Abstract
Throughout Southeast Asia, repressive drug laws have resulted in high rates of imprisonment in people who inject drugs and people living with HIV (PLH), greatly magnifying the harm associated with HIV, tuberculosis, and addiction. We review findings from Malaysia's largest prison to describe the synergistic effects of HIV, tuberculosis, addiction, and incarceration that contribute to a‘perfect storm’of events challenging public and personal health and offer insights into innovative strategies to control these converging epidemics. The majority of PLH who are imprisoned in Malaysia are opioid dependent. Although promoted by official policy, evidence-based drug treatment is largely unavailable, contributing to rapid relapse and/or overdose after release. Similarly, HIV treatment in prisons and compulsory drug treatment centers is sometimes inadequate or absent. The prevalence of active tuberculosis is high, particularly in PLH, and over 80% of prisoners and prison personnel are latently infected. Mandatory HIV testing and subsequent segregation of HIV-infected prisoners increases the likelihood of tuberculosis acquisition and progression to active disease, enlarging the reservoir of infection for other prisoners. We discuss strategies to control these intersecting epidemics including screening linked to standardized treatment protocols for all three conditions, and effective transitional programs for released prisoners. For example, recently introduced evidence-based interventions in prisons like antiretroviral therapy (ART) to treat HIV, isoniazid preventive therapy to treat latent tuberculosis infection, and methadone maintenance to treat opioid dependence, have markedly improved clinical care and reduced mortality. Since introduction of these interventions in September 2012, all-cause and HIV-related mortality have decreased by 50.0% and 75.7% respectively. We discuss the further deployment of these interventions in Malaysian prisons.
Keywords: HIV, tuberculosis, opioid dependence, prisoners, mortality, healthcare
Introduction
In Asia, over 3.89 million people are currently detained in prisons and jails (Walmsley 2016) with an additional 235,000, perhaps more, held in compulsory drug detention centers (CDDCs) (Kamarulzaman and McBrayer 2015; Tanguay et al. 2015). Criminal justice settings are dynamic, with up to 30 million persons released from prisons worldwide each year (Kinner and Wang 2014). Incarceration rates in Asia (excluding China and India) increased 37.6% from 2000 to 2015, compared to a 17.5% increase in Asian national populations during the same period (Walmsley 2016). A key factor in the growth of prison populations in Southeast Asia has been the costly and mainly ineffective “War on Drugs” (Csete et al. 2016). In pursuit of a “drug free” Association of Southeast Asian Nations (ASEAN) by 2020, Member States have enacted some of the toughest drug laws in the world, including capital punishment for drug trafficking. Although mostly unsuccessful at reducing drug use (Crofts and Azim 2015), these laws have increased rates of imprisonment among people who inject drugs (PWID), many of whom are HIV-infected (Degenhardt et al. 2014; Mathers et al. 2008) and have significant co-morbidity (Csete et al. 2016), including substance use disorders and other mental illnesses (Zahari et al. 2010). These individuals, in turn, are at increased risk for HIV infection and concomitant opportunistic infections as a result of the immunosuppressant effects of HIV, including latent tuberculosis infection (LTBI) and rapid progression to active tuberculosis (TB). In Southeast Asia where HIV, TB, and addiction are syndemic, incarceration is also an independent risk factor for ART non-adherence through disruptions in care (Milloy et al. 2011), needle sharing and sexual risk behaviors that transmit HIV (Milloy et al. 2013), and reduced lifespan (Patterson 2013). Here, evidence from past and ongoing research is presented to address critical gaps and formulate key lessons for prevention and treatment of HIV, tuberculosis, and addiction within the Malaysian criminal justice system. We draw on our experiences in Malaysia, one of a few countries in Southeast Asia where HIV-related mortality, especially from TB, continues to increase despite reductions worldwide.
Substance use disorders, and especially drug injection, continue to play an important role in HIV transmission in Southeast Asia (Hser et al. 2016), including countries with expanding epidemics like Malaysia and Indonesia, which are included in 16 countries where prevalence of PWID, and HIV in PWID, are highest, yet prevention and treatment coverage including needle and syringe exchange programs (NSPs) and opioid agonist therapy (OAT) are mostly low (United Nations Office on Drugs and Crime 2014). Use of contaminated injection equipment by PWIDs provides an efficient vector for blood-borne infections, especially HIV and viral hepatitis. PWIDs are also at high risk for tuberculosis (TB), especially if HIV infected (Deiss et al. 2009). Asia has the world's highest TB burden (15% of the global total) and 16% of all HIV-infected TB cases globally (Joint United Nations Programme on HIV/AIDS 2013). Despite reductions in HIV incidence, morbidity and mortality (Joint United Nations Programme on HIV/AIDS (UNAIDS) 2014), such advances have not occurred similarly in PWID despite numerous evidence-based HIV prevention recommendations (Dutta et al. 2012; Joint United Nations Programme on HIV/AIDS (UNAIDS) 2014). It is increasingly recognized that law enforcement strategies have failed to curb drug use (Irwanto et al. 2015) and contribute greatly to the risk of injection-related HIV infection (Booth et al. 2013; Ti et al. 2014). Punitive drug policies including compulsory drug detention for PWID and the death penalty for drug trafficking, continue to be a direct barrier to evidence-based HIV prevention services for PWIDs in Southeast Asia, including access to needle and syringe programs (NSPs) and opioid agonist therapies (OAT) like methadone or buprenorphine (Irwanto et al. 2015; United Nations Office on Drugs and Crime 2014).
Repressive drug policies in many Asian countries have resulted in high rates of drug-related arrest, imprisonment of PWID and prison overcrowding, which have been counterproductive to HIV prevention and treatment (Jurgens et al. 2010). Although some risk behaviors decrease during incarceration, both HIV and hepatitis C virus (HCV) transmission related to unsafe drug injection continues to occur among prisoners and detainees (Dolan et al. 2015), often complicated by co-infection with TB (Biadglegne et al. 2015). Unfortunately, few criminal justice settings offer comprehensive prevention or treatment services in spite of international guidelines that urge wide-ranging public health measures, including provision of OAT (World Health Organization (WHO) 2014; World Health Organization (WHO) 2015c), sterile injection equipment (United Nations Office on Drugs and Crime (UNODC) 2010; United Nations Office on Drugs and Crime (UNODC) 2012; WHO/UNODC/UNAIDS 2007), and routine screening for TB (World Health Organization (WHO) 2000; World Health Organization (WHO) 2014). In both prisons and the community, interventions to prevent and treat HIV, HCV and TB in PWID are gravely underfunded, especially in many middle-income countries where large numbers of PWID live. Moreover, HIV and TB programs for PWID that were expanded with support from the Global Fund to Fight AIDS, TB and Malaria (GFATM) have lost funding due to changes in the fund's eligibility criteria. In this global context, we provide an overview of addiction, HIV, TB and the criminal justice system in Malaysia, a high middle-income country in Southeast Asia with an emerging economy and over 29.2 million people.
