Abstract
Coronary revascularization decisions for patients with CKD stage 5D present a dilemma for clinicians because of high baseline risks of mortality and future cardiovascular events. This population differs from the general population regarding characteristics of coronary plaque composition and behavior, accuracy of noninvasive testing, and response to surgical and percutaneous revascularization, such that findings from the general population cannot be automatically extrapolated. However, this high-risk population has been excluded from all randomized trials evaluating outcomes of revascularization. Observational studies have attempted to address long-term outcomes after surgical versus percutaneous revascularization strategies, but inherent selection bias may limit accuracy. Compared with percutaneous strategies, surgical revascularization seems to have long–term survival benefit on the basis of observational data but associates with substantially higher short–term mortality rates. Percutaneous revascularization with drug-eluting and bare metal stents associates with a high risk of in-stent restenosis and need for future revascularization, perhaps contributing to the higher long–term mortality hazard. Off–pump coronary bypass surgery and the newest generation of drug–eluting stent platforms offer no definitive benefits. In this review, we address the nuances, complexities, and tradeoffs that clinicians face in determining the optimal method of coronary revascularization for this high-risk population.
Keywords: coronary revascularization, chronic kidney disease, cardiovascular disease
Cardiovascular disease accounts for the highest proportion of deaths among patients with CKD stage 5 on dialysis (5D), a fact corroborated by registry data and adjudicated end points from randomized trial data.1,2 Revascularization for acute coronary syndromes (ACSs) constitutes 54% of all procedures among patients with CKD 5D in the United States.3 As a corollary, 46% of procedures occur in the context of stable coronary artery disease (CAD); for a sizeable proportion of these patients, incidental CAD is likely detected during evaluation for renal transplant surgery. Patients with CKD 5D arguably represent patients with some of the highest risk undergoing revascularization in the contemporary era. Studies consistently show gloomy survival rates of about 70% at 1 year and about 25% at 5 years after revascularization by either surgical or percutaneous technique.4,5 Not surprisingly, procedures occurring in the context of ACS are associated with higher mortality rates.3
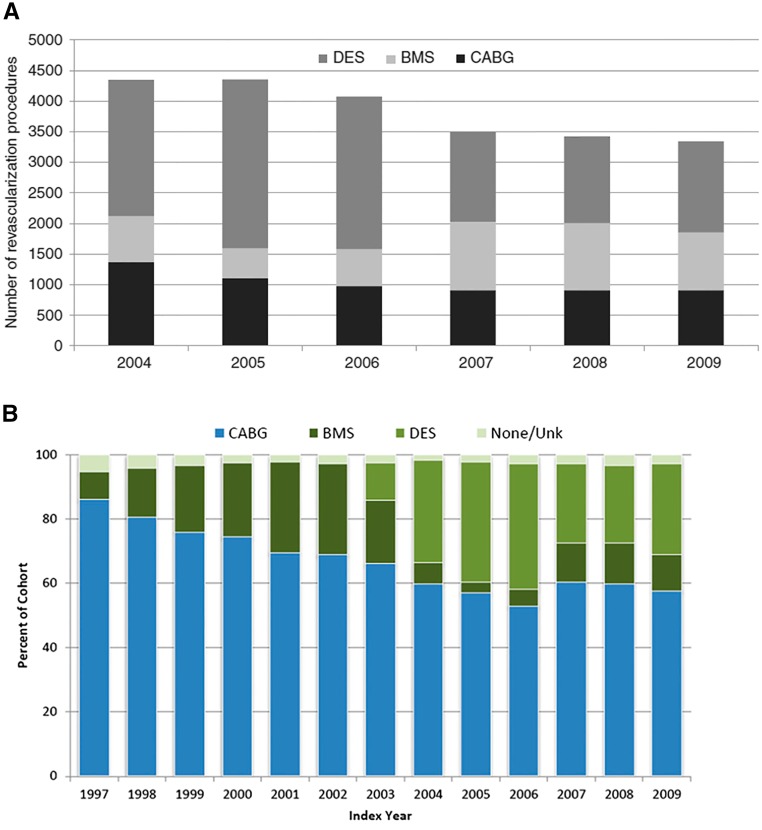
Revascularization trends in patients with CKD 5D in the United States in the past two decades have mirrored those in the general population. Between 2004 and 2009, an overall decrease in annual revascularization procedures occurred.4 The average volume of coronary artery bypass graft (CABG) surgeries remained relatively constant at about 25%–30% of total procedures, but from 2006 to 2007, use of drug-eluting stents (DESs) decreased markedly, with a corresponding increase in use of bare metal stents (BMSs) (Figure 1A). Among patients with CKD 5D with multivessel CAD between 1997 and 2009, the volume of CABG procedures was much higher, reaching a peak of about 86% in 1997, steadily dropping to a nadir of 53% in 2006, and subsequently plateauing at about 60% thereafter.5 Conversely, DESs constituted 87% of all percutaneous coronary intervention (PCI) procedures in 2005 but tapered to about 61% in 2008 (Figure 1B). These corroborative observations of nationwide trends have vital implications for both short– and long–term mortality rates in this population.
Figure 1.
Temporal trends in coronary revascularization procedures among CKD 5D patients in the United States. (A) Trends in coronary revascularization procedures with CABG, DES, and BMS from 2004 to 2009 using data from the US Renal Data System.4 Reprinted from Shroff et al.4, with permission. (B) Trends in multivessel revascularization with CABG, DES, and BMS from 1997 to 2009 using data from the US Renal Data System.5 Unk, unknown. Reprinted from Chang et al.5, with permission.
