Abstract
Purpose
Many Americans continue to smoke, increasing their risk of disease and premature death. Both telephone-based counseling and in-person tobacco cessation classes may improve access for smokers seeking convenient support to quit. Little research has assessed whether such programs are effective in real-world clinical populations.
Design
Retrospective cohort study comparing wellness coaching participants with two groups of controls.
Setting
Kaiser Permanente, Northern California (KPNC), a large integrated health care delivery system.
Subjects
241 patients who participated in telephonic tobacco cessation coaching from 1/1/2011–3/31/2012, and two control groups: propensity-score matched controls, and controls who participated in a tobacco cessation class during the same period. Wellness coaching participants received an average of two motivational interviewing based coaching sessions that engage the patient, evoke their reason to consider quitting and help them establish a quit plan.
Measures
Self-reported quitting of tobacco and fills of tobacco cessation medications within 12 months of follow-up.
Analysis
Logistic regressions adjusting for age, gender, race/ethnicity, and primary language.
Results
After adjusting for confounders, tobacco quit rates were higher among coaching participants vs. matched controls (31% vs. 23%, P<0.001) and comparable to class attendees (31% vs. 29%, P=0.28). Coaching participants and class attendees filled tobacco-cessation prescriptions at a higher rate (47% for both) than matched controls (6%, P<0.001).
Conclusions
Telephonic wellness coaching was as effective as in-person classes and was associated with higher rates of quitting compared to no treatment. The telephonic modality may increase convenience and scalability for health care systems looking to reduce tobacco use and improve health.
Keywords: tobacco cessation, wellness coaching, motivational interviewing, program evaluation
Purpose
Tobacco use is a major cause of premature death worldwide.1 While adult tobacco use rates have declined steadily in the United States for the past 60 years, the annual burden of smoking-attributable mortality in the United States has remained above 400,000 for more than a decade, with millions more living with smoking-related diseases.2 Tobacco use rates have stubbornly persisted at a level of approximately 20% of all U.S. adults over the past half century, with rates sharply higher among the poor, the least educated, and people who have coexisting mental health conditions or who abuse alcohol or other substances.3,4 On a global level, in 2013, the World Health Organization called for a 30% relative reduction in prevalence of tobacco use in persons aged 15+ years by 2025. This ambitious goal is vital to saving years of life for millions of smokers. Those who have smoked cigarettes since early adulthood but stop at 30, 40, or 50 years of age gain about 10, 9, and 6 years of life expectancy, respectively.5
Tobacco cessation programs that combine both access to pharmacological treatments and behavioral counseling have become the gold standard in the health care industry.6 However, research suggests that many patients do not participate in these types of programs,7,8 likely due to health system barriers such as the costs of providing these services to the broader population, and patient barriers such as time and access concerns that limit ability to participate. Services are needed outside of standard clinical office visits, given that—while clinicians commonly advise smokers to quit—few provide counseling or discuss the behavioral components involved in quitting.9 Indeed, while about 70% of smokers visit a primary care physician each year, only about 30% report that they leave these visits having received evidence-based counseling and medication for tobacco cessation.10 Therefore, the current challenge is to provide tobacco users with convenient, affordable access to evidence-based programs that are scalable for large populations.7,8
Providing access to these types of programs through telephone-based quit tobacco programs (e.g., quit lines) which do not require in-person participation has been shown to be effective in supporting tobacco users to quit.11 In this modality, counselors work directly with participants over the phone, which eliminates geographical access and transportation barriers. However, the actual counseling and program content likely varies among telephonic programs based on such factors as inclusion of pharmacological treatments, number of phone counseling sessions offered, and counselors’ training and educational background. Programs where counselors utilize motivational interviewing (MI) have been shown to be more effective than other more directive or educational-based interventions.12 However, very few studies have examined these programs when implemented within real-world clinical settings and offered broadly to insured populations; the effectiveness of such programs on rates of pharmacologic treatment use and tobacco cessation is unknown.