The HIV Epidemic in Malaysia
The HIV epidemic in Malaysia was initially concentrated in people who inject drugs (PWID), and HIV was therefore regarded by some public health officials and criminal justice authorities as a problem that would remain confined to PWID (Crofts and Azim 2015). HIV quickly spread along drug trafficking routes in Southeast Asia (Beyrer et al. 2000) and began to enter other high-risk populations through sexual transmission. Although HIV prevalence in the general population (<0.5%), indicates a concentrated epidemic similar to neighboring countries (United Nations Programme on HIV/AIDS 2014), much higher prevalence rates are observed in key populations including the estimated 205,000 (170,000-240,000) PWID (Degenhardt et al. 2014) of which 15.8% (95%CI: 12.5%-19.2%) are HIV infected (Bazazi et al. 2015a).
Malaysia has made significant progress in ensuring access to HIV testing. Of the estimated 105,000 (range: 91,000-110,000) people living with HIV (PLH) in Malaysia, (Ministry of Health 2015), most (88.1%) are already diagnosed, many as a result of mandatory HIV testing in criminal justice settings (Bazazi et al. 2015a). Yet only 21,700 (21.7%) of PLH received antiretroviral therapy (ART) in 2014 (United Nations Programme on HIV/AIDS 2014) and ART coverage in PWID fails to reach even 5% (Degenhardt et al. 2014; Wolfe et al. 2010), despite ART being free and fully subsidized by the Ministry of Health since 2005. Consequently, HIV-related mortality in Malaysia increased 20% from 2005 to 2013 (Joint United Nations Programme on HIV/AIDS (UNAIDS) 2014); one of the few countries in Asia where incidence has not stabilized or decreased (Joint United Nations Programme on HIV/AIDS 2013).
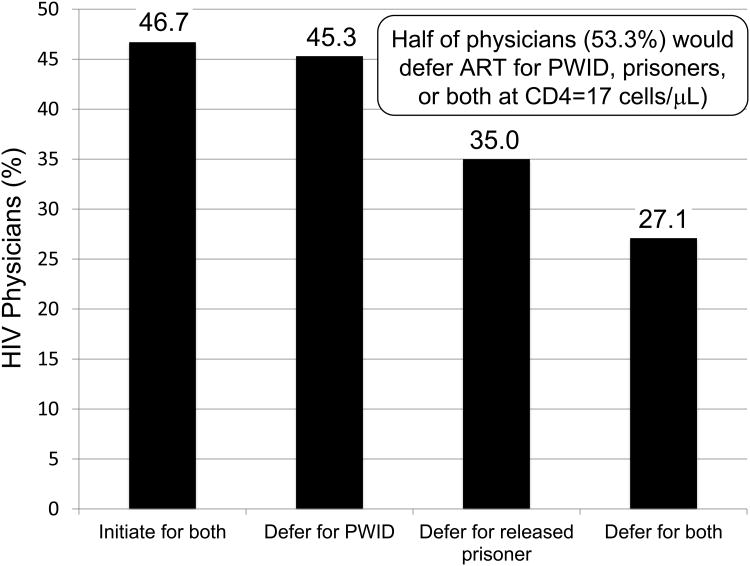
Our research with healthcare students and providers in Malaysia has generated compelling insights into the reasons behind Malaysia's HIV treatment gap. Recent surveys of medical students (Earnshaw et al. 2014; Jin et al. 2014) and physicians (Ferro et al., under review) have identified stigmatizing attitudes and intentions to discriminate against members of key populations, including PWID and released prisoners, which could substantially reduce the number of PLH (even those with severely compromised immunity) who access care or receive treatment. Figure 1 shows results from a study of 214 ART-prescribing Malaysian physicians. When presented with hypothetical case scenarios, over half (53.3%) indicated that they would defer ART for both PWID and released prisoners with markedly advanced (CD4=17cells/μL) HIV infection (Ferro et al., under review). Although the reasons why Malaysian physicians would defer ART for certain key populations are not clear, both stigmatizing attitudes toward prisoners and PWID and unsubstantiated concerns about ART adherence may play roles.
Figure 1.
Decisions by Malaysian HIV Physicians (n=214) to Defer ART for released prisoners, PWID, or both.
The Tuberculosis Epidemic in Malaysia
Globally, there has been a 47% reduction in tuberculosis-related mortality since 1990 and TB incidence has dropped by 18%, with nearly all improvements occurring since establishing the 2000 Millennium Development Goals (MDGs). Yet few countries have achieved MDGs for halving incidence, prevalence, and mortality by 2015 compared to 1990 figures. In 2014 alone, 9.6 million new TB cases were reported and TB killed ∼1.5 million (World Health Organization (WHO) 2015a). In 2014, there was an estimated 31,000 (25,000-37,000) new TB cases in Malaysia, translating to 103 cases per 100,000 population, a number that has increased over the past decade. Low levels of community engagement (<2%) to assist with TB treatment completion remains problematic, however, a case detection rate of 78% (World Health Organization 2015) is in line with WHO targets and TB mortality (10/100,000) is generally lower than in neighboring countries like Thailand (18/100,000), Vietnam (20/100,000) or Indonesia (49/100,000). TB mortality rates are much higher in PLH than in those without HIV, attesting to delayed identification and provision of early ART after TB diagnosis (World Health Organization (WHO) 2015a). Of the estimated 3,020 TB-related deaths in Malaysia, 620 (20%) were among the approximately 105,000 PLH, for a crude TB-related mortality rate of 590 deaths per 100,000 PLH compared to 8 deaths per 100,000 in the HIV-uninfected adult population.
The Criminal Justice System in Malaysia
Since 2000, Malaysia's drug policies have resulted in substantial increases (45%) in its incarceration rate from 116 to 171 per 100,000, with a total of 51,946 persons incarcerated in 39 prisons and pre-trial detention centers nation-wide (Walmsley 2016). Overcrowding is common with many facilities operating at or above designed occupancy capacity (Institute for Criminal Policy Research 2015). HIV testing is mandatory upon entry and HIV-infected prisoners (∼4.8% of sentenced prisoners) are segregated in special housing units, elevating the risk of explosive TB outbreaks (McLaughlin et al. 2003; Spradling et al. 2002; Valway et al. 1994), and reinforcing the stigmatization of HIV in the prison setting. Our team has documented high levels of psychiatric comorbidity (Zahari et al. 2010), substance use (Choi et al. 2010) and infectious diseases (Al-Darraji et al. 2014a; Al-Darraji et al. 2013; Bachireddy et al. 2011; Bick et al. 2013; Margolis et al. 2013; Wickersham et al. 2013b) in Malaysian prisoners, especially those with HIV, yet healthcare resources, including trained medical staff, are inadequate to address the health needs of prisoners.
In addition to drug laws that crowd PWID into jails and prisons, PWID in Malaysia are often forcibly placed into compulsory drug detention centers (CDDC) known as PUSPEN. These centers were enacted as part of the 1952 Dangerous Drugs Act and 1983 Drug Dependence (Treatment and Rehabilitation) Act, to detain people who test positive for drugs for a mandatory two-year period without due process and against their will (Gill 2010; Kamarulzaman 2009b). CDDCs in Malaysia and other Southeast Asian countries have been criticized for a variety of human rights violations (Amon et al. 2013; Amon et al. 2014; Pearshouse and Amon 2012), including indefinite detention, physical abuse and torture of detainees (Amon et al. 2013; Amon et al. 2014), and the denial or inadequate provision of medical care including evidence-based addiction treatment despite high prevalence of substance use disorders among detainees (Fu et al. 2012; Tanguay 2011; Tanguay et al. 2015). Despite international criticism, the number of CDDCs has continued to increase in East and Southeast Asia (Tanguay et al. 2015; UNODC 2010). By 2012, over 235,000 people were detained in over a thousand CDDCs (Lewis 2012), including 6,658 individuals detained in 28 CDDCs in Malaysia (Fu et al. 2012).