Coronary Plaque Characteristics and Noninvasive Imaging
Coronary atherosclerotic lesions in patients with advanced CKD differ substantially from those in the general population, but the vulnerability of plaques in patients with advanced CKD is a matter of controversy. It has been shown that worsening CKD is accompanied by a higher lipid/necrotic core, lower fibrous content,6,7 increased neovascularization, and intraplaque hemorrhage,8 factors that predispose to increased vulnerability to plaque rupture. Another school of thought suggests that, with worsening CKD, the proportion of calcific/necrotic core increases, possibly leading to greater plaque stability.9 An autopsy study showed that, despite the overall plaque area being comparable, patients with ESRD have greater coronary calcification and medial thickness compared with more fibroatheromatous plaques in patients without kidney disease.10
The quest for the optimal noninvasive modality to detect obstructive CAD has been contentious. Selecting patients with advanced CKD for noninvasive evaluation is particularly challenging for clinicians because of a variety of influencing factors, including frequent lack of typical anginal symptoms; structural/physiologic considerations affecting stress testing, such as marked left ventricular hypertrophy and impaired coronary reserve; and high prevalence of baseline troponin levels in asymptomatic patients. Although baseline troponin elevations have been shown to predict a two- to fivefold increase in mortality in patients with ESRD,11 they lack specificity in predicting obstructive CAD in asymptomatic patients (probably reflecting nonatherosclerotic mechanisms, such as apoptosis). Experts have suggested screening algorithms for asymptomatic patients with CKD 5D on the basis of clinical risk factors and biomarkers.12 However, caution would be prudent in the use of such algorithms, which have not been shown to affect meaningful outcomes.
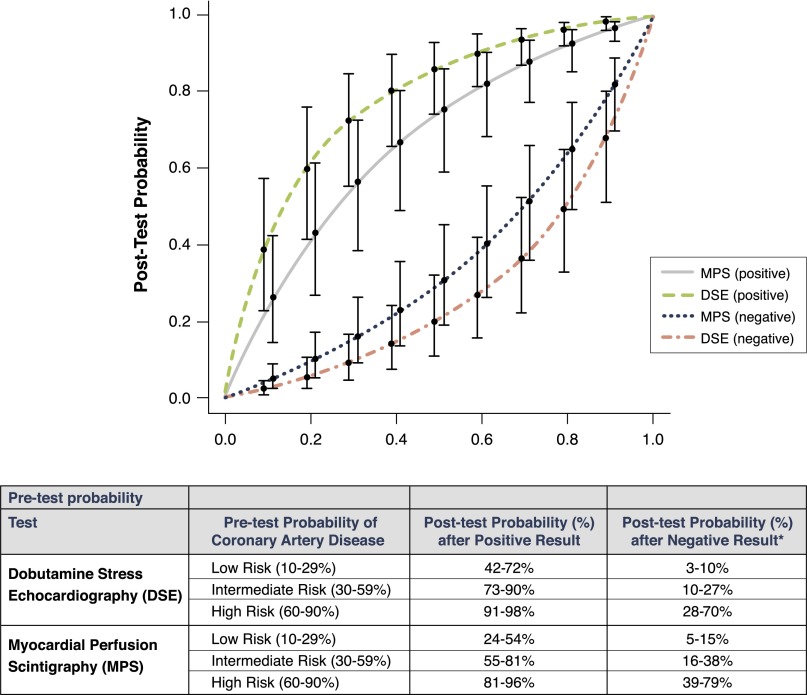
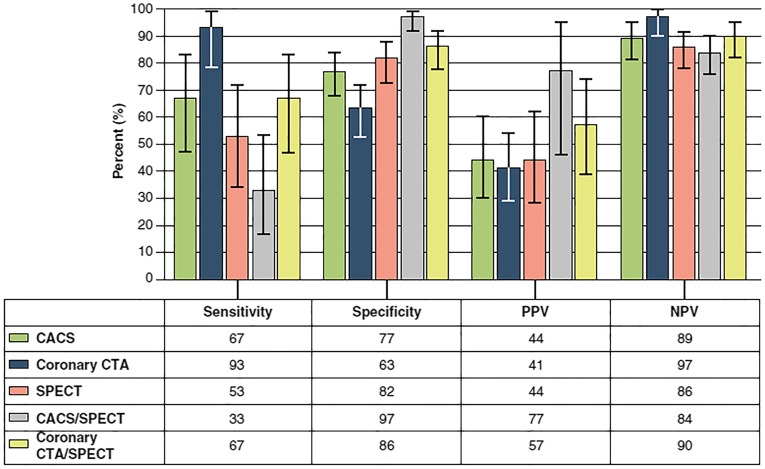
A high proportion of noninvasive evaluation in patients with CKD 5D occurs in the context of evaluation for renal transplant. In a pooled analysis of smaller studies comparing dobutamine stress echocardiography with myocardial perfusion imaging (MPI),13 both modalities had moderate sensitivity/specificity for detecting CAD among renal transplant candidates. The authors concluded that dobutamine stress echocardiography was more accurate than MPI when all studies were included (Figure 2).13 The decrease in microcirculatory flow reserve in CKD has been postulated to reduce the responsiveness to vasodilation with MPI. Winther et al.14 prospectively studied 138 patients (43% on dialysis) undergoing pretransplant evaluation by obtaining MPI, computed tomography coronary angiography (CCTA), coronary artery calcium (CAC), and invasive coronary angiography on every patient. The overall prevalence of obstructive CAD (>50% stenosis) was 22%, and two thirds of these patients had proximal epicardial stenosis. This was the first study to show that the sensitivity to detect obstructive CAD with structural imaging outperformed functional evaluation in this population (93% CCTA versus 53% MPI) (Figure 3). However, MPI had higher specificity for obstructive CAD (82% versus 63% CCTA). In this study, CAC was prevalent in 75% of the population. Using a threshold of 400 Agatston units, CAC had 67% sensitivity and 77% specificity to predict obstructive CAD compared with invasive coronary angiography.
Figure 2.