The purpose of this study was to compare the effectiveness of MI-based telephonic tobacco cessation wellness coaching to two groups, smoking cessation class participants and those who did not receive either (controls). The study was conducted in the real world health care delivery setting of Kaiser Permanente Northern California (KPNC) with coaches trained in MI.
Methods
Design
We conducted retrospective cohort analyses of the effect of wellness coaching participation on tobacco-use outcomes. The first analysis aimed to contrast outcomes between patients who received MI-based telephonic wellness coaching (exposed group) and patients who did not (control group). Patients were selected for the control group using propensity score matching described below. The second analysis aimed to contrast outcomes between patients that participated in telephonic wellness coaching (exposed group) and patients who attended a tobacco cessation class during the same period (control group).
Sample
Our study populations were derived from patients within KPNC, an integrated medical care delivery system covering an enrolled population of 3.3 million members. Patients were considered exposed to wellness coaching if they initiated coaching for tobacco cessation between January 2011 and March 2012. Of the 2,905 members who initiated Wellness Coaching during the study period, 321 members discussed quitting tobacco during their first call. A total of 241 (75%) of those members had valid outcome and covariate data available and were included in this study (Table 1). Wellness coaching participants were majority female (66%) with a primary language of English (97%), which was consistent with matched control group (66% female, 96% English speaking) and the class attendees (58% female, 99% English speaking). The majority of participants in the exposed and controls groups were white (59%, 59%, and 65% respectively). The mean age was between 48–49 years old for all groups. There was no significant difference between groups on the percent who were former tobacco users at baseline (8%, 10%, and 9%, respectively). Almost half (46.5%) of the 241 Wellness Coaching participants were referred to the program by their primary care physician, and 24.5% were referred to the program by their KP facility; the referral method was unknown for approximately 1/4 of the patients (data not shown.)
Table 1.
Demographic Characteristics for Wellness Coaching Participants, Matched Controls and Class Attendees
| Wellness coaching participants (N=241) |
Matched controls (N=4,820) |
Class attendees (N=4,535) |
|||
|---|---|---|---|---|---|
| no (%) | no (%) | P value* | no (%) | P value* | |
| Age, mean (SD) | 49 (14) | 48 (16) | .25 | 49 (13) | .79 |
| Female | 159 (66%) | 2162 (66%) | .91 | 2644 (58%) | .02 |
| Race/ethnicity | .99 | <0.001 | |||
| Asian, American Indian, Alaskan or Hawaiian native, Pacific Islander |
5 (2%) | 91 (2%) | 307 (7%) | ||
| Black or African American |
44 (18%) | 885 (18%) | 684 (15%) | ||
| Hispanic | 42 (17%) | 835 (17%) | 408 (9%) | ||
| White | 143 (59%) | 2850 (59%) | 2959 (65%) | ||
| Unknown or not reported | 7 (3%) | 159 (3%) | 177 (4%) | ||
| Primary language | .75 | <0.001 | |||
| English | 233 (97%) | 4641 (96%) | 4499 (99%) | ||
| Spanish | 8 (3%) | 179 (4%) | 36 (1%) | ||
| Former tobacco users at baseline |
20 (8%) | 490 (10%) | .35 | 417 (9%) | .64 |
Determined by a χ2 test for the difference in proportions or a t test for the difference in means between the wellness coaching participants and the control group.
Coaching participants were excluded if their tobacco-use status was not recorded in the EMR in the year before and the year after their index date, which was defined as the date of their first coaching session. We also excluded members who did not have all potential confounding variables measured or whose primary language was not English or Spanish.