In 2012, however, a plan began to transform many CDDCs in Malaysia to voluntary treatment clinics that provide methadone treatment (Al-Darraji et al. 2014b) known as Cure & Care Clinics (Tanguay et al. 2015). Part of this transformation occurred as a result of research showing that CDDCs did not effectively treat addiction, with relapse rates exceeding 70% to 90% within a year (UNODC 2010), and did not provide healthcare (Fu et al. 2012). Consequently, several United Nations agencies called for their immediate closure (Amon et al. 2013; Amon et al. 2014) due to a lack of evidenced-based addiction treatment and medical care including for HIV and TB (Fu et al. 2012). Recent data from Malaysia suggest that transforming CDDCs to voluntary treatment centers is feasible, acceptable to patients, provides evidence-based treatments, and attracts patients who might not be involved with the criminal justice system (Ghani et al. 2015; Khan et al. 2015; Krishnan et al. 2016), and is markedly more effective in curbing relapse (Wegman et al., under review). Nevertheless, the question of whether to maintain CDDCs remains contentious and, for as long as the drug laws and policies remain as they are, criminalization will continue to be the mainstay of the response despite the progress of public health interventions in recent years.
Malaysia's Response to the Growing HIV Epidemic
Official data regarding HIV risk in new infections, although not fully substantiated, suggest that from 2002 to 2014, the total number of new HIV cases annually in Malaysia declined from 6,978 to 3,517 (United Nations Malaysia 2016), as did the proportion of new infections attributable to drug injection. Although a declining share of new HIV cases, PWID comprise the majority (66%) of all people living with HIV (Ministry of Health 2015), and remain an important focus of interventions to control the spread of HIV. In Malaysia, many PWID continue to engage in multiple high-risk behaviors that span diverse social networks (Bazazi et al. 2015a) although access to harm reduction services and opioid-agonist therapy (OAT) appears limited, and prevalence of non-fatal overdose is correspondingly high (Bazazi et al. 2015b). As a mobile population disproportionately subject to imprisonment, PWID face formidable barriers to HIV prevention and treatment services (Milloy et al. 2012), despite high prevalence of comorbidities including HCV- and alcohol-related liver disease (Larney et al. 2013), and AIDS- and non-AIDS related death (Mathers and Degenhardt 2014).
After decades of deploying a strictly punitive approach toward PWIDs, Malaysia introduced evidence-based harm reduction programs in 2002, including needle and syringe programs (NSPs) and opioid agonist therapies (OAT) with methadone (Kamarulzaman 2009a). Buprenorphine therapy was introduced in 2001, but its expansion was undermined by buprenorphine diversion and negative unanticipated health consequences (Bruce et al. 2008; Bruce et al. 2009). Supported primarily by the Ministry of Health and the Global Fund to Fight AIDS, Tuberculosis, and Malaria (GFATM), NSPs have been implemented in all states in peninsular Malaysia (Malaysian AIDS Council and Malaysian AIDS Foundation 2014). Methadone was expanded through a three-phase program within 1) addiction specialty clinics; 2) primary care clinics; and then 3) prisons (Noordin et al. 2008; Wickersham et al. 2013a; Wickersham et al. 2013b). The National Anti-Drug Agency (AADK), which is also responsible for CDDCs, also increased voluntary addiction treatment units that provide methadone in some former CDDCs (Al-Darraji et al. 2014b; Degenhardt et al. 2014; Fu et al. 2012; Ghani et al. 2015).
Nevertheless, many challenges and barriers remain in terms of sustaining and scaling up OAT for PWID. For example, law enforcement practices, including surveillance and arrest of clients receiving methadone and accessing NSPs in the community, are not aligned with the aims of harm reduction. Also, more work remains to be done to address persistent negative stereotypes, for example, the notion that methadone represents another form of addiction, and discrimination against patients enrolled in methadone treatment programs and NSPs (Beg et al. 2015). Among PWID in the community, low levels of treatment readiness and ongoing use of buprenorphine and methadone outside of treatment settings, could undermine acceptance for OAT despite awareness of its efficacy (Bachireddy et al. 2011; Vijay et al. 2015). Also, the market for synthetic drugs and amphetamine type stimulants in Asia is large and expanding (United Nations Office on Drugs and Crime 2013). OAT may not have the same benefits for persons who are exclusively dependent upon or engaged in risk behaviors related to methamphetamine, which can adversely influence ART adherence (Moore et al. 2012), and contribute to high-risk sexual behaviors and HIV transmission, especially among men who have sex with men (Hser et al. 2016).
Incarceration in People Who Inject Drugs in Malaysia
Malaysia's punitive drug laws have resulted in high rates of incarceration among PWIDs. In a sample of 461 PWID in Kuala Lumpur, 53.5% (95% CI: 48.9% - 58.0%) had a lifetime history of incarceration, and 61.5% (95% CI: 57.2% - 65.9%) had been detained in CDDCs. Within the previous 6 months, 44.1% (95%CI: 39.6-48.7) had been in jail, 13.9% (95% CI: 10.9% - 17.2%) had been to prison, and 3.1% (95% CI: 1.5-4.8%) had been detained in a CDDC (Bazazi et al. 2015b; Vijay et al. 2015). Incarceration of PWID (many of whom are HIV-infected and medically underserved) results in an ethical and legal mandate to provide necessary and decent care (Lines 2008) including the following evidence-based interventions: 1) access to condoms and deterrents to sexual assault; 2) needle and syringe programs; 3) bleach and decontamination strategies; and 4) OAT as part of addiction treatment (Jürgens et al. 2009; United Nations Office on Drugs and Crime (UNODC) 2012; United Nations Office on Drugs and Crime (UNODC) 2013).
Unfortunately, very few prisons offer comprehensive HIV prevention services, and even when they are offered, social and environmental conditions within prisons are often extremely counterproductive to treating HIV or addiction. For example, although OAT programs have been implemented in prisons in at least 29 countries (Larney and Dolan 2009), including Malaysia, addiction treatment services may reach only a small number of prisoners who need them. This is in part because methadone may be stigmatized within a prison subculture where drug use and high-risk drug injection are prevalent and accepted, and prisoners spend large parts of their day finding, paying for, and using drugs (Culbert et al. 2015). In fact, a main benefit of OAT identified by Australian prisoners, is the financial advantage of not buying drugs in prison (Sindicich et al. 2016). Similarly, in Malaysia where 95% of HIV-infected male prisoners meet criteria for opioid dependence and two-thirds (66%) shared needles immediately before incarceration (Bachireddy et al. 2011), very few had used methadone (3.9%). Especially damaging were prisoner's perceptions that heroin and methadone represent different forms of addiction, which has been documented among HIV-infected prisoners in Malaysia (Choi et al. 2010) and Indonesia (Culbert et al. 2015). Such attitudes also exist in countries like Ukraine and Moldova where OAT was introduced a decade ago, at a similar time to Malaysia. Reasons for negative attitudes toward OAT in prisons are complex and may be related to negatives attitudes perpetuated by prison personnel (Polonsky et al. 2015), opposition to OAT by persons tied to the prison drug economy (Polonsky et al. 2016a), the misperception that addiction is not a chronic and recurring illness (Polonsky et al. 2016a; Polonsky et al. 2016b), or the belief that OAT is not effective (Bachireddy et al. 2011). In Malaysia, such negative attitudes toward OAT as an effective treatment for opioid addiction persist among PWID in the community as well (Vijay et al. 2015).
