Abstract
Background
To study the long-term development (104 weeks) of insulin antibodies during treatment with insulin detemir (IDet) and insulin aspart (IAsp) in children with type 1 diabetes aged 2–16 years.
Methods
A 52-week, two-arm, randomized trial comparing IDet and neutral protamine Hagedorn insulin, both in combination with IAsp, was followed by a one-arm, 52-week extension trial of the IDet + IAsp arm. The present analysis was conducted in children who completed the randomized trial and entered into the extension trial.
Results
Of the 177 children randomized to IDet treatment, 146 entered the extension trial. IDet–IAsp cross-reacting antibodies peaked within the first 39 weeks of treatment before gradually declining. A similar pattern was seen for IDet-specific and IAsp-specific antibodies. At end of trial (EOT), no correlation was observed between the level of IDet-specific or IAsp-specific antibodies or IDet–IAsp cross-reacting antibodies and either glycated hemoglobin (HbA1c) or basal insulin dose. Mean HbA1c was stable during the treatment period, with a slight increase over time from 8.41% (68.4 mmol/mol) at baseline to 8.74% (72 mmol/mol) at EOT. Mean IDet dose increased from 0.43 U/kg at baseline to 0.66 U/kg at EOT. Mean IAsp dose increased from 0.46 U/kg to 0.51 U/kg at EOT.
Conclusion
Although treatment with IDet and IAsp is associated with development of specific and cross-reacting antibodies, no correlation between insulin antibodies and basal insulin dose or HbA1c was found.
Funding
Novo Nordisk A/S.
ClinicalTrials.gov identifiers: NCT00435019 and NCT00623194.
Electronic supplementary material
The online version of this article (doi:10.1007/s13300-016-0196-5) contains supplementary material, which is available to authorized users.
Keywords: Children, Clinical trial, Glycemic control, Immunity, Insulin aspart, Insulin detemir, Insulin therapy, Type 1 diabetes
Introduction
Injections of non-purified insulin lead to the formation of high levels of insulin antibodies in most patients with diabetes [1, 2]; however, with the introduction and use of purified animal insulin [and later, purified human insulin (HI) preparations], the prevalence and levels of insulin antibodies have decreased [2, 3]. In clinical practice, up to 68% of people treated with subcutaneous HI have been shown to develop insulin antibodies [4], which can lead to complications including injection-site reactions [5], cutaneous lipodystrophies (especially lipoatrophy) [6], and insulin resistance [7]. Insulin analogs (e.g., insulin detemir [IDet], insulin glargine, and insulin aspart [IAsp]) have also been associated with the development of insulin antibodies [8].
IDet is a long-acting, soluble acylated analog of HI (LysB29 [Nε-tetradecanoyl]des[B30] insulin human) with a protracted action profile due to the combination of increased self-association at the injection site and buffering of insulin concentration via albumin binding in both the subcutaneous tissue and the blood [9]. A clinical trial in adults with type 1 diabetes who had not previously been exposed to IDet showed that insulin antibodies developed after IDet administration [10]. Although the median IDet dose increased over the 2-year study period, after 1 year of treatment, antibody levels stabilized, followed by a decreasing trend in the subsequent year. Furthermore, glycemic control was not affected by insulin antibody formation [10].
IAsp is a rapid-acting analog of HI with a substitution of aspartic acid for proline in position B28, which accelerates hexamer dissociation after subcutaneous administration, leading to a faster rate of absorption [11]. In a previous study [4], patients with type 1 or type 2 diabetes who were exposed to IAsp developed cross-reacting antibodies (antibodies capable of binding both IAsp and HI), which increased for up to 3 months before declining to baseline levels at 9–12 months. No correlation was identified between adverse events or glycemic control and antibody levels [4].
A large amount of data in the published scientific literature describes the presence and effect of insulin antibodies, including those specific for IDet and IAsp, in adults with diabetes. However, few data exist on insulin antibodies, and no data exist on IDet-specific antibodies, in children with diabetes. Therefore, the aim of the current analysis was to investigate the development of IDet–IAsp cross-reacting antibodies and IDet- and IAsp-specific antibodies during 104 weeks of IDet/IAsp treatment in children 2–16 years of age with type 1 diabetes.