Accuracy of dobutamine stress echocardiography versus myocardial perfusion scintigraphy for diagnosing CAD in renal transplant candidates. Receiver operating characteristic curves for diagnosing CAD in renal transplant candidates.13 Modified from Wang et al.13, with permission.
Figure 3.
A comparison of accuracy of various non-invasive imaging techniques to detect CAD in renal transplant candidates. Diagnostic performance of noninvasive imaging modalites during evaluation for renal transplant compared with invasive coronary angiography.14 CACS, coronary artery calcium score; CTA, computed tomogram angiography; NPV, negative predictive value; PPV, positive predictive value; SPECT, single–photon emission computed tomography. Reprinted from Winther et al.14, with permission.
Surgical Versus Percutaneous Revascularization: Lessons from Observational Studies
Despite the high-risk nature of this population, patients with CKD 5D have been systematically excluded from randomized trials. Clinicians are, therefore, forced to rely on observational studies for guidance regarding optimal strategies. Despite the best statistical maneuvering, the problems of selection bias and unmeasured confounders cannot be surmounted in the absence of randomization. Several clinical variables cannot be identified accurately in observational studies derived from administrative data, such as assessment of revascularization completeness and differentiating between future repeat target lesion and target vessel revascularization.
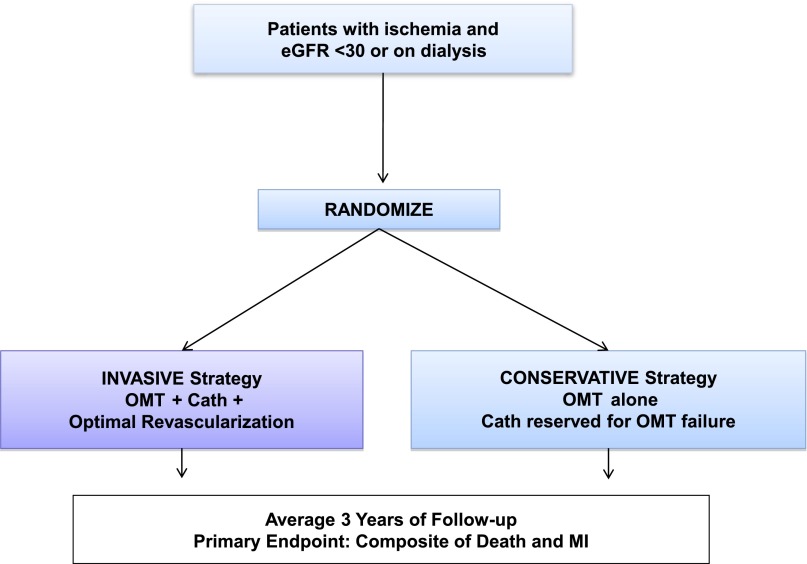
An important question to address a priori relates to the benefit of revascularization compared with optimal medical therapy alone in patients with stable CAD. The issue is particularly relevant given the high baseline mortality in this population and the potential for asymptomatic CAD to be detected while screening renal transplant candidates. Hemmelgarn et al.15 collected information about patients on dialysis undergoing cardiac catheterization; adjusted 8-year survival rates were 44.8% for CABG, 41.2% for PCI, and 30.4% for patients who did not undergo revascularization. Survival was worse without revascularization, but the patients who did not undergo revascularization likely had substantial comorbidity that obviated it. Without accounting for the selection biases inherent in the decision to undergo revascularization, this study does not definitively address the issue of whether coronary revascularization indeed improves outcomes. The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches—Chronic Kidney Disease (ISCHEMIA-CKD) Trial (clinicaltrials.gov identifier NCT01985360), sponsored by the National Heart, Lung, and Blood Institute, is currently enrolling participants with CKD to evaluate this matter more definitively (Figure 4).16
Figure 4.
The ISCHEMIA-CKD Trial. Design of the ongoing ISCHEMIA-CKD Trial sponsored by the National Heart, Lung, and Blood Institute. Cath, cardiac catheterization/coronary angiography; OMT, optimal medical therapy.
Studies spanning several decades have sequentially compared outcomes after CABG with outcomes after percutaneous transluminal coronary angioplasty, BMS, and DES among patients with CKD 5D and consistently showed a long–term survival advantage of CABG over percutaneous techniques.4,5,17–19 Nevis et al.20 performed a systematic review of the literature to amalgamate data between 1977 and 2002. Of the 17 studies meeting qualifications, most were small with considerable heterogeneity in patient characteristics, statistical methodology, and outcome variables, limiting the ability to derive definitive conclusions. In an exploratory meta-analysis, the pooled absolute 30-day mortality was significantly higher with CABG versus PCI (10.6% versus 5.4%; unadjusted relative risk, 1.91; 95% confidence interval [95% CI], 1.44 to 2.52). Over long–term follow-up (mean duration of 28–31 months), cumulative mortality was favorable for CABG over PCI (51.6% versus 59.5%; unadjusted, 0.93; 95% CI, 0.88 to 0.98; P<0.01).