Addressing HIV, Tuberculosis, and Opioid Addiction in Prisoners
In Malaysia, prison-based OAT was initiated through pilot programs in two prisons in 2008-2009 and now reaches about 250 prisoners (Wickersham et al. 2013a; Wickersham et al. 2013b). These programs developed from evidence that provision of OAT during incarceration and after release to the community was associated with significantly improved post-release health outcomes in PLH (Gordon et al. 2011; Kinlock et al. 2009), and so initially targeted PLH within the prison setting. Prior to introducing methadone maintenance therapy (MMT) at these sites, we conducted a formative assessment, which suggested a number of important implementation barriers, including undesirable methad one side effects, lack of physician training, and law enforcement practices that interfered with methadone treatment in released prisoners (Wickersham et al. 2013a). One of the most important lessons to emerge was that patients who were released on a daily methadone dose >80mg were more likely to be retained on methadone 1 year after release (Wickersham et al. 2013b). This turned our attention to the importance of optimizing MMT dose and addressing cravings and side effects prior to and during community re-entry - a period accurately perceived by prisoners as high risk for drug relapse (Cepeda et al. 2015b; Choi et al. 2010) and risk behaviors (Cepeda et al. 2015a).
Equipped with these insights, we embarked on a study in 2011, Project HARAPAN, to evaluate (through a randomized controlled trial) the relative effectiveness of methadone maintenance therapy (MMT) alone, and in combination with a behavioral intervention (Holistic Health Recovery Program, HHRP) for reducing HIV risk behaviors and drug use in HIV-infected, opioid-dependent Malaysian prisoners. In the process of adapting HHRP to the Malaysian context (HHRP-M), we learned that HIV status disclosure, social support, and accessing ART after release were seen by prisoners as especially challenging and therefore adapted HHRP to address the knowledge and interpersonal skills needed to successfully access care and negotiate safer sex, harm reduction, and HIV status disclosure during the immediate post-release period (Copenhaver et al. 2011).
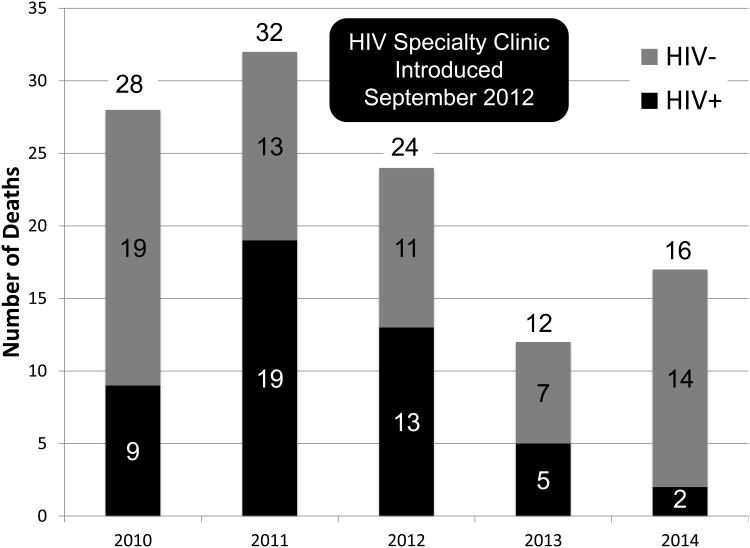
It also became apparent that HIV-related mortality within prison was extraordinarily high. During the first two years of Project HARAPAN alone, there were 28 HIV-related deaths within a single prison, with some participants not surviving long enough to receive the methadone/HHRP intervention. Closer examination revealed large gaps in HIV treatment and a lack of clinical resources and healthcare staffing allocated to address the high burden of illness in HIV+ prisoners. For example, although HIV testing was mandatory, which does not conform to international recommendations (UNODC 2009) subsequent linkage to HIV treatment and care failed to meet clinical or ethical standards (Basu et al. 2005), with less than half (48.4%) of eligible HIV+ prisoners receiving ART (Bick et al. 2013). To address these gaps in care, our team established an HIV subspecialty clinic within Malaysia's largest prison in September 2012, with staffing from the University of Malaya and Yale University. The clinicians worked alongside the existing prison doctors, introduced routine CD4 testing and monitoring and provided ART in close accordance with Malaysian Ministry of Health guidelines (CD4<350/μL). As a result, we saw a 50% decline in all-cause mortality from 2010 to 2014 (see Figure 2), and HIV-related deaths were reduced 75.7% over the same period from an average of 14.3 deaths annually from 2010 to 2012, to 3.5 deaths annually from 2013 to 2014. As a proportion of all deaths, HIV–related deaths declined 95% from 2010-12 to 2013-14.
Figure 2. All-Cause and HIV-related Mortality in Prisoners before and after Introduction of HIV Specialty Clinic.
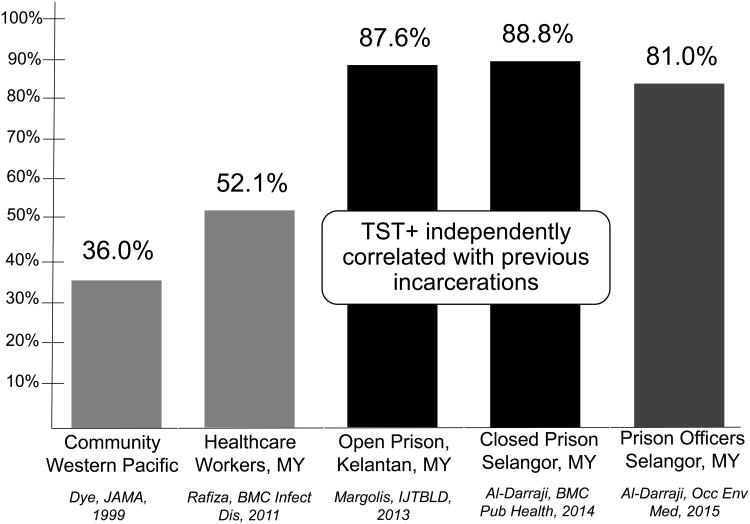
Tuberculosis in prisoners in Malaysia, especially those with HIV, remains problematic. Screening studies for LTBI in a variety of prisons (see Figure 3), including those housed in closed dormitories (Al-Darraji et al. 2014a) as well as those with open-air housing conditions (Margolis et al. 2013), show the prevalence of LTBI to exceed 80%, with prevalence being higher in those without HIV, likely due to the immunosuppressant effects of HIV and inability to respond to tuberculin skin testing (TST). Additional data suggest that the prevalence of LTBI in PWIDs in community settings is similar to that reported in prisons, through which many PWID had previously transitioned, suggesting that prisons are extraordinary amplifiers of TB (Al-Darraji et al. 2014b). Also confirming the high risk environment for TB in prisons is the finding that correctional officers and other personnel who work in the prison, regardless of the amount of time spent in the prison setting, had a prevalence of LTBI similar to that of prisoners (Al-Darraji et al. 2015). The prevalence of LTBI in prisoners (88.8%) and prison personnel (81.0%), however, was much higher than in Southeast Asia (46.0%) or the Western Pacific (32.0%). or even among Malaysian healthcare workers (52.1%) (Rafiza et al. 2011). Not only is LTBI infection high, but using standard screening strategies with symptoms and sputum tested for TB using AFB smear, GeneXpert and culture, 17.9% of 134 HIV-infected prisoners had TB disease; 15 (12.0%) of the 125 without previously known TB were newly diagnosed. Important from this screening study is that the WHO-recommended symptom surveys and GeneXpert MTB/RIF with a single sputum examination sub-optimally identified MTB cases (Al-Darraji et al. 2013).