Methods
Patients
The present analysis included European children and adolescents with type 1 diabetes who had completed 52 weeks of treatment with IDet/IAsp in a randomized trial [12, 13] and were enrolled in a 52-week extension trial. The randomized and extension trials are both registered at ClinicalTrials.gov (NCT00435019 and NCT00623194, respectively). As previously described in detail [13], inclusion criteria for the randomized trial required children to be diagnosed with type 1 diabetes for a minimum of 12 months prior to inclusion, receiving a total daily insulin dose ≤2.0 U/kg and with glycated hemoglobin (HbA1c) ≤11.0% (96.7 mmol/mol), IDet-naïve and non-obese (maximum body mass index 20–27 kg/m2, depending on age).
Trial Design
The randomized trial (first 52 weeks of treatment) was conducted as previously described [13]. Children in the IDet arm who completed this trial were offered the option to continue treatment with IDet (once or twice daily) together with IAsp (2–4 times daily with meals) for a further 52 weeks (extension trial), for a total of 104 weeks of treatment (total treatment period). During the extension trial, patient visits were conducted every 13 weeks (five visits in total), and basal and bolus insulin doses were adjusted over the extension trial according to the titration guidelines previously described [13]. Both studies were approved by local ethics committees and health authorities and carried out in accordance with International Conference on Harmonisation Good Clinical Practice [14] and the Declaration of Helsinki 1964 (given the time of the study, the 2008 version of the declaration was used) [15]. Written informed consent was obtained from all children (where appropriate) and their parents or legal representatives before initiation of any trial-related activities.
Cross-Reacting Antibodies
The primary endpoint of the extension trial was to evaluate the development of IDet and IAsp cross-reacting antibodies following a total of 104 weeks of treatment. Antibody levels were measured using a subtraction radioimmunoassay, which was developed by Novo Nordisk A/S (Copenhagen, Denmark) and performed by Celerion Switzerland AG (Fehraltorf, Switzerland). At each patient visit, serum samples were collected for antibody measurements. Thereafter, the samples were kept at −20 °C until analysis. Three subgroups of antibodies were determined: cross-reacting antibodies between IDet and IAsp, specific antibodies for IDet, and specific antibodies for IAsp. Measurements were expressed as the percent bound radioactivity relative to the total amount of radioactivity present (%B/T). An IDet tracer (125I-[Tyr-A14] IDet] and IAsp tracer [125I-[Tyr-A14] IAsp) (Novo Nordisk A/S), both with specific activities of 30 mCi/mg, were used. Novo Nordisk A/S provided non-radioactive IDet and IAsp. The results obtained at 52 weeks in the randomized trial [13] were from a separate set of serum samples from those used as baseline samples for the extension trial. This accounts for the differences in the values at week 52 and why there are two sets of mean values at that time point (Fig. 1).
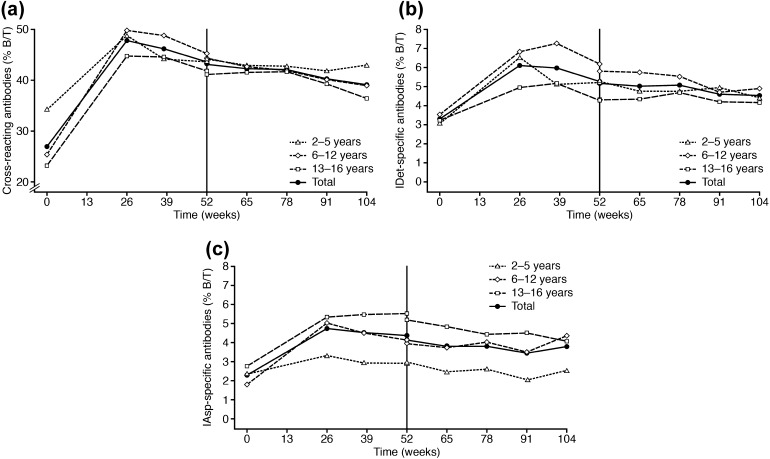
Fig. 1.
Observed mean antibodies (%B/T) over the total treatment period for children participating in the extension trial: a IDet–IAsp cross-reacting antibodies by age; b IDet-specific antibodies by age; c IAsp-specific antibodies by age. %B/T percent bound radioactivity relative to the total amount of radioactivity present, IAsp insulin aspart, IDet insulin detemir
Equal volumes (50 μL) of cold insulin/buffer, tracer, and sample were mixed and incubated overnight at 4 °C. Before mixing and centrifugation, polyethylene glycol (PEG) 6000 MW solution was added to a final concentration of 12.5% vol/vol. Before counting pellet radioactivity, the pellet was washed with 12.5% PEG. Intra-assay variation was less than 5% for medium and high antibody responses and up to 11% for low antibody responses. Day-to-day variation was always under 15%.