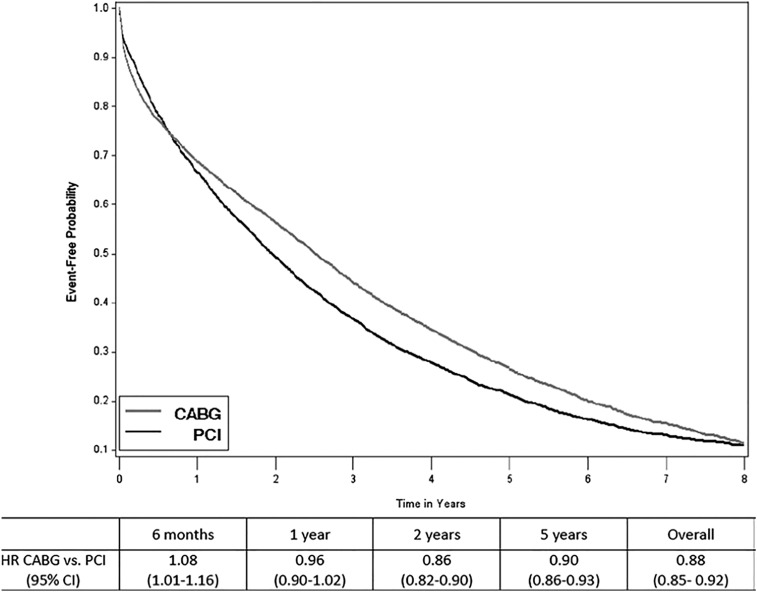
Since this systematic review, large observational studies have explored trends and outcomes in revascularization among patients on dialysis in the contemporary era of newer generation stents. Chang et al.5 evaluated 21,981 patients with ESRD undergoing multivessel revascularization from 1997 to 2009. CABG was independently associated with significant reduction in 5-year hazard for mortality versus PCI (hazard ratio [HR], 0.87; 95% CI, 0.84 to 0.9). Interestingly, there was a higher initial mortality hazard with CABG (Figure 5). Survival was comparable at 1 year but favorable for CABG at 2 years from the index revascularization and sustained thereafter. In an analysis of revascularization outcomes among patients on dialysis from 2004 to 2009,4 in-hospital mortality for patients undergoing CABG (n=6178) was 8.2%; 1- and 5-year survival rates were 70% and 28%, respectively. For patients undergoing PCI with DES (n=11,844) and BMS (n=5011), in–hospital mortality rates were 2.7% and 4.9%, respectively, and 1- and 5-year survival rates were 71% and 24% and 63% and 19%, respectively. Accounting for high competing risks of death, the probability of repeat revascularization was much higher in the PCI group: 29% with DES and 25% with BMS versus 12.5% with CABG as the index procedure. Bangalore et al.19 assessed outcomes with CABG versus PCI with newer generation everolimus–eluting stents in multivessel CAD from 2008 to 2011. Among the 486 patients on dialysis identified from 11,305 patients with CKD, a twofold higher hazard of long-term mortality was noted with PCI versus CABG (54.3% versus 39.1%; HR, 2.02; 95% CI, 1.4 to 2.93; P<0.001), findings that contrast with findings from the general population.21 Importantly, PCI was also associated with a higher hazard of future myocardial infarction (MI; 31.9% versus 16.7%; HR, 1.68; 95% CI, 0.99–2.85; P=0.05) and repeat revascularization (48.3% versus 25%; HR, 2.44; 95% CI, 1.50–3.96; P<0.001).
Figure 5.
Long-term survival of CABG vs. PCI among dialysis patients with multivessel CAD. Kaplan–Meier curves for all-cause survival between CABG and PCI among patients on dialysis undergoing multivessel PCI between 1997 and 2009 in the United States.5 Reprinted from Chang et al.5, with permission.
In summary, despite the absence of randomized data, the signal is clear from observational data spanning several decades indicating a long–term survival advantage of CABG and reduced rates of future revascularization in patients with CKD 5D but at the cost of a significantly higher short–term mortality hazard relative to PCI. Notably, similar thematic conclusions of favorable benefits of CABG versus PCI have been drawn in observational studies of patients with nondialysis-dependent CKD.22,23 Conceivably, the high short–term mortality after CABG selects out a population that is more likely to have an improved long–term survival advantage. However, despite the consistent observations of long-term benefits from surgical revascularization, current societal guidelines do not specifically endorse any revascularization approach in the CKD 5D population.
CABG Versus PCI: Special Considerations
Off-Pump Versus On-Pump CABG and Use of the Internal Mammary Artery
High short–term mortality rates in patients with CKD 5D have remained the Achilles heel of surgical revascularization.24 The endeavor to reduce in-hospital mortality raised valid questions about the potential benefit of off–pump coronary artery bypass (OPCAB) relative to on–pump coronary artery bypass (ONCAB) surgery. In a large dialysis cohort (n=13,085; 18% OPCAB) from 2001 to 2006, a modestly decreased hazard of all-cause mortality was noted in favor of OPCAB (HR, 0.92; 95% CI, 0.86 to 0.99); the survival benefit was apparent in the first year after surgery and disappeared after 2 years.25 Importantly, in-hospital mortality with OPCAB versus ONCAB was similar (9.7% versus 11.0%; P=0.06). Lim et al.26 performed a meta-analysis of 10 observational studies comparing these surgical approaches in patients with ESRD (OPCAB, n=2762; ONCAB, n=11,310); they concluded that in–hospital, short–term, and longer–term mortality rates were comparable between the two groups.26 Hence, the available evidence suggests no meaningful survival advantage of OPCAB versus ONCAB.
Use of the internal mammary artery (IMA) during CABG has a proven benefit in the general population, and observational data indicate similar findings in patients on dialysis. Among 13,085 patients on dialysis undergoing CABG from 2001 to 2006, IMA use was independently associated with improved survival (HR, 0.92; 95% CI, 0.87 to 0.98; P<0.01).25 In a more contemporary cohort of patients on dialysis undergoing CABG from 2004 to 2009, IMA use was independently associated with reduced mortality (HR, 0.83; 95% CI, 0.77 to 0.9; P<0.001).4 However, complete arterial revascularization with bilateral IMAs has not been shown to affect survival.27 The left internal mammary artery (LIMA) is conventionally anastomosed to the left anterior descending artery (LAD); use of the LIMA is, thus, likely a surrogate of successful revascularization of the anterior circulation (i.e., there is significant disease in the LAD necessitating revascularization, and equally importantly, the LAD is of sufficient caliber to be anatomically suitable for coronary revascularization with a LIMA graft). Although there are documented cases of myocardial ischemia induced by hemodialysis in patients with LIMA grafts and ipsilateral upper extremity arteriovenous (AV) fistula,28,29 the overall clinical importance of this issue is still uncertain; the presence of a left arm AV fistula should not (in our opinion) proscribe the use of a LIMA graft.