Figure 3. Comparison of The Prevalence of Tuberculosis Infection in Malaysian Prisons and Communities.
Preparing for the Perfect Storm
The convergence of the HIV, tuberculosis (TB), and addiction epidemics in populations that are overwhelmingly exposed to incarceration and its negative long-term health effects (Patterson 2013) will drastically increase the magnitude of harm and costs associated with these epidemics to individuals and communities. Preventing this ‘perfect storm’ requires stakeholders to prioritize evidence-based strategies to reduce the consequences to individuals and communities (El-Bassel et al. 2013). This will be especially crucial for Malaysia to meet the 2020 UNAIDS 90-90-90 goals to ensure 90% of PLH are diagnosed, with 90% of these on ART and 90% of ART patients achieving viral suppression. This translates to viral suppression rates exceeding 73% (Joint United Nations Programme on HIV/AIDS 2014).
Although the use of incarceration as a drug control measure has failed to stem rates of addiction in the community (REF) and arguably exacerbated problems associated with HIV and addiction, prisons regrettably remain a main source of HIV primary care services for people who use drugs throughout Asia. If resources are adequately allocated, the Malaysian criminal justice system could play an important role in helping Malaysia to meet its 90-90-90 targets. Malaysian prisons, where the majority of PLH are diagnosed due to mandatory HIV testing, identify nearly all PLH who are incarcerated. Given the new WHO guidelines to provide ART to all PLH, irrespective of CD4 count (World Health Organization (WHO) 2015b), this would overcome logistical issues or coordinating CD4 monitoring before initiating ART. Successfully placing all PLH in prisons on ART would have the immediate benefit of reducing morbidity and mortality, especially from TB, by restoring the immune systems of patients, and secondarily reducing sexual and vertical transmission after release to the community.
A recent systematic review suggested that the period immediately after release from prison is when ART linkage is least successful and results in sustained treatment interruptions (Iroh et al. 2015), but is mitigated in PLH receiving OAT with methadone or buprenorphine (Springer et al. 2010; Springer et al. 2012; Wickersham et al. 2013b), especially with adequately high doses. Initiating ART and OAT within prison would begin to address low rates of ART coverage in PWID and, coupled with effective transitional care, be especially crucial for ensuring viral suppression during community re-entry (Springer et al. 2011). Last, because TB is so prevalent in prisoners and has devastating consequences when HIV patients are congregated, morbidity and mortality could be reduced further by removing segregation policies, implementing standardized screening programs for TB, promptly isolating those with suspected and confirmed contagious TB, and initiating treatment for those with active disease and isoniazid preventive therapy (IPT) for those with LTBI (Granich et al. 2010; Theron et al. 2011; World Health Organization (WHO) 2011). Continuation of treatment for TB and LTBI would also be optimized by integrating OAT with TB treatments (Getahun et al. 2013; Morozova et al. 2013; UNODC 2006; WHO/UNODC/UNAIDS 2008), similar to recommendations for ART. This is especially true since 67% of patients identified with either active or LTBI infection have inadequate time remaining on their prison sentence to complete treatment and therefore need effective transitional care (Al-Darraji et al. 2016). Together, these interventions will forestall the negative consequence of the perfect storm and promote individual and public health.
Acknowledgments
Funding: Funding for this research was provided by the National Institute on Drug Abuse for research (R01 DA025943 to F.L.A.) and career development (K24 DA017072 to F.L.A., K01 DA038529 to J.A.W, F30 DA039716 to A.R.B). Additional funding was provided for research by the University of Malaya's High Impact Research Grant (E-000001-20001 to A.K) and for career development by NIAID Global Health Equity Scholars Program (R25 TW009338 to G.J.C.), National Institute of Mental Health (F30MH105153 to M.P.W.), Doris Duke Charitable Foundation through a grant supporting the Doris Duke International Clinical Research Fellows Program at Yale University School of Medicine to M.P.W., and Yale University (Yale College Fellowship for Research in Health Studies) to E.G.F.
Footnotes
Conflict of Interest Statement: All authors report no conflicts of interest.
Bibliography
- Al-Darraji HA, Altice FL, Kamarulzaman A. Undiagnosed pulmonary tuberculosis among prisoners in Malaysia: An overlooked risk for tuberculosis in the community. Trop Med Int Health. 2016 doi: 10.1111/tmi.12726. In Press. [DOI] [PubMed] [Google Scholar]
- Al-Darraji HA, Kamarulzaman A, Altice FL. Latent tuberculosis infection in a Malaysian prison: implications for a comprehensive integrated control program in prisons. BMC Public Health. 2014a;14:22. doi: 10.1186/1471-2458-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Darraji HA, Tan C, Kamarulzaman A, Altice FL. Prevalence and correlates of latent tuberculosis infection among employees of a high security prison in Malaysia. Occup Environ Med. 2015;72:442–447. doi: 10.1136/oemed-2014-102695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Darraji HA, et al. Tuberculosis screening in a novel substance abuse treatment center in Malaysia: implications for a comprehensive approach for integrated care. J Subst Abuse Treat. 2014b;46:144–149. doi: 10.1016/j.jsat.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Darraji HAA, Razak HA, Ng KP, Altice FL, Kamarulzaman A. The Diagnostic Performance of a Single GeneXpert MTB/RIF Assay in an Intensified Tuberculosis Case Finding Survey among HIV-Infected Prisoners in Malaysia. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0073717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amon J, Pearshouse R, Cohen J, Schleifer R. Compulsory drug detention centers in China, Cambodia, Vietnam, and Laos: health and human rights abuses. Health Hum Rights. 2013;15:124–137. [PubMed] [Google Scholar]
- Amon JJ, Pearshouse R, Cohen JE, Schleifer R. Compulsory drug detention in East and Southeast Asia: evolving government, UN and donor responses. Int J Drug Policy. 2014;25:13–20. doi: 10.1016/j.drugpo.2013.05.019. [DOI] [PubMed] [Google Scholar]
- Bachireddy C, Bazazi AR, Kavasery R, Govindasamy S, Kamarulzaman A, Altice FL. Attitudes toward opioid substitution therapy and pre-incarceration HIV transmission behaviors among HIV-infected prisoners in Malaysia: implications for secondary prevention. Drug Alcohol Depend. 2011;116:151–157. doi: 10.1016/j.drugalcdep.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S, Smith-Rohrberg D, Hanck S, Altice FL. HIV testing in correctional institutions: evaluating existing strategies, setting new standards. AIDS Public Policy J. 2005;20:3–24. [PubMed] [Google Scholar]