Glycemic Control
Secondary endpoints for assessment of glycemic control included levels of HbA1c, fasting plasma glucose (FPG), and self-measured plasma glucose (SMPG). Blood samples for HbA1c were drawn at screening, randomization, and approximately every 13 weeks thereafter for the total treatment period. Prior to all visits, blood samples for FPG were taken at home in the morning before breakfast and insulin injection. Additionally, SMPG profiles were assessed before breakfast and dinner on the last 3 days before each scheduled visit throughout the treatment period.
Hypoglycemia
Hypoglycemic episodes were classified according to the 2009 guidelines from the International Society for Pediatric and Adolescent Diabetes (ISPAD). These were the guidelines available at the time of the trial data analysis [16, 17]. Hypoglycemia was classified as mild if symptoms were present and the subject was able to treat him/herself, or moderate if the episodes were symptomatic and the subject could not treat him/herself but responded to oral treatment. Severe hypoglycemia was defined as episodes that required third-party assistance where the subject was semi-conscious/unconscious/in coma and where parenteral treatment may have been required. In addition to the ISPAD categorization, a category of biochemical hypoglycemic episodes was defined as plasma glucose <3.6 mmol/L (65 mg/dL) without signs or symptoms of hypoglycemia.
Body Weight
Body weight was standardized by standard deviation (SD) scores (also known as Z-scores) to compare different age groups and gender. Accurate and detailed growth standards were not available for all 11 participating countries, so British standards were used [18].
Statistical Analysis
Since the extension trial was uncontrolled, and therefore no comparator was available, only descriptive statistics were made, except for the primary endpoint, for which an exploratory analysis was made. The development of antibodies over the total treatment period was studied using a simplified linear mixed model including country, pubertal status at baseline, gender, age according to stratification at randomization, HbA1c at end of treatment (EOT), insulin dose at EOT, baseline antibody level, time (number of days since randomization in the randomized trial), and time2 in the model. Patient was included as a random effect. The term time2 was included in the model to determine whether the antibody level would plateau or decrease over time. An estimated negative parameter to time2 would suggest this. Backward elimination was used to reduce the number of variables in the model. The model should not be used to extrapolate beyond the observed time period. To investigate any apparent correlation between antibodies and HbA1c and basal insulin dose, scatter plots were made and inspected to assess whether a clear correlation was present. Children dropping out during the randomized trial, completing the randomized trial but not participating in the extension trial, or subjects not completing the extension trial were included in selected descriptive statistics output with last observation carried forward as a sensitivity measure. Statistical analysis was performed using SAS software version 9.1.3 (SAS Institute Inc., Cary, NC, USA).
Results
Patients
Of the 177 children initiating treatment with IDet/IAsp, 164 completed the randomized trial; one withdrew because of a non-treatment-emergent adverse event, acute leukemia, after eight days of treatment (2–5 years age group); one because of lack of efficacy (6–12 years age group); three because of non-compliance (two in the 6–12 years age group, one in the 13–16 years age group); and eight for unspecified other reasons (three in the 6–12 years age group, five in the 13–16 years age group). Of the 164 children completing the randomized trial, 146 continued on to the extension trial; there is no information on the reasons why eighteen children did not consent to the extension trial.
The 146 children continuing in the extension trial were presented according to the age groups defined at baseline in the randomized trial [13]. There were 37 children aged 2–5 years (25%), 59 children aged 6–12 years (41%), and 50 children aged 13–16 years (34%). In total, 141 children completed the extension trial. Of the five children withdrawn, one was from the 2–5 years age group (parental decision), one was from the 6–12 years age group (ineffective therapy), and three were from the 13–16 years age group (non-compliance). No children were withdrawn from the extension trial because of adverse events. Unless otherwise specified, the study population for this analysis includes subjects who completed the randomized trial and continued on to the extension trial.
Baseline characteristics of the children who were included in the initial IDet arm of the randomized trial and the extension trial are listed in Table 1.
Table 1.