In recent years, an optimistic nationwide trend has emerged. Parikh et al.30 reported a dramatic decline in in-hospital mortality from 31% to 5.4% between 1988 and 2003 among patients with ESRD undergoing CABG without valve surgery, compared with from 4.7% to 1.8%, respectively, among patients without ESRD. Pertinently, the median length of hospital stay also declined from 25 to 13 days. The authors hypothesized that these hopeful data in the face of increasing surgical volumes/experience likely represent advancement in techniques for temperature management during surgery, myocardial preservation, and reducing atheroembolic complications along with increasing expertise in minimally invasive techniques.30 Improved patient selection and better perioperative (including improved dialysis) management likely also contribute. Importantly, these data30 underline the fact that in-hospital mortality in patients with ESRD after CABG remains threefold higher than that in patients without ESRD in the contemporary era.
DES Versus BMS: Mortality and In-Stent Restenosis
Hemodialysis is an independent predictor of mortality among patients undergoing DES placement.31 However, among patients with CKD, in general, DES is deemed safer than BMS and associated with improved survival,32–35 although not all studies are concordant in this regard.36 In a large cohort of 121,446 patients with CKD, Tsai et al.37 reported that, at all stages of CKD, DES was associated with improved survival compared with BMS. Survival after BMS is lower than after either CABG or DES among patients with CKD 5D in both ACS and non-ACS settings.3,4 However, trends in coronary revascularization showed an uptick in BMS use in 2007–2009 in the United States, probably coincident with nationwide concerns regarding the risk of stent thrombosis with DES. Although deriving firm conclusions from these observational data is problematic, it is conceivable that patients undergoing BMS placement in clinical practice reflect a sicker population that is not eligible for revascularization with other modalities because of clinical contraindications, such as bleeding diathesis, predisposition to major bleeding, inability to receive long–term antiplatelet therapy because of concern regarding bleeding complications, or likelihood of major surgery in the near future.
Observational data are also convincing in showing that patients with CKD 5D have a high incidence of in-stent restenosis, regardless of whether they have DES or BMS platforms (approximately 22%–30% DES and 24%–40% BMS), signaling need for future revascularization.25,38–40 Hemodialysis has been identified as an independent predictor of repeat target lesion revascularization after both sirolimus- (19.4% versus 6.6%; P<0.001)31 and paclitaxel-eluting (odds ratio, 6.6; 95% CI, 2.34 to 18.6) stents41; the newer generation of everolimus-eluting stents likely has lower in–stent restenosis rates.42 Hemodialysis was an independent predictor of major adverse cardiovascular outcomes at 2 years after DES among patients with CKD 5D versus patients without CKD driven by higher mortality (12% versus 0.6%) and target vessel revascularization (24% versus 9%) rates.43
Effect of Acute MI/ACS on Revascularization Outcomes
Patients with CKD 5D who experience an acute MI have markedly elevated 1- and 2-year mortality rates of 59% and 73%, respectively.44 Recent trends (1993–2008) show reduced in–hospital mortality from 32% to 18%, but this was apparent only among patients with ST segment elevation MI.45 Chang et al.5 included a sizable representation of patients on dialysis with MI as index presentation (18% in the CABG arm and 26% in the PCI arm). In secondary analysis of prespecified subgroups, the authors reported that the overall study results of improved long–term survival with multivessel CABG versus PCI also applied to patients with MI on index presentation.5 We evaluated survival outcomes of patients with CKD 5D undergoing revascularization in ACS versus non-ACS settings from 2004 to 2009.3 All–cause mortality rates at both short- and long-term intervals with both CABG and PCI were higher when the procedure occurred in the context of ACS. In ACS settings (n=12,473; 54%), revascularization with DES was an independent predictor of mortality compared with CABG (HR, 1.08; 95% CI, 1.02 to 1.15; P<0.01). However, in the absence of ACS (n=10,560; 46%), mortality was similar in the CABG and DES arms (HR, 1.01; 95% CI, 0.95 to 1.07). Thus, patients with ACS represent a higher-risk group that derives a greater long–term survival benefit with surgical revascularization.
Putting It All Together: Pragmatic Tradeoffs in the Choice of Coronary Revascularization Strategy among Patients with CKD 5D
Choosing the optimal coronary revascularization procedure for any patient is complex and multifaceted but especially so for patients with CKD 5D because of the higher risk of mortality and future revascularization. The bleak long–term survival of patients with CKD 5D undergoing any revascularization is a unifying theme and a common denominator underlying the choice of any strategy pursued. We strongly recommended a heart team approach that includes the patient and the nephrologist for careful deliberation of the tradeoffs and nuances involved. Clinicians need to consider the variables discussed above in the choice of revascularization strategy: extent and location of coronary involvement, necessity for and ability to use the LIMA (including complicating factors, such as left arm AV fistula for hemodialysis access), probability of repeat revascularization, bleeding risk and imminent major surgeries, coexisting or anticipated progression of valve disease, anticipated life expectancy and comorbidity that may affect perioperative and short-term survival, institutional experience/volume, and, certainly, the patient’s preference. We cannot overemphasize the importance of a patient-centered approach to these complex decisions regarding coronary revascularization in patients on dialysis.