- Bazazi AR, Crawford F, Zelenev A, Heimer R, Kamarulzaman A, Altice FL. HIV Prevalence Among People Who Inject Drugs in Greater Kuala Lumpur Recruited Using Respondent-Driven Sampling. AIDS Behav. 2015a;19:2347–2357. doi: 10.1007/s10461-015-1191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazazi AR, Zelenev A, Fu JJ, Yee I, Kamarulzaman A, Altice FL. High prevalence of non-fatal overdose among people who inject drugs in Malaysia: Correlates of overdose and implications for overdose prevention from a cross-sectional study. Int J Drug Policy. 2015b;26:675–681. doi: 10.1016/j.drugpo.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beg M, Strathdee SA, Kazatchkine M. State of the art science addressing injecting drug use, HIV and harm reduction. Int J Drug Policy. 2015;26(1):S1–4. doi: 10.1016/j.drugpo.2014.11.008. [DOI] [PubMed] [Google Scholar]
- Beyrer C, Razak MH, Lisam K, Chen J, Lui W, Yu XF. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14:75–83. doi: 10.1097/00002030-200001070-00009. [DOI] [PubMed] [Google Scholar]
- Biadglegne F, Rodloff AC, Sack U. Review of the prevalence and drug resistance of tuberculosis in prisons: a hidden epidemic. Epidemiol Infect. 2015;143:887–900. doi: 10.1017/s095026881400288x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bick J, Koh C, Kamarulzaman A, Altice FL. HIV, TB, and Drug Treatment within the Malaysian Prison System: the Kajang Prison Experience. Paper presented at the 11th International Congress on AIDS in Asia and the Pacific (ICAAP 11); Bangkok, Thailand. 2013. [Google Scholar]
- Booth RE, et al. Law enforcement practices associated with HIV infection among injection drug users in Odessa. Ukraine AIDS Behav. 2013;17:2604–2614. doi: 10.1007/s10461-013-0500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce RD, Govindasamy S, Sylla L, Haddad MS, Kamarulzaman A, Altice FL. Case series of buprenorphine injectors in Kuala Lumpur, Malaysia. Am J Drug Alcohol Abuse. 2008;34:511–517. doi: 10.1080/00952990802122259. [DOI] [PubMed] [Google Scholar]
- Bruce RD, Govindasamy S, Sylla L, Kamarulzaman A, Altice FL. Lack of reduction in buprenorphine injection after introduction of co-formulated buprenorphine/naloxone to the Malaysian market. Am J Drug Alcohol Abuse. 2009;35:68–72. doi: 10.1080/00952990802585406. doi:908653249[pii]10.1080/00952990802585406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda JA, Niccolai LM, Lyubimova A, Kershaw T, Levina O, Heimer R. High-risk behaviors after release from incarceration among people who inject drugs in St. Petersburg, Russia. Drug Alcohol Depend. 2015a;147:196–202. doi: 10.1016/j.drugalcdep.2014.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda JA, Vetrova MV, Lyubimova AI, Levina OS, Heimer R, Niccolai LM. Community reentry challenges after release from prison among people who inject drugs in St. Petersburg, Russia. Int J Prison Health. 2015b;11:183–192. doi: 10.1108/IJPH-03-2015-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi P, Kavasery R, Desai MM, Govindasamy S, Kamarulzaman A, Altice FL. Prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Int J STD AIDS. 2010;21:416–423. doi: 10.1258/ijsa.2009.009180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copenhaver MM, Tunku N, Ezeabogu I, Potrepka J, Zahari MMA, Kamarulzaman A, Altice FL. Adapting an evidence-based intervention targeting HIV-infected prisoners in malaysia. AIDS research and treatment. 2011 doi: 10.1155/2011/131045. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crofts N, Azim T. Harm reduction in Asia and the Pacific: an evolving public health response. Harm Reduct J. 2015;12:47. doi: 10.1186/s12954-015-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csete J, et al. Public health and international drug policy. The Lancet. 2016 doi: 10.1016/s0140-6736(16)00619-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert GJ, Waluyo A, Iriyanti M, Muchransyah AP, Kamarulzaman A, Altice FL. Within-prison drug injection among HIV-infected male prisoners in Indonesia: A highly constrained choice. Drug Alcohol Depend. 2015;149:71–79. doi: 10.1016/j.drugalcdep.2015.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, et al. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010-2012? A review of the six highest burden countries. Int J Drug Policy. 2014;25:53–60. doi: 10.1016/j.drugpo.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Deiss RG, Rodwell TC, Garfein RS. Tuberculosis and illicit drug use: review and update. Clin Infect Dis. 2009;48:72–82. doi: 10.1086/594126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan K, Moazen B, Noori A, Rahimzadeh S, Farzadfar F, Hariga F. People who inject drugs in prison: HIV prevalence, transmission and prevention. Int J Drug Policy. 2015;26(1):S12–15. doi: 10.1016/j.drugpo.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Dutta A, Wirtz AL, Baral S, Beyrer C, Cleghorn FR. Key harm reduction interventions and their impact on the reduction of risky behavior and HIV incidence among people who inject drugs in low-income and middle-income countries. Curr Opin HIV AIDS. 2012;7:362–368. doi: 10.1097/COH.0b013e328354a0b5. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Jin H, Wickersham J, Kamarulzaman A, John J, Altice FL. Exploring intentions to discriminate against patients living with HIV/AIDS among future healthcare providers in Malaysia. Tropical medicine & international health : TM & IH. 2014;19:672–679. doi: 10.1111/tmi.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Strathdee SA, El Sadr WM. HIV and people who use drugs in central Asia: confronting the perfect storm. Drug Alcohol Depend. 2013;132(1):S2–6. doi: 10.1016/j.drugalcdep.2013.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu JJ, Bazazi AR, Altice FL, Mohamed MN, Kamarulzaman A. Absence of antiretroviral therapy and other risk factors for morbidity and mortality in Malaysian compulsory drug detention and rehabilitation centers. PLoS One. 2012;7:e44249. doi: 10.1371/journal.pone.0044249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getahun H, Baddeley A, Raviglione M. Managing tuberculosis in people who use and inject illicit drugs. Bull World Health Organ. 2013;91:154–156. doi: 10.2471/BLT.13.117267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghani MA, et al. An exploratory qualitative assessment of self-reported treatment outcomes and satisfaction among patients accessing an innovative voluntary drug treatment centre in Malaysia. Int J Drug Policy. 2015;26:175–182. doi: 10.1016/j.drugpo.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill J. Anxiety Disorders Among Incarcerated Drug Users. Malaysian Journal of Psychiatry. 2010;19 [Google Scholar]
- Gordon MS, Kinlock TW, Miller PM. Medication-assisted treatment research with criminal justice populations: challenges of implementation. Behav Sci Law. 2011;29:829–845. doi: 10.1002/bsl.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granich R, Akolo C, Gunneberg C, Getahun H, Williams P, Williams B. Prevention of tuberculosis in people living with HIV. Clin Infect Dis. 2010;50(3):S215–222. doi: 10.1086/651494. [DOI] [PubMed] [Google Scholar]
- Hser YI, Liang D, Lan YC, Vicknasingam BK, Chakrabarti A. Drug Abuse, HIV, and HCV in Asian Countries. J Neuroimmune Pharmacol. 2016 doi: 10.1007/s11481-016-9665-x. [DOI] [PubMed] [Google Scholar]
- Institute for Criminal Policy Research. World Prison Brief: Malaysia. [Accessed Spetember 27, 2015];2015 http://www.prisonstudies.org/country/malaysia. 2015.