Baseline characteristics
| Week 0 (start of randomized trial, IDet arm) [13] n = 177 | Week 52 (start of extension trial) n = 146 | |
|---|---|---|
| Age, years | 10.0 (4.09) | 11.1 (4.20) |
| Stratification by age, n (%) | ||
| 2–5 years | 42 (23.7) | 37 (25.3)a |
| 6–12 years | 79 (44.6) | 59 (40.4)a |
| 13–16 years | 56 (31.6) | 50 (34.2)a |
| Duration of diabetes, years | 3.70 (2.66) | 4.71 (2.68) |
| Gender, n (%) | ||
| Female | 94 (53.1) | 77 (52.7) |
| Male | 83 (46.9) | 69 (47.3) |
| Race, n (%) | ||
| White | 174 (98.3) | 144 (98.6) |
| Other | 0 (0) | 0 (0) |
| Unknownb | 3 (1.7) | 2 (1.4) |
| Pubertal status, n (%) | ||
| Tanner grade 1 | 104 (58.8) | 83 (56.8)c |
| Tanner grade 2 or more | 73 (41.2) | 63 (43.2)c |
| BMI, kg/m2 | 18.00 (2.74) | 18.44 (3.07) |
| HbA1c, % | 8.41 (1.11) | 8.57 (1.50) |
| HbA1c, mmol/mol | 68.4 (12.1) | 70.2 (16.4) |
| FPG, mmol/L | 8.36 (4.38) | 7.48 (4.13)d |
| Insulin doses given at start of trial, U/kg | ||
| Basal insulin | 0.43 (0.20) | 0.61 (0.24)e |
| Bolus insulin | 0.46 (0.21) | 0.47 (0.18)e |
| Country, n (%) | ||
| Bulgaria | 21 (11.9) | 19 (13.0) |
| Czech Republic | 19 (10.7) | 18 (12.3) |
| Denmark | 10 (5.6) | 6 (4.1) |
| Finland | 9 (5.1) | 7 (4.8) |
| France | 3 (1.7) | 2 (1.4) |
| Hungary | 14 (7.9) | 10 (6.8) |
| Macedonia | 11 (6.2) | 11 (7.5) |
| Poland | 26 (14.7) | 20 (13.7) |
| Russia | 42 (23.7) | 40 (27.4) |
| Turkey | 16 (9.0) | 11 (7.5) |
| UK | 6 (3.4) | 2 (1.4) |
Values are mean (SD) unless otherwise indicated
aAge of children at start of randomized trial, not start of extension period
brace unknown for French children
c n = 144
d n = 143
epubertal status at week 0 for children who entered into the extension trial
BMI body mass index, FPG fasting plasma glucose, HbA1c glycated hemoglobin, IDet insulin detemir, SD standard deviation
Cross-Reacting Antibodies
The mean observed IDet–IAsp cross-reacting antibodies over the total treatment period were similar for all age groups and peaked by week 39, before continually decreasing over time until EOT (week 104) (Fig. 1a). This was supported by the exploratory statistical analyses, in which the estimated parameter for time2 was statistically significantly different from zero (P < 0.05) and negative. Sensitivity analyses, which included all dropouts from the randomized and extension trials, further corroborated these findings.
IDet-specific and IAsp-specific Antibodies
Throughout the total treatment period, the observed mean levels of IDet-specific antibodies increased from the start of the trial and peaked by week 39 before decreasing and plateauing until EOT (Fig. 1b). Mean IAsp-specific antibodies also increased from the start of the trial and peaked by week 39 before decreasing and plateauing until EOT (Fig. 1c). The findings above were supported by a sensitivity analysis, which included all subjects who did not complete the randomized or extension trials.
Cross-Reacting and Specific Antibodies by HbA1c and Basal Insulin Dose
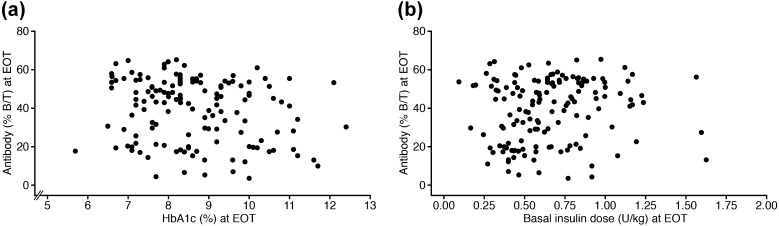
There was no trend observed at EOT between HbA1c and IDet–IAsp cross-reacting antibodies (Fig. 2a) or IDet-specific or IAsp-specific antibodies (data on file, Novo Nordisk A/S). In addition, there was no trend observed at EOT between basal insulin dose and IDet–IAsp cross-reacting antibodies (Fig. 2b) or IDet-specific or IAsp-specific antibodies (data not shown).
Fig. 2.