Despite the evolution of PCI techniques and development of newer generations of DES, the survival advantage of CABG in patients with CKD 5D seems to be quite consistent over the years. This could be explained by potential benefits of CABG or relative lack of benefit of DES. The rationale underlying a survival benefit with CABG is akin to that for patients with diabetes and severe proximal multivessel CAD46,47 likely stemming from complete revascularization in the context of extensive CAD, including the anterior circulation, compared with relatively incomplete revascularization with PCI that typically targets areas with the most severe stenosis. Another potential explanation is downstream protection offered by CABG from future plaque rupture in multiple coronary beds in patients vulnerable to recurrent plaque ruptures. Clinicians should explicitly discuss with their patients the tradeoffs of considerably higher upfront risk of in-hospital mortality with CABG but long–term survival benefit and reduced probability of future revascularization. Notably, use of the LIMA seems to be an important determinant of the success of CABG. Inability to use the LIMA raises legitimate but unanswered questions about any benefit of CABG over PCI with DES. Need for future revascularization is another important determinant of long-term outcomes; PCI with either DES or BMS associates with significantly higher rates of repeat revascularization compared with CABG,4 probably reflecting the higher rates of in-stent restenosis. Clinical events caused by in-stent restenosis and downstream revascularization could contribute to the increased mortality hazard with DES in the long term.43 The signal pertaining to adverse clinical outcomes with BMS seems to be quite consistent as well, despite the observational nature of the data; BMS would seem to be a less preferable clinical choice unless extenuating circumstances exist, such as major bleeding diathesis or upcoming high–risk surgery.
On the basis of differences in short– and long–term mortality rates in the ACS and non-ACS settings, it seems prudent for future studies evaluating outcomes after coronary revascularization to distinguish the clinical context. Perhaps this observation more broadly identifies patients more or less vulnerable (ACS versus non-ACS setting) to future plaque rupture. Specifically, in a non-ACS setting, probably because of lower baseline mortality, the longer-term advantage of CABG may be attenuated relative to DES. Taking a step back, it would be particularly relevant to fundamentally assess the benefits of any revascularization over optimal medical therapy alone in stable CAD; the authors appeal to the medical community to consider referral of these patients for enrollment in the ISCHEMIA-CKD Trial, because evidence from a randomized study in this matter is sorely needed, and it is rare for patients with CKD 5D to be offered the opportunity to enroll in one. Finally, we hope for a randomized trial comparing long-term survival after surgical versus percutaneous revascularization, which will be the only means of obtaining definitive answers in this complex population.
Disclosures
None.
Acknowledgments
The authors thank Chronic Disease Research Group colleague Nan Booth for manuscript editing.
This work was supported by the Chronic Disease Research Group, Minneapolis Medical Research Foundation.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.US Renal Data System : USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 2.Wheeler DC, London GM, Parfrey PS, Block GA, Correa-Rotter R, Dehmel B, Drüeke TB, Floege J, Kubo Y, Mahaffey KW, Goodman WG, Moe SM, Trotman ML, Abdalla S, Chertow GM, Herzog CA; EValuation Of Cinacalcet HCl Therapy to Lower CardioVascular Events (EVOLVE) Trial Investigators : Effects of cinacalcet on atherosclerotic and nonatherosclerotic cardiovascular events in patients receiving hemodialysis: The EValuation Of Cinacalcet HCl Therapy to Lower CardioVascular Events (EVOLVE) trial. J Am Heart Assoc 3: e001363, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shroff GR, Solid CA, Herzog CA: Impact of acute coronary syndromes on survival of dialysis patients following surgical or percutaneous coronary revascularization in the United States. Eur Heart J Acute Cardiovasc Care 5: 205–213, 2016 [DOI] [PubMed] [Google Scholar]
- 4.Shroff GR, Solid CA, Herzog CA: Long-term survival and repeat coronary revascularization in dialysis patients after surgical and percutaneous coronary revascularization with drug-eluting and bare metal stents in the United States. Circulation 127: 1861–1869, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang TI, Shilane D, Kazi DS, Montez-Rath ME, Hlatky MA, Winkelmayer WC: Multivessel coronary artery bypass grafting versus percutaneous coronary intervention in ESRD. J Am Soc Nephrol 23: 2042–2049, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayano S, Ichimiya S, Ishii H, Kanashiro M, Watanabe J, Kurebayashi N, Yoshikawa D, Amano T, Matsubara T, Murohara T: Relation between estimated glomerular filtration rate and composition of coronary arterial atherosclerotic plaques. Am J Cardiol 109: 1131–1136, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Baber U, Stone GW, Weisz G, Moreno P, Dangas G, Maehara A, Mintz GS, Cristea E, Fahy M, Xu K, Lansky AJ, Wennerblom B, Mathey DG, Templin B, Zhang Z, Serruys PW, Mehran R: Coronary plaque composition, morphology, and outcomes in patients with and without chronic kidney disease presenting with acute coronary syndromes. JACC Cardiovasc Imaging 5[Suppl]: S53–S61, 2012 [DOI] [PubMed] [Google Scholar]