We used propensity score matching to select controls from the population of KPNC members who had been current tobacco users at any point in the two years prior to eligibility. We required that controls be in the age range of the coaching participants (18–81 years) and have available all the variables needed for the propensity score model. Controls who participated in wellness coaching prior to April 1, 2013 or whose primary language was not English or Spanish were excluded. Because coaching participants enrolled over five quarters (quarter 1, 2011 to quarter 1, 2012) and the propensity score model included several time-varying measures, eligibility for the controls was determined for each quarter separately. Matches were only considered if the control was eligible for the quarter during which the coaching participant began wellness coaching. Propensity scores, i.e. the probability of participating in wellness coaching, were calculated from a logistic regression model with the following variables: age, gender, race/ethnicity, primary language, number of primary care visits in previous year, quarter, KPNC service area (defined geographical area), baseline tobacco status (the most recent tobacco-use status recorded prior to the quarter), and Diagnostic Cost Group risk score (DxCG, an empirical, individual-level measure of financial resource use arising from patient morbidity; Verisk Health, Inc., Waltham, MA). The index date for the controls was defined as the first day of the quarter for which they were matched.
The second control group was comprised of KPNC members who attended a single or multi-session tobacco cessation class between January 2011 and March 2012. The class provides information about nicotine addiction, tobacco cessation medications and developing a quit plan. The curricula is delivered through both didactic and experiential methods. Participants are encouraged to set a quit date, identify triggers and set up a support system. In addition, participants receive information regarding additional resources such as behavioral therapy and chemical dependence programs. The single session workshop is 3 hours in length while the multi-session series meets 90 minutes once per week for 8 weeks. Instructors assess patient’s interest in using tobacco cessation medications and coordinate care with their primary care physician to request prescriptions electronically. There are no additional fees or copays for KPNC members to attend any of the tobacco cessation classes. While the EMR does capture whether a member attended a class, it does not currently capture the exact number of sessions attended. We excluded class attendees whose EMR did not have a recorded tobacco-use status in the year before and year after their index date, which was defined as the date of their first tobacco cessation class in the study period. Class attendees who were outside the 18–81 year age range, had been exposed to wellness coaching prior to April 1, 2013, or whose primary language was not English or Spanish were also excluded.
Measures
The primary outcome was the last tobacco-use status in the year following the index date. Members were categorized as being current or former tobacco users. During each office visit, KPNC members’ tobacco-use status is assessed and documented in the EMR. While no cotinine plasma samples were collected to verify participants’ self-reported tobacco-use, the reliability of self-reported tobacco use is relatively high.13
The secondary outcome was whether the member collected a tobacco cessation medication (i.e., nicotine patches, lozenges, gums; bupropion [Zyban]; varenicline) at a KPNC pharmacy in the year following the index date.14 While we cannot confirm all medications were filled within the KPNC delivery system, it is unlikely that members would obtain prescription medications from other pharmacies given most have KPNC drug benefits (95%).15 In addition, this benefit allows KPNC members discounted prices on over-the-counter tobacco medications as well.
Intervention
The Wellness Coaching Center opened in January 2010 to support patients with five primary lifestyle changes: tobacco use cessation, more healthful eating, increased physical activity, weight management, and stress reduction.16,17 Wellness coaching is a covered benefit offered at no cost to the approximately 2 million adult KPNC members who are made aware of the program through referrals by KPNC providers and staff, partnerships with employers, and direct patient outreach. The program is staffed by wellness coaches who are Master’s level clinical health educators extensively trained in MI, a patient-centered counseling style for addressing the common problem of ambivalence about change.18 MI has been effective for both weight loss and substance abuse, even in brief interventions.19, 20, 21 Through collaborative conversations, wellness coaches evoke member’s internal motivation, affirm individuals’ autonomy and attempts to change, as well as offer tailored recommendations as appropriate.
Patients participate by first scheduling an appointment with a wellness coach, and coaches call patients at a designated time. A typical coaching engagement consists of one initial session (30 minutes) and one or more briefer follow-up contacts (10 to15 minutes). Although, participants are offered up to four coaching sessions per calendar year, the average number of encounters per member for tobacco cessation is two. The sessions are tailored for the patient based on current readiness and past attempts at quitting tobacco, as well as current interest in utilization of tobacco cessation medications. In addition to setting a quit date, clients are supported through the process of preparing to quit, eliciting support from others, and planning for potential relapse and triggers. Wellness coaches document the sessions in the member’s electronic medical record (EMR) and are able to directly coordinate care with KPNC physicians to request prescriptions electronically for tobacco cessation medications. Per protocol, participants are not enrolled in multiple cessation programs simultaneously, however coaches can refer members to other non-tobacco related KPNC services such as behavioral health and online health education programs.