Cross-reacting antibodies at EOT for children participating in the extension trial: a by HbA1c; b by daily basal insulin dose per kg. %B/T percent bound radioactivity relative to the total amount of radioactivity present, EOT end of trial, HbA1c glycated hemoglobin
Insulin Dose
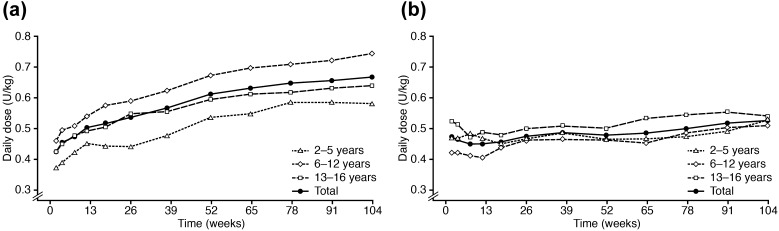
The starting dose per kg body weight of daily basal insulin at week 2 of the total treatment period was lowest in the 2–5 years group (0.38 U/kg) and highest in the 6–12 years group (0.46 U/kg), while the starting dose of daily bolus insulin was lowest in the 6–12 years group (0.42 U/kg) and highest in the 13–16 years group (0.52 U/kg). The overall mean daily basal insulin dose per kg increased throughout the total treatment period for all age groups (0.43 U/kg at baseline to 0.66 U/kg at EOT) (Fig. 3a), while the overall mean daily bolus insulin dose per kg remained relatively stable throughout the total treatment period for all age groups (0.46 U/kg at baseline to 0.51 U/kg at EOT) (Fig. 3b).
Fig. 3.
Observed mean daily insulin dose (LOCF) (U/kg) over the total treatment period for children participating in the extension trial: a basal insulin dose; b bolus insulin dose. LOCF last observation carried forward
Glycemic Control
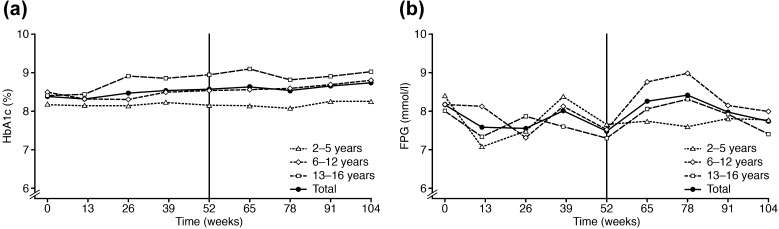
Observed mean HbA1c was relatively stable throughout the total treatment period in all age groups with a slight increase over time (8.41% [68.4 mmol/mol] at baseline to 8.74% [72 mmol/mol] at EOT) (Fig. 4a). Similar results were found from the sensitivity analysis that included all dropouts. HbA1c was lowest in the 2–5 years age group and highest in the 13–16 years age group. Observed mean FPG varied substantially throughout the total treatment period for all age groups (observed mean for all children was 8.18 mmol/L at baseline and 7.71 mmol/L at EOT) (Fig. 4b).
Fig. 4.
Observed mean a HbA1c and b FPG over the total treatment period for children participating in the extension trial. FPG fasting plasma glucose, HbA1c glycated hemoglobin
Hypoglycemia
Overall, during the total treatment period, 99.3% of all children experienced one or more hypoglycemic episodes (Supplementary Table 1). The number of hypoglycemic episodes per year was slightly higher in the 6–12 years age group than the 2–5 or 13–16 years age groups. Seven severe hypoglycemic episodes were reported, six of which occurred during the extension period.
Adverse Events
In total, 116 of the children reported 714 adverse events (rate of 2.47 [number of events per exposure year]) during the total treatment period, which were mainly mild in severity (620 mild [rate of 2.14], 83 moderate [rate of 0.29], 11 severe [rate of 0.04]). The majority of the adverse events were assessed as being unlikely to be related to IDet or IAsp (Supplementary Table 2). The most common adverse events, reported by more than 5 % of all children, were nasopharyngitis, upper respiratory tract infection, pharyngitis, influenza, gastroenteritis, bronchitis, viral infection, rhinitis, acute tonsillitis, headache, upper abdominal pain, abdominal pain, and vomiting. Eight children had injection-site reactions that were possibly or probably related to IDet, including lipodystrophy, lipoatrophy, lipohypertrophy, erythema, and injection-site nodules.
The most frequent serious adverse events occurring in more than one patient were diabetic ketoacidosis (three episodes reported by three children), hypoglycemia (three episodes reported by two children), and gastroenteritis (two episodes reported by two children). No deaths were reported in this trial.