- 8.Nakano T, Ninomiya T, Sumiyoshi S, Onimaru M, Fujii H, Itabe H, Nakashima Y, Sueishi K, Tsuruya K, Oda Y, Kitazono T, Kiyohara Y: Chronic kidney disease is associated with neovascularization and intraplaque hemorrhage in coronary atherosclerosis in elders: Results from the Hisayama Study. Kidney Int 84: 373–380, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Kono K, Fujii H, Nakai K, Goto S, Shite J, Hirata K, Fukagawa M, Nishi S: Composition and plaque patterns of coronary culprit lesions and clinical characteristics of patients with chronic kidney disease. Kidney Int 82: 344–351, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Nakano T, Ninomiya T, Sumiyoshi S, Fujii H, Doi Y, Hirakata H, Tsuruya K, Iida M, Kiyohara Y, Sueishi K: Association of kidney function with coronary atherosclerosis and calcification in autopsy samples from Japanese elders: the Hisayama study. Am J Kidney Dis 55: 21–30, 2010 [DOI] [PubMed] [Google Scholar]
- 11.Apple FS, Murakami MM, Pearce LA, Herzog CA: Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation 106: 2941–2945, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Hakeem A, Bhatti S, Chang SM: Screening and risk stratification of coronary artery disease in end-stage renal disease. JACC Cardiovasc Imaging 7: 715–728, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Wang LW, Fahim MA, Hayen A, Mitchell RL, Baines L, Lord S, Craig JC, Webster AC: Cardiac testing for coronary artery disease in potential kidney transplant recipients. Cochrane Database Syst Rev 12: CD008691, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Winther S, Svensson M, Jørgensen HS, Bouchelouche K, Gormsen LC, Pedersen BB, Holm NR, Bøtker HE, Ivarsen P, Bøttcher M: Diagnostic performance of coronary CT angiography and myocardial perfusion imaging in kidney transplantation candidates. JACC Cardiovasc Imaging 8: 553–562, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Hemmelgarn BR, Southern D, Culleton BF, Mitchell LB, Knudtson ML, Ghali WA; Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease (APPROACH) Investigators : Survival after coronary revascularization among patients with kidney disease. Circulation 110: 1890–1895, 2004 [DOI] [PubMed] [Google Scholar]
- 16.New York University School of Medicine: International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA)-Chronic Kidney Disease Trial, 2016. Available at: https://clinicaltrials.gov/ct2/show/NCT01985360. Accessed March 16, 2016
- 17.Herzog CA, Ma JZ, Collins AJ: Long-term outcome of dialysis patients in the United States with coronary revascularization procedures. Kidney Int 56: 324–332, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Herzog CA, Ma JZ, Collins AJ: Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation 106: 2207–2211, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Bangalore S, Guo Y, Samadashvili Z, Blecker S, Xu J, Hannan EL: Revascularization in patients with multivessel coronary artery disease and chronic kidney disease: Everolimus-eluting stents versus coronary artery bypass graft surgery. J Am Coll Cardiol 66: 1209–1220, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nevis IF, Mathew A, Novick RJ, Parikh CR, Devereaux PJ, Natarajan MK, Iansavichus AV, Cuerden MS, Garg AX: Optimal method of coronary revascularization in patients receiving dialysis: Systematic review. Clin J Am Soc Nephrol 4: 369–378, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bangalore S, Guo Y, Samadashvili Z, Blecker S, Xu J, Hannan EL: Everolimus-eluting stents or bypass surgery for multivessel coronary disease. N Engl J Med 372: 1213–1222, 2015 [DOI] [PubMed] [Google Scholar]
- 22.Charytan DM, Li S, Liu J, Herzog CA: Risks of death and end-stage renal disease after surgical compared with percutaneous coronary revascularization in elderly patients with chronic kidney disease. Circulation 126[Suppl 1]: S164–S169, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan W, Ivanov J, Ko D, Fremes S, Rao V, Jolly S, Cantor WJ, Lavi S, Overgaard CB, Ruel M, Tu JV, Džavík V: Clinical outcomes of treatment by percutaneous coronary intervention versus coronary artery bypass graft surgery in patients with chronic kidney disease undergoing index revascularization in Ontario. Circ Cardiovasc Interv 8: 8, 2015 [DOI] [PubMed] [Google Scholar]
- 24.Liu JY, Birkmeyer NJ, Sanders JH, Morton JR, Henriques HF, Lahey SJ, Dow RW, Maloney C, DiScipio AW, Clough R, Leavitt BJ, O’Connor GT; Northern New England Cardiovascular Disease Study Group : Risks of morbidity and mortality in dialysis patients undergoing coronary artery bypass surgery. Circulation 102: 2973–2977, 2000 [DOI] [PubMed] [Google Scholar]
- 25.Shroff GR, Li S, Herzog CA: Survival of patients on dialysis having off-pump versus on-pump coronary artery bypass surgery in the United States. J Thorac Cardiovasc Surg 139: 1333–1338, 2010 [DOI] [PubMed] [Google Scholar]
- 26.Lim JY, Deo SV, Jung SH, Altarabsheh SE, Erwin PJ, Dillon JJ, Park SJ: Does off-pump coronary artery bypass confer any advantage in patients with end-stage renal failure? A systematic review and meta-analysis. Heart Lung Circ 24: 55–61, 2015 [DOI] [PubMed] [Google Scholar]
- 27.Nakatsu T, Tamura N, Sakakibara Y, Hagio K, Ishigami M: Long-term survival after coronary arterial grafts in patients with end-stage renal disease. Ann Thorac Surg 90: 738–743, 2010 [DOI] [PubMed] [Google Scholar]
- 28.Gaudino M, Serricchio M, Luciani N, Giungi S, Salica A, Pola R, Pola P, Luciani G, Possati G: Risks of using internal thoracic artery grafts in patients in chronic hemodialysis via upper extremity arteriovenous fistula. Circulation 107: 2653–2655, 2003 [DOI] [PubMed] [Google Scholar]