- Iroh PA, Mayo H, Nijhawan AE. The HIV Care Cascade Before, During, and After Incarceration: A Systematic Review and Data Synthesis. Am J Public Health. 2015;105:e5–16. doi: 10.2105/ajph.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwanto, Wirawan DN, Praptoraharjo I, Irianto S, Mulia SM. Evidence-informed response to illicit drugs in Indonesia. Lancet. 2015;385:2249–2250. doi: 10.1016/s0140-6736(15)61058-3. [DOI] [PubMed] [Google Scholar]
- Jin H, Earnshaw VA, Wickersham JA, Kamarulzaman A, Desai MM, John J, Altice FL. An assessment of health-care students' attitudes toward patients with or at high risk for HIV: implications for education and cultural competency. AIDS Care. 2014;26:1223–1228. doi: 10.1080/09540121.2014.894616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. HIV in Asia and the Pacific. UNAIDS; 2013. [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. 90-90-90- An ambitious treatment target to help end the AIDS epidemic. New York: 2014. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva, Switzerland: 2014. [Google Scholar]
- Jürgens R, Ball A, Verster A. Interventions to reduce HIV transmission related to injecting drug use in prison. The Lancet Infectious Diseases. 2009;9:57–66. doi: 10.1016/s1473-3099(08)70305-0. [DOI] [PubMed] [Google Scholar]
- Jurgens R, Csete J, Amon JJ, Baral S, Beyrer C. People who use drugs, HIV, and human rights. Lancet. 2010;376:475–485. doi: 10.1016/s0140-6736(10)60830-6. [DOI] [PubMed] [Google Scholar]
- Kamarulzaman A. Impact of HIV prevention programs on drug users in Malaysia. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2009a;52:S17–S19. doi: 10.1097/QAI.0b013e3181bbc9af. [DOI] [PubMed] [Google Scholar]
- Kamarulzaman A. Impact of HIV prevention programs on drug users in Malaysia. J Acquir Immune Defic Syndr. 2009b;52(1):S17–19. doi: 10.1097/QAI.0b013e3181bbc9af00126334-200911011-00006[pii]. [DOI] [PubMed] [Google Scholar]
- Kamarulzaman A, McBrayer JL. Compulsory drug detention centers in East and Southeast Asia. Int J Drug Policy. 2015;26(1):S33–37. doi: 10.1016/j.drugpo.2014.11.011. [DOI] [PubMed] [Google Scholar]
- Khan F, et al. Assessment of an Innovative Voluntary Substance Abuse Treatment Program Designed to Transition from Compulsory Drug Detention Centers in Malaysia. Subst Use Misuse. 2015 doi: 10.1080/10826084.2016.1267217. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O'Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abuse Treat. 2009;37:277–285. doi: 10.1016/j.jsat.2009.03.002. doi:S0740-5472(09)00030-0[pii]10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinner SA, Wang EA. The case for improving the health of ex-prisoners. Am J Public Health. 2014;104:1352–1355. doi: 10.2105/AJPH.2014.301883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan A, Brown SE, Khan F, Ghani M, Kaur S, Kamarulzaman A, Altice FL. Pre-treatment Drug Use Characteristics and Experiences among Patients in a Voluntary Substance Abuse Treatment Center in Malaysia: A Mixed Methods Approach. Substance Abuse. 2016 doi: 10.1080/08897077.2016.1146648. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Dolan K. A literature review of international implementation of opioid substitution treatment in prisons: equivalence of care? Eur Addict Res. 2009;15:107–112. doi: 10.1159/000199046. doi:000199046[pii]10.1159/000199046. [DOI] [PubMed] [Google Scholar]
- Larney S, Randall D, Gibson A, Degenhardt L. The contributions of viral hepatitis and alcohol to liver-related deaths in opioid-dependent people. Drug Alcohol Depend. 2013;131:252–257. doi: 10.1016/j.drugalcdep.2012.11.012. [DOI] [PubMed] [Google Scholar]
- Lewis G. Opening Remarks: Second Regional Consultation on Compulsory Centres for Drug Users. Kuala Lumpur, Malaysia: Oct 1, 2012. 2012. [Google Scholar]
- Lines R. The right to health of prisoners in international human rights law. Int J Prison Health. 2008;4:3–53. doi: 10.1080/17449200701862145. [DOI] [PubMed] [Google Scholar]
- Malaysian AIDS Council, Malaysian AIDS Foundation. 2013 Annual Report 2014 [Google Scholar]
- Margolis B, Al-Darraji HA, Wickersham JA, Kamarulzaman A, Altice FL. Prevalence of tuberculosis symptoms and latent tuberculous infection among prisoners in northeastern Malaysia. Int J Tuberc Lung Dis. 2013;17:1538–1544. doi: 10.5588/ijtld.13.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L. Examining non-AIDS mortality among people who inject drugs. AIDS. 2014;28(4):S435–444. doi: 10.1097/QAD.0000000000000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers BM, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. The Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- McLaughlin SI, Spradling P, Drociuk D, Ridzon R, Pozsik CJ, Onorato I. Extensive transmission of Mycobacterium tuberculosis among congregated, HIV-infected prison inmates in South Carolina, United States. Int J Tuberc Lung Dis. 2003;7:665–672. [PubMed] [Google Scholar]
- Milloy MJ, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203:1215–1221. doi: 10.1093/infdis/jir032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJ, Kerr T, Salters K, Samji H, Guillemi S, Montaner J, Wood E. Incarceration is associated with used syringe lending among active injection drug users with detectable plasma HIV-1 RNA: a longitudinal analysis. BMC Infect Dis. 2013;13:565. doi: 10.1186/1471-2334-13-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJ, Montaner J, Wood E. Barriers to HIV treatment among people who use injection drugs: implications for ‘treatment as prevention’. Curr Opin HIV AIDS. 2012;7:332–338. doi: 10.1097/COH.0b013e328354bcc8. [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Malaysia. Global AIDS Response Progress Report, Malaysia. Malaysian Ministry of Health; Kuala Lumpur: 2015. [Google Scholar]
- Moore DJ, Blackstone K, Woods SP, Ellis RJ, Atkinson JH, Heaton RK, Grant I. Methamphetamine use and neuropsychiatric factors are associated with antiretroviral non-adherence. AIDS Care. 2012;24:1504–1513. doi: 10.1080/09540121.2012.672718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morozova O, Dvoryak S, Altice FL. Methadone treatment improves tuberculosis treatment among hospitalized opioid dependent patients in Ukraine. Int J Drug Policy. 2013;24:e91–98. doi: 10.1016/j.drugpo.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noordin NM, Merican MI, Rahman HA, Lee SS, Ramly R. Substitution treatment in Malaysia. Lancet. 2008;372:1149–1150. doi: 10.1016/S0140-6736(08)61479-8. doi:S0140-6736(08)61479-8[pii]10.1016/S0140-6736(08)61479-8. [DOI] [PubMed] [Google Scholar]