Body Weight
The mean change in body weight SD score (body weight standardized by age and gender) during the total treatment period was −0.07.
Discussion
As expected, treatment with IDet gave rise to the formation of antibodies in children not previously exposed to this insulin preparation. Results showed that the overall observed mean level of IDet–IAsp cross-reacting antibodies, as well as the overall observed mean level of IDet-specific and IAsp-specific antibodies, increased and peaked within the first 39 weeks of treatment and then decreased. This trend corresponds with the observations in a study by Holmberg and colleagues, who showed that, in children, IAsp–HI cross-reacting antibodies increased for the first 24 weeks of treatment before plateauing until the end of the study at week 30 [3]. Furthermore, previous studies in adults have shown an increase in antibody development following treatment with IDet relative to neutral protamine Hagedorn insulin [19, 20]; however, the two former trials had a relatively short duration (26 and 52 weeks, respectively) and antibodies were only analyzed at baseline and at EOT. Antibody formation has not been studied in direct comparisons of IDet vs. insulin glargine in adults or children. Although immunological competence declines with increasing age [21], the trend in antibody development for the present 104-week trial in children is similar to that previously observed in a 2-year trial in adults [10]. Bartley and colleagues found that mean levels of IDet–IAsp cross-reacting antibodies, as well as mean levels of IDet-specific and IAsp-specific antibodies, increased between baseline and 64 weeks of treatment, but stabilized and tended to decrease during the second year of treatment [10]. In addition, the level of insulin antibodies did not appear to have any impact on metabolic control [10]. Similar findings were found in adults with type 1 diabetes taking insulin glargine over 52 weeks where there was no relationship between insulin antibody levels and HbA1c, insulin dose or hypoglycemia [22].This finding of lack of impact of the level of insulin antibodies was also seen in children, in whom levels of IAsp–HI cross-reacting antibodies had no effect on HbA1c [3].
The efficacy results from the present trials showed that glycemic control, measured as HbA1c, was stable, or presented a slight increase, throughout the total treatment period. This finding reflects the challenges in treating children effectively; factors such as social status, diabetes care in schools, variable routines, and fear of hypoglycemia can influence glycemic control [23]. In addition, it should be noted that the present trial was not a treat-to-target trial, which may have affected the investigators’ titration of IDet. The mean daily doses per kg of IDet steadily increased during the trial, as would be expected in growing children; it is normal in children for the required insulin dose to rise before puberty and then decline afterwards [24]. At EOT, there was no clear trend observed between the development of IDet–IAsp cross-reacting antibodies or IDet-specific or IAsp-specific antibodies and either HbA1c or basal insulin dose.
The safety results from the present trial showed that the majority of adverse events were mild in severity. Eight children (5.5%) reported injection-site reactions that were related to IDet, or to both IDet and IAsp. This was comparable with a previous pediatric trial in which 3.4% of the children treated with IDet reported injection-site reactions [25].
During the total treatment period, 99.3% of all children experienced one or more hypoglycemic episodes. Owing to the definition of moderate hypoglycemia (episodes that require assistance by another person, but respond to oral treatment), small children would be expected to have more moderate episodes of hypoglycemia than adults, as they are likely to need help from parents or other adults during episodes. The majority of hypoglycemic episodes were diurnal and were mild or biochemical. Very few severe hypoglycemic episodes were reported during the total treatment period, but the majority of these were reported in the extension trial; the reason for this is unclear.
A possible selection bias in the extension trial cannot be excluded, even though all children continuing after finalizing treatment with IDet in the randomized trial [13] were asked to continue in the extension trial. It is likely that only participants in whom IDet was well tolerated continued in the extension trial. For the remaining 18 children, no information exists regarding reasons for not continuing in the extension trial; however, it cannot be assumed that they did not tolerate IDet, as the reported adverse events for these children were primarily in the ‘mild’ category and not related to insulin therapy. Furthermore, no clear pattern emerged between the subjects continuing in the extension trial and those who did not. The great majority (89%) of IDet-treated children completing the first year of the trial proceeded into the extension. To further address any selection bias in our study, we conducted a sensitivity analysis on all subjects who were exposed to IDet throughout the total treatment period and this analysis corroborated the reported findings.
Our findings provide valuable information in a population in whom antibody response is not well studied. The results indicate that, although treatment with IDet and IAsp was associated with an initial increase in IDet–IAsp cross-reacting antibodies, this had no clinically relevant influence on efficacy or safety.