In addition, the wellness coaching program has an extensive quality oversight process. All calls are recorded, and coaches review calls monthly with a senior quality consultant. Senior quality consultants are rigorously trained in MI and assess calls for fidelity to the coaching model. During monthly “skill building” meetings with a senior quality consultant, wellness coaches receive feedback on strengths, and collaboratively identify opportunities for improvement.
Analysis
In the comparison with propensity-scored matched controls, we aimed to estimate the average treatment effect on the treated (ATET) defined as the mean difference between outcomes from patients who participated in wellness coaching and their outcomes had they not participated in wellness coaching. To estimate this effect, each wellness coaching participant was matched to 20 controls (without replacement) using propensity score estimates and a nearest-neighbor algorithm.22, 23 In the comparison with class attendees, we estimated the average treatment effect (ATE) using an estimator of the average outcome difference between the exposed and control groups. To see if differences in groups remained after adjusting for confounders, we ran logistic regressions of the outcomes which included age, gender, race/ethnicity, primary language, tobacco use at baseline and tobacco medication fill at baseline. We also examined whether there were differences between the baseline and follow-up periods (within the three groups separately) by running logistic regressions of the outcomes which included an indicator for the time period and the same confounders as above. Pearson chi-square tests of independence and two sample t tests were used to compare the baseline characteristics and outcomes