- 29.Coskun I, Colkesen Y, Altay H, Ozkan U, Demirturk OS, Gulcan O, Guvener M: Hemodynamic effects of left upper extremity arteriovenous fistula on ipsilateral internal mammary coronary artery bypass graft. Thorac Cardiovasc Surg 61: 663–667, 2013 [DOI] [PubMed] [Google Scholar]
- 30.Parikh DS, Swaminathan M, Archer LE, Inrig JK, Szczech LA, Shaw AD, Patel UD: Perioperative outcomes among patients with end-stage renal disease following coronary artery bypass surgery in the USA. Nephrol Dial Transplant 25: 2275–2283, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Otsuka Y, Ishiwata S, Inada T, Kanno H, Kyo E, Hayashi Y, Fujita H, Michishita I: Comparison of haemodialysis patients and non-haemodialysis patients with respect to clinical characteristics and 3-year clinical outcomes after sirolimus-eluting stent implantation: Insights from the Japan multi-centre post-marketing surveillance registry. Eur Heart J 32: 829–837, 2011 [DOI] [PubMed] [Google Scholar]
- 32.El-Menyar AA, Al Suwaidi J, Holmes DR Jr.: Use of drug-eluting stents in patients with coronary artery disease and renal insufficiency. Mayo Clin Proc 85: 165–171, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yachi S, Tanabe K, Tanimoto S, Aoki J, Nakazawa G, Yamamoto H, Otsuki S, Yagishita A, Kishi S, Nakano M, Taniwaki M, Sasaki S, Nakajima H, Mise N, Sugimoto T, Hara K: Clinical and angiographic outcomes following percutaneous coronary intervention with sirolimus-eluting stents versus bare-metal stents in hemodialysis patients. Am J Kidney Dis 54: 299–306, 2009 [DOI] [PubMed] [Google Scholar]
- 34.Abdel-Latif A, Mukherjee D, Mesgarzadeh P, Ziada KM: Drug-eluting stents in patients with end-stage renal disease: Meta-analysis and systematic review of the literature. Catheter Cardiovasc Interv 76: 942–948, 2010 [DOI] [PubMed] [Google Scholar]
- 35.Chang TI, Montez-Rath ME, Tsai TT, Hlatky MA, Winkelmayer WC: Drug-eluting versus bare-metal stents during PCI in patients with end-stage renal disease on dialysis. J Am Coll Cardiol 67: 1459–1469, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ichimoto E, Kobayashi Y, Iijima Y, Kuroda N, Kohno Y, Komuro I: Long-term clinical outcomes after sirolimus-eluting stent implantation in dialysis patients. Int Heart J 51: 92–97, 2010 [DOI] [PubMed] [Google Scholar]
- 37.Tsai TT, Messenger JC, Brennan JM, Patel UD, Dai D, Piana RN, Anstrom KJ, Eisenstein EL, Dokholyan RS, Peterson ED, Douglas PS: Safety and efficacy of drug-eluting stents in older patients with chronic kidney disease: A report from the linked CathPCI Registry-CMS claims database. J Am Coll Cardiol 58: 1859–1869, 2011 [DOI] [PubMed] [Google Scholar]
- 38.Ikari Y, Tanabe K, Koyama Y, Kozuma K, Sano K, Isshiki T, Katsuki T, Kimura K, Yamane M, Takahashi N, Hibi K, Hasegawa K, Ishiwata S, Kiyooka T, Yokoi H, Uehara Y, Hara K: Sirolimus eluting coronary stent implantation in patients on maintenance hemodialysis: The OUCH study (outcome of cypher stent inhemodialysis patients). Circ J 76: 1856–1863, 2012 [DOI] [PubMed] [Google Scholar]
- 39.Aoyama T, Ishii H, Toriyama T, Takahashi H, Kasuga H, Murakami R, Amano T, Uetani T, Yasuda Y, Yuzawa Y, Maruyama S, Matsuo S, Matsubara T, Murohara T: Sirolimus-eluting stents vs bare metal stents for coronary intervention in Japanese patients with renal failure on hemodialysis. Circ J 72: 56–60, 2008 [DOI] [PubMed] [Google Scholar]
- 40.Ishio N, Kobayashi Y, Takebayashi H, Iijima Y, Kanda J, Nakayama T, Kuroda N, De Gregorio J, Kouno Y, Suzuki M, Haruta S, Komuro I: Impact of drug-eluting stents on clinical and angiographic outcomes in dialysis patients. Circ J 71: 1525–1529, 2007 [DOI] [PubMed] [Google Scholar]
- 41.Takeuchi I, Moriguchi M, Imaki R, Fukaya H, Shinagawa H, Shimohama T, Tojo T, Fukuda N, Inomata T, Aoyama N, Soma K, Izumi T: Hemodialysis is an independent predictor of coronary in-stent restenosis after paclitaxel eluting stent implantation. Intern Med 49: 2379–2384, 2010 [DOI] [PubMed] [Google Scholar]
- 42.Sakakibara T, Ishii H, Toriyama T, Aoyama T, Takahashi H, Kamoi D, Kawamura Y, Kawashima K, Yoneda K, Amano T, Tanaka M, Yoshikawa D, Hayashi M, Matsubara T, Murohara T: Sirolimus-eluting stent vs. everolimus-eluting stent for coronary intervention in patients on chronic hemodialysis. Circ J 76: 351–355, 2012 [DOI] [PubMed] [Google Scholar]
- 43.Ota T, Umeda H, Yokota S, Miyata S, Takamura A, Sugino S, Hayashi K, Ishiki R, Takeichi Y, Iwase M, Inagaki H, Murohara T: Relationship between severity of renal impairment and 2-year outcomes after sirolimus-eluting stent implantation. Am Heart J 158: 92–98, 2009 [DOI] [PubMed] [Google Scholar]
- 44.Herzog CA, Ma JZ, Collins AJ: Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med 339: 799–805, 1998 [DOI] [PubMed] [Google Scholar]
- 45.Shroff GR, Li S, Herzog CA: Trends in mortality following acute myocardial infarction among dialysis patients in the United States over 15 years. J Am Heart Assoc 4: e002460, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Farkouh ME, Domanski M, Sleeper LA, Siami FS, Dangas G, Mack M, Yang M, Cohen DJ, Rosenberg Y, Solomon SD, Desai AS, Gersh BJ, Magnuson EA, Lansky A, Boineau R, Weinberger J, Ramanathan K, Sousa JE, Rankin J, Bhargava B, Buse J, Hueb W, Smith CR, Muratov V, Bansilal S, King S 3rd, Bertrand M, Fuster V; FREEDOM Trial Investigators : Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 367: 2375–2384, 2012 [DOI] [PubMed] [Google Scholar]
- 47.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators : Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 360: 961–972, 2009 [DOI] [PubMed] [Google Scholar]