Conclusion
The results after a 104-week treatment period with IDet and IAsp in a basal–bolus regimen have demonstrated that the initial increase in antibodies leveled off after approximately 39 weeks of treatment. The development of antibodies did not appear to be associated with clinically relevant impaired insulin action (measured by HbA1c and basal insulin dose at EOT). We further observed a low rate of hypoglycemic episodes and no inappropriate weight gain. These findings confirm that IDet may safely be used in children with type 1 diabetes, including children as young as 2–5 years of age.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Novo Nordisk A/S. Editorial assistance was provided by Watermeadow Medical, an Ashfield company, and funded by Novo Nordisk A/S.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. All authors contributed to the design of the study, interpretation of the data, and writing/reviewing the manuscript. L. Bjerring Jensen and L. Conradsen Hiort conducted the data analysis.
Disclosures
N. Thalange has received support for travel and fees for speaking and consulting from Novo Nordisk A/S. A. Bereket has received support for travel related to the present study, and fees for speaking from Novo Nordisk. At the time work on the manuscript was carried out, L. Conradsen Hiort was an employee of Novo Nordisk A/S, and holds stock in Novo Nordisk A/S. L. Bjerring Jensen is employed by and holds stock in Novo Nordisk A/S. V. Peterkova did not receive financial support for the study described in the article, but has received funding from Novo Nordisk for other projects.
Compliance with ethics guidelines
Both studies were approved by local ethics committees and health authorities and carried out in accordance with International Conference on Harmonisation Good Clinical Practice and Helsinki Declaration of 1964 (given the time of the study, the 2008 version of the Declaration was used). Written informed consent was obtained from all children (where appropriate) and their parents or legal representatives before initiation of any trial-related activities.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to www.medengine.com/Redeem/4595F06074625CE4.
References
- 1.Schernthaner G. Immunogenicity and allergenic potential of animal and human insulins. Diabetes Care. 1993;16(Suppl. 3):155–165. doi: 10.2337/diacare.16.3.155. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz AB, Nabarro JD. Circulating insulin-binding antibodies. Diabetologia. 1980;19:329–334. doi: 10.1007/BF00280515. [DOI] [PubMed] [Google Scholar]
- 3.Holmberg H, Mersebach H, Kanc K, Ludvigsson J. Antibody response to insulin in children and adolescents with newly diagnosed type 1 diabetes. Diabet Med. 2008;25:792–797. doi: 10.1111/j.1464-5491.2008.02468.x. [DOI] [PubMed] [Google Scholar]
- 4.Lindholm A, Jensen LB, Home PD, Raskin P, Boehm BO, Rastam J. Immune responses to insulin aspart and biphasic insulin aspart in people with type 1 and type 2 diabetes. Diabetes Care. 2002;25:876–882. doi: 10.2337/diacare.25.5.876. [DOI] [PubMed] [Google Scholar]
- 5.Radermecker RP, Scheen AJ. Allergy reactions to insulin: effects of continuous subcutaneous insulin infusion and insulin analogues. Diabetes Metab Res Rev. 2007;23:348–355. doi: 10.1002/dmrr.714. [DOI] [PubMed] [Google Scholar]
- 6.Radermecker RP, Pierard GE, Scheen AJ. Lipodystrophy reactions to insulin: effects of continuous insulin infusion and new insulin analogs. Am J Clin Dermatol. 2007;8:21–28. doi: 10.2165/00128071-200708010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Davidson JK, DeBra DW. Immunologic insulin resistance. Diabetes. 1978;27:307–318. doi: 10.2337/diab.27.3.307. [DOI] [PubMed] [Google Scholar]
- 8.Hattori N, Duhita MR, Mukai A, Matsueda M, Shimatsu A. Development of insulin antibodies and changes in titers over a long-term period in patients with type 2 diabetes. Clin Chim Acta. 2014;433:135–138. doi: 10.1016/j.cca.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Havelund S, Plum A, Ribel U, et al. The mechanism of protraction of insulin detemir, a long-acting, acylated analog of human insulin. Pharm Res. 2004;21:1498–1504. doi: 10.1023/B:PHAM.0000036926.54824.37. [DOI] [PubMed] [Google Scholar]
- 10.Bartley PC, Bogoev M, Larsen J, Philotheou A. Long-term efficacy and safety of insulin detemir compared to neutral protamine Hagedorn insulin in patients with type 1 diabetes using a treat-to-target basal-bolus regimen with insulin aspart at meals: a 2-year, randomized, controlled trial. Diabet Med. 2008;25:442–449. doi: 10.1111/j.1464-5491.2007.02407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brange J, Owens DR, Kang S, Volund A. Monomeric insulins and their experimental and clinical implications. Diabetes Care. 1990;13:923–954. doi: 10.2337/diacare.13.9.923. [DOI] [PubMed] [Google Scholar]
- 12.Thalange N, Bereket A, Larsen J, Hiort LC, Peterkova V. Treatment with insulin detemir or NPH insulin in children aged 2–5 year with type 1 diabetes mellitus. Pediatr Diabetes. 2011;12:632–641. doi: 10.1111/j.1399-5448.2010.00750.x. [DOI] [PubMed] [Google Scholar]
- 13.Thalange N, Bereket A, Larsen J, Hiort LC, Peterkova V. Insulin analogues in children with type 1 diabetes: a 52-week randomized clinical trial. Diabet Med. 2013;30:216–225. doi: 10.1111/dme.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Conference on Harmonisation. ICH harmonised tripartite guideline. guideline for good clinical practice E6(R1). www.ich.org/products/guidelines/efficacy/article/efficacy-guidelines.html. Accessed Nov 2015.