of the wellness coaching participants and the sets of control groups separately. All tests were two-sided with an alpha level of 0.05 to determine significance. We used SAS software version 9.3 (SAS Institute Inc., Cary, North Carolina) for all data management and analysis. The KPNC Institutional Review Board approved this study.
Results
Of the 2,905 members who initiated Wellness Coaching during the study period, 321 members discussed quitting tobacco during their first call. A total of 241 (75%) of those members had valid outcome and covariate data available and were included in this study (Table 1). Wellness coaching participants were majority female (66%) with a primary language of English (97%), which was consistent with matched control group (66% female, 96% English speaking) and the class attendees (58% female, 99% English speaking). The majority of participants in all three groups were white (59%, 59%, and 65% respectively). The mean age was between 48–49 years old for all groups. There was no significant difference between groups on the percent who were former tobacco users at baseline (8%, 10%, and 9%, respectively).
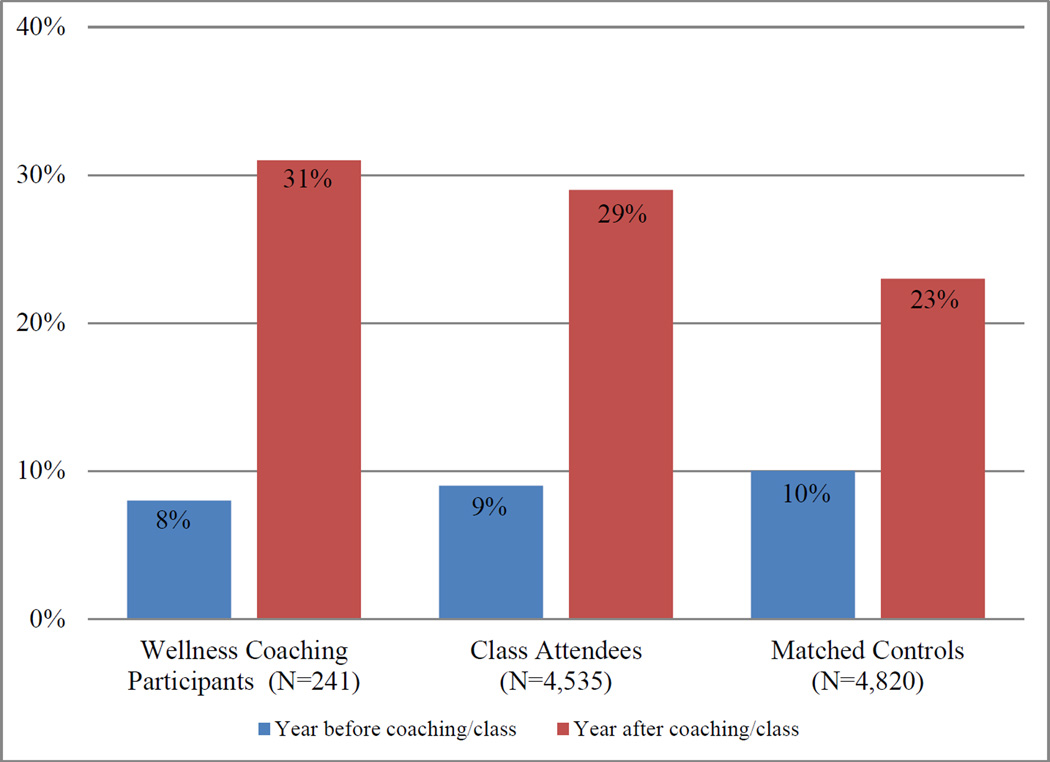
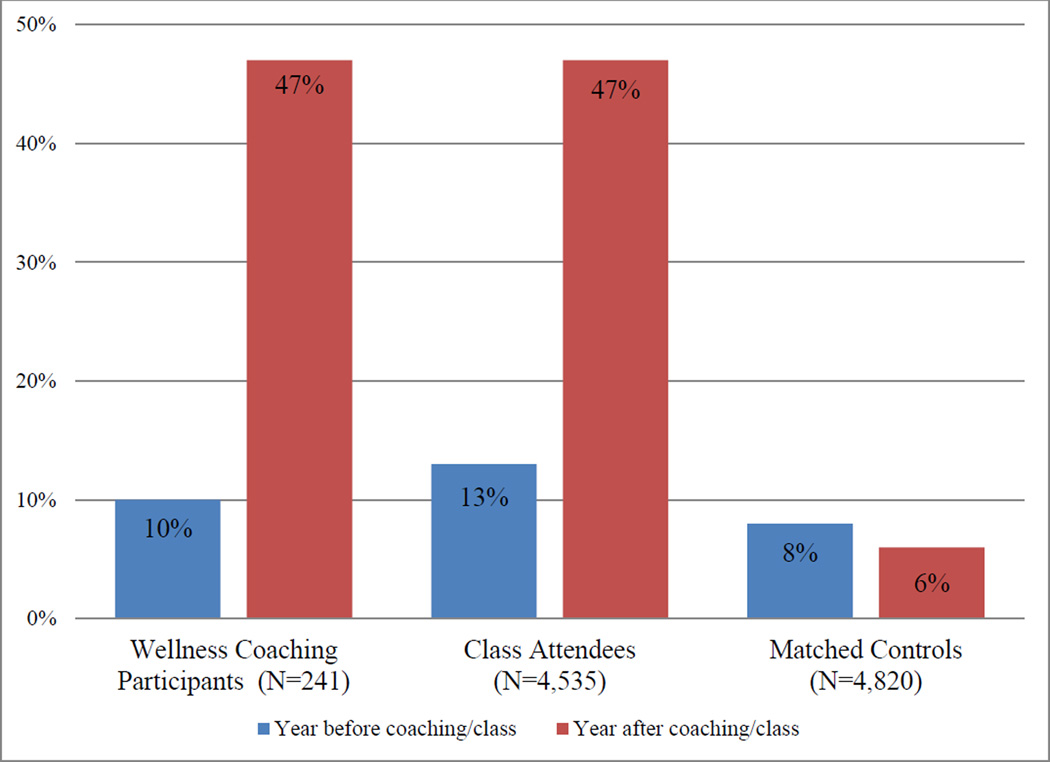
In comparing wellness coaching participants with the matched control group, both tobacco cessation quit rates (31% vs. 23%, P<0.001) and tobacco cessation medications fill rates (47% vs. 6%, P<0.001) were significantly higher in the wellness coaching group after adjusting for potential confounders (Figs. 1 and 2). Whereas, in comparing wellness coaching participants with class attendees, quit rates (31% vs. 29%, P=0.28) and tobacco cessation medication fill rates (47% vs. 47%, P=0.93) were not significantly different (Figs. 1 and 2).
