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lerner EB, Billittier AJ, Dorn JM, Wu YW. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10:949–54. doi: 10.1111/j.1553-2712.2003.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 46.Blackwell TH, Kaufman JS. Response time effectiveness: comparison of response time and survival in an urban emergency medical services system. Acad Emerg Med. 2002;9:288–95. doi: 10.1111/j.1553-2712.2002.tb01321.x. [DOI] [PubMed] [Google Scholar]
- 47.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? The American journal of emergency medicine. 1995;13:133–5. doi: 10.1016/0735-6757(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 48.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34:252–61. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 49.Dinh MM, Bein K, Roncal S, Byrne CM, Petchell J, Brennan J. Redefining the golden hour for severe head injury in an urban setting: the effect of prehospital arrival times on patient outcomes. Injury. 2013;44:606–10. doi: 10.1016/j.injury.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 50.Pons PT, Haukoos JS, Bludworth W, Cribley T, Pons KA, Markovchick VJ. Paramedic response time: does it affect patient survival? Acad Emerg Med. 2005;12:594–600. doi: 10.1197/j.aem.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 51.Clark DE, Winchell RJ, Betensky RA. Estimating the effect of emergency care on early survival after traffic crashes. Accident; analysis and prevention. 2013;60:141–7. doi: 10.1016/j.aap.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 52.Tien HC, Jung V, Pinto R, Mainprize T, Scales DC, Rizoli SB. Reducing time-to-treatment decreases mortality of trauma patients with acute subdural hematoma. Annals of surgery. 2011;253:1178–83. doi: 10.1097/SLA.0b013e318217e339. [DOI] [PubMed] [Google Scholar]
- 53.Winkleby MA, Cubbin C. Influence of individual and neighbourhood socioeconomic status on mortality among black, Mexican-American, and white women and men in the United States. J Epidemiol Community Health. 2003;57:444–52. doi: 10.1136/jech.57.6.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54:517–24. doi: 10.1136/jech.54.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ali MT, Hui X, Hashmi ZG, Dhiman N, Scott VK, Efron DT, et al. Socioeconomic disparity in inpatient mortality after traumatic injury in adults. Surgery. 2013;154:461–7. doi: 10.1016/j.surg.2013.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Center NTA. National EMS Database. NEMSIS Research Dataset. v.2.2.1. 2014 [Google Scholar]
- 57.American College of Surgeons. National Trauma Data Bank. 2015 [Google Scholar]
- 58.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj Prev. 2015;21:325–30. doi: 10.1136/injuryprev-2014-041524. [DOI] [PubMed] [Google Scholar]
- 59.Rotondo MF, Cribari C, Smith RS, Williams C, Clemency J, Lozada M, et al. Resources for the Optimal Care of the Injured Patient: 2014. 2014 [Google Scholar]