- 15.World Medical Association. WMA Declaration of Helsinki—Ethical principles for medical research involving human subjects. www.wma.net/en/20activities/10ethics/10helsinki/index.html. Accessed Nov 2015.
- 16.International Society for Pediatric and Adolescent Diabetes. ISPAD Clinical Practice Consensus Guidelines 2009. www.ispad.org/?page=ISPADClinical. Accessed Nov 2015.
- 17.Clarke W, Jones T, Rewers A, Dunger D, Klingensmith GJ. Assessment and management of hypoglycemia in children and adolescents with diabetes. Pediatr Diabetes. 2008;9:165–174. doi: 10.1111/j.1399-5448.2008.00405.x. [DOI] [PubMed] [Google Scholar]
- 18.Cole TJ, Freeman JV, Preece MA. British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med. 1998;17:407–429. doi: 10.1002/(SICI)1097-0258(19980228)17:4<407::AID-SIM742>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 19.Russell-Jones D, Simpson R, Hylleberg B, Draeger E, Bolinder J. Effects of QD insulin detemir or neutral protamine Hagedorn on blood glucose control in patients with type 1 diabetes mellitus using a basal–bolus regimen. Clin Ther. 2004;26:724–736. doi: 10.1016/S0149-2918(04)90072-0. [DOI] [PubMed] [Google Scholar]
- 20.Standl E, Lang H, Roberts A. The 12-month efficacy and safety of insulin detemir and NPH insulin in basal–bolus therapy for the treatment of type 1 diabetes. Diabetes Technol Ther. 2004;6:579–588. doi: 10.1089/dia.2004.6.579. [DOI] [PubMed] [Google Scholar]
- 21.Fineberg SE, Kawabata TT, Finco-Kent D, et al. Immunological response to exogenous insulin. Endocr Rev. 2007;28:625–652. doi: 10.1210/er.2007-0002. [DOI] [PubMed] [Google Scholar]
- 22.Ilag LL, Deeg MA, Costigan T, et al. Evaluation of immunogenicity of LY2963016 insulin glargine compared with Lantus® insulin glargine in patients with type 1 or type 2 diabetes mellitus. Diabetes Obes Metab. 2016;18:159–168. doi: 10.1111/dom.12584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perantie DC, Lim A, Wu J, et al. Effects of prior hypoglycemia and hyperglycemia on cognition in children with type 1 diabetes mellitus. Pediatr Diabetes. 2008;9:87–95. doi: 10.1111/j.1399-5448.2007.00274.x. [DOI] [PubMed] [Google Scholar]
- 24.Wiegand S, Raile K, Reinehr T, et al. Daily insulin requirement of children and adolescents with type 1 diabetes: effect of age, gender, body mass index and mode of therapy. Eur J Endocrinol. 2008;158:543–549. doi: 10.1530/EJE-07-0904. [DOI] [PubMed] [Google Scholar]
- 25.Robertson KJ, Schoenle E, Gucev Z, Mordhorst L, Gall MA, Ludvigsson J. Insulin detemir compared with NPH insulin in children and adolescents with type 1 diabetes. Diabet Med. 2007;24:27–34. doi: 10.1111/j.1464-5491.2007.02024.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.