Figure 1. Percent of Former Tobacco Users Among Wellness Coaching Participants, Matched Controls, and Class Attendees*†.
* After adjusting for age, gender, race/ethnicity, primary language, tobacco use at baseline, and tobacco medication fill at baseline, the quit rate among wellness coaching participants at follow-up (31%) was statistically different from that of the matched controls (23%, P<0.001) but not that of the class attendees (29%, P=0.28).
† After adjusting for age, gender, race/ethnicity, primary language, and tobacco medication fill at baseline, there was a significant increase in the quit rate between baseline and follow-up within each group: wellness coaching participants (23%, P<0.001), class attendees (20%, P<0.001), and matched controls (13%, P<0.001).
Figure 2. Percent Who Filled a Tobacco Cessation Medication Among Wellness Coaching Participants, Matched Controls, and Class Attendees*†.
* After adjusting for age, gender, race/ethnicity, primary language, tobacco use at baseline, and tobacco medication fill at baseline, the medication fill-rate among wellness coaching participants at follow-up (47%) was statistically different from that of the matched controls (6%, P<0.001) but was not statistically different from that of the class attendees (47%, P=0.93).
† After adjusting for age, gender, race/ethnicity, primary language, and tobacco use at baseline, there was a significant difference in the medication fill rate between baseline and follow-up for the wellness coaching participants (37%, P<0.001), class attendees (34%, P<0.001), and matched controls (−2%, P<0.001).
In addition, we performed an exploratory sensitivity analysis to determine if different demographic groups had more success with the wellness coaching program or the in-person tobacco cessation class. Stratified by the program type, we ran logistic regression models predicting quitting tobacco with the following covariates: age, gender, race/ethnicity, and primary language. For the wellness coaching participants (n = 241), the only significant predictor of success was Hispanic ethnicity (OR 2.22, referent group White, P = .04). For the class attendees (n = 4,535), greater age was positively associated (OR 1.01 per 1 year, P < .01) and being African American was negatively associated (OR 0.78, referent group White, P = .01) with quitting tobacco (data not shown.)
Discussion
This study was designed to evaluate the effectiveness of a telephonic tobacco cessation wellness coaching program using motivational interviewing, conducted in the real world health care delivery setting of KPNC. Among participants, we found a significantly higher quit rate and medication fill rate compared to a group of matched controls who did not engage in wellness coaching. Telephonic-based coaching services such as the wellness coaching program may help to provide effective tobacco cessation support to the broader population of tobacco users seeking help with quitting, and reduce the rates of tobacco-related complications and mortality. The use of tobacco cessation medications as part of cessation therapy has been documented to significantly increase the rates of long-term tobacco abstinence.10 Our finding that tobacco cessation medication use is higher in patients who participated in wellness coaching compared with matched controls suggests that telephone-based tobacco cessation services can increase the use of these evidence-based therapies.
Our study found a comparable quit rate and tobacco cessation medication fill rate between those who participated in wellness coaching and tobacco cessation classes. In-person classes have some advantages, such as supportive group dynamics and interactive activities. However, the phone coaching program opens up less time intensive options for those unable to travel or who cannot take time to attend in-person sessions during the specific time the class is being offered. Given the common use of mobile phones today, this service meets the needs of those who prefer to receive counseling by phone. In addition, it offers a level of anonymity that a class environment cannot provide.
As discussed, tobacco-use rates continue to persist, and are highest among those least likely to be able to afford services.4 There is an urgent need for convenient, effective and affordable tobacco-cessation interventions conducted outside of the medical office and classroom that are both sustainable and can be used widely across populations. Wellness coaching is one such example and is made available at no additional cost to all KPNC members.