- Patterson EJ. The dose-response of time served in prison on mortality: New York State, 1989-2003. Am J Public Health. 2013;103:523–528. doi: 10.2105/AJPH.2012.301148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearshouse R, Amon JJ. The ethics of research in compulsory drug detention centres in Asia. J Int AIDS Soc. 2012;15:18491. doi: 10.7448/IAS.15.2.18491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, et al. Accessing methadone within Moldovan prisons: Prejudice and myths amplified by peers. Int J Drug Policy. 2016a;29:91–95. doi: 10.1016/j.drugpo.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, Altice FL. Challenges to implementing opioid substitution therapy in Ukrainian prisons: Personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug Alcohol Depend. 2015;148:47–55. doi: 10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, et al. Attitudes Toward Addiction, Methadone Treatment, and Recovery Among HIV-Infected Ukrainian Prisoners Who Inject Drugs: Incarceration Effects and Exploration of Mediators. AIDS Behav. 2016b doi: 10.1007/s10461-016-1375-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafiza S, Rampal KG, Tahir A. Prevalence and risk factors of latent tuberculosis infection among health care workers in Malaysia. BMC Infect Dis. 2011;11:19. doi: 10.1186/1471-2334-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sindicich N, Zador D, Larney S, Dolan K. Patient motivations, perceptions, and experiences of opioid substitution therapy in prison. National Drug and Alcohol Research Centre, University of New South Wales; 2016. [Google Scholar]
- Spradling P, et al. Drug-drug interactions in inmates treated for human immunodeficiency virus and Mycobacterium tuberculosis infection or disease: an institutional tuberculosis outbreak. Clin Infect Dis. 2002;35:1106–1112. doi: 10.1086/343047. [DOI] [PubMed] [Google Scholar]
- Springer SA, Chen S, Altice FL. Improved HIV and substance abuse treatment outcomes for released HIV-infected prisoners: the impact of buprenorphine treatment. J Urban Health. 2010;87:592–602. doi: 10.1007/s11524-010-9438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012;7:e38335. doi: 10.1371/journal.pone.0038335. http://dx.doi.org/10.1371%2Fjournal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53:469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanguay P. Policy responses to drug issues in Malaysia. International Drug Policy Consortium; 2011. [Google Scholar]
- Tanguay P, et al. Facilitating a transition from compulsory detention of people who use drugs towards voluntary community-based drug dependence treatment and support services in Asia. Harm Reduct J. 2015;12:31. doi: 10.1186/s12954-015-0071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theron G, et al. Evaluation of the Xpert MTB/RIF assay for the diagnosis of pulmonary tuberculosis in a high HIV prevalence setting. American journal of respiratory and critical care medicine. 2011;184:132–140. doi: 10.1164/rccm.201101-0056OC. [DOI] [PubMed] [Google Scholar]
- Ti L, Hayashi K, Kaplan K, Suwannawong P, Wood E, Kerr T. Contextual Factors Associated with Rushed Injecting Among People Who Inject Drugs in Thailand. Prev Sci. 2014:1–8. doi: 10.1007/s11121-014-0477-z. [DOI] [PubMed] [Google Scholar]
- United Nations Malaysia. Malaysia Millenium Development Goals Report, 2015. Kuala Lumpur: 2016. [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report, 2013. UNODC; 2013. [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report. UNODC; Vienna: 2014. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) HIV in prisons: Situation and needs assessment toolkit. Vienna, Austria: 2010. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) Drug Dependence Treatment: Interventions for Drug Users in Prison. TreatNet; Vienna, Austria: 2012. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) Policy Brief: HIV prevention, treatment and care in prisons and other closed settings: a comprehensive package of interventions. Vienna, Austria: 2013. [Google Scholar]
- United Nations Programme on HIV/AIDS. The Global AIDS Response Progress Report, 2014: Malaysia. HIV/STI Section of Ministry of Health Malaysia; Geneva: 2014. [Google Scholar]
- UNODC. HIV testing and counselling in prisons and other closed settings. Vienna: 2009. [PubMed] [Google Scholar]
- UNODC. Report of the Regional Consultation on Compulsory Centres for Drug Users in Asia and the Pacific. Bangkok: 2010. [Google Scholar]
- UNODC W. HIV/AIDS Prevention Care, Treatment and Support in Prision Setting A Framework for and Effective National Response. Geneva: 2006. [Google Scholar]
- Valway SE, Richards SB, Kovacovich J, Greifinger RB, Crawford JT, Dooley SW. Outbreak of multi-drug-resistant tuberculosis in a New York State prison, 1991. American journal of epidemiology. 1994;140:113–122. doi: 10.1093/oxfordjournals.aje.a117222. [DOI] [PubMed] [Google Scholar]
- Vijay A, Bazazi AR, Yee I, Kamarulzaman A, Altice FL. Treatment readiness, attitudes toward, and experiences with methadone and buprenorphine maintenance therapy among people who inject drugs in Malaysia. J Subst Abuse Treat. 2015;54:29–36. doi: 10.1016/j.jsat.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walmsley R. World Prison Population List. 11th. London: 2016. 11th edn. [Google Scholar]
- WHO/UNODC/UNAIDS. Effectivness of Interventions to Address HIV in Prisons. Geneva: 2007. [Google Scholar]
- WHO/UNODC/UNAIDS. Policy Guidelines for Collaborative HIV and TB Services for Injecting and Other Drug Users: An Integrated Approach. 2008 [PubMed] [Google Scholar]
- Wickersham JA, Marcus R, Kamarulzaman A, Zahari MM, Altice FL. Implementing methadone maintenance treatment in prisons in Malaysia. Bull World Health Organ. 2013a;91:124–129. doi: 10.2471/BLT.12.109132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013b;132:378–382. doi: 10.1016/j.drugalcdep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Tuberculosis Country Profile, Malaysia 2015 [Google Scholar]
- World Health Organization (WHO) Tuberculosis Control in Prisons: A Manual for Programme Managers. Geneva: 2000. [Google Scholar]
- World Health Organization (WHO) Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. Geneva, Switzerland: 2011. [Google Scholar]
- World Health Organization (WHO) Prisons and Health. Regional Office of Europe; Copenhagen, Denmark: 2014. [Google Scholar]
- World Health Organization (WHO) Global tuberculosis report, 2015. 20th. Geneva, Switzerland: 2015a. [Google Scholar]
- World Health Organization (WHO) Guideline on when to start antiretroviral tehrapy and on pre-exposure prophylaxis for HIV. Geneva, Switzerland: 2015b. [PubMed] [Google Scholar]
- World Health Organization (WHO) HIV in Prisons. Regional Office for Europe. [Accessed on August 7, 2015];2015c at http://www.euro.who.int/en/health-topics/communicable-diseases/hivaids/policy/policy-guidance-for-key-populations-most-at-risk2/hiv-in-prisons.
- Zahari MM, Hwan Bae W, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36:31–38. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]