The program utilizes quality control measures to enhance the consistency of services provided. All calls are recorded and a senior quality consultant performs regular call reviews with coaches, providing feedback on strengths and collaboratively identifying opportunities for improvement. The coaching model is rooted in MI principles which have been shown to be more effective than other more directive or educational-based interventions.21 The present results suggest that providing telephonic wellness coaching based on MI within an integrated delivery system that facilitates safe and quick access to tobacco cessation medications is an effective approach to reducing the rate of tobacco use. The success of this program supports the need for a new integrated model of care to provide accessible, evidence-based tobacco cessation services to patients.
Limitations
This study has several limitations worth noting. We relied on tobacco use status recorded in the EMR, using the last observation of self-reported quit status in the follow-up period; it is possible that patient’s tobacco-use status may have changed between the last visit and the end of the follow up period. In addition, this study is not a randomized control trial, therefore we were unable to offer pharmacological help to some and not others. There may be differences in motivation between patients who selected wellness coaching versus in-person classes (versus no health plan-based intervention) that we could not assess or control for in these analyses though we did find similar quit rates. We have insufficient data on the varying extent of participation in both the class and coaching participants, which may have impacted cessation outcomes. While some patients are referred by their physician, participation in wellness coaching is voluntary. This study did not assess whether patients sustained their efforts to quit tobacco over time; future research to test the endurance of this program on maintained quit rates is desirable. Still, given the tendency for tobacco users to require multiple quit attempts to ultimately succeed in maintaining tobacco abstinence,24 even quit attempts that are not maintained long-term can be considered a desirable outcome of the program. While this program was made available to all KPNC members who currently use tobacco (approximately 10% of the KPNC population25), a relatively small percentage of these patients took advantage of the program during our observation window. While smoking prevalence among KPNC members is similar to the smoking rates across California (13% in 2012), these rates are lower than the general U.S. population.26 Future research should assess which methods are most effective at enrolling patients in the program who may benefit most from wellness coaching services.
Conclusion
MI-based telephonic tobacco cessation wellness coaching was as effective in helping tobacco users quit as in-person classes and resulted in significantly higher rates of quitting versus patients who did not participate in a health plan-based tobacco cessation program. Future research on the cost-effectiveness of both telephonic tobacco cessation coaching and in-person programs would be valuable to further compare each resource.
The usefulness of telephonic coaching applies to settings where tobacco cessation classes are difficult to provide and is helpful for individuals who prefer a confidential one-on-one patient-centered counseling approach. The scalability of this evidence-based program makes it an attractive option for health care systems looking to drive down tobacco use and ultimately improve the health of the greater population.
So What? Implications for Health Promotion Practitioners and Researchers
-
What is already known on this topic?
Few studies have examined the effectiveness of telephone-based tobacco cessation coaching implemented in real-world clinical practice.
-
What does this article add?
This article demonstrates that telephone-based tobacco cessation coaching grounded in motivational interviewing techniques was equally as effective at helping patients quit tobacco use and fill tobacco cessation medications as in-person classes and significantly more effective compared to no intervention.
-
What are the implications for health promotion practice and research?
Telephone-based tobacco cessation programs can be an important tool for health promotion practitioners seeking to reduce tobacco use and improve the health of the population. Future research should examine what patients might benefit most from telephonic tobacco cessation coaching, and the most effective methods for enrolling patients and disseminating these programs widely into health care practice.
Acknowledgments
This study was funded by the Centers for Disease Control and the NIDDK [U58 DP002721]. Drs. Ferrara and Schmittdiel were also supported by the Health Delivery Systems Center for Diabetes Translational Research (CDTR) [NIDDK grant 1P30-DK092924]. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding organizations. The authors would like to gratefully acknowledge the editorial assistance of Eleanor Vincent and Karen R. Hansen.
References
- 1.Jha P. Avoidable global cancer deaths and total deaths from smoking. Nat Rev Cancer. 2009;9:655–664. doi: 10.1038/nrc2703. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. The health consequences of smoking —50 years of progress: A report of the Surgeon General. [Accessed August 26, 2014];2014 http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf.
- 3.Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. [Accessed August 26, 2014]; http://www.cdc.gov/nchs/data/hus/hus09.pdf.
- 4.Fiore MC, Baker TB. Clinical practice. Treating smokers in the health care setting. N Engl J Med. 2011;365:1222–1231. doi: 10.1056/NEJMcp1101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014;370:60–68. doi: 10.1056/NEJMra1308383. [DOI] [PubMed] [Google Scholar]
- 6.A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service report. The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. JAMA. 2000;283:3244–3254. [PubMed] [Google Scholar]
- 7.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD001292.pub2. CD001292. [DOI] [PubMed] [Google Scholar]
- 8.Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD001007.pub2. CD001007. [DOI] [PubMed] [Google Scholar]
- 9.Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. Am J Prev Med. 2008;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 10.Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. May, [Google Scholar]
- 11.Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;8 doi: 10.1002/14651858.CD002850.pub3. CD002850. [DOI] [PubMed] [Google Scholar]
- 12.Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD006936.pub2. CD006936. [DOI] [PubMed] [Google Scholar]
- 13.From Attebring M, Herlitz J, Berdnt AK, Karlsson T, Hjalmarson A. Are patients truthful about their smoking habits? A validation of self-report about smoking cessation with biochemical markers of smoking activity amongst patients with ischaemic heart disease. J Intern Med. 2001;249:145–151. doi: 10.1046/j.1365-2796.2001.00770.x. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein A, Gee S, Mirkin R. Tobacco dependence program: a multifaceted systems approach to reducing tobacco use among kaiser permanente members in northern california. Perm J. 2005;9:9–18. doi: 10.7812/tpp/04-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmittdiel JA, Karter AJ, Dyer WT, Chan J, Duru OK. Safety and effectiveness of mail order pharmacy use in diabetes. Am J Manag Care. 2013;19:882–887. [PMC free article] [PubMed] [Google Scholar]
- 16.Schmittdiel JA, Brown SD, Neugebauer R, et al. Health-plan and employer-based wellness programs to reduce diabetes risk: The Kaiser Permanente Northern California NEXT-D Study. Prev Chronic Dis. 2013;10:E15. doi: 10.5888/pcd10.120146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams SR, Goler NC, Sanna RS, et al. Patient satisfaction and perceived success with a telephonic health coaching program: the Natural Experiments for Translation in Diabetes (NEXT-D) Study, Northern California, 2011. Prev Chronic Dis. 2013;10:E179. doi: 10.5888/pcd10.130116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller WR, Rollnick S. Motivational Interviewing, Third Edition: Helping People Change (Applications of Motivational Interviewing) Third. New York, NY: The Guilford Press; 2012. [Google Scholar]
- 19.Butler C, Rollnick S, Cohen D, Bachmann I, Stott N. Motivational consulting versus brief advice for smokers in general practice: a randomized trial. Br J Gen Pract. 1999;49:611–616. [Google Scholar]
- 20.Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]
- 21.Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- 22.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 23.Coca-Perraillon M. Local and Global Optimal Propensity Score Matching. Boston, MA: Health Care Policy Department, Harvard Medical School; 2007. [Google Scholar]
- 24.U.S. Department of Health and Human Services. Women and smoking: a report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2001. [Accessed August 26, 2014]. http://www.cdc.gov/tobacco/data_statistics/sgr/2001/complete_report/index.htm. Published March 27, 2001. [PubMed] [Google Scholar]
- 25.Gordon NP. Highlights of results of the Kaiser Permanente Northern California 2011 Member Health Survey. Oakland, CA: Kaiser Permanente Northern California Division of Research; 2013. [Google Scholar]
- 26.California Department of Public Health. Health Equity Summit – Data Charts. [Accessed Date: August 26, 2014];2013 http://www.cdph.ca.gov/programs/tobacco/Pages/CTCPFactSheets.aspx. Updated July 7